Abstract
Background:
There is limited evidence on the efficacy of per-oral endoscopic myotomy (POEM) in patients with esophageal diverticula.
Aims:
This meta-analysis aimed to assess the efficacy and safety profile of POEM in patients with Zenker’s (ZD) and epiphrenic diverticula.
Methods:
With a literature search through August 2020, we identified 12 studies (300 patients) assessing POEM in patients with esophageal diverticula. Primary outcome was treatment success. Results were expressed as pooled rates and 95% confidence intervals (CI).
Results:
Pooled rate of technical success was 95.9% (93.4%−98.3%) in ZD patients and 95.1% (88.8%−100%) in patients with epiphrenic diverticula. Pooled rate of treatment success was similar for ZD (90.6%, 87.1%−94.1%) and epiphrenic diverticula (94.2%, 87.3%−100%). Rates of treatment success were maintained at 1 year (90%, 86.4%−97.4%) and 2 years (89.6%, 82.2%−96.9%) in ZD patients. Pooled rate of symptom recurrence was 2.6% (0.9%−4.4%) in ZD patients and 0% in patients with epiphrenic diverticula. Pooled rates of adverse events and severe adverse events were 10.6% (4.6%−16.6%) and 3.5% (0%−7.4%) in ZD and 8.4% (0%−16.8%) and 8.4% (0%−16.8%) in epiphrenic diverticula, respectively.
Conclusions:
POEM represents an effective and safe therapy for the treatment of esophageal diverticula.
Keywords: POEM, Septotomy, Endoscopy, Zenker
INTRODUCTION
Esophageal diverticula are rare structural abnormalities which account for <5% of all patients with dysphagia1. Zenker’s diverticulum (ZD) is the most common type of esophageal diverticula, with a reported prevalence ranging from 0.01 % to 0.11 %2, whereas diverticula located in the distal esophagus, called epiphrenic diverticula, are frequently associated with esophageal motility disorders and have an estimated prevalence of 0.015%3. Treatment is recommended for symptomatic patients as esophageal diverticula can lead to complications, such as aspiration and severe dysphagia. Surgical diverticulectomy with myotomy represents the standard surgical treatment, able to provide excellent results (symptom relief 85–100%)2,3, but with long operation times and high rates of adverse events, including leaks, pulmonary complications, and 0–7% risk of mortality2,3.
Direct flexible endoscopic septotomy has been routinely practiced but carries a relatively high recurrence rate due to incomplete division of the septum4. On the other hand, submucosal tunneling septotomy by diverticular peroral endoscopic myotomy (D-POEM) was introduced several years ago. It is performed using a submucosal tunneling approach and, thus, allows complete septum division5. Recently this technique was used effectively for septotomy in patients with Zenker’s6,7 (where it is called Z-POEM) and epiphrenic diverticula8. D-POEM has the potential advantage of allowing a complete septotomy to be performed in a single session and thus potentially reducing recurrence rates.
Given the increasing number of studies testing POEM in patients with esophageal diverticula, there is a pressing need to systematically revise the available body of evidence in this field; hence, we performed a meta-analysis to provide a pooled estimate of the efficacy and safety profile of D-POEM. As a secondary analysis, we examined the comparative efficacy of D-POEM with respect to standard flexible endoscopic treatments.
METHODS
Selection Criteria
The literature search strategy was based on the following inclusion criteria: (1) observational or cohort studies assessing POEM in adult patients with esophageal diverticula; (2) studies published in English; (3) articles reporting treatment success. Small case series <5 patients, non-endoscopic studies, review articles, animal models, and studies not reporting separately subgroup data according to diverticulum location were excluded.
Search Strategy
Literature search was conducted on PubMed, EMBASE, Cochrane Library, and Google Scholar including all studies fulfilling the inclusion criteria published through August 2020, based on the string “Search ((POEM) AND Zenker) OR Esophageal diverticula”.
Relevant reviews and meta-analyses in the field were examined for potential additional suitable studies. Authors of included studies and conference abstracts were contacted to obtain full text or further information when needed. Manual search on the proceedings of the main international endoscopic and gastroenterological conferences was also performed.
Data extraction was performed by 2 authors (AF and YI) and the quality of included studies was rated by 2 reviewers independently (AF and YI) based on the Newcastle-Ottawa scale for non-randomized studies9. Disagreements were solved by discussion and after a third opinion (MAK).
Outcomes Assessed
The primary efficacy outcome was treatment success, defined based on decrease of Eckardt score (which measures symptom severity for dysphagia, regurgitation, retrosternal pain and weight loss)10 to ≤3 in 3 studies11,12,22, decrease of Dakkak and Bennett score (0, no dysphagia; 1, dysphagia to solids; 2, dysphagia to semisolids; 3, dysphagia to liquids; 4, complete dysphagia)13 to 0 or 1 in 5 studies14–19, improvement of dysphagia in 1 study8, not specified in other 2 series20,21. Secondary outcomes included technical success, recurrence, procedural times, length of hospital stay, and safety profile.
Statistical Analysis
Study outcomes were pooled separately according to diverticulum location (Zenker’s versus epiphrenic) through a random-effects model based on DerSimonian and Laird test, and results were expressed as rates and 95% confidence interval (CI).
The presence of heterogeneity was calculated through I2 tests with I2<20% and interpreted as low-level and I2 between 20% to 50% as moderate heterogeneity. Any potential publication bias was verified through visual assessment of funnel plots. Sensitivity analysis was conducted in the subset of ZD patients restricted to (1) high quality studies, (2) prospective studies, and (3) according to study location (East versus West). A further sensitivity analysis was performed restricted only to studies with standard Z-POEM.
Subgroup analysis of the primary outcome (treatment success) concerning ZD patients was performed based on timing of response assessment (3 months versus 1 year versus >1 year). In order to explore the impact of diverticulum size, timing of response assessment, and prior treatments on the primary endpoint, a meta-regression model was built based on a stepwise backward approach23.
All pooled analyses were conducted using OpenMeta[Analyst] software whereas R 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria), metafor package24 was used for meta-regression. For all calculations a 2-tailed P value of less than 0.05 was considered statistically significant.
RESULTS
Studies
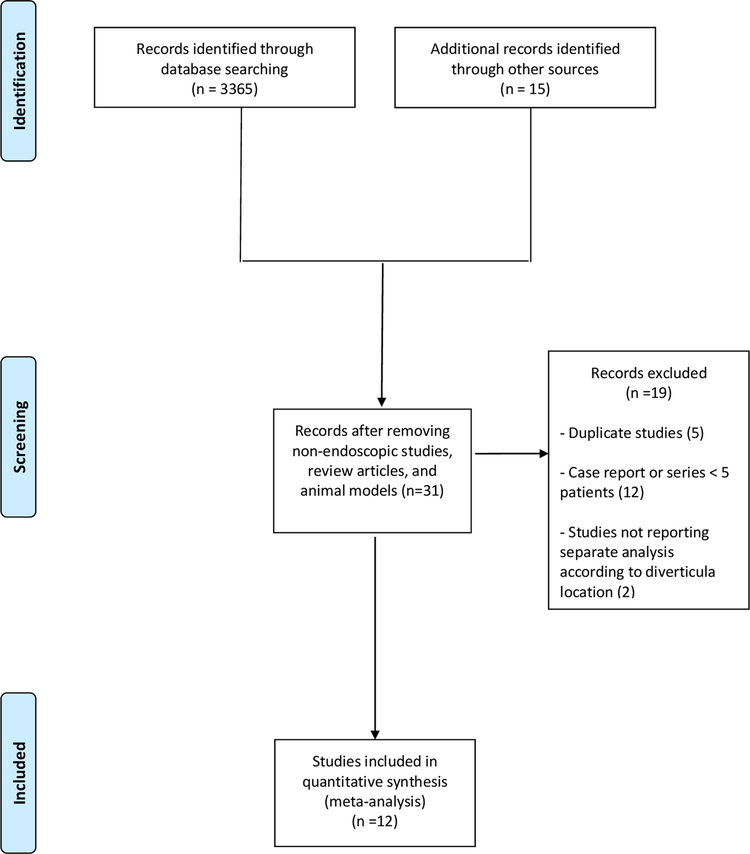
As shown in Figure 1, of 3380 studies initially identified, after exclusion of articles not fulfilling the inclusion criteria, 12 studies8,11,12,14–22 with 300 patients treated with POEM were included in the meta-analysis. Of 12 included studies, 4 were retrospective case-control studies comparing POEM to flexible endoscopic treatment14,19–21, 7 were retrospective single-cohort series8,11,12,15,16,18,22 and one was a prospective series17.
Figure 1.
Flow chart of the included studies
The main characteristics of the included studies were reported in Table 1. The recruitment period ranged from 2013 to 2020. Four studies were conducted in Asia12,20–22 and the 4 comparative studies14,19–21 presented 2 well-balanced cohorts in terms of baseline patients characteristics. Three studies were published as conference abstracts14,20,21. Seven studies tested POEM in patients with Zenker’s diverticula14,16–21, 4 studies in epiphrenic diverticula8,11,12,22, a single study included patients with different diverticulum locations15. The majority of treated patients were male and mean diverticulum size ranged from 1.75 to 6.07 cm.
Table 1.
Characteristics of included studies
| Study | Country; study period | Sample size; Diverticulum location | Control group (sample size) | Age years | Gender male | Diverticular size (cm) | Symptoms; baseline score | Prior treatments | Technique; sedation | Definition of treatment success; timing of assessment |
|---|---|---|---|---|---|---|---|---|---|---|
| Al Ghamdi 202014a | USA/France/Romania/Mexico; 2016–2019 | 91; Zenker | Flexible and rigid endoscopic septomyotomy (67) | 71 | 86 (54.4%) | 3 | Dysphagia in 63% regurgitation in 34%; Dakkak and Bennett: 1.7±0.9 |
No | Z-POEM; NR | Dakkak and Bennett ≤1; 3 months |
| Aslan 2019 20a | Turkey; 2015–2018 | 9; Zenker | Flexible endoscopic septomyotomy (20) | NR | NR | NR | NR | No | Z-POEM; NR | NR |
| Basile 20208 | France; 2017–2018 | 7; Epiphrenic | No | From 62 to 90 | 3 (42.8%) | NR | all pts dysphagia, 3 pts retrosternal pain, 4 regurgitation, 1 dyspnea, 5 weigh loss; NR | 2 pts (28.5%) POEM; 1 pt (14.2%) botulin injection | POEM + diverticular septotomy; general anaesthesia | Complete or partial regression of dysphagia; 3 months |
| Demeter 202011 | Slovakia; 2015–2018 | 7; Epiphrenic |
No | 67 (43–77) | 3 (42.8%) | 6.07±2 | Regurgitation the most common, dysphagia and pain; Eckardt: 6.6 (5–9) | PD in 1 patient, surgical diverticulectomy in 1 patient | POEM; general anaesthesia | Eckard score <3; 3 months and 2 years |
| Desai 201921a | India; 2013–2018 | 7; Zenker | Flexible endoscopic septomyotomy (8) | 71.4 (67–81) | 9 (60%) | NR | Dysphagia in 78.6%; NR | No | Z-POEM; NR | NR; 18 months |
| Kinoshita 202022 | Japan; 2015–2018 | 14; Epiphrenic | No | 72.5 (46–85) | 8 (57.1%) | 2.65 (0.9–9) | NR; Eckardt: 5 (3–11) | PD in 3 pts (21.4%) | POEM; general anaesthesia | NR; 3 months and 1 year |
| Klingler 202019 | USA; 2015–2020 | 19; Zenker | Flexible endoscopic septomyotomy (7) | 75 (72.5–82) | 13 (68.4%) | 2.6 (2–3.85) | Dysphagia in 100%, Regurgitation in 52.9%, Aspiration in 21%; Dakkak and Bennet 1.74±0.87 | No | Z-POEM; general anaesthesia | Dakkak and Bennett ≤1; 2 years |
| Li 201912 | China; 2016–2017 | 8; Epiphrenic | No | 66.25±7.17 | 5 (62.5%) | From 2.5 to 6.9 | NR; Eckardt: 6.88±3.04 | No | POEM + diverticular septotomy; deep sedation | Eckardt score <3; 1 year |
| Yang 201915 | USA/China; 2014–2017 | 11; 7 pts Zenker, 1 mid and 3 epiphrenic | No | 76.2±11.7 | 4 (36.3%) | 3.45±1.65 | dysphagia in 9 pts (81.8%), regurgitation in 2 pts (18.2%); Dakkak and Bennett: 2.7 | Surgery in 1 pt (9%) with Zenker’s diverticulum | Z-POEM in patients with Zenker’s diverticula and POEM+diverticular septotomy in patients with epiphrenic diverticula; general anaesthesia | Dakkak and Bennet ≤1; 3 months |
| Yang 202016 | Multicenter; 2014–2018 | 75; Zenker | No | 73.3±1.2 | 42 (56%) | 3.13±0.16 | dysphagia in all pts, regurgitation in 37 pts (49.3%); Dakkak and Bennett: 1.96±0.68 | Surgery in 5 pts (6.7%), endoscopic septotomy in 6 pts (8%) | Z-POEM; general anaesthesia | Dakkak and Bennet ≤1; 2 years |
| Repici 202017* | Italy; 2017–2019 | 20; short-septum Zenker | No | 67.9±14.3 | 12 (60%) | 1.75 | dysphagia in all pts, regurgitation in 12 pts (60%); Dakkak and Bennett: 2.7±0.5 |
No | POES; deep sedation | Dakkak and Bennet ≤1; 1 year |
| Sanaei 202018 | USA/India; Romania; Mexico; 2015–2019 | 32; Zenker | No | 72±11.4 | 19 (59.4%) | 2.94 (1–6.5) | dysphagia in all pts, regurgitation in 17 pts (53.1%); Dakkak and Bennett: 2 (1–2) |
100%: surgery in 10 pts (31.3%), rigid endoscopy in 9 pts (28.1%), flexible endoscopy in 13 pts (40.6%), Z-POEM in 3 pts (9.4%), botulin injection in 1 pt (3.1%) | Z-POEM in 28 pts (87.5%); hybrid in 2 pts (6.25%); standard septotomy in 2 pts who failed Z-POEM; general anaesthesia | Dakkak and Bennet ≤1; 6 months |
Data are reported as absolute numbers (percentages) or mean (± standard deviation or with range)
Study published as conference abstract
Prospective study
Abbreviations: NR, Not Reported; PD, Pneumatic Dilation; POEM, Per-Oral Endoscopic Myotomy; POES, Per-Oral Endoscopic Septotomy.
Among the studies conducted in patients with epiphrenic diverticula, three studies used POEM with septum division8,12,15 and two studies used POEM alone (hence with diverticulum left intact)11,22. On the other hand, patients with Zenker’s diverticula were treated with Z-POEM (septotomy of Zenker’s diverticula by diverticular peroral endoscopic myotomy) in all of the included studies except the series by Repici et al17 where a variant of Z-POEM with short mucosotomy (peroral endoscopic septotomy [POES]) was performed.
Six studies included only patients not previously treated for esophageal diverticula [12,14,17,19–21], five studies included 4% to 28% of patients with prior treatments8,11,15,16,22, and 1 cohort included only patients with previous treatments18. Most of the patients with epiphrenic diverticula were affected by achalasia.
Quality was deemed moderate to high in 9 studies8,11,12,15–19,22 whereas 3 studies14,20,21 were rated as low-quality articles mainly due to incomplete outcome reporting.
Details on the quality assessment of the included articles are shown in Supplementary Table 1.
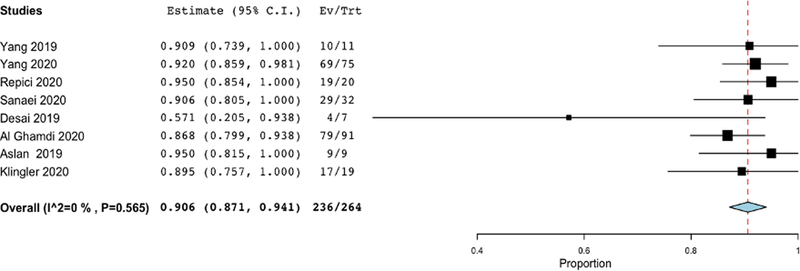
Treatment success in ZD patients
As depicted in Figure 2, pooled rate of treatment success with POEM in patients with Zenker’s diverticula was 90.6% (87.1%−94.1%), with no evidence of heterogeneity (I2=0%). Rates of treatment success observed at 3 months (130 patients, 90.6%, 85.7%−95.5%) were maintained at 1 year (72 patients, 90%, 86.4%−97.4%) and 2 years (101 patients, 89.6%, 82.2%−96.9%; Table 2).
Figure 2. Pooled analysis of treatment success with POEM in patients with Zenker’s diverticula.
Pooled rate of treatment success with POEM in patients with Zenker’s diverticula was 90.6% (87.1%−94.1%), with no evidence of heterogeneity (I2=0%).
Table 2.
Subgroup analysis of treatment success in patients with Zenker’s diverticula. Subgroup analysis was performed based on timing of response assessment (3 months versus 1 year versus 2 years).
| Variable | Subgroup | No. of Cohorts | No. of patients | Summary Estimate (95% CI) | Within-group heterogeneity (I2) |
|---|---|---|---|---|---|
| Treatment success | |||||
| Timing of assessment | 3 months | 5 | 130 | 90.6% (85.7%–95.5%) | 0% |
| 1 year | 4 | 72 | 90% (86.4%–97.4%) | 0% | |
| 2 years | 3 | 101 | 89.6% (82.2%–96.9%) | 15.7% | |
Abbreviation: CI, Confidence Interval.
The aforementioned findings were confirmed in sensitivity analysis restricted to high quality studies, prospective series, and according to study location (Supplementary Table 2). Furthermore, sensitivity analysis restricted to studies using standard Z-POEM (hence by excluding the study by Repici et al17 where POES was used) also confirmed the results of the main analysis (pooled success rate 89.8%, 85.9%−93.8%; Supplementary Table 2).
The kinetics of symptomatic scores in treated patients is reported in the Supplementary Figure 1. In patients with ZD, mean Dakkak and Bennett score decreased from 2.18 (1.78–2.57) at baseline to 0.04 (0–0.14) at 6 months and 0.26 (0.15–0.36) at 1 year (Supplementary Figure 1a).
Meta-regression aiming to correlate several baseline variables to the primary outcome did not find any significant impact of prior treatments, timing of response assessment, and diverticulum size on treatment success (Supplementary Table 3).
In particular, as reported in the Supplementary Figure 2, there was no correlation between the proportion of patient with previous treatments (Supplementary Figure 2a) and mean diverticular size (Supplementary Figure 2b) with treatment success. No evidence of publication bias was observed through visual inspection of the funnel plot (Supplementary Figure 3a).
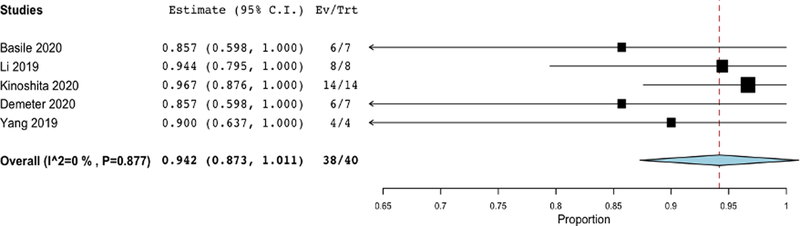
Treatment success in patients with epiphrenic diverticula
As reported in Figure 3 and Table 2, pooled rate of treatment success with POEM in patients with epiphrenic diverticula was 94.2% (87.3%−100%), again with no evidence of heterogeneity (I2=0%). Subgroup analysis showed 91.8% (80.2%−100%) pooled success in patients treated with POEM with septum division and 95.5% (86.9%−100%) efficacy in patients treated with POEM alone. Mean Eckardt score in patients with epiphrenic diverticula and achalasia decreased from 8.38 (2.17–14.6) at baseline to 2.54 (0–7.54) at 6 months and 1.51 (0–3.82) at 1 year (Supplementary Figure 1b).
Figure 3. Pooled analysis of treatment success with POEM in patients with epiphrenic diverticula.
Pooled rate of treatment success with POEM in patients with epiphrenic diverticula was 94.2% (87.3%−100%), with no evidence of heterogeneity (I2=0%).
As above reported in ZD patients, also in patients with epiphrenic diverticula meta-regression aiming to correlate several baseline variables to the primary outcome did not find any significant correlation of baseline variables with treatment success (Supplementary Table 3).
No evidence of publication bias was observed through visual inspection of the funnel plot (Supplementary Figure 3b).
Secondary outcomes
Secondary efficacy outcomes are reported in Table 3.
Table 3.
Other outcomes reported stratified according to diverticulum location (Zenker’s versus epiphrenic)
| Outcome | Subgroup | No. of Cohorts | No. of patients | Summary Estimate (95% CI) | Within-group heterogeneity (I2) |
|---|---|---|---|---|---|
| Technical success | Zenker’s | 8 | 260 | 95.9% (93.4%–98.3%) | 0% |
| Epiphrenic | 5 | 40 | 95.1% (88.8%–100%) | 0% | |
| Symptoms recurrence | Zenker’s | 8 | 260 | 2.6% (0.9%–4.4%) | 0% |
| Epiphrenic | 5 | 40 | 0% | 0% | |
| Adverse events | Zenker’s | 8 | 260 | 10.6% (4.6%–16.6%) | 47.2% |
| Epiphrenic | 5 | 40 | 8.4% (0%–16.8%) | 0% | |
| Severe adverse events | Zenker’s | 8 | 260 | 3.5% (0%–7.4%) | 62.3% |
| Epiphrenic | 5 | 40 | 8.4% (0.1%–16.8%) | 0% | |
| Procedure time | Zenker’s | 7 | 233 | 44.7 min (30.03–59.4) | 45% |
| Epiphrenic | 2 | 33 | 61.7 min (38.4–84.9) | 41% | |
| Length of hospital stay | Zenker’s | 7 | 233 | 1.23 days (1–1.4) | 48% |
| Epiphrenic | 2 | 33 | 5.6 days (4.8–6.4) | 44.3% |
Abbreviation: CI, Confidence Interval.
Technical success:
Pooled rate of technical success was 95.9%, (93.4%−98.3%) in ZD patients and 95.1% (88.8%−100%) in patients with epiphrenic diverticula.
Symptoms recurrence:
Mean follow-up length was 15±3 months in ZD patients and 10.5±5 months in patients with epiphrenic diverticula. Pooled rate of symptom recurrence was 2.6% (0.9%−4.4%) in ZD patients and 0% in patients with epiphrenic diverticula.
Procedure time:
Procedure time in patients with epiphrenic diverticula was 61.7 minutes (38.4–84.9) whereas it was 44.7 minutes (30–59.4) in ZD patients.
Length of hospital stay:
Length of hospital stay was 5.6 days (4.8–6.4) in patients with epiphrenic diverticula and 1.2 days (1–1.1) in ZD patients.
Safety profile:
Pooled rate of adverse events was 7.6% (4.1%−11.1%) in the overall cohort, in particular it was 10.6% (4.6%−16.6%) in ZD patients and 8.4% (0%−16.8%) in patients with epiphrenic diverticula. Overall pooled rate of serious adverse events was 3.5% (0%−7.4%) in ZD patients and 8.4% (0%−16.8%) in patients with epiphrenic diverticula. The adverse events observed in the included studies are detailed in Supplementary Table 4. Perforation represented the most frequent complication, followed by bleeding. Two studies did not specify the adverse events registered14,21.
DISCUSSION
Surgery and standard flexible endoscopic treatment represent the most frequent therapeutic strategies in patients with esophageal diverticula. In recent years, POEM, a minimally invasive procedure used to treat esophageal disorders such as achalasia25, has emerged as an endoscopic therapy for esophageal diverticula, termed D-POEM.
Previous meta-analyses explored this important issue but with several limitations, such as very low number of studies (particularly focused on ZD patients), lack of long-term outcomes, and limited assessment of the impact of potentially confounding factors on treatment outcomes through adequate statistical methods26,27.
Through a meta-analysis of 12 studies, we made several key observations about the clinical role of POEM in patients with esophageal diverticula. First, POEM resulted in very high rates of treatment success (beyond 90%) both in patient with Zenker’s and epiphrenic diverticula. These favorable outcomes were maintained over time even at 2 years from treatment and rate of symptom recurrence was very low (2.6% in ZD patients and 0% in subjects with epiphrenic diverticula). In meta-regression analysis, treatment outcomes were maintained regardless of diverticulum size and prior treatments. Further, the rate of technical success was over 95% for both Zenker’s and epiphrenic diverticula. Second, POEM showed a promising safety profile, with only 7.6% and 3.3% of overall and serious adverse events, respectively. Thus, findings of this meta-analysis support that POEM is a valuable alternative treatment option for esophageal diverticula, and seems to provide equal if not better outcomes with supposed shorter hospital stay and lower rates of complications compared to standard endoscopic techniques.
ZD is commonly treated through flexible endoscopy diverticulotomy. In a recent meta-analysis, flexible endoscopic treatment had a favorable pooled success rate of 91% in ZD patients28. However, recurrence rate following flexible endoscopic diverticulotomy was 11.3% and adverse event rate was 11%, both higher than that reported with Z-POEM28. Results of our meta-analysis seem considerably more favorable in particular in terms of decreased recurrence rates while adverse events, although with a similar rate as in standard procedures, were mainly mild with no serious impact on patient outcomes.
Several approaches and techniques have been suggested for POEM. The endoluminal functional lumen imaging probe (EndoFLIP) was devised as a method for evaluating the pathogenesis and distensibility of the EGJ. EGJ distensibility can be expressed as the distensibility index (DI) and represents the degree of impaired LES relaxation.29 During POEM, some endoscopist uses EndoFLIP as a means to acquring information on the efficacy of the intervention.30 Yoo et al. reported that posttreatment DI by EndoFLIP was useful for predicting POEM clinical outcomes in patients with achalasia.31 However, while Endoflip technology shows promise, there remains debate on the most appropriate timing for using Endoflip (i.e. follow-up) as well as the selection of appropriate patients; as a result more research is needed.29,30Less is known regarding the use of EndoFLIP in patients with esophageal diverticula.
Optical coherence tomography (OCT) is another emerging technique used by endoscopists during POEM. Desai et al. evaluated the utility of OCT in providing pre-POEM esophageal information such as the degree of vascularity and thickness of the circular muscular layer.32 Using this data, an approach such as anterior or posterior myotomy could be undertaken. To this end, the authors enrolled 84 patients of which 51patients underwent pre-POEM OCT. Using OCT esophageal data, 24 (47 %) of patients underwent anterior POEM while 27 (53 %) underwent posterior POEM. Technical success was achieved in 96 % of patients. The authors also noted that there were significantly less bleeding in patients who had OCT vs those who did not [4 (8 %) vs. 14 (43 %), p = 0.0001]. Procedure was also signifiantly less in the OCT group compared with controls (85.8 vs. 121.7 min, p = 0.000097). While OCT shows promising results, this technology is less available to endoscopists and studies are very sparse to make any concrete recomendations.
POEM consists of 4 consecutive steps: (1) mucosal incision for entry into the submucosa, (2) submucosal tunneling, (3) myotomy, and (4) closure of the mucosal entry. Prior to the procedure, a high-definition gastroscope is commonly fitted with a cap to aid in scarping off residual and adherent tissue on the esophageal mucosa. Anecdotal reports suggest securing the cap on the endoscope tip with tape to avoid dislodging the cap within the submucosal tunnel.33
While myotomy remains the core procedure for POEM, there are debatable concerns regarding the optimal orientation, depth, and length in performing a myotomy. For achalasia types I or II, a 6–8-cm-long myotomy is generally recommended, while a longer myotomy is recommended for type III achalasia.34 Previously, Wang et al. reported 46 achalasia patients who received short myotomy (mean, 5.4 cm) which showed excellent short-term (3 months) outcomes.35 Recently, Nabi et al reported a randomized trial comparing outcomes of short (3 cm, n = 34) versus long (6 cm and above, n = 37) esophageal myotomy in patients undergoing POEM for type I and II achalasia.36 Clinical success was comparable in both groups at 1 year. The mean operative time was shorter in the short myotomy group than in the long myotomy group (44.03 ± 13.78 and 72.43 ± 27.28 minutes, respectively; P < 0.001). No difference in adverse events was observed between both groups. Overall, the results indicate that a long esophageal myotomy was not superior to short myotomy for type I and II achalasia patients.
This technique has been adopted for treating esophageal diverticula which is essentially a septotomy of the diverticulum using the POEM technique. The technique reveals the septal wall following submucosal tunneling which is completely dissected to the base of the diverticula while the myotomy is extended about 1 cm proximally.37 In cases of esophageal outflow obstruction, the myotomy is extended about 2 to 3 cm beyond the gastroesophageal junction to allow complete dissection of the lower esophageal sphincter.37 Finally, clips are applied to close the mucosal entry site.
Different cutting devices are available and used by endoscopists depending on their training and experience such as needle-knife, hook-knife, monopolar forceps, argon plasma coagulation.38 The most frequently used device is the hook knife and the needle knife (Olympus medical, Tokyo, Japan).38 While variations exists among endoscopic technique, there are no randomized control trials.
The POEM procedure can be performed via a so-called “anterior” approach or “posterior” approach. Anterior myotomy involves performing POEM at the 1- to 2-o’clock position with patients in the supine position; posterior myotomy is performed at the 5- to 6-o’clock position.39,40 Theoretically, anterior myotomy may reduce the risk of damage to the angle of His and the sling muscle fibers located over the greater curvature, which support the natural antireflux mechanism.39,40 The posterior approach, on the other hand, may allow for superior alignment of the endoscopic tools used to perform the myotomy, as the working channel for most endoscopes is located over the 5- or 7-o’clock position.39,40 The posterior myotomy approach may risk damage to the sling muscles that are located around the 8-o’clock area and thereby disrupt the natural antireflux mechanism.39,40 A recent meta-analysis of 1247 patients from 18 studies (623 patients (11 cohorts) treated via anterior myotomy and 624 patients (12 cohorts) treated via posterior myotomy) demonstrated comparable outcomes in terms of clinical success, GERD, and adverse events.41 However, total procedure time with posterior myotomy is shorter than with anterior myotomy.
Selective circular myotomy or full-thickness myotomy could also be performed during the procedure.42 For selective myotomy, it is more technically difficult than full-thickness myotomy with longer learning curves.43 The increase in operation time for patients with selective myotomy also leads to increased risk in severe gas-related complications.43 Li et al. retrospectively reported a series of 234 patients who underwent full thickness myotomy (n=103) and selective inner circular myotomy (n=131).44 No significant difference was noted in regards to clinical reflux, treatment scores or LES pressures between both groups. Full thickness myotomy was associated with a shorter procedure time. Similar findings have been noted in other reports.45 Additionally, based on an international survey of endoscopist who perform POEM, some operators are still in favor of selective myotomy.46
Epiphrenic diverticula are traditionally repaired through a laparoscopic thoracotomy approach. Prior meta-analysis reports an efficacy rate of 88.5% of surgical treatment of epiphrenic diverticula, which is lower than the pooled efficacy rate of 94.2% in this meta-analysis of POEM for epiphrenic diverticula.47 Moreover, the prior meta-analysis reported a staggering 21% morbidity rate following surgical treatment of epiphrenic diverticula.47 Therefore, surgical epiphrenic diverticulectomy is a challenging procedure with long operation time and high postoperative complication rates; in this context, an effective and safe endoscopic approach such as POEM could represent a valuable option in this setting although head-to-head series directly comparing surgical versus endoscopic treatment are lacking and it would be probably very difficult to conduct such a study in the clinical scenario.
Post-op care for POEM varies according to institutional practice. Post-operatively patients are usually given fluids and progress to soft foods within 24 hours. Some centers perform a contrast swallow study but this test is not often performed unless concerns for mucosal breach are present.48 However, other endoscopists recommend a swallow study with fluoroscopy inspite of any clinical symptoms.49 Diet is advanced to soft following 48 hours and continued for 10 to 14 days before regular foods can be consumed.49
Additionally, some operators recommend a course of intravenous antibiotics which is stopped on post-op day 3 while oral antibiotics is continue for a total of 7 days.49 However, Maselli et al. conducted a very recent randomized clinical trial comparing single dose versus short course of antibiotics in patients undergoing POEM.50 The study reported that a single dose of a cefazolin-based prophylaxis without the need for prolonged antibiotic exposure was sufficient for patients undergoing POEM procedures due to a very low residual infectivity risk.
There are certain limitations to this study. First, the low number of included studies and enrolled patients requires particular caution in interpreting our findings, in particular concerning patients with epiphrenic diverticula. However, we deliberately decided to restrict inclusion criteria to series with at least 5 patients, thus excluding small case reports, to provide more robust and homogenous outcome estimates. Second, the very limited number of comparative studies and the lack of randomized trials did not enable us to conduct a direct comparison between POEM and flexible endoscopic techniques.
Third, evaluation of long-term (beyond 2 years) outcomes and the assessment of other potential complications of POEM, such as the incidence of gastro-esophageal reflux disease (GERD) in the case of epiphrenic diverticula, were not feasible due to the lack of available data. Fourth, techniques used in the included studies were not homogeneous with some differences (Z-POEM versus POES in Zenker’s diverticula patients and POEM + septotomy versus POEM alone in epiphrenic diverticula patients). However, multiple sensitivity analyses considering these technical features were performed, confirming the results of the main analysis. Finally, economic considerations and assumptions on the impact of POEM were beyond the scope of the study. These limitations highlight the opportunity for future work in this field including well designed head-to-head trials to compare POEM to standard techniques.
Furthermore, we fully acknowledge the recent publication of two meta-analyses in this field.51,52 However, these studies had significant limitations which we overcame, thus making our analysis novel and of interest. The meta-analysis by Kamal et al included only 7 studies (of which only 5 published as full text papers) whereas our analysis includes 12 studies with nearly double the number of patients.51 Moreover, Kamal et al did not perform an analysis at different time points so the kinetics and magnitude of patient response over time could not be assessed. Additionally, meta-regression analysis of main potential confounders was not performed. We think that these aspects were adequately considered in our manuscript (including meta-regression) and constitute important sources of novelty. The other meta-analysis by Ren et al. although being conducted with a more rigorous approach, also did not report specific time points or subclassification according to type of diverticula.52 These are two important limitations completely expanded in our analysis.
In conclusion, this meta-analysis highlights that POEM is a safe and effective technique in patients with esophageal diverticula, including both ZD and epiphrenic diverticula. These data seem similarly effective to standard surgical and flexible endoscopic techniques, but with lower complication rates with POEM. Therefore, patients with esophageal diverticula should be offered a POEM approach among standard techniques, if the appropriate expertise is available.
Supplementary Material
Acknowledgments
Disclosures:
AF, YI, VA: None
MAK: Consultant for BSCI, Medtronic, Olympus and GI Supply.
RY: Consultant: Medtronic, Ironwood Pharmaceuticals, Diversatek; Research support: Ironwood Pharmaceuticals; Advisory Board: Phatom Pharmaceuticals
SW: Consultant for Boston Scientific, Medtronic, Interpace, Cernostics. Supported by the Department of Medicine Outstanding Early Scholars Program
References:
- 1.Sato H, Takeuchi M, Hashimoto S, et al. Esophageal diverticulum: New perspectives in the era of minimally invasive endoscopic treatment. World J Gastroenterol. 2019;25(12):1457–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herbella FA, Patti MG. Modern pathophysiology and treatment of esophageal diverticula. Langenbeck Arch Surg 2012; 397: 29–35 [DOI] [PubMed] [Google Scholar]
- 3.Zaninotto G, Portale G, Costantini M, et al. Therapeutic strategies for epiphrenic diverticula: systematic review. World J Surg 2011;35(7):1447–53 [DOI] [PubMed] [Google Scholar]
- 4.Sakai P Endoscopic myotomy of Zenker’s diverticulum:lessons from 3 decades of experience. Gastrointest Endosc 2016; 83: 774–5 [DOI] [PubMed] [Google Scholar]
- 5.Li QL, Chen WF, Zhang XC, et al. Submucosal tunneling endoscopic septum division: A novel technique for treating Zenker’s diverticulum. Gastroenterology 2016; 151: 1071–4 [DOI] [PubMed] [Google Scholar]
- 6.Hernandez Mondragon OV, Solorzano Pineda MO, Blancas Valencia JM. Zenkerʼs diverticulum: Submucosal tunneling endoscopic septum division (Z-POEM). Dig Endosc 2018; 30:124. [DOI] [PubMed] [Google Scholar]
- 7.Costamagna G, Iacopini F, Bizzotto A, et al. Prognostic variables for the clinical success of flexible endoscopic septotomy of Zenkerʼs diverticulum. Gastrointest Endosc 2016; 83: 765–73 [DOI] [PubMed] [Google Scholar]
- 8.Basile P, Gonzalez JM, Le Mouel JP, et al. Per-oral endoscopic myotomy with septotomy for the treatment of distal esophageal diverticula (D-POEM). Surg Endosc. 2020;34(5):2321–5. [DOI] [PubMed] [Google Scholar]
- 9.Wells GA, Shea B, O’Connell D, et al. The Newcastle – Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses; available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm, accessed on August 2020.
- 10.Eckardt VF. Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am. 2001;11(2):281–vi. [PubMed] [Google Scholar]
- 11.Demeter M, Ďuriček M, Vorčák M, et al. S-POEM in treatment of achalasia and esophageal epiphrenic diverticula - single center experience. Scand J Gastroenterol. 2020;55(4):509–14. [DOI] [PubMed] [Google Scholar]
- 12.Li X, Zhang W, Yang J, et al. Safety and efficacy of submucosal tunneling endoscopic septum division for epiphrenic diverticula. Endoscopy. 2019;51(12):1141–5. [DOI] [PubMed] [Google Scholar]
- 13.Dakkak M, Bennett JR. A new dysphagia score with objective validation. J Clin Gastroenterol 1992; 14: 99–100 [DOI] [PubMed] [Google Scholar]
- 14.Al Ghamdi SS, Farha J, Meybodi MA, et al. International multicenter study comparing Z-POEM and flexible/rigid endoscopic Zenker’s diverticulotomy. Gastrointest Endosc 2020;91(6):AB3–4. [Google Scholar]
- 15.Yang J, Zeng X, Yuan X, et al. An international study on the use of peroral endoscopic myotomy (POEM) in the management of esophageal diverticula: the first multicenter D-POEM experience. Endoscopy. 2019;51(4):346–9. [DOI] [PubMed] [Google Scholar]
- 16.Yang J, Novak S, Ujiki M, et al. An international study on the use of peroral endoscopic myotomy in the management of Zenker’s diverticulum. Gastrointest Endosc. 2020;91(1):163–8. [DOI] [PubMed] [Google Scholar]
- 17.Repici A, Spadaccini M, Belletrutti PJ, et al. Peroral endoscopic septotomy for short-septum Zenker’s diverticulum. Endoscopy. 2020;52(7):563–8. [DOI] [PubMed] [Google Scholar]
- 18.Sanaei O, Ichkhanian Y, Hernandez Mondragon OV, et al. Impact of Prior treatment on Feasibility and Outcomes of Zenker’s PerOral Endoscopic Myotomy (Z-POEM). Endoscopy 2020, in press. [DOI] [PubMed] [Google Scholar]
- 19.Klingler MJ, Landreneau JP, Strong AT, et al. Endoscopic mucosal incision and muscle interruption (MIMI) for the treatment of Zenker’s diverticulum. Surg Endosc 2020, in press. [DOI] [PubMed] [Google Scholar]
- 20.Aslan F, Yilmaz O, Sengun B, et al. A new technique in treatment of Zenker diverticulum: submucosal tunnelling endoscopic septum division (Z-POEM) versus classic endoscopic septomyotomy techeniques. Gastrointest Endosc 2019;89(6S):AB629. [Google Scholar]
- 21.Desai PN, Kabrawala MV. Submucosal tunnelling endoscopic septum division for Zenker’s diverticulum (Z POEM): a new emerging technique compared to conventional endoscopic septotomy. Gastrointest Endosc 2019;89(6S):AB450. [Google Scholar]
- 22.Kinoshita M, Tanaka S, Kawara F, et al. Peroral endoscopic myotomy alone is effective for esophageal motility disorders and esophageal epiphrenic diverticulum: a retrospective single-center study. Surg Endosc 2020, in press. [DOI] [PubMed] [Google Scholar]
- 23.Facciorusso A, Di Maso M, Muscatiello N. Drug-eluting beads versus conventional chemoembolization for the treatment of unresectable hepatocellular carcinoma: A meta-analysis. Dig Liver Dis. 2016;48(6):571–7. [DOI] [PubMed] [Google Scholar]
- 24.http://cran.r-project.org/web/packages/metafor/index.html [accessed August 2020].
- 25.Facciorusso A, Singh S, Abbas Fehmi SM, et al. Comparative efficacy of first-line therapeutic interventions for achalasia: a systematic review and network meta-analysis. Surg Endosc. 2020, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamal F, Khan MA, Lee-Smith W, et al. Peroral Endoscopic Myotomy Is a Safe and Feasible Option in Management of Esophageal Diverticula: Systematic Review and Meta-Analysis. Dig Dis Sci. 2020, in press. [DOI] [PubMed] [Google Scholar]
- 27.Ren L, Xie W, Mulmi Shrestha S, et al. Peroral ceroral endoscopic myotomy treatment for symptomatic esophageal diverticulum: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2020, in press. [DOI] [PubMed] [Google Scholar]
- 28.Ishaq S, Hassan C, Antonello A, et al. Flexible endoscopic treatment for Zenker’s diverticulum: a systematic review and meta-analysis. Gastrointest Endosc. 2016;83(6):1076–89. [DOI] [PubMed] [Google Scholar]
- 29.Kim GH. Is EndoFLIP Useful for Predicting Clinical Outcomes after Peroral Endoscopic Myotomy in Patients with Achalasia?. Gut liver. 2019;13(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weusten BL, Barret M, Bredenoord AJ, et al. Endoscopic management of gastrointestinal motility disorders–part 1: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020;52(06):498–515. [DOI] [PubMed] [Google Scholar]
- 31.Yoo IK, Choi SA, Kim WH, et al. Assessment of clinical outcomes after peroral endoscopic myotomy via esophageal distensibility measurements with the endoluminal functional lumen imaging probe. Gut Liver. 2019;13:32–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Desai AP, Tyberg A, Kedia P, et al. Optical coherence tomography (OCT) prior to peroral endoscopic myotomy (POEM) reduces procedural time and bleeding: a multicenter international collaborative study. Surg Endosc. 2016;30(11):5126–33. [DOI] [PubMed] [Google Scholar]
- 33.Kumbhari V, Khashab MA. Peroral endoscopic myotomy. World J Gastrointest Endosc. 2015;7(5):496–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kane ED, Budhraja V, Desilets DJ, Romanelli JR. Myotomy length informed by high-resolution esophageal manometry (HREM) results in improved per-oral endoscopic myotomy (POEM) outcomes for type III achalasia. Surg Endosc. 2019;33:886–894 [DOI] [PubMed] [Google Scholar]
- 35.Wang J, Tan N, Xiao Y, et al. Safety and efficacy of the modified peroral endoscopic myotomy with shorter myotomy for achalasia patients: a prospective study. Dis Esophagus. 2015;28:720–727 [DOI] [PubMed] [Google Scholar]
- 36.Nabi Z, Ramchandani M, Sayyed M, et al. Comparison of short versus long esophageal myotomy in cases with idiopathic achalasia: a randomized controlled trial. J Neurogastroenterol Motil. 2021;27:63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miutescu BP, Khan S, Mony S, Khashab MA. Role of Peroral Endoscopic Myotomy (POEM) in the Management of Esophageal Diverticula. Clin Endosc. 2020;53(6):646–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maselli R, Spadaccini M, Cappello A, et al. Flexible endoscopic treatment for Zenker’s diverticulum: from the lumen to the third space. Ann Gastroenterol. 2021;34(2):149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Inoue H, Minami H, Kobayashi Y et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010; 42: 265–271 [DOI] [PubMed] [Google Scholar]
- 40.Ren Z, Zhong Y, Zhou P et al. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc 2012; 26: 3267–3272 [DOI] [PubMed] [Google Scholar]
- 41.Mohan BP, Ofosu A, Chandan S, et al. Anterior versus posterior approach in peroral endoscopic myotomy (POEM): a systematic review and meta-analysis. Endoscopy. 2020;52(04):251–8. [DOI] [PubMed] [Google Scholar]
- 42.Bechara R, Ikeda H, Inoue H. Peroral endoscopic myotomy: an evolving treatment for achalasia. Nat Rev Gastroenterol Hepatol. 2015;12(7):410–26. [DOI] [PubMed] [Google Scholar]
- 43.Liu X, Yao L, Cheng J, et al. Landscape of Adverse Events Related to Peroral Endoscopic Myotomy in 3135 Patients and a Risk-Scoring System to Predict Major Adverse Events. Clin Gastroenterol Hepatol. 2021;S1542–3565(21)00467–5 [DOI] [PubMed] [Google Scholar]
- 44.Li QL, Chen WF, Zhou PH, et al. Peroral endoscopic myotomy for the treatment of achalasia: a clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg 2013;217(3):442–51. [DOI] [PubMed] [Google Scholar]
- 45.Li C, Gong A, Zhang J, et al. Clinical outcomes and safety of partial full-thickness myotomy versus circular muscle myotomy in peroral endoscopic myotomy for achalasia patients Gastroenterol Res Prac. 2017;2017:2676513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stavropoulos SN, Modayil RJ, Friedel D, Savides T. The international per oral endoscopic myotomy survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc. 2013;27(9):3322–38. [DOI] [PubMed] [Google Scholar]
- 47.Chan DSY, Foliaki A, Lewis WG, et al. Systematic Review and Meta-analysis of SurgicalTreatment of Non-Zenker’s Oesophageal Diverticula. J Gastrointest Surg. 2017;21(6):1067–1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Crosthwaite GL, Sejka M. Per-oral endoscopic myotomy (POEM): overview and experience of 100 cases by a single surgeon in Australia.. Ann Esophagus 2020;3:12. [Google Scholar]
- 49.Ahmed Y, Othman MO. Peroral endoscopic myotomy (POEM) for achalasia. J Thorac Dis. 2019. Aug;11(Suppl 12):S1618–S1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maselli R, Oliva A, Badalamenti M, Galtieri PA, et al. Single-dose versus short-course prophylactic antibiotics for peroral endoscopic myotomy: a randomized controlled trial. Gastrointest Endosc. 2021. Jun 10:S0016–5107(21)01418–8. doi: 10.1016/j.gie.2021.05.045. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 51.Kamal F, Khan MA, Lee-Smith W, et al. Peroral Endoscopic Myotomy Is a Safe and Feasible Option in Management of Esophageal Diverticula: Systematic Review and Meta-Analysis. Dig Dis Sci. 2020, doi: 10.1007/s10620-020-06678-5. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 52.Ren L, Xie W, Mulmi Shrestha S, et al. Peroral ceroral endoscopic myotomy treatment for symptomatic esophageal diverticulum: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2020, doi: 10.1097/MEG.0000000000002001. Epub ahead of print [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.