Abstract
Objective:
Surgeon scientists bring to bear highly specialized talent and innovative and impactful solutions for complicated clinical problems. Our objective is to inform and provide framework for early stage surgeon scientist training and support.
Summary of Background Data:
Undergraduate, medical student, and residency experiences impact the career trajectory of surgeon scientists. To combat the attrition of the surgeon scientist pipeline, interventions are needed to engage trainees and to increase the likelihood of success of future surgeon scientists.
Methods:
A surgery resident writing group at an academic medical center, with guidance from faculty, prepared this guidance document for early stage surgeon scientist trainees with integration of the published literature to provide context. The publicly available National Institutes of Health RePORTER tool was queried to provide data salient to early stage surgeon scientist training.
Results:
The educational path of surgeons and the potential research career entry points are outlined. Challenges and critical supportive elements needed to inspire and sustain progress along the surgeon scientist training path are detailed. Funding mechanisms available to support formal scientific training of early stage surgeon scientists are identified and obstacles specific to surgical careers are discussed.
Conclusions:
This guidance enhances awareness of essential education, communication, infrastructure, resources, and advocacy by surgery leaders and other stakeholders to promote quality research training in residency and to re-invigorate the surgeon scientist pipeline.
Keywords: academic surgery, research in residency, surgeon scientist
Surgically treatable conditions account for an estimated one-third of the global burden of disease.1 Immersing surgical trainees in the breadth of foundational sciences necessary to conduct research at a high-level is critical for continued excellence and advancement in surgical care. Rigorously trained surgeon scientists provide immense societal value by leveraging their wealth of clinical experience and specialized scientific expertise to identify and resolve health care challenges through research, innovation, and team leadership. Surgeon scientists through discovery and mentorship of the next generation have great capacity to advance patient care and earn public trust for the return on investment in research funding.
Kibbe et al, recently raised the alarm over the threat of extinction of surgeon scientists, highlighting a downward trend of surgeon scientist pursuit of basic and translational research careers and decreased National Institutes of Health (NIH) awards to surgeon scientists over the last decade.2 Keswani et al reported a 27% decline in NIH funding to surgical departments between 2007 and 2014.3 Basic and translational science abstracts submitted to the Academic Surgical Conference declined from 48% to 27% between 2011 and 2015.2 Survey responses from many academic surgeons and leaders reflect their belief that it is no longer possible to be a successful surgeon scientist in today’s environment.3 Perceived obstacles for early career faculty include excessive clinical or administrative demands, a challenging funding environment and insufficient protected time.2–4 Losing the surgeon scientist pipeline would remove a critical segment of scientists who are motivated and uniquely positioned to recognize, investigate and craft innovative and impactful solutions for surgical patients. The concern over a vanishing surgeon scientist pipeline has been echoed in publications representing many surgical subspecialties including cardiothoracic surgery,5 pediatric surgery,6 and transplant surgery.7
Although much emphasis is justifiably oriented towards the mentorship and development of early career faculty towards scientific success, the training of early stage surgeon scientists at the undergraduate, medical student and resident levels warrants equal emphasis. Scientific exposure, formal training, and mentorship at early stages are associated with successful later-term outcomes for physician scientists.3,8 It is, therefore, necessary to explore the unique challenges faced by early surgeon scientist trainees and propose solutions that can facilitate successful long-term outcomes and, ultimately, the re-invigoration of the surgeon scientist pipeline. A variety of factors contribute to the obstacles facing early stage surgeon scientists seeking to pursue both a surgery and research career. The purpose of this document is to offer guidance for early stage surgeon scientist trainees (undergraduate, medical student, and resident trainees), surgeon scientist mentors, and residency programs seeking to enhance the research training experience. Additionally, it is our goal to communicate to funding agencies, including the NIH, how the uniquely lengthy surgeon scientist training path warrants special consideration and/or redesign of fellowship and training grant mechanisms to better align with the educational timeline for surgeon scientist trainees.
TRAINING PATHWAYS TO BECOMING A SURGEON SCIENTIST
The surgeon scientist training path is highly variable and distinct from other specialties. Opportunities to obtain formal research training can occur before medical school, during medical school (through summer research, longitudinal opportunities or a dedicated research year), through combined MD, PhD degree programs, in the immediate post-MD time frame, or as research during residency (Fig. 1). A common sentiment is that surgeon scientist trainees must “make their own path,” often feeling like this requires reinventing the wheel, specifically at key transition points that are vulnerable to attrition from the physician-scientist career path. Although common, this sentiment usually reflects an environment that lacks infrastructure and support which decreases the likelihood of long-term success. Critical opportunities exist to strengthen discrete stages along the surgeon scientist training pathway and form the basis for this guidance document.
FIGURE 1.

The early stage surgeon scientist training timeline. The path to becoming a surgeon scientist consists of a diverse array of formal research training opportunities spanning undergraduate education to surgery residency. Because a “proscriptive pathway” to academic research is not universal for surgeons, the mechanisms in place to support early career surgeon scientists must, therefore, be diverse and flexible. The surgeon scientist career path creates a unique gap between terminal research experience and the first faculty position that adversely impacts readiness for prototypical early career awards. This highlights the pressing need to create mechanisms that align with the unique surgeon scientist training timeline.
CAREER STAGE SPECIFIC GUIDANCE FOR SURGEON SCIENTIST TRAINEES
The Undergraduate and Medical Student Pipeline for Surgeon Scientist Careers
Perhaps one of the greatest challenges for the surgeon scientist pipeline at the undergraduate and medical student level is the issue of visibility. Surgeon scientists are often underrepresented in mentorship for students, and this results in a lack of awareness about the possibility and rewards of a surgeon scientist career. Likewise, many surgeon scientists are unaware or uninvolved in the organizations and programs that provide direct access and information to students, resulting in a bidirectional knowledge and communication gap. For example, medical students who visit the American Physician Scientists Association website will note the absence of surgery in the index for specialties.9 Although the main page does include surgery as an option for browsing by specialty, further investigation reveals only a single listed “surgery” program compared to multiple “medicine” programs. To create a robust surgeon scientist pipeline, intentional engagement of trainees at the earliest stages is needed to bridge this gap.
Core concepts for successfully engaging and training students include a broad exposure to scientific disciplines and methodology, availability of surgeon scientist mentors, and thoughtful planning to achieve meaningful and productive early research experiences. Surgeon scientist faculty have many opportunities to engage with undergraduate and medical students (Table 1) and to facilitate their exposure to surgeon scientists at a variety of career and training stages including senior students, residents, fellows, and junior faculty. Productive experiences are facilitated by tailored, level-appropriate research projects with progressive responsibility over a longitudinal experience of 1 year or more. For senior medical students, it is important to facilitate networking with career surgeon scientists and administrative leadership faculty who are committed to supporting surgeon scientist careers. These factors can overcome historical bias against the pursuit of research careers in surgery for young scientific trainees, a key barrier to recruitment.
TABLE 1.
Strategies for Surgeon Scientist Faculty to Engage Undergraduate and Medical Students Into the Surgeon Scientist Pipeline
| Undergraduates |
|
| Medical Students |
|
NIH indicates National Institutes of Health.
A key service that must be provided to medical students interested in surgeon scientist careers is help in identifying residency programs that support a future research career. Most residency programs voice interest in research at some level, but the extent of the infrastructure and support available within a program is not always easily interpreted for medical students. Ambiguity, a high degree of variability in program structure, junior status as a student, and stress associated with the residency match contribute to this problem. One way to facilitate this process for students is to empower them with concrete and informative questions to ask of programs (Table 2). It is important to examine the academic activities of the most senior leadership in a department including the chair, program director, research director, and others who are directly responsible for trainee education. Academic activities to note include the quality, quantity and types of publications, primary research project grant funding, participation in study sections or other research sponsorship and oversight organizations, and participation in national advocacy for research or research education. It is important to understand which principal investigators are available to directly mentor and train the resident surgeon scientist. Equally important is a concrete understanding of available funding sources, for both salary support and supply costs for research trainees in a program. Inquiring about the presence of a structured research experience is essential including opportunities for advanced degrees, supplemental coursework that will advance training, opportunities for presentation and department engagement with those presentations, and opportunities for travel for scientific presentations and meetings. Finally, students must look at the outcomes of a research training program. Although it may be possible to achieve a prolific surgeon scientist career based on training without these elements, lack of empowerment to ask the right questions should not be a limitation.
TABLE 2.
Questions to Guide Medical Students in Assessment of Research Training in Surgery Residency
|
NIH indicates National Institutes of Health.
One way to assess the feasibility of physician scientist pipeline recruitment into surgical specialties is to examine outcomes from dual degree MD, PhD training programs. In April 2018, the American Association of Medical Colleges (AAMC) released a longitudinal outcomes report of surveys sent to 10,591 known graduates of MD, PhD programs from 1975 to 2015.10 At the time of the report, it was noted that 10.2% of all graduates still in residency training were distributed amongst the surgical specialties. To analyze trends, data were subdivided into those who had completed residency training and those currently still in training. Amongst those who had completed training (1975–2014), 7.9% (280/3,543) of all men and 4.4% (49/1104) of all women pursued a surgical specialty. Amongst those still in training (as of 2015), 11.8% (157/1331) of all men and 7.6% (60/793) of all women entered a surgical specialty (Fig. 2, left panel). When analyzed by surgical specialty, the majority of graduates pursued training in general surgery or neurosurgery (Fig. 2, right panel), and this finding was not changed between MD, PhD graduates who had completed residency versus those who were still in residency. Collectively, this data highlights a promising upward trend in terms of recruitment of physician scientist trainees into surgical specialties but emphasizes the urgent need to ensure deliberate surgeon scientist recruitment, comprehensive surgeon scientist career development, and robust research training during residency.
FIGURE 2.

Entry of MD, PhD graduates into surgical specialties. Data were obtained from the 2018 AAMC report,14 Supplemental Tables 7 and 8 reviewing longitudinal career outcomes of trainees (6786 survey respondents out of 10,591 alumni identified) from combined MD, PhD training programs. Internal medicine is provided as a reference as the most frequently chosen specialty. In the cohort of graduates who had completed residency training (1975–2014), 7.9% (280/3543) of all men and 4.4% (49/1104) of all women pursued a surgical specialty. In the cohort of those still in residency training (as of 2015), 11.8% (157/1331) of all men and 7.6% (60/793) of all women entered a surgical specialty. Neurosurgery and General Surgery were the 2 most common surgical specialties chosen by MD, PhD program graduates. CRS indicates colon and rectal surgery; CTS, cardiothoracic surgery; ENT, otolaryngology; GS, general surgery; NS, neurosurgery; OS, orthopedic surgery; PS, plastic surgery; US, urologic surgery; VS, vascular surgery.
Core Components for Training Residents as Surgeon Scientists
Residency training represents the most common career stage for initial exposure to research for many surgeon scientists.11 Exposure to clinical dilemmas and unique patient populations during training is a pivotal motivator for many residents who ultimately become surgeon scientists.11,12 Core components for training residents in research include dedicated program administration, advanced preparation before entering dedicated research years, protected research time that includes a structured research experience with formal coursework, career development opportunities and a mentoring plan, and assistance navigating the bridge to first faculty appointment (Table 3).
TABLE 3.
Best Practices for Research in Residency Training for Surgeon Scientists
| Program administration |
|
| Before the research years |
|
| During the research years |
|
| After the research years |
|
Research Program Administration
Dedicated program leadership, faculty, staff, and financial resources are critical to the success of the research program. Financial resources are needed for resident salary and benefits, personnel, educational activities, tuition, and scientific travel. A successful program requires the availability of dedicated, successful, and diverse research mentors at multiple career stages (assistant, associate, and full professor). Not all surgical trainees require a surgical faculty research mentor and many should consider mentors and/or co-mentors outside of the surgical department. However, there should be sufficient critical mass of research mentors in the department and intellectual buy-in from the entire surgical faculty whether or not they lead independent research programs. This latter point is important to cultivate an environment that values and continually underscores the connection between research and optimal patient care.
Before Entering the Research Years
Formal research training for residents requires purposeful planning that must occur before entering the research years. Preparation must begin as early as the intern year. Key components of preparation include exposing residents to different types of research (basic science, health services, quality improvement, education, global surgery, innovation, and policy research), the identification of mentor and project, formal instruction in fellowship-specific grant writing, and planning for enrollment in advanced degree programs.
Trainees can be exposed to different research disciplines and methodologies by engaging in bi-weekly or monthly seminars with invited speakers during their early clinical years. This serves the dual purpose of exposure to different disciplines and also potential mentors. An additional way to jumpstart mentor selection efficiently is to hold a “research interest day” or a “research interest seminar series” where faculty who are actively seeking to recruit trainees are invited to present available projects.
Early selection of the research mentor and establishment of the research project enables timely preparation and submission of fellowship applications. A common pitfall is that surgical trainees often begin this process too late. For example, the time from an NIH F32 individual postdoctoral research fellowship application submission to award start date can be as great as 10 months. This does not include the common necessity for revision and resubmission (an additional 6 months) or the initial time to draft the proposal (4–6 months). Therefore, if an applicant waits to begin contemplating a competitive grant submission until the beginning of a 2-year research in residency experience, they will not have time to fully benefit from funding obtained. We recommend that a program hold informational sessions reviewing available fellowship funding opportunities and begin formal education for grant writing early. It is important to include both general grant writing topics and instruction for fellowship-specific grant writing. It is fundamental that these sessions include an overview of the NIH organization and processes, as the largest public source of biomedical research funding in the United States.
Lastly, trainees should consider a degree-granting program during their research time. Depending on the type of research pursued, obtaining an advanced degree may be useful but should be discussed with the mentor team regarding the pros and cons. Obtaining an advanced degree, such as a Master program (including Master of Medical Science, Public Health, Health Administration etc), or a PhD, provides a structured research experience, formal coursework, interaction with trainees in other fields outside of surgery, additional career development opportunities, and an advantage for pursuit of future research endeavors. The pursuit of additional degrees can be viewed as an opportunity for multiple “on-ramps” for surgeon scientists. Advanced degree training during residency has distinct advantages for surgeon scientists and other physician scientists with longer clinical training timelines. Daye et al noted that timing PhD training when trainees have already selected their area of clinical specialty better aligns training for a future physician scientist career. They also posit “by placing their intensive PhD research training closer to the time of research independence, trainees will be far less removed from the research techniques and expertise they have developed.13“ Funding for certain advanced degrees can be obtained through tuition-assistance programs available to employees of academic medical centers, through allocated departmental funds or institutional training grants, or through a specific budget line-item for tuition available on many individual research fellowship awards. Pursuit of an additional degree requires programmatic planning designed with the trainee well before entering the dedicated research years.
During the Research Years
Protected Research Time
Central to an effective research training program is the establishment of a departmental culture and environment that visibly supports the research mission. One way to establish research as a priority within a training environment is the allotment of formal protected time for trainee research.14 Length of protected time can vary. In general, many residency programs incorporate 1 to 3 years of formal research training after the second or third clinical year.12 Protected time should be of sufficient length to allow for peak productivity and to achieve the trainee’s goals, which may vary substantially depending on scientific discipline and methodology. It is also important to note that many research fellowship sponsors expect a commitment of at least 2 years. The maximum number of years allowed for protected research usually depends on multiple factors including Accreditation Council for Graduate Medical Education and Residency Review Committee limitations. The recommendation for protected research time during surgery residency is supported by literature demonstrating that the inclusion of protected research time substantially increases research productivity and future funding success.11,14–16 A protected research experience during surgery residency is also associated with selection of a career path in academic surgery, continued engagement in research, success in applying for research funding including NIH funding and advancement to leadership positions in academic surgery.17
Research Mentorship
The establishment of a diverse mentorship committee consisting of 3 to 4 faculty mentors for each resident is highly recommended. The quality of the research mentoring relationship is the most important for future success of an independent research program.18 Responsibilities for faculty research mentors within and outside the Department of Surgery must be clearly communicated. Similarly, responsibilities of surgical trainees for their own lifelong learning, mentor expectations, and contribution to the learning environment require clarity and consistent reinforcement. These responsibilities and expectations should be consistent with national guidelines such as the AAMC Postdoctoral Compact19 and communicated in multiple formats including in-person group informational sessions, one-on-one with trainees by the program director and program coordinator, codified in a departmental research training program handbook and with a signed mentor/mentee compact before initiation of the research training experience. Frequent oversight by program leadership to monitor the health of these interactions is an important responsibility.
Structured Research Experience
A structured research experience should include an orientation, development of a mentoring plan, conduct of a mentored research project, formal didactics, periodic evaluation of trainee progress, and opportunities to engage in scientific communication and networking (Table 3). The resident, in collaboration with the mentor, should prepare an individual development plan that outlines trainee goals and a concrete plan for how to achieve them. An individual development plan establishes a structured, goal-oriented research experience, and should be updated at least annually. Regardless of the type of research or advanced degree program, curricular content should include instruction in research methods and design, biostatistics, research ethics, and grant writing and include seminars or journal clubs for critical review of scientific literature.
The importance of enhancing oral and written science communication skills through scientific presentations and publications cannot be overstated. Scientific presentation skills should be practiced at the individual research group level (such as a lab meeting), at the departmental or institutional level (such as Works-In-Progress seminar series or annual research conferences), and at the national level. To become adept at scientific communication, trainees must present their work frequently and progressively over a longitudinal experience to a panel of established scientific mentors capable of providing constructive feedback. Presentation at national forums allows trainees to experience input from a diverse scientific audience and also provides critical networking opportunities. Publication productivity is an important metric because publication number correlates with later success in competing for extramural research funding.20,21
During research training, residents should gain experience preparing their NIH Biosketch and personal statement, understand fundamentals of the NIH organization, be aware of NIH physician scientist career development award funding mechanisms, and understand fundamentals of the grant submission and review process and the associated timelines. At the completion of research education and training, residents should have acquired the knowledge and skills to identify important clinical problems and to design a focused research project to answer a specific question, to think critically as they review papers and analyze data, to identify and resolve research related ethical issues, to write high quality manuscripts, to deliver high quality presentations, to identify research funding opportunities and apply for grants, and to prepare research compliance applications such as human subjects research (Institutional Review Board) or animal use (Institutional Animal Care and Use Committee) protocols. These recommendations are supported by research correlating formal research training curriculum during residency with increased publication productivity and quality22–24 and success in obtaining research funding22,25
Career Development
Residents should have many opportunities to enhance their professional development through self-reflection, serial feedback from mentors and program leaders, research teamwork, collaborative team science, professional networking, and formal guidance in preparing for next steps in their academic career. One example from the authors’ institution includes a “Career Development for Surgeons” course that reviews professional academic skills specific to surgeon scientists. Content examples of this course include identifying and adapting career goals, selection of academic mentors, continuous self-improvement for surgical excellence, leadership and collaboration skills, fundamentals of healthcare economics, introduction to professional and surgical societies, career resources, and strategies to optimize the first faculty appointment.
Funding for Resident Surgeon Scientists
A key consideration for residency training programs is funding to support residents during research years. Surgery departments plays an important role in funding residents for research through either departmental funds or philanthropic sources. Even when a trainee is successful in obtaining intramural or extramural stipend support, gaps in the level of support or benefits can still occur. It is important that departmental supplemental funding is available to cover these gaps. Residents should not incur a pay-cut or loss of benefits relative to their postgraduate year (PGY) level salary and benefits when they transition to the research years as this penalization provides substantial disincentive to pursue research training.
Diversification of funding sources beyond departmental funds can be achieved by facilitating early resident applications to multiple research training sponsors. Resources that distill and explain both internal and external sources of funding are crucial for junior residents as they establish research training plans. Additionally, conversations about funding should extend beyond salary support to include details about funding for research supplies, conference registration fees and travel, poster printing, and tuition for advanced coursework. Empowerment with this information is crucial for residents to select a research environment that best fits their goals. Many academic medical centers offer institutional fellowship awards through a research center fellowship program, institutional NIH T32 training grants or an NIH Clinical and Translational Science Awards affiliated TL1 training program. Surgeon scientist faculty should consider leadership of NIH T32 training grants that support resident postdoctoral research training. A recent single institution experience reported that leadership of T32 NIH grants by departmental faculty was independently predictive of research productivity for their residents.26 In a survey of 200 residency programs, 24% of resident research fellowships were supported by T32s.27 Residents are also eligible to apply for NIH F32 individual postdoctoral fellowship awards (F32). US citizenship or permanent residency is required for all NIH sponsored training awards. These awards provide funding for stipend and benefits and tuition. Research grants for residents are also offered by professional organizations such as the American College of Surgeons, the Society for University Surgeons, the Association for Academic Surgery, and by many surgery subspecialty and disease-focused professional organizations. An example of the return on investment of surgical society-sponsored fellowship awards can be appreciated by data indicating that 48% percent of prior Society of University Surgeons fellowship awardees successfully competed for peer-reviewed funding and, of these, 30% received an R01 or equivalent funding.28
The experience of applying for competitive fellowship funding exposes residents to the fundamentals and nuances of grant writing and better prepares them for future applications. Indeed, data suggests that trainees able to successfully compete for funding during residency translate to funding awards following training.28,29 The NIH F32 mechanism is highly competitive, most commonly pursued by PhD postdoctoral trainees, and underutilized by surgeon scientist postdoctoral trainees. We reviewed F32s awarded by surgical department and identified only 32 awards in total to surgical departments, nationally, for the years 2018 and 2019 (Fig. 3). Of these, most were awarded to PhD postdoctoral trainees in the respective surgical department whereas only 9 were awarded to surgeon scientist trainees possessing either MD or MD, PhD degrees. We posit that surgical residents may be insufficiently mentored on how to apply for F32s, and/or that the necessity of early submission between the PGY-1 to PGY-3 years before the dedicated research years may limit applications. The discordance between the F32 mechanism with surgeon scientist training timeline undoubtedly reflects the meager number of F32 awards to surgical trainees. F32 recipients, however, are more likely to receive future R01 funding, and it is, therefore, important to increase awareness about this highly competitive and recognized mechanism for surgeon scientist trainees.30 Residents should be informed that they can concurrently apply for an NIH T32 or F32 award and to the NIH loan repayment program. Loan repayment program awardees receive up to $50,000 per year in repayment of student educational debt.
FIGURE 3.
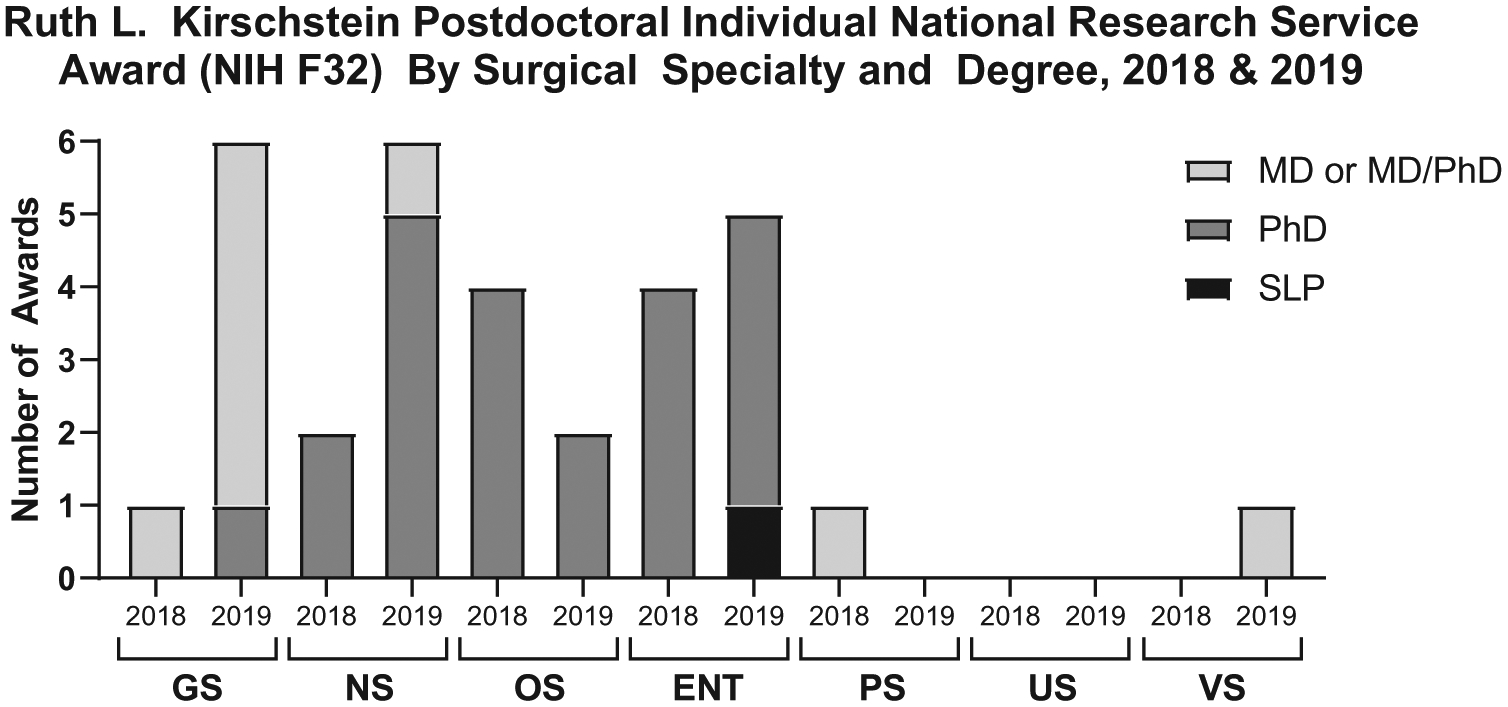
Paucity of NIH F32 Awards to MD or dual degree MD, PhD applicants in Surgical Departments (2018, 2019). Data were obtained by NIH RePORTER search for F32 awards (2018, 2019) and filtered by department. Data were refined to include the available surgical department categories on NIH Reporter: neurosurgery, urology, otolaryngology, surgery, orthopedic surgery, and plastic surgery. F32 awardees were cross-referenced by institutional profiles for credentials and categorized by degrees MD, MD, and PhD, PhD or SLP (speech language pathology). The number of NIH F32 awards to MD or dual degree MD, PhD applicants in surgical departments ranged from 0 to 5. NIH RePORTER data were accessed March 2020. Data are only available for awards primarily distributed to a surgical department, with the possibility of undercounting surgical trainee awards that may be primarily distributed to other departments. NIH indicates National Institutes of Health.
In response to the NIH Director’s 2014 ad hoc Physician Scientist Working Group report31 highlighting disturbing downward trends in the physician-scientist pipeline, the NIH initiated new training grant funding mechanisms that specifically encourage research during residency. The “Stimulating Access to Research in Residency” (StARR/R38) grant seeks to provide research funding and opportunities integrated into clinical training and is specifically applicable only for residents in training. This mechanism also provides trainees with a subsequent R38-linked option to apply for a “Transitional Scholar” K38 grant to support mentored research during a clinical fellowship or early faculty position. The inherent flexibility of this pathway helps alleviate the gap in funding and lack of sufficient protected time for research that clinical residents and fellows often encounter when they transition to a junior faculty position, enhancing the likelihood of successful transition to research independence. K38 awardees are eligible to subsequently apply for conventional K career development grants (K08, K23, KL2, and K99) and independent research project awards (eg, R21, R01). Currently, only 4 NIH institutes participate in this R38/K38 funding opportunity including National Heart, Lung and Blood Institute, National Cancer Institute (NCI), National Institute on Aging, and National Institute on Allergy and Infectious Diseases. Unfortunately, this research in residency opportunity remains limited as only 3 institutions have successfully competed for funding to pilot this new mechanism and only 1 of the 3 funded R38 programs includes eligibility for surgical trainees (cardiovascular surgical trainees). Another relatively new physician-scientist funding opportunity is the K99/R00 Physician-Scientist Pathway to Independence Award that aims to facilitate transition from mentored postdoctoral position to independent physician-scientist.
Diversity in the Biomedical Workforce
NIH values diversity in the biomedical workforce and has many funding mechanisms in place to support underrepresented in medicine (URM) research trainees. One mechanism that is available to support URM trainees being trained in the laboratory of an NIH funded investigator is the “NIH Research Supplement to Promote Diversity in Health-Related Research.” These are awarded as an administrative supplement to the parent NIH award (also known as NIH Diversity Supplements) and are an excellent way for surgeon scientists to diversify the surgeon scientist pipeline.
After the Research Years: Bridging From Terminal Research Training to First Faculty Position
After the completion of research years, navigating the bridge from the terminal research training experience to the first faculty position can be a perilous transition with high attrition for surgeon scientists. This period is challenged by the variability in time available for research and publication productivity during surgical fellowships.32 Successful residency training programs are those that place an emphasis on mentoring future surgeon scientists in navigating this transition by assisting with fellowship selection and placement, providing support for planning early career award applications, and advice for negotiating the first faculty appointment.
Brass et al examined the AAMC report of MD, PhD program outcomes, specifically addressing the percent effort dedicated towards research in graduates’ faculty position. It was noted that 67% of graduates in all fields of surgery reported a full-time academic appointment, which approached the mean for academic careers amongst MD, PhD graduates across all specialties. Notably, however, only 16% of graduates who transitioned into surgery were appointed at a minimum of 50% research effort, which was substantially lower than in pediatrics (50%), internal medicine (53%), and neurology (54%).33 Although it is possible that this data does not reflect the actual amount of time devoted to research, it may also represent an alarming rate of attrition of research effort for surgeons, resulting in substantial loss of the training investment in physician-scientist careers. These findings highlight the critical need for national and institutional financial investment to support surgeon scientist research effort especially at this critical stage, and intentional career development for surgeon scientist trainees to navigate critical career transitions.
Surgical training is unique in its longer duration of residency, longer gaps between formal research experiences, and a large gap between the terminal research experience and first faculty appointment (Fig. 1). This contrasts with the more common physician scientist training model for medical specialists where residency and clinical fellowships are often followed by formal postdoctoral research training that segues into the first faculty position. The advantage of the latter is that it allows for the necessary maturation of research ideas, preliminary data gathering, and mentorship to compete for early career awards, such as the K-series, in immediate succession. This pathway can be “fast-tracked” for medical specialists through physician scientist training programs (PSTP) that mirror the earlier medical scientist training programs (MSTP). However, even within these established frameworks, attrition at transition points in training remains a concern.34
As a result of the lengthy delay for surgeons between the terminal research experience and application for early career awards, valuable opportunities for preliminary data generation, mentorship and planning are lost at this critical junction. The average length of time for surgeon scientists across surgical disciplines to obtain K award funding is 3.9 (+/− 2.0) years with the greatest length of time occurring for plastic surgeons (4.8+/− 2.4 years) and the shortest length of time occurring for neurosurgeons (3.4+/− 1.5 years) (P = ns) (Fig. 4). Another challenge for surgeon scientists is the incongruence between departmental/divisional expectations for clinical productivity and NIH requirement of 75% effort on K career development awards. The National Institute of Diabetes and Digestive and Kidney Diseases and NCI are unique in their longstanding exception for urologic surgeons in requiring a minimum of 50% protected time.35 This exception recognizes that surgeons must remain technically adept through clinical practice, and especially early-career clinical practice. However, this exception is not widely available to all surgeon scientists. In 2017, the National Heart, Lung, and Blood Institute policy was revised to permit less than 75% effort on K08 and K23 grants for procedure-oriented specialties including cardiothoracic, vascular, and trauma surgeons, interventional cardiologists, and electrophysiology cardiologists.36 Other NIH Institutes and Centers that now have comparable effort exceptions for specific surgical subspecialties are listed in Table 4.37–39 Physician-scientist trainees in other nonsurgical specialties have highlighted the benefit of “relaxing” the percent effort requirement and lengthening the training period on K grants to accommodate clinical responsibilities of junior faculty.13 However, the explicit permission for less than 75% effort on K career development awards across all NIH institutes will likely only be achieved through focused advocacy efforts by major professional organizations such as the American Surgical Association, the American College of Surgeons, the American Board of Surgery, the Society of Surgical Chairs, Society of University Surgeons, Association of Academic Surgery and subspecialty organizations. Propagation of awareness and need for advocacy regarding surgeon scientist-specific challenges are especially important to communicate with funding agencies.
FIGURE 4.

Years from completion of clinical training to K award for surgeon scientists across surgical specialties. Data were obtained by NIH RePORTER search for K series awards (2014–2019) and filtered by department. Data were refined to include the available surgical department categories on NIH RePORTER: neurosurgery, urology, otolaryngology, surgery, orthopedic surgery, and plastic surgery. Year of terminal clinical training (fellowship or residency if no fellowship) was obtained from publicly available institutional faculty profiles or Linked In profile account, and the difference calculated. Groups were compared using a 1-way ANOVA with Tukey test for multiple comparisons. NIH RePORTER data were accessed March 2020. ANOVA indicates analysis of variance; NIH, National Institutes of Health.
TABLE 4.
NIH Institutes and Centers with Effort Exceptions for Surgeon Scientist K-Awards
| NIH Institute or Center | Eligibility and Surgical Specialty Effort Exception | Reference |
|---|---|---|
| NIDDK and NCI |
|
35 |
| NHLBI |
|
36 |
| NCI | NCI Request for Information (RFI) pending:
|
37 |
| NEI |
|
38 |
| NIAMS |
|
38 |
| NIDCD |
|
38 |
| NIMH |
|
38 |
| NINDS |
|
38 |
| NCATS (KL2 through CTSA) |
|
38 |
CTSA, Clinical and Translational Science Awards; NCATS, National Center for Advancing Translational Sciences; NCI, National Cancer Institute; NEI, National Eye Institute; NIAMS, National Institute of Arthritis and Musculoskeletal and Skin Diseases; NIDCD, National Institute on Deafness and Other Communication Disorders; NIMH, National Institute of Mental Health; NINDS, National Institute of Neurological Disorders and Stroke; NHLBI, National Heart, Lung and Blood Institute; NIDDK, National Institute of Diabetes and Digestive and Kidney Diseases.
LOOKING TO THE FUTURE: THE DEVELOPMENT OF COMBINED SURGEON SCIENTIST TRAINING PROGRAMS
There is a tendency to compartmentalize training for physician scientists. Trainees are instructed to focus only on clinical training during 1 period, worry about the science later, and vice versa during other stages. It is worth questioning the wisdom of this approach. The NIH recognizes the value of combined training approaches by supporting MSTP whereby dual-degree MD, PhD trainees are continually engaged in translational scientific curriculum throughout the duration of their training. The benefit is that, although learning clinical medicine and developing scientific expertise, they are also simultaneously practicing a third element provided by the MD, PhD program infrastructure, which is the discrete skill set required to merge the 2.
The integration of clinical and scientific training affords a critically valuable opportunity to think about clinical problems through a scientific lens and to think about clinical application of new scientific methodologies and discoveries. However, if this experience for surgeon scientists is not realized until the junior faculty level, it may be exceedingly difficult to capitalize upon this translational potential when also challenged with high clinical and professional demands. Training before the first faculty position usually requires 16–20 years beyond postsecondary education. Imagine the benefit of continually engaging in a combined, integrated, translational mindset for 16–20 years. What benefit might this achieve in preparing early faculty to establish an independent research program along with their clinical practice? Many would argue that the beginning stages of switching thought processes back and forth between the clinic and the lab is difficult and that the translational mindset is a learned skill that must be practiced. Innovative ways to allow surgeon scientist trainees to “practice” this skillset throughout the entirety of their training are needed.
Combined training programs, such as the MSTPs and PSTPs have proven success for high yield outcomes including publication productivity, retention in academic medicine, and competitiveness for early career funding and subsequent research project grant funding.40–43 This argues against the need to re-invent the wheel, but rather to learn and adopt from already established principles. As envisioned in the new NIH pilot StARR program, scientific training can be dispersed during residency. Research training could begin during short periods at the outset of residency leading to full time research at the later stages of clinical training establishing the foundation for a competitive application for an early career development award. Departments could consider establishing a resident research lab sourced with equipment, research technicians, and a lab manager that could facilitate ongoing resident-led experimentation even after returning to clinical training.44
Variability between research training opportunities in individual departments results in few trainees obtaining formal scientific training at any given time. The downstream consequence of this is a decreased opportunity to establish pipeline infrastructure and prescriptive training paradigms, in part, due to lack of “critical mass” to warrant investment in infrastructure. This is especially problematic for surgical subspecialties where only 1 or 2 trainees may be pursuing scientific experiences at a time. To accrue economies of scale and foster multidisciplinary trainee collaborations and teamwork, perhaps all surgical disciplines could combine surgeon scientist training under 1 umbrella institutional “Surgeon Scientist Training Program,” similar to the umbrella PSTPs for the Internal Medicine subspecialties. Academic medical centers stand to benefit from investment in infrastructure for training and support of all physician-scientist trainees and faculty, as this workforce distinguishes the unique role, capacity, and transformational potential of academic medical centers to spearhead innovations in health care.
Leadership is necessary to achieve national visibility of the importance of the surgeon scientist workforce, to establish centralized oversight for the quality and outcomes of surgeon scientist training, and to advocate for surgeon scientist funding from the NIH, academic medical centers, surgery professional organizations, and philanthropic sources. The American College of Surgeons, by virtue of its prestige, diverse membership, and organizational breadth and depth, is poised to lead this effort as advocated in the 2004 Blue Ribbon Committee Report.10 Progress towards these goals will synergize to transform the current path fraught with variability in surgeon scientist training and career development, insufficient financial resource allocation, and high vulnerability for attrition into a structured and transparent career path designed for success.
ACKNOWLEDGMENT
The authors would like to acknowledge Jacob Zbinden for assistance with figure formatting.
JCB was supported by NIH F32HL144120, NIH T32AI106704, and the Ohio State University President’s Postdoctoral Scholar Program. AJ was supported by NIH T32AI106704. AO was supported by NIH T32AI106704 and the AAS/AASF Trainee Basic Science/Translational Research Fellowship Award. RS was supported by an NIH Diversity Supplement Award. GLB is PI/PD of the NIH T32AI106704 (Advanced Training in Immunology for Surgical Trainees). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors report no conflicts of interest.
REFERENCES
- 1.Meara JG, Leather AJ, Hagander L, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–624. [DOI] [PubMed] [Google Scholar]
- 2.Kibbe MR, Velazquez OC. The extinction of the surgeon scientist. Ann Surg. 2017;265:1060–1061. [DOI] [PubMed] [Google Scholar]
- 3.Keswani SG, Moles CM, Morowitz M, et al. The future of basic science in academic surgery: identifying barriers to success for surgeon scientists. Ann Surg. 2017;265:1053–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hu Y, Edwards BL, Brooks KD, et al. Recent trends in National Institutes of Health funding for surgery: 2003 to 2013. Am J Surg 2015. 2015;209:1083–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Narahari AK, Mehaffey JH, Hawkins RB, et al. Surgeon scientists are disproportionately affected by declining nih funding rates. J Am Coll Surg. 2018;226:474–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Markel TA, Valsangkar NP, Bell TM, et al. Endangered academia: preserving the pediatric surgeon scientist. J Pediatr Surg. 2017;52:1079–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Englesbe MJ, Sung RS, Segev DL. Young transplant surgeons and NIH funding. Am J Transplant. 2011;11:245–252. [DOI] [PubMed] [Google Scholar]
- 8.Strong MJ, Busing N, Goosney DL, et al. The rising challenge of training physician-scientists: recommendations from a Canadian National Consensus Conference. Acad Med. 2018;93:172–178. [DOI] [PubMed] [Google Scholar]
- 9.American Physician Scientists Association. Available at: www.physician-scientists.org. Accessed November 1, 2020.
- 10.Akabas MH, Tartakovsky I, Brass LF. National MD-PhD Program Outcomes Study. 2018. Available at: https://store.aamc.org/downloadable/download/sample/sample_id/162/. Accessed July 5, 2020.
- 11.Goldstein AM, Blair AB, Keswani SG, et al. A roadmap for aspiring surgeon scientists in today’s healthcare environment. Ann Surg. 2019;269:66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mansukhani NA, Patti MG, Kibbe MR. Rebranding “the lab years” as “professional development” in order to redefine the modern surgeon scientist. Ann Surg. 2017;266:937–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daye D, Patel CB, Ahn J, et al. Challenges and opportunities for reinvigorating the physician-scientist pipeline. J Clin Invest. 2015;125:883–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arbuckle MR, Gordon JA, Pincus HA, et al. Bridging the gap: supporting translational research careers through an integrated research track within residency training. Acad Med. 2013;88:759–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pickering CR, Bast RC Jr, Keyomarsi K. How will we recruit, train, and retain physicians and scientists to conduct translational cancer research? Cancer. 2015;121:806–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andriole DA, Klingensmith ME, Fields RC, et al. Is dedicated research time during surgery residency associated with surgeons’ future career paths?: a national study. Ann Surg. 2020;271:590–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhattacharya SD, Williams JB, de la Fuente SG, et al. Does protected research time during general surgery training contribute to graduates’ career choice? Am Surg. 2011;77:907–910. [PMC free article] [PubMed] [Google Scholar]
- 18.Lienard JF, Achakulvisut T, Acuna DE, et al. Intellectual synthesis in mentorship determines success in academic careers. Nat Commun. 2018;9:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.AAMC. Compact Between Postdoctoral Appointees and Their Mentors. Available at: https://store.aamc.org/compact-between-postdoctoral-appointees-and-their-mentors-pdf.html. Accessed July 5, 2020.
- 20.Ellis MC, Dhungel B, Weerasinghe R, et al. Trends in research time, fellowship training, and practice patterns among general surgery graduates. J Surg Educ. 2011;68:309–312. [DOI] [PubMed] [Google Scholar]
- 21.Lessin MS, Klein MD. Does research during general surgery residency correlate with academic pursuits after pediatric surgery residency? J Pediatr Surg. 1995;30:1310–1313. [DOI] [PubMed] [Google Scholar]
- 22.Hsieh H, Paquette F, Fraser SA, et al. Formal research training during surgical residency: scaffolding for academic success. Am J Surg. 2014;207:141–145. [DOI] [PubMed] [Google Scholar]
- 23.Joshua Smith J, Patel RK, Chen X, et al. Does intentional support of degree programs in general surgery residency affect research productivity or pursuit of academic surgery? J Surg Educ. 2014;71:486–491. [DOI] [PubMed] [Google Scholar]
- 24.Farrokhyar F, Amin N, Dath D, et al. Impact of the surgical research methodology program on surgical residents’ research profiles. J Surg Educ. 2014;71:513–520. [DOI] [PubMed] [Google Scholar]
- 25.Lopez J, Ameri A, Susarla SM, et al. Does formal research training lead to academic success in plastic surgery? A comprehensive analysis of U.S. academic plastic surgeons. J Surg Educ. 2016;73:422–428. [DOI] [PubMed] [Google Scholar]
- 26.Chen JX, Kozin ED, Sethi RK, et al. Increased resident research over an 18-year period: a single institution’s experience. Otolaryngol Head Neck Surg. 2015;153:350–356. [DOI] [PubMed] [Google Scholar]
- 27.Robertson CM, Klingensmith ME, Coopersmith CM. Prevalence and cost of full-time research fellowships during general surgery residency. Ann Surg. 2009;250:352. [DOI] [PubMed] [Google Scholar]
- 28.Hassan B, Bernstam E, Hines OJ, et al. Career track of society of university surgeons resident research award recipients. J Surg Res. 2013;185:92–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones DR, Mack MJ, Patterson GA, et al. A positive return on investment: research funding by the Thoracic Surgery Foundation for Research and Education (TSFRE). J Thorac Cardiovasc Surg. 2011;141:1103–1106. [DOI] [PubMed] [Google Scholar]
- 30.Price M Training Fellowship Recipients Are More Likely To Get Future Funding. Science 2018. Apr. 25, 2018. Available at: https://www.sciencemag.org/careers/2018/04/training-fellowship-recipients-are-more-likely-get-future-funding. Accessed July 5, 2020.
- 31.Ginsburg D, Mills S, Shurin S, et al. Phyisician-Scientist Workforce Working Group Report. NIH ACD Report. 2014. Available at: https://acd.od.nih.gov/documents/reports/PSW_Report_ACD_06042014.pdf. Accessed July 5, 2020.
- 32.Grova MM, Yang AD, Humphries MD, et al. Dedicated research time during surgery residency leads to a significant decline in self-assessed clinical aptitude and surgical skills. J Surg Educ. 2017;74:980–985. [DOI] [PubMed] [Google Scholar]
- 33.Brass LF, Akabas MH. The national MD-PhD program outcomes study: relationships between medical specialty, training duration, research effort, and career paths. JCI Insight. 2019;4:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Williams CS, Iness AN, Baron RM, et al. Training the physician-scientist: views from program directors and aspiring young investigators. JCI Insight. 2018;3:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.NIDDK and NCI Career Development Program Urologic Surgeons. Available at: https://grants.nih.gov/grants/guide/notice-files/NOT-DK-05-015.html. Accessed November 1, 2020.
- 36.NHLBI Policy Concerning Mentored Career Development (K08 and K23) Awards: Percent Effort. Available at: https://grants.nih.gov/grants/guide/notice-files/NOT-HL-21-003.html. Accessed November 1, 2020.
- 37.NOT-CA-21–027: Request for Information (RFI): Inviting Comments and Suggestions on the surgeon scientist effort requirement on K08 awards from the National Cancer Institute. Available at: https://grants.nih.gov/grants/guide/notice-files/NOT-CA-21-027.html. Accessed January 30, 2021.
- 38.PA-20–203: Table of IC-Specific Information, Requirements and Staff Contacts. Available at: https://grants.nih.gov/grants/guide/contacts/parent-K08-CT-not-allowed.html. Accessed January 30, 2021.
- 39.PAR-18–464: Clinical and Translational Science Award (U54 Clinical Trial Optional). Available at: https://grants.nih.gov/grants/guide/pa-files/PAR-18-464.html. Accessed January 30, 2021.
- 40.Muslin AJ, Kornfeld S, Polonsky KS. The physician scientist training program in internal medicine at Washington University School of Medicine. Acad Med. 2009;84:468–471. [DOI] [PubMed] [Google Scholar]
- 41.Harding CV, Akabas MH, Andersen OS. History and outcomes of 50 years of physician-scientist training in medical scientist training programs. Acad Med. 2017;92:1390–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kosik RO, Tran DT, Fan AP, et al. Physician scientist training in the United States: a survey of the current literature. Eval Health Prof. 2016;39:3–20. [DOI] [PubMed] [Google Scholar]
- 43.Brass LF, Akabas MH, Burnley LD, et al. Are MD-PhD programs meeting their goals? An analysis of career choices made by graduates of 24 MD-PhD programs. Acad Med. 2010;85:692–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dzirasa K, Krishnan RR, Williams RS. Incubating the research independence of a medical scientist training program graduate: a case study. Acad Med. 2015;90:176–179. [DOI] [PMC free article] [PubMed] [Google Scholar]


