Abstract
Vitellointestinal duct anomalies, although one of the most frequent malformations to be found (2%–3% in population), they are most unlikely to cause symptoms. A persistent Vitellointestinal duct can induce abdominal pain, bowel obstruction, intestinal haemorrhage and umbilical sinus, fistula or hernia which commonly occurs in children. Patent vitellointestinal duct or persistent omphalomesenteric duct is a very unusual congenital anomaly which occurs in 2% of the population related to the embryonic yolk stalk. Similarly, urachal anomalies remain a rare finding, with the most common being a cyst or sinus followed by patent urachus and rarely a urachal diverticulum. Presenting symptoms include periumbilical discharge, pain and a palpable mass.
Here, we report a case of an adult patient with patent vitellointestinal duct and urachus identified intraoperatively on diagnostic laparoscopy when being operated for umbilical hernia repair.
Keywords: General surgery, Small intestine
Case presentation
A man in his 60s with no comorbidities, came with complaints of reducible swelling in the umbilical region since the past 1 year. He had right lower abdominal pain without any precipitating or relieving factors and had no nausea, vomiting, constipation, obstipation or fever.
There was no history of chronic cough, lifting heavy weights or any problems with micturition.
He denied any addictions as smoking or alcohol consumption and did not have any abdominal surgery in past. He had no known allergies.
On examination, the patient was haemodynamically stable with soft non distended abdomen with partially reducible swelling in umbilicus with a defect of 2 cm. There was expansile impulse on coughing at the umbilicus without any divarication of rectus.
History and clinical findings were all pointing towards the diagnosis of an uncomplicated partially reducible umbilical hernia.
Investigations
Routine investigation such as a complete haemogram, liver function tests, renal function tests, coagulation profile, ECG, chest and abdominal radiographs were within normal limits.
Ultrasonography of the abdomen revealed a 2 centimetres (cms) defect with a partially reducible omentum as content. As the diagnosis seemed straight forward, computerised tomography (CT scan) was not done in this case.
Differential diagnosis
Clinical and sonography findings were straight forward and were suggestive of partially reducible umbilical hernia.
Treatment
The patient was planned for laparoscopic underlay prosthetic repair (Lap IPOM Plus). Pneumoperitoneum was created with Veress needle at Palmers point. A 10 mm optical port was introduced in left anterior axillary line between subcostal and anterior superior iliac spine and two working ports on either side of the same about 5 cm away more medial to the first port to have triangulation. The laparoscopic findings were suggestive of an umbilical defect with urachal remnants and a patent vitellointestinal duct herniating through it (figures 1A, B and 2). The urachus and vitellointestinal duct were adherent to each other. The procedure was converted to a mini laparotomy and meticulous dissection was done to separate the VI duct and urachus. The urachus was traced back to the bladder and oversewn with POLYDIOXANONE 2.0 (synthetic delayed absorbable monofilament suture). The vitellointestinal duct was traced back to the antimesenteric border of ileum about 2.5 ft proximal to ileocecal junction. It was resected along with a wedge of the ileum and sutured in 2 layers with 3.0 SILK (non-absorbablemultifilament sutures). The abdomen was closed with delayed absorbable POLYDIOXANONE N0 1 in continuous monolayer and any use of prosthesis was deferred in view of bowel resection.
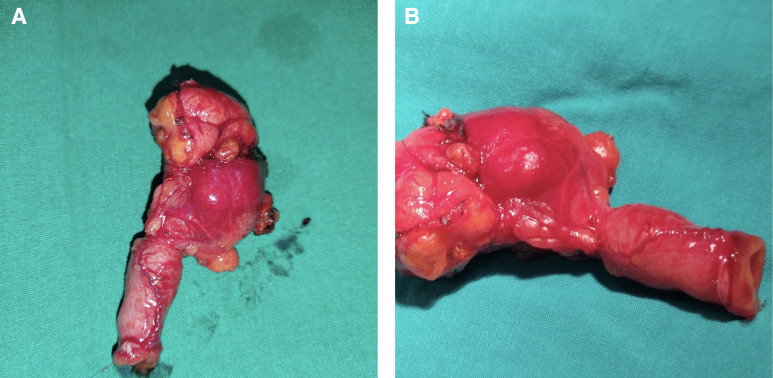
Figure 1.
(A, B) Resected specimen showing ileal segment containing patent vitellointestinal duct and the urachus.
Figure 2.
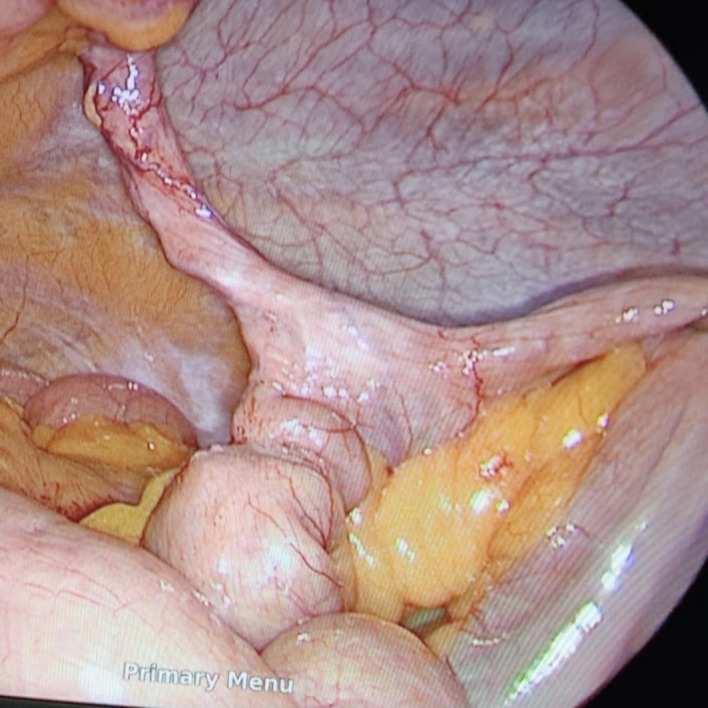
Intraoperative photograph of the vitellointestinal duct and the urachus, which were contents of the umbilical hernia.
Outcome and follow-up
The patient had an uneventful recovery with orals started on day 3 and discharged on postoperative day 6. Histopathology confirmed patent vitellointestinal duct with lining of intestinal type mucosa with pancreatic tissue within wall in between.
Discussion
Umbilical hernia is a common surgical problem encountered in outpatient departments. The content of the hernia in majority of the cases is omentum, preperitoneal fat and small intestine.1
During the course of normal development the vitellointestinal duct regresses and obliterated urachus remains as the median umbilical ligament (figures 3–5, drawn by VBS). Omphalomesenteric duct malformations2 comprise a wide spectrum of an anatomic structures and associated symptoms. They may range from a completely patent omphalomesenteric duct at the umbilicus to a variety of lesser remnants including cysts, fibrous cords connecting the umbilicus to the distal ileum, granulation tissue at the umbilicus, umbilical hernias, and the famous diverticulum of Meckel. Patients may be either totally asymptomatic or can present with faecal fistulas at the umbilicus, intussusception of ileum at the umbilicus, intestinal obstruction from a variety of causes, malena, anaemia and abdominal pain due to inflammation.3 Although symptoms most frequently occur during childhood years (especially first 2 years of life), they make occur through adult years as well.4
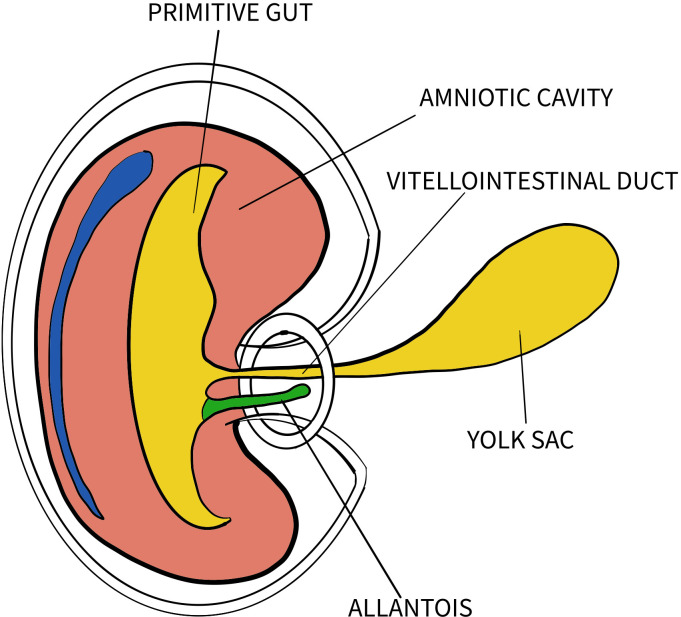
Figure 3.
Diagram showing primitive umbilical cord (drawn by VBS).
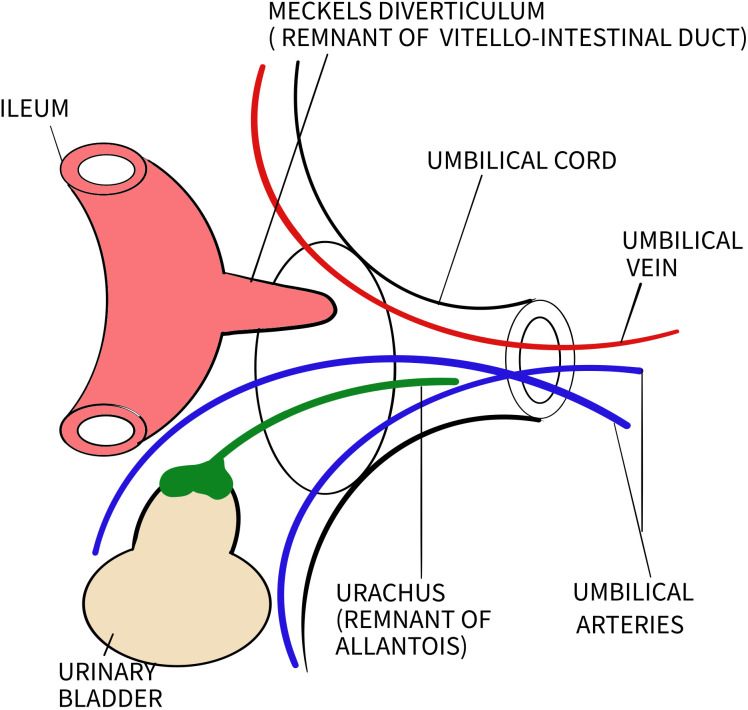
Figure 4.
Diagram showing definitive umbilical cord (drawn by VBS).
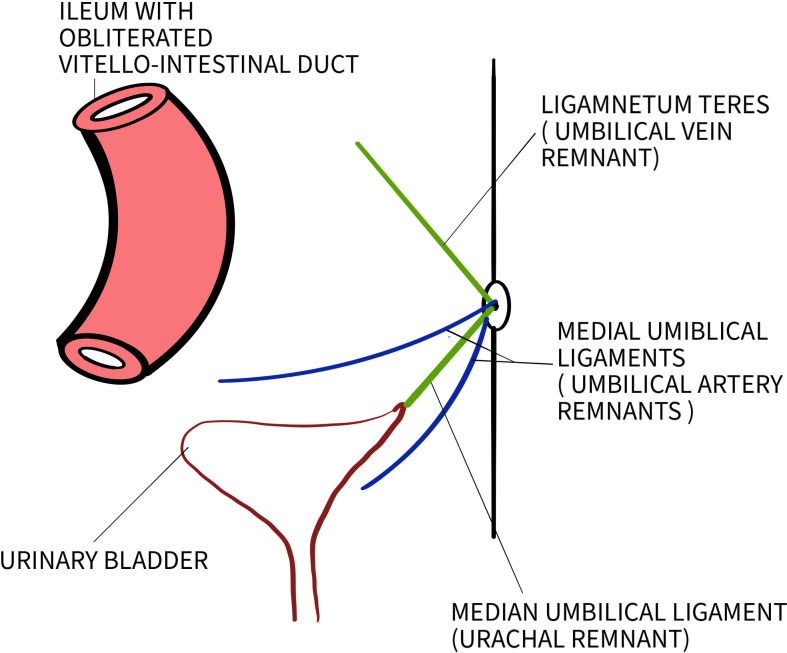
Figure 5.
Diagram showing normal anatomy of umbilicus (drawn by VBS).
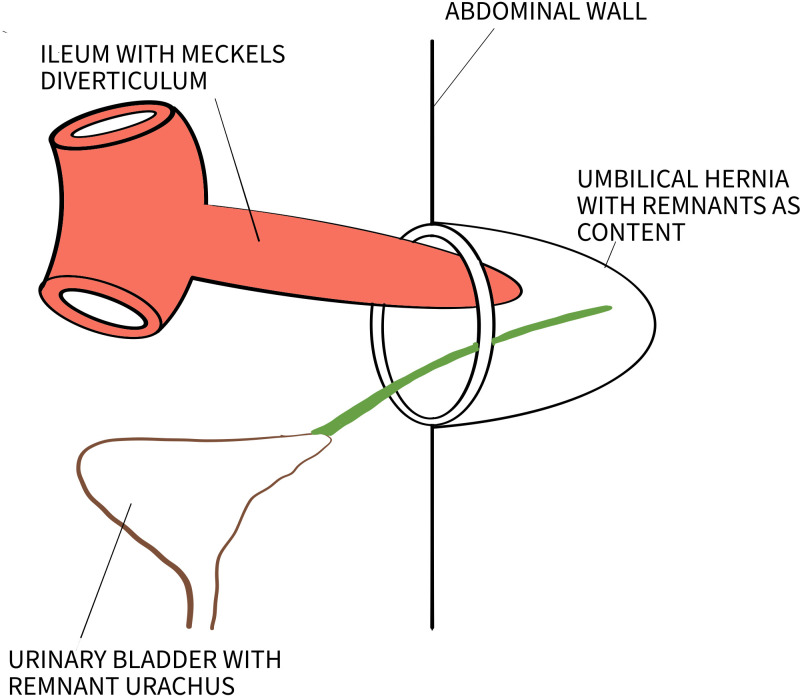
Our patient presented with umbilical hernia with no other symptoms or clinical findings. The association of a hernia with urachus or vitellointestinal duct is rare (figure 6, drawn by VBS) and can pose diagnostic dilemmas.5 CT scan of the abdomen would have helped preoperative diagnosis, however, in absence of any symptoms was deferred in our patient. The finding could have still been missed, if an external approach (not involving opening of the sac) been adopted for the repair.
Figure 6.
Diagram showing both remnants as part of umbilical hernia (drawn by VBS).
Many studies have mentioned different approaches for symptomatic persistent vitellointestinal duct such as open surgical excision or laparoscopic excision.6 7 Review of literature suggested complete resection up to the bladder dome in management of urachal remnant in adults.8 Incomplete resection of these remnants carries risk for recurrent symptoms and potential for malignant transformation.9
Patient’s perspective.
I started developing mild pain in the abdomen and noticed a swelling at my umbilicus a year back. On consulting my local doctor, I got to know that it was a hernia and that I need to get it repaired or I may land up in problems. Hence, I consulted a surgeon and wished to get myself operated. All my tests were perfect, and the operation was performed. I was told later that things were not as simple as the surgeon expected it to be. I was told that a Ct scan before the surgery could have predicted what was to lie inside and so I wondered why it wasn’t done.
I was explained that it is not routine practice, especially considering that what was found in the hernia was not common. I was relieved to hear that I got rid of two problems with one surgery especially after getting to know what problems the contents removed could have caused later. I thanked my surgeon for a successful surgery. (Translated from Marathi)
Learning points.
In conclusion, urachal and vitellointestinal duct anomalies are rare and rarest when it is associated with an umbilical hernia. So, the diagnosis needs to be kept in mind.
The diagnosis of this condition clinically is difficult and may remain presumptive until clearly confirmed by imaging and surgical finding.
Imaging modalities like ultrasonography and CT scan should be used to confirm the diagnosis with high index of suspicion.
The suggested management remains complete resection to avoid future problems of recurrence of symptoms or malignancy.
Footnotes
Contributors: Conceptualisation: SAR, VBS. Original draft preparation: VBS, MJ. Review and editing: SAR.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
References
- 1.Kulaçoğlu H. Current options in umbilical hernia repair in adult patients. Ulus Cerrahi Derg 2015;31:157–61. 10.5152/UCD.2015.2955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sawada F, Yoshimura R, Ito K, et al. Adult case of an omphalomesenteric cyst resected by laparoscopic-assisted surgery. World J Gastroenterol 2006;12:825. 10.3748/wjg.v12.i5.825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vane DW, West KW, Grosfeld JL. Vitelline duct anomalies. experience with 217 childhood cases. Arch Surg 1987;122:542–7. 10.1001/archsurg.1987.01400170048007 [DOI] [PubMed] [Google Scholar]
- 4.Moore TC. Omphalomesenteric duct malformations. Semin Pediatr Surg 1996;5:116–23. [PubMed] [Google Scholar]
- 5.Gregory GC, Vijay R, Ligaj M, et al. Laparoscopic management of urachal cyst associated with umbilical hernia. Hernia 2011;15:93–5. 10.1007/s10029-009-0618-7 [DOI] [PubMed] [Google Scholar]
- 6.Bueno Lledó J, Serralta Serra A, Planeéis Roig M, et al. Intestinal obstruction caused by omphalomesenteric duct remnant: usefulness of laparoscopy. Rev Esp Enferm Dig 2003;95:736–8. [PubMed] [Google Scholar]
- 7.Nursal TZ, Yildirim S, Tarim A, et al. Laparoscopic resection of patent omphalomesenteric duct in an adult. Surg Endosc 2002;16:1638. 10.1007/s00464-002-4209-2 [DOI] [PubMed] [Google Scholar]
- 8.Siow SL, Mahendran HA, Hardin M. Laparoscopic management of symptomatic urachal remnants in adulthood. Asian J Surg 2015;38:85–90. 10.1016/j.asjsur.2014.04.009 [DOI] [PubMed] [Google Scholar]
- 9.Chiarenza SF, Bleve C. Laparoscopic management of urachal cysts. Translational Pediatrics 2017;5:275–81. 10.21037/tp.2016.09.10 [DOI] [PMC free article] [PubMed] [Google Scholar]