Abstract
Five medications are approved by the US Food and Drug Administration for chronic weight management, yet less than 2% of adults with obesity use these medications. The purpose of this study was to identify reasons nurse practitioners are reluctant to prescribe obesity pharmacotherapy. This was a cross-sectional study of a U.S. sample of nurse practitioners. Questionnaires were administered online that evaluated practice patterns and attitudes concerning obesity pharmacotherapy. The survey was completed by 74 nurse practitioners, and of those 17.6% prescribed obesity pharmacotherapy and 82.4% did not. Nurse practitioners who did and did not prescribe obesity pharmacotherapy had similar scores on weight bias. Nurse practitioners who did not prescribe obesity pharmacotherapy, compared to those who did, more often reported that patients do not ask for obesity pharmacotherapy (p=0.01), patients did not want to use pharmacotherapy (p=0.02), and that they were not familiar with obesity medications (p=0.02). While this survey was limited by a low response, we found many beliefs, opinions, and attitudes toward adults with obesity did not differ between groups. However, nurse practitioners who did not prescribe obesity pharmacotherapy, compared to those who did, identified more barriers related to the lack of obesity pharmacotherapy awareness and education.
Keywords: nurse practitioner, obesity, pharmacotherapy, weight loss
Introduction
Obesity, defined as a body mass index (BMI) ≥ 30 kg/m2, is a serious public health threat. The prevalence of obesity in U.S. adults is 42.4% (Hales et al., 2020). Obesity increases the risk of a myriad of conditions such as type 2 diabetes, hypertension, cardiovascular disease, and depression (Abdullah et al., 2011; Kannel et al., 1967; Roberts et al., 2003). Weight loss can help to improve and even ameliorate obesity-related conditions (Knowler et al., 2002; Look AHEAD Research Group, 2013, 2014; Wing et al., 2011).
Types of obesity treatment available include lifestyle modification, dietary intervention, pharmacotherapy, and metabolic/bariatric surgery. Guidelines recommend that these treatments are provided in a stepwise approach based on increasing BMI as well as obesity-related comorbidities (Apovian et al., 2015; Jensen et al., 2014). For individuals with a BMI ≥ 25 kg/m2, lifestyle intervention is recommended. For patients with a BMI ≥ 30 kg/m2 or ≥ 27 kg/m2 with obesity-related comorbidities, pharmacotherapy as an adjunct to lifestyle intervention can be considered. Individuals who have a BMI ≥ 35 kg/m2 with an obesity-related comorbidity or BMI ≥ 40 kg/m2 may be referred for metabolic/bariatric surgery. Weight loss causes physiological changes in energy balance, appetite, and satiety that encourage weight regain to the body’s original body weight “set-point” (Sumithran et al., 2011). Pharmacotherapy can help to combat some of the internal, physiological perturbations associated with obesity.
A combination of lifestyle modification and pharmacotherapy can help patients lose weight and keep it off. The US Food and Drug Administration (FDA) has approved five medications for chronic weight management: orlistat, phentermine/topiramate, naltrexone/bupropion, liraglutide, and semaglutide. Weight loss medications result in 5–10% of original weight loss and can improve hunger, cravings, and other measures of appetite (Chao et al., 2019; Khera et al., 2016). Unfortunately, the adoption and utilization of these medications by healthcare providers are low. Fewer than 2% of adults with obesity are offered and fill a prescription for one of these medications (Thomas et al., 2016). The low prescription of obesity pharmacotherapy creates a therapeutic gap in obesity treatment. There is a population of patients who are “stuck” in-between lifestyle modification therapy and metabolic/bariatric surgery. Paradoxically, obesity pharmacotherapies are under prescribed relative to hypertension and diabetes, which are some of the most common comorbidities associated with obesity (Petrin et al., 2016). For example, 86% of those with type 2 diabetes mellitus are prescribed medication (Thomas et al., 2016).
Little is known about why healthcare providers are reluctant to prescribe these medications. Some healthcare providers may have negative attitudes and stereotypes about people with obesity (Phelan et al., 2015). Research shows that such attitudes influence perceptions, judgment, interpersonal behavior, decision-making, and the care they provide patients (Phelan et al., 2015). Weight stigma may influence a providers’ willingness to prescribe obesity pharmacotherapy. However, this relationship has not been well explored. Additional barriers may include high costs, lack of insurance coverage, time, safety concerns, and knowledge (Elangovan et al., 2021; Fujioka & Harris, 2020; Granara & Laurent, 2017). For example, Medicare does not cover obesity pharmacotherapies. Liraglutide 3.0 mg is covered by 57% of commercial insurances and 62% of state Medicaid plans (Fujioka & Harris, 2020).
The purpose of this exploratory study was to evaluate provider-level factors that may be associated with prescribing weight loss medications for patients with obesity. Our first aim was to examine the relationship between weight bias and prescription of obesity pharmacotherapy by nurse practitioners. We hypothesized that providers who prescribed pharmacotherapy would have lower implicit and explicit weight stigma than those who did not prescribe obesity pharmacotherapy. Our second aim was to evaluate if providers’ views of the causal attributions of obesity are associated with the likelihood of prescribing weight management pharmacotherapy. Since there is a common public perception that obesity is a matter of will power and an issue of “personal responsibility”, rather than a chronic disease (Hilbert et al., 2008), we hypothesized that providers who view obesity as a biologically-based disease will be more willing to prescribe pharmacotherapy compared to those who do not. Lastly, we examined whether perceived barriers to using obesity pharmacotherapy medication were associated with a greater likelihood of prescribing obesity pharmacotherapy.
Methods
We used a cross-sectional design to gather information from a nationwide sample of adult nurse practitioners using emailed surveys.
Participants
The target population was practicing adult or family nurse practitioners in the US who were most likely to be involved with the care of adults with obesity. The major inclusion criteria were adult or family nurse practitioners practicing in the US that provide care to individuals ≥18 years of age. The major exclusion criteria were those not currently practicing or those with an inactive license. Nurse practitioners were selected using a random sample of nurse practitioners from state registries and nursing boards in each state which was available through a paid, commercial vendor that also delivered messages to recipients via email. The participants were pulled from all geographic locations across the nation. To compensate for the lower than anticipated responses we initially received via these emails, we supplemented recruitment using a multimodal strategy of online advertisements circulated by various nurse practitioner groups across the United States, as well as through emails sent to alumni networks.
Procedures
Procedures were based on Dillman’s tailored design method and guidelines to maximize response rates (Dillman et al., 2014). Questionnaires were self-administered online. Advertisements and emails requested nurse practitioners to complete a brief online survey about obesity treatment and they were provided a link to the survey. The survey initially asked participants to fill out a consent form, and agreeable participants were then prompted with screening questions, and the survey measures described below. Participants who completed the survey were given the option to provide an email address to receive an Amazon gift card to compensate them for their time.
Measures
Questionnaires took approximately 15 minutes to complete.
Demographic, clinical, and practice information.
Demographic and clinical information collected from participants included age, gender, race/ethnicity, weight, height, weight loss history, and healthcare practice type (i.e., solo private practice; group private practice; hospital/medical center; public clinic/community health center; university health system; practice network/HMO; or other).
Training in obesity.
We asked about prior training in the assessment and diagnosis of obesity and how prevalent respondents believed obesity was in their clinic. We also asked whether providers had training in obesity pharmacotherapy (e.g., formal lectures, CEUs).
Practices concerning obesity pharmacotherapy.
Participants were asked about their clinical practices regarding behavioral and pharmacological treatment for obesity. Whether providers did or did not prescribe obesity pharmacotherapy was assessed through the question ‘What is typically your minimum requirement for prescribing drug therapy for obesity treatment”(Petrin et al., 2016). Responses included: ‘I do not prescribe drug therapy for obesity’; ‘BMI greater ≥ 30 kg/m2 with a comorbid condition’; ‘BMI ≥ 30 kg/m2; BMI ≥ 35 kg/m2 with a comorbid condition’; ‘BMI ≥ 35 kg/m2; BMI ≥ 40 kg/m2.”
Causal Attributions for Obesity.
Participants completed the Causal Attributions for Obesity (CAO) scale (Pearl et al., 2018). The scale asked participants to rate (from 1–7) the extent to which obesity is caused by 16 potential factors. Items were divided into four factors: Biology/Brain (genetic factors; metabolic defect; endocrine/hormonal disorder; addictive properties of food; and psychological problems); Behavior (eating the wrong foods and not enough physical activity); Environment (poor nutritional knowledge; limited access to healthy food; marketing of unhealthy foods; and low income); and Personal Responsibility (weakness of character; lack of willpower; and laziness).
Stigmatizing Attitudes Toward Obesity.
To assess stigmatizing attitudes toward obesity, we used the Nurses’ Attitudes Toward Obesity and Obese Patients Scale (Watson et al., 2008). The Nurses’ Attitudes Towards Obesity and Obese Patients Scale is a 36-item instrument that measures attitudes toward adults with obesity. Items were framed on a 100-mm visual analog scale with a horizontal line with anchors ranging from “seldom” to “often” or “agree” to “disagree,” depending on the item stem. Most items were phrased so that a higher score indicated a more negative attitude. However, to avoid response bias, five items were phrased in the opposite direction and reverse scored for analysis. This measure was selected because it is one of the most reliable and valid scales that has been used to assess healthcare provider’s perceptions of obesity (Lacroix et al., 2017). Factors include response to patients with obesity; characteristics of individuals with obesity; controllable factors contributing to obesity; stereotypic characteristics of patients with obesity; supportive roles in caring for patients with obesity. The Beliefs About Obese Persons Scale, was used to measure explicit beliefs regarding the controllability of obesity (Allison et al., 1991). Each item asked respondents to indicate the extent to which they agreed or disagreed with a specific statement about the controllability of obesity. Each of the 8 items was scored on a 6-point Likert scale; thus, the total score ranges from 0 to 48. Higher scores indicated fewer negative beliefs about obesity.
Barriers.
We assessed barriers including perceived effectiveness of the medications, adverse events, medication interactions, cost, insurance coverage, patient motivation, insufficient knowledge about available medication options and guidelines, training and skills related to overall obesity management, and time.
Statistical Analysis
Data were assessed for missing data and out-of-range values with basic statistical procedures such as univariate statistics (i.e., means, standard deviations, ranges, frequencies, proportions, percentiles) and graphs, such as histograms, box and whisker plots, and scatter plots. Due to small cell sizes, healthcare practice types were merged into 2 groups: 1) individual/group private practice or hospital/medical center and university health system versus 2) public clinic/community health center and other for statistical comparison. The primary analysis was a comparison in the Nurses’ Attitudes Toward Obesity and Obese Patients Scale and Beliefs about Obese Persons Scale between participants who were likely to prescribe obesity pharmacotherapy and those who were not. This was analyzed using independent sample t-tests. Similar analyses were conducted for secondary aims.
Results
A total of 74 nurse practitioners completed the survey, and of those 17.6% prescribed obesity pharmacotherapy and 82.4% did not. Nurse practitioners who did and did not prescribe pharmacotherapy did not differ significantly by age, sex, race/ethnicity, weight, BMI, history of obesity, history of participation in a weight loss program, or practice type (ps>0.05; Table 1).
Table 1.
Comparison of participant characteristics, weight bias, and attitudes towards patients with obesity between nurse practitioners who do and do not prescribe obesity pharmacotherapy
| Prescribes obesity pharmacotherapy | Did not prescribe obesity pharmacotherapy | P-Value | |
|---|---|---|---|
| N (%) | 13 (17.6) | 61 (82.4) | N/A |
| Age, years | 48.0 (13.7) | 52.3 (11.2) | 0.25 |
| Sex, females | 13 (100) | 56 (91.8) | 0.58 |
| Race/ethnicitya | 0.86 | ||
| Asian | 1 (7.7) | 2 (3.3) | |
| Black | 1 (7.7) | 4 (6.6) | |
| White | 11 (84.6) | 53 (86.9) | |
| Multiracial | 0 (0) | 1 (1.6) | |
| Practice type | 0.43b | ||
| Solo/group private practice | 8 (61.5) | 17 (27.9) | |
| Hospital/medical center | 0 (0) | 25 (41.0) | |
| Public clinic/community health center | 2 (15.4) | 2 (3.3) | |
| University health system | 1 (7.7) | 9 (14.7) | |
| Practice network/HMO | 1 (7.7) | 1 (1.6) | |
| Other | 1 (7.7) | 7 (11.5) | |
| Weight, lbs | 149.8 (27.0) | 166.2 (45.9) | 0.22 |
| BMI | 25.5 (5.0) | 27.7 (7.2) | 0.29 |
| History of obesity | 5 (38.5) | 23 (37.7) | >0.99 |
| History of participation in weight loss program | 6 (46.2) | 33 (54.1) | 0.76 |
| Casual attributions of obesity | |||
| Biology/Brain | 4.9 (0.8) | 4.7 (0.9) | 0.55 |
| Behavior | 5.2 (0.8) | 5.2 (1.0) | 0.98 |
| Environment | 5.2 (0.7) | 5.1 (0.9) | 0.76 |
| Personal Responsibility | 3.2 (1.8) | 2.5 (1.4) | 0.15 |
| Beliefs about obese person scale | 32.7 (5.6) | 32.2 (3.8) | 0.70 |
| Attitudes towards patients with obesity | |||
| Response to patients with obesity | 420.4 (358.8) | 373.7 (198.5) | 0.70 |
| Characteristics of individuals with obesity | 460.0 (108.9) | 543.6 (85.6) | 0.07 |
| Controllable factors contributing to obesity | 392.1 (85.6) | 445.3 (95.4) | 0.11 |
| Stereotypic characteristics of people with obesity | 41.1 (52.8) | 34.6 (35.9) | 0.73 |
| Supportive roles in caring for patients with obesity | 146.5 (50.4) | 149.4 (41.6) | 0.85 |
Note.
N=1 person did not report race/ethnicity.
Due to small cell sizes, statistical comparison was performed as 1) solo/group private practice, hospital/medical center, university health system, practice network/HMO versus 2) public clinic/community health center and other.
Participants who did and did not prescribe obesity pharmacotherapy had similar scores on causal beliefs about obesity related to biological, behavioral, environmental, and personal factors (Table 1). The groups did not differ significantly in beliefs about the controllability of obesity. In addition, nurse practitioners who did and did not prescribe obesity pharmacotherapy had similar ratings in stigmatizing attitudes toward obesity (Table 1).
There were significant differences in reported barriers between nurse practitioners who did and did not prescribe pharmacotherapy (Figure 1). Nurse practitioners who did not prescribe pharmacotherapy, compared to those who did, reported that patients do not ask for obesity pharmacotherapy (p=0.01), patients did not want to use pharmacotherapy (p=0.02), and that they were not familiar with obesity medications (p=0.02).
Figure 1.
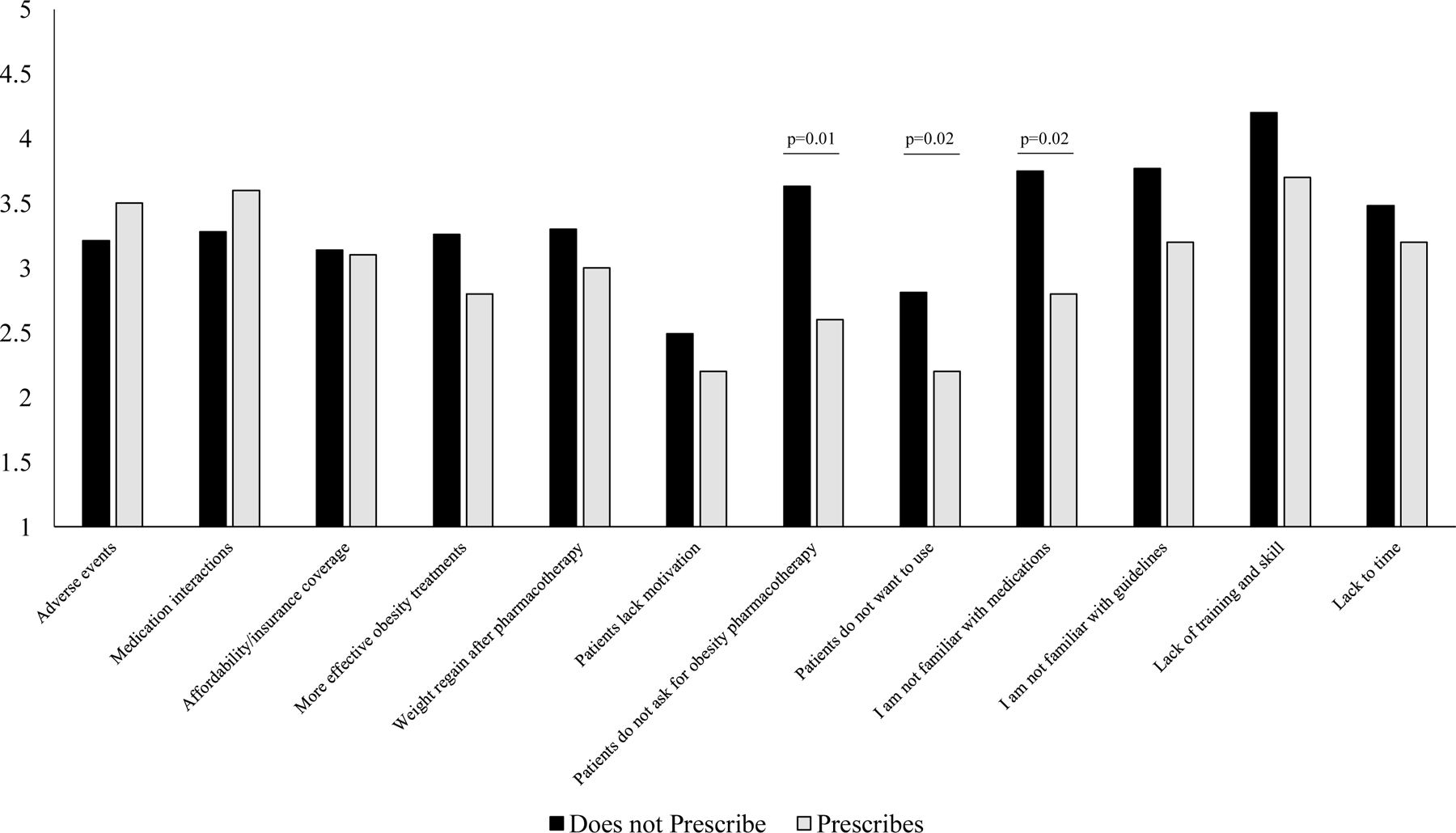
Barriers to Prescribing Obesity Pharmacotherapy. Scores range from 1 (strongly disagree) to 5 (strongly agree).
Discussion
In a nationwide survey, nurse practitioners who provided obesity pharmacotherapy, compared to those who did not, had similar beliefs, opinions, and attitudes towards people with obesity. However, important differences in perceived barriers were identified. Nurse practitioners who did not prescribe obesity pharmacotherapy, compared to those who did, perceived that there were higher barriers related to patients not asking for or wanting to use obesity pharmacotherapy, and that the providers were not familiar with obesity medications. There barriers are consistent with prior research findings (Fujioka & Harris, 2020; Simon & Lahiri, 2018). This highlights the need for greater awareness and education about obesity pharmacotherapy. However, results should be interpreted cautiously due to the low survey response.
The results of this study make a novel contribution by suggesting that the main cause of low obesity pharmacotherapy prescribing patterns among nurse practitioners is less about explicit stigmatizing attitudes toward obesity, and more about difficulty with perceived barriers related to patients wanting to use these medications and provider familiarity with the medications. Contrary to our hypothesis, the two prescribing groups did not differ in the degree to weight stigma nor causal attributions of obesity. Unlike previous studies that found that providers that do and do not prescribe obesity pharmacotherapy differ in their stigmatizing attitudes towards obesity, we found that they do not (Phelan et al., 2015; Schwartz et al., 2003). The current study focused on explicit attitudes, and it may be possible that implicit weight bias attitudes may have differed. We did find variability between participants who did and did not prescribe obesity pharmacotherapy when assessing barriers. This suggests that clinical training and education on obesity pharmacotherapy options are needed to improve prescribing rates among nurse practitioners. Ultimately, better and more inclusive insurance coverage of obesity medications will be needed to expand the use of this treatment to patients.
This study has several limitations including the low survey response. This survey was initially disseminated via email to 5000 nurse practitioners nationwide. After receiving a low response rate, we changed our sampling procedure to include convenience sampling in which we sent emails to colleagues and alumni, as well as posted in Facebook and LinkedIn groups. This may contribute to non-response bias. Another limitation is that the cost of medications also plays a role in the perception of pharmacotherapy and availability to patients and was not well explored in the current study. Type of practice also may be an important factor related to prescription, but we did not have adequate power to assess this factor. For example, nurse practitioners in specialty practices may defer obesity medications to the primary care provider.
In conclusion, we did not find that weight bias or causal attributions for obesity were associated with obesity pharmacotherapy prescribing practices. However, nurse practitioners who did not prescribe obesity pharmacotherapy reported unfamiliarity with these medications. Educational programs will need to be developed so nurse practitioners can learn more about this valuable treatment option. Once these factors are addressed, obesity pharmacotherapy may more widely be prescribed for weight loss, which could have a significant effect on rates of obesity and related conditions.
Acknowledgments
Funding: This study was funded by the University of Pennsylvania, School of Nursing Student Grant Award. AMC was supported, in part, by the National Institute of Nursing Research of the National Institutes of Health under Award Number K23NR017209.
Footnotes
Conflicts of interest: AMC reports grants from Eli Lilly and Company and WW International, Inc., outside the submitted work. The other author declares no conflicts of interest.
References
- Abdullah A, Stoelwinder J, Shortreed S, Wolfe R, Stevenson C, Walls H, de Courten M, & Peeters A (2011). The duration of obesity and the risk of type 2 diabetes. Public Health Nutrition, 14(1), 119–126. [DOI] [PubMed] [Google Scholar]
- Allison DB, Basile VC, & Yuker HE (1991). The measurement of attitudes toward and beliefs about obese persons. International Journal of Eating Disorders, 10(5), 599–607. [Google Scholar]
- Apovian CM, Aronne LJ, Bessesen DH, McDonnell ME, Murad MH, Pagotto U, Ryan DH, & Still CD (2015). Pharmacological management of obesity: an Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 100(2), 342–362. [DOI] [PubMed] [Google Scholar]
- Chao AM, Wadden TA, Walsh OA, Gruber KA, Alamuddin N, Berkowitz RI, & Tronieri JS (2019). Effects of liraglutide and behavioral weight loss on food cravings, eating behaviors, and eating disorder psychopathology. Obesity, 27(12), 2005–2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillman DA, Smyth JD, & Christian LM (2014). Internet, phone, mail, and mixed-mode surveys: the tailored design method John Wiley & Sons. [Google Scholar]
- Elangovan A, Shah R, & Smith ZL (2021). Pharmacotherapy for obesity—Trends using a population level national database. Obesity Surgery, 31(3), 1105–1112. [DOI] [PubMed] [Google Scholar]
- Fujioka K, & Harris SR (2020). Barriers and solutions for prescribing obesity pharmacotherapy. Endocrin Metab Clin North Am, 49(2), 303–314. [DOI] [PubMed] [Google Scholar]
- Granara B, & Laurent J (2017). Provider attitudes and practice patterns of obesity management with pharmacotherapy. Journal of the American Association of Nurse Practitioners, 29(9), 543–550. [DOI] [PubMed] [Google Scholar]
- Hales C, Carroll M, Fryar C, & Ogden C (2020). Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief, no 360. National Center for Health Statistics: Hyattsville, MD, USA. [PubMed] [Google Scholar]
- Hilbert A, Rief W, & Braehler E (2008). Stigmatizing attitudes toward obesity in a representative population‐based sample. Obesity, 16(7), 1529–1534. [DOI] [PubMed] [Google Scholar]
- Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, Hu FB, Hubbard VS, Jakicic JM, & Kushner RF (2014). 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Journal of the American College of Cardiology, 63(25 Part B), 2985–3023. [DOI] [PubMed] [Google Scholar]
- Kannel WB, Brand N, Skinner JJJ, Dawber TR, & McNamara PM (1967). The relation of adiposity to blood pressure and development of hypertension: the Framingham study. Annals of Internal Medicine, 67(1), 48–59. [DOI] [PubMed] [Google Scholar]
- Khera R, Murad MH, Chandar AK, Dulai PS, Wang Z, Prokop LJ, Loomba R, Camilleri M, & Singh S (2016). Association of pharmacological treatments for obesity with weight loss and adverse events: a systematic review and meta-analysis. JAMA, 315(22), 2424–2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, & Nathan DM (2002). Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine, 346(6), 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacroix E, Alberga A, Russell-Mathew S, McLaren L, & von Ranson K (2017). Weight bias: A systematic review of characteristics and psychometric properties of self-report questionnaires. Obesity Facts, 10(3), 223–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Look AHEAD Research Group. (2013). Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. New England Journal of Medicine, 369(2), 145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Look AHEAD Research Group. (2014). Impact of intensive lifestyle intervention on depression and health-related quality of life in type 2 diabetes: the Look AHEAD Trial. Diabetes Care, 37(6), 1544–1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl RL, Wadden TA, Allison KC, Chao AM, Alamuddin N, Berkowitz RI, Walsh O, & Tronieri JS (2018). Causal attributions for obesity among patients seeking surgical versus behavioral/pharmacological weight loss treatment. Obesity Surgery, 28(11), 3724–3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrin C, Kahan S, Turner M, Gallagher C, & Dietz W (2016). Current practices of obesity pharmacotherapy, bariatric surgery referral and coding for counselling by healthcare professionals. Obesity Science & Practice, 2(3), 266–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, & van Ryn M (2015). Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obesity Reviews, 16(4), 319–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts RE, Deleger S, Strawbridge WJ, & Kaplan GA (2003). Prospective association between obesity and depression: evidence from the Alameda County Study. International Journal of Obesity, 27(4), 514–521. [DOI] [PubMed] [Google Scholar]
- Schwartz MB, Chambliss HON, Brownell KD, Blair SN, & Billington C (2003). Weight bias among health professionals specializing in obesity. Obesity Research, 11(9), 1033–1039. [DOI] [PubMed] [Google Scholar]
- Simon R, & Lahiri SW (2018). Provider practice habits and barriers to care in obesity management in a large multicenter health system. Endocrine Practice, 24(4), 321–328. [DOI] [PubMed] [Google Scholar]
- Sumithran P, Prendergast LA, Delbridge E, Purcell K, Shulkes A, Kriketos A, & Proietto J (2011). Long-term persistence of hormonal adaptations to weight loss. New England Journal of Medicine, 365(17), 1597–1604. [DOI] [PubMed] [Google Scholar]
- Thomas CE, Mauer EA, Shukla AP, Rathi S, & Aronne LJ (2016). Low adoption of weight loss medications: A comparison of prescribing patterns of antiobesity pharmacotherapies and SGLT 2s. Obesity, 24(9), 1955–1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson L, Oberle K, & Deutscher D (2008). Development and psychometric testing of the nurses’ attitudes toward obesity and obese patients (NATOOPS) scale. Research in Nursing and Health, 31(6), 586–593. [DOI] [PubMed] [Google Scholar]
- Wing RR, Lang W, Wadden TA, Safford M, Knowler WC, Bertoni AG, Hill JO, Brancati FL, Peters A, & Wagenknecht L (2011). Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care, 34(7), 1481–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]


