Abstract
Objective
In the beginning of the COVID-19 pandemic in spring 2020, elective and oncologic surgical cases were cancelled. After adequate safety protocols were established, each subspecialty within otolaryngology faced unique challenges in reengaging patients for surgical scheduling.
Study Design
Retrospective review from March to May 2020.
Setting
Single academic institution.
Methods
Patients whose otolaryngology surgery was cancelled due to COVID-19 hospital precautions were identified. Rescheduling rates were analyzed by subspecialty. Case completion was determined as the percentage of initially cancelled cases that were completed within 6 months of their original planned dates.
Results
Of 833 otolaryngology cases scheduled between March 16 and May 29, 2020, a total of 555 (66.63%) were cancelled due to COVID-19 precautions, and 71.17% were rescheduled within 6 months. Cancellation and rescheduling rates per subspeciality were as follows, respectively: head and neck surgery, 42.79% and 88.76%; sleep surgery, 83.92% and 64.07%; rhinology and skull base, 72.67% and 64.80%; facial plastic and reconstructive surgery, 80.00% and 74.17%; otology and neurotology, 71.05% and 66.67%; and laryngology, 68.57% and 79.17%. The case completion rates were as follows: head and neck surgery, 95.2%; laryngology, 85.7%; facial plastic and reconstructive surgery, 79.3%; otology and neurotology, 76.3%; rhinology and skull base, 74.4%; and sleep surgery, 69.9%.
Conclusion
Differences for surgical rescheduling rates during the COVID-19 pandemic shutdown exist among otolaryngology subspecialties. Our experience suggests that subspecialties that functioned on an elective nature were more likely to face lower rates of case completion.
Keywords: case rescheduling, COVID-19, otolaryngology, pandemic
COVID-19 is a novel coronavirus that was identified in December 2019.1,2 After national lockdown restrictions were enacted in March 2020, COVID-19 affected the practice of many specialties, including otolaryngology.3,4 Otolaryngology was deemed to be a high-risk specialty for COVID-19 transmission due to its primary focus on the nasopharynx and respiratory tract and to the substantial aerosol production during operative procedures.5-7 Numerous studies have indicated the localization of large viral loads in the nasal epithelial cells, with the nasal cavity and nasopharynx having the highest concentrations of virus in the upper respiratory tract.5-7 These factors, in combination with reports of inadequate personal protective equipment and delayed turnaround time for diagnostic testing, placed otolaryngology providers at high risk during surgical procedures in the early stages of the pandemic.5-8
Within otolaryngology, subspecialties vary in their elective nature as well as the risk of COVID-19 exposure, with rhinology and head and neck surgery at highest risk. 5 Nasal and transnasal endoscopic procedures are among the highest-risk procedures in otolaryngology, whereas the risk for transmission in head and neck surgery procedures is directly proportional to the degree of mucosal exposure; thus, neck and thyroid surgery tends to be of lower transmission risk as compared with transoral procedures. 6 Various otolaryngology-related tiering systems were consequently developed at hospitals across the world, including Thomas Jefferson University, to decrease nosocomial COVID-19 transmission to patients and providers while providing timely care.9-11 These tiering systems placed emergent surgery as the top priority and cancelled all nonurgent and elective surgery. Although the risk for transmission of COVID-19 during surgery remains high, a study from the United Kingdom indicated that head and neck surgical procedures are safe with proper personal protective equipment, as 0 of 47 patients contracted COVID-19 from surgery. 11
Once adequate safety protocols were established to mitigate nosocomial spread of COVID-19, hospitals faced a new challenge of reengaging patients for elective surgical procedures. There are no published studies yet regarding the surgical rescheduling challenges in otolaryngology or variability in rescheduling rates across subspecialties. In addition, there are limited studies regarding the rate of COVID-19 transmission during otolaryngologic surgical procedures. 5 This study aims to investigate the cancellation and rescheduling rates among otolaryngology subspecialties during COVID-19 and the accompanying challenges of reengaging patients to pursue elective surgical procedures. We hypothesize that subspecialties with cases that face significant risk for disease progression will have the lowest cancellation and highest rescheduling rates, whereas subspecialties with more elective surgery will face higher cancellation rates and lower rates of rescheduled cases.
Methods
Study Design
This retrospective chart review included all patients scheduled for otolaryngology procedures at Thomas Jefferson University Hospital during the COVID-19 pandemic lockdown between March 16 and May 29, 2020. Thomas Jefferson University Hospital is a tertiary care center in Philadelphia, Pennsylvania. This study was approved by the Thomas Jefferson University Hospital Institution Review Board.
Study Population
The Department of Otolaryngology–Head and Neck Surgery at Thomas Jefferson University Hospital consists of 18 physicians covering the subspecialties of head and neck surgery, sleep surgery, rhinology and skull base surgery, facial plastic and reconstructive surgery, otology and neurology, and laryngology. All patients in this study were scheduled for any otolaryngology procedure between March 16 and May 29, 2020, at a single hospital system (with a focus on 1 tertiary university hospital within that system). Any patient who was offered a surgical appointment, whether an existing patient or a new one, was included in the study. The initial scheduled surgery date was defined as any case that was originally scheduled within the time frame of interest, regardless of cancellation or rescheduling. This time frame represents when the hospital system restricted elective surgical cases due to COVID-19 precautions. The hospital developed a prioritization system for elective or nonelective cases to determine which were cancelled vs which were able to proceed within the study time frame.
Tiering System
Thomas Jefferson University Hospital established a tiering system for all operations and procedures early in the COVID-19 pandemic. Patients in whom a delay in surgery would be life threatening were prioritized to tier 1, which included most cancers. Tiers 2 and 3 consisted of patients who could delay surgery 1 and 2 months, respectively, without a significant impact on survival or clinical outcome. Within the otolaryngology department, this tiering system was applied in deciding if surgical procedures were prioritized as urgent or rescheduled. Cases for patients with carcinoma of the oropharynx, nasopharynx, or larynx were considered tier 1, while thyroid-related cases were generally classified as tier 2, and cases such as septoplasty and turbinectomy were classified as tier 3.
Outcome Measures
The primary outcome measure was the rate of case cancellation and subsequent rescheduling within the defined time frame. Cases that were rescheduled were performed within 6 months of the originally scheduled surgery.
The secondary outcome measure was the median time to procedure completion for rescheduled cases. Cases were considered rescheduled if there was a new case date scheduled for the patient within 6 months of the original case date. Time to procedure completion was calculated from the original case date to the rescheduled case date.
The tertiary outcome measure was the percentage of each prioritization tier (1, 2, and 3) for cancelled and subsequently rescheduled cases per subspecialty. The cases that were not cancelled were not included for this analysis.
The quaternary outcome measure was the rate of COVID-19 nosocomial infection for patients who had otolaryngologic procedures within the defined time frame. All patients were required to have a negative COVID-19 test result prior to the surgical procedure. COVID-19 tests were not regularly administered to patients while admitted to the hospital; however, tests were administered if patients demonstrated symptoms or there was concern of infection. Nosocomial transmission of COVID-19 was defined as a positive test result within 2 weeks of a patient’s scheduled procedure.
Analysis
For each specialty, the case completion rate was calculated with the following formula: (total cases scheduled – cancelled cases + rescheduled cases) / total cases scheduled.
Results
Of the 833 otolaryngology cases scheduled between March 16 and May 29, 2020, a total of 555 (66.63%) were cancelled due to COVID-19 precautions. For the entire department, 395 (71.17%) of the cancelled surgical procedures were rescheduled within 6 months of the originally scheduled date. The 833 cases were categorized by subspeciality. For each subspecialty, the cancellation and rescheduled rates were calculated, as well as the case completion rate ( Table 1 ). The overall median time to procedure completion for rescheduled cases was 70 days ( Table 2 ).
Table 1.
Case Completion Rate by Subspecialty. a
| Cases | Head and neck surgery | Sleep surgery | Rhinology and skull base surgery | Facial plastic and reconstructive surgery | Otology and neurotology | Laryngology |
|---|---|---|---|---|---|---|
| Total | 208 | 199 | 172 | 150 | 38 | 35 |
| Cancelled | 89 | 167 | 125 | 120 | 27 | 24 |
| Rescheduled | 79 | 107 | 81 | 89 | 18 | 19 |
| Completion rate, % | 95.2 | 69.9 | 74.4 | 79.3 | 76.3 | 85.7 |
For each specialty, the case completion rate was calculated by the following formula: (total cases scheduled – cancelled cases + rescheduled cases) / total cases scheduled.
Table 2.
Median Time to Procedure Completion. a
| Median time, d | |
|---|---|
| Head and neck surgery | 56 |
| Sleep surgery | 73 |
| Rhinology and skull base surgery | 71 |
| Facial plastic and reconstructive surgery | 63 |
| Otology and neurotology | 81 |
| Laryngology | 81 |
For each specialty, the median time to procedure completion was calculated from the original case date to the rescheduled case date.
Head and Neck Surgery
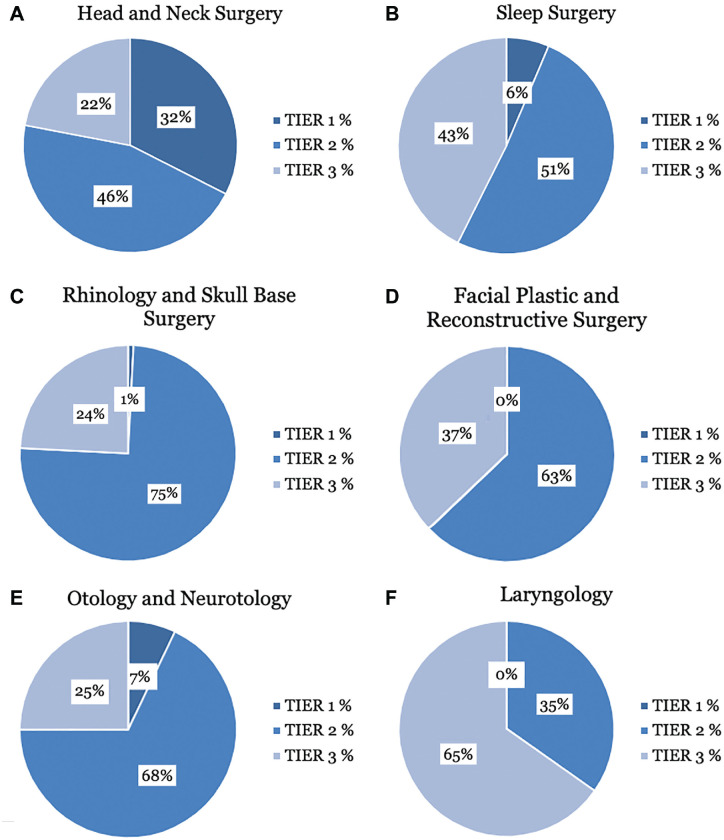
Of the 208 head and neck surgery cases, 89 (42.79%) were cancelled and 79 (88.76%) were rescheduled. Ten (11.24%) head and neck surgery cases were not rescheduled within 6 months of the originally scheduled surgery date. The case completion rate was 95.2%. The median time to procedure completion for rescheduled cases was 56 days. The percentages of tiers 1, 2, and 3 for cancelled cases were 32.5%, 45.5%, and 22%, respectively ( Figure 1A ).
Figure 1.
The distributions of tiers 1, 2, and 3 within each otolaryngology subspecialty.
Sleep Surgery
Of the 199 sleep surgery cases, 167 (83.92%) were cancelled and 107 (64.07%) were rescheduled. Sixty (35.93%) sleep surgery cases were not rescheduled within 6 months of the originally scheduled surgery date. The case completion rate was 69.9%. The median time to procedure completion for rescheduled cases was 73 days. The percentages of tiers 1, 2, and 3 for cancelled cases were 6.4%, 51%, and 42.6% ( Figure 1B ).
Rhinology and Skull Base Surgery
Of the 172 rhinology and skull base cases, 125 (72.67%) were cancelled and 81 (64.80%) were rescheduled. Forty-four (35.20%) rhinology and skull base cases were not rescheduled within 6 months of the originally scheduled surgery date. The case completion rate was 74.4%. The median time to procedure completion for rescheduled cases was 71 days. The percentages of tiers 1, 2, and 3 for cancelled cases were 0.8%, 75%, and 24.2% ( Figure 1C ).
Facial Plastic and Reconstructive Surgery
Of the 150 facial plastic and reconstructive surgery cases, 120 (80.00%) were cancelled and 89 (74.17%) were rescheduled. Thirty-one (25.83%) facial plastic and reconstructive surgery cases were not rescheduled within 6 months of the originally scheduled surgery date. The case completion rate was 79.3%. The median time to procedure completion for rescheduled cases was 63 days. The percentages of tiers 1, 2, and 3 for cancelled cases were 0%, 62.9%, and 37.1% ( Figure 1D ).
Otology and Neurotology
Of the 38 otology and neurotology cases, 27 (71.05%) were cancelled and 18 (66.67%) were rescheduled. Nine (33.33%) otology and neurotology cases were not rescheduled within 6 months of the originally scheduled surgery date. The case completion rate was 76.3%. The median time to procedure completion for rescheduled cases was 81 days. The percentages of tiers 1, 2, and 3 for cancelled cases were 7.1%, 67.9%, and 25% ( Figure 1E ).
Laryngology
Of the 35 laryngology cases, 24 (68.57%) were cancelled and 19 (79.17%) were rescheduled. Five (20.83%) laryngology cases were not rescheduled within 6 months of the originally scheduled surgery date. The case completion rate was 85.7%. The median time to procedure completion for rescheduled cases was 81 days. The percentages of tiers 1, 2, and 3 for cancelled cases were 0%, 34.8%, and 65.3% ( Figure 1F ).
Nosocomial Infection Rate
No patients who underwent surgery during the studied time frame tested positive for COVID-19. In addition, no providers within the otolaryngology department tested positive.
Discussion
Hospital COVID-19 lockdown precautions and cancellation of elective and nonurgent procedures affected many surgical subspecialties. The field of otolaryngology faced a unique challenge of preventing nosocomial spread to patients and providers while handling often time-sensitive procedures. The findings in our study demonstrate that high-priority cases were more frequently completed without cancellation or were rescheduled, whereas specialties that primarily work with noncancer cases faced lower completion rates. In our department, head and neck surgery had the highest number of cases originally scheduled, the lowest number of cases cancelled, and the highest number of cases rescheduled. In contrast, sleep surgery had the most cases cancelled and the fewest cases rescheduled. When compared with head and neck surgery, all other specialties within otolaryngology saw a sharply contrasted rate of patients who did not reschedule within 6 months, with losses 2 to 3 times greater.
The median time to procedure completion for rescheduled cases across all subspecialties was 70 days. Head and neck surgery had the shortest median time to completion at 56 days, and laryngology and otology and neurotology had the longest median time at 81 days. In terms of tier distribution among subspecialties, head and neck surgery had the highest amount of tier 1 cases at 32.5%. Rhinology and skull base surgery had the most tier 2 cases at 75%, and laryngology had the most tier 3 cases at 65.3%. Head and neck surgery had the highest percentage of time-sensitive and oncologic procedures as compared with the other otolaryngology subspecialties, as demonstrated by having the shortest median time to procedure completion ( Table 2 ) and highest proportion of Tier 1 cases ( Figure 1 ). In comparison, more elective subspecialties experienced higher cancellation rates and fewer cases rescheduled. For example, 93% of sleep surgery cases were tier 2 or 3, and this subspecialty experienced the most cases cancelled and the fewest rescheduled. Prior to the lockdown, the otolaryngology department experienced an average cancellation rate of 16.83%.
Since establishing adequate testing and safety protocols for resuming elective surgery, health care systems have faced a significant challenge in reengaging patients across specialties. Tawfik et al reported a backlog >1 million orthopedic cases since the cessation of elective surgery during the initial months of the pandemic. 12 Hesitancy to resume elective cases poses a health-related risk to patients and a financial burden to institutions.12,13 Moverman et al found that over half of patients expressed concern about contracting COVID-19 during hospitalization for elective surgery and fear for exposure of family members in surgical waiting areas. 13 Roughly 46% of patients also stated that they would delay elective surgery >3 months once restrictions were lifted. Our findings seemingly reflect this hesitancy. Subspecialties operating on a more elective basis faced the highest initial cancellation rates, notably facial plastics with 80% of cases initially cancelled. Interestingly, facial plastic and reconstructive surgery cases were more frequently rescheduled than otology, rhinology, and sleep subspecialties. While not analyzed in this study, these disparities in rescheduling are likely multifactorial, such as patient demographics, perceived severity of condition and benefit of surgery, and functional or quality-of-life impact of patients’ conditions. As COVID-19 continues to pose a challenge to the health care field with emergence of new viral variants with successive waves, providers must effectively communicate with patients when faced with diminished resources and actively reengage them when appropriate.
Limitations and Future Directions
This study had several limitations. First, this study represents 1 institution’s experience with case cancellation and rescheduling during the COVID-19 pandemic. Second, the time frame that was analyzed was an institution-specific lockdown between March 16 and May 29, 2020. Hospital safety protocols have constantly and rapidly evolved throughout the pandemic, and surgical delays were most significant in the Philadelphia region at this time. Third, case prioritization for rescheduling was based on many factors, including tiering systems created by the department as well as individual patient preferences. Future studies should aim at investigating patient beliefs and attitudes regarding perceived benefit of interventions as compared with the perceived risk of COVID-19 transmission.
Conclusion
The discrepancies among cancellation, rescheduling, and case completion rate within the otolaryngology subspecialties are multifactorial and likely include surgeon and patient perceptions of time sensitivity of interventions and trepidation regarding nosocomial transmission of COVID-19. Our experience demonstrates that subspecialties that function on a more elective nature faced increased rescheduling difficulty and challenges with patient reengagement during the COVID-19 pandemic. There is an increased need for medical professionals to take an active role in communicating with patients during the remainder of the COVID-19 pandemic to ensure that patients are not lost to follow-up and that time-sensitive and elective surgical procedures are effectively rescheduled.
Footnotes
Author Contributions: Emily S. Sagalow, design, data collection, analysis, manuscript writing; Alexander Duffy, design, data collection, analysis, manuscript writing; Priyanga Selvakumar, design, data collection, analysis, manuscript writing; David M. Cognetti, design, manuscript writing.
Disclosures: Competing interests: None
Sponsorships: None.
Funding source: None
ORCID iD: Emily S. Sagalow  https://orcid.org/0000-0003-4467-3277
https://orcid.org/0000-0003-4467-3277
References
- 1. Fauci AS, Lane HC, Redfield RR. COVID-19—navigating the uncharted. N Engl J Med. 2020;382:1268-1269. doi: 10.1056/NEJMe2002387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Listings of WHO’s response to COVID-19. Accessed February 28, 2021. https://www.who.int/news/item/29-06-2020-covidtimeline
- 3. Ralli M, Minni A, Candelori F, Cialente F, Greco A, de Vincentiis M. Effects of COVID-19 pandemic on otolaryngology surgery in Italy: the experience of our university hospital. Otolaryngol Head Neck Surg. 2020;163(1):86-88. doi: 10.1177/0194599820928970 [DOI] [PubMed] [Google Scholar]
- 4. Lee Y, Kirubarajan A, Patro N, Soon MS, Doumouras AG, Hong D. Impact of hospital lockdown secondary to COVID-19 and past pandemics on surgical practice: a living rapid systematic review. Am J Surg. Published online November 12, 2020. doi: 10.1016/j.amjsurg.2020.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Piccirillo JF. Otolaryngology–head and neck surgery and COVID-19. JAMA. 2020;324(12):1145-1146. doi: 10.1001/jama.2020.15779 [DOI] [PubMed] [Google Scholar]
- 6. Anagiotos A, Petrikkos G. Otolaryngology in the COVID-19 pandemic era: the impact on our clinical practice. Eur Arch Otorhinolaryngol. 2021;278(3):629-636. doi: 10.1007/s00405-020-06161-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Couloigner V, Schmerber S, Nicollas R, et al. COVID-19 and ENT surgery. Eur Ann Otorhinolaryngol Head Neck Dis. 2020;137(3):161-166. doi: 10.1016/j.anorl.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ranney ML, Griffeth V, Jha AK. Critical supply shortages—the need for ventilators and personal protective equipment during the COVID-19 pandemic. N Engl J Med. 2020;382:e41. doi: 10.1056/NEJMp2006141 [DOI] [PubMed] [Google Scholar]
- 9. Gallo O, Locatello LG, Orlando P, et al. The clinical consequences of the COVID-19 lockdown: a report from an Italian referral ENT department. Laryngoscope Investig Otolaryngol. 2020;5:824-831. doi: 10.1002/lio2.446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fan T, Workman AD, Miller LE, et al. The impact of COVID-19 on otolaryngology community practice in Massachusetts. Otolaryngol Head Neck Surg. Published online February 2, 2021. doi: 10.1177/0194599820983732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brar S, Ofo E, Hyde N, et al. Outcomes of elective head and neck confirmed or suspected cancer surgery during the COVID-19 pandemic. Eur Arch Otorhinolaryngol. Published online July 15, 2020. doi: 10.1007/s00405-020-06194-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tawfik AM, Silver JM, Katt BM, Patankar A, Rivlin M, Beredjiklian PK. Patient perceptions of COVID-19 precautions and their effects on experiences with hand surgery. J Hand Surg Glob Online. 2021;3(4):167-171. doi: 10.1016/j.jhsg.2021.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moverman MA, Puzzitiello RN, Pagani NR, Barnes CL, Jawa A, Menendez ME. Public perceptions of resuming elective surgery during the COVID-19 pandemic. J Arthroplasty. 2021;36(2):397-402.e2. doi: 10.1016/j.arth.2020.07.037 [DOI] [PMC free article] [PubMed] [Google Scholar]