Abstract
Background:
Induction of labor (IOL) is a technique to establish vaginal delivery when the risks for continuing the pregnancy for mother or baby are higher than the risks of delivery. It is usually performed in high-risk pregnancies, but can also be beneficial in low-risk populations, as shown in the ARRIVE trial.
Objective:
To evaluate the effectiveness and safety of slow-release vaginal dinoprostone (prostaglandin E2 10 mg) for labor induction in women with low-risk pregnancies.
Methods:
A prospective study was performed at Hanoi Obstetrics and Gynecology Hospital, Vietnam. We recruited women with low-risk pregnancies from 39 weeks + 0 days to 40 weeks + 6 days of gestation and an unfavorable cervix. Women who participated received 10 mg intravaginal slow-release dinoprostone (Propess) for induction of labor. Labor, deliveries, and post-partum management were performed according to the local protocol.
Results:
From September 2020 to March 2021, 102 low-risk women were eligible to participate in the study. Among these women, 67.6% had vaginal deliveries, 6.9% had postpartum bleeding, and 3.9% experienced tachysystole. All newborns were healthy, with good APGAR scores. None of the women needed respiratory support or intensive care unit admission. All other maternal or fetal complications were explored. The rate of cesarean section was 3.8 higher in nulliparous than multiparous women and 2.2 times higher in women who did not receive epidural analgesia than in those who did. The risk of cesarean section increased if the time between labor induction and active labor was greater than 12.5 hours.
Conclusion:
Slow-release dinoprostone insert is safe and effective for the induction of labor in low-risk pregnant women. The risk of cesarean section was elevated in nulliparous patients and those who did not receive epidural analgesia during labor. As the time from labor induction to active labor increased, the risk of cesarean section increased.
Keywords: induction, labor, low-risk, dinoprostone, vaginal
1. BACKGROUND
Induction of labor (IOL) is a technique to establish vaginal delivery when the risks for continuing the pregnancy for mother or baby are higher than the risks of delivery. It is usually performed in high-risk pregnancies, but can also be beneficial in low-risk populations, as shown in the ARRIVE trial (1). Based on the ARRIVE results, the American College of Obstetricians and Gynecologists (ACOG) suggested considering labor induction at the 39th week of gestation. Since then, there has been a trend toward inducing labor before the due date. In addition, increasing numbers of pregnant women prefer to reduce the duration of pregnancy or control the delivery date. Therefore, an optimal method of labor induction for low-risk pregnancies should be identified.
The main mechanisms for cervical ripening fall into two groups: mechanical and pharmacological. A Cochrane systematic review and other recent meta-analyses have shown that cervical ripening with a balloon is probably as effective as the induction of labor with vaginal dinoprostone (2-4). However, this conclusion was based on low-to-moderate quality evidence. Many of the studies included only high-risk subjects (5-7) or mixed populations (8-9). No studies have attempted to identify the best method of labor induction in women with low-risk pregnancies or the effect of the method of labor induction in such women.
2. OBJECTIVE
Thus, we conducted this study to evaluate the effectiveness and safety of vaginal dinoprostone insert in elective labor induction in women with low-risk pregnancy at 39 weeks + 0 days to 40 weeks + 6 days of gestation.
3. MATERIAL AND METHODS
This six-month prospective study was performed from September 2020 to March 2021 at Hanoi Obstetrics and Gynecology Hospital and was approved by the Institutional Review Board (IRB) of Hanoi Obstetrics and Gynecology Hospital (IRB No 03/PS-HDDD).
Inclusion criteria
The inclusion criteria included: maternal age ≥ 18, singleton pregnancy, gestational age from 39 weeks + 0 days to 40 weeks + 6 days, cephalic presentation, intact membrane, unfavorable cervix (Bishop < 6), informed consent.
Exclusion criteria
Maternal medical illness associated with increased risk of adverse pregnancy outcome (diabetes mellitus, any hypertensive disorder, etc), abnormal placenta (significant active vaginal bleeding or placenta previa, placenta accreta, vasa previa, or abnormal amniotic fluid volume), abnormal fetus, previous C-section, planned-for C-section or contraindication to labor, cerclage or use of pessary in the current pregnancy. Also excluded were women with a history of allergy to dinoprostone and those participating in any other interventional study that would influence the management of labor at delivery or perinatal morbidity or mortality.
Study procedure
All low-risk women at 36 weeks + 0 days to 37 weeks + 0 days of gestation with a live singleton fetus in cephalic presentation, who had no contraindication to vaginal delivery and no cesarean delivery planned were given a study information sheet. Low risk was defined as having no maternal illness, no placental or amniotic disorder and no abnormal fetus. For women who conceived after assisted reproductive technology (ART), gestational age was determined by the date of embryo transfer or intrauterine insemination. For patients who conceived naturally, gestational age was determined from the menstrual history and confirmed by the fetal crown-to-rump length on ultrasound at 8 weeks + 0 days to 13 weeks + 6 days.
At 39 weeks + 0 days to 40 weeks + 6 days of gestation, these women were screened for eligibility by research doctors. After screening, they received a patient information sheet and consent form and were invited to a thorough discussion of the study with the investigators. When a patient signed an informed-consent form, she was considered to be enrolled in the study. After the eligible women signed the informed-consent form, they were followed up and treated according to local protocol.
Vaginal dinoprostone insert (Propess) was inserted by a research doctor with or without a speculum. As in the catheter procedure, fetal heart rate (FHR) was monitored 30 min before and 2 hours after placement. CTG and vaginal examination were performed every 6 hours. The vaginal system was left in place for a maximum of 24 hours. If it was expulsed in the first 12 hours and the patient had no contractions or still had an unfavorable cervix, another vaginal system was inserted and left in place for a maximum of 24 additional hours.
The patients were examined in case of extreme pain or ruptured membranes. The system was kept or removed following local protocols and according to individual indications. Labor, deliveries, and postpartum management were also conducted according to local protocols.
Study outcomes
The primary outcome was the proportion of vaginal deliveries. The secondary outcomes included maternal and neonatal complications, side effects of the vaginal dinoprostone insert, and factors associated with cesarean delivery. Standard core outcomes for labor induction studies (10) were identified and used to classify maternal and neonatal outcomes.
The maternal outcomes included vaginal delivery and vaginal delivery within 24 hours, side effects of the induction method (fever, nausea, vomiting, diarrhea, pain, etc), oxytocin augmentation, uterine tachysystole (defined as > 5 contractions in 10 minutes over 2 x 10 minutes with FHR changes and/or a contraction of > 3 minutes with FHR changes), use of epidural analgesia, time from labor induction to active labor, time from labor induction to delivery, indication for cesarean delivery, maternal postpartum hemorrhage (defined as blood loss > 500 ml at vaginal birth or > 1000 ml at cesarean birth within 24 hours after birth), uterine atony (defined as the use of ≥ 2 uterotonics other than oxytocin), manual uterine compression, other surgical interventions (eg, uterine compression with sutures, uterine artery ligation, embolization, hypogastric ligation, or balloon tamponade), maternal postpartum blood transfusion, uterine dehiscence or rupture, maternal infection (defined as fever or initiation of intravenous broad-spectrum antibiotics with clinical and subclinical evidence of infection), surgical complications (hysterectomy and/or damage to internal organs), severe maternal morbidity (intensive care admission, maternal death, or referred hospital transfer for severe morbidities such as pulmonary embolus, stroke, or cardiorespiratory arrest).
Neonatal outcomes included neonatal weight, death of the baby (intrapartum, neonatal, or perinatal), Apgar scores < 7 at 5 minutes, intensive care unit (ICU) admission, need for respiratory support (intubation, CPAP, or high-flow nasal cannula for ventilation or cardiopulmonary resuscitation within the first 72 hours), neonatal birth trauma (bone fractures, traumatic pneumothorax, facial nerve palsy, other neurologic injuries), hypoxic-ischemic encephalopathy or need for therapeutic hypothermia, meconium aspiration syndrome, neonatal infection (suspected systemic infection in a clinically ill infant with positive blood, cerebrospinal fluid, or catheterized/supra-pubic urine culture; or, in the absence of positive cultures, clinical evidence of cardiovascular collapse or an X-ray confirming infection), neonatal seizures, intracranial hemorrhage, subgaleal hematoma, subdural hematoma, subarachnoid hematoma, referred hospital transfer for severe morbidities.
Statistical analysis
Qualitative variables were represented as numbers and percentages. The Chi-square test was used to compare the rates. Quantitative variables were tested for normal distribution with skewness and kurtosis tests. With non-normally distributed variables, median and interquartile ranges were used in the descriptive statistics. The Mann–Whitney test was applied to compare the groups. Stata (version 14.0) software was used for the analysis. P values < .05 were considered statistically significant.
4. RESULTS
The baseline characteristics of the 102 patients who received vaginal dinoprostone insert for induction of labor in this study are described in Table 1. Sixty-seven (65.7%) were nulliparous. After being provided with the informed consent form, 42 pregnant women agreed to induce labor actively before the estimated due date (Table 1).
Table 1. Maternal Characteristics at Baseline. Characteristics.
| Characteristics | Total (n=102) no. (%) |
Mean (SD)/ median (interquartile range) |
|---|---|---|
| Age (years) | 27 (25 – 30) | |
| BMI | 28.3 (0.68) | |
| Parity | ||
| Nulliparous | 67 (65.7) | |
| Multiparous | 35 (34.3) | |
| Gestational age – weeks | 40.03 (0.34) | |
| 39/ – 39/ | 42 (41.2) | |
| ≥ 40/ | 60 (58.8) | |
| Bishop score before IOL | 40.03 (0.34) | |
| 3 | 25 (24.5) | |
| 4 | 47 (46.1) | |
| 5 | 30 (29.4) |
The vaginal delivery rate and maternal outcomes after induction of labor are shown in Table 2. Among the women studied, 66.6% had vaginal deliveries, and the median time between induction and delivery was 12.0 hours. After induction of labor, 92 women went into active labor with cervical dilation ≥ 4 cm. The median time to reach the active phase was 9 hours. The other 10 women underwent cesarean section before reaching the active phase because of fetal failure (3 cases), failure to progress (4 cases), or uterine tachysystole (3 cases). Among the 33 total cases of cesarean section, the most common indication was failure to progress (22 cases; 66.7%). We recorded 7 cases of postpartum hemorrhage, accounting for 6.9% of deliveries. All were in the vaginal delivery group; 5 of the cases required blood transfusion. We did not observe other maternal complications such as uterine atony, uterine dehiscence/rupture, surgical complications, infection, or severe morbidity. Fever was the only side effect of vaginal dinoprostone (6 cases; 5.9%). In all cases, the fever was mild and did not affect the fetus.
Table 2. Maternal Outcomes.
| Variables | no. (%) | Mean (SD)/median (interquartile range) |
|---|---|---|
| Vaginal delivery | 69 (67.6) | |
| Cesarean delivery | 33 (32.4) | |
| Side effects | 6 (5.9) | |
| Oxytocin augmentation | 25 (24.5) | |
| Uterine tachysystole | 4 (3.9) | |
| Epidural analgesia | 66 (64.7) | |
| Active phase | 92 (90.20) | |
| Time from induction to active labor (n=92) in hours | 9.0 (5.3 – 15.1) | |
| Time from induction to vaginal delivery (n=69) in hours | 12.0 (8.2 – 18.0) | |
| Time from induction to cesarean section (n=33) in hours | 20.7 (13.0 – 25.0) | |
| Indication for caesarean section (n=33) | ||
| Fetal distress | 7 (21.2) | |
| Failure to progress | 22 (66.7) | |
| Uterine tachysystole | 4 (12.1) | |
| Postpartum hemorrhage | 7 (6.9) | |
| Blood transfusion | 5 (4.9) | |
| Uterine atony | 0 (0.0) | |
| Uterine dehiscence/rupture | 0 (0.0) | |
| Surgical complications | 0 (0.0) | |
| Infection | 0 (0.0) | |
| Severe morbidities | 0 (0.0) |
Neonatal outcomes are shown in Table 3. The mean neonatal weight was 3208 grams, and all of the babies had good Apgar scores. There was no neonatal mortality or need for neonatal respiratory support or ICU admission in this study, nor did any other neonatal complications occur.
Table 3. Neonatal Outcomes.
| Variables | no. (%) | Mean (SD) |
|---|---|---|
| Neonatal weight (grams) | 3208.3 (255.2) | |
| < 3000 | 17 (16.7) | |
| 3000–3499 | 67 (65.7) | |
| ≥ 3500 | 18 (17.6) | |
| Death of the baby | 0 (0.0) | |
| Apgar scores < 7 at 5 min | 0 (0.0) | |
| ICU admission | 0 (0.0) | |
| Respiratory support | 0 (0.0) | |
| Neonatal complications | 0 (0.0) |
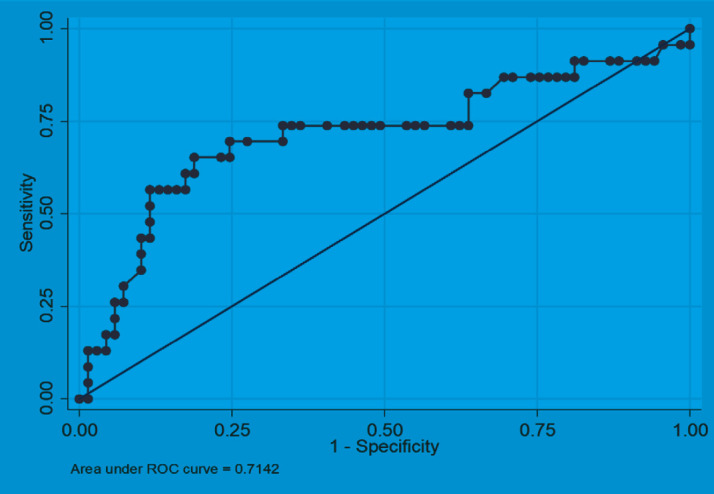
The factors related to cesarean section are shown in Table 4. Of the many factors analyzed, only 3 were associated with cesarean section: parity, epidural analgesia, and time from the induction of labor to active labor. Among them, time from the induction of labor to active labor was most likely to predict cesarean section, with an area under the curve of 0.7142, a sensitivity of 65.2%, a specificity of 81.2% and a cutoff point of 12.5 hours (Figure 1).
Table 4. Factors Associated with Cesarean Section (CS).
| Variables | Vaginal delivery | CS | p | RR (95% CI) |
|---|---|---|---|---|
| Maternal Age | 28.0 (4.8) | 27.7 (3.2) | > 0.05 | |
| Parity – n (%) | ||||
| Nulliparous | 38 (56.7) | 29 (43.3) | 0.001 | 3.8 (1.4–9.9) |
| Multiparous | 31 (88.6) | 4 (11.4) | ||
| Gestational age – n (%) | ||||
| < 40/ | 30 (71.4) | 12 (28.6) | > 0.05 | |
| ≥ 40/ | 39 (65.0) | 21 (35.0) | ||
| Bishop score | ||||
| Mean | 4.09 (0.74) | 3.97 (0.73) | > 0.05 | |
| Bishop 3 (n=25) – n (%) | 16 (64.0) | 9 (36.0) | > 0.05 | |
| Bishop 4 (n=47) – n (%) | 31 (66.0) | 16 (34.0) | ||
| Bishop 5 (n=30) – n (%) | 22 (73.3) | 8 (26.7) | ||
| Neonatal weight | ||||
| Mean | 3234.1(244.4) | 3154.6 (272.2) | > 0.05 | |
| < 3000 (n=17) | 8 (47.1) | 9 (52.9) | > 0.05 | |
| 3000–3499 (n=67) | 49 (73.1) | 18 (26.9) | ||
| ≥ 3500 (n=18) | 12 (66.7) | 6 (33.3) | ||
| Epidural analgesia – no. (%) | ||||
| No | 18 (50.0) | 18 (50.0) | 0.005 | 2.2 (1.3–3.8) |
| Yes | 51 (77.3) | 15 (22.7) | ||
| Time from induction to active labor in hours (n = 92) | 9.0 (5.2) | 14.0 (7.0) | 0.0022 |
Figure 1. Time from induction of labor to active labor predicts cesarean section.
5. DISCUSSION
Induction of labor in low-risk pregnant women has been shown to be beneficial for the neonate and mother so labor induction in this group is of increasing interest. Our study showed that vaginal dinoprostone insert was effective in inducing labor, resulting in a vaginal delivery rate of 67.6% and cesarean section rate of 32.4%. The cesarean section rate was higher than in other studies of labor induction in low-risk pregnant women (1) but lower than in the general population of pregnant women in Vietnam (11). Recently published studies showed that Vietnam has a very high cesarean section rate of 58.6% (11). There are many reasons, including medical factors relating to local protocols and social factors such as fear among pregnant women and their families (12). In the clinical and social context of Vietnam, the induction of labor in low-risk pregnant women by vaginal dinoprostone insert reduces the rate of cesarean section.
In addition, vaginal dinoprostone insert (Propess) appeared to function safely, with a low incidence of complications. The rate of oxytocin augmentation was low at 25%, similar to the rates reported in some previous studies (13,14). Only 4 women (3.92%) experienced uterine tachysystole. Other studies have reported that vaginal dinoprostone produced uterine hyperstimulation in approximately 10% of pregnant women but with no serious adverse maternal or fetal outcomes (13,15). This once again confirms that prostaglandin E2 is effective at stimulating uterine contractions. The rate of postpartum bleeding was 6.9%, and only 5 cases (4.9%) required blood transfusion. This rate is not significantly higher than the spontaneous postpartum hemorrhage rate of 5% reported by WHO (16). In a study published in the New England Journal of Medicine, the postpartum bleeding rate of the labor induction group was similar at 4.6% (1). Other maternal complications such as uterine atony, uterine dehiscence/rupture, surgical complications, infection, and severe morbidity were not noted in this study. The reported side effects of vaginal dinoprostone include fever, nausea, vomiting, and diarrhea, but we recorded only 6 cases of mild fever (5.9%) and no other side effects.
The neonatal outcomes in our study were excellent. There were no complications in any of the babies. Other labor induction studies have recorded neonatal complications such as seizures, birth trauma, meconium aspiration syndrome, and intracranial or subgaleal hemorrhages but at very low rates (1,2,4,14,15). The lack of complications that we observed was probably due to the low-risk participants, local protocols, and labor monitoring. Early cesarean section was performed as soon as problems that could affect delivery occurred. This also increased the rate of cesarean section.
We found that three factors affected the delivery method: parity, epidural analgesia, and time from induction of labor to active labor. The rate of caesarean section in multiparous women was only 11.4%. Nulliparous women had a cesarean section rate of 43.3% and were 3.8 times more likely to have a caesarean section than multiparous women. Similarly, the study of labor induction study by Obeidat (17) reported caesarean section rates of 58.7% and 17.8% in nulliparous and multiparous women, respectively, but the participants were not exclusively low-risk pregnant women. The cesarean rate of 11.2% among the multiparous women in our study and the lack of neonatal complications are promising indicators of the efficacy of vaginal dinoprostone insert in the induction of labor in low-risk multiparous women.
Pain relief during labor not only makes labor more convenient but also helps pregnant women to feel more relaxed and coordinate better with the doctor. In our study, going through labor without epidural analgesia was associated with a 2.2 times increased risk of cesarean section. Time from the induction of labor to active labor was a predictor of cesarean section, with an area under the curve of 0.7142, a sensitivity of 65.2%, and a specificity of 81.2%. We explored the cutoff point of the ROC curve, finding that the risk of cesarean section increased above a cutoff point of 12.5 (that is, when the time from the induction of labor to the active phase was more than 12.5 hours). Although there are studies that consider factors related to cesarean section after labor induction (17-19), this is the first study to report that the time from labor induction to active labor predicts cesarean section.
Our study has two main strengths. First, we studied a method of labor induction in low-risk pregnant women. Second, we collected data on the standard core outcomes reported in labor induction studies. We are also aware that our study has limitations. There was no control group, and the sample size was small. A large randomized controlled trial will be needed to identify the optimal method of labor induction in low-risk pregnant women.
6. CONCLUSION
Slow-release dinoprostone insert was effective and safe for the induction of labor in low-risk pregnant women. In our study population, the risk of cesarean section was higher in nulliparous women and women who did not have epidural analgesia during labor. As the time from labor induction to active labor increased, the risk of cesarean section increased.
Ethical Statement:
This study was approved by the Institutional Review Board (IRB) of Hanoi Obstetrics and Gynecology Hospital (IRB No 03/PS-HDDD).
Author’s Contribution:
Nguyen DA gave a substantial contribution in acquisition, analysis, and data interpretation. Tran AD and Nguyen MD prepared, drafted, and revised manuscript critically for important intellectual content. Each author gave the final approval of the version to be published and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
ICMJE Statement and Conflict of interest:
The authors declare that there is no conflict of interest
Funding Statement:
The authors received no specific funding for this work
REFERENCES
- 1.Grobman WA, Rice MM, Reddy UM, Tita ATN, Silver RM, Mallett G, Hill K, Thom EA, El-Sayed YY, Perez-Delboy A, Rouse DJ, Saade GR, Boggess KA, Chauhan SP, Iams JD, Chien EK, Casey BM, Gibbs RS, Srinivas SK, Swamy GK, Simhan HN, Macones GA Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor Induction versus Expectant Management in Low-Risk Nulliparous Women. N Engl J Med. 2018 Aug 9;379(6):513–523. doi: 10.1056/NEJMoa1800566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Du YM, Zhu LY, Cui LN, Jin BH, Ou JL. Double-balloon catheter versus prostaglandin E2 for cervical ripening and labour induction: a systematic review and meta-analysis of randomised controlled trials. BJOG. 2017 May;124(6):891–899. doi: 10.1111/1471-0528.14256. [DOI] [PubMed] [Google Scholar]
- 3.Liu YR, Pu CX, Wang XY, Wang XY. Double-balloon catheter versus dinoprostone insert for labour induction: a meta-analysis. Arch Gynecol Obstet. 2019 Jan;299(1):7–12. doi: 10.1007/s00404-018-4929-8. [DOI] [PubMed] [Google Scholar]
- 4.de Vaan MD, Ten Eikelder ML, Jozwiak M, Palmer KR, Davies-Tuck M, Bloemenkamp KW, Mol BWJ, Boulvain M. Mechanical methods for induction of labour. Cochrane Database Syst Rev. 2019 Oct 18;10(10):CD001233. doi: 10.1002/14651858.CD001233.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shechter-Maor G, Haran G, Sadeh-Mestechkin D, Ganor-Paz Y, Fejgin MD, Biron-Shental T. Intra-vaginal prostaglandin E2 versus double-balloon catheter for labor induction in term oligohydramnios. J Perinatol. 2015 Feb;35(2):95–98. doi: 10.1038/jp.2014.173. [DOI] [PubMed] [Google Scholar]
- 6.Du C, Liu Y, Liu Y, Ding H, Zhang R, Tan J. Double-balloon catheter vs. dinoprostone vaginal insert for induction of labor with an unfavorable cervix. Arch Gynecol Obstet. 2015 Jun;291(6):1221–1227. doi: 10.1007/s00404-014-3547-3. [DOI] [PubMed] [Google Scholar]
- 7.Wang W, Zheng J, Fu J, Zhang X, Ma Q, Yu S, Li M, Hou L. Which is the safer method of labor induction for oligohydramnios women? Transcervical double balloon catheter or dinoprostone vaginal insert. J Matern Fetal Neonatal Med. 2014 Nov;27(17):1805–1808. doi: 10.3109/14767058.2014.880880. [DOI] [PubMed] [Google Scholar]
- 8.Cromi A, Ghezzi F, Uccella S, Agosti M, Serati M, Marchitelli G, Bolis P. A randomized trial of preinduction cervical ripening: dinoprostone vaginal insert versus double-balloon catheter. Am J Obstet Gynecol. 2012 Aug;207(2):125.e1–7. doi: 10.1016/j.ajog.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 9.Suffecool K, Rosenn BM, Kam S, Mushi J, Foroutan J, Herrera K. Labor induction in nulliparous women with an unfavorable cervix: double balloon catheter versus dinoprostone. J Perinat Med. 2014 Mar;42(2):213–218. doi: 10.1515/jpm-2013-0152. [DOI] [PubMed] [Google Scholar]
- 10.Dos Santos F, Drymiotou S, Antequera Martin A, Mol BW, Gale C, Devane D, Van’t Hooft J, Johnson MJ, Hogg M, Thangaratinam S. Development of a core outcome set for trials on induction of labour: an international multistakeholder Delphi study. BJOG. 2018 Dec;125(13):1673–1680. doi: 10.1111/1471-0528.15397. [DOI] [PubMed] [Google Scholar]
- 11.Giang HTN, Ulrich S, Tran HT, Bechtold-Dalla Pozza S. Monitoring and interventions are needed to reduce the very high Caesarean section rates in Vietnam. Acta Paediatr. 2018 Dec;107(12):2109–2114. doi: 10.1111/apa.14376. [DOI] [PubMed] [Google Scholar]
- 12.Takegata M, Smith C, Nguyen HAT, Thi HH, Thi Minh TN, Day LT, Kitamura T, Toizumi M, Dang DA, Yoshida LM. Reasons for Increased Caesarean Section Rate in Vietnam: A Qualitative Study among Vietnamese Mothers and Health Care Professionals. Healthcare (Basel) 2020 Feb 21;8(1):41. doi: 10.3390/healthcare8010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang X, Zhang C, Li X, Qi H, Liu Q, Lei J. Safety and efficacy of titrated oral misoprostol solution versus vaginal dinoprostone for induction of labor: A single-center randomized control trial. Int J Gynaecol Obstet. 2021 Sep;154(3):436–443. doi: 10.1002/ijgo.13546. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.De Bonrostro Torralba C, Tejero Cabrejas EL, Envid Lázaro BM, Franco Royo MJ, Roca Arquillué M, Campillos Maza JM. Low-dose vaginal misoprostol vs vaginal dinoprostone insert for induction of labor beyond 41st week: A randomized trial. Acta Obstet Gynecol Scand. 2019 Jul;98(7):913–919. doi: 10.1111/aogs.13556. [DOI] [PubMed] [Google Scholar]
- 15.Gaudineau A, Senat MV, Ehlinger V, Gallini A, Morin M, Olivier P, Roth E, Orusco E, Javoise S, Fort J, Lavergne C, Arnaud C, Rozenberg P, Vayssiere C Groupe de Recherche en Obstétrique rt Gynécologie. Induction of labor at term with vaginal misoprostol or a prostaglandin E2 pessary: a noninferiority randomized controlled trial. Am J Obstet Gynecol. 2021 Nov;225(5):542.e1–542.e8. doi: 10.1016/j.ajog.2021.04.226. [DOI] [PubMed] [Google Scholar]
- 16.Vogel JP, Oladapo OT, Dowswell T, Gülmezoglu AM. Updated WHO recommendation on intravenous tranexamic acid for the treatment of post-partum haemorrhage. Lancet Glob Health. 2018 Jan;6(1):e18–e19. doi: 10.1016/S2214-109X(17)30428-X. [DOI] [PubMed] [Google Scholar]
- 17.Obeidat RA, Almaaitah M, Ben-Sadon A, Istaiti D, Rawashdeh H, Hamadneh S, Hammouri H, Bataineh A. Clinical predictive factors for vaginal delivery following induction of labour among pregnant women in Jordan. BMC Pregnancy Childbirth. 2021 Oct 7;21(1):685. doi: 10.1186/s12884-021-04151-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sinkey RG, Blanchard CT, Szychowski JM, Ausbeck E, Subramaniam A, Neely CL, Casey BM, Tita AT. Elective Induction of Labor in the 39th Week of Gestation Compared With Expectant Management of Low-Risk Multiparous Women. Obstet Gynecol. 2019 Aug;134(2):282–287. doi: 10.1097/AOG.0000000000003371.. Erratum in: Obstet Gynecol. 2019 Oct; 134(4):884. [DOI] [PubMed] [Google Scholar]
- 19.Tolcher MC, Holbert MR, Weaver AL, McGree ME, Olson JE, El-Nashar SA, Famuyide AO, Brost BC. Predicting Cesarean Delivery After Induction of Labor Among Nulliparous Women at Term. Obstet Gynecol. 2015 Nov;126(5):1059–1068. doi: 10.1097/AOG.0000000000001083. [DOI] [PMC free article] [PubMed] [Google Scholar]


