Abstract
The COVID-19 pandemic significantly affected health care and in particular surgical volume. However, no data surrounding lost hospital revenue due to decreased cardiac surgical volume have been reported. The National Inpatient Sample database was used with decreases in cardiac surgery at a single center to generate a national estimate of decreased cardiac operative volume. Hospital charges and provided charge to cost ratios were used to create estimates of lost hospital revenue, adjusted for 2020 dollars. The COVID period was defined as January to May of 2020. A Gompertz function was used to model cardiac volume growth to pre-COVID levels. Single center cardiac case demographics were internally compared during January to May for 2019 and 2020 to create an estimate of volume reduction due to COVID. The maximum decrease in cardiac surgical volume was 28.3%. Cumulative case volume and hospital revenue loss during the COVID months as well as the recovery period totaled over 35 thousand cases and 2.5 billion dollars. Institutionally, patients during COVID months were younger, more frequently undergoing a CABG procedure, and had a longer length of stay. The pandemic caused a significant decrease in cardiac surgical volume and a subsequent decrease in hospital revenue. This data can be used to address the accumulated surgical backlog and programmatic changes for future occurrences.
Keywords: Cardiac surgery, COVID 19, Pandemic, Economic burden, Hospital charges, Hospital costs, Health care
Abbreviations: CABG, coronary artery bypass graftin; ICD, international classification of diseases; NIS, national inpatient samples; CCS, clinical classification software
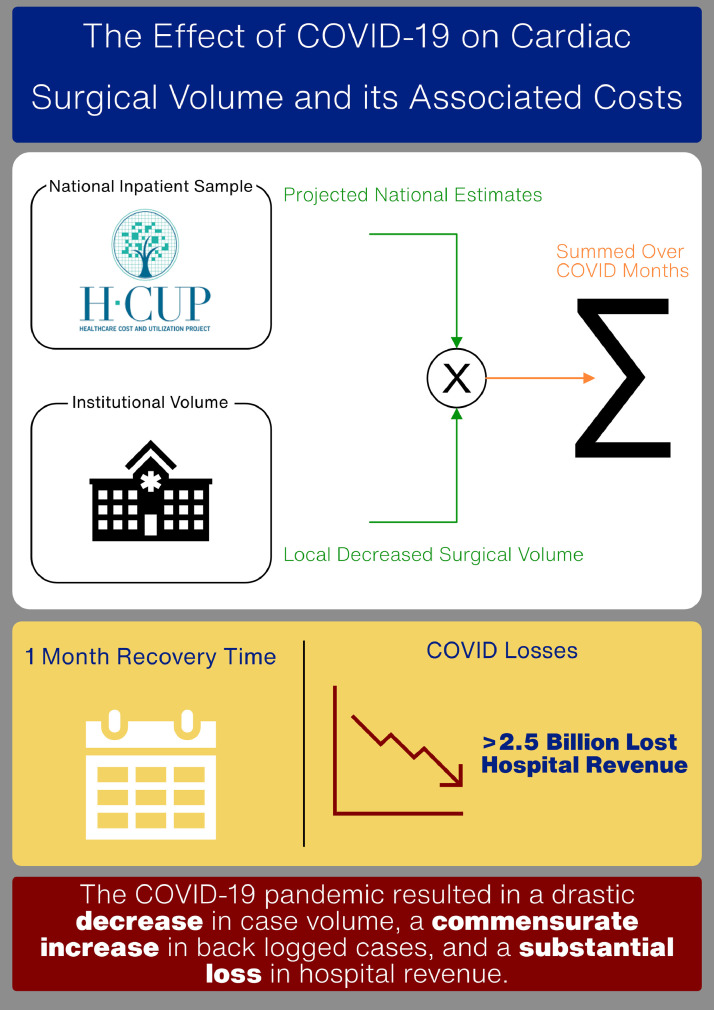
Graphical Abstract
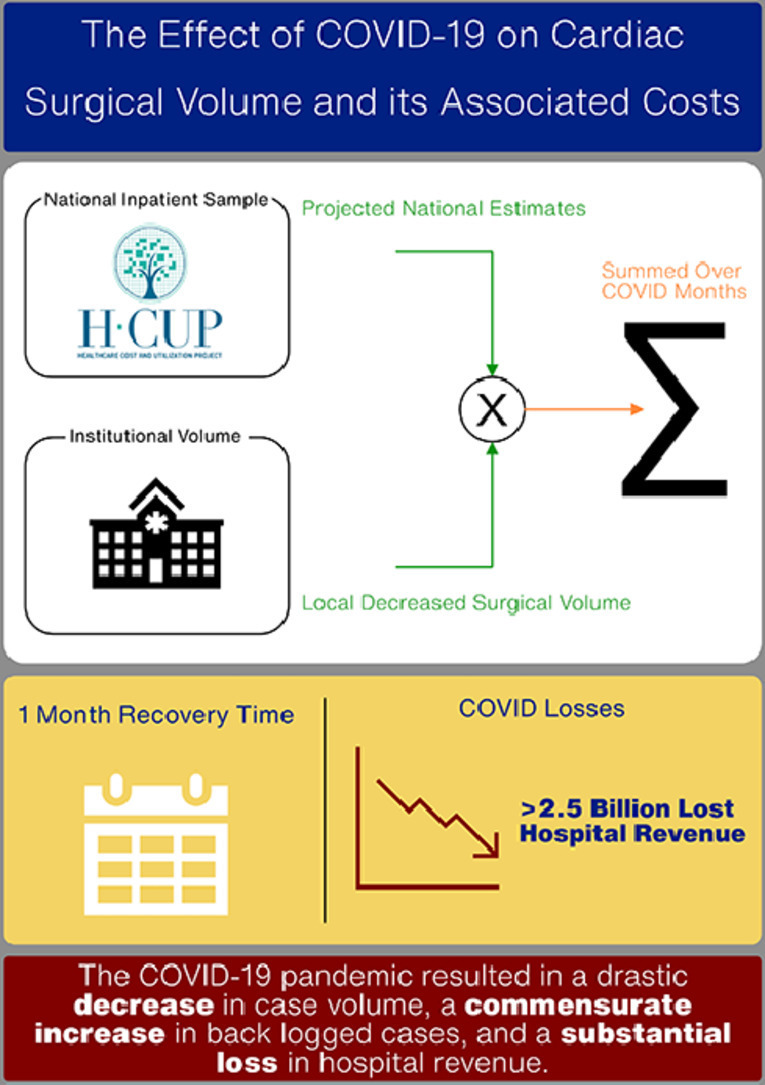

Projected lost surgical cases (blue bars) and hospital revenue (orange circles).
Alt-text: Unlabelled box
Central Message.
'The COVID-19 pandemic significantly decreased cardiac operative volume across the country. Our center underwent a fast recovery, but an nationally estimated substantial decrease in hospital revenue and case backlog occurred.
Alt-text: Unlabelled box
Perspective Statement.
The effects of COVID-19 on the health care system are profound. As cardiothoracic surgery is a top earner for hospital systems, decreases in operative volume likely result in significant lost revenue. The use of a national database allows for an estimate of lost revenue using institutional and published decreased cardiac surgery volume with the goal of ameliorating current and future pandemic effects.
Alt-text: Unlabelled box
INTRODUCTION
The COVID-19 pandemic has wrought unprecedented disturbances throughout society, not just in the United States but globally.1 , 2 From layoffs, city shutdowns, economic turmoil, and loss of life, almost no facet of society is untouched, and health care is no exception.3 The effects on health care have been variable. While the volume of some services and elective procedures has decreased,4 , 5 there has been an inundation of patients in other areas, such as the intensive care unit.6, 7, 8 While surgery as a whole has been affected, various specialties have had different experiences with changes to case volume-based primarily on the urgency of the surgery required. This reallocation shift and eventual return to pre-pandemic protocols for patient care will continue to impact hospitals, surgeons, and patients significantly.
The American Hospital Association estimated a loss of more than 160 billion dollars from all canceled surgeries and other services between March and June of 2020 due to COVID.9 As cardiothoracic operations are routinely high charging procedures for hospitals,10 , 11 a decrease in case volume is likely to reduce hospital revenue significantly. In a recent survey of cardiothoracic surgery program directors and their response to COVID-19, over 95% of respondents reported canceling elective and nonurgent operations, with a further 33% restricting urgent operations during the peak of the pandemic.12 In another survey, with 502 cardiac surgeons responding, 81% indicated that only urgent and emergent cases were scheduled, with 76% reporting a greater than 50% decrease in surgery volume.13 In this paper, we sought to use our institution's change in cardiac surgery volume, representative of a large volume academic center, and the National Inpatient Sample (NIS) database to estimate the nationwide effect of COVID-19 on hospital volume and the associated lost hospital revenue.
METHODS
Patient Population and Baseline Variables
The National Inpatient Sample Database (NIS) is a prospectively maintained database created by the Health Care Cost and Utilization Project. This database is drawn from all states and covers over 97% of the US population. The data given is a 20% stratified sample of all discharges with provided weights to estimate the national population. Furthermore, the NIS includes ICD 9 and 10 codes of the diagnosis and procedures performed for each patient and the hospital charges for each stay. The NIS was filtered for all patients with hospital stays between 2004 and 2017 who underwent cardiac surgery. The procedure-related Clinical Classifications Software (CCS) numbers used to screen for cardiac surgery cases are outlined in Table 1 . The CCS aggregates ICD 9 and 10 codes to useful groupings for broader categories of operations, facilitating a constant comparison between ICD 9 and 10 codes. These patients were stratified by month and year of their hospital stay. All hospital charges were adjusted to 2020 dollars using each year's gross domestic product.14 The NIS provides event level weights which were applied to generate national estimates of volume and charges. Additionally, hospital level charge-to-cost ratios were provided by the database and used to convert hospital charges to hospital costs. It is important to clarify that hospital costs are a better estimate of the revenue a hospital would receive for a patient stay. As such, changes in the hospital cost due to COVID can be considered lost revenue, which will be addressed as such from here on. Additionally, our institutional Society of Thoracic Surgery Database was utilized to analyze cases between January and May of 2019 and 2020 to compare baseline features and outcomes. During COVID peak weeks in the state of Pennsylvania, all elective cases at our institutions were carefully scrutinized and only urgent and emergent cases were performed. Most patients undergoing elective surgery for coronary, valvular or aortic disease were reviewed by 2 surgeons to ensure that the risk of watchful waiting exceeded risk of contracting COVID-19 while an inpatient during surgery and hospitalization. Moreover, every patient was tested for COVID-19 prior to elective or urgent surgery IRB approval was waived for this project.
Table 1.
List of Clinical Classification Software Numbers Used
| Clinical Classification Number | Procedure Category |
|---|---|
| 43 | Heart Valve Procedures |
| 44 | Coronary Artery Bypass Graft |
| 49 | Other Operating Room Heart Procedure |
| 50 | Extra Corporeal Circulation Auxiliary to Open Heart Procedures |
| 52 | Aortic Resection; replacement or anastomosis |
Statistical Methods
The NIS data was available through 2017, and thus the case volume and hospital charges were projected to 2020. Linear regression was carried on cardiac surgery volume and hospital charges using the month as the dependent variable. The resulting regression equation was used to estimate the 2020 COVID-19 period for the months January to May. Our institutional volume from January to May was compared to the previous year's (2019) to estimate volume loss. Each month of both years was compared as a percentage of our average monthly institutional volume across 2019, increasing the comparison's robustness. The subsequent change in the percentages was treated as a change in volume. This percentage loss was then applied to the monthly case and revenue projections from the linear regression and summed over this period to create cumulative loss estimates (Fig. 1 ). In short, NIS data was used to create projections for expected cardiac surgery volume and revenue in 2020. Our institutional volume experience decreased in 2020 when compared to 2019 served as a percentage change due to COVID that was then projected onto the national estimates, resulting in a national decrease due to COVID. A Gompertz function, a growth model, was fit to our institution's data starting in May and ending in June, which is when our hospital volume returned to normal.
Figure 1.
Single center volume decrease due to COVID was extrapolated to the nation using a national database. While the single center experience showed a rapid recovery, the possible national effect was a substantial amount of backlogged surgical cases with significant lost hospital revenue. (Color version of figure is available online at http://www.semthorcardiovascsurg.com.)
Institution cases were compared with those in 2019 representing the control cases. Categorial and continuous variables were analyzed with Chi Squared and Student's t-test respectively. R (4.0.0 ‘Arbor Day’) was utilized for the analysis.
RESULTS
A total of 976 cases were done between January and May in 2019 and 551 cases were done during the same months in 2020 (Table 2 ). Patients were younger (67 vs 64, p < 0.001) and more frequently male (66.1% vs 71.5%, p < 0.001) during COVID months. Patient BMI was not statistically different and patients had similar STS predicted risk of mortality between the pre-COVID and COVID months. There was an increase in the number of CABG procedures (54.2% vs 64.8%, p < 0.001) whereas the frequency of elective procedures did not differ between cohorts. The length of stay was longer during COVID (9.5 vs 10.5 days, p = 0.044) and 30-day mortality was similar (3.1% vs 4.4%, p = 0.247) between cohorts.
Table 2.
Institutional Case Volume Demographics
| Variable | Pre-COVID | COVID | p-value | |
|---|---|---|---|---|
| Number of Cases | 976 | 551 | - | |
| Age | 67.38 ± 12.98 | 64.65 ± 11.82 | <0.001 | |
| Female | 331 (33.9%) | 157 (28.5%) | 0.034 | |
| BMI | 30.07 ± 6.85 | 30.18 ± 6.74 | 0.758 | |
| STS PROM | 2.15 ± 2.98 | 2.18 ± 3.64 | 0.893 | |
| Operative Cases | <0.001 | |||
| Aortic Root | 33 (3.4%) | 16 (2.9%) | ||
| CABG | 529 (54.2%) | 357 (64.8%) | ||
| Valve | 186 (19.1%) | 122 (22.1%) | ||
| Other | 228 (23.4%) | 56 (10.2%) | ||
| Surgical Status | 0.113 | |||
| Elective | 587 (60.1%) | 304 (55.2%) | ||
| Urgent | 341 (34.9%) | 214 (38.8%) | ||
| Emergent | 45 (4.6%) | 33 (6.0%) | ||
| Salvage | 3 (0.3%) | 0 (0.0%) | ||
| Length of Stay | 9.47 ± 9.45 | 10.52 ± 10.10 | 0.044 | |
| 30-d Mortality | 30 (3.1%) | 24 (4.4%) | 0.247 | |
Variables are presented as count (frequency) and mean (standard deviation) for categorical and continuous variables respectively.
BMI, body mass index; CABG, coronary artery bypass grafting; STS PROM, society of thoracic surgery predicted risk of mortality.
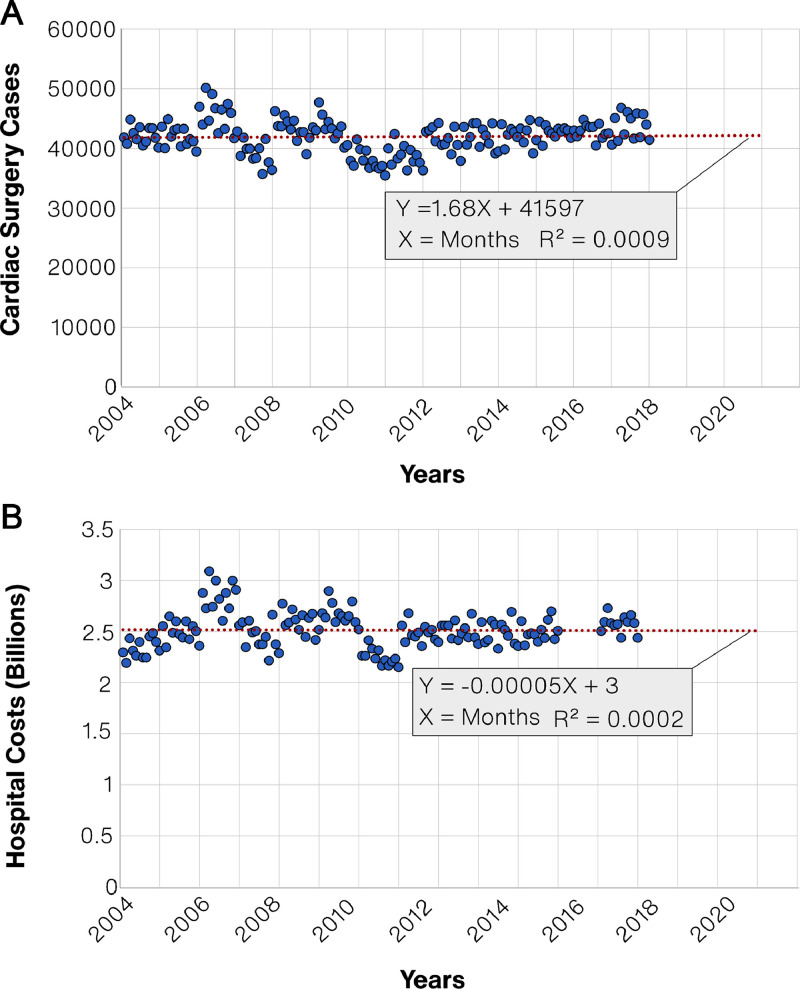
The linear regression for case volume and hospital revenue is presented in Figure 2 . Projected hospital volume remained relatively unchanged over time with a regression slope of 1.68, an intercept of 41,597, and an R2 of 0.0009. Projected hospital revenue was also relatively stable over the study period, with a slope of -0.0005, an intercept of 3, and an R2 of 0.0002 (note units are in billions of dollars). Projected national hospital volume slightly increased from 41,922 cases in January to 41,929 cases in May (Table 3 ). Projected hospital revenue marginally decreased from 2.9895 billion to 2.9892 billion. Note that there is not an R2 for the recovery function. This is because the resolution of our institutional data is month to month and since the recovery occurred over a month, we only have the start and end of the recovery model. There are no datapoints of the dynamic between these 2 points, not allowing for a calculation of a R2.
Figure 2.
Linear Regressions for Surgery Volume and Hospital Revenue. (A) Regression on cardiac surgery volume on a monthly scale. The red dotted line indicates the regression line. (B) Regression on hospital revenue on a monthly scale. The red dotted line indicated the regression line. (Color version of figure is available online at http://www.semthorcardiovascsurg.com.)
Table 3.
Projected National Hospital Volume and Revenue Pre and Post COVID
| Pre-COVID |
COVID |
|||
|---|---|---|---|---|
| Month | Hospital Volume | Hospital Revenue (Billions) | Hospital Volume | Hospital Revenue (Billions) |
| January | 41,921.9 | 2.9895 | 33,868.5 | 2.4152 |
| February | 41,923.6 | 2.9894 | 37,364.9 | 2.6643 |
| March | 41,925.3 | 2.9893 | 39,341.9 | 2.8051 |
| April | 41,927.0 | 2.9893 | 37,367.9 | 2.6642 |
| May | 41,928.7 | 2.9892 | 30,074.5 | 2.1441 |
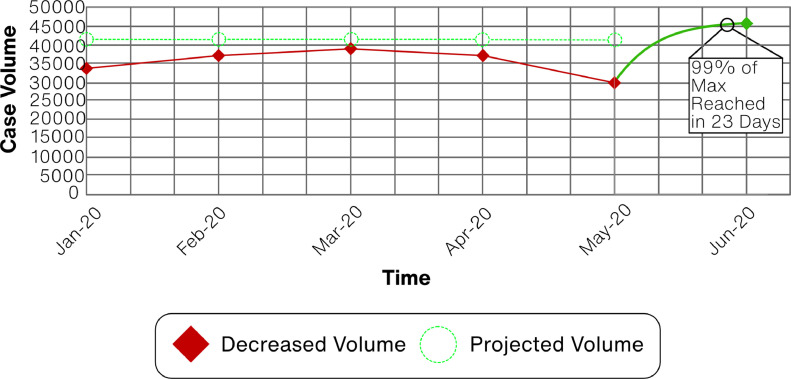
Institutional, and thus nationwide, decreases in cases and subsequent revenue were -19.2%, -10.9%, -6.2%, -10.9%, and -28.3% for months January through May respectively (Fig. 3 ). This translated into decreased national hospital volume of 33,868.5, 37,364.9, 39,341.9, 37,367.9, and 30,074.5 respectively (Table 3). Similarly, the reduced hospital revenue were 2.4, 2.7, 2.8, 2.7, and 2.1 billion dollars, respectively. The Gompertz function modeled recovery from May and June and found a growth coefficient of 0.125. From January through June, when full recovery occurred, lost hospital volume and revenue increased, reaching a maximum of 35,705 cases and 2.55 billion dollars in hospital revenue (Fig. 4 ).
Figure 3.
Case Volume Plot. Case volume is plotted from January to June 2020. Decreased volume (red diamonds) and expected (green circles) are shown for each month. The expected values are projections from the NIS data and the decreased volume is the institutional experience applied to the projected case values. The Gompertz recovery function (solid green) was modeled between the May and June data points. (Color version of figure is available online at http://www.semthorcardiovascsurg.com.)
Figure 4.
Cumulative Lost Cases and Revenue. Lost surgical cases (blue bars) and hospital revenue (orange circles) are plotted to summarize the current and all preceding months. (Color version of figure is available online at http://www.semthorcardiovascsurg.com.)
It is important to place these results in the context of other findings, such as a recent survey which places the overall decrease in cardiac surgery volume to between 45%15 and 47%16 of pre-COVID levels, potentially resulting in 125 thousand lost cases totaling 8.9 billion in lost hospital revenue.
DISCUSSION
In this manuscript, we used our institutional data in conjunction with the National Inpatient Sample database to estimate the effect of COVID-19 on cardiac surgery cases and hospital revenue in the United States. There are 3 main findings of this paper: (1) the overall NIS projections show a steady cardiac surgery volume over time without dramatic increases or decreases in volume along with stable hospital revenue, (2) a significant estimated amount of national hospital revenue was lost due to COVID-19, and (3) recovery from the effects of the pandemic was rapid at a single institution. However, despite the rapid recovery, the case and charge loss's full effect will take time to realize.
The relatively unchanged volume of national cardiac surgery cases from 2004-2017 is in slight disagreement with the Society of Thoracic Surgeon's (STS) 2018 report, which reported an overall increase in procedure volume from 2006 to 2014.17 This can be explained by the difference in data acquisition and sampling. The NIS contains hospital-level data on discharge with a 20% sampling. The STS Adult Cardiac Database comprises surgeon-level data, is independent of the hospital, and does not subsample. Moreover, through CCS codes, the included procedures may be broader than the subsets reported by the STS. Finally, some of the less standard procedures such as intracardiac masses, isolated MAZE, hybrid procedures, ECMO were likely not accounted for in this analysis.
After adjusting for inflation rates, national hospital revenue was relatively unchanged over the study period. Two main factors of national hospital revenue for procedures are postoperative complications as well as the use of new technology. While operative complications have been implicated in increasing revenue of hospital stay,18 , 19 their incidence has been low and without an increase for frequently performed operations in this period,17 , 20 which would result in decreased revenue. On the other end of the spectrum, cardiac surgery is intimately connected with technology, readily adopting advances in devices. These advancements, however, typically carry an increased cost.21 , 22 Yet, this increased cost may be upfront and not indicative of complications, as some studies show that transcatheter aortic valve patients have a shorter length of stay compared with surgical aortic valve patients.23 This is of relevance given the recent surge in endovascular devices to treat aortic stenosis and aortic dissection. All these competing factors obfuscate what an expected trend of hospital revenue would look like. A final variable that significantly affects revenue prediction is hospital variability in charges and revenue,24 , 25 which can cause biases in a subsampled dataset. Nevertheless, the national estimated lost revenue is substantial, and it is promising that cardiac surgery volume was able to recover quickly.
The Gompertz function is used to model growth in numerous situations, including tumor growth, virus spreading, recovery, and can be applied to hospital volume.26, 27, 28, 29 Recovery at our institution occurred over a month, with 99% of maximal capacity being estimated at 23 days. This is in stark contrast to a study done by Jain et al., which used Gompertz functions to estimate the recovery time in elective orthopedic surgery.28 They did not benefit from a known end point for recovery and opted for Monte Carlo simulations over 3 model growth rates, resulting in estimated recovery times between 7 and 16 months. There are 2 key points to address to put this finding in the proper context. First, there is a substantial difference in estimated pre-COVID case numbers, 170,000 and 41,000 monthly cases for elective orthopedic and all cardiac surgery, respectively. Secondly, cardiac surgery patients likely have increased comorbidities than an elective orthopedic population, necessitating a more immediate intervention and differing rates of elective, urgent, and emergent procedures. This difference in the nature of the cases is easily understood when comparing the lowest hospital volumes of 3% in orthopedic surgical patients and 71.7% for the cardiac surgery cohort. The higher projected volume with a larger percentage of lost cases in orthopedic surgery leads to the longer recovery time seen in the elective orthopedic cohort. This illustrates how COVID-19 can disproportionately affect surgical specialties and is a crucial consideration for departments and hospitals developing response plans and projecting future productivity. While cardiac surgery did not have as severe a reduction in volume as others,28 , 30 , 31 the lost potential revenue was substantial, amassing an estimated greater than 2 billion dollars in lost hospital revenue.
The estimates provided here can be considered conservative. While the lowest volume seen at our institution was 72.7% of pre-COVID levels, this level of decrease may not apply to all hospitals. In fact, recent national estimates have placed the overall decrease in cardiac surgery volume to between 45%15 and 47%16 of pre-COVID levels. The reason for this discrepancy is that COVID infection cases differed dramatically between states. As COVID and hospital policy was enacted on a state and hospital levels, differences in COVID volume (both duration and magnitude) would likely affect hospital surgical volume, leading to inter-hospital variability. Indeed, a recent study by Ad et al.15 showed an extensive range of decreases in cardiac surgical volumes between regions of the US. Using the national-level estimates from these publications, we can generate ranges of volume and revenue loss. Despite the differing degrees of decreased volume, our institutional trends mirror what was seen in cardiac surgery centers, with an increasing proportion of CABG procedures15 and an increased length of stay.32 However, it is likely that the COVID burden in our cardiac surgery population was minimal given the similar 30-day mortality compared to the previous year, and the lower 30-day mortality compared to other centers.15 , 33 Using the most significant national decrease15 in cardiac surgery case volume (45%), the range of lost hospital cases is 37,505–125,000, with an accompanying hospital revenue loss of 2.55–8.9 billion.
Limitations
The most significant limitation in this study is the use of a single center extrapolated to the nation. While this institution's experience is of a large volume academic center, there could be differences between such centers, their proportion of elective and urgent/emergent cases, and their changes in volumes throughout, thus biasing our results. This is of particular importance as the COVID-19 policy was enacted on a state-by-state basis. Moreover, different institutions could have different recovery dynamics that my not be governed by the Gompertz growth function used or by a generalized Gompertz growth function at all. This would result in biases for the lost cases and revenue during the recovery period. This is also likely true in that our relatively unchanged elective surgery volume was not typical of the national trend, which would make the estimates presented here conservative in nature. Additionally, we did not have access to our institutional change in costs which can bias the results. The second limitation is that the reduction in surgery was assumed to be proportional among all procedures. It is possible that some cases were affected more than others, which could influence the actual reduction in charges and revenue as different cardiac surgery operations will have differing associated economic burdens. Additionally, there are inherent limitations in using the NIS database and CCS coding, which may not capture the complete volume or heterogeneity in cardiac surgery volume as well as the fact that the data was projected to make estimates for expected 2020 volume, potentially adding bias. Another point to emphasize is the difference in volume trends from the NIS and the national STS data, with the STS data showing a larger increase. This would further make these estimates conservative. Lastly, clinical classification software may not capture the full spectrum of cardiac surgery.
CONCLUSION
Using our institutional cardiac surgery case volume in parallel with a nationwide database, we estimated the cardiac surgical case volume and hospital charge loss associated with the COVID-19 pandemic. There was a significant estimated reduction in national case volume, national loss of hospital revenue, and the cumulative backlog of patients. However, there was an expedient return to baseline case volume at our institution which could extend to other institutions. Despite the rapid recovery, the question remains as to how to address this backlog of patients. While a subset has pathology that allows them to await intervention safely, others may transition from an elective situation to an urgent one, likely carrying increased morbidity and mortality along with an increased cost to the hospital system. It will be up to hospital leadership to develop plans to develop strategies to address this backlog and react to any future loss in case volume.
Webcast
To view the Webcast of this AATS 101st Annual Meeting presentation see the URL below: Webcast URL: https://aats.blob.core.windows.net/media/21%20AM/AM21_A17/AM21_A17_01.mp4.
Footnotes
Read at the AATS 101st Annual Meeting: A Virtual Learning Experience, April 30-May 2, 2021.
IS receives institutional research funding from Atricure and Medtronic and consults for Medtronic Vascular. These conflicts are unrelated to this project.
Conference: Oral Presentation, AATS 2021.
Classifications: Procedural volume, COVID 19, hospital revenue.
Funding: No funding was received for this study.
Conflicts of Interest: The authors report no conflict of interest pertaining to this work.
REFERENCES
- 1.Pawar M. The global impact of and responses to the COVID-19 pandemic. Int J Commun Soc Devel. 2020;2:111–120. [Google Scholar]
- 2.Poudel K, Subedi P. Impact of COVID-19 pandemic on socioeconomic and mental health aspects in Nepal. Int J Soc Psychiatry. 2020;66:748–755. doi: 10.1177/0020764020942247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nicola M, Alsafi Z, Sohrabi C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diaz A, Sarac BA, Schoenbrunner AR, et al. Elective surgery in the time of COVID-19. Am J Surg. 2020;219:900–902. doi: 10.1016/j.amjsurg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American College of Surgeons. COVID-19: guidance for triage of non-emergent surgical procedures. 2020
- 6.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: Early experience and forecast during an emergency response. JAMA. 2020;323:1545–1546. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 7.Lauren Leatherby JK, Tompkins Lucy, Smart Charlie, et al. The New York Times; 2020. 'There's No Place for Them to Go': I.C.U. Beds Near Capacity Across U.S.https://www.nytimes.com/interactive/2020/12/09/us/covid-hospitals-icu-capacity.html [Google Scholar]
- 8.Sultan I, Habertheuer A, Usman AA, et al. The role of extracorporeal life support for patients with COVID-19: Preliminary results from a statewide experience. J Card Surg. 2020;35:1410–1413. doi: 10.1111/jocs.14583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Hospital Association; 2020. Hospitals and Health Systems Face Unprecedented Financial Pressures Due to COVID-19.https://www.aha.org/system/files/media/file/2020/05/aha-covid19-financial-impact-0520-FINAL.pdf [Google Scholar]
- 10.Resnick AS, Corrigan D, Mullen JL, et al. Surgeon contribution to hospital bottom line: Not all are created equal. Ann Surg. 2005;242:530–539. doi: 10.1097/01.sla.0000184693.61680.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.2019 physician inpatient/outpatient revenue survey 2019
- 12.Coyan GN, Aranda-Michel E, Kilic A, et al. The impact of COVID-19 on thoracic surgery residency programs in the US: A program director survey. J Card Surg. 2020;35:3443–3448. doi: 10.1111/jocs.14954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seese L, Aranda-Michel E, Sultan I, et al. Programmatic responses to the coronavirus pandemic: A survey of 502 cardiac surgeons. Ann Thorac Surg. 2020;110:761–763. doi: 10.1016/j.athoracsur.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dunn A, Grosse SD, Zuvekas SH. Adjusting health expenditures for inflation: A review of measures for health services research in the United States. Health Serv Res. 2018;53:175–196. doi: 10.1111/1475-6773.12612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ad N, Luc JGY, Nguyen TC. COVID-19 North American Cardiac Surgery Survey Working Group. Cardiac surgery in North America and coronavirus disease 2019 (COVID-19): Regional variability in burden and impact. J Thorac Cardiovasc Surg. 2021;162(3):893–903.e4. doi: 10.1016/j.jtcvs.2020.06.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen TC, Thourani VH, Nissen AP, et al. The Effect of COVID-19 on Adult Cardiac Surgery in the United States in 717 103 Patients. Ann Thorac Surg. 2022;113(3):738–746. doi: 10.1016/j.athoracsur.2021.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.D'Agostino RS, Jacobs JP, Badhwar V, et al. The society of thoracic surgeons adult cardiac surgery database: 2018 update on outcomes and quality. Ann Thorac Surg. 2018;105:15–23. doi: 10.1016/j.athoracsur.2017.10.035. [DOI] [PubMed] [Google Scholar]
- 18.Stevens M, Shenoy AV, Munson SH, et al. Healthcare utilization and costs of cardiopulmonary complications following cardiac surgery in the United States. PLoS One. 2019;14 doi: 10.1371/journal.pone.0226750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Osnabrugge RL, Speir AM, Head SJ, et al. Prediction of costs and length of stay in coronary artery bypass grafting. Ann Thorac Surg. 2014;98:1286–1293. doi: 10.1016/j.athoracsur.2014.05.073. [DOI] [PubMed] [Google Scholar]
- 20.ElBardissi AW, Aranki SF, Sheng S, et al. Trends in isolated coronary artery bypass grafting: An analysis of the society of thoracic surgeons adult cardiac surgery database. J Thorac Cardiovasc Surg. 2012;143:273–281. doi: 10.1016/j.jtcvs.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 21.Reynolds MR, Lei Y, Wang K, et al. Cost-effectiveness of transcatheter aortic valve replacement with a self-expanding prosthesis versus surgical aortic valve replacement. J Am Coll Cardiol. 2016;67:29–38. doi: 10.1016/j.jacc.2015.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McClure RS, Brogly SB, Lajkosz K, et al. Economic burden and healthcare resource use for thoracic aortic dissections and thoracic aortic aneurysms—A population‐based cost‐of‐illness analysis. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.119.014981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Virtanen MPO, Eskola M, Jalava MP, et al. Comparison of outcomes after transcatheter aortic valve replacement vs surgical aortic valve replacement among patients with aortic stenosis at low operative risk. JAMA Netwk Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.5742. -e195742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kilic A, Shah AS, Conte JV, et al. Understanding variability in hospital-specific costs of coronary artery bypass grafting represents an opportunity for standardizing care and improving resource use. J Thorac Cardiovasc Surg. 2014;147:109–116. doi: 10.1016/j.jtcvs.2013.08.024. [DOI] [PubMed] [Google Scholar]
- 25.AFM Alan T.Marty, Danielson Ross, O'Reilly Richard. The variation in hospital charges: A problem in determining cost/benefit for cardiac surgery. Ann Thorac Surg. 1977 doi: 10.1016/s0003-4975(10)63433-9. [DOI] [PubMed] [Google Scholar]
- 26.Vaghi C, Rodallec A, Fanciullino R, et al. Population modeling of tumor growth curves and the reduced Gompertz model improve prediction of the age of experimental tumors. PLoS Computat Biol. 2020;16 doi: 10.1371/journal.pcbi.1007178. -e1007178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Diaz Perez FJ, Chinarro D, Otin RP, et al. Comparison of growth patterns of COVID-19 cases through the ARIMA and Gompertz models. Case studies: Austria, Switzerland, and Israel. Rambam Maimonides Med J. 2020;11:e0022. doi: 10.5041/RMMJ.10413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jain A, Jain P, Aggarwal S. SARS-CoV-2 impact on elective orthopaedic surgery: Implications for post-pandemic recovery. J Bone Joint Surg. 2020;102:e68. doi: 10.2106/JBJS.20.00602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tjørve KMC, Tjørve E. The use of Gompertz models in growth analyses, and new Gompertz-model approach: An addition to the Unified-Richards family. PLoS One. 2017;12 doi: 10.1371/journal.pone.0178691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Analysis: Ophthalmology lost more patient volume due to COVID-19 than any other specialty: Strata decision technology; 2020
- 31.Healthcare professionals and the impact of COVID-19. A comparative study of revenue and utilization: FAIR health; 2020
- 32.Sanders J, Akowuah E, Cooper J, et al. Cardiac surgery outcome during the COVID-19 pandemic: A retrospective review of the early experience in nine UK centres. J Cardiothorac Surg. 2021;16:43. doi: 10.1186/s13019-021-01424-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: An international cohort study. Lancet. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]