Abstract
Background:
Delays from the time of an anterior cruciate ligament (ACL) tear to surgical reconstruction are associated with an increased incidence of meniscal and chondral injuries.
Purpose:
To evaluate the association between delays in ACL reconstruction (ACLR) and risk factors for intra-articular injuries across 8 patient demographic subsets.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
We performed a retrospective chart review of all patients who underwent ACLR from January 2009 to May 2015 at a single institution. Variables collected were age, sex, body mass index, time from injury to surgery, and presence of meniscal tears and chondral injuries. Demographic subsets were created according to sex, age (<27 vs ≥27 years), body mass index (<25 vs ≥25 kg/m2), and injury setting (sports vs non–sports related). Subsets were divided by time from injury to ACLR: 0 to <6 months (control group), 6 to <12 months, and ≥12 months. Multivariate logistic regression–generated odds ratios (ORs) were calculated.
Results:
Overall, 410 patients were included. ORs were significant for an increased incidence of medial meniscal tears (MMTs) (OR, 1.12-3.72; P = .02), medial femoral condyle (MFC) injuries (OR, 1.18-4.81; P = .02), and medial tibial plateau (MTP) injuries (OR, 1.33-31.07; P = .02) with surgical delays of 6 to <12 months. With ≥12-month delays, significance was found for MMTs (OR, 2.92-8.64; P < .001), MFC injuries (OR, 1.86-5.88; P < .001), MTP injuries (OR, 1.37-21.22; P = .02), lateral femoral condyle injuries (OR, 2.41-14.94; P < .001), and lateral tibial plateau injuries (OR, 1.15-5.27; P = .02). In the subset analysis, differences in the timing, location, rate, and pattern of chondral and meniscal injuries became evident. Female patients and patients with non–sports-related ACL tears had less risk of associated injuries with delayed surgery, while other demographic groups showed an increased injury risk.
Conclusion:
When analyzing patients who were symptomatic enough to eventually require surgery, an increased incidence of MMTs and medial chondral injuries was associated with ≥6-month delays in ACLR, and an increased incidence of lateral chondral injuries was associated with ≥12-month delays. Female patients and patients with non–sports-related ACL tears had less risk of injuries with delayed ACLR.
Keywords: ACL, demographics, delayed, injury
The anterior cruciate ligament (ACL) functions to stabilize the knee by restraining anterior motion of the tibia relative to the femur. Additionally, it provides torsional stability to the knee, which is important during cutting and pivoting activities. ACL-deficient knees tend to experience additional intra-articular injuries, as other structures must compensate for the lack of an ACL, and it is well-established that longer delays from the time of an ACL tear to definitive surgical reconstruction are associated with an increased incidence of meniscal and chondral injuries at the time of surgery. 1 , 3 -6
There is a paucity of literature, however, on the increased injury risk associated with delayed ACL reconstruction (ACLR) across various demographic groups. The purpose of this study was to evaluate the association between intra-articular injuries and delays in ACLR across 8 patient demographic subsets. We hypothesized that different subsets of patients would indeed demonstrate varying increases in injuries at the time of surgery with delayed ACLR.
Methods
This study was approved by our institutional review board. We conducted a retrospective cross-sectional cohort chart review of all patients who underwent ACLR from January 1, 2009, to May 14, 2015, at a single academic teaching institution. Patients were excluded if they sustained a previous ipsilateral ACL injury, if they sustained other simultaneous ligamentous knee injuries, if they had undergone previous ipsilateral knee surgery, or if the operative report was unavailable.
Demographic variables collected were age at presentation, sex, body mass index (BMI) at presentation, and injury setting (sports related vs non–sports related). Of the variables of interest, if a patient was found to have some, but not all, of the variables, they were included in the study. Variables collected from operative reports included the presence of a medial meniscal tear (MMT), a lateral meniscal tear (LMT), and any chondral injury to the medial femoral condyle (MFC), lateral femoral condyle (LFC), medial tibial plateau (MTP), lateral tibial plateau (LTP), and patellofemoral (PF) joint. Surgical delay was recorded and defined as the time, in months, from the injury to ACLR. This time was based on the patient’s recollection of the injury date, as recorded in the medical record.
Descriptive statistics were calculated, including the mean and standard deviation for normally distributed variables and the median for non-normally distributed variables. Proportions were calculated for categorical variables. In addition to an aggregate group that included all study participants, 8 demographic subsets were created for analysis according to sex, age, BMI, and injury setting. Each patient was included in every demographic subset to which they belonged. To categorize by age, a cutoff of 27 years was used, as it yielded the greatest degree of combined sensitivity and specificity (Youden index) in predicting associated injuries. A BMI cutoff of 25 kg/m2 was selected, as it divided the patient sample relatively evenly and distinguished normal from overweight or obese participants according to the standards of the United States Centers for Disease Control and Prevention.
The association of surgical delay with intra-articular injuries was assessed for the aggregate group as well as each subset through multivariate logistic regression. Within each subset, surgical delay was stratified into 6 to <12 months and ≥12 months, with patients undergoing surgery at 0 to <6 months after an ACL injury serving as the control group. In each regression, relevant demographic variables including age, BMI, sex, and injury setting were controlled for to mitigate confounding bias. The output of each regression was an odds ratio (OR), indicating an association of a secondary injury with surgical delay relative to the control group. ORs are displayed graphically with corresponding 95% confidence intervals, and P < .05 was considered statistically significant. All statistical analyses were conducted using Stata 15.0 software (StataCorp).
Results
Overall, 489 patients underwent ACLR during the study period. After exclusions, 410 participants remained in the study. The mean age was 27.4 ± 8.8 years (range, 14-59 years), with a median of 26.0 years. More than half of the participants (63.2%) had a BMI ≥25 kg/m.2 Male patients comprised a majority of the study population (70.5% ). Regarding surgical delays, 51.3% of patients underwent ACLR at 0 to <6 months from the injury, 17.8% at 6 to <12 months, and 30.9% at ≥12 months. The patient characteristics are summarized in Table 1.
TABLE 1.
Characteristics of the Study Cohort (n = 410) a
| Variable | Value |
|---|---|
| Age, y | 27.4 ± 8.8 (26.0) |
| Body mass index, kg/m2 | 26.7 ± 4.4 (26.1) |
| Time to ACLR, mo | 18.1 ± 40.8 (5.6) |
| Sex | |
| Male | 289 (70.5) |
| Female | 121 (29.5) |
| Injury setting b | |
| Sports related | 323 (81.0) |
| Non–sports related | 76 (19.0) |
a Data are reported as mean ± SD (median) or n (%). ACLR, anterior cruciate ligament reconstruction.
b Data are missing for 11 participants.
The incidence of concomitant abnormalities in the control group was 43.54% for MMTs, 61.43% for LMTs, 18.57% for MFC injuries, 1.43% for MTP injuries, 4.31% for LFC injuries, 6.70% for LTP injuries, and 19.52% for PF joint injuries. Patients with surgical delays of 6 to <12 months had significantly increased odds of MMTs (OR, 1.12-3.72; P = .02), MFC injuries (OR, 1.18-4.81; P = .02), and MTP injuries (OR, 1.33-31.07; P = .02). With surgical delays of ≥12 months, ORs were again significant for an increased incidence of MMTs (OR, 2.92-8.64; P < .001), MFC injuries (OR, 1.86-5.88; P < .001), and MTP injuries (OR, 1.37-21.22; P = .02); in addition, significance was seen for injuries to the LFC (OR, 2.41-14.94; P < .001) and LTP (OR, 1.15-5.27; P = .02) (Figure 1).
Figure 1.
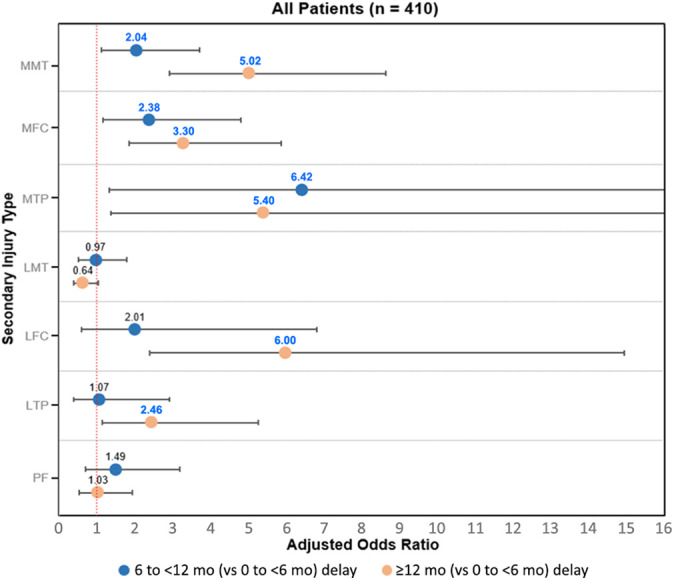
Intra-articular injury after delayed anterior cruciate ligament reconstruction (ACLR): all patients. Values presented are odds ratios from multivariate logistic regression. Blue text indicates statistical significance (P < .05).
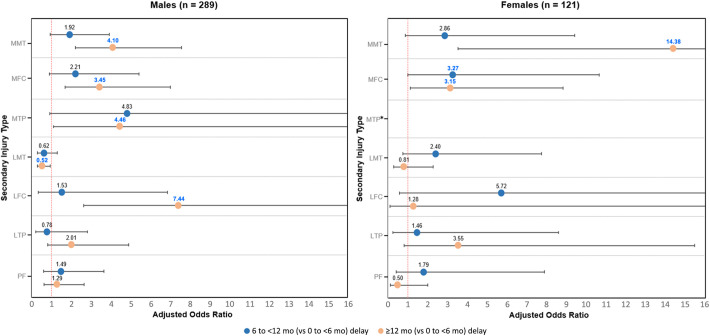
For male patients with surgical delays of 6 to <12 months, ORs were not significant for medial compartment injuries. For male patients with surgical delays of ≥12 months, there was a significant risk for MMTs (OR, 2.21-7.60; P < .001) and for injuries to the MFC (OR, 1.69-7.03; P = .001), MTP (OR, 1.11-17.99; P = .04), and LFC (OR, 2.63-21.02; P < .001). In addition, a significantly decreased risk of LMTs (OR, 0.29-0.95; P = .03) was seen with surgical delays of ≥12 months in male patients (Figure 2). In contrast, female patients with surgical delays of 6 to <12 months did show a significant risk for MFC injuries (OR, 1.00-10.66; P = .05). In female patients with surgical delays of ≥12 months, ORs were significant for both MMTs (OR, 3.53-58.53; P < .001) and MFC injuries (OR, 1.13-8.82; P = .03) (Figure 2).
Figure 2.
Intra-articular injury after delayed anterior cruciate ligament reconstruction (ACLR): male and female sex. Values presented are odds ratios from multivariate logistic regression. Blue text indicates statistical significance (P < .05). *Odds ratio could not be calculated because of a lack of a specified secondary injury.
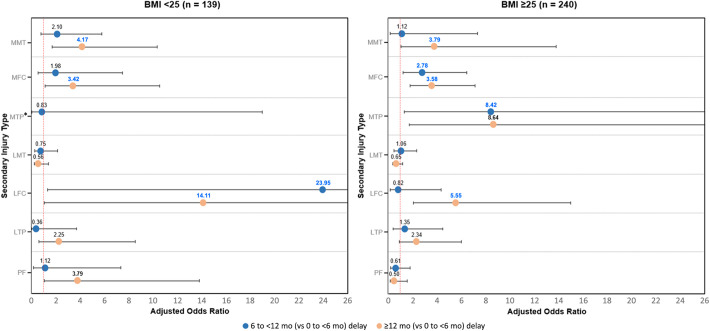
Data on BMI at presentation were missing for 11 patients. Of the available participants, those with BMIs <25 kg/m2 and surgical delays of 6 to <12 months had a significantly increased risk of LFC injuries (OR, 1.33-432.90; P = .03). Patients with BMIs ≥25 kg/m2 and surgical delays of 6 to <12 months had a significantly increased risk for injuries to the MFC (OR, 1.20-6.45; P = .02) and MTP (OR, 1.31-54.01; P = .03) (Figure 3). With surgical delays of ≥12 months, odds were significantly increased for MMTs, MFC injuries, and LFC injuries in patients with BMIs of both <25 and ≥25 kg/m2. ORs for MTP injuries with surgical delays of ≥12 months could not be calculated because of a lack of observed injuries in the subset of BMI <25 kg/m2 (Figure 3).
Figure 3.
Intra-articular injury after delayed anterior cruciate ligament reconstruction (ACLR): body mass index (BMI) <25 and ≥25 kg/m.2 Values presented are odds ratios from multivariate logistic regression. Blue text indicates statistical significance (P < .05). *Odds ratio could not be calculated because of a lack of a specified secondary injury.
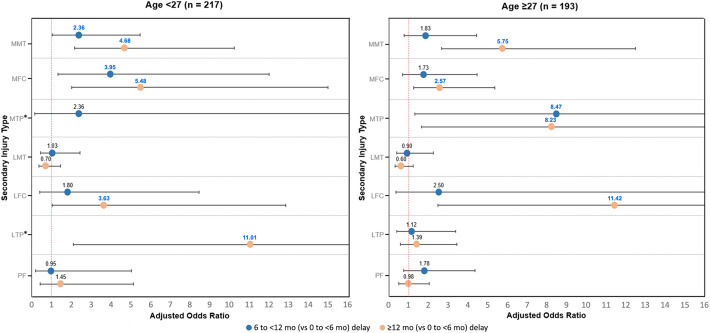
For patients aged <27 years, a surgical delay of 6 to <12 months led to a significantly increased risk of MMTs (OR, 1.02-5.45; P = .04) and MFC injuries (OR, 1.31-11.97; P = .02), and a surgical delay of ≥12 months led to a significantly increased risk of MMTs (OR, 2.15-10.21; P < .001), MFC injuries (OR, 2.01-14.95; P = .001), LFC injuries (OR, 1.03-12.80; P = .045), and LTP injuries (OR, 2.09-58.10; P = .01). In contrast, for patients aged ≥27 years with a surgical delay of 6 to <12 months, ORs were significant for MTP injuries (OR, 1.29-55.60; P = .03); with a surgical delay of ≥12 months, ORs were significant for MMTs (OR, 2.65-12.50; P < .001), MFC injuries (OR, 1.23-5.35; P = .01), MTP injuries (OR, 1.64-41.45; P = .01), and LFC injuries (OR, 2.46-53.06; P = .002) (Figure 4).
Figure 4.
Intra-articular injury after delayed anterior cruciate ligament reconstruction (ACLR): age <27 and ≥27 years. Values presented are odds ratios from multivariate logistic regression. Blue text indicates statistical significance (P < .05). *Odds ratio could not be calculated because of a lack of a specified secondary injury.
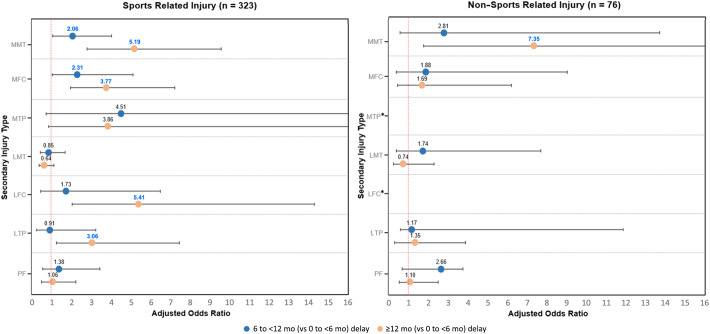
Data regarding injury setting were missing for 11 patients. For those injuries that occurred while playing sports and with surgical delays of 6 to <12 months, ORs were significant for MMTs (OR, 1.06-4.04; P = .03) and MFC injuries (OR, 1.04-5.13; P = .04). With surgical delays of ≥12 months, ORs were significant for MMTs (OR, 2.81-9.59; P < .001) and injuries to the MFC (OR, 1.96-7.25; P < .001), LFC (OR, 2.05-14.30; P = .001), and LTP (OR, 1.25-7.47; P = .01). For non–sports-related injuries and surgical delays of 6 to <12 months, no ORs were significant; with surgical delays of ≥12 months, ORs were significant for MMTs (OR, 1.78-30.40; P = .01) (Figure 5).
Figure 5.
Intra-articular injury after delayed anterior cruciate ligament reconstruction (ACLR): sports- and non–sports-related injuries. Values presented are odds ratios from multivariate logistic regression. Blue text indicates statistical significance (P < .05). *Odds ratio could not be calculated because of a lack of a specified secondary injury.
Discussion
When analyzing all patients who were symptomatic enough to eventually require surgical care, an increased incidence of medial meniscal and medial chondral injuries was associated with ≥6-month ACLR delays as well as an increased incidence of lateral chondral injuries with ≥12-month delays. Female patients and patients with non–sports-related ACL tears tended to have fewer increases in injuries with delayed ACLR, while other demographic groups had increases in injuries, resembling all patients combined. This study is further evidence that delayed ACLR is associated with an increased incidence of intra-articular injuries. 1,3 –6 Our study findings are in agreement with other studies, 5,7,10,24 showing that a medial compartment injury was found in the setting of chronic ACL deficiency. Additionally, we found a significantly increased incidence of lateral chondral injuries with ACL deficiency beyond 12 months, which is in agreement with previously published reports. 4,18,22
It is well-known that ACL tears often occur with concurrent injuries to the menisci and articular cartilage. In addition, it has been well-established that a delay in reconstruction of an ACL-deficient knee increases the risk of further injuries to these associated structures. 15,18,19,23 This is thought to occur as the knee, without the ACL to resist translational and rotary forces, moves outside of normal physiological parameters. The altered knee kinematics affects loading of the menisci and may compromise articular surface load distribution and contact congruity. 2
Understanding that ACL-deficient knees tend to sustain meniscal and chondral injuries and that identifying patients with these abnormalities are important, as these intra-articular injuries impact long-term outcomes and the development of degenerative knee arthritis. 12 –14,20,21 Few studies have separated patients into different subsets before analyzing for an increased incidence of meniscal and chondral injuries with delayed reconstruction. 10,15,23 When the 8 subsets of patients in this study were analyzed independently for an increased incidence of meniscal and chondral injuries with delayed reconstruction, differences between subsets in the timing, location, rate, and pattern of chondral and meniscal injuries became evident.
When comparing patients according to sex, male patients had an increased incidence of chondral injuries in both the medial and lateral compartments with delayed surgery, while female patients only had an increased incidence of medial chondral injuries. The incidence of meniscal injuries significantly increased with ≥12-month surgical delays in both men and women. This is compatible with both Slauterbeck et al, 22 who found that male patients and increasing surgical delays were associated with an increased incidence of meniscal and chondral injuries, and O’Connor et al, 16 who found that the risk of meniscal injuries increased at a higher rate over time among women. In contrast, Granan et al 10 found that female patients had reduced odds of having a meniscal tear with surgical delays, with no effect on the risk for cartilage lesions. Of note, male patients in our study also had a decreased incidence of LMTs with ≥12-month delays, which was the only instance of a decreased injury incidence with a surgical delay at any intra-articular location for any subset. A significant decrease in the incidence of injuries seems counterintuitive but could be explained by lateral meniscus healing over the course of the ≥12-month delay in undergoing ACLR. Prior studies have found that the incidence of LMTs does not increase significantly with surgical delays. 9
For the BMI subsets, overweight and obese patients developed chondral injuries more quickly than those with a normal BMI. Patients with normal BMIs were the only subset to have any increased incidence of PF joint injuries with delayed reconstruction, which was significant with delays of ≥12 months. To our knowledge, the effect of a surgical delay on intra-articular injuries in patients stratified by BMI has not been studied extensively. Prior studies have found that a higher BMI is independently associated with an increased incidence of intra-articular injuries at the time of surgery in adults and children, but this was without consideration of a surgical delay. 3,4,8
While the chondral injury profiles with a surgical delay for the 2 age subsets were similar, patients aged <27 years demonstrated an increased incidence of MMTs with delays of 6 to <12 months, while patients aged ≥27 years only had an increased incidence of MMTs with surgical delays of ≥12 months. This corroborates the findings of Sri-Ram et al 23 but contrasts with the findings of Magnussen et al, 15 who separated patients by age and found that patients older than 22 years had a significantly increased incidence of MFC injuries with delayed reconstruction while patients younger than 22 years showed no increased incidence of injuries at any location in the knee. Our study found an increase in the incidence of MFC injuries with surgical delays in the younger population. Comparisons are difficult to make, however, as the previous study by Magnussen et al 15 involved a younger study cohort (age cutoff of 22 vs 27 years in our study) and a relatively short time from the injury to surgery in the delayed reconstruction population (median time to surgery was only 6 weeks, while ours was 5.6 months).
Granan et al 10 included 3 age groups and had similar findings: the incidence of chondral injuries increased with longer delays to reconstruction for the older and younger adult groups but not children. They also found that the incidence of meniscal tears only increased for the younger adult group with a longer time to ACLR but not for the older adults or children. As a limitation, this previous study did not specify whether the meniscal or chondral injury was medial or lateral. While it is difficult to compare the results of Granan et al 10 directly with our study’s findings because of the different age cutoffs utilized, there were similar findings of an increased incidence of chondral and meniscal injuries with delayed ACLR in the young adult subsets. Finally, other previous studies have found that older people have an increased incidence of meniscal and chondral injuries at the time of surgery but do not comment specifically on the impact of surgical delays within this patient population. 9,18,23
While the subset of sports-related tears had an increased incidence of injuries similar to all patients combined, the non–sports-related tear subset had only a significantly increased incidence of MMTs at ≥12 months. The significance here may have been limited by the smaller sample size of patients who sustained their ACL tear during non-sporting activity. The injury setting subsets were created in an attempt to separate athletes from nonathletes. Although an imprecise distinction, our data suggest that nonathletes—or at least those who sustain an ACL tear in a non–sports-related setting—may accrue fewer intra-articular injuries in the setting of delayed ACLR. This contrasts with the findings of Joseph et al, 11 who documented an increased incidence of meniscal and chondral injuries associated with ACL deficiency in both athletic and nonathletic patients.
While the collection of data on the reasons for a delay in ACLR was beyond the scope of this study, attempting to understand why patients delay surgery is important to provide appropriate care and counseling. Patients may elect nonoperative treatment for a variety of reasons (work or family demands, sedentary lifestyle, fear of undergoing an operative procedure, etc). Others may have little to no functional instability and therefore elect nonoperative treatment. Some patients may present in a delayed fashion either because of time limitations or limitations in access to proper care. Pierce et al 17 demonstrated that patient insurance type can greatly affect access to care for adolescents with acute knee injuries. This is one area in which individual surgeons can have meaningful impact by being available to all patients to help minimize disparities in access to care.
The strengths of this study include a moderate sample size, a high prevalence of long delays from the injury to surgery, and multivariate regression analysis. There were a number of limitations in reaching statistically significant and clinically meaningful conclusions. First, immediate postinjury imaging was not performed; thus, we cannot know what injuries occurred at the time of the ACL tear or transpired because of ACL deficiency. Second, the nature and severity of associated intra-articular lesions or the need for treatment were not included in the analysis. Lesions were simply noted as present or absent. Third, we do not have data on factors that could contribute to the incidence of injuries, such as activity level, preoperative rehabilitation or return to sports, type of employment, access to health care, and other unidentifiable factors of our patient population. Fourth, no postoperative outcome or functional scores were utilized, limiting the clinical significance of our findings. Also, this study included only symptomatic patients with ACL-deficient knees in whom it is unclear whether they were counseled on the risk of reinjuries or on prevention strategies for a reinjury. Next, all patients were from a single institution, which introduces selection bias and limits the generalizability of the results. In addition, 11 patient charts did not have a record of the BMI at presentation or the injury setting. These patients were not excluded, as we felt that this would not introduce sufficient selection bias to outweigh including these patients. Also, several subsets had small sample sizes, limiting power as well as internal and external validity. Finally, this study does not include a comparison group of patients who did not undergo ACLR and cannot comment on whether reconstructing the ACL prevents the occurrence of additional intra-articular injuries. Based on the results of this study and despite its limitations, it appears that broad generalizations about the development of intra-articular injuries with delayed ACLR cannot be applied to all types of patients.
Conclusion
When analyzing all patients who were symptomatic enough to eventually require surgical care, an increased incidence of medial meniscal and medial chondral injuries was associated with ≥6-month ACLR delays as well as an increased incidence of lateral chondral injuries with ≥12-month delays. Female patients and patients with non–sports-related ACL tears tended to have fewer increases in injuries with delayed ACLR, while other demographic groups had increases in injuries, resembling all patients combined.
Acknowledgment
The authors thank Dr Sheena Black for her input and help with the preparation of this study and subsequent article.
Footnotes
Final revision submitted August 29, 2021; accepted September 16, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: G.K. has received education support from Liberty Surgical. M.K. has received consulting fees, nonconsulting fees, and honoraria from Wright Medical. K.J.C. has received education payments from Arthrex, consulting fees from Medical Device Business Services, nonconsulting fees from Arthrex, and hospitality payments from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Texas Southwestern Medical Center (No. STU 052012-051).
References
- 1. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(2):275–281. [DOI] [PubMed] [Google Scholar]
- 2. Arner JW, Irvine JN, Zheng L, et al. The effects of anterior cruciate ligament deficiency on the meniscus and articular cartilage. Orthop J Sports Med. 2016;4(4):2325967116639895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barrett GR, Thibodeaux KE, Replogle WH, Barrett A, Parks T, Baker D. Body mass index as an indicator of associated intra-articular injuries in patients with anterior cruciate ligament tears. J Surg Orthop Adv. 2015;24(3):159–163. [PubMed] [Google Scholar]
- 4. Brambilla L, Pulici L, Carimati G, et al. Prevalence of associated lesions in anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(12):2966–2973. [DOI] [PubMed] [Google Scholar]
- 5. Chhadia AM, Inacio MCS, Maletis GB, Csintalan RP, Davis BR, Funahashi TT. Are meniscus and cartilage injuries related to time to anterior cruciate ligament reconstruction? Am J Sports Med. 2011;39(9):1894–1899. [DOI] [PubMed] [Google Scholar]
- 6. Church S, Keating JF. Reconstruction of the anterior cruciate ligament. Bone Joint J. 2005;87(12):1639–1642. [DOI] [PubMed] [Google Scholar]
- 7. Cipolla M, Scala A, Gianni E, Puddu G. Different patterns of meniscal tears in acute anterior cruciate ligament (ACL) ruptures and in chronic ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc. 1995;3(3):130–134. [DOI] [PubMed] [Google Scholar]
- 8. Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears. Am J Sports Med. 2012;40(9):2128–2133. [DOI] [PubMed] [Google Scholar]
- 9. Ghodadra N, Mall N, Karas V, et al. Articular and meniscal pathology associated with primary anterior cruciate ligament reconstruction. J Knee Surg. 2012;26(3):185–194. [DOI] [PubMed] [Google Scholar]
- 10. Granan L-P, Bahr R, Lie SA, Engebretsen L. Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears. Am J Sports Med. 2009;37(5):955–961. [DOI] [PubMed] [Google Scholar]
- 11. Joseph C, Pathak SS, Aravinda M, Rajan D. Is ACL reconstruction only for athletes? Int Orthop. 2008;32(1):57–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Karikis I, Åhlén M, Sernert N, Ejerhed L, Rostgård-Christensen L, Kartus J. The long-term outcome after early and late anterior cruciate ligament reconstruction. Arthroscopy. 2018;34(6):1907–1917. [DOI] [PubMed] [Google Scholar]
- 13. Louboutin H, Debarge R, Richou J, et al. Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee. 2009;16(4):239–244. [DOI] [PubMed] [Google Scholar]
- 14. Magnussen RA, Mansour AA, Carey JL, Spindler KP. Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg. 2009;22(4):347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Magnussen RA, Pedroza AD, Donaldson CT, Flanigan DC, Kaeding CC. Time from ACL injury to reconstruction and the prevalence of additional intra-articular pathology: is patient age an important factor? Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2029–2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. O’Connor DP, Laughlin MS, Woods GW. Factors related to additional knee injuries after anterior cruciate ligament injury. Arthroscopy. 2005;21(4):431–438. [DOI] [PubMed] [Google Scholar]
- 17. Pierce TR, Mehlman CT, Tamai J, Skaggs DL. Access to care for the adolescent anterior cruciate ligament patient with Medicaid versus private insurance. J Pediatr Orthop. 2012;32(3):245–248. [DOI] [PubMed] [Google Scholar]
- 18. Ralles S, Agel J, Obermeier M, Tompkins M. Incidence of secondary intra-articular injuries with time to anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(6):1373–1379. [DOI] [PubMed] [Google Scholar]
- 19. Roe J, Sri-Ram K, Salmon L, Pinczewski L. The incidence of secondary pathology after anterior cruciate ligament rupture in over 5000 patients. J Sci Med Sport. 2012;15:S354. [DOI] [PubMed] [Google Scholar]
- 20. Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. Am J Sports Med. 2000;28(4):446–452. [DOI] [PubMed] [Google Scholar]
- 21. Shirazi R, Shirazi-Adl A. Analysis of partial meniscectomy and ACL reconstruction in knee joint biomechanics under a combined loading. Clin Biomech (Bristol, Avon). 2009;24(9):755–761. [DOI] [PubMed] [Google Scholar]
- 22. Slauterbeck JR, Kousa P, Clifton BC, et al. Geographic mapping of meniscus and cartilage lesions associated with anterior cruciate ligament injuries. J Bone Joint Surg Am. 2009;91(9):2094–2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sri-Ram K, Salmon LJ, Pinczewski LA, Roe JP. The incidence of secondary pathology after anterior cruciate ligament rupture in 5086 patients requiring ligament reconstruction. Bone Joint J. 2013;95(1):59–64. [DOI] [PubMed] [Google Scholar]
- 24. Warren RF, Levy IM. Meniscal lesions associated with anterior cruciate ligament injury. Clin Orthop Relat Res. 1983;172:32–37. [PubMed] [Google Scholar]