Abstract
Objectives
The health effects of work-time arrangements have been largely studied for long working hours, whereas a lack of knowledge remains regarding the potential health impact of reduced work-time interventions. Therefore, we conducted this review in order to assess the relationships between work-time reduction and health outcomes.
Design
Systematic review of published studies. Medline, PsycINFO, Embase and Web of Science databases were searched from January 2000 up to November 2019.
Outcomes
The primary outcome was the impact of reduced working time with retained salary on health effects, interventional and observational studies providing a quantitative analysis of any health-related outcome were included. Studies with qualitative research methods were excluded.
Results
A total of 3876 published articles were identified and 7 studies were selected for the final analysis, all with a longitudinal interventional design. The sample size ranged from 63 participants to 580 workers, mostly from healthcare settings. Two studies assessed a work-time reduction to 6 hours per day; two studies evaluated a weekly work-time reduction of 25%; two studies evaluated simultaneously a reduced weekly work-time reduction proportionally to the amount of time worked and a 2.5 hours of physical activity programme per week instead of work time; one study assessed a reduced weekly work-time reduction from 39 to 30 hours per week. A positive relationship between reduced working hours and working life quality, sleep and stress was observed. It is unclear whether work time reduction determined an improvement in general health outcomes, such as self-perceived health and well-being.
Conclusions
These findings suggest that the reduction of working hours with retained salary could be an effective workplace intervention for the improvement of employees’ well-being, especially regarding stress and sleep. Further studies in different contexts are needed to better evaluate the impact of work-time reduction on other health outcomes.
Keywords: occupational & industrial medicine, public health, health & safety, health policy
Strengths and limitations of this study.
This is the first systematic review carried out in English to evaluate the impact of reduced working hours on both self-reported and measured health outcomes.
All of the included studies had a longitudinal design, and in all studies except two the employment of extrapersonnel allowed to prevent a compensatory increase in workload, which may have limited the effectiveness of work-time reduction.
The included studies were carried out in the Scandinavian setting, thus limiting the generalisability of the results in other contexts, different from a social, cultural and economic point of view.
Three out of seven studies had a weak quality according to the authors, and most of the studies were carried out in the healthcare setting.
Introduction
In Organisation for Economic Cooperation and Development (OECD) countries, the average working week consists of 37 hours.1 OECD data on annual average working hours show that, despite a declining trend in the amount of worked hours, many Countries still exceed the standard.2 Working long hours is widely recognised as detrimental for employees’ health. Indeed, several studies investigating the health effects of working overtime reported concerning findings, including increased risk of stroke, coronary heart disease, anxiety, depression, sleep disorders and adverse pregnancy outcomes in women.3–5 Furthermore, a systematic assessment of evidence in literature with meta-analyses conducted by Rivera et al found moderate-grade evidence linking long work-hours with stroke and low-grade evidence on the association between long work-hours with coronary disease, depression and pregnancy complications, including low birthweight babies and preterm delivery.6 Long working hours have also been associated with reduced levels of work–life balance and increased work–family conflict.7
Conversely, the effects of reduced work-hours (RWH) have not been extensively examined as for long work-hours so far. Indeed, several experiments of reducing working time have been conducted throughout the years, both in the public and private sector. One of the most notable examples was the adoption of the ‘35-hour workweek’ between 1998 and 2000 by the French Government, which allowed the reduction of weekly working hours from 39 to 35, with the aim of fighting the high unemployment rates. However, aside from two surveys examining employees’ satisfaction with modified work-hours and their work-family conflict, no other impacts on health and well-being have been evaluated.8 9 The authors argue that the French 35-hour law increased overall dissatisfaction with modified work hours among employees, mainly because it did not take into account the heterogeneity of work organisation. It appears that employees increased workload to maintain high productivity. Indeed, reducing working time without employing extrapersonnel may compromise the fine balance between job demand and resources, which in turn would undermine employees’ wellbeing.10 Further interventions have been carried out on a company level. In Germany, Volkswagen reduced the working week from 36 to 28.8 hours11 and more recently, Microsoft Japan tested a 4 days work week.12 Similarly, Perpetual Guardian, a New Zealand firm operating in the management of trusts, wills and estates, ran a 4-day work week trial for all its 240 employees.13 Although companies reported successful results, they did not take into consideration the potential health impact of these experiences.
Besides, there are few studies even in scientific literature that investigate the role of RWH on workers’ health. To our knowledge, only one literature review was conducted in 2005 and authors concluded that no relevant effects on health were observed.14 However, the review was published in Swedish, hence it may represent an issue due to language barriers. Furthermore, the studies included in their work were mostly reports from Swedish ministerial committees and critical reviews on work time arrangements. Indeed, in the studies published before 2000 authors were primarily interested in the economic consequences of reducing work-hours, exploring the feasibility of the project, and little attention was paid to the effects of work-time reduction on the health of employees. Since 2000, several interventional studies have been published. Therefore, we decided to conduct a review of the literature examining studies focusing on the relationship between RWH and health effects, published since 2000, in which employees retained their salary and proportionally decreased their work time and workload.
Methods
Search strategy
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist, we carried out a literature search for articles published in Medline, PsycInfo, Embase and Web of Science databases from January 2000 up to November 2019. Search terms included terms like ‘work’, ‘health’, ‘well-being’, ‘mental-health’, ‘worktime reduction’, ‘reduced work hours’. Full search strings for each database are provided in online supplemental file 1. First, duplicates were excluded. Next, AS, DC, EB and GV independently screened retrieved sources by title and abstract following inclusion criteria. The same authors, always in an independent fashion, performed a full text review. Finally, consensus was reached through discussion about uncertain cases between all reviewers. Authors chose Rayyan QCRI as a tool for selecting and extracting relevant records.15
bmjopen-2021-051131supp001.pdf (50.8KB, pdf)
Inclusion and exclusion criteria
We decided to include primary sources in any form, both interventional and observational studies, provided that quantitative analysis of any health-related outcome were performed. Hence, studies with qualitative research methods were excluded because we were interested on the effects of the interventions in terms of quantitatively measured outcomes. Articles had to investigate the association between reduced working time with retained salary and health effects, without excluding beforehand any category of workers. No salary reduction was considered crucial in order to avoid a selection bias possibly leading to exclude low-income workers. Another inclusion criterion was the replacement of working activity with any workplace-based intervention, provided that the amount of work hours was effectively reduced. Conversely, studies specifically focused on work-time reduction policies regarding activities with excessively long working hours, such as medical residency, were not consistent with the concept of RWH and retained salary and were therefore excluded from our work. No language restriction was set. Due to the heterogeneity in the outcomes evaluated by the studies selected, a meta-analysis of data could not be conducted. Data and information regarding study design, country, participant characteristics, observation period, intervention description, outcomes measured and results were extracted and synthesised in a systematic literature review.
Quality assessment
The quality of the included studies was assessed using the ‘Quality Assessment Tool for Quantitative Studies’ developed by the Effective Public Health Practice Project.16 This quality appraisal tool provides a standardised means to assess study quality and develop recommendations for study findings considering eight components of study methodology: selection bias, study design, presence of confounders, blinding of participants and outcome assessors, validity and reliability of data collection methods and study dropouts and withdrawals. The overall quality of each study is then expressed as weak, moderate or strong. Previous evaluation of the tool has shown it to be valid and reliable.17 Two reviewers, namely AS and SR, independently performed quality assessment. Discrepancies between the reviewers, such as differences in interpretation of criteria and studies, were resolved by discussion in order to reach consensus.
Patient and public involvement
No patient involved. Results will be disseminated throughout conferences and social media in order to enrich public debate on health outcomes of working hours rearrangements.
Results
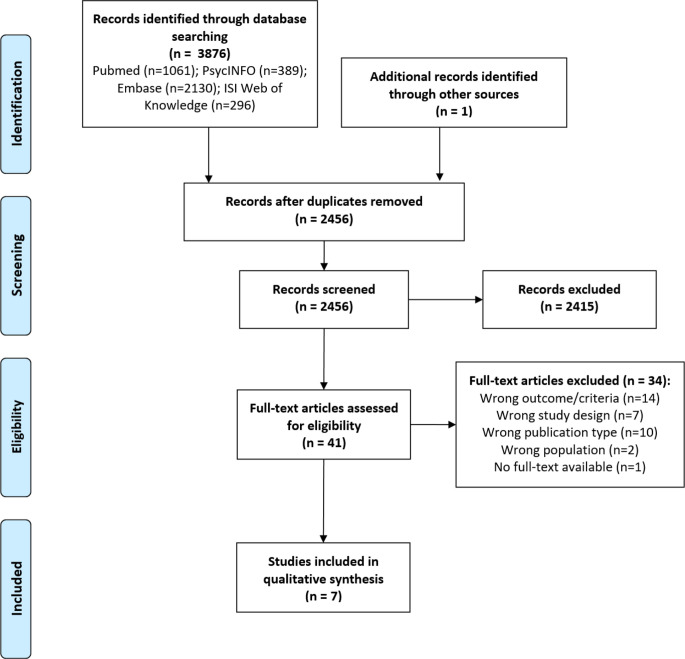
As results of the bibliographic search, a total of 3876 published articles were identified (figure 1).
Figure 1.
Systematic review: selection process. From: Moher D, et al.31
Duplicates were excluded and remaining 2456 records were reviewed. A full-text review was conducted on 40 articles. Finally, after evaluating the inclusion criteria, seven articles were selected (one article was originally added by citation chasing). In total seven articles, with a longitudinal interventional design, were included in the final analysis.18–24 A brief summary of included articles is provided in table 1.
Table 1.
Characteristics of the studies included in systematic review
| Author | Study Design |
Country and participants | Observation period | Intervention description | Outcome (measures) | Results | Quality assessment rating |
| Åkerstedt et al, 200124 | Longitudinal intervention study | Sweden, N=63, full-time workers in healthcare service. | 36 months | Intervention group (N=41): reduced WWH from 39 hrs/week to 30 hrs/week. Control group (N=22): unchanged working time. |
|
Subjective sleep quality (SSQ), mental fatigue and heart/respiratory symptoms, time for social activity, time for family and friends improved significantly more in the experimental group than in the control group. No significant effects for sickness absence or self-rated health. | Weak |
| Wergeland et al, 200322 | Longitudinal intervention study | Norway and Sweden, N=403. Workers in nursing homes, home care services and kindergartens |
12–22 months | Intervention group: reduced DWH to 6 hrs/day. Reference group: unchanged working time. |
|
A significant interaction was found for neck-shoulder pain and for exhaustion after work in the intervention group. No significant effects were observed in the reference group. |
Weak |
| von Thiele Schwarz et al, 200820 | Longitudinal intervention study | Sweden, N=177 employees from six workplaces at public dental healthcare organisation | 12 months | PE group: 2.5 hrs/week of physical activity instead of work time. Reduced work hours group: reduced WWH proportionally to the amount of time worked. Reference group: unchanged working time. |
|
Physical activity level increased in all three groups but significantly more in PE group. Glucose levels and upperextremity disorders were found to be significantly decreased in the exercise group, while a significant increase in HDL and waist-to-hip ratio was found among those working reduced hours. Participants working reduced hours also had significantly increased total cholesterol, while no changes in LDL-to-HDL ratio were recorded. |
Strong |
| von Thiele Schwarz et al, 201121 | Longitudinal intervention study | Sweden, N=177 employees from six workplaces at a public dental healthcare organisation | 12 months | PE group: 2.5 hrs/week of physical activity instead of work time. Reduced work hours group: reduced WWH proportionally to the amount of time worked. Reference group: unchanged working time. |
|
Physical activity was significantly associated with an increase in self-rated productivity in terms of increased quantity of work and work-ability and decreased frequency and number of days of sickness absence. No effect was found in the work hours reduction group. In all three groups there was an increase in the number of treated patients per therapist, significantly greater in the reduced work hours group. | Strong |
| Barck-Holst et al, 201718 | Longitudinal quasi-experimental trial | Sweden, N=204 A total of 125 participants were deemed as per protocol |
18 months | Intervention group: reduced work hours by 25%. Reference group: unchanged working time. |
|
The intervention group significantly improved restorative sleep, stress, memory difficulties, negative emotion, sleepiness, fatigue and exhaustion on both work days and weekends. Improved demands, instrumental manager support and work intrusion on private life were observed to be significantly higher in the intervention group. | Moderate |
| Lorentzon 201723 | Longitudinal intervention study | Sweden, N=124, nurses working in a centre for the elderly | 23 months | Intervention group: work-time reduction to 6 hours/day. Reference group: unchanged working time. |
|
Good perceived health and alertness level, satisfactory level of perceived fatigue. Energy left at home, feeling calm, satisfactory levels of stress, average sleep time increased in intervention group. General symptoms, sleep and musculoskeletal symptoms improved in the intervention group, and dropped in the control group. Collaboration and personal development improved; improved sense of collaboration between nurses. Sick leave increased in the intervention group. No inferential statistics provided. |
Weak |
| Schiller et al, 201719 | Longitudinal controlled intervention study | Sweden, N=580, workers from 33 workplaces in the public sector | 18 months | Intervention group: reduced WWH by 25%. Reference group: unchanged working time. |
|
On workdays, the intervention group displayed significantly improved SSQ, decreased sleepiness and perceived stress, less feelings of worries and stress at bedtime when work hours were reduced. Also, a significant 23 min extension of sleep duration was detected. The intervention showed similar positive effects on days off, except for sleep duration. |
Strong |
HDL, high-density lipoprotein; LDL, low-density lipoprotein; PE, physical exercise; WWH, weekly worked hours.
The included studies were published between 200124 and 201718 19 23 and they were performed in northern Europe.18–24 The sample size ranged from 63 participants24 to 580 workers,19 mostly from healthcare settings.20–24 Only one of the included studies enrolled workers from different workplaces in the public sector (Schiller et al).19 All the studies included had a longitudinal design and the observation period was between 12 months20–22 and 23 months.23 Although all the studies compared the intervention group to a control group with no work-time modifications, the intervention exanimated were different. In particular, two studies assessed a work-time reduction to 6 hours per day,22 23 two studies evaluated a weekly work-time reduction of 25%,18 19 two studies evaluated simultaneously a reduced weekly work-time reduction proportionally to the amount of time worked (RWH group) and a 2.5 hours per week physical activity instead of work time programme (physical exercise group, PE)20 21 and one study assessed a reduced weekly work-time reduction from 39 to 30 hours per week.24 The included studies assessed a variety of different outcomes. In particular general symptoms,20 23 24 neuropsychological symptoms,18 23 24 working life quality,18 20–24 quality of life,18 23 24 physical activity,20 23 24 sleep,18 19 23 24 musculoskeletal disorders20 22 23 and biological markers20 were assessed. After quality assessment phase, overall quality was found to be strong for three studies,19–21 moderate for one study23 and weak for three studies.22–24
In particular, Åkerstedt et al performed a longitudinal cohort study in five different healthcare settings, in order to compare the effects of work-hours reduction among healthcare and day care nursery personnel.24 The study involved a total of 63 nurses, 41 in the experimental group, a 9 hours reduction of the working week from 39 hours per week to 30 hours, retaining full pay, and 22 in the control group. The experimental group showed a significant improvement for heart/respiratory symptoms, mental fatigue, sleep quality, time for social, time for family/friends, influence on work-hours and satisfaction with work-hours. Additionally, most of these variables also showed a significant change over time. Furthermore, there was a positive change over time for pain/ache complaints, nervous symptoms, gastrointestinal complaints, insomnia complaints, refreshed at awakening, sleepiness at work/leisure time, involuntary sleep at work and leisure time and satisfaction with the work situation. On the contrary, no significant interaction was found between RWH and exercise, weight and body mass index.24
Similar results were published by Barck-Holst et al.18 They performed a longitudinal quasi experimental study involving seven public social service agencies. Employees in the intervention group reduced their work hours by 25% but retained their previous salary and their organisations were fully reimbursed and staff to compensate the loss of work hours was hired. After controlling for baseline values, gender and age, there was a significant difference in change over time between intervention and control group during workdays on the restorative sleep index, average stress level, the stress index, the memory difficulties index, the negative emotion index, average sleepiness and the fatigue and exhaustion index.18
In addition, a longitudinal controlled intervention study evaluating a 25% reduction of weekly work hours was published in 2017 by Schiller et al. In this paper, participants worked at 33 different workplaces, in four sectors: social services (n=170); technical services (n=236); care and welfare (n=159); call-centre (n=71). The intervention group (n=370) reduced work-time to 75% with preserved salary during 18 months. Data were collected at baseline (1–2 months before the intervention) and approximately 9 months and 18 months after the introduction of RWH. On workdays, the intervention group (N=354) displayed improved subjective sleep quality (SSQ), 23 min extended sleep duration (over the whole period of 18 months), decreased sleepiness and perceived stress and less feelings of worries and stress at bedtime when work hours were reduced (p<0.002). Gender, age, having children living at home, and baseline values of sleep quality and worries and stress at bedtime, considered as additional between-group factors, did not influence the results significantly.19
Similar outcomes were assessed in a cohort study, performed between February 2015 and December 2016 by Lorentzon.23 In this paper, 68 nurses from the intervention group had their working time reduced to 6 hours per day with retaining their full-time pay. On the contrary, nurses in the control group (n=56) had no working hours reduction. Outcomes were assessed using several questionnaires before, during and after the experimentation. In particular, the sick leave was 6.1% in the intervention group and 12.3% in the control group. Furthermore, health perceived as good (72% vs 60%), alertness level perceived as good (65% vs 50%), satisfactory level of perceived fatigue (+20% vs −22%), feeling having a lot of energy left when arriving at home (51% vs 7%, both starting from 20%), feeling calm (64% vs 45%), satisfactory levels of stress (+20%, −5%), average sleep time (7 hours vs 5.8 hours) had better values in the intervention group compared with the control group. Additionally, in the intervention group, satisfaction regarding physical activity increased (+7% vs −15%). Finally, general symptoms, sleep and symptoms affecting the musculoskeletal system improved in the intervention group, and dropped for the control group.23 Unfortunately, no statistical inference was provided by Authors.
Similarly, a previous paper assessing the occurrence of musculoskeletal disorders in the experimental and control groups was published by Wergeland et al.22 In their longitudinal intervention study, involving subjects enrolled from different institutions, workers in the experimental group had their daily work-hours reduced to 6 hours, with retained salary and extrapersonnel employed to compensate for the reduction in work-hours. Participants were involved through a self-administered questionnaire about pain in the neck-shoulder and back regions prior to and during the work-time reduction. By using a multivariable analysis on data from all the institutions, authors found a significant interaction for neck-shoulder pain (p=0.034) and exhaustion after work (p=0.009). No significant interaction was found for back pain. Additionally, the intervention group showed increased job satisfaction after the reduction in work-hours.22
Finally, von Thiele Schwarz et al performed two longitudinal studies in Stockholm, Sweden, involving employees from six workplaces in a large public dental healthcare organisation, randomly allocated to one of three groups: PE group, RWH group, and reference group (R).20 21 At the two workplaces acting as reference, no intervention was carried out; at the two workplaces in the PE group, 2.5 hours of weekly work hours were allocated to mandatory PE on two different days; at the two workplaces in the RWH group, full-time weekly hours were reduced from 40 hours/week to 37.5 hours/week. All employees in the intervention groups retained their salaries, and no additional personnel were employed. The final sample consisted of 177 employees, mainly women. Participants were instructed to complete self-ratings at baseline, after 6 months and after 12 months.20 21
In the paper published in 2008,20 blood samples were and questionnaire were used to explore the areas of physical activity, recovery from work stress, work-home interference, self-related health, work ability, general and musculoskeletal symptoms. The results showed a significant increase in PE in all three groups over time, with post hoc tests showed that the increase in the PE group was significantly greater than in the other two groups. Additionally, the analysis showed increasing levels of all of the blood lipids in the reference group (p<0.001, for total cholesterol; p=0.016, for triglycerides; p=0.003, for high-density lipoprotein (HDL); p<0.001, for low-density lipoprotein (LDL)). In the RWH group, total cholesterol and HDL had increased significantly (p=0.019, for total cholesterol; p=0.016, for HDL), while only total cholesterol had increased significantly in the PE group (p=0.018). Glucose showed a significant time ×group effect (p=0.04), and a significant decrease in the PE group (p=0.036). Work ability decreased in the reference group (p=0.005); similar results were found for general symptoms.20
In the paper published in 2011,21 three outcomes were measured: on-the-job productivity, measured with a single item asking the respondents to rate their current work ability as compared with their individual best work ability on a 10-point scale; sickness presenteeism and sickness absenteeism, assessed with three questions; objective production levels, in terms of the number of treated patients and the number of therapists per month for each participating worksite as well as for all worksites combined. The results showed a significant increase in self-rated quantity of work (p=0.029) and work ability (p=0.046) in the PE group. Work ability decreased significantly in the reference group (p=0.004). In the PE group, frequency of sickness absence (p=0.037) and sickness duration (p=0.029) decreased significantly. In the reference group changes in sickness absence duration (p=0.041) and sickness presenteeism (p=0.028) were each significant.21
Discussion
The purpose of this review was to analyse the results of studies conducted in order to explore the consequences of work time reduction on health outcomes, which is an emerging and debated issue especially in western countries with a developed welfare system, as the ones in Northern Europe. Unfortunately, there is no standard health outcome in the literature that can be used as a comparison in all studies to investigate the effects of reducing working hours on workers' health such as self-perceived health and well-being. Then, we analysed seven published articles exploring several different health outcomes, and all of them were investigated and discussed.
General and physical symptoms
Four longitudinal studies analysed the relationship between work-time reduction and a broad spectrum of general and physical symptoms. Åkerstedt et al24 found a significant improvement of hearth/respiratory symptoms in the experimental group compared with the control group. However, when self-rated health was explored as an outcome, they did not find any statistically significant differences before and after the intervention, neither between the experimental and the control group, nor over time among the same group. Similar results were obtained by von Thiele Schwarz et al, which did not find any significant differences between the intervention and the reference group regarding neither general symptoms nor self-rated health.20 As the Authors suggest, the lack of significant results could be explained by the fact that the study was carried out on healthy subjects, consequently reducing the effect size, especially for self-ratings. On the other hand, Lorentzon et al found an improvement in perceived health in the intervention group compared with the control group.23 Wergeland et al, in their three-project study, found a significant reduction of neck/shoulder and back pain prevalence in the intervention group,22 in agreement with Lorentzon,23 possibly due to a reduction of time spent in the sitting position during work-time.
Data are still contradictory and it is possible to hypothesise that the real impact of workload reduction on general and physical symptoms, despite having a possible effect on specific physical symptoms, remains to be determined through further larger studies.
Neuro-psychological symptoms
Four studies evaluated the relationship between work-time reduction and neuro-psychological symptoms.18 19 23 24 General stress was the most frequently explored outcome. Barck-Holst et al found an average stress level and a stress index significantly decreased in the intervention group, but this difference was higher on workdays compared with weekends.18 This is consistent with the results of Schiller et al, who found a significant reduction of stress both during the day and at bedtime in the intervention group.19 Lorentzon found that workers with reduced work-time reported satisfactory levels of stress and perceived fatigue more often in comparison with workers in the control group.23 Åkerstedt et al found a significant reduction of mental fatigue in the experimental group.24 In addition, they found a reduction of nervous symptoms and pain/ache complaints over time, but this difference was not significant between the experimental and the control group. As the authors suggest, the project in itself may have increased the awareness of work organisation and health, with positive effects on both groups.24
Globally, these results suggest that the reduction of work-time is associated with a significant improvement in stress and other neuropsychological symptoms, probably due to the decrease of workload and the consequent increase of free time for leisure activities.
Sleep
Sleep condition was evaluated in five studies.18–20 23 24 Åkerstedt et al and Schiller et al measured SSQ using the same items and improvements were observed significantly more in the intervention group than in the reference group.19 24 Similar results were reported by Barck-Holst et al.18 In their study on nurses, Lorentzon et al found that those nurses working less hours as a part of the experiment averagely slept more than nurses who kept working with regular hours.23 von Tiele et al evaluated the presence of sleep disturbances as part of a more comprehensive questionnaire—a modified version of QPSNordic—investigating general symptoms.20 25 Although they found no improvements in the experimental group regarding general symptoms, we cannot tell whether the occurrence of sleep disturbances taken alone differed among their participants. Despite different measurements being adopted, almost all studies found a significant improvement in sleep among intervention groups compared with control groups. As already reported by previous research, long working hours have shown to negatively influence sleep in many ways26 27 and this effect may be explained by higher work demands and work-related stress.28 Thus, we hypothesise that the positive effects of reduced work-time on stress and workload may explain the positive effects on sleep.
Quality of working life
All studies except one investigated whether RWH had measurable effects on working life quality.18–20 22–24 Åkerstedt et al found no effects on work demands, but workload had decreased for both intervention and control group.24 As hypothesised by the authors, it is possible that an increased awareness of work organisation following the experiment may be the cause of such findings.24 No effects on sickness absence were found, as opposed to von Tiele Schwarz and Hasson, where employees in the intervention group decreased frequency and number of days of sickness absence, as well as perceiving improved self-rated work ability.21 Other work-related factors were reported as significantly improved after the experiment, including exhaustion after work, sense of collaboration between colleagues, demands, instrumental manager support and work intrusion on private life.18 22 23 The last finding is in line with results from Anntila et al, in which shorter working hours were associated with positive work-family interaction.29 Overall, RWH seem to improve working-life quality.
Quality of life
Three studies evaluated the effect of work-time reduction on quality of life outside of work.20 23 24 Åkerstedt et al found a significant increase in time for family/friends and social activities in the experimental group, and this increase was significant also over time among the experimental group.24 However, as mentioned above, they did not find any improvement in the self-rated health. It is possible that the extra free time, despite exerting a positive effect on general quality of life, does not necessarily determine an improvement in self-perceived health. These results are consistent with the results of von Thiele Schwarz et al, who did not find any significant differences regarding work-time interaction, neither between the intervention groups and the reference group nor over time among the same groups.20 In addition, Lorentzon et al found that healthy behaviours, such as healthy eating, did not improve in the intervention group.23 Overall, these results suggest that work time reduction per se is not necessarily associated with an improvement in the balance between work and private life. Hence, beside work-time reduction, it is also important to focus on how the extra free time is spent, in order to make the reduction in work-time and workload really effective in exerting positive effects on individual health.
Physical activity
Physical activity was evaluated by three studies.20 23 24 While Åkerstedt et al found no significant improvements regarding PE,24 von Thiele et al and Lorentzon et al observed an increase in physical activity in participants experimenting RWH.20 23 However, the study design by von Thiele Schwarz et al consisted in three groups (physical activity group, RWH group and reference group) and such increases were observed in all of them.20 We do not know whether these changes were a consequence of an increased awareness towards PE brought by the experiment. Moreover, the number of studies evaluating this specific outcome are too few. Although previous research has shown that there seems to be an inverse association between work hours and physical activity,30 for the reasons listed above it cannot be concluded that RWH are associated with increased levels of physical activity. Indeed, we do not know whether employees working for reduced work time would engage their spare time into PE. Hence, more experiments are needed to better determine this subject.
Biological markers
Only et al evaluated the effect of work-time reduction on several biological markers.20 They found in the reference group increasing levels of all of the blood lipids. In the RWH group, total cholesterol and HDL had increased significantly, while only total cholesterol had increased significantly in the PE group. Regarding metabolic measures, glucose showed a significant decrease in the PE group only, while the waist-to-hip ratio increased in the RWH group. These last findings suggest that the work time reduction alone is not sufficient to exert positive metabolic effects, but it should be associated with other healthy habits in the extra free time outside of work, like physical activity. that. On the other hand, in this study, the increase of total cholesterol in the exercise group, without any significant reduction in LDL and waist-to-hip ratio, is unexpected and it could be related to other factors, such as diet, which this study did not analyse. Hence, it is impossible to state that a reduction in work hours has a significant and positive effect on biomarkers and metabolic outcomes, and other studies are therefore necessary to clarify these discrepancies.
Strengths and limitations
To date, this is the first literature review carried out in English to establish the relationship between RWH and health effects. Furthermore, our review evaluates the effect of RWH on both self-reported and measured health outcomes. Nevertheless, it has some limitations that must be acknowledged. First of all, the studies we included in our analysis were published in Scandinavian countries, traditionally known for placing a high value on work-life balance. Hence, the results of this review are not easily generalisable in other contexts, which could be different from a social, cultural and economic point of view. Furthermore, even taking into account excluded records, few studies addressed the issue of work time reduction, suggesting that, despite emerging as a relevant topic in public debate over the last few years, the issue of work-time reduction has not been studied enough so far. However, our selection could have missed some relevant studies due to language limitations. In addition, three out of seven studies were evaluated as of weak quality by the authors. The main reason for this was the impossibility to ensure blinding of both participants and outcome assessors in this kind of studies. Nonetheless all of them had a longitudinal design, over a period of time ranging from 12 up to 36 months. Furthermore, in all studies except two, employment of extrapersonnel allowed to prevent a compensatory increase in workload, which could have significantly undermined the effectiveness of work-time reduction.
In the end, a great limitation of our review is the remarkable heterogeneity of workers in the seven selected studies.
Most of the studies focus on health service workers and this may limit the generalisability of the review to the context of health services that represent a particular work setting with high emotional stress.
Conclusions
Factors affecting health in the workplace are manifold and include organisational, cultural and social aspects. It is not clear whether changes in working hours alone is a robust enough factor that influences ‘stress’ or other health variables in workers.
However, our review shows that the reduction of work hours is associated with an improvement of sleep habits, lower levels of stress and better working life quality. We did not find a positive influence of work time reduction neither on quality of life outside of work, nor on physical activity. Hence, we can conclude that a reduction of work-hours, with preserved salary and without an increase in total workload, may exert a positive effect on specific health outcomes, especially stress and sleep, but it is also essential to investigate how other work variables such as load, type and organisation of work affect the health of the worker. Another important factor that could affect health is how the extra free time is spent. Therefore, further studies are needed to investigate the correlation between different working variables, working time and extra free time with standardised health outcomes in order to evaluate the real impact of working time on workers' health. It is also important to study whether providing prescriptions on how to spend extra free time healthily can improve workers' health. The conflicting results of this review suggest that work time reduction may be truly effective only if it determines a parallel improvement in healthy habits, which can then be main responsible for a real increase of overall health and quality of life.
Supplementary Material
Footnotes
Contributors: The review was conceived by GV, MRG and RS. Data extraction was carried out by GV, AS, DC, SR and EB with support from MRG, FB and RS. Reporting of findings was led by GV and MRG with support from FB and RS. All authors contributed to manuscript preparation and approved the final version. MRG is responsible for the overall content as the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information. Not applicable, this is a review.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.OECD . Average usual Weekly hours worked on the main job. OECD employment and labour market statistics (database), 2021. Available: https://stats.oecd.org/Index.aspx?DataSetCode=AVE_HRS [Accessed 26 Jan 2020].
- 2.OECD . Average annual hours actually worked per worker. OECD employment and labour market statistics (database), 2021. Available: https://stats.oecd.org/Index.aspx?DataSetCode=ANHRS [Accessed 26 Jan 2021].
- 3.Bannai A, Tamakoshi A. The association between long working hours and health: a systematic review of epidemiological evidence. Scand J Work Environ Health 2014;40:5–18. 10.5271/sjweh.3388 [DOI] [PubMed] [Google Scholar]
- 4.Kivimäki M, Jokela M, Nyberg ST, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet 2015;386:1739–46. 10.1016/S0140-6736(15)60295-1 [DOI] [PubMed] [Google Scholar]
- 5.Virtanen M, Jokela M, Madsen IE, et al. Long working hours and depressive symptoms: systematic review and meta-analysis of published studies and unpublished individual participant data. Scand J Work Environ Health 2018;44:239–50. 10.5271/sjweh.3712 [DOI] [PubMed] [Google Scholar]
- 6.Rivera AS, Akanbi M, O'Dwyer LC, et al. Shift work and long work hours and their association with chronic health conditions: a systematic review of systematic reviews with meta-analyses. PLoS One 2020;15:e0231037. 10.1371/journal.pone.0231037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fagan C, Lyonette C, Smith M. "The influence of working time arrangements on work-life integration or 'balance' : a review of the international evidence," ILO Working Papers 994705033402676. International Labour Organization, 2012. [Google Scholar]
- 8.Estevão M, Sa F. The 35-hour workweek in France: Straightjacket or welfare improvement? Econ Policy 2008;23:417–63. 10.1111/j.1468-0327.2008.00204.x [DOI] [Google Scholar]
- 9.Fagnani J, Letablier MT. Work and family life balance: the impact of the 35-hour laws in France. Work Employ Soc 2004;18:551–72. [Google Scholar]
- 10.Bakker AB, Demerouti E. The job Demands‐Resources model: state of the art. J Manag Psychol 2007;22:309–28. 10.1108/02683940710733115 [DOI] [Google Scholar]
- 11.Ferdinand P. VW plan for 4-day Workweek is adopted, 1993. New York Times. Available: https://www.nytimes.com/1993/11/26/business/vw-plan-for-4day-workweek-is-adopted.html
- 12.Paul K. Microsoft Japan tested a four-day work week and productivity jumped by 40%. The Guardian. 2019. https://www.theguardian.com/technology/2019/nov/04/microsoft-japan-four-day-work-week-productivity [Google Scholar]
- 13.Charlotte G-M. A 4-day Workweek? A test run shows a surprising result. New York Times, 2018. https://www.nytimes.com/2018/07/19/world/asia/four-day-workweek-new-zealand.html [Google Scholar]
- 14.Brynja O, Bildt C. Arbetstidsförkortning och hälsa: En litteraturgenomgång av befintlig forskning [Reduced working hours and health: a literature review of existing studies], 2005. Available: http://nile.lub.lu.se/arbarch/arb/2005/arb2005_11.pdf
- 15.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile APP for systematic reviews. Syst Rev 2016;5:210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Effective Public Health Practice Project . Quality assessment tool for quantitative studies. University Toronto, 2010: 1–4. https://merst.ca/wp-content/uploads/2018/02/quality-assessment-tool_2010.pdf [Google Scholar]
- 17.Armijo-Olivo S, Stiles CR, Hagen NA, et al. Assessment of study quality for systematic reviews: a comparison of the Cochrane collaboration risk of bias tool and the effective public health practice project quality assessment tool: methodological research. J Eval Clin Pract 2012;18:12–18. 10.1111/j.1365-2753.2010.01516.x [DOI] [PubMed] [Google Scholar]
- 18.Barck-Holst P, Nilsonne Åsa, Åkerstedt T, et al. Reduced working hours and stress in the Swedish social services: a longitudinal study. Int Soc Work 2017;60:897–913. 10.1177/0020872815580045 [DOI] [Google Scholar]
- 19.Schiller H, Lekander M, Rajaleid K, et al. The impact of reduced worktime on sleep and perceived stress – a group randomized intervention study using diary data. Scand J Work Environ Health 2017;43:109–16. 10.5271/sjweh.3610 [DOI] [PubMed] [Google Scholar]
- 20.von Thiele Schwarz U, Lindfors P, Lundberg U. Health-Related effects of worksite interventions involving physical exercise and reduced workhours. Scand J Work Environ Health 2008;34:179–88. 10.5271/sjweh.1227 [DOI] [PubMed] [Google Scholar]
- 21.von Thiele Schwarz U, Hasson H. Employee self-rated productivity and objective organizational production levels: effects of worksite health interventions involving reduced work hours and physical exercise. J Occup Environ Med 2011;53:838–44. 10.1097/JOM.0b013e31822589c2 [DOI] [PubMed] [Google Scholar]
- 22.Wergeland EL, Veiersted B, Ingre M, et al. A shorter workday as a means of reducing the occurrence of musculoskeletal disorders. Scand J Work Environ Health 2003;29:27–34. 10.5271/sjweh.701 [DOI] [PubMed] [Google Scholar]
- 23.Följeforskning om försök med reducerad arbetstid. Bengt Lorentzon, följeforskare, VD Pacta Guideline. 2017-05-24. URL 1960:729.
- 24.Åkerstedt T, Olsson B, Ingre M, et al. A 6-hour working day--effects on health and well-being. J Hum Ergol 2001;30:197–202. [PubMed] [Google Scholar]
- 25.Dallner M, Elo AL, Gamberale F. Validation of the general Nordic questionnaire (QPSNordic) for psychological and social factors at work. Nord Counc Minist 2000;12. [Google Scholar]
- 26.Virtanen M, Ferrie JE, Gimeno D, et al. Long working hours and sleep disturbances: the Whitehall II prospective cohort study. Sleep 2009;32:737–45. 10.1093/sleep/32.6.737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nakashima M, Morikawa Y, Sakurai M, et al. Association between long working hours and sleep problems in white-collar workers. J Sleep Res 2011;20:110–6. 10.1111/j.1365-2869.2010.00852.x [DOI] [PubMed] [Google Scholar]
- 28.Akerstedt T, Fredlund P, Gillberg M, et al. Work load and work hours in relation to disturbed sleep and fatigue in a large representative sample. J Psychosom Res 2002;53:585–8. 10.1016/S0022-3999(02)00447-6 [DOI] [PubMed] [Google Scholar]
- 29.Anttila T, Nätti J, Väisänen M. The experiments of reduced working hours in Finland. Community Work Fam 2005;8:187–209. 10.1080/13668800500049704 [DOI] [Google Scholar]
- 30.Bauman AE, Reis RS, Sallis JF, et al. Correlates of physical activity: why are some people physically active and others not? Lancet 2012;380:258–71. 10.1016/S0140-6736(12)60735-1 [DOI] [PubMed] [Google Scholar]
- 31.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-051131supp001.pdf (50.8KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information. Not applicable, this is a review.