Abstract
Background
A major barrier to adequate headache care is the relative lack of formal education and training of healthcare professionals. Concerted efforts should be made to pinpoint major gaps in knowledge in healthcare professionals to facilitate better educational policies in headache training. The aim of this study was to identify deficiencies and barriers in headache training among residents in neurology in Denmark.
Methods
We conducted a national cross-sectional survey of residents in neurology in Denmark from April 2019 to September 2019. The survey included questions on participant demographics, knowledge of and barriers in headache disorders, guidelines and diagnostic tools usage, contact with primary and tertiary care, medication overuse, and non-pharmacological interventions. Furthermore, respondents were asked to provide a ranked list from most to least interesting for six sub-specializations/disorders, i.e., cerebrovascular disease, dementia, epilepsy, headache, multiple sclerosis, Parkinson's disease.
Results
Sixty (40%) out of estimated a population of ~ 150 resident across Denmark accepted the invitation. Of these, 54/60 (90%) completed the survey. Although two-thirds, 35/54 (65%), of the respondents had prior formalized training in headache disorders, we identified gaps in all explored domains including diagnosis, management, and referral patterns. Particularly, there was an inconsistent use of guidelines and diagnostic criteria from the Danish Headache Society (2.74 (± 1.14)), the Danish Neurological Society (3.15 (± 0.86)), and the International Classification of Headache Disorders (2.33 (± 1.08)); 1: never/have not heard of, 4: always. Headache was ranked second to last out of six sub-specializations in interest.
Conclusions
Overall knowledge on headache disorders amongst neurology residents in Denmark do not meet the expectations set out by national and international recommendations. Stakeholders should make strategic initiatives for structured education in headache for improved clinical outcomes in parallel with costs reduction through resource optimization.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-022-03299-6.
Keywords: Training, Education, Barrier, Residency, Headache, Migraine, Medication overuse, Tension-type headache
Introduction
Headache disorders are leading contributors to years lived with disability worldwide [1]. This is a largely avoidable addition to global disease burden since cost-effective treatments exist for the largest contributors, i.e., migraine and tension-type headache [2–5]. Despite this reality, serious deficiencies are reported worldwide in awareness among healthcare providers [2]. Indeed, the largest barriers to adequate headache care are found in the relative lack of formal education and training of healthcare professionals in wealthy nations and low- and middle-income countries (LMICs) alike [2, 6]. Typically, worldwide, only four hours on average are dedicated to headache disorders in undergraduate medical curricula, and a similar picture is found in postgraduate neurology specialization [6]. Furthermore, limited funding within the field of headache research continues to be a barrier [7].
In Denmark, headache disorders make up more than one-third of all disability-adjusted life years (DALYs) due to neurological disorders according to the Global Burden of Disease [8]. Neurology specialist training is largely categorized into the introduction program (1st year residents) and the main program (2nd, 3rd, 4th, and 5thyear residents). It is expected that residents at all levels obtain knowledge about headache disorders through clinical experience in combination with self-study, but there is no mandatory formalized course in headache until residents are enrolled into the main program. Furthermore, while there is a requirement of experience with headache management obtained through specialist outpatient clinics, there is no formalized requirement of a dedicated training rotation in headache with a set amount of hours. These factors allow for a discrepancy in knowledge during the fundamental years of future neurologists [9]. These challenges are not limited to Denmark, but also extends to other regions including the United States [10, 11]. Concerted efforts should be made to pinpoint major gaps in knowledge in healthcare professionals to facilitate better educational policies in headache training. The aim of this study was to identify deficiencies and barriers in headache training among residents in neurology in Denmark.
Methods
Overview
The present study is a national cross-sectional survey of self-reported knowledge of residents in neurology in Denmark conducted from April 2019 to September 2019. Protocols for conducting of surveys is subject to exemption from processing at the National Committee on Health Research Ethics in Denmark. The ethical approval for this study was exempted by the National Committee on Health Research Ethics in Denmark. All methods were carried out in accordance with the Declaration of Helsinki. Informed consent was obtained from all subjects and/or their legal guardian(s). We handled survey data confidentially and maintained anonymity of respondents throughout the study.
Questionnaire
The survey was designed by clinicians and experts in headache disorders from the Danish Headache Center and Akershus University Hospital in collaboration with the Danish Knowledge Center on Headache Disorders, a non-profit organization focusing on raising the level of knowledge about headaches both among professionals and patients. The survey included questions related to participant demographics, knowledge of and barriers in headache disorders, guideline and diagnostic tools usage. Furthermore, we included topics of particular interest includingmedication overuse and non-pharmacological interventions. A full overview of questions is provided in Supplemental File 1.
Surveys
Surveys were sent to the residency training directors and departmental chairs of all neurological departments for distribution among their current residents. Furthermore, contacts were asked about the number of residents at their department. Of note, neurology specialist training is largely categorized into the introduction program (1st year residents) and the main program (2nd, 3rd, 4th, and 5th year residents). Pediatric neurology is not included in this survey as we only invited residents in a neurological residency; in Denmark, pediatric neurology is a sub-specialization of pediatrics. We did not conduct a pilot trial prior to the survey. The initial invitation was sent out in April 2019. Reminders were sent after two weeks to the training directors.
Statistical analysis
We performed descriptive analyses of the data in Microsoft Excel, version 2103 (16.0.13901.20400) / April 13, 2021. We present data as frequencies or means with standard deviations (SD).
Results
Demographics
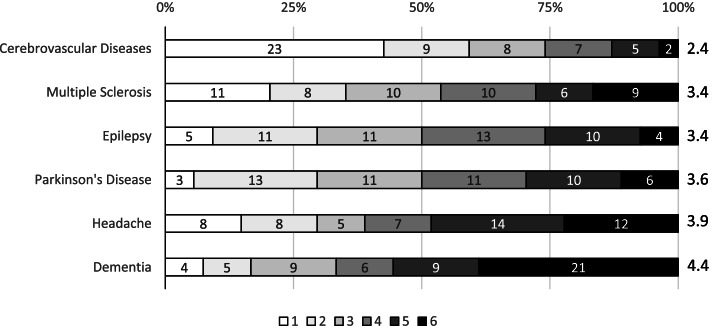
We identified 15 neurological departments in Denmark across five regions; of these, 14/15 departments were included as one was excluded due to no current residents associated with the department. There is no official tally of number of residents in Denmark, but we estimated a population of ~ 150 residents based on information derived from residency training directors. Sixty residents from the 14 included departments accepted the invitation, which corresponds to 40% of all possible potential participants; 54/60 (90%) of respondents completed all questions of the survey. Participants were from all five regions of Denmark with an approximate even distribution between residents in the introduction program and main program (Table 1); 35 of respondents had previously participated in a headache education program or training (Table 1). Headache disorders ranked as the second to least popular sub-specialization among residents (Fig. 1).
Table 1.
Respondent demographics
| Participants | 54 |
|---|---|
| Region | |
| ● Capital Region of Denmark | 21 (39%) |
| ● Central Denmark Region | 5 (9%) |
| ● North Denmark Region | 8 (15%) |
| ● Region of Southern Denmark | 12 (22%) |
| ● Region Zealand | 8 (15%) |
| Residency program | |
| ● Introductory program | 25 (46%) |
| ● Main program | 29 (54%) |
| Prior headache education/training | |
| ● All residents | 35 (65%) |
| ○ Residents in introductory program | 11 (44%) |
| ○ Residents in main program | 24 (83%) |
A total of 54 participants across all five regions in Denmark were included in the survey. There was an approximately even distribution between residents currently enrolled in the introduction program (1st year residents) and the main program (2nd, 3rd, 4th and 5th year residents). Two-thirds had prior training in headache disorders
Fig. 1.
Interest in neurological sub-specializations. All respondents were asked to list neurological sub-specializations in a ranked order, 1: most interesting, 6: least interesting. The number represent how many respondents ranked the sub-specialization a specific rank, e.g., 23 respondents ranked “Cerebrovascular Diseases” at the top of their list, i.e., rank 1. “Cerebrovascular diseases” is on average ranked as the most interesting sub-specialization whereas”Headache” ranks second to last. 1: highest ranked, 6; lowest ranked
Knowledge, barriers and challenges
Residents were most knowledgeable about tension-type headache and migraine whereas knowledge on post-traumatic headache was reported as most lacking (Table 2). The common disease-oriented barriers were challenging diagnostics, unclear medical history, and lack of effective treatment options. The largest physician-oriented barrier was reported as lack of prescribed efficacy of given treatment.
Table 2.
Self-reported knowledge, barriers, and challenges in headache disorders
| All participants (n = 54) | Introduction program (n = 25) | Main program (n = 29) | |
|---|---|---|---|
| Self-reported knowledge of headache disordersa | Mean (SD) | Mean (SD) | Mean (SD) |
| ● Migraine | 3.91 (0.65) | 3.76 (0.83) | 4.03 (0.42) |
| ● Tension-type headache | 3.94 (0.65) | 3.80 (0.82) | 4.07 (0.46) |
| ● Cluster headache | 3.68 (0.75) | 3.33 (0.92) | 3.89 (0.49) |
| ● Trigeminal neuralgia | 3.48 (0.84) | 3.12 (0.93) | 3.79 (0.62) |
| ● Medication overuse headache | 3.56 (0.86) | 3.28 (0.89) | 3.39 (0.77) |
| ● Post-traumatic headache | 3.15 (0.97) | 2.96 (0.98) | 3.31 (0.97) |
| Patient and disease-oriented barriersb | n (%) | n (%) | n (%) |
| ● Challenging diagnosis | 31 (57%) | 15 (60%) | 16 (55%) |
| ● Comorbidities | 23 (43%) | 9 (36%) | 14 (48%) |
| ● Patient anxiety of adverse events | 13 (23%) | 4 (16%) | 9 (31%) |
| ● Treatment failure due to adverse events | 19 (35%) | 6 (24%) | 13 (45%) |
| ● Unclear medical history | 31 (57%) | 17 (68%) | 14 (48%) |
| ● Lack of effective treatment options | 31 (57%) | 12 (48%) | 19 (66%) |
| ● No challenges | 3 (6%) | 1 (4%) | 2 (7%) |
| ● Other | 8 (15%) | 3 (12%) | 5 (17%) |
| Physician-oriented barriersb | n (%) | n (%) | n (%) |
| ● Own lack of knowledge | 17 (31%) | 12 (48%) | 5 (17%) |
| ● Find headache patients difficult to diagnose and treat | 26 (48%) | 12 (48%) | 14 (48%) |
| ● Challenges in physician/patient collaboration | 17 (31%) | 6 (24%) | 11 (38%) |
| ● Insufficient consultation time | 15 (28%) | 3 (12%) | 12 (41%) |
| ● Lack of prescribed treatment efficacy | 31 (57%) | 16 (64%) | 15 (52%) |
| ● Insufficient support from other specialists | 13 (24%) | 2 (8%) | 11 (38%) |
| ● No barriers | 5 (9%) | 3 (12%) | 2 (7%) |
aScale from 1–5; 1: very bad, 5: very good. bParticipants were asked to choose one or more options
Guidelines and diagnostic tools
The majority of respondents reported that they use guidelines for management of headache disorders (Table 3). Overall respondents rank an inconsistent use of the International Classification of Headache Disorders (ICHD) [12] and headache diaries for diagnosis (2.33 (1.08), 3.31 (0.77), respectively; 1: never/have not heard of, 4: always). For outcome assessment, residents rate a higher consistent use of headache diaries and quality of life parameters (3.14 (0.93), 3.04 (0.80), respectively; 1: never/have not heard of, 4: always).
Table 3.
Use of guidelines, classification and tools for diagnosis and outcome assessment
| All participants (n = 54) | Introduction program (n = 25) | Main program (n = 29) | |
|---|---|---|---|
| Guidelines | Mean (SD) | Mean (SD) | Mean (SD) |
| ● Guidelines from the Danish Headache Society | 2.74 (1.14) | 2.4 (1.19) | 3.03 (1.02) |
| ● Guidelines from the Danish Neurological Society | 3.15 (0.86) | 2.96 (1.02) | 3.31 (0.66) |
| Diagnostic tools | Mean (SD) | Mean (SD) | Mean (SD) |
| ● The International Classification of Headache Disorders | 2.33 (1.08) | 2.36 (1.04) | 2.31 (1.14) |
| ● Headache diary for diagnosis | 3.31 (0.77) | 3.28 (0.84) | 3.34 (0.72) |
| Outcome assessment | Mean (SD) | Mean (SD) | Mean (SD) |
| ● Headache calendar for outcome assessment | 3.14 (0.93) | 2.96 (1.09) | 3.31 (0.76) |
| ● Quality of life parameters (e.g., sickness absence, reduced participation in social events) | 3.04 (0.80) | 2.88 (0.89) | 3.17 (0.71) |
Scale from 1–4; 1: never/have not heard of, 4: always
Contact and referral patterns
In most cases, the respondents estimate that headache consultations take up 11–20% of patient contacts (Table 4). Contact and collaboration with primary care is inconsistent and is skewered towards a lower score (2.37 (1.29), 2.63 (0.79), respectively; 1: never/very bad, 5: very frequently). Residents largely estimate 11–20% of consultations need referral to a tertiary center. The most common reason for further referral to tertiary/specialist care was lack of treatment efficacy and diagnostic uncertainty. When asked about whether residents find it beneficial to refer patients to tertiary care, the result was skewed towards a negative outcome (not at all), and one-fifth reported they did not know.
Table 4.
Contact and referral patterns
| All participants (n = 54) | Introduction program (n = 25) | Main program (n = 29) | |
|---|---|---|---|
| Proportion of consultations related to headache | n (%) | n (%) | n (%) |
| ● 1–10% | 13 (24%) | 10 (40%) | 3 (10%) |
| ● 11–20% | 29 (54%) | 7 (28%) | 22 (76%) |
| ● 21–30% | 8 (15%) | 5 (20%) | 3 (10%) |
| ● 31–40% | 0 (0%) | 0 (0%) | 0 (0%) |
| ● > 40% | 4 (7%) | 3 (12%) | 1 (3%) |
| ● None | 0 (0%) | 0 (0%) | 0 (0%) |
| Primary care | Mean (SD) | Mean (SD) | Mean (SD) |
| ● Contact from primary care for professional advice on headachea | 2.37 (1.29) | 1.89 (0.96) | 2.86 (1.36) |
| ● Collaboration with primary care for referred headache patientsb | 2.63 (0.79) | 2.60 (0.77) | 2.66 (0.83) |
| Proportion of headache patients referred to tertiary/specialist care | n (%) | n (%) | n (%) |
| ● 1–10% | 9 (17%) | 4 (16%) | 5 (17%) |
| ● 11–20% | 35 (65%) | 14 (56%) | 21 (72%) |
| ● 21–30% | 7 (13%) | 5 (20%) | 2 (7%) |
| ● 31–40% | 1 (2%) | 1 (4%) | 0 (0%) |
| ● > 40% | 1 (2%) | 0 (0%) | 1 (3%) |
| ● Never | 1 (2%) | 1 (4%) | 0 (0%) |
| Most common reason for referring to tertiary/specialist carec | n (%) | n (%) | n (%) |
| • Diagnostic uncertainty | 20 (37%) | 11 (44%) | 9 (31%) |
| • Suspicion of serious underlying cause | 2 (4%) | 2 (8%) | 0 (0%) |
| • Lack of treatment efficacy | 32 (59%) | 11 (44%) | 21 (72%) |
| • Desire/expectation of the patient | 11 (20%) | 5 (20%) | 6 (21%) |
| •Other | 8 (15%) | 5 (20%) | 3 (10%) |
| Wait time for referral to tertiary/specialist care | n (%) | n (%) | n (%) |
| ● Short | 0 (0%) | 0 (0%) | 0 (0%) |
| ● Acceptable | 16 (30%) | 11 (44%) | 5 (17%) |
| ● Long | 21 (39%) | 8 (32%) | 13 (45%) |
| ● Unacceptably long | 8 (15%) | 2 (8%) | 6 (21%) |
| ● Do not know | 9 (17%) | 4 (16%) | 5 (21%) |
| Helpful for patients to be referred to tertiary/specialist cared | Mean (SD) 2.33 (0.74) | Mean (SD) 2.00 (0.76) | Mean (SD) 2.62 (0.74) |
aScale from 1–5; 1: never, 5: very frequently. bScale from 1–5; 1: none/very bad, 5: very good. cParticipants could choose up to two answers. dScale from 1–5; 1: not at all, 5: to a great extent. 10 (19%) responded they did not know
Medication overuse
Participants on average ranked that medication overuse is a problem during clinical management of headache disorders (Table 5). The majority of respondents could correctly identify simple analgesics and migraine acute medications as potential causes of medication overuse headache whereas fewer could correctly identify opioids. The majority (80%) could provide the recommended maximum use of simple analgesics.
Table 5.
Medication overuse headache
| All participants (n = 54) | Introduction program (n = 25) | Main program (n = 29) | |
|---|---|---|---|
| Medication overuse headache is a problem among your headache patientsa | Mean (SD) 3.31 (0.86) | Mean (SD) 3.04 (0.84) | Mean (SD) 3.55 (0.82) |
| Kind of medications that can cause medication overuse headache | n (%) | n (%) | n (%) |
| ● Simple analgesics | 53 (98%) | 24 (83%) | 29 (100%) |
| ● Opioids | 32 (59%) | 12 (48%) | 20 (69%) |
| ● Migraine acute medicine (e.g., triptans) | 42 (78%) | 16 (64%) | 26 (90%) |
| ● Migraine preventive medicine (e.g., beta blockers) | 5 (9%) | 2 (8%) | 3 (10%) |
| ● Do not know | 0 (0%) | 0 (0%) | 0 (0%) |
| Recommended maximum use of simple analgesics for headache patients | n (%) | n (%) | n (%) |
| ● 1 day a week | 1 (2%) | 1 (4%) | 0 (0%) |
| ● 2–3 days a week | 43 (80%) | 17 (68%) | 26 (90%) |
| ● 4–5 days a week | 4 (7%) | 1 (4%) | 3 (10%) |
| ● 6 days a week | 0 (0%) | 0 (0%) | 0 (0%) |
| ● Do not know | 6 (11%) | 6 (24%) | 0 (0%) |
aScale from 1–5; 1: not at all, 5: to a great extent
Non-pharmacological interventions
Respondents were neutral (mean: 3 (1.13); 1: never, 5: very frequently) whether patients seek advice on non-pharmacological treatments. When asked about whether they feel equipped for this task, the result was skewered towards not at all (Table 6). The most popular recommended non-pharmacological interventions were physiotherapy, exercise, and psychological treatment.
Table 6.
Non-pharmacological interventions
| All participants (n = 54) | Introduction program (n = 25) | Main program (n = 29) | |
|---|---|---|---|
| Use of non-pharmacological interventions | Mean (SD) | Mean (SD) | Mean (SD) |
| ● Patients seek advice on non-pharmacological treatment optionsa | 3.00 (1.13) | 2.84 (1.25) | 3.14 (1.03) |
| ● Feel equipped to advise patients on non-pharmacological treatment optionsb | 2.29 (0.82) | 2.08 (0.81) | 2.48 (0.76) |
| Recommended non-pharmacological interventionsc | n (%) | n (%) | n (%) |
| ● Acupuncture | 15 (28%) | 9 (36%) | 6 (24%) |
| ● Craniosacral therapy | 3 (6%) | 1 (4%) | 2 (7%) |
| ● Diet | 28 (52%) | 13 (52%) | 15 (52%) |
| ● Ear (daith) piercing | 1 (2%) | 0 (0%) | 1 (3%) |
| ● Exercise | 45 (83%) | 19 (76%) | 26 (90%) |
| ● Medical cannabis | 0 (0%) | 0 (0%) | 0 (0%) |
| ● Neurostimulation | 1 (2%) | 1 (4%) | 0 (0%) |
| ● Physiotherapy | 50 (93%) | 22 (88%) | 28 (97%) |
| ● Psychological treatment | 41 (76%) | 17 (68%) | 24 (83%) |
| ● Reflexology | 4 (7%) | 2 (8%) | 2 (7%) |
| ● Other | 6 (11%) | 3 (12%) | 3 (10%) |
| ● None of the above | 0 (0%) | 0 (0%) | 0 (0%) |
aScale from 1–5; 1: never, 5: very frequently. bScale from 1–5; 1: not at all, 5: to a great extent. cParticipants could choose multiple answers
Discussion
In this national cross-sectional survey of neurology residents in Denmark, we identified several areas for improvement for headache education of healthcare providers.
Diagnostic criteria
Approximate half of respondents report that diagnosis and treatment of patients with headache is challenging (Table 2). This is particularly worrying as the majority estimate 11–20% of consultations are related to headache (Table 4) – a significant proportion. Yet these findings are not surprising and in line with findings from studies conducted in other regions [13–15]. As there are no biomarkers or diagnostic tests for most headache disorders, diagnosis rely on the medical history. While headache diaries in general are used for diagnosis and outcome assessment, there is an apparent inconsistent use of the ICHD (Table 3). The expectation is that residents would have a more consistent use and knowledge of diagnostic criteria over time due to accumulation of experience, but the pattern is similar for residents in the introduction program and the main program. With a limited number of training hours during residency, the low utilization of specific diagnostic criteria may be caused by a higher emphasis on stratification of cases into high-risk (secondary headache disorders, e.g., headache attributed to trauma) and low-risk patients (primary headache disorders, e.g., migraine) rather than specific diagnoses during early training [16–18]. This is not unreasonable as secondary headache disorders may cause significant morbidity, and for some etiologies, a relatively high mortality [17]. Nonetheless, correct diagnosis is the mainstay of clinical management of primary headache disorders, and targeted educational interventions are needed. In an international survey of neurologists, explicit diagnostic criteria are only used in 56% of cases [6]. These data confirm that these deficiencies are not necessarily corrected after completion of specialization and substantiates the need for improvement already during residency.
Treatment and management
More than half of respondents identify lack of treatment options and efficacy as a barrier to care (Table 2). While it cannot be excluded that this is due to rare headache disorders with few evidence-based options, cost-effective treatments do exist for the largest headache burdens, i.e., migraine and tension-type headache [2–5]. These findings are surprising as most residents are more than moderately confident in their self-reported knowledge of headache disorders (Table 2). Furthermore, less than two-thirds of respondents could correctly identify opioids as a potential cause of medication overuse headache, and more worrying, a few respondents both in the introduction program and main program incorrectly reported prophylactic medications as a potential cause (Table 5). This misinterpretation can lead to a worse clinical outcome, and provides a possible explanation of poor use of preventive medications in eligible cases [19]. Most respondents recommended one non-pharmacological interventions (Table 6), which provides a multidisciplinary approach to clinical management. However, for some of the more popular recommended options (e.g., physiotherapy, acupuncture, and diet), data on potential therapeutic gain of these therapies is discordant, and may also explain why respondents on average feel less confident in advising patients on non-pharmacological treatment options [2]. These gaps in treatment and management could be related to a lacking use of available national guidelines [20], but the use of guidelines is reported to be higher than moderate (Table 3).
Primary care and tertiary care
In Denmark, headache services are divided in three levels: primary care (general practitioner), specialist care (general neurology), and tertiary care (specialized headache center). Headache is the most common neurological symptom in primary care [21], and should in 90% of cases be initiated and maintained in primary care [22, 23]. While there are cases where specialist care can be necessary, treatment of a headache patient and repatriation to primary care should be coordinated with the general practitioner to ensure continuity of care. However, contact from primary care for professional advice on headache and collaboration with primary care for referred headache patients is inadequate in the present study (Table 4). A possible consequence is unnecessary escalation and referral to tertiary care. This is also reflected by the fact that most respondents estimated up to one-fifth of patients require referral to tertiary care with one of the common reasons being diagnostic uncertainty (Table 4), which may be caused by the inconsistent use of diagnostic criteria provided by ICHD (Table 3). For migraine, presumably compromising the largest proportion of patients, requires only 1% of cases to be referred to tertiary care [2]. Specialist services are scarce and impeded by long waiting lists [2]. This is also the case in a high-income country as Denmark, where more than half of the residents estimated the waiting list to be either long or unacceptable. Furthermore, while tertiary care do provide better care due to greater expertise and access to a multidisciplinary approach [24], residents do not necessarily find it beneficial for patients to be referred (Table 4).
Barriers to care
The most common patient and disease-related barriers were connected to diagnosis and treatment (Table 2). An unclear medical history is reported by more than half of residents as an impediment, which may also overlap with comorbidities also being reported as a common barrier [2, 4, 25]. This is troubling as diagnosis of headache disorders rely on the medical history. Interestingly, these may be related to a high frequency of challenges in physician/patient collaboration and insufficient consultation time as both would affect obtaining a good medical history.
Headache education
Even if headache training is not mandatory until the main program, almost half of all residents in the introduction program had already completed a formalized course in headache prior to this survey (Table 1). This likely reflects an interest and need for education already at an early career stage. The European Union of Medical Specialistscategorize applied clinical knowledge in four different levels, and it is recommended that trainees obtain at level 3 and 4 within the first two years of training [26]; level 4 is the ability to make a complete diagnosis and optimize treatment. As such, residents in the main program should be confident in all aspects of headache management before completion of specialization, however, not all residents had completed formalized headache training prior to the survey, and there were gaps in all explored domains. Almost one-fifth of residents in the main program reported their own knowledge as a personal barrier to care (Table 2). Overall, the expectations are discordant with the actual level of self-reported knowledge. In a survey of neurology chairs and resident directors in the United States, two-thirds of respondents found headache education inadequate or had no opinion [11]. Implementation of a mandatory rotation in an specialized outpatient clinic with a set number of hours improved gaps in an United States-based institution [27], and it is not unreasonable to assume that a similar intervention may improve the findings of our survey. While this cannot be concluded based on the available data, one may speculate whether the overall low interest in headache as a sub-specialization is an important factor (Fig. 1) [28, 29]. Increased availability and emergence of novel disease-specific treatment options and scientific advances may help improve interest in the future [3, 30–32].
Strengths and limitations
This is the first national cross-sectional study of residents in neurology in Denmark. The study included approximate 40% of all residents in Denmark, which we evaluate as representative of the population as the sample included residents from both inside and outside the Capital Region of Denmark (greater Copenhagen area). Nonetheless, as there is no official tally of number of residents in Denmark, and that we included less than half the possible the estimated number of residents, we may have introduced a selection bias. Furthermore, we did not inquire about specific year of training for residents in the main program, which spans from 2nd to 5th year residents. Surveys may introduce recall bias, but we find no suspect systematic bias in this domain.
Conclusions
Even in a developed country such as Denmark with excellent headache services [33], the overall knowledge of neurology residents on headache disorders do not meet the expectations set out by both national and international recommendations. We identified several deficiencies and barriers in headache management amongst residents particularly related to diagnosis. Parallel investigations should be investigated at other levels of systems of care (e.g., primary care) and in other regions to assess for similar trends. Strategic initiatives for structured education in headache would likely result in improved clinical outcomes in parallel with costs reductions and should be prioritized by both regional and national stakeholders.
Supplementary Information
Acknowledgements
Messoud Ashina was supported by the Lundbeck Foundation Professor Grant (R310-2018-3711).
Abbreviations
- DALY
Disability-adjusted life year
- ICHD
International Classification of Headache Disorders
- LMIC
Low- and middle-income country
Authors’ contributions
MD, SS, ESK, and JMH contributed to conception and design of the work. MD and SS contributed to acquisition of data for the work. TPD, MD, and SS contributed to analysis of data for the work. TPD, ESK, MA, and JMH contributed to interpretation of data for the work. TPD wrote the first draft of the manuscript. All authors contributed to critical revision of the work for important intellectual content. The authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
Anonymized datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request and following the acquisition of necessary permissions.
Declarations
Ethics approval and consent to participate
Protocols for conducting of surveys is subject to exemption from processing at the National Committee on Health Research Ethics in Denmark. The ethical approval for this study was exempted by the National Committee on Health Research Ethics in Denmark. All methods were carried out in accordance with the Declaration of Helsinki. Informed consent was obtained from all subjects and/or their legal guardian(s). We handled survey data confidentially and maintained anonymity of respondents throughout the study.
Consent for publication
Not applicable.
Competing interests
ESK is supported by University of Oslo and Akershus University Hospital. MA is a consultant, speaker, or scientific advisor for AbbVie, Allergan, Amgen, Eli Lilly, Lundbeck, Novartis, and Teva and a primary investigator for ongoing AbbVie/Allergan, Amgen, Eli Lilly, Lundbeck, Novartis, and Teva trials. Messoud Ashina has no ownership interest and does not own stocks of any pharmaceutical company. Messoud Ashina serves as associate editor of Cephalalgia, associate editor of the Journal of Headache and Pain, and associate editor of Brain. TPD, MD, SS, and JMH report no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Saylor D, Steiner T. The global burden of headache. Semin Neurol. 2018;38:182–190. doi: 10.1055/s-0038-1647245. [DOI] [PubMed] [Google Scholar]
- 2.Ashina M, et al. Migraine: epidemiology and systems of care. Lancet. 2021 doi: 10.1016/S0140-6736(20)32160-7. [DOI] [PubMed] [Google Scholar]
- 3.Ashina M, et al. Migraine: integrated approaches to clinical management and emerging treatments. Lancet. 2021 doi: 10.1016/S0140-6736(20)32342-4. [DOI] [PubMed] [Google Scholar]
- 4.Ashina S, et al. Tension-type headache. Nat Rev Dis Prim. 2021;7:24. doi: 10.1038/s41572-021-00257-2. [DOI] [PubMed] [Google Scholar]
- 5.Ashina M. Migraine. N Engl J Med. 2020;383:1866–1876. doi: 10.1056/NEJMra1915327. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Atlas of headache disorders and resources in the world. 2011. https://www.who.int/mental_health/management/who_atlas_headache_disorders.pdf?ua=1.
- 7.Sobocki P, Lekander I, Berwick S, Olesen J, Jönsson B. Resource allocation to brain research in Europe (RABRE) Eur J Neurosci. 2006;24:2691–2693. doi: 10.1111/j.1460-9568.2006.05116.x. [DOI] [PubMed] [Google Scholar]
- 8.GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed]
- 9.Sundhedsstyrelsen & Neurologisk Selskab. Målbeskrivelse for speciallægeuddannelsen i Neurologi. 2015. https://neuro.dk/wordpress/wp-content/uploads/2012/09/60306cf29c73999672cde2cb68f17e3f.pdf.
- 10.Ahmed ZA, Faulkner LR. Headache education in adult neurology residency: a survey of program directors and chief residents. Headache J Head Face Pain. 2016;56:871–877. doi: 10.1111/head.12822. [DOI] [PubMed] [Google Scholar]
- 11.Kommineni M, Finkel AG. Teaching headache in america: survey of neurology chairs and residency directors. Headache J Head Face Pain. 2005;45:862–865. doi: 10.1111/j.1526-4610.2005.05154.x. [DOI] [PubMed] [Google Scholar]
- 12.Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1-211. 10.1177/0333102417738202. [DOI] [PubMed]
- 13.Kristoffersen ES, Faiz KW, Winsvold BS. Neurology residents’ knowledge of the management of headache. Cephalalgia. 2019;39:1396–1406. doi: 10.1177/0333102419847973. [DOI] [PubMed] [Google Scholar]
- 14.Ong JJY, Chan YC. Medical undergraduate survey on headache education in singapore: knowledge, perceptions, and assessment of unmet needs. Headache J Head Face Pain. 2017;57:967–978. doi: 10.1111/head.13110. [DOI] [PubMed] [Google Scholar]
- 15.Bösner S, Hartel S, Diederich J, Baum E. Diagnosing headache in primary care: a qualitative study of GPs’ approaches. Br J Gen Pract. 2014;64:e532–e537. doi: 10.3399/bjgp14X681325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Do TP, la Cour Karottki NF, Ashina M. Updates in the diagnostic approach of headache. Curr Pain Headache Rep. 2021;25:80. doi: 10.1007/s11916-021-00995-8. [DOI] [PubMed] [Google Scholar]
- 17.Do TP, et al. Red and orange flags for secondary headaches in clinical practice. Neurology. 2019;92:134–144. doi: 10.1212/WNL.0000000000006697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pohl H, et al. Green flags and headache: a concept study using the delphi method. Headache J Head Face Pain. 2021;61:300–309. doi: 10.1111/head.14054. [DOI] [PubMed] [Google Scholar]
- 19.Kristoffersen ES, Grande RB, Aaseth K, Lundqvist C, Russell MB. Management of primary chronic headache in the general population: the Akershus study of chronic headache. J Headache Pain. 2012;13:113–120. doi: 10.1007/s10194-011-0391-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schytz HW, Amin FM, Jensen RH, Carlsen L, Maarbjerg S, Lund N, Aegidius K, Thomsen LL, Bach FW, Beier D, Johansen H, Hansen JM, Kasch H, Munksgaard SB, Poulsen L, Sørensen PS, Schmidt-Hansen PT, Cvetkovic VV, Ashina M, Bendtsen L. Referenceprogramme: diagnosis and treatment of headache disorders and facial pain. Danish Headache Society, 3rd edition, 2020. J Headache Pain. 2021;22(1):22. 10.1186/s10194-021-01228-4. [DOI] [PMC free article] [PubMed]
- 21.Latinovic R. Headache and migraine in primary care: consultation, prescription, and referral rates in a large population. J Neurol Neurosurg Psychiatry. 2005;77:385–387. doi: 10.1136/jnnp.2005.073221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steiner TJ, et al. Recommendations for headache service organisation and delivery in Europe. J Headache Pain. 2011;12:419–426. doi: 10.1007/s10194-011-0320-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lenz B, et al. Headache service quality evaluation: implementation of quality indicators in primary care in Europe. J Headache Pain. 2021;22:33. doi: 10.1186/s10194-021-01236-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katsarava Z, Mania M, Lampl C, Herberhold J, Steiner TJ. Poor medical care for people with migraine in Europe - evidence from the Eurolight study. J Headache Pain. 2018;19:10. doi: 10.1186/s10194-018-0839-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ashina H, et al. Post-traumatic headache attributed to traumatic brain injury: classification, clinical characteristics, and treatment. Lancet Neurol. 2021;20:460–469. doi: 10.1016/S1474-4422(21)00094-6. [DOI] [PubMed] [Google Scholar]
- 26.EUROPEAN UNION OF MEDICAL SPECIALISTS. European Training Requirements for Neurology. 2016. https://www.uems.eu/__data/assets/pdf_file/0008/30689/European-Training-Requirements-Neurology-Oct-16-changes-marked-in-red.pdf.
- 27.Zhang N, Cowan RP. On making a headache medicine rotation mandatory in neurology training. Headache J Head Face Pain. 2019;59:1841–1845. doi: 10.1111/head.13667. [DOI] [PubMed] [Google Scholar]
- 28.Zis P, et al. Subspecialty preferences among neurologists of the future. Eur J Neurol. 2018;25:597–601. doi: 10.1111/ene.13526. [DOI] [PubMed] [Google Scholar]
- 29.Kristoffersen ES, Winsvold BS, Faiz KW. Prestige of neurological disorders among future neurologists in Norway. Acta Neurol Scand. 2019;139:555–558. doi: 10.1111/ane.13087. [DOI] [PubMed] [Google Scholar]
- 30.Ashina M, et al. Migraine: disease characterisation, biomarkers, and precision medicine. Lancet. 2021;397:1496–1504. doi: 10.1016/S0140-6736(20)32162-0. [DOI] [PubMed] [Google Scholar]
- 31.Do TP, Al-Saoudi A, Ashina M. Future prophylactic treatments in migraine: beyond anti-CGRP monoclonal antibodies and gepants. Rev Neurol (Paris) 2021;177:827–833. doi: 10.1016/j.neurol.2021.06.005. [DOI] [PubMed] [Google Scholar]
- 32.Dominguez-Moreno R, Do TP, Ashina M. Calcitonin gene-related peptide and pituitary adenylate cyclase-activating polypeptide in migraine treatment. Curr. Opin. Endocrinol. Diabetes Obes: Publish Ah; 2022. [DOI] [PubMed] [Google Scholar]
- 33.Olesen J. The danish headache center: From origin to full development. Cephalalgia. 2017;37:5–6. doi: 10.1177/0333102417709392. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Anonymized datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request and following the acquisition of necessary permissions.