Abstract
Background
Falls are a common and serious public health issue among older adults, contributing to the loss of independence, psychological distress, and incapability to engage in meaningful occupations, etc. However, there is a lack of abundant information about the fall risk self-evaluation scale for community-dwelling older people. Therefore, this study aimed to evaluate the preliminary reliability and validity of the fall risk self-assessment scale (FRSAS) among community-dwelling older adults.
Methods
A cross-sectional study was conducted. A total of 230 individuals aged 65 years and over were recruited by a convenience sampling between October and December 2020 from three communities in Haidian district, Beijing. Eligible participants were required to fill in the general condition questionnaire and the fall risk self-assessment scale. The reliability and validity were analyzed by using SPSS 20.0.
Results
Two hundred twenty-two participants completed the assessment as required (the completion rate was 96.52%). The most items of FRSAS were understood by older adults, which was completed in 10 min. Cronbach’s α and intraclass correlation coefficient ICC (2,1) of the scale were 0.757 and 0.967 respectively, suggesting good internal consistency and test-retest reliability. Exploratory factor analysis yielded 14 factors that explained 61.744% of the variance. Five items failed to be categorized into any factors because the factor loading of these items was less than 0.4. A future large-sample study needs to be conducted to explore its construct validity. The total scores and dimensional scores except for C-dimension showed significant differences between participants who had experienced a fall in the previous 6 months and those who had not (P < 0.05), indicating good discriminant validity.
Conclusions
The fall risk self-assessment scale including 41 items demonstrated relatively high feasibility as well as satisfactory results in the internal consistency, test-retest reliability, and discriminant validity.
Trial registration
Registration number: ChiCTR2000038856; Date of registration: 7 Oct 2020.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-022-02962-3.
Keywords: Fall risk self-assessment scale, Older adults, Community, Reliability, Validity
Background
Falls are a common and serious public health issue among older adults [1, 2]. It is reported that the annual rate of falls in Chinese community-dwelling older people ranged from 14.7 to 34% and the annual incidence of falling more than once was 4 to 5% [3]. A fall is universally defined as “an event resulting in a person who comes to rest inadvertently on the ground, floor or other lower-level” [4]. Although falling is not regarded as a determinant of an underlying poor health condition, ramifications of falls may predispose individuals to adverse outcomes ranging from minor injuries (e.g., bruises, abrasions, lacerations, strains and sprains) to serious consequences, including fractures, loss of independence or even death [5–7]. Besides physical injuries, psychological problems resulting from falls should not be underestimated, such as fear of falling [8]. Evidence showed that the cost of fall-related injury among older adults ranged from US$16 to US$3812 per person per fall in China [9]. The possibility of falls will significantly increase with the number of fall risks identified, supported by a prospective study with the percentage which fell within 1 year nearly folded with each additional risk factor in community-dwelling older persons [10]. Therefore, assessing fall risks prospectively can curb the fall incidences effectively and decrease the costs of either hospital agency or family.
Although a few fall risk assessment tools are readily available, most have been tested or used in primary care settings [11]. Gate et al. emphasized that tools developed in one setting (e.g., inpatient) may be less efficacious when used in another setting (e.g., outpatient) [12]. Based on that, other fall risk assessment tools have been developed for predicting fall-related risks in community-dwelling older adults. Through searching the database including PubMed, Medline, Embase and China National Knowledge Infrastructure (CNKI), several fall risk assessment tools used in community settings have been identified [13–25]. As shown in Table 1, these assessment tools can be roughly divided into three categories including the performance-based tests, the fall-related psychological evaluations and the multifactorial fall risk assessment tools. Regarding the performance-based tests, they are nearly performed by the healthcare providers, which requires relative longer administrative time and a certain number of qualified staffs. Although the fall-related psychological evaluations can be completed by the older adults themselves, these evaluations just attend to the psychological aspects of fall-related risks, excluding the physical agents. In addition, the fact that the multifactorial fall risk assessment tools are time-consuming, albeit rather comprehensive, suggests that they are rarely incorporated into the daily routine of community-dwelling older adults to predict the risk of falls. Lastly and importantly, there are some advantages and disadvantages for the first two self-rated multifactorial fall risk assessment tools. Specifically, the self-rated Fall Risk Questionnaire (self-rated FRQ) is characterized as a simple and fast-screening tool, which is the fall risk screening component of the STEADI (Stopping Elderly Accidents, Deaths, and Injuries) toolkit [11]. However, Song et al. found that the Cronbach’s α of the self-rated FRQ was a bit low (0.670) when testing in the Chinese community-dwelling older adults, implying that the items in the questionnaire are not highly correlated and more relevant items are required to be added to increase its internal consistency [19]. The Chinese Home-FAST self-reported screening tool mainly focuses on assessing home environmental hazards which are classified as extrinsic factors, not paying much attention to intrinsic risks (dependent on the individualized agent) [20].
Table 1.
The summary of fall risk assessments used for community-dwelling older adults
| Scale | Author/Year | Items | Scores | Reliability | Validity | Self-assessment |
|---|---|---|---|---|---|---|
| The Performance-based Tests | ||||||
| Berg Balance Scale (BBS) | Muir et al. 2008 [13] | 14 | 0 ~ 56 | NR |
Sen: 61% Spe: 53% Cut-off point: 54 AUC:0.59 |
No |
| Time Up and Go test (TUGT) | Kang et al. 2017 [14] | 1 | Time recorded | NR |
Sen: 67.5% Spe: 56.3% Cut-off point: 10.15 s AUC:0.607 |
No |
| Functional Gait Assessment (FGA) | Wrisley & Kumar 2010 [15] | 10 | 0 ~ 30 | NR |
Sen: 100.0% Spe: 82.8% Cut-off point: 20 AUC:0.92 |
No |
| Dynamic Gait Index (DGI) | Wrisley & Kumar 2010 [15] | 8 | 0 ~ 24 | NR |
Sen: 100.0% Spe: 75.9% Cut-off point: 20 AUC:0.91 |
No |
| The Fall-related Psychological Evaluations | ||||||
| Activities-specific Balance Confidence (ABC) scale | Guan et al. 2012 [16] | 16 | 0 ~ 100% |
Cronbach’s α: 0.94 Inter-rater: ICC = 0.98 Test-retest: ICC = 0.96 |
Significant discriminatory validity (t = 3.45, P < 0.01) | Yes |
| Fall Efficacy Scale-International (FES-I) | Guo et al. 2015 [17] | 16 | 16 ~ 64 |
Cronbach’s α: 0.921 Test-retest: ICC = 0.906 |
Sen: 71% Spe: 63% Cut-off point: 35 AUC:0.741 |
Yes |
| Iconographical Falls Efficacy Scale-Short Version (Icon-FES) | Chan et al. 2018 [18] | 10 | 10 ~ 40 |
Cronbach’s α: 0.91 Test-retest: ICC = 0.93 |
Concurrent validity: correlate with FES-I (r = 0.75, P < 0.001) |
No (Interview-based) |
| The Multifactorial Fall Risk Assessment Tools | ||||||
| The self-rated Fall Risk Questionnaire (self-rated FRQ) | Song et al. 2020 [19] | 12 | 0 ~ 14 | Cronbach’s α: 0.670 |
Sen: 81.03% Spe: 51.72% Cut-off point: 4 AUC:0.743 |
Yes |
| The Chinese Home-FAST self-reported screening tool | Lai et al. 2020 [20] | 20 | 0 ~ 20 |
Cronbach’s α: 0.94 Inter-rater: ICC = 0.89 Test-retest: ICC = 0.88 |
Satisfactory discriminatory validity (Wilks’ lambda = 0.78, F = 42.04, P < 0.001) | Yes |
| The Fall-risk Assessment Profile | Chen et al. 2020 [21] | 8 | 0 ~ 17 | NR |
Sen: 75.16% Spe: 52.75% Cut-off point: 6 AUC: 0.70 |
No |
| The Short-form Physiological Profile Assessment (S-PPA) | Liu & Ng. 2019 [22] | 5 | NR |
Inter-rater: ICC = 0.83 Intra-rater: ICC = 0.74 |
Sen: 39% Spe: 81% Cut-off point: 0.87 AUC: 0.62 |
No |
| The Fall Risks for Older People in the Community screening tool (FROP-Com screen) | Ng et al. 2020 [23] | 3 | 0 ~ 9 |
Inter-rater: ICC = 0.79 Test-retest: ICC = 0.70 |
Concurrent validity: correlate with BBS (rho = 0.38, P < 0.01), TUG (rho = 0.35, P < 0.01), and ABC-C (rho = − 0.65, P < 0.001). |
No |
| The Fall Risk Screening Tool | Fielding et al. 2013 [24] | 23 | 0 ~ 33 |
Cronbach’s α: 0.869 Inter-rater: ICC = 0.830 |
NR | No |
| LASA Fall Risk Profile | Peeters et al. 2010 [25] | 9 | 0 ~ 30 | NR |
Sen: 56.6% Spe: 71.4% Cut-off point: 8 AUC: 0.65 |
No |
Sen Sensibility, Spe Specificity, AUC Area Under Curve, NR Not Reported
Currently, there is a lack of abundant information regarding the comprehensive fall risk self-evaluation scale for older people living in the community. Thus, it is indispensable to develop a fall risk self-assessment scale tailored to Chinese community-dwelling older adults, which is a major issue of immediate and far-reaching significance in a sense. Early chunks of research had been conducted to develop the fall risk self-assessment scale in community-dwelling older people (FRSAS) using the three-round modified Delphi method [26]. Therefore, this study aimed to evaluate the reliability and validity of the FRSAS among community-dwelling older adults.
Methods
Participants
This was a cross-sectional study using a convenience sampling to recruit older people between October and December 2020. A total of 230 community-dwelling older people aged 65 years and over were recruited through posters in the three local community healthcare centers of Haidian district, Beijing. Inclusion criteria of participants were: aged 65 years or older; had resided in the current community for at least 1 year; no communication barriers including written or verbal communication (based on the self-report information of participants and observation of researchers); able to ambulate independently (including with the help of assistive devices, such as cane and walking aid, etc.). Older adults were excluded who were completely immobilized (e.g., paralysis or amputation), had moderate to severe cognitive impairment or had mental disorders (judged by the self-report information of participants and observation of researchers, which indicated that participants would be required to do further assessments including MMSE if necessary). According to Kendall’s guidelines [27], the ratio of variables in the scale and samples should be no less than 5:1. The attrition rate considered, a minimum of 220 participants was determined. The study was approved by the Peking University Third Hospital Medical Science Research Ethics Committee (Ref: M2020392). Informed consent was obtained from all participants in the beginning of the study and the collected data were kept blindly.
Procedures
This study involved two stages: 1) Development of the FRSAS and 2) Testing its reliability and validity.
Stage 1: development of the FRSAS
The development of the FRASA was composed of two steps. Firstly, the item pool of fall-related risk factors was compiled from a literature review or current assessments utilized commonly in practice and complemented by the recommendations of stakeholders derived from the focus group. Secondly, a three-round modified Delphi study was employed to reach a consensus within an expert panel.
In step one, a literature review was conducted by searching PubMed, Medline, Embase, Wanfang Data and China National Knowledge Infrastructure (CNKI) in the last 5 years. The main search terms were ‘older ‘or ‘aged’, ‘falls’ or ‘accidental falls’, ‘risk assessment’ or ‘risk screening’, ‘scale’ or ‘tool’ or ‘instrument’, in various combinations using a Boolean operator. Only searching results from prospective cross-sectional or cohort studies, clinical trials, reviews and meta-analysis published in English or Chinese were included for further evaluation (For the process of literature review referred to Additional file 1). The current assessments were utilized for reference, such as the Morse Fall Scale [28], Hendrich II Fall Risk Model [29] and the Home Falls and Accidents Screening Tool (HOME FAST) [30]. The items extracted from the literature review and the current assessment tools were discussed by a focus group. The inclusion criteria of invited experts in the focus group were: (1) experts specialized in rehabilitation, nursing, geriatrics or gerontology, including clinicians, nurses and physical therapy (had work experience in community healthcare center); (2) experts who had been engaged in clinical or research work for more than 5 years; (3) experts who had possessed advanced title. Finally, the two-level item pool was settled, where 5 first-level indicators and 37 second-level indicators were included.
In step two, a three-round modified Delphi process was conducted according to published procedures and guidelines between January and June 2020 [31, 32]. Twenty-nine experts recruited in the process were asked to rate the importance of first-and-second level indicators, using 5-point Likert scales with ratings from 1 (definitely not important) to 5 (extremely important) and provide suggestions or comments about their ratings.
Stage 2: testing its reliability and validity
Eligible participants were requested to complete the FRSAS assessment by themselves independently as much as possible. If it were challenging for participants to fill in the scale, such as the blurred vision of themselves, the caregivers or researchers would verbally repeat the items to them and tick what they chose. In other words, the choice made in each item was based on the participants’ response. Some demographic and clinical data were recorded initially, including age, gender, height, weight, marital status, educational level, living condition and residential type. Additional questions were asked regarding the fall accidents and fear of falling: “In the past 12 months, do you have any falls including a slip or trip in which you lost your balance and landed on the floor or ground or lower level?” and “generally speaking, do you have the fear of falling?”. To examine test-retest reliability, fifty participants who were selected from the total sample by using random number table were invited to complete the FRSAS assessment once more in 1 week apart. The FRSAS could be re-evaluated by an in-person or phone call.
Instruments
The FRSAS, which is developed by our research team, constitutes 41 items in 5 dimensions: demographic characteristic, physical functions, general conditions, contexts and health-related issues and medication. All items are dichotomously rated as “Yes” if the picture described in the scale is present and “No” if the picture is not fit for the older adults. Each item can be scored as 0 or 1 depending on the question, while the scoring of item H12 rests with the number of chronic diseases identified ranging from 0 to 6. Individuals’ scores from each of the 5 dimensions are added to produce a total possible score of 46. A higher score on the FRSAS indicates a higher risk of falling.
Statistical analysis
Data analyses were performed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA). Descriptive data were reported as frequency and percentage (%). Continuous data with normally distribution were given as mean and standard deviation (SD); otherwise, medians and 1st and 3rd quartiles were calculated. P < 0.05 was considered as statistical significance for the differences.
Feasibility was assessed by using the completion rate, the time taken to complete the scale and the understandability of the scale (this information was collected by the feedback of participants). Internal consistency of FRSAS was measured using Cronbach’s α. According to the literature, Cronbach’s α greater than 0.9 was considered as excellent, 0.8–0.9 as good, 0.7–0.8 as acceptable, 0.6–0.7 as questionable, 0.5–0.6 as poor and lower than 0.5 as unacceptable [33]. The test-retest reliability was examined using the intra-class correlation ICC (2,1), which was classified into four categories based on ICC value: poor (less than 0.5), moderate (between 0.5 and 0.75), good (between 0.75 and 0.9) and excellent (greater than 0.90) [34]. Absolute reliability was assessed by calculating the standard error of measurement (SEM) for the repeated measurements. The inverse relationship is presented between ICC and SEM, which indicates the higher reliability a test has, the fewer error of measurement [35].
The Bland and Altman method was performed to evaluate agreement in scores between two tests by calculating the difference score and mean score between test and retest and plotting them against each other. Acceptable agreement between the two tests was found when 95% of the mean scores fell between the limits of agreement [36]. It is suggested that the participants will score more fall risks in the initial test than the repeated if the mean difference is positive, whereas a negative mean difference indicates the opposite. Meanwhile, no difference is found in the FRSAS score between the two tests when the mean difference is zero.
Exploratory factor analysis (EFA) was applied to determine which subgroup each item could be categorized. Kaiser-Meyer-Olkin’s test and Bartlett’s test of sphericity were performed to determine the sample adequacy and the inter-variables relationship, respectively. The factor structure was explored using principal component analysis with varimax rotation. We used t-tests or Wilcoxon rank-sum test to analyze the differences in total scores and sub-dimensional scores of FRSAS between the faller and nonfaller groups. P < 0.05 was considered as statistical significance for the differences.
Results
Development of the FRSAS
Through three-round consultations, 5 first-level and 41 second-level indicators were finalized, as presented in Table 2.
Table 2.
The first-level and second-level indicators of the FRSAS
| First-level indicator | Code | Second-level indicator |
|---|---|---|
| Demographic (D) | D1 | Age ≥ 80 years |
| Physical functions (P) | P1 | Getting in and out of bed safely and effortlessly |
| P2 | Rising from the chair and sitting down safely and effortlessly | |
| P3 | Toileting safely and effortlessly | |
| P4 | Bathing safely and effortlessly | |
| P5 | Reaching/Carrying the commonly used items effortlessly without inducing a fall | |
| P6 | Stopping to pick up little items, such as pieces of paper, coin, etc. | |
| P7 | Translating the food from kitchen to table safely and effortlessly | |
| P8 | Comfortable and non-slip shoes | |
| P9 | Donning and doffing pants, skirts, shoes, and socks effortlessly | |
| P10 | Going up and down stairs smoothly (assistive device can be used, such as rails) | |
| P11 | Stepping over obstacles smoothly | |
| P12 | Walking with mobility aid, such as cane. | |
| General conditions (G) | G1 | Good quality of sleep |
| G2 | Being fatigue easily during daily activities | |
| G3 | Going to be bathroom habitually at night | |
| G4 | Exercising more than half an hour daily | |
| G5 | Fear of falling | |
| Contexts (C) | C1 | Flat ground at home |
| C2 | Debris clustered on the ground | |
| C3 | Moveable mat or carpet unsteadily | |
| C4 | Water residual on the ground frequently | |
| C5 | Switching on and off the light conveniently in the bed | |
| C6 | Well-lit corridor, house, and community | |
| C7 | Immobilized non-slip mat in the bathroom | |
| C8 | Handrails installed in the bathroom | |
| C9 | Residing in a bungalow or walk-up building | |
| C10 | Living alone | |
| C11 | Understanding fall prevention heretofore | |
| Health-related issues and medication (H) | H1 | Dizziness and vertigo |
| H2 | Arthrodynia of lower extremity | |
| H3 | ROM (Range of motion) limitation or deformity of lower extremity | |
| H4 | Vision problems | |
| H5 | Toileting frequently for bowel and bladder dysfunction | |
| H6 | Numbness and pain in lower extremities for cervical and/or lumbar disease | |
| H7 | History of brain injury and cerebrovascular accident (CVA) | |
| H8 | Taking antiepileptic drug (AED) | |
| H9 | Taking antipsychotic | |
| H10 | Fall histories | |
| H11 | Excessive drinking daily (the average of alcohol consumption more than 25 g per day for male, which equals to 750 ml beer, 250 ml wine, 75 g liqueur with 38°and 50 g highly liqueur, while the threshold is 15 g for female) | |
| H12 |
Chronic disease (Tick where relevant): Alzheimer’s Disease Parkinsonian Syndrome Coronary Heart Disease Chronic Obstructive Pulmonary Disease (COPD) Osteoporosis Diabetes Mellitus |
The demographics of participants
Of the 230 participants recruited in the study, 222 participants completed the assessment as required through two-round quality check. Among the 222 qualified participants, 82 were male accounting for 36.94% and 140 females representing 63.06% of the total. The mean age of participants was 73.84 ± 7.46 years, ranging from 65 to 90 years. Around 30% of older adults reported a history of falls in the past 12 months. Meanwhile the number of participants who had a fear of falling doubled to those who had not. The demographic information of participants was enlisted in Table 3.
Table 3.
Demographics of participants (n = 222)
| Project | Category | Frequency (N) | Percentage (%) |
|---|---|---|---|
| Sex | Male | 82 | 36.94 |
| Female | 140 | 63.06 | |
| Age (years) | 65 ~ 74 | 130 | 58.56 |
| 75 ~ 84 | 62 | 27.93 | |
| ≥85 | 30 | 13.51 | |
| BMI (kg/m2) | <18.5 | 8 | 3.60 |
| 18.5 ~ 23.9 | 97 | 43.69 | |
| 24.0 ~ 27.9 | 83 | 37.39 | |
| ≥28 | 34 | 15.32 | |
| Marital status | Unmarried | 2 | 0.90 |
| Married | 180 | 81.08 | |
| Divorced | 2 | 0.90 | |
| Widowed | 38 | 17.12 | |
| Educational level | Primary school or below | 23 | 10.36 |
| Secondary school | 58 | 26.13 | |
| High school | 55 | 24.77 | |
| Junior college | 41 | 18.47 | |
| Undergraduate | 41 | 18.47 | |
| Master or above | 4 | 1.80 | |
| Living condition | Alone | 28 | 12.61 |
| With family members | 194 | 87.39 | |
| Residential type | Bungalow | 8 | 3.60 |
| Walk-up building | 119 | 53.60 | |
| Building with elevator | 95 | 42.79 | |
| Fear of falling | Yes | 159 | 71.62 |
| No | 63 | 28.38 | |
| History of falls in the past 12 months | Yes | 73 | 32.88 |
| No | 149 | 67.12 |
Feasibility
The completion rate of the FRSAS was 96.52% and the FRSAS could be completed in 10 min. The majority of items on the FRSAS could be easily understood without ambiguity. Based on the feedback of the respondents, some ambiguous items should be modified or elaborated to reach a consensus. For example, item P11 “stepping over obstacles smoothly” can be parenthetically noted the characteristics of obstacles (e.g., the height and width) and item G1 “good quality of sleep” can be appended with some explanatory descriptions to explicate the good quality of sleep. Overall, the FRSAS had relatively high feasibility.
Internal consistency
The internal consistency of the entire FRSAS was acceptable with Cronbach’s α = 0.757. Cronbach’s α if item deleted ranged between 0.746 and 0.768. When removing eight items in which Cronbach’s α if item deleted was lower than 0.757, the total Cronbach’s α rose to 0.800.
Test-retest reliability
Fifty older adults participated in the retest of FRSAS by either in-person or phone call. The standard error of measurement (SEM) of the FRSAS was 0.186. The distribution of difference scores between test and retest were conformed to a normal distribution (determined by the Shapiro-Wilks test). The overall ICC (2,1) value for the test-retest reliability was 0.967 (Table 4).
Table 4.
Results of analyses of test–retest reliability
| Test 1 | Test 2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N = 222 | Mean | SD | Range | Mean | SD | Range | ICC (2,1) | 95%CI | SEM |
| FRSAS | 13.54 | 5.02 | 6 ~ 26 | 13.12 | 5.12 | 5 ~ 25 | 0.967 | 0.943 ~ 0.981 | 0.186 |
FRSAS Fall Risk Self-Assessment Scale, SD Standard Deviation, ICC (2,1) Intra-Class Correlation, SEM Standard Error of Measurement
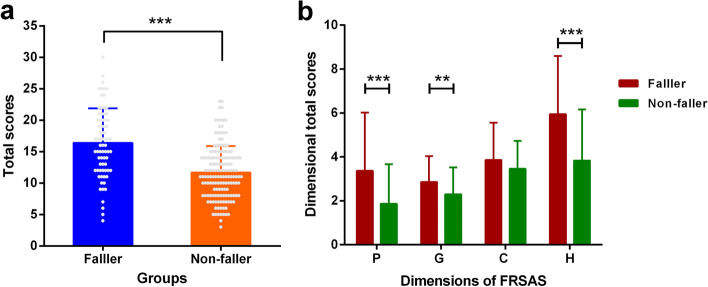
A minor positive mean difference (Mean = 0.06) yielded on FRSAS scoring between the initial and repeated assessments and 95% of the difference score fell between the limits of agreement (95% LoA: −2.519 ~ 2.639), indicating that the consistency of the scoring was obtained over time as depicted in Fig. 1.
Fig. 1.
Bland and Altman plot on the agreement between test and retest
Construct validity
The KMO’s value was 0.728 (value higher than 0.7 was considered as acceptable) and Bartlett’s test of sphericity was significant (P < 0.001), both of them suggested that factor analysis was appropriate to analyze the data [37]. According to Kaiser criterion [38], 14 factors with eigenvalues greater than 1 were extracted, explaining 61.744% of the total variance. Items were considered to fall in each factor if its factor loading was 0.40 or above [39]. However, five items consisting of G3, C1, C7, H1 and H5 did not fit for any factor with its factor loading ranging from 0.347 to 0.397.
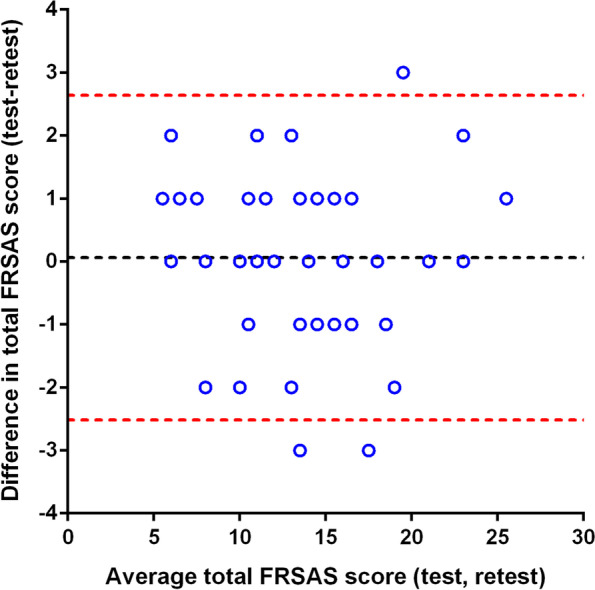
Discriminant validity
The FRSAS total score was significantly higher for older adults who have fallen than for older adults who have not fallen in their past 12 months (Fig. 2a). When we compared dimensional total scores (except for D dimension, because it was not distributed normally) between faller and non-faller groups, the average dimensional score was significantly higher in those with a history of fall apart from C-dimension (Fig. 2b). There was no difference in the C-dimensional scores between the faller and non-faller groups (t = 1.809, P = 0.073). Our results showed a significant difference in D-dimensional scores between the two groups by Wilcoxon rank-sum test (Z = 2.248, P < 0.05).
Fig. 2.
The difference of scores between faller and non-faller groups. a The difference of total scores between faller and non-faller groups. b The difference of dimensional total scores between faller and non-faller groups. ** p < 0.01, *** p < 0.001
Discussion
The development of the FRSAS including five dimensions (i.e., the demographic, physical functions, general conditions, contexts, health-related issues and medications) is tailored to the Chinese geriatric-characteristic culture, which is reflected in the specific operational definition of each item. The FRSAS, characterized by its simplicity, understandability, fast-screening and administrator-free, can evaluate the intrinsic and extrinsic risk factors of falls comprehensively. Furthermore, our findings indicated that the FRSAS had relatively good levels of reliability and validity, signifying that this tool could be utilized to assess fall risk in the community-dwelling Chinese older population.
The results showed that the internal consistency of the FRSAS was acceptable (Cronbach’s α = 0.757). If eight items (Cronbach’s α became higher than the previous one when deleting the item) were removed, Cronbach’s α increased to 0.800. Neither a low Cronbach’s α nor a very high Cronbach’s α indicates an acceptable correlation between the items in the scale [40]. The former makes the items unjustified. The latter manifests the redundancy of one or more items. Compared with the self-rated Fall Risk Questionnaire (Cronbach’α =0.670) and the Chinese Home-FAST self-reported screening tool (Cronbach’α =0.940) with regard to the internal consistency [19, 20], the Cronbach’α of the scale obtained in this study was good, indicating that each item of the scale has a good homology.
The Intraclass Correlation Coefficient ICC (2,1) of FRSAS was 0.967 (95%CI: 0.943 ~ 0.981), indicating its excellent reproducibility. It is noteworthy that the ICC (2, 1) is very sensitive and directly impacted by the intra- and inter-subject variability [41]. The FRSAS scores also showed good agreement based on the SEM value and Bland-Altman plot for both tests in the one-week interval. Ng et al. reported that the ICC of the Falls Risk for Older People in the community screening tool was only 0.70 [23]. Likewise, Lai et al. found that ICC of the Chinese Home-FAST self-reported screening tool was 0.88 [20]. Both suggested that the FRSAS had good reproducibility.
According to the exploratory factor analysis, the whole scale was divided into 14 factors. The criterion used in this study to determine how many factors to retain is the Kaiser criterion, which proposed that an eigenvalue greater than 1.0 is a good lower bound for expecting a factor to be meaningful [38]. Controversially, the consensus was reached in the literature that the Kaiser criterion probably gets less accurate as more items are analyzed [42]. Based on this, researchers suggested that the Kaiser criterion can be employed in conjunction with examination of the scree plot for deciding the number of factors to extract in an exploratory factor analysis [43]. However, Ruscio & Roche pointed out that both the Kaiser criterion and scree plots have been shown to overestimate the number of dimensions in data. In the future study, it is recommended that taking advantage of parallel analysis (PA) supplemented by comparison data (CD) can help researchers model their data more precisely and ultimately to develop more reliable and valid assessment instruments [44].
In term of the discriminant validity, the FRSAS scores in the faller group were significantly higher than the non-faller group, verifying our predefined hypotheses that FRSAS would show greater scores among older individuals who have fallen in the previous 1 year than among those who have not. Likewise, the inherent dimensions also yielded the same result except for C-dimension (i.e., contexts). Non-significantly statistical differences for the C-dimension might be explained from following aspects. First of all, the samples included in this study were the community-dwelling older population in Beijing, whose living environment had common problems such as old floors and narrow space, resulting in the consequence that the distinction between falling and the non-falling older population was not high. If older adults in other areas (e.g., western, eastern, southern, or central regions of China) were included, the scores of contextual dimensions might show statistical differences due to the change in a living environment. Secondly, since older adults were gathered in the specific place for fall risk assessment, the identification of home hazards in the scale mainly depended on retrospective information rather than observation in real-life environments and contexts, which caused the insignificant difference of contextual dimension in the older population with or without falling. Finally, home hazards could not be efficaciously reflected using the 11 items in the scale. Some tools that existed for home hazards evaluation had proven to be valid. The Chinese HOME FAST self-reported screening tool provided satisfactory discriminatory ability concerning unplanned fall incidents [20]. However, the items in this self-reported screening tool are not as simple as the one we developed, which causes that more time is required for older adults to consolidate their identification of home hazards. Overall, we can use it as reference to enhance the differentiation of the contextual dimension of this scale in the group with or without falls.
The strength of this study is that it is the first study to develop a FRSAS accommodated to Chinese geriatric-characteristic culture and evaluate its reliability and validity among community-dwelling older people. FRSAS once developed successfully, can assist the clinicians or general healthcare providers for fall prevention among older people living in a community setting. However, it must be taken into account that some limitations were not avoided in this study. First of all, some inclusion and exclusion criteria were dependent on the self-reported information of participants, such as no communication barrier, moderate to severe cognitive impairment or mental disorders. Secondly, all the participants were recruited from three communities in Beijing by the convenience sampling strategy, causing that the sample could not be completely representative of the whole population and the results in the pilot study could not be generalized to the whole population. Thirdly, since this was a cross-sectional study, falling information was taken retrospectively, which caused the information bias to some extent. Furthermore, the assessment of falls and fear of falling were self-reported by participants. Lastly, the criterion validity and the responsiveness of FRSAS was not detected.
Conclusions
To sum up, the FRSAS including 41 items demonstrated relatively good feasibility as well as satisfactory results in the internal consistency, test-retest reliability, and discriminant validity. However, some concerns had arisen regarding the construct validity in the pilot study. Adaptation of the FRSAS is the next stage of our future work, followed by testing in different types of population using larger sample sizes as well as providing a more convenient and fast-screening tool for Chinese community-dwelling older people.
Supplementary Information
Additional file 1. The process of literature review.
Acknowledgements
The authors thank the panel members who participated in the modified Delphi process and the staffs who assisted in data collection in three communities, Haidian district, Beijing.
Abbreviations
- FRSAS
The Fall Risk Self-Assessment Scale
- D
Demographic Characteristics
- P
Physical Functions
- G
General Conditions
- C
Contexts
- H
Health-related Issues and Medication
- Sen
Sensibility
- Spe
Specificity
- AUC
Area Under Curve
- BBS
Berg Balance Scale
- TUG
Time “Up & Go” test
- ABC-C
Chinese version of the Activities-specific Balance Confidence Scale
- HOME FAST
The Home Falls and Accidents Screening Tool
- SD
Standard Deviation
- ICC
Intra-Class Correlation
- SEM
Standard Error of Measurement
- 95% LoA
95% Limits of Agreement
- EFA
Exploratory Factor Analysis
- KMO
Kaiser-Meyer-Olkin
Authors’ contributions
MWZ, YYY, LG and ZZW conceived and designed the study. MWZ supervised the project and revised the manuscript. YTR, XMD and ZZW contributed to the data collection. YTR, XMD, LG and ZZW analyzed and interpreted the collected data. ZZW was a major contributor in drafting the manuscript. LG, YYY and MWZ critically revised the manuscript. All authors read and approved the final manuscript.
Funding
This study has been funded by National Key R&D Program of China (Grant No. 2018YFC2001400). The funders played no role in study design or conduct.
Availability of data and materials
The datasets used and/or analyzed during the study are available from the corresponding author or first author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was performed in accordance with the principles of the Declaration of Helsinki and was approved by the Peking University Third Hospital Medical Science Research Ethics Committee (Ref: M2020392). Written informed consents were obtained from all participants in the beginning of the study.
Consent for publication
Not applicable.
Competing interests
No potential conflict of interest was reported by the authors.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.DeGrauw X, Annest JL, Stevens JA, Xu L, Coronado V. Unintentional injuries treated in hospital emergency departments among persons aged 65 years and older, United States, 2006–2011. J Saf Res. 2016;56:105–109. doi: 10.1016/j.jsr.2015.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heinrich S, Rapp K, Rissmann U, Becker C, König HH. Cost of falls in old age: a systematic review. Osteoporosis Int. 2010;21(6):891–902. doi: 10.1007/s00198-009-1100-1. [DOI] [PubMed] [Google Scholar]
- 3.Kwan MM, Close JC, Wong AK, Lord SR. Falls incidence, risk factors, and consequences in Chinese older people: a systematic review. J Am Geriatr Soc. 2011;59(3):536–543. doi: 10.1111/j.1532-5415.2010.03286.x. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . WHO global report on falls prevention in older age. 2016. [Google Scholar]
- 5.Hopewell S, Adedire O, Copsey BJ, Boniface GJ, Sherrington C, Clemson L, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2018;7:CD012221. doi: 10.1002/14651858.CD012221.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peel NM, Kassulke DJ, McClure RJ. Population based study of hospitalised fall related injuries in older people. Inj Prev. 2002;8(4):280–283. doi: 10.1136/ip.8.4.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Malley N, Clifford AM, Comber L, Coote S. Fall definitions, faller classifications and outcomes used in falls research among people with multiple sclerosis: a systematic review. Disabil Rehabil. 2020;44(6):856–864. doi: 10.1080/09638288.2020.1786173. [DOI] [PubMed] [Google Scholar]
- 8.Gazibara T, Kurtagic I, Kisic-Tepavcevic D, Nurkovic S, Kovacevic N, Gazibara T, Pekmezovic T. Falls, risk factors and fear of falling among persons older than 65 years of age. Psychogeriatrics. 2017;17(4):215–223. doi: 10.1111/psyg.12217. [DOI] [PubMed] [Google Scholar]
- 9.Peng K, Tian M, Andersen M, Zhang J, Liu Y, Wang Q, et al. Incidence, risk factors and economic burden of fall-related injuries in older Chinese people: a systematic review. Inj Prev. 2019;25(1):4–12. doi: 10.1136/injuryprev-2018-042982. [DOI] [PubMed] [Google Scholar]
- 10.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 11.Phelan EA, Mahoney JE, Voit JC, Stevens JA. Assessment and management of fall risk in primary care settings. Med Clin North Am. 2015;99(2):281–293. doi: 10.1016/j.mcna.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gates S, Smith LA, Fisher JD, Lamb SE. Systematic review of accuracy of screening instruments for predicting fall risk among independently living older adults. J Rehabil Res Dev. 2008;45(8):1105–1116. [PubMed] [Google Scholar]
- 13.Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg balance scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449–459. doi: 10.2522/ptj.20070251. [DOI] [PubMed] [Google Scholar]
- 14.Kang L, Han P, Wang J, Ma Y, Jia L, Fu L, et al. Timed up and go test can predict recurrent falls: a longitudinal study of the community-dwelling elderly in China. Clin Interv Aging. 2017;12:2009–2016. doi: 10.2147/CIA.S138287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wrisley DM, Kumar NA. Functional gait assessment: concurrent, discriminative, and predictive validity in community-dwelling older adults. Phys Ther. 2010;90(5):761–773. doi: 10.2522/ptj.20090069. [DOI] [PubMed] [Google Scholar]
- 16.Guan Q, Han H, Li Y, Zhao L, Jin L, Zhan Q. Activities-specific balance confidence (ABC) scale adapted for the mainland population of China. Clin Rehabil. 2012;26(7):648–655. doi: 10.1177/0269215511427748. [DOI] [PubMed] [Google Scholar]
- 17.Guo QY, Guo MJ, Zhang L, Li D, Guo LN, Gao H, Liu K. Evaluation of the reliability and validity of Chinese version of falls efficacy scale. Chinese General Practice. 2015;18(35):4273–4276. [Google Scholar]
- 18.Chan PPW, Chan APS, Lau E, Delbaere K, Chan YH, Jin XK, et al. Translation and validation study of the Chinese version iconographical falls efficacy scale-short version (icon-FES) Arch Gerontol Geriatr. 2018;77:1–7. doi: 10.1016/j.archger.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 19.Song JM, Wan DT, Zheng ZM. Reliability and validity of US CDC self-rated fall risk questionnaire among Chinese community-dwelling older adults. Chin J Public Health. 2020;36(4):592–595. [Google Scholar]
- 20.Lai FHY, Yan EWH, Mackenzie L, Fong KNK, Kranz GS, Ho ECW, et al. Reliability, validity and clinical utility of a self-reported screening tool in the prediction of fall incidence in older adults. Disabil Rehabil. 2020;42(21):3098–3105. doi: 10.1080/09638288.2019.1582721. [DOI] [PubMed] [Google Scholar]
- 21.Chen PL, Lin HY, Ong JR, Ma HP. Development of a fall-risk assessment profile for community-dwelling older adults by using the National Health Interview Survey in Taiwan. BMC Public Health. 2020;20(1):234. doi: 10.1186/s12889-020-8286-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu TW, Ng SSM. Assessing the fall risks of community-dwelling stroke survivors using the short-form physiological profile assessment (S-PPA) PLoS One. 2019;14(5):e0216769. doi: 10.1371/journal.pone.0216769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ng SSM, Liu TW, Kwong PWH, Choy HM, Fong TYK, Lee JYC, et al. Psychometric testing of the fall risks for older people in the community screening tool (FROP-com screen) for community-dwelling people with stroke. PLoS One. 2020;15(5):e0233045. doi: 10.1371/journal.pone.0233045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fielding SJ, McKay M, Hyrkas K. Testing the reliability of the fall risk screening tool in an elderly ambulatory population. J Nurs Manag. 2013;21(8):1008–1015. doi: 10.1111/jonm.12192. [DOI] [PubMed] [Google Scholar]
- 25.Peeters GM, Pluijm SM, van Schoor NM, Elders PJ, Bouter LM, Lips P. Validation of the LASA fall risk profile for recurrent falling in older recent fallers. J Clin Epidemiol. 2010;63(11):1242–1248. doi: 10.1016/j.jclinepi.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 26.Wang ZZ, Gu L, Zhou MW, Yang YY, Dai HL, Liu XX. Preliminary development of the fall risk self-assessment scale for home-dwelling elderly in China. Chinese J Rehabil Med. 2021;36(12):1505–1511. [Google Scholar]
- 27.Jialiang W. Clinical epidemiology: clinical research design, measurement and evaluation (published in Chinese) Shanghai: Shanghai Scientific & Technical Publishers; 2014. [Google Scholar]
- 28.Bóriková I, Žiaková K, Tomagová M, Záhumenská J. The risk of falling among older adults in long-term care: screening by the Morse fall scale. KONTAKT. 2018;20(2):e111–e119. [Google Scholar]
- 29.Ivziku D, Matarese M, Pedone C. Predictive validity of the Hendrich fall risk model II in an acute geriatric unit. Int J Nurs Stud. 2011;48(4):468–474. doi: 10.1016/j.ijnurstu.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 30.Romli MH, Mackenzie L, Lovarini M, Tan MP, Clemson L. The interrater and test-retest reliability of the home falls and accidents screening tool (HOME FAST) in Malaysia: using raters with a range of professional backgrounds. J Eval Clin Pract. 2017;23(3):662–669. doi: 10.1111/jep.12697. [DOI] [PubMed] [Google Scholar]
- 31.Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, Wales PW. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67(4):401–409. doi: 10.1016/j.jclinepi.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 32.Hsu C, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval. 2007;12(10):1–8. [Google Scholar]
- 33.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. [Google Scholar]
- 34.Portney LG, Watkins MP. Foundations of clinical research: applications to practice. Harlow: Pearson Education UK; 2013. [Google Scholar]
- 35.Harvill LM. An NCME instructional module on. Standard error of measurement. Educ Meas-Issues Pract. 1991;10(2):33–41. [Google Scholar]
- 36.Giavarina D. Understanding bland Altman analysis. Biochem Medica. 2015;25(2):141–151. doi: 10.11613/BM.2015.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yong AG, Pearce S. A beginner’s guide to factor analysis: focusing on exploratory factor analysis. Tutor Quant Methods Psychol. 2013;9(2):79–94. [Google Scholar]
- 38.Kaiser HF. A second generation little jiffy. Psychometrika. 1970;35:401–415. [Google Scholar]
- 39.Hair JF, Jr, Black WC, Babin BJ, et al. Multivariate data analysis (seventh edition) Edinburgh: Pearson; 2014. [Google Scholar]
- 40.Terwee CB, Bot SDM, de Boer MR, van der Windt DAWM, Knol DL, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 41.Rinderknecht MD, Lambercy O, Raible V, Büsching I, Sehle A, Liepert J, Gassert R. Reliability, validity, and clinical feasibility of a rapid and objective assessment of post-stroke deficits in hand proprioception. J NeuroEng Rehabil. 2018;15(1):47. doi: 10.1186/s12984-018-0387-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Osborne J, Costello A, Kellow J. Best practices in exploratory factor analysis. In: Osborne J, editor. Best practices in quantitative methods. Thousand Oaks: SAGE Publications, Inc.; 2008. pp. 86–99. [Google Scholar]
- 43.Cattell RB. The scree test for the number of factors. Multivariate Behav Res. 1966;1(2):245–276. doi: 10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- 44.Ruscio J, Roche B. Determining the number of factors to retain in an exploratory factor analysis using comparison data of known factorial structure. Psychol Assess. 2012;24(2):282–292. doi: 10.1037/a0025697. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. The process of literature review.
Data Availability Statement
The datasets used and/or analyzed during the study are available from the corresponding author or first author on reasonable request.