Abstract
Background
Physical exercise is an effective strategy for preserving functional capacity and improving the symptoms of frailty in older adults. In addition to functional gains, exercise is considered to be a cornerstone for enhancing cognitive function in frail older adults with cognitive impairment and dementia. We assessed the effects of the Vivifrail exercise intervention for functional capacity, cognition, and well‐being status in community‐dwelling older adults.
Methods
In a multicentre randomized controlled trial conducted in three tertiary hospitals in Spain, a total of 188 older patients with mild cognitive impairment or mild dementia (aged >75 years) were randomly assigned to an exercise intervention (n = 88) or a usual‐care, control (n = 100) group. The intervention was based on the Vivifrail tailored multicomponent exercise programme, which included resistance, balance, flexibility (3 days/week), and gait‐retraining exercises (5 days/week) and was performed for three consecutive months (http://vivifrail.com). The usual‐care group received habitual outpatient care. The main endpoint was change in functional capacity from baseline to 1 and 3 months, assessed with the Short Physical Performance Battery (SPPB). Secondary endpoints were changes in cognitive function and handgrip strength after 1 and 3 months, and well‐being status, falls, hospital admission rate, visits to the emergency department, and mortality after 3 months.
Results
The Vivifrail exercise programme provided significant benefits in functional capacity over usual‐care. The mean adherence to the exercise sessions was 79% in the first month and 68% in the following 2 months. The intervention group showed a mean increase (over the control group) of 0.86 points on the SPPB scale (95% confidence interval [CI] 0.32, 1.41 points; P < 0.01) after 1 month of intervention and 1.40 points (95% CI 0.82, 1.98 points; P < 0.001) after 3 months. Participants in the usual‐care group showed no significant benefit in functional capacity (mean change of −0.17 points [95% CI −0.54, 0.19 points] after 1 month and −0.33 points [95% CI −0.70, 0.04 points] after 3 months), whereas the exercise intervention reversed this trend (0.69 points [95% CI 0.29, 1.09 points] after 1 month and 1.07 points [95% CI 0.63, 1.51 points] after 3 months). Exercise group also obtained significant benefits in cognitive function, muscle function, and depression after 3 months over control group (P < 0.05). No between‐group differences were obtained in other secondary endpoints (P > 0.05).
Conclusions
The Vivifrail exercise training programme is an effective and safe therapy for improving functional capacity in community‐dwelling frail/prefrail older patients with mild cognitive impairment or mild dementia and also seems to have beneficial effect on cognition, muscle function, and mood status.
Keywords: Multicomponent exercise programme, Functional capacity, Falls, Frailty
Introduction
The global population is progressively aging, and lifespan is predicted to continue increasing over the next decades. 1 While substantial gains have been made in the application of precision medicine to prevent and treat aging‐related health complications, frailty syndrome remains prevalent among the oldest old, reducing their ability to perform activities of daily living (ADLs) through loss of muscle function (i.e. muscle mass and muscle strength/power), ultimately leading to functional deterioration and disability. 2 Many age‐related processes leading to frailty in older adults are also likely responsible for brain aging and related cognitive impairment. 3 Indeed, cognitive decline is closely associated with frailty syndrome as both diseases share several pathophysiological mechanisms and short‐term and long‐term consequences such as increased incidence of falls, hospitalization, institutionalization, and death. 2 , 4 Accordingly, healthcare professionals should prioritize strategies to prevent or reverse functional and cognitive deterioration in older populations, which may reduce visits to primary care and emergency departments and lessen hospital resources and, ultimately, healthcare costs.
Physical inactivity seems to play a key role in the loss of muscle function and functional capacity, which in turn appears to be a crucial factor related to frailty. 5 Against this background, the potential benefits of different exercise interventions in frail individuals have been widely demonstrated in the literature, showing marked improvements in frailty hallmarks––for instance, gait ability, muscle strength, balance, and falls. 6 , 7 It is recognized that physical exercise improves metabolic health by suppressing muscle atrophy, blunting inflammatory responses, and protecting against loss of bone density, and it may also contribute to preserve insulin sensitivity, mitochondrial activity, and physical function. 8 There is strong evidence to support that the inclusion of tailored exercise programmes is probably the best method to improve the hallmarks of frailty, including functional capacity, muscle function, and health status. 9 , 10 In particular, multicomponent exercise programmes consisting of resistance (power), balance, and gait‐retraining exercises are the most effective interventions for preventing most, if not all, of the complications of frailty syndrome (i.e. poor balance, reduced muscle strength, poor gait ability, and increased incidence of falls), and their prescription is recommendable for frail older adults, as well as for persons with prefrailty. 6 , 10 , 11 Additionally, physical exercise and specifically multicomponent exercise training may be a cornerstone for improving physical and cognitive function in frail individuals with mild cognitive impairment (MCI) and dementia. 12 In line with this concept, we recently developed an innovative multicomponent exercise training programme termed Vivifrail (http://vivifrail.com/resources/), which is based on promoting exercise in older population through individualized programmes designed to prescribe tailored physical exercise. 13 In a recent study, 11 the Vivifrail multicomponent tailored exercise programme was very effective in the short‐term (4 weeks) and prevented severe functional decline and strength loss in institutionalized older (i.e. physical frailty reversion and recovery of autonomy). Multicomponent exercise face‐to‐face interventions would seem advisable as an essential activity to protect older adults from severe functional decline. 14 The community‐based approach is the best way forward, and physical exercise is one of the main interventions with systemic effect proven to improve physical impairment related to frailty (low body mass, strength, mobility, physical activity level, and energy). 15 The present multicentre study aimed to examine the effects of the Vivifrail multicomponent exercise intervention performed by frail/prefrail community‐dwelling older adults with cognitive impairment and mild dementia for functional, cognition, and well‐being status.
Materials and methods
Design
The study was a multicentre, randomized clinical trial (RCT) (NCT03657940) performed according to the Spirit 2013 and the CONSORT statement for transparent reporting (Supporting Information, Data S1). 16 It is an open label, blinded adjudication study. The study protocol has been published. 17 The multicentre RCT was conducted from 1 September 2017 to 31 May 2020, in the outpatient geriatrics clinics of three tertiary hospitals in Spain (Geriatric Department of Hospital Universitario de Navarra, the Matia Fundazioa in San Sebastian and the Hospital of Getafe). Regarding the sample size calculations, assuming an alpha error of 5%, a correlation between pre‐intervention and post‐intervention values of the Short Physical Performance Battery (SPPB) of ρ = 0.5 and a standard deviation for the SPPB of σ = 2.5, the required sample size to have a power of 90% to detect a minimum difference of 1 point between groups in the post–pre SPPB score was 101 patients per group. Taking into account an expected loss of patients along the follow‐up of 15%, the final sample size required was 120 per group for this multicentre study. 17
The study followed the principles of Declaration of Helsinki and was approved by the Complejo Hospitalario de Navarra Clinical Research Ethics Committee. All patients or their legal representatives provided written informed consent. There was no financial compensation.
Patients who met the inclusion criteria were randomly assigned to the intervention or control (usual‐care) group. Prior to randomization, the attending geriatricians reviewed the absolute and relative contraindications to participate in the intervention and provided general information about the study. Usual care was offered to the patients by the geriatricians and consisted of normal outpatient care, including physical rehabilitation when needed.
Participants and randomization
Potentially eligible outpatient participants were initially evaluated by the geriatricians. We focused on a particularly vulnerable population segment but at the same time with sufficient functional and cognitive reserve to be able to complete the exercise programme. A trained research assistant (A. C.‐H., I. A.‐R., I. M.‐E., F. R.‐E., and R. P.‐T.) conducted the screening interview to evaluate the following inclusion criteria: age >75 years, Barthel Index score ≥60 (scale, 0 [severe functional dependence] to 100 [functional independence]), being able to communicate and ambulate (with/without assistance), MCI or mild dementia according to Diagnostic and Statistical Manual of Mental Disorders (DSM) V criteria, Global Deterioration Scale (GDS)‐4 (Reisberg classification), pre‐frail and frail status according to the Fried criteria, 18 and having someone to help supervise the exercises. Exclusion criteria were any factor that affected physical exercise performance or testing procedures, including terminal illness, uncontrolled arrhythmias, recent myocardial infarction, unstable angina pectoris, uncontrolled arterial hypertension, unstable cardiovascular disease or other unstable medical condition, recent pulmonary thromboembolism, upper or lower extremity fracture in the past 3 months, and institutionalized older adults or pending entry into institution.
After the baseline assessment was performed, participants were randomly assigned to the intervention and control (i.e. usual‐care) groups following a simple randomization procedure, in a 1:1 ratio without restrictions. The simple randomization sequence was generated by a statistician not involve in the RCT using an online system (www.randomizer.org) for the three hospitals. The assessment staff were blinded to the study design and group allocation in the course over the 3 months, and participants (or their families) were explicitly informed and reminded not to discuss their randomized allocation with the assessment staff. Drop‐out was considered only when the baseline assessment was completed.
The costs related to the intervention were fundamentally those generated by hiring one physiotherapist ad hoc for the project and the collaboration of other research assistants who shared the work for 5 days a week for the duration of the study. An initial investment of €8840 (US $10 008) was made to buy variable resistance equipment (i.e. €7840 [US $9408] for two leg‐press machines) for measuring muscle strength and approximately €1000 (US $1200) for elastic resistance bands, ankle weights, and handgrip balls.
Intervention
Participants in the usual‐care group were instructed to continue with their normal ADLs and received habitual outpatient clinical care, including medical treatments and physical rehabilitation when needed. In addition to habitual outpatient care, the intervention group received the recently developed Vivifrail multicomponent exercise programme (http://vivifrail.com/resources/). 19 The Vivifrail programme is a home‐based exercise programme focused on individualized multicomponent exercise prescription according to the functional capacity of the older adults and consisted of resistance/power, balance, flexibility and cardiovascular endurance exercises (i.e. walking). Adherence to the programme was documented in a daily register, and two phone calls were performed during the intervention period to guarantee patient adherence and to address doubts and questions related to the intervention. At the end of the baseline visit, patients were familiarized with their specific exercise routine before the start of the intervention and their family members or caregivers were instructed in monitoring the exercise intervention for 30 min.
After the baseline assessment, patients in the intervention group were enrolled into one of the following individualized Vivifrail training programmes, according to their physical functional status: Disability (0–3 points in the SPPB score), Frailty (4–6 points), Prefrailty (7–9 points), and Robust (10–12 points). A copy of their specific exercise protocol was delivered for each patient. The initial load for resistance exercises was established according to the Vivifrail exercise prescription guidelines (www.vivifrail.com/resources/) through a progressive loading protocol, adjusting the load until the patient was able to complete ~30 repetitions with some effort. Initial load was set at 0.5 kg (dumbbells) and gradually increased in 0.5 kg increments for upper‐body exercise; lower‐body leg extensions started with free weight repetitions and gradually increased in 0.5‐kg increments using ankle weights to gradually increase the intensity of lower‐body leg exercises based on the functional reserve of the older patients. The exercise intervention comprised a 5‐day‐a‐week routine of multicomponent exercises (i.e. resistance, balance, and flexibility exercises 3 days per week and walking 5 days per week) during 12 consecutive weeks (for more details, see http://vivifrail.com/resources/). After the first month of exercise prescription and at the end of the 1 month follow‐up visit, a new exercise training programme was given to patients and caregivers according to patients' functional status at that time.
Endpoints
The primary endpoint was the change in functional capacity from baseline (beginning of the intervention) to 12 weeks after intervention, as assessed with the SPPB, which combines balance, gait velocity, and leg strength as a single score on a 0 (worst) to 12 (best scale). 20 The meaningful clinical change is considered 1 point for the SPPB. 21
Secondary endpoints included changes in cognitive function assessed by the Spanish validated version of the Minimental Cognitive State Examination 22 (MEC‐Lobo; 0 [worst] to 35 [best] score) for older adults with dementia and the Montreal Cognitive Assessment 23 (MOCA; 0 [worst] to 30 [best] score) for those with MCI. Changes in functional status of the patients during the intervention were also measured by the Barthel Index of ADLs, 24 which ranges from 0 (severe functional dependence) to 100 (functional independence). Also assessed were changes in mood status (15‐item Yesavage Geriatric Depression Scale Spanish version [GDS]; scale of 0 [best] to 15 [worst]), 25 visual analog scale of the EuroQol‐5 Dimension (EQ‐5D) 26 questionnaire for quality of life (QoL) assessment (Spanish version of the EQ‐5D; scale of 0 [worst health state imaginable] to 100 [best health state imaginable]), and handgrip strength (dominant hand). 27 Other secondary endpoints included falls, hospital admissions, visits to the emergency department, institutionalization, and mortality after 3 months of the intervention. Number of falls were based on self‐report. Additionally, patients and caregivers were asked about hospital admissions, visits to the emergency department and institutionalization in the last 3 months, and these endpoints were checked from medical history. Mortality data were also collected from hospital records.
Statistical analysis
We used the intention‐to‐treat approach for data analysis. Between‐group comparisons of continuous variables were performed using linear mixed models for continuous variables and with ordinal mixed models for ordinal variables (i.e. patients' distribution based on the Vivifrail classification). The models included group, time, and group by time interaction as fixed effects and participants as random effects and were adjusted for age, sex, endpoint baseline value, and SPPB baseline value, all of them included as fixed effects. Cognitive endpoints (i.e. MOCA and MEC‐Lobo) models were also adjusted for years of education, baseline CIRS, and baseline Yesavage GDS values. Data are expressed as change from baseline (when intervention started) to 1 and 3 months for each group, determined by the time coefficients (95% confidence interval [CI]) of the model. The primary conclusions about the effectiveness of physical exercise were focused on between‐group comparisons of change in functional capacity assessed with the SPPB and determined by the time by group interaction coefficients of the model. The same strategy was used for examining the effectiveness of the intervention on secondary endpoints including cognition, muscle function, and well‐being status.
Comparisons of secondary endpoints indicative of adverse events were analysed using the Mann–Whitney test for non‐normally distributed quantitative data, mid‐P value exact test for rates, and χ 2 or Fisher's test for categorical data. Normality of data was checked graphically and through the Kolmogorov–Smirnov test. The residuals were also checked graphically, and no noticeable deviation from normality was observed. All comparisons were two‐sided, and the significance level was established at P < 0.05. All statistical analyses were made with SPSS, version 20 (IBM Corp) and R, version 3.2.2 (R Foundation) software.
Results
The study flow diagram is shown in Figure 1. Of the 188 patients included in the analyses, 132 were women (70.2%); the mean age was 84.1 (4.8) years (range 73–95 years). Demographic and clinical characteristics of the participants are shown in Table 1. The mean adherence to the exercise sessions in the intervention group was 79% in the first 4 weeks and 68% in the following 8 weeks, and 5% of the participants in the control group received physical rehabilitation. No adverse effects associated with the prescribed exercises were recorded, and no patient had to stop the intervention because of it.
Figure 1.
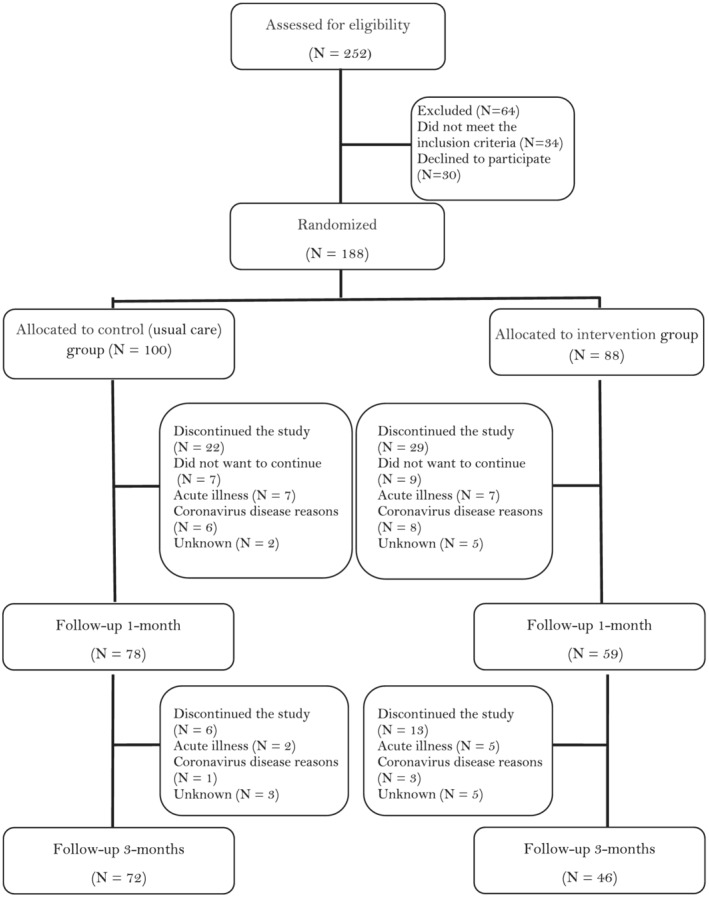
Study flow diagram.
Table 1.
Baseline characteristics of the participants
| Variable | Control group (N = 100) | Intervention group (N = 88) |
|---|---|---|
| Demographic data | ||
| Age, years | 84.0 (4.8) | 84.2 (4.8) |
| Women, N (%) | 69 (69.0%) | 63 (71.6%) |
| Body mass index, kg/m 2 | 27.0 (4.3) | 27.1 (3.6) |
| Education, N (%) | ||
| <12 years | 80 (80.0%) | 67 (76.1%) |
| ≥12 years | 20 (20.0%) | 21 (23.9%) |
| Living status, N (%) | ||
| Alone | 26 (26.0) | 19 (21.6) |
| Caregivers | 12 (12.0) | 9 (10.2) |
| Family members | 60 (60.0) | 58 (65.9) |
| Others | 2 (2.0) | 2 (2.3) |
| Clinical data | ||
| MCI, N (%) | 63 (63.0) | 49 (55.7) |
| Mild dementia, N (%) | 37 (37.0) | 38 (43.2) |
| Fried criteria, N (%) | ||
| Prefrail (1–2 points) | 64 (64.0) | 57 (64.8) |
| Frail (3–5 points) | 36 (36.0) | 31 (35.2) |
| CIRS score, median (IQR) | 5.0 (5.0) | 7.0 (6.0) |
| MNA score, median (IQR) | 13.0 (3.0) | 13.0 (3.0) |
| 1RM leg press, kg | 49.4 (27.2) | 48.0 (24.1) |
| 5 m GVT, s | 7.8 (2.9) | 8.7 (5.5) |
| Primary endpoint measures | ||
| SPPB scale, score | 7.7 (2.5) | 6.8 (2.7) |
| Secondary endpoint measures | ||
| MOCA, score | 15.4 (5.2) | 15.8 (5.2) |
| MEC Lobo, score | 27.1 (4.5) | 26.4 (5.3) |
| Barthel Index, score | 91.7 (10.2) | 91.1 (9.3) |
| Handgrip, kg | 19.2 (7.7) | 19.6 (6.7) |
| Yesavage GDS, score | 3.4 (2.9) | 3.9 (2.9) |
| QoL (EQ‐VAS), score | 71.4 (18.2) | 70.6 (20.6) |
Data are mean (SD) unless otherwise stated. Significant differences were found between groups for SPPB score and CIRS score (P < 0.05).
CIRS, Cumulative Illness Rating Scale; EQ‐VAS, Visual analog scale of the EuroQol questionnaire; GVT, Gait Velocity Test; IQR, interquartile range; MNA, Mini‐Nutritional Assessment; MCI, Mild Cognitive Impairment; MEC, Minimental Cognitive Exam; MOCA, Montreal Cognitive Assessment; QoL, Quality of Life; SPPB, Short Physical Performance Battery; Yesavage GDS, Yesavage Geriatric Depression Scale; 1RM, one‐repetition maximum.
With regard to the primary endpoint, the physical exercise programme provided a significant benefit over clinical usual‐care. The exercise group showed a mean increase (over usual care) of 0.86 points in the SPPB score (95% CI 0.32, 1.41; P < 0.01) after 1 month and 1.40 points (95% CI 0.82, 1.98; P < 0.001) after 3 months of exercise training (Figure 2, Table 2). The percentage distribution of patients in different Vivifrail categories (Disability, Frailty, Prefrailty, and Robust) also significantly differed between the two groups from baseline to 3 months of the intervention (P < 0.001) (Figure 3), indicating a beneficial effect––for instance, the percentage of patients in the disability category progressively decreased in the intervention group (14.8% at baseline, 6.8% at 1 month, and 6.5% at 3 months), whereas no such trend was found in the control group (4.0% at baseline, 5.2% at 1 month and 11.4% at 3 months; odds ratio intervention vs. control 0.14 [0.05, 0.45]).
Figure 2.
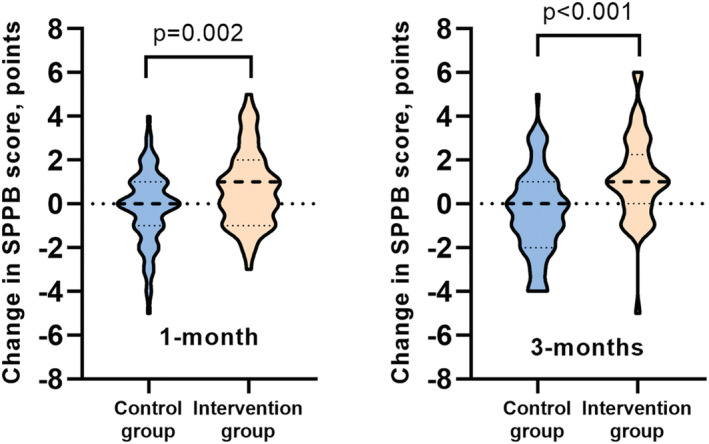
Within‐group SPPB score change distribution for both groups.
Table 2.
Results of study endpoints by group at 1 and 3 months post‐intervention
| Endpoints | Time | Control group | Exercise group | Between‐group difference (95% CI) | p‐value between groups |
|---|---|---|---|---|---|
| Primary Endpoint: Changes in functional capacity | |||||
| SPPB scale (points) | 1 month | −0.17 (−0.54, 0.19) | 0.69 (0.29, 1.09) | 0.86 (0.32, 1.41) | 0.002 |
| 3 months | −0.33 (−0.70, 0.04) | 1.07 (0.63, 1.51) | 1.40 (0.82, 1.98) | <0.001 | |
| Secondary Endpoints: Changes in functional, cognition, muscle function, and mood status | |||||
| Barthel Index (points) | 1 month | 0.18 (−1.80, 2.14) | 1.69 (−0.51, 3.89) | 1.51 (−1.44, 4.46) | 0.319 |
| 3 months | −0.10 (−2.11, 1.99) | 0.99 (−1.40, 3.39) | 1.09 (−2.04, 4.21) | 0.499 | |
| MOCA (points) | 1 month | 0.50 (−0.42, 1.42) | 2.25 (1.08, 3.41) | 1.75 (0.27, 3.24) | 0.340 |
| 3 months | −0.13 (−1.08, 0.82) | 2.05 (0.80, 3.28) | 2.17 (0.61, 3.72) | 0.014 | |
| MEC‐Lobo (points) | 1 month | 0.64 (0.03, 1.26) | 0.75 (0.07, 1.43) | 0.10 (−0.81, 1.02) | 0.826 |
| 3 months | −0.50 (−1.13, 0.13) | 0.63 (−0.09, 1.36) | 1.13 (0.18, 2.10) | 0.023 | |
| Handgrip strength (kg) | 1 month | 0.08 (−0.54, 0.71) | 0.70 (0.00, 1.40) | 0.62 (−0.32, 1.56) | 0.200 |
| 3 months | −0.70 (−1.35, −0.05) | 0.35 (−0.42, 1.12) | 1.05 (0.05, 2.06) | 0.042 | |
| Yesavage GDS (points) | 3 months | 0.61 (0.15, 1.07) | −0.51 (−1.04, 0.02) | −1.12 (−1.82, −0.42) | 0.002 |
| QoL (EQ‐VAS) (score) | 3 months | −0.71 (−4.49, 3.08) | −0.49 (−4.93, 3.96) | 0.22 (−5.62, 6.06) | 0.942 |
Data are expressed as mean (95% CI). All data were derived from linear mixed‐effects model. For each group, data are expressed as change from baseline to 1 month and 3 months post‐intervention, determined by the time coefficients (95% CI) of the model. Between‐group differences were determined with time x group interaction. All the endpoints were adjusted by age, sex, endpoint baseline value, and SPPB baseline value. Additionally, cognitive endpoints (MOCA and MEC‐Lobo) were also adjusted by Yesavage GDS, CIRS baseline value, and years of education. A total of 137 patients (78.0% of patients in the control group and 67.0% in the intervention group) at 1 month post‐intervention and 118 patients (72.0% of patients in the control group and 52.3% in the intervention group) at 3 months post‐intervention reached their functional and muscle function endpoints. Cognitive data correspond to 137 patients (78.0% of patients in the control group and 67.0% in the intervention group) at 1 month post‐intervention and 118 patients (71.0% of patients in the control group and 53.4% in the intervention group) at 3 months post‐intervention.
CIRS, Cumulative Illness Rating Scale; EQ‐VAS, Visual Analog Scale of the EuroQol Questionnaire; MEC, Minimental Cognitive Exam; MOCA, MOCA, Montreal Cognitive Assessment; QoL, Quality of Life; SPPB, Short Physical Performance Battery; Yesavage GDS, Yesavage Geriatric Depression Scale.
Figure 3.
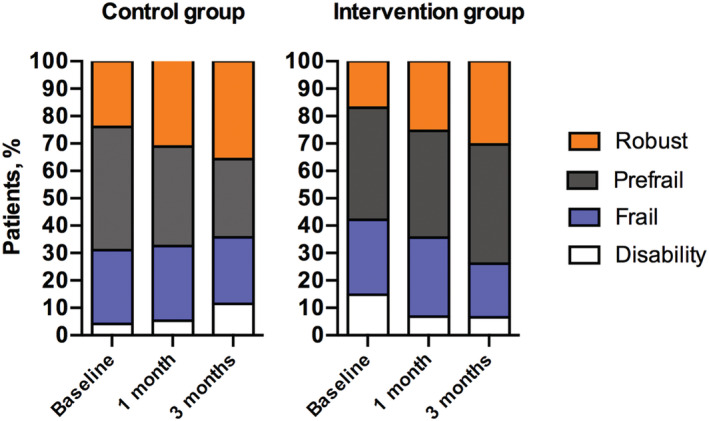
Changes in the functional categories at baseline, 1 month, and 3 months after intervention according to the Vivifrail classification: Disability (SPPB score 0–3 points), Frailty (4–6 points), Prefrailty (7–9 points), and Robust (10–12 points). P‐value after 1 month = 0.062. P‐value after 3 months ≤ 0.001.
Regarding the secondary endpoints, the exercise intervention also seemed to provide benefits on cognitive function. Indeed, the intervention group showed improvements in the MOCA test after 3 months of exercise intervention (2.05 points; 95% CI 0.80, 3.28), whereas no such trend was found in the control group (after 3 months −0.13 points; 95% CI −1.08, 0.82) (P < 0.05) (Table 2). Similar between‐group differences were found in the MEC‐Lobo test for those patients with dementia (Table 2). We also found significant between‐group differences in handgrip strength and in mood status (depression) (both P < 0.05) after 3 months of intervention (Table 2). However, no significant between‐group differences were observed for the remainder secondary endpoints, including health‐related quality of life (visual analog scale of the EQ‐5D), Barthel Index of functional ability in ADLs (Table 2), falls, hospital admissions, visits to the emergency department, and mortality (all P > 0.10) (Table 3).
Table 3.
Results of secondary endpoints indicative of adverse events for each group
| Endpoints (3 months) | Control group | Exercise group | Rate ratio (95% CI) | P‐value between groups |
|---|---|---|---|---|
| Falls rate (100 person‐month) | 15.4 (10.6, 21.6) | 20.8 (14.2, 29.3) | 1.25 (0.83, 2.21) | 0.225 |
| Hospital readmission rate (100 person‐month) | 3.28 (1.41, 6.46) | 1.72 (0.35, 5.04) | 0.53 (0.11, 1.92) | 0.358 |
| Visits to emergency department rate (100 person‐month) | 9.76 (6.25, 14.5) | 6.32 (3.15, 11.3) | 0.65 (0.31, 1.31) | 0.234 |
| Mortality, % | 0 | 0 | ||
| Transfer, % | ||||
| Home | 100 | 100 | ||
| Institutionalization | 0 | 0 | ||
| Other | 0 | 0 | ||
Data are expressed as rate (95% CI) unless otherwise indicated.
Discussion
The present multicentre RCT adds to the growing body of evidence for the beneficial effects of physical exercise in community dwelling older adults. Our RCT shows that the Vivifrail individualized, tailored multicomponent intervention of moderate‐intensity muscle strengthening, balance, flexibility, and endurance exercises is safe and provides significant benefit over usual clinical care in frail older patients with MCI and dementia, as well as contributes to prevent or reverse the functional decline that often occurs in this population. In addition to functional gains, our findings indicate that the Vivifrail exercise programme promotes mood, cognitive, and muscle function enhancements after 3 months of intervention compared with usual clinical care.
The protective effect of physical exercise in community dwelling older adults has been well confirmed in the literature, supporting exercise as a cornerstone for preserving functional status and muscle function in this population. 10 , 15 , 28 Contrastingly, physical inactivity is recognized to promote frailty, and physical exercise is known to maintain or improve the function of many of the physiological systems that can be altered in frailty, including muscle and heart function, endocrine function (e.g. glucose metabolism), and inflammation, and delay the onset of multiple chronic diseases. 29 Previous trials have highlighted the potential benefits of a multicomponent exercise programme (resistance, endurance, flexibility, and balance exercises) on the functional capacity in older populations and for reducing the likelihood of developing disability after long‐time exercise interventions (i.e. 6 months or over). 6 , 30 , 31 One of the main findings of our study is that 1 month of the intervention was sufficient for improving functional capacity in the oldest old. In addition to functional and muscle function (i.e. handgrip strength) gains, our results show that the Vivifrail exercise programme has a beneficial effect on cognition in older frail/prefrail patients with MCI and mild dementia, assessed by MOCA and MEC‐Lobo, respectively. The role of physical exercise on cognitive function has been widely investigated in older adults, 32 , 33 and specifically, multicomponent exercise training seems to provide the best results on cognition in older patients with MCI and dementia. 6 , 12 Strikingly, cognitive function enhancements might mediate physical function improvements in acutely hospitalized frail elders. 34 Thus, physical activity shows promise as modifiable risk factor to reduce the risk of dementia and related neurodegenerative diseases. 35 Mechanistically, the neural and vascular adaptations induced by exercise in older adults are hypothesized to promote cognitive enhancements through stimulation of neurogenesis, angiogenesis, and synaptic plasticity and by reducing pro‐inflammatory processes and cellular damage brought about by oxidative stress. 36 Moreover, the combination of different training modalities, with special emphasis on resistance training, appears to be the best strategy for preserving or improving cognitive function, but further research is warranted to better understand the underlying physiological mechanisms induced by exercise in community dwelling frail older adults with MCI and dementia. Considering the mood status, patients in the exercise group also had better outcomes regarding depression than peers in the control group. The exercise programme was, however, unable to influence the occurrence of falls during the intervention period. Although there is consistent evidence for exercise as an effective therapy for falls prevention in community dwelling older adults, 37 our findings reveal no difference in incidence between groups. These findings should be interpreted with caution due to the short duration of the intervention period (i.e. 3 months).
The present study is in line with the previously published World Health Organization (WHO) Clinical Consortium of Healthy Aging, which stresses the importance of maintaining intrinsic capacity domains (i.e. locomotion, vitality, cognition, psychological, and sensory) and specifically functional status to preserve autonomy and independence in everyday activities that enables wellbeing. 38 Our results suggest that the Vivifrail multicomponent exercise programme may help to mitigate the trajectory of frailty and disability in community dwelling older adults with MCI and/or mild dementia and seems to also provide benefits in mood, cognitive, and muscle function, which are key components of intrinsic capacity. Our data support the notion that, in accordance with the WHO framework, tailored physical exercise should be prescribed to older adults and should be considered a frontline treatment for preventing functional decline, cognitive impairment, and muscle function deterioration that commonly occurs during the aging process. 14 , 39
Our study has several strengths including its multicentre randomized design. Also, we focused on a particularly vulnerable segment of the older adult population, which included patients with multiple co‐morbidities and geriatric syndromes as MCI/mild dementia (who are frequently excluded from exercise studies). Our findings suggest that a home‐based, individualized multicomponent exercise programme (Vivifrail; www.vivifrail.com) has beneficial effects on many health‐related outcomes, overcoming barriers often encountered with traditional exercise interventions such as material resources and transport limitations. Finally, to minimize the potential bias, the assessment researchers were unaware of the study design and group allocation.
Our study has several limitations, including recruitment challenges to achieve the sample size proposed in the study protocol. 17 The ‘lockdown’ for coronavirus disease 2019 had a negative impact on the recruitment process and made it difficult to reach the sample size initially calculated. Although a rigorous randomization procedure was carried out, significant between‐group differences were obtained at baseline for functional capacity (SPPB scale) and co‐morbidities (CIRS score). Also, there was missing data at 1 and 3 months post‐intervention due to the characteristics of the study population (octogenarians and nonagenarians with multiple geriatric syndromes) and the coronavirus lockdown during March–June 2020. Additionally, more patients discontinued the study in the intervention group compared with the control group, which could have influenced in the results obtained. The specific features of the study population (i.e. frail or prefrail older patients according to the Fried criteria 18 with MCI or mild dementia) limit the generalizability of our results. Thus, care should be taken when extrapolating our findings to other cohorts. Lastly, the adherence to the exercise training programme progressively dropped during the intervention period (79% of the total sessions were completed after 1 month of intervention and 68% at 3 months). Our exercise adherence rate was, however, higher than in other studies that developed similar home‐based exercise interventions. 40
Our findings highlight several future directions for research. The effectiveness and safety of the Vivifrail exercise programme may be examined in future RCTs with longer intervention periods (> 3 months). In addition to physical exercise, further research is needed to establish consistent evidence about the effect of multidomain interventions including cognitive training on functional capacity and cognition in community dwelling older adults with cognitive impairment.
Conclusions
The Vivifrail multicomponent exercise training programme appears to be an effective and safe intervention for improving functional capacity in community dwelling frail/prefrail older patients with MCI or mild dementia. In fact, a 1 month of exercise intervention is sufficient to enhance physical function in this population. In addition to functional gains, the individualized multicomponent exercise programme also seems to have a beneficial effect on cognition, muscle function, and mood status after 3 months of exercise intervention.
Conflict of interest
The authors declare no conflict of interest.
Supporting information
Data S1. Supporting Information
Acknowledgements
This study has been funded by a Gobierno de Navarra project grant and fondos FEDER (Resolución 426/2016, del 30 de septiembre 28/16). Mikel Izquierdo is funded by a research grant PI17/01814 of the Ministerio de Economía, Industria y Competitividad (ISCIII, FEDER). We also want to thank Fundacion Miguel Servet (Navarrabiomed) for all its support during the implementation of the trial. Finally, thanks to all our patients and their families for their confidence in the research team. The authors certify that they comply with the ethical guidelines for publishing in the Journal of Cachexia, Sarcopenia and Muscle: update 2021. 41
Casas‐Herrero Á., Sáez de Asteasu M. L., Antón‐Rodrigo I., Sánchez‐Sánchez J. L., Montero‐Odasso M., Marín‐Epelde I., Ramón‐Espinoza F., Zambom‐Ferraresi F., Petidier‐Torregrosa R., Elexpuru‐Estomba J., Álvarez‐Bustos A., Galbete A., Martínez‐Velilla N., and Izquierdo M. (2022) Effects of Vivifrail multicomponent intervention on functional capacity: a multicentre, randomized controlled trial, Journal of Cachexia, Sarcopenia and Muscle, 13, 884–893, 10.1002/jcsm.12925
Trial Registration: ClinicalTrials.gov identifier: NCT03657940
References
- 1. Beard JR, Bloom DE. Towards a comprehensive public health response to population ageing. Lancet Lond Engl 2015;385:658–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet Lond Engl 2019;394:1365–1375. [DOI] [PubMed] [Google Scholar]
- 3. Ward DD, Wallace LMK, Rockwood K. Frailty and risk of dementia in mild cognitive impairment subtypes. Ann Neurol. Published online March 11 2021;89:1221–1225. [DOI] [PubMed] [Google Scholar]
- 4. Robertson DA, Savva GM, Kenny RA. Frailty and cognitive impairment‐‐a review of the evidence and causal mechanisms. Ageing Res Rev 2013;12:840–851. [DOI] [PubMed] [Google Scholar]
- 5. Rodriguez‐Mañas L, Fried LP. Frailty in the clinical scenario. Lancet Lond Engl 2015;385:e7–e9. [DOI] [PubMed] [Google Scholar]
- 6. Cadore EL, Moneo ABB, Mensat MM, Muñoz AR, Casas‐Herrero A, Rodriguez‐Mañas L, et al. Positive effects of resistance training in frail elderly patients with dementia after long‐term physical restraint. Age (Dordr) 2014;36:801–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Freiberger E, Häberle L, Spirduso WW, Zijlstra GAR. Long‐term effects of three multicomponent exercise interventions on physical performance and fall‐related psychological outcomes in community‐dwelling older adults: a randomized controlled trial. J Am Geriatr Soc 2012;60:437–446. [DOI] [PubMed] [Google Scholar]
- 8. Valenzuela PL, Castillo‐García A, Morales JS, Izquierdo M, Serra‐Rexach JA, Santos‐Lozano A, et al. Physical exercise in the oldest old. Compr Physiol 2019;9:1281–1304. [DOI] [PubMed] [Google Scholar]
- 9. Izquierdo M, Morley JE, Lucia A. Exercise in people over 85. BMJ 2020;368:m402. [DOI] [PubMed] [Google Scholar]
- 10. Izquierdo M, Merchant RA, Morley JE, Anker SD, Aprahamian I, Arai H, et al. International Exercise Recommendations in Older Adults (ICFSR): expert consensus guidelines. J Nutr Health Aging 2021;25:824–853. [DOI] [PubMed] [Google Scholar]
- 11. Courel‐Ibáñez J, Pallarés JG, García‐Conesa S, Buendía‐Romero Á, Martínez‐Cava A, Izquierdo M. Supervised exercise (Vivifrail) protects institutionalized older adults against severe functional decline after 14 weeks of COVID confinement. J Am Med Dir Assoc 2021;22:217–219.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Heyn P, Abreu BC, Ottenbacher KJ. The effects of exercise training on elderly persons with cognitive impairment and dementia: a meta‐analysis. Arch Phys Med Rehabil 2004;85:1694–1704. [DOI] [PubMed] [Google Scholar]
- 13. Izquierdo M, Rodriguez‐Mañas L, Sinclair AJ. Editorial: what is new in exercise regimes for frail older people ‐ how does the erasmus Vivifrail project take us forward? J Nutr Health Aging 2016;20:736–737. [DOI] [PubMed] [Google Scholar]
- 14. Izquierdo M, Duque G, Morley JE. Physical activity guidelines for older people: knowledge gaps and future directions. Lancet Healthy Longev 2021;2:e380–e383. [DOI] [PubMed] [Google Scholar]
- 15. Lazarus NR, Izquierdo M, Higginson IJ, Harridge SDR. Exercise deficiency diseases of ageing: the primacy of exercise and muscle strengthening as first‐line therapeutic agents to combat frailty. J Am Med Dir Assoc 2018;19:741–743. [DOI] [PubMed] [Google Scholar]
- 16. Chan A‐W, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Casas‐Herrero A, Anton‐Rodrigo I, Zambom‐Ferraresi F, Sáez de Asteasu ML, Martinez‐Velilla N, Elexpuru‐Estomba J, et al. Effect of a multicomponent exercise programme (VIVIFRAIL) on functional capacity in frail community elders with cognitive decline: study protocol for a randomized multicentre control trial. Trials 2019;20:362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–M156. [DOI] [PubMed] [Google Scholar]
- 19. Izquierdo M, Casas‐Herrero A, Zambom‐Ferraresi F, Martínez‐Velilla N, Alonso‐Bouzón C & Rodríguez‐Mañas L. Multicomponent physical exercise program VIVIFRAIL. Available at: http://www.vivifrail.com/resources/. Accessed April 3, 2021.
- 20. Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self‐reported disability and prediction of mortality and nursing home admission. J Gerontol 1994;49:M85–M94. [DOI] [PubMed] [Google Scholar]
- 21. Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 2006;54:743–749. [DOI] [PubMed] [Google Scholar]
- 22. Lobo A, Ezquerra J, Gomez F, Sala JM, Seva Diaz A. El “Mini –Examen Cognoscitivo”: Un test sencillo, practico, para detectar alteraciones intelectivas en paciente médicos. Actas Lus‐Esp Neuol Psiquiatr 1979;3:189–202. [PubMed] [Google Scholar]
- 23. Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695–699. [DOI] [PubMed] [Google Scholar]
- 24. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J 1965;14:61–65. [PubMed] [Google Scholar]
- 25. Martinez De La Iglesia J, Onis Vilches O, Duenas Herrero R, Colomer CA, Aguado Taberne C, Luque R. The Spanish version of the Yesavage abbreviated questionnaire (GDS) to screen depressive dysfunctions in patients older than 65 years: adaptation and validation [in Spanish]. MEDIFAM 2002;12:620–630. [Google Scholar]
- 26. Badia X, Roset M, Montserrat S, Herdman M, Segura A. The Spanish version of EuroQol: a description and its applications. European Quality of Life scale. Med Clin (Barc) 1999;112:79–85. [PubMed] [Google Scholar]
- 27. Laukkanen P, Heikkinen E, Kauppinen M. Muscle strength and mobility as predictors of survival in 75‐84‐year‐old people. Age Ageing 1995;24:468–473. [DOI] [PubMed] [Google Scholar]
- 28. Hubbard RE, Fallah N, Searle SD, Mitnitski A, Rockwood K. Impact of exercise in community‐dwelling older adults. PLoS ONE 2009;4:e6174. 10.1371/journal.pone.0006174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pedersen BK, Saltin B. Exercise as medicine ‐ evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports 2015;25:1–72. [DOI] [PubMed] [Google Scholar]
- 30. Pahor M, Guralnik JM, Ambrosius WT, Blair S, Bonds DE, Church TS, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA 2014;311:2387–2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cadore EL, Casas‐Herrero A, Zambom‐Ferraresi F, Idoate F, Millor N, Gómez M, et al. Multicomponent exercises including muscle power training enhance muscle mass, power output, and functional outcomes in institutionalized frail nonagenarians. Age 2014;36:773–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. de Asteasu ML S, Martínez‐Velilla N, Zambom‐Ferraresi F, Casas‐Herrero Á, Izquierdo M. Role of physical exercise on cognitive function in healthy older adults: a systematic review of randomized clinical trials. Ageing Res Rev 2017;37:117–134. [DOI] [PubMed] [Google Scholar]
- 33. Angevaren M, Aufdemkampe G, Verhaar HJJ, Aleman A, Vanhees L. Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev 2008;3:CD005381. 10.1002/14651858.CD005381.pub3 [DOI] [PubMed] [Google Scholar]
- 34. de Asteasu ML S, Martínez‐Velilla N, Zambom‐Ferraresi F, Ramírez‐Vélez R, García‐Hermoso A, Izquierdo M. Cognitive function improvements mediate exercise intervention effects on physical performance in acutely hospitalized older adults. J Am Med Dir Assoc 2021;22:787–791. [DOI] [PubMed] [Google Scholar]
- 35. Prakash RS, Voss MW, Erickson KI, Kramer AF. Physical activity and cognitive vitality. Annu Rev Psychol 2015;66:769–797. [DOI] [PubMed] [Google Scholar]
- 36. Rasmussen P, Brassard P, Adser H, Pedersen MV, Leick L, Hart E, et al. Evidence for a release of brain‐derived neurotrophic factor from the brain during exercise. Exp Physiol 2009;94:1062–1069. [DOI] [PubMed] [Google Scholar]
- 37. Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev 2019;1:CD012424. 10.1002/14651858.CD012424.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. WHO Clinical Consortium on Healthy Ageing 2017 –report of consortium meeting 21 and 22 November 2017 in Geneva, Switzerland. Geneva: World Health Organization; 2018. [Google Scholar]
- 39. Izquierdo M, Rodriguez‐Mañas L, Casas‐Herrero A, Martinez‐Velilla N, Cadore EL, Sinclair AJ. Is it ethical not to precribe physical activity for the elderly frail? J Am Med Dir Assoc 2016;17:779–781. [DOI] [PubMed] [Google Scholar]
- 40. Clemson L, Fiatarone Singh MA, Bundy A, Cumming RG, Manollaras K, O'Loughlin P, et al. Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): randomised parallel trial. BMJ 2012;345:e4547. 10.1136/bmj.e4547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. von Haehling S, Morley JE, Coats AJS, Anker SD. Ethical guidelines for publishing in the Journal of Cachexia, Sarcopenia and Muscle: update 2021. J Cachexia Sarcopenia Muscle 2021;12:2259–2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting Information


