Highlights
-
•
This case presented with very rare feature of active Pulmonary TB.
-
•
It denotes that Empyema Necessitans can mimick mesothelioma.
-
•
Unusual CT findings of Empyema Necessitans.
-
•
It states importance of induced sputum for TB diagnosis.
-
•
We recommend to test induced sputum for extrapulmonary tuberculosis to halt the spread of TB in the communities.
1. Introduction and importance
Empyema necessitans or Necessitasis (EN), is a relatively rare clinical entity in which the empyema (bus in the pleura space) extends through the parietal pleura into the adjacent soft tissue and under the musculature of the chest wall [1]. EN can be caused by an untreated parapneumonic effusion [2] and sometimes, it presents as a rare manifestation of tuberculous (TB) infection [3], or Actinomyces meyeri [4]. Untreated tuberculous empyema results in empyema necessitans with multisystem involvement and, infrequently, broncho-cutaneous fistulae. Patients typically present with constitutional symptoms such as fevers, night sweats, anorexia, weight loss, and chest wall lumps [5]. Here we present a case of an unusually challenging TB empyema necessitans with active pulmonary TB who presented with a rapidly increasing lump on the anterior chest wall associated with mild fever and scattered multiple pleural-based solid lesions mimicking mesothelioma in the CT scan but, after incision and drainage, an active pulmonary TB with positive sputum for Mycobacterium associated pleural involvement as an Empyema Necessitans was confirmed by the GeneXpert/RR test.
2. Case presentation
An 18-year-old male, previously healthy, came to our outpatient department complaining of a rapidly increasing lump in the right anterior chest wall and a mild fever for two weeks. He denied dyspnea, productive cough, hemoptysis, night sweating, weight loss, and appetite loss. He also denied any history of lung disease, smoking, Qat chewing, alcoholism, and vaping. There was no family history of chronic lung diseases or recent TB history in the family. The patient was afebrile and clinically stable. On palpation, an immobile lump in the right anterior mid-clavicular area with no tenderness or discoloration was noted. On auscultation, normal vesicular breathing and bilateral air entry. Initial investigations revealed an ESR of 61 mm/hr, a CRP of 31 mg/L, and a WBC of 7.52 × 109/L with normal differential cell counts. Serology revealed negative HIV, HBsAg, and HCV. Chest CT revealed pleural focal solid lesions in the right hemithorax, the largest measuring 2.5 cm and indicating malignancy, as well as a 4 cm hypodense lesion that extended to the right pectoral muscle and communicated with the right anterior pleural space, indicating an abscess (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5). A senior thoracic surgery specialist decided to perform an excisional biopsy in our tertiary hospital to rule out malignancy and drain the abscess. After opening the lesion, we found a frank yellowish-white colored, odorless bus collection under the pectoralis major, which extends to the intra-thoracic cavity and communicates with the pleura but is enclosed by a capsule-like layer. We drained the collection and closed the incision. The patient was admitted to the ward and broad-spectrum antibiotics were started. We sent the fluid for microscopy, culture, and sensitivity, and an acid fast bacilli test for tuberculosis. The results showed no growth for bacteria, but the acid-fast bacilli test resulted positive for Mycobacterium TB. Fluid cytology was negative for malignancy. The patient was transferred to the national TB centers where investigation of sputum by PCR/GeneXpert/RR test was done and it confirmed Rifampicin Sensitive mycobacterium Tuberculosis in the sputum. The diagnosis of active pulmonary tuberculosis with atypical presentation of extra-pulmonary complications was the definitive diagnosis of our case, and the first-line anti-TB drug regimen was started. One month later, the patient returned for follow up with no symptoms and the site of the incision healed. This work has been reported in line with the SCARE 2020 criteria [6].
Fig. 1.
Chest T scan without contrast, mediastinal window showing a 4 cm sized hypdoense lesion that extends to the right pectoral muscle communicating with the right anterior pleura (arrow).
Fig. 2.
Chest T scan without contrast, mediastinal window showing pleural based solid lesion in the right hemithorax adjacent to the vertebra (arrow). Mimicking malignancy.
Fig. 3.
Chest T scan without contrast, mediastinal window showing pleural based solid lesion in the right hemithorax at the level of the right diaphragmatic dome. Mimicking malignancy.
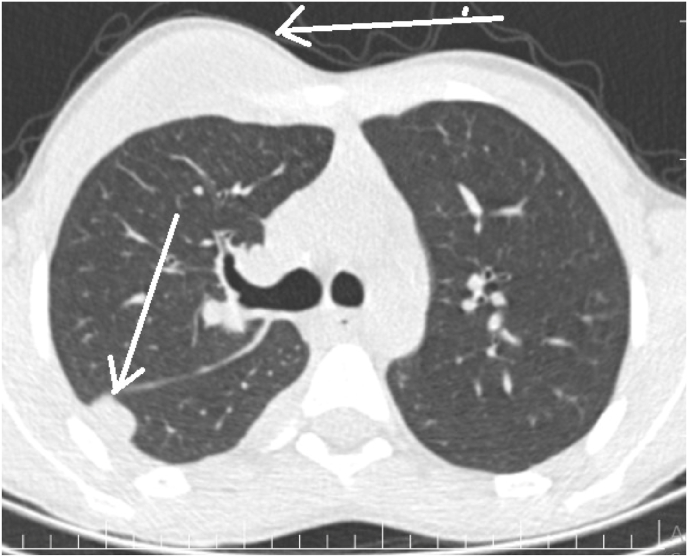
Fig. 4.
Chest T scan without contrast, parenchymal window showing pleural based solid lesion in the right hemithorax at the level of the crina (back faced arrow) Mimicking malignancy and mass in the pertoral area (lateral arrow).
Fig. 5.
Chest T scan without contrast, parenchymal window showing two pleural based solid lesions in the right hemithorax (arrows). Mimicking malignancy.
3. Clinical discussion
Tuberculosis (TB) is one of the top 10 causes of death worldwide and is the leading cause of death from a single infectious agent [7]. An empyema necessitans occurs when an untreated empyema dissects through the parietal pleura and forms abscesses in the subcutaneous tissue of the anterior chest wall [3]. Empyema necessitans can be divided into tubercular and non-tubercular causes. Mycobacterium tuberculosis accounts for approximately 70% of cases of EN. Actinomyces is considered the second most common cause [8]. In tubercular empyema necessitans, patients often present with non-specific symptoms due to their suppressed inflammatory process and immunological response [9]. Our case was an immune-competent young male with no previous history of chronic diseases but he presented with a lump and mild fever. A chronic inflammatory process, such as an abscess, empyema, osteomyelitis, or tuberculosis, was frequently responsible for the breach in the chest wall boundary [10,11]. Our patient presented acutely without the usual symptoms of active pulmonary TB or previous history of TB disease. This case presented with a rapidly growing anterior chest wall mass and mild fever without other symptoms of TB like anorexia, night sweating, weight loss, productive cough, and chest pain, which is different from the common presentation of TB empyema necessitans, including constitutional symptoms of fever, weight loss, productive cough, and chest pain [12]. Radiological findings of most of the cases reported in the literature about empyema necessitate the presence of features of empyema or massive effusions which extrude outside of the pleural space [13], while our case showed scattered multifocal pleural-based solid lesions in different locations of the ipsilateral pleura without communication between these lesions or evidence of pleural effusion, while one of the masses with a central hypo-dense appearance was extending outside of the pleural space through the chest wall under the pectoralis major muscle. The strange feature of our case was that the patient was immune-competent and had active pulmonary TB confirmed by GeneXpert/RR without clinical or radiological presentation of the active pulmonary TB. Empyema Necessitans is very rare in this country, and this is the second case reported in our hospital, and this is the first active pulmonary TB presenting with only Empyema Necessitans in our hospital.
4. Conclusion
Empyema necessitans is a rare complication of tuberculosis empyema which dissects and extends into the outside of the thoracic cavity. Usually, its presentations include fever, weight loss, chest mass, and chest pain, but it can rarely be present only with an anterior chest mass. We report a case of asymptomatic active pulmonary TB presenting as an empyema necessitans, mimicking mesothelioma due to scattered pleural-based lesions. Empyema necessitans can become the only clinical presentation of active pulmonary tuberculosis in immune-competent patients.
Ethical approval
In our hospital there is no need ethical approval for case reports.
These are needed only in the full articles.
Sources of funding
There are no sponsors or any funding sources for this work.
Author contribution
1. Abdirahman Mohamed Hassan Dirie; encountered the patient in OPD, did follow up, he has done literature review, wrote introduction, case presentation and parts of discussion. 2. Hasan Özdemir; senior thoracic surgeon, who did the operation, wrote parts of the discussion. 3. Abdinafic Mohamud Hussein: Made a radiological diagnosis of the patient, description of the images in the manuscript. 4. Ali Mohamed Warsame took part in discussion, conclusion.
Registration of research studies
-
1.
Name of the registry: Not applicable
-
2.
Unique Identifying number or registration ID: Not applicable
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): Not applicable
Guarantors
Abdirahman Mohamed Hassan Dirie.
Hasan Özdemir.
Abdinafic Mohamud Hussein.
Ali Mohamed Warsame.
Consent
Authors have taken written consent from the patient's mother, and it will be available on request.
Provenance and peer review
Not commissioned, externally peer reviewed.
Declaration of competing interest
Authors have no any financial or personal conflict that can influence this work.
References
- 1.Homsi N., Kapila R. Aggregatibacter actinomycetemcomitans causing empyema necessitans and pyomyositis in an immunocompetent patient. Cureus. 2020;12(7) doi: 10.7759/cureus.9454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sahn S.A. Diagnosis and management of parapneumonic effusions and empyema. Clin. Infect. Dis. 2007;45(11):1480–1486. doi: 10.1086/522996. [DOI] [PubMed] [Google Scholar]
- 3.Benaragama H.N., Pushpakumara J., Wanigasuriya K.P. Empyema necessitans due to interruption of antituberculosis treatment. Case Rep Infect Dis. 2019;2019:1–5. doi: 10.1155/2019/4810354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jung H.W., Cho C.R., Ryoo J.Y., et al. Actinomyces meyeri empyema: a case report and review of the literature. Case Rep Infect Dis. 2015;2015(212):1–4. doi: 10.1155/2015/291838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Correa G., Taylor D., Vogel D., Wyncoll D. A case of broncho-cutaneous fistula secondary to tuberculosis successfully managed with awake veno-venous extracorporeal membrane oxygenation. Respir Med Case Reports. 2021;32(December 2020):101351. doi: 10.1016/j.rmcr.2021.101351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrabi C., et al. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization . 2020. World Health Organization GLOBAL TUBERCULOSIS REPORT 2020. [Google Scholar]
- 8.Bandaru S., Manthri S., Sundareshan V., Prakash V. Empyema necessitans in the setting of methicillin-susceptible Staphylococcus aureus causing pneumonia and bacteremia. Case Rep Infect Dis. 2018;2018:1–5. doi: 10.1155/2018/4906547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Babamahmoodi F., Davoodi L., Sheikholeslami R., Ahangarkani F. Tuberculous empyema necessitatis in a 40-year-old immunocompetent male. Case Rep Infect Dis. 2016;2016:1–4. doi: 10.1155/2016/4187108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhat V.S., Poojaramuddanahalli M., Rajagopalan N., Gadabanahalli K. Spontaneous chest wall interstitial emphysema secondary to chronic empyema thoracis. J. Clin. Diagn. Res. 2015;9(6):TD05–TD06. doi: 10.7860/JCDR/2015/12846.6082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hussein A.M., Korkmaz U.T.K., Yapici K., Ali A.A., Kizilay M. Successfully managed case of cardiac tamponade due to tuberculous pericardial effusion: a case study. Iran Hear J. 2021;22(1):109–111. [Google Scholar]
- 12.Ellebrecht D.B., Pross M.M.F., Schierholz S., Palade E. vol. 1. 2019. pp. 57–61. (Actinomyces Meyeri Empyema Necessitatis — A Case Report and Review of the Literature). 212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gomes M.M., Alves M., Correia J.B., Santos L. Empyema necessitans: very late complication of pulmonary tuberculosis. BMJ Case Rep. Published online. 2013:1–4. doi: 10.1136/bcr-2013-202072. [DOI] [PMC free article] [PubMed] [Google Scholar]