Abstract
It shows a pseudo ‐A‐V‐V‐A response after stopping overdrive atrial pacing of a broad complex tachycardia.

1. CASE PRESENTATION
A 27‐year‐old‐woman with frequent episodes of palpitations and a documented history of broad complex tachycardia was referred for an electrophysiological study and radiofrequency ablation. A baseline 12‐lead electrocardiogram showed normal sinus rhythm without any obvious preexcitation (Figure 1A). History, physical examination, and echocardiography did not demonstrate any significant abnormality.
FIGURE 1.
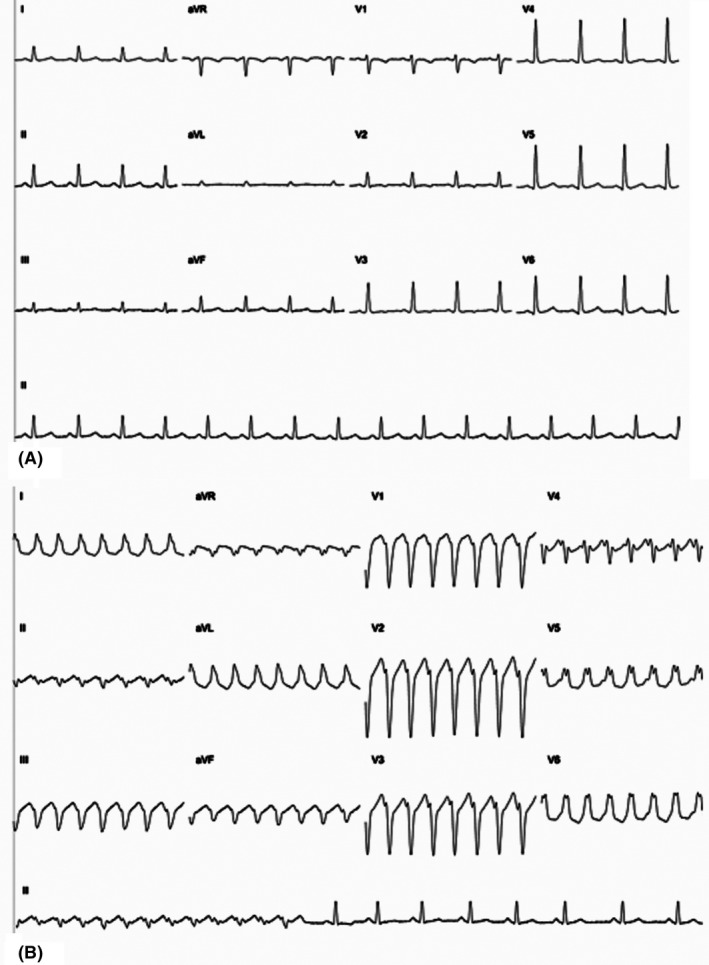
A, 12‐lead electrocardiogram during sinus rhythm. B, 12‐lead electrocardiogram during the arrhythmia
At baseline electrophysiologic study, atrio‐His (AH) and His‐ventricular (HV) intervals were 70 and 39 ms, respectively.
Incremental ventricular stimulation showed concentric decremental retrograde conduction, and VA Wenckebach at a paced cycle length (CL) of 280 ms.
Incremental atrial pacing did not reveal any preexcitation and induced a broad complex tachycardia with LBBB morphology, left superior axis, QRS duration of 160 ms, and cycle length of 280 ms (Figure 1B). Intracardiac signals showed one to one ventriculoatrial (VA) association with a VA interval of 108 ms. The atrial activation sequence was identical to that seen during ventricular pacing with no clearly visible His signal before the QRS. The arrhythmia terminated spontaneously with reappearance of His signal before QRS (Figure 2A).
FIGURE 2.
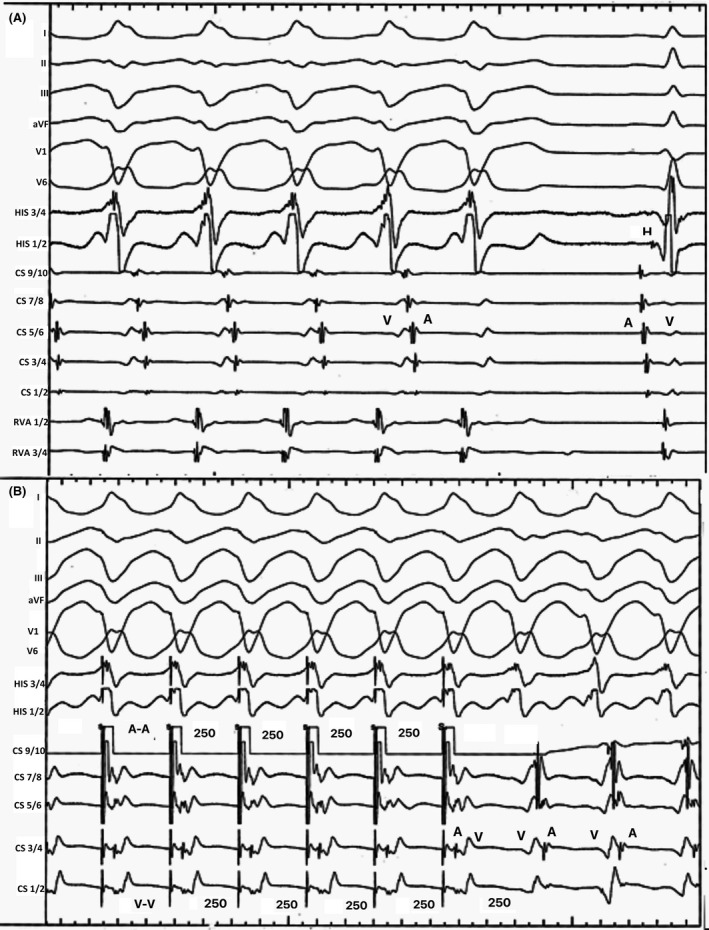
A, Intracardiac electrograms during the arrhythmia and after its termination. B, Atrial overdrive pacing during the arrhythmia at a pacing cycle length of 250 ms and the intracardiac electrograms after the cessation of pacing. A, atrial; H, his; V, ventricular
Programmed atrial extrastimulation demonstrated dual atrioventricular (AV) nodal physiology and then induced the same broad complex tachycardia.
During sustained arrhythmia, the delivery of a His‐refractory ventricular extra stimulus did not affect the atrial cycle length. Ventricular (RV apex) overdrive pacing at a CL of 260 ms resulted in a ventricular‐atrial‐ventricular response upon cessation of pacing, resumption of the arrhythmia, and post‐pacing interval of 300 ms.
Atrial overdrive pacing during sustained arrhythmia at a pacing CL of 250 ms resulted in acceleration of the arrythmia with no change in the ventricular activation sequence or QRS morphology. An atrial‐ventricular‐ventricular‐atrial response was observed upon cessation of pacing with resumption of the arrhythmia (Figure 2B).
What is this tachycardia?
The differential diagnosis of this broad complex tachycardia includes ventricular tachycardia in a normal heart, bundle branch reentrant tachycardia, supraventricular tachycardia with aberrant conduction, or supraventricular tachycardia using an accessory pathway.
Supraventricular tachycardia with aberrant conduction and bundle branch reentrant tachycardia can be excluded as the HV interval is normal in sinus rhythm and very short during the arrhythmia.
Atrial overdrive pacing at a cycle length of 20–40 ms shorter than the arrhythmia is a useful manoeuvrer to distinguish ventricular tachycardia from supraventricular arrhythmias. After confirming atrial capture with resetting of the arrhythmia, the activation sequence must next be assessed. If atrial overdrive pacing causes the ventricular rate to increase to that of the atrial rate, with a change in activation sequence, ventricular tachycardia must be considered as the most likely possibility.
The electrogram sequence then needs to be reviewed after cessation of atrial overdrive pacing. Ventricular tachycardia can be diagnosed if the atrial electrogram from the last paced beat conducts to the ventricle with no change in the activation sequence but a ventricular electrogram with an activation sequence identical to that of the clinical tachycardia appears before the next atrial electrogram.
However, if a return electrogram from the atrium occurs without an intervening second ventricular electrogram, antidromic AVRT or SVT with aberrancy is more likely. 1 In our patient, if we pay attention to the cycle lengths after stopping overdrive atrial pacing, the first non‐entrained V signal was the second V signal after stopping atrial pacing. Therefore, in fact the response was a V‐A‐V response, and we can refer to it a pseudo‐A‐V‐V‐A.
Delivering an atrial premature beat (APB) during a broad complex tachycardia is another useful manoeuvrer. If a His refractory atrial premature beat, delivered from lateral wall advances (or delays) the ventricular signal but the septal atrial electrogram is not advanced on the beat for the APB, an accessory pathway is present. 1 In our patient, an atrial extra stimulus from lateral wall of right atrium delivered during the arrhythmia when His bundle was refractory terminated the arrhythmia, repetitively which establishes the presence of an extra‐nodal pathway and its participation in the re‐entrant circuit.
Moreover, the difference between the post‐pacing interval after tachycardia entrainment from the right ventricular apex and the tachycardia CL (PPI – TCL) is 10 ms which is in favor of an antidromic AVRT versus an AVNRT using a bystander accessory pathway. 3
These findings are consistent with a Mahaim accessory pathway (atriofascicular or atrioventricular) and the arrhythmia can be diagnosed an antidromic AVRT (anterograde conduction via the accessory pathway and retrograde conduction via the His‐Purkinje system). Accessory pathway ablation was performed successfully in the right atrium at 10:00 on tricuspid annulus.
Distinguishing an atriofascicular pathway from an atrioventricular Mahaim pathway can be challenging. In patients with atriofascicular pathway, QRS width during the arrhythmia is often between 120 and 140 ms, while it is more in atrioventricular Mahaim pathways. Furthermore, measuring the VH interval during tachycardia is useful to distinguish these variants. In general, VH interval during arrhythmia in patients with atriofascicular accessory pathway is less than HV interval in sinus rhythm. 2 , 4 In our patient, the QRS duration during arrhythmia was 160 ms which is wider than usual QRS duration in atriofascicular pathways. Moreover, we could not observe any clear His signal as it had fallen within the QRS and the VH interval looked relatively long. Therefore, we considered the accessory pathway an atrioventricular Mahaim.
In patients with atriofascicular accessory or atrioventricular Mahaim pathway, usually incremental atrial pacing shows progressive prolongation of the AH interval and shortening of HV interval until a total antidromic capture of the ventricle and retrograde activation of His. In unusual circumstances, these pathways can only manifest during antidromic tachycardia due to the dominance of anterograde conduction via the atrioventricular node (latent Mahaim). 2
In our patient, the antegrade conduction pathway of the arrhythmia had decremental conduction properties. Therefore, the reason for a pseudo‐A‐V‐V‐A response after stopping overdrive atrial pacing is the slow conduction of the accessory pathway (like pseudo‐V‐A‐A‐V response after stopping overdrive atrial pacing in atypical AVNRT).
CONFLICT OF INTEREST
Authors declare no conflict of interests for this article.
Alasti M, Pawade T, Alison J. (2022). Ventricular tachycardia or supraventricular tachycardia?. J Arrhythmia. 2022;38:259–262. 10.1002/joa3.12682
REFERENCES
- 1. Asirvatham S. Diagnostic Manoeuvres commonly used in the electrophysiology laboratory. In: Asirvatham S, Cha YM, Friedman PA, editors. Mayo Clinic Electrophysiology Manual. First ed. Oxford University Press; 2014. p. 85–127. [Google Scholar]
- 2. Correa FS, Lokhandwala Y, Filho FC, et al. Part II—clinical presentation, electrophysiologic characteristics, and when and how to ablate atriofascicular pathways and long and short decrementally conducting accessory pathways. J Cardiovas Electrophysiol 2019; 30: 3079–3096. [DOI] [PubMed] [Google Scholar]
- 3. Quinn FR, Mitchell B, Mardell A, Veenhuyzen GD. Overdrive ventricular pacing to clarify the diagnosis of a left bundle branch block morphology tachycardia. Heart Rhythm. 2008;5:1479–81. [DOI] [PubMed] [Google Scholar]
- 4. Hoffmayer KS, Han FT, Singh D, Scheinman MM. Variants of accessory pathways. Pac Clin Electrophysiol. 2020;43:21–9. [DOI] [PubMed] [Google Scholar]


