Abstract
Background:
The current systematic review aimed to determine the effect of telemedicine services on adherence in patients with chronic obstructive pulmonary disease (COPD) and to describe the type of adherence and applied devices and modules.
Materials and Methods:
We reviewed PubMed, Scopus, Web of Science, and Embase databases to identify relevant studies from the time of inception of these databases to March 10, 2019, using three groups of keywords. The first group comprised words describing COPD, the second group included words describing types of telemedicine interventions, and the third group contained words describing adherence. The reference list of identified articles was also hand-searched to retrieve possibly relevant articles.
Results:
In total 21 articles were included, in which 13 reported a positive effect for telemedicine on patients’ adherence. Adherence to treatment was classified under six categories. The highest frequency belongs to the adherence to performing exercises and participation in training sessions, using the system, using devices, measuring (like blood pressure, oxygen saturation, heart rate, weight, temperature, sputum volume) and reporting symptoms and the results of measurements, completing tasks, and medication.
Conclusion:
This study demonstrated the effectiveness of telemedicine services on adherence to treatment plans in patients with COPD. The following factors contribute to the effectiveness of telemedicine services: patient support by healthcare professionals and easy access to them, uninterrupted execution of telemedicine programs, follow-up and supervision of providers, creating and maintaining motivation in patients, and provision of different self-management modules.
Keywords: Chronic obstructive pulmonary disease, Adherence, Telemedicine
INTRODUCTION
Chronic diseases are a major cause of mortality in developed countries, with respiratory diseases being the second leading cause of death(1). Chronic obstructive pulmonary disease (COPD) is a prevalent respiratory disease characterized by the obstruction of airways and highly affecting the physical, mental, and social performance of patients(2). In addition, it claims several lives annually worldwide (3), which not only has negative effects on public health and quality of life (QoL) of patients but also imposes a heavy social and economic burden on healthcare systems(4). According to the World Health Organization (WHO) estimates about 251 million people suffer from COPD worldwide (5). In addition, it is predicted that COPD will become the third leading cause of global mortality by 2030 (6). Furthermore, readmission is an important problem for those who suffer from COPD, so that 10–20% of patients with COPD are re-admitted within 30 days (7). In the United States, the 30-day readmission rate for COPD patients is 22.6 percent(8).
The most important factors affecting the progression of the disease, which in turn translate into increased healthcare costs, include the lack of sufficient training, patients’ non-adherence to disease guidelines, and lack of timely diagnosis of the symptoms (9). In COPD, self-management and support are essential for the desired control and timely diagnosis of the disease(10). In addition, self-management is the basis of successful management in patients with COPD(11). Patient's QoL and unplanned hospitalization can be managed through enhancing self-management and adherence to treatment (12). Self-management of the disease refers to patients’ ability to manage symptoms and health-related behaviors, which results in increased QoL. Accordingly, self-management requires the active participation of patients in managing their health status (13), which decreases their anxiety, limits the occurrence of complications, increases independence and adherence to performing daily activities, and reduces costs (14). Therefore, there is an increasing need for self-management tools in patients with COPD, for not only controlling the disease and its symptoms but also teaching adaptation to daily activities, disease management, and changing their lifestyle (15). Telemedicine services are a self-management tool for supporting patients (1). In a broad definition, the WHO has defined telemedicine as the delivery of health care services at a distance using electronic means for “diagnosing the disease, make a decision about treatment, prevention of disease and injuries, research and evaluation, and education of providers” (16). Telemedicine uses several multimedia tools which creates a kind of time and place independence in medical services using a large number of modern technologies(17). Many telemedicine systems are equipped with a wide range of devices, equipment, modules, and technologies to provide better services to patients, which are essential for advancing health and achieving better communication between providers and patients(18).
On the one hand, telemedicine services can be useful and effective only when patients accept the system and adhere to the treatment plan(19). Adherence to treatment is defined as a person’s behavior in accordance with the treatment regimen and consumption of medications or changing the lifestyle based on guidelines recommended by healthcare service providers (20). Non-adherence to the treatment plan is a major obstacle to reaching positive results in the treatment plan (21). Hence, it can be argued that in the absence of patients believe in their capabilities to improve their health status through changing their behaviors, telemedicine plans won't achieve their goals. In addition, patients believe plays a unique role in treatment adherence, even if considerable time, energy, and costs are spent on the establishment of a telemedicine service (22). By adhering to treatment plans, one can reduce the occurrence of serious complications, control the progress of the disease, reduce healthcare costs, limit hospitalization and mortality, and improve patients’ QoL (23). Research indicates that adherence to treatment plans is poor in patients with COPD (24, 25), varying from 40 to 90% (26). Some studies reported declining adherence over time (26, 27). Although adherence is essential for the optimization of COPD management,(28) few studies have focused on this topic (24, 29). Moreover, systematic studies on management in patients with COPD have mostly focused on the experience of clinical specialists, specific functions and interventions, or the use of specific systems in hospitals or houses (30–32). Some other systematic reviews have investigated the effectiveness of telemedicine interventions on the clinical outcomes of patients (33, 34), reduction of the use of healthcare services (35), and the feasibility study of telemedicine for patients with COPD (36). To the best of our knowledge, no systematic review has been conducted on the effect of telemedicine services on the adherence of patients with COPD. A systematic review conducted by Cruz et al. (2014) (37) has only investigated the effect of home telemonitoring on the satisfaction and adherence of patients with COPD. Therefore, the present systematic review aimed to determine the effect of telemedicine services on adherence in patients with COPD and to describe the type of adherence and applied devices and modules.
MATERIALS AND METHODS
Information sources and search strategy
The current systematic review aimed to determine the effect of telemedicine systems on the adherence of patients with COPD. The systematic search strategy was designed using MeSH terms, previous studies, and the ideas of authors. Then, the search was conducted in PubMed, Scopus, Web of Science, and Embase databases up to March 10, 2019. The search for articles was performed in all fields by combining three groups of keywords relevant to the research topic. The first group comprised words describing COPD, the second group included words describing types of telemedicine interventions, and the third group contained words describing adherence. All three groups were combined using the OR operator and then with other keywords using the AND operator. Moreover, the wildcard operator “*” was used when the derivatives of a word had to be searched. Keywords employed for searching articles are presented in Table 1. The reference list of identified articles was also hand-searched to retrieve possibly relevant articles.
Table 1.
Search strategy in scientific databases
| Time | Search was conducted up to March 10, 2019 | |
|---|---|---|
| Criteria | Language | English |
| Databases | PubMed: All fields | |
| Scopus: All fields | ||
| Embase: All fields | ||
| ISI: All fields | ||
| #1 | “Chronic Obstructive Pulmonary Disease” OR “COPD” OR “Pulmonary Disease” OR “Chronic Obstructive” OR “Chronic Obstructive Airway Disease” OR “Airway Obstruction*” OR “ COAD” OR “Chronic Obstructive Lung Disease” OR “COLD” OR “Airflow Obstruction*” OR “Respiratory Tract Diseases” OR “Lung Diseases” OR “Bronchitis” OR “Pulmonary Emphysema” OR “Emphysema” OR “Lung emphysema” | |
| #2 | “Telemedicine” OR “Telecommunications” OR “Telemetry” OR “Telepathology” OR “Teleradiology” OR “Telerehabilitation” OR “Communications Media” OR “Remote Consultation” OR “Mobile Health” OR “Mhealth” OR “Telehealth” OR “Ehealth” | |
| #3 | “Adherence” OR “Compliance” OR “Follow-up” OR “Trace” | |
| Search | #1 AND #2 AND #3 |
Eligibility criteria
This systematic review is structured according to preferred reporting items for systematic reviews (PRISMA) guideline (38).
Inclusion Criteria: Inclusion criteria were English language articles, journal articles, conference papers, randomized clinical trials (RCTs), and quasi-experimental studies up to 2019/03/10; these studies had to meet the following two criteria: 1) using telemedicine services for managing patients with COPD, and 2) partly or fully focusing on the adherence of patients to the treatment plan.
Exclusion Criteria
Exclusion criteria were reporting other diseases in addition to COPD, observational studies that did not include a telemonitoring intervention, and case studies.
Non-original papers, including reviews, study protocols, editorials, and commentaries were not deemed eligible and were, consequently, excluded from the present review; still, their reference lists were carefully examined.
Study selection
In the screening phase, two authors independently evaluated the titles and abstracts of the retrieved articles and excluded irrelevant studies based on inclusion and exclusion criteria. In the second phase (eligibility), two authors independently read the full text of all articles remaining from the first phase, and then selected articles meeting the inclusion criteria. In case of a disagreement, a consensus was reached through discussion or, if necessary, the third reviewer was consulted. Furthermore, the most prominent authors were contacted with a request for gray literature, i.e. conference papers.
Data collection process
Data extraction was performed using a structured table format, which included: bibliographical information, type of study, location of study, number of patients, age of patients, number of people in the comparison group and number of people in the control group, type of intervention, duration of intervention, devices and modules used in the telemedicine service, type of adherence, and the effect to telemedicine on adherence in patients with COPD.
Methodology Quality Assessment
Methodological quality assessment was conducted independently by two reviewers via a modified version of the scoring system designed by Hailey et al. (39) to assess telemedicine research. A quality score was computed based on five areas of study performance and one area of research design. For study performance, the following five areas of interest were taken into account: patient selection, intervention description/specification, study specification and analysis, patient disposal, and the outcomes reported. For research design, scores were allocated to four types of research: large-scale randomized controlled trials (RCT) (≥50 participants in each arm), smaller RCTs, prospective non-randomized studies, and retrospective comparative studies. Disagreements between the reviewers were resolved by consulting a third independent researcher. Finally, the quality score was classified into five categories, ranging from A (high quality) to E (poor quality). Details for the telemedicine studies checklist are provided in Table 2.
Table 2.
Telemedicine Studies Checklist Scores and Items
| Items on checklist | Details | Score* | |
|---|---|---|---|
| Performance | Patient selection | Methods of randomization/selection; equivalence of intervention and control groups; drop-outs before start of intervention | 2 |
| Description/specification of the interventions | Adequate description for both intervention and control groups | 2 | |
| Specification and analysis of study | Sample size; statistical methods used; clear specification of outcome measures | 2 | |
| Patient disposal | Length of follow-up; drop-outs; compliance failures | 2 | |
| Outcomes reported | Fullness and clarity of reporting; missing results; statistical summary; whether conclusions were consistent with data | 2 | |
| Design | Large randomized controlled trials | Defined as those with at least 50 subjects in each arm | 5 |
| Smaller randomized controlled trials | 3 | ||
| Prospective non-randomized studies | 2 | ||
| Retrospective comparative studies | 1 |
Category A: scores 11.5–15 (High quality)
Category B: scores 9.5– 11 (Good quality)
Category C: scores 7.5–9 (Fair to good quality)
Category D: scores 5.5–7 (Poor to fair quality)
Category E: scores 1– 5 (Poor quality)
RESULTS
Summary of Study Characteristics
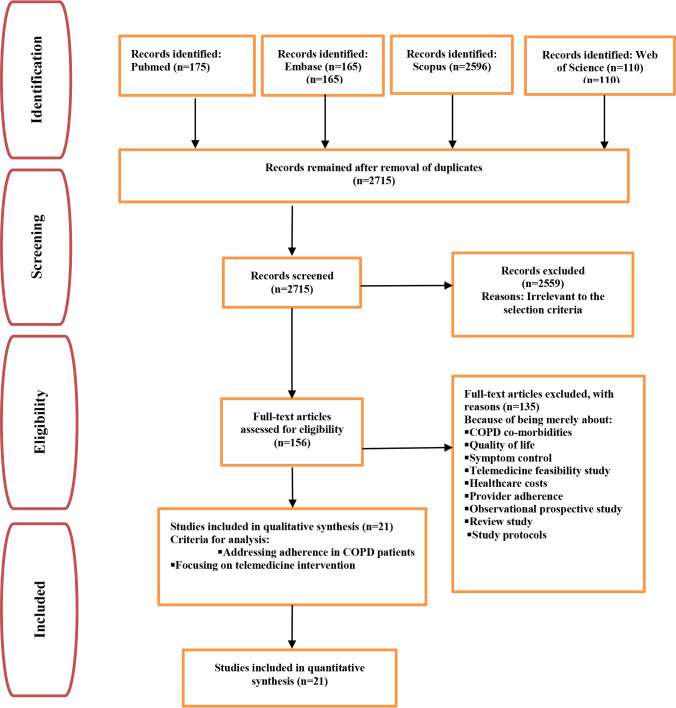
Number of studies: Initially, searching four target databases yielded a total of 3046 articles, which were subsequently imported into the reference management software, EndNote. After removing duplicates and unrelated articles based on their titles, abstracts, and texts, 21 articles were ultimately selected. Of the 21 selected studies, 13 were RCTs and eight were quasi-experimental studies. The workflow of the article selection is shown in Figure 1.
Figure 1.
Flow diagram of included and excluded studies
Sources of the studies
Most studies were conducted in the UK (four studies), followed by the Netherlands (three), Spain, Norway, and Australia (two each). Other studies reported different data on locations.
Characteristics of telemedicine intervention
The number of participants varied from nine to 301. Moreover, the mean age of participants ranged from 55 to 75 years. The most frequent telemedicine service was telemonitoring (n=9), followed by telerehabilitation (n=8). Furthermore, the duration of intervention using telemedicine services ranged from four weeks to two years. The characteristics of the studies are presented in Table 3.
Table 3.
Main Characteristics and Description of the Technology Used in the Studies
| ID | First author (year) | Study design | Location | Participants | Age Mean(std), (CG/IG) | Type of Telemedicine services | Telemedicine duration |
|---|---|---|---|---|---|---|---|
| 1 | Calvo GS/2014(3) | RCT | Spain | 59; IG(n=29), CG(n=30) | 72.7 ± 9.3 / 75.0 ± 9.7 | Home Telemonitoring | 7-months |
| 2 | Sanchez-Morillo D/2015(9) | UBA | Spain | IG(n=15) | 70.2±6.6 | Home Telemonitoring | 6-months |
| 3 | Tabak M/2014(2) | RCT | Netherlands | 12; IG(n=10)/CG(n=2) | 62.8±7.4/64.1±9.0 | Home Telemonitoring and Teleconsultation | 9 months |
| 4 | Tabak M / 2014 (48) | RCT | Netherlands | 30; IG(n = 14 )/CG (n = 16) | 67.9 ± 5.7 / 65.2 ± 9.0 | Home Telerehabilitation | 4 weeks |
| 5 | Hoaas H/2016(27) | UBA | Norway | IG(n=10) | 55.2 | Home Telerehabilitation | Two-year |
| 6 | Dekker-van Weering MGH/2016(52) | UBA | Netherlands | IG(n=22) | 61.7 (9.3) | Home Telemonitoring and Telecommunication | 12 weeks |
| 7 | Hoaas H/2016(53) | UBA | Norway | IG(n=9) | 58.1±6 | Home Telerehabilitation | 2-year |
| 8 | Benzo RP/2018(51) | UBA | Rochester | IG(n=12) | >=40 | Home Telerehabilitation | 8-week |
| 9 | Velardo C / 2017(50) | RCT | United Kingdom | 166;IG(n=110)/CG(n=56) | >=40 in IG | Home Telemonitoring | 12-month |
| 10 | Tsai LLY/2017(49) | RCT | Australia | 36; IG(n=19)/CG(n=17) | 75 (9) / 73 (8) | Home Telerehabilitation | 8-week |
| 11 | Thomas RM/2017(55) | UBA | United States | IG(n=35) | 67.5 ±6.6 | Home Videoconferencing | 3 months |
| 12 | Moy ML / 2016(46) | RCT | United States | 237; IG(n=153),CG (n=84) | 66.4 (9.2)/67 (8.6) | Home Telemonitoring | 12 months |
| 13 | Bourne S/2017(42) | RCT | United Kingdom | 90;IG (n=64), CG (n=26) | 71.4 (8.6)/69.1 (7.9) | Home Telerehabilitation | 6 weeks |
| 14 | Antoniades NC/2012(40) | RCT | Australia | 36; IG(n=16), CG(n=20) | 68 (9) / 70 (10) | Home Tele monitoring | 12 months |
| 15 | Farmer A/2017(45) | Multicenter RCT | United Kingdom | 141;IG(n=93), CG(n=48) | 69.8 (10.6)/69.8 (9.1) | Telemonitoring | 12 months |
| 16 | Ringbaek TJ / 2016(47) | NRCT | Denmark | 99; IG(n=42), CG(n=57) | 68.8 (11.0) / 68.4 (9.1) | Home Telerehabilitation | 7–10weeks |
| 17 | Vitacca M/2013(56) | UBA | Italy | IG(n=39) | 72 ± 8.6 | Home Tele-assistance | 6 months |
| 18 | Blumenthal JA/2014(41) | RCT | Columbus | 301; IG (N=150)/CG N=151) | 66.6 (8.7)/65.6 (7.9) | Telephone-based coping skills training (CST) | 16 weeks |
| 19 | Smith HS / 2016(54) | UBA | NA | IG(n=30) | 72.2 (5.7)/67.8 (7.0) | Home Telecommunication and Telemonitoring | 320 days |
| 20 | Broadbent E / 2018(43) | RCT | New Zealand | 51; IG(n=25), CG(n=26) | 69.10 (9.85)/70.57 (10.34) | Home Telerobotic | 4 months |
| 21 | Cox M / 2018(44) | RCT | United Kingdom | 58;IG (n=43)/CG(n=15) | 67.8 (11.12) | Home Telerehabilitation | 7 months |
UBA – uncontrolled before and after study; NRCT– non-randomized controlled trial; RCT – randomized controlled trial; NA – no information available; IG – intervention group; CG – control group; SD – standard deviation
Quality Assessment
Assessment quality levels differed across articles: 12 were rated A (high-quality) (3, 40–50), and nine were rated B (good quality) (2, 9, 27, 51–56).
Telemedicine Description
In some studies, the details on telemedicine services in terms of the employed equipment and modules were provided:
Equipment used in the telemedicine system
The devices and equipment used in telemedicine services varied across studies. The most frequently used devices were monitoring and measurement devices (2, 3, 27, 40, 43–46, 48, 49, 51, 53, 55), mobile applications (2, 9 , 41, 46, 48, 50, 51, 54–56), and computers and laptops (9, 27, 40, 45–47, 49–51, 53), in that order.
Modules used in the telemedicine system
The most frequently used modules in telemedicine services were modules related to monitoring (27, 43, 44, 47, 52, 54, 56), followed by those related to self-management ( 2, 27, 40, 45, 50, 53), video modules (43, 45, 47, 51, 55), modules related to exercise training (27, 42, 44, 52), and communication, chatting, and consulting modules (2, 46, 50, 52).
Patient Adherence
Since patients’ adherence to the use of telemedicine services was the focus of this study, the data belonging to the control group (if any) were not entered. Data on the type of adherence and the effect of telemedicine services on patients’ adherence are given in Table 4.
Table 4.
Impact of Telemedicine Services on Adherence
| Row | Measures on adherence | Effect of telemedicine on adherence |
|---|---|---|
| 1 | Adherence was calculated as the percentage of the total days the patient utilized the devices to monitor the parameters (3). | + |
| 2 | Compliance rate was defined as the ratio of completed tasks (the number of days in which a valid questionnaire and respiratory recording were received) (9). | + |
| 3 | Adherence to the exercise scheme was calculated by dividing the number of schemes prescribed by the number of schemes performed (2). | − |
| 4 | Compliance was calculated by dividing the number of days the activity sensor was worn by the minimum number of days that it was prescribed (i.e. ≥ four days/week) (48). | + |
| 5 | Adherence was measured in terms of the frequency of registrations on the webpage (27). | − |
| 6 | Adherence to the exercises was defined as the percentage of exercises performed versus the exercises prescribed (52). | + |
| 7 | Adherence rate was calculated based on the recommendation of regular daily diary registrations and three training sessions per week (53). | − |
| 8 | Adherence rates were defined as the percentage of the days the task (daily completion data on 12-minute walking, full-body exercises, and the check-in wellness questionnaire) was completed (51). | + |
| 9 | Compliance was calculated as the number of days a week that a patient used the system (maximum compliance could be as high as 7) (50). | + |
| 10 | Compliance was calculated in terms of the number of completed exercise training sessions as prescribed out of a possible 24 sessions (49). | + |
| 11 | Self-reported inhaler training adherence (55) | + |
| 12 | Device adherence was defined as the percentage of days with valid step-count data (46). | + |
| Adherence for website engagement was examined by the number of log-ins to the website each month (46). | − | |
| 13 | Adherence was calculated as attendance at exercise sessions (seven sessions) (42). | − |
| 14 | Adherence was the percentage of days with completed measurements (forced spirometry, relaxed spirometry, SpO2, body temperature, blood pressure, weight) (40). | + |
| 15 | Adherence was measured using the Medication Adherence Report Scale (45). | − |
| Compliance was defined by the use of the system (days per week of use across all patients) (45). | + | |
| 16 | Adherence to pulmonary rehabilitation (47). | − |
| 17 | Compliance was defined as the use of the Respicard (expected 24 cards/6 months) | + |
| (Respicard is a clinical scoring system employed in the tele-assistance of COPD.) (56) | ||
| 18 | Treatment adherence was calculated in terms of attendance in the CST (coping skills training) phone calls (ranging from one to 14 sessions) (41). | + |
| 19 | Adherence to symptoms reports was defined as the number of reports made divided by the number of days enrolled in the program for each patient (54). | + |
| 20 | Adherence to medication was calculated as the percentage of prescribed doses taken. Adherence was also measured using the Medication Adherence Report Scale (43). | + |
| Adherence to the respiratory exercise was assessed by asking patients how many times they performed their respiratory exercises over the past week at the baseline and at follow-up (43). | + | |
| 21 | Adherence was defined as attendance in 80% of the sessions, including (rounded to) three sessions for home EPR (early pulmonary rehabilitation) (44). | + |
| Adherence was defined as attendance in 80% of the sessions, including 12 sessions for hospital EPR (early pulmonary rehabilitation) (44). | - |
Type of Adherence to Treatment
The type of adherence and its estimation are reported differently across studies. In general, adherence to treatment was classified under six categories. The highest frequency belonged to adherence to performing exercise and participation in training sessions (2, 41–44, 47, 49, 52, 53, 55), adherence to the use of the system (27, 45, 46, 50, 56), adherence to the use of devices (3, 46, 48), adherence to measurement and reporting the symptoms and results of measurements (40, 54), adherence to medications (43, 45), and adherence to completing tasks (filling in the questionnaires, walking, and respiratory recording) (9, 51).
The effect of telemedicine on patients’ adherence
Of selected 21 studies, 13 reported a positive effect for telemedicine on patients’ adherence (3, 9, 40, 41, 43, 48–52, 54–56), whereas five found a negative effect (2, 27, 42, 47, 53). Some studies examined two types of adherence to treatment (44–46). Moreover, in some cases, the effect of telemedicine was reported to be positive in some cases and negative in others.
DISCUSSION
The present systematic review examined the effects of telemedicine services on adherence to treatment in patients with COPD and described the types of adherence and devices and modules employed. The results demonstrated that interventions based on telemedicine services are effective on the adherence of patients with COPD. In general, in this study, adherence to reporting symptoms and measurements and adherence to performing tasks were positive when using telemedicine services. Moreover, the adherence to sessions and training exercises, using the system, and using the devices were positively influenced by telemedicine interventions in most studies. Examining the effectiveness of strategies intended to increase the adherence to medication in patients with COPD, a systematic review by Bryant et al.(57) indicated that five reported improvements in adherence in short- or long-term from the seven interventional studies. Furthermore, the systematic review by Cruz et al. (37) reported positive results due to adherence among patients with COPD using the telemonitoring system.
In general, numerous factors contribute to the adherence of patients using telemedicine services. These factors were examined in studies reporting a positive result due to adherence. It was found that utilizing easy-to-use devices and equipment (3), usability in the design and development of telemedicine services (9), and design and development of attractive and motivational telemedicine services for patients can increase patients’ adherence (55). Since the provision of self-care equipment and services and their design and use are not enough for adherence, some studies reported other factors that are capable of enhancing adherence. Patients’ satisfaction and adherence can be enhanced by the flexibility of the treatment plans to make them compatible with patients’ needs and interests (51). Moreover, the patient-healthcare provider interaction is the key to successful telehealth interventions (50).
Healthcare professionals play a key role in helping patients to enhance their self-management skills and adherence, because their negative attitudes towards telemedicine interventions may make patients lose their trust in these technologies, leading to non-adherence to the treatment plan (58).
In addition, regular treatment plans and easy and timely access to healthcare professionals promote adherence in patients (59). In this review, one study reported a high level of adherence in reporting symptoms. Patients mentioned that a symptom report was prepared for them in less than two minutes, which did not take much. Moreover, they were ensured about the quick examination of their reports (54).
In one study, satisfactory results are reported concerning adherence to sessions and exercises using a robot. The social aspects and visualizing a robot increased access to exercise instructions, and equipping robots with a reminder and alarm system contributed to the acceptance of this system and increased the adherence of patients (43). Adherence to exercises and training sessions, medication plan, and the use of the system had a decreasing trend in some studies. Results of a systematic review by Maeder et al. (60) showed that the level of adherence is reduced over the first weeks and months in most studies. It seems that the use of technologies that are not motivating or stimulating enough may decrease adherence over time (2). Furthermore, the results of another study demonstrated that holding group sessions may pose an obstacle to adherence in some patients with COPD and thus justify its decreasing trend (42). Chau et al. (61) reported that, when patients transfer data only once a day, their adherence is increased; however, if they send data three times a day, their adherence is decreased. Therefore, it seems that a difference in treatment protocols can affect the adherence of patients. Moreover, the chronic nature of the disease, consumption of multiple drugs, symptom remission periods, aging, and insufficient training for patients with COPD may decrease adherence (62). In the present study, the most commonly used devices were monitoring and measurement devices followed by mobiles and computers. Mobile and wireless monitoring technologies are increasingly employed in healthcare for communication, data collection, monitoring the patients, training, and facilitating adherence in the management of chronic diseases. A systematic review by Hamine et al. (63) examining the effect of mHealth on the management of adherence to treatment in chronic diseases suggested that an emphasis on understanding and improving mHealth tools can overcome specific barriers to adherence.
Moreover, the results of the present study demonstrated that telemedicine services are equipped with certain modules, including those for self-monitoring, self-management, and consultation. Findings of a review study on strategies that may increase adherence showed that interventions which are a combination of information, reminders, self-monitoring, self-management, consultation, and supportive care are the most effective option to enhance adherence(57). Therefore, to enhance adherence, it seems essential to equip telemedicine services with self-management and self-care modules in chronic diseases, including COPD.
Advantages and Limitations of the Study
This study was limited by some factors. First, the language of articles was restricted to English, and the inclusion of other languages may have offered different results. The second limitation was not conducting a meta-analysis, but this was because a meta-analysis could not be performed due to the difference in research designs, tools of measurement, and the nature of the reported findings.
The advantage of this study lies in the fact that, to the best of our knowledge, it is the first systematic review examining the effect of telemedicine services on the adherence of patients with COPD.
Recommendations for future telemedicine interventions
It is recommended that patients’ ideas, opinions, needs, and interests be taken into account when designing and implementing telemedicine services in order to enhance adherence in patients with COPD.
CONCLUSION
It can be generally concluded from the findings that the use of telemedicine services and interventions can affect the level of adherence in patients with COPD to the treatment plan. To enhance adherence to treatment plan using telemedicine services, factors such as usability and user-friendly design, patients’ support by healthcare professionals, easy access to them, uninterrupted execution of telemedicine programs, security and confidentiality of the collected data, follow-up and supervision of providers, keeping patients motivated, use of easy and accessible devices, provision of different self-management modules, and availability of alarms and reminders for patients must be taken into account.
Footnotes
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
REFERENCES
- 1.Pedone C, Lelli D. Systematic review of telemonitoring in COPD: an update. Pneumonol Alergol Pol 2015;83(6):476–84. [DOI] [PubMed] [Google Scholar]
- 2.Tabak M, Brusse-Keizer M, van der Valk P, Hermens H, Vollenbroek-Hutten M. A telehealth program for self-management of COPD exacerbations and promotion of an active lifestyle: a pilot randomized controlled trial. Int J Chron Obstruct Pulmon Dis 2014;9935–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Segrelles Calvo G, Gómez-Suárez C, Soriano JB, Zamora E, Gónzalez-Gamarra A, González-Béjar M, et al. A home telehealth program for patients with severe COPD: the PROMETE study. Respir Med 2014;108(3):453–62. [DOI] [PubMed] [Google Scholar]
- 4.Bourbeau J, Casan P, Tognella S, Haidl P, Texereau JB, Kessler R. An international randomized study of a home-based self-management program for severe COPD: the COMET. Int J Chron Obstruct Pulmon Dis 2016;111447–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chronic obstructive pulmonary disease (COPD) . Available from url: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd). [Cited 2020 October 19]. [Google Scholar]
- 6.Hashemi SY, Momenabadi V, Faramarzi A, Kiani A. Trends in burden of chronic obstructive pulmonary disease in Iran, 1995–2015: findings from the global burden of disease study. Arch Public Health 2020;78:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simmering JE, Polgreen LA, Comellas AP, Cavanaugh JE, Polgreen PM. Identifying Patients With COPD at High Risk of Readmission. Chronic Obstr Pulm Dis 2016;3(4):729–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kong CW, Wilkinson TMA. Predicting and preventing hospital readmission for exacerbations of COPD. ERJ Open Res 2020;6(2):00325–2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sánchez-Morillo D, Crespo M, León A, Crespo Foix LF. A novel multimodal tool for telemonitoring patients with COPD. Inform Health Soc Care 2015;40(1):1–22. [DOI] [PubMed] [Google Scholar]
- 10.Gagné M, Lauzier S, Babineau-Therrien J, Hamel C, Penney SE, Bourbeau J, et al. COPD-Specific Self-Management Support Provided by Trained Educators in Everyday Practice is Associated with Improved Quality of Life, Health-Directed Behaviors, and Skill and Technique Acquisition: A Convergent Embedded Mixed-Methods Study. Patient 2020;13(1):103–119. [DOI] [PubMed] [Google Scholar]
- 11.Billington J, Coster S, Murrells T, Norman I. Evaluation of a Nurse-Led Educational Telephone Intervention to Support Self-Management of Patients With Chronic Obstructive Pulmonary Disease: A Randomized Feasibility Study. COPD 2015;12(4):395–403. [DOI] [PubMed] [Google Scholar]
- 12.Russell S, Ogunbayo OJ, Newham JJ, Heslop-Marshall K, Netts P, Hanratty B, et al. Qualitative systematic review of barriers and facilitators to self-management of chronic obstructive pulmonary disease: views of patients and healthcare professionals. NPJ Prim Care Respir Med 2018;28(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van de Velde D, De Zutter F, Satink T, Costa U, Janquart S, Senn D, et al. Delineating the concept of self-management in chronic conditions: a concept analysis. BMJ Open 2019;9(7):e027775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee YM. Chronic obstructive pulmonary disease: respiratory review of 2014. Tuberc Respir Dis (Seoul) 2014;77(4):155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ambrosino N, Bertella E. Lifestyle interventions in prevention and comprehensive management of COPD. Breathe (Sheff) 2018;14(3):186–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Serper M, Volk ML. Current and Future Applications of Telemedicine to Optimize the Delivery of Care in Chronic Liver Disease. Clin Gastroenterol Hepatol 2018;16(2):157–161.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta R, Gamad RS, Bansod P. Telemedicine: A brief analysis. Cogent Engineering 2014;1(1):966459. [Google Scholar]
- 18.Li KF. Smart home technology for telemedicine and emergency management. J Ambient Intell Humaniz Comput 2013;4(5):535–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roberts AW, Crisp GD, Esserman DA, Roth MT, Weinberger M, Farley JF. Patterns of medication adherence and health care utilization among patients with chronic disease who were enrolled in a pharmacy assistance program. N C Med J 2014;75(5):310–8. [DOI] [PubMed] [Google Scholar]
- 20.Goudarzi H, Barati M, Bashirian S, Moeini B. Determinants of medication adherence among hypertensive patients using the Pender's health promotion model. J Educ Health Promot 2020;9:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naghavi S, Mehrolhassani MH, Nakhaee N, Yazdi-Feyzabadi V. Effective factors in non-compliance with therapeutic orders of specialists in outpatient clinics in Iran: a qualitative study. BMC Health Serv Res 2019;19(1):413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vitacca M, Montini A, Comini L. How will telemedicine change clinical practice in chronic obstructive pulmonary disease? Ther Adv Respir Dis 2018;12:1753465818754778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neiman AB, Ruppar T, Ho M, Garber L, Weidle PJ, Hong Y, et al. CDC Grand Rounds: Improving Medication Adherence for Chronic Disease Management - Innovations and Opportunities. MMWR Morb Mortal Wkly Rep 2017;66(45):1248–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rogliani P, Ora J, Puxeddu E, Matera MG, Cazzola M. Adherence to COPD treatment: Myth and reality. Respir Med 2017;129117–123 [DOI] [PubMed] [Google Scholar]
- 25.López-Campos JL, Quintana Gallego E, Carrasco Hernández L. Status of and strategies for improving adherence to COPD treatment. Int J Chron Obstruct Pulmon Dis 2019;141503–1515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Celler B, Argha A, Varnfield M, Jayasena R. Patient Adherence to Scheduled Vital Sign Measurements During Home Telemonitoring: Analysis of the Intervention Arm in a Before and After Trial. JMIR Med Inform 2018;6(2):e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoaas H, Andreassen HK, Lien LA, Hjalmarsen A, Zanaboni P. Adherence and factors affecting satisfaction in long-term telerehabilitation for patients with chronic obstructive pulmonary disease: a mixed methods study. BMC Med Inform Decis Mak 2016;16:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jardim JR, Nascimento OA. The Importance of Inhaler Adherence to Prevent COPD Exacerbations. Med Sci (Basel) 2019;7(4):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Montes de Oca M, Menezes A, Wehrmeister FC, Lopez Varela MV, Casas A, Ugalde L, et al. Adherence to inhaled therapies of COPD patients from seven Latin American countries: The LASSYC study. PLoS One 2017;12(11):e0186777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alwashmi M, Hawboldt J, Davis E, Marra C, Gamble JM, Abu Ashour W. The Effect of Smartphone Interventions on Patients With Chronic Obstructive Pulmonary Disease Exacerbations: A Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth 2016;4(3):e105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jeppesen E, Brurberg KG, Vist GE, Wedzicha JA, Wright JJ, Greenstone M, et al. Hospital at home for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012;(5):CD003573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kamei T, Yamamoto Y, Kajii F, Nakayama Y, Kawakami C. Systematic review and meta-analysis of studies involving telehome monitoring-based telenursing for patients with chronic obstructive pulmonary disease. Jpn J Nurs Sci 2013;10(2):180–92. [DOI] [PubMed] [Google Scholar]
- 33.Polisena J, Tran K, Cimon K, Hutton B, McGill S, Palmer K, et al. Home telehealth for chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Telemed Telecare 2010;16(3):120–7. [DOI] [PubMed] [Google Scholar]
- 34.Lundell S, Holmner Å, Rehn B, Nyberg A, Wadell K. Telehealthcare in COPD: a systematic review and meta-analysis on physical outcomes and dyspnea. Respir Med 2015;109(1):11–26. [DOI] [PubMed] [Google Scholar]
- 35.McLean S, Nurmatov U, Liu JL, Pagliari C, Car J, Sheikh A. Telehealthcare for chronic obstructive pulmonary disease: Cochrane Review and meta-analysis. Br J Gen Pract 2012;62(604):e739–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bolton CE, Waters CS, Peirce S, Elwyn G, EPSRC and MRC Grand Challenge Team . Insufficient evidence of benefit: a systematic review of home telemonitoring for COPD. J Eval Clin Pract 2011;17(6):1216–22. [DOI] [PubMed] [Google Scholar]
- 37.Cruz J, Brooks D, Marques A. Home telemonitoring in COPD: a systematic review of methodologies and patients' adherence. Int J Med Inform 2014;83(4):249–63. [DOI] [PubMed] [Google Scholar]
- 38.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hailey D, Ohinmaa A, Roine R. Study quality and evidence of benefit in recent assessments of telemedicine. J Telemed Telecare 2004;10(6):318–24. [DOI] [PubMed] [Google Scholar]
- 40.Antoniades NC, Rochford PD, Pretto JJ, Pierce RJ, Gogler J, Steinkrug J, et al. Pilot study of remote telemonitoring in COPD. Telemed J E Health 2012;18(8):634–40. [DOI] [PubMed] [Google Scholar]
- 41.Blumenthal JA, Emery CF, Smith PJ, Keefe FJ, Welty-Wolf K, Mabe S, et al. The effects of a telehealth coping skills intervention on outcomes in chronic obstructive pulmonary disease: primary results from the INSPIRE -II study. Psychosom Med 2014;76(8):581–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bourne S, DeVos R, North M, Chauhan A, Green B, Brown T, et al. Online versus face-to-face pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: randomised controlled trial. BMJ Open 2017;7(7):e014580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Broadbent E, Garrett J, Jepsen N, Li Ogilvie V, Ahn HS, Robinson H, et al. Using Robots at Home to Support Patients With Chronic Obstructive Pulmonary Disease: Pilot Randomized Controlled Trial. J Med Internet Res 2018;20(2):e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cox M, O'Connor C, Biggs K, Hind D, Bortolami O, Franklin M, et al. The feasibility of early pulmonary rehabilitation and activity after COPD exacerbations: external pilot randomised controlled trial, qualitative case study and exploratory economic evaluation. Health Technol Assess 2018;22(11):1–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Farmer A, Williams V, Velardo C, Shah SA, Yu LM, Rutter H, et al. Self-Management Support Using a Digital Health System Compared With Usual Care for Chronic Obstructive Pulmonary Disease: Randomized Controlled Trial. J Med Internet Res 2017;19(5):e144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Moy ML, Martinez CH, Kadri R, Roman P, Holleman RG, Kim HM, et al. Long-Term Effects of an Internet-Mediated Pedometer-Based Walking Program for Chronic Obstructive Pulmonary Disease: Randomized Controlled Trial. J Med Internet Res 2016;18(8):e215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ringbaek TJ, Lavesen M, Lange P. Tablet computers to support outpatient pulmonary rehabilitation in patients with COPD. Eur Clin Respir J 2016;3:31016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tabak M, Vollenbroek-Hutten MM, van der Valk PD, van der Palen J, Hermens HJ. A telerehabilitation intervention for patients with Chronic Obstructive Pulmonary Disease: a randomized controlled pilot trial. Clin Rehabil 2014;28(6):582–91. [DOI] [PubMed] [Google Scholar]
- 49.Tsai LL, McNamara RJ, Moddel C, Alison JA, McKenzie DK, McKeough ZJ. Home-based telerehabilitation via real-time videoconferencing improves endurance exercise capacity in patients with COPD: The randomized controlled TeleR Study. Respirology 2017;22(4):699–707. [DOI] [PubMed] [Google Scholar]
- 50.Velardo C, Shah SA, Gibson O, Clifford G, Heneghan C, Rutter H, et al. Digital health system for personalised COPD long-term management. BMC Med Inform Decis Mak 2017;17(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Benzo RP, Kramer KM, Hoult JP, Anderson PM, Begue IM, Seifert SJ. Development and Feasibility of a Home Pulmonary Rehabilitation Program With Health Coaching. Respir Care 2018;63(2):131–140. [DOI] [PubMed] [Google Scholar]
- 52.Dekker-van Weering MG, Vollenbroek-Hutten MM, Hermens HJ. Adherence to an online exercise program for COPD patients in the home environment-a pilot study. Health and technology 2016;6(4):259–68. [Google Scholar]
- 53.Hoaas H, Morseth B, Holland AE, Zanaboni P. Are Physical activity and Benefits Maintained After Long-Term Telerehabilitation in COPD? Int J Telerehabil 2016;8(2):39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Smith HS, Criner AJ, Fehrle D, Grabianowski CL, Jacobs MR, Criner GJ. Use of a SmartPhone/Tablet-Based Bidirectional Telemedicine Disease Management Program Facilitates Early Detection and Treatment of COPD Exacerbation Symptoms. Telemed J E Health 2016;22(5):395–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thomas RM, Locke ER, Woo DM, Nguyen EHK, Press VG, Layouni TA, et al. Inhaler Training Delivered by Internet-Based Home Videoconferencing Improves Technique and Quality of Life. Respir Care 2017;62(11):1412–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vitacca M, Rossin M, Assoni G, Baratti D, Zanardini M, Ruocco G, et al. Tele-assistance Respiratory card: feasibility of self-reporting in patients with severe COPD. Telemed J E Health 2013;19(2):99–103. [DOI] [PubMed] [Google Scholar]
- 57.Bryant J, McDonald VM, Boyes A, Sanson-Fisher R, Paul C, Melville J. Improving medication adherence in chronic obstructive pulmonary disease: a systematic review. Respir Res 2013;14(1):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bussell JK, Cha E, Grant YE, Schwartz DD, Young LA. Ways Health Care Providers Can Promote Better Medication Adherence. Clin Diabetes 2017;35(3):171–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guo SE, Bruce A. Improving understanding of and adherence to pulmonary rehabilitation in patients with COPD: a qualitative inquiry of patient and health professional perspectives. PLoS One 2014;9(10):e110835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maeder A, Poultney N, Morgan G, Lippiatt R. Patient Compliance in Home-Based Self-Care Telehealth Projects. J Telemed Telecare 2015;21(8):439–42. [DOI] [PubMed] [Google Scholar]
- 61.Chau JP, Lee DT, Yu DS, Chow AY, Yu WC, Chair SY, et al. A feasibility study to investigate the acceptability and potential effectiveness of a telecare service for older people with chronic obstructive pulmonary disease. Int J Med Inform 2012;81(10):674–82. [DOI] [PubMed] [Google Scholar]
- 62.Blasi F, Raddi F, Miravitlles M. Interactive Monitoring Service and COPD: Is it Possible to Reduce Nonadherence? COPD 2015;12(3):227–32. [DOI] [PubMed] [Google Scholar]
- 63.Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res 2015;17(2):e52. [DOI] [PMC free article] [PubMed] [Google Scholar]