Abstract
Rationale & Objective
Burnout decreases job satisfaction and leads to poor patient outcomes but remains underinvestigated in nephrology. We explored the prevalence and determinants of burnout among a sample of nephrologists.
Study Design
Cross-sectional.
Setting & Participants
The nephrologists were approached via the American Medical Association Physicians Masterfile, National Kidney Foundation listserv, email, and social media between April and August 2019. The predictors were demographics and practice characteristics. The outcome was burnout, defined as responding “once a week” or more on either 1 of the 2 validated measures of emotional exhaustion and depersonalization or both.
Analytical Approach
Participant characteristics were tabulated. Responses were compared using χ2 tests. Multivariable logistic regression was used to estimate the odds ratios (ORs) of burnout for risk factors. Free text responses were thematically analyzed.
Results
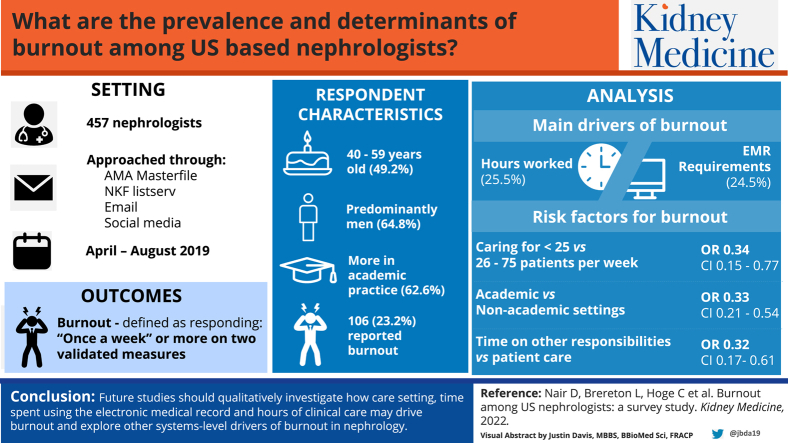
About half of 457 respondents were 40-59 years old (n=225; 49.2%), and the respondents were more predominantly men (n=296; 64.8%), US medical graduates (n=285; 62.4%), and in academic practice (n=286; 62.6%). Overall, 106 (23.2%) reported burnout. The most commonly reported primary drivers of burnout were the number of hours worked (n=27; 25.5%) and electronic health record requirements (n=26; 24.5%). Caring for ≤25 versus 26-75 patients per week (OR, 0.34; 95% confidence interval [95% CI], 0.15-0.77), practicing in academic versus nonacademic settings (OR, 0.33; 95% CI, 0.21-0.54), and spending time on other responsibilities versus patient care (OR, 0.32; 95% CI, 0.17-0.61) were each independently associated with nearly 70% lower odds of burnout after adjusting for age, sex, race, and international medical graduate status. The free text responses emphasized disinterested health care systems and dissatisfaction with remuneration as the drivers of burnout.
Limitations
Inability to precisely capture response rate.
Conclusions
Nearly one-quarter of the nephrologists in our sample reported burnout. Future studies should qualitatively investigate how the care setting, time spent on electronic medical records, and hours of clinical care drive burnout and explore other system-level drivers of burnout in nephrology.
Index Words: Burnout, depersonalization, emotional exhaustion, nephrology, survey
Graphical abstract
Plain-Language Summary.
Burnout remains underinvestigated in nephrology. We conducted a cross-sectional survey to explore the burden of and risk factors for burnout among nephrologists in the United States. Nearly one-quarter of the responding nephrologists reported burnout. Nephrologists who cared for fewer patients per week, practiced in academic settings, and primarily spent time on other responsibilities compared with that spent on patient care were much less likely to report burnout. The nephrologists also reported frustration with perceived lack of control over work, frustration with the time spent on electronic medical records, and not being able to cure patients as the sources of burnout.
Editorial, 100426
Burnout, a psychological syndrome in response to chronic, job-related stressors, is conceptualized as a combination of emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment.1 Investigating burnout in the US health care workforce remains of critical importance. Population-based cohort studies in the United States have supported that burnout is more prevalent among health care workers than among the general population (37.9% vs 27.8%, respectively).2 When unaddressed, burnout is associated with medical errors, interpersonal conflicts, mood disorders, substance abuse, suicidal ideation, and an estimated annual health care cost of $4.6 billion because of job turnover.3, 4, 5, 6 Thought leaders in nephrology have made urgent calls to assess and address burnout; yet, there is limited research examining and exploring its prevalence and determinants among practicing nephrologists.7, 8, 9 Thus, the most impactful drivers of burnout in nephrology remain unidentified, and targeted strategies to improve nephrologists’ personal well-being, maintain patient safety, increase job satisfaction, and enhance workforce recruitment remain underdeveloped.
The only prior investigation to examine burnout among practicing nephrologists in the United States assessed burnout using unvalidated measures.10 Recent evidence using validated measures has shown that burnout is prevalent among US nephrology trainees and practicing nephrologists in Poland.11,12 Given the threat of unaddressed burnout on nephrologists’ quality of life, capability to deliver optimal patient care, and ability to attract prospective applicants to the field, we aimed to explore the reported prevalence and determinants of burnout in a sample of practicing nephrologists in the United States and identify additional themes and issues via free text responses. We hypothesized that themes identified in free text responses would guide next steps and help outline targeted solutions.
Methods
We developed a 15-item, anonymous survey to explore the prevalence and determinants of burnout in a sample of practicing nephrologists in the United States. The survey was developed by members of the National Kidney Foundation (NKF) education committee, a group of nephrologists and scientists with expertise in survey-based research and implementation, educational outreach, and the promotion of evidence-based recommendations to support optimal kidney health. The key determinants of burnout germane to nephrology were selected based on a review of the literature, a group discussion within the committee, and the Job Demands–Resources model, a conceptual framework in psychology that posits that occupational stress occurs because of imbalances between demands on individuals and their access to resources to cope with those demands.13, 14, 15 The selected determinants included the number of hours worked per week, electronic medical record requirements, patient illness severity and medical complexity, and a decreased sense of autonomy (see Item S1 for survey instrument). The questions were pilot tested among the committee members. The survey took approximately 3 minutes to complete. Race categories were defined using National Institutes of Health criteria, and geographic location was defined using US Census Bureau criteria.16,17
Using Research Electronic Data Capture electronic survey database, emails with a survey link unique to the participant were sent up to 3 times to practicing US adult and pediatric nephrologists (including those with specialization in transplantation, interventional nephrology, critical care, or palliative care) who were a part of the American Medical Association Physicians Masterfile or the NKF listserv between April and August 2019.18,19 Each listserv contained unique emails of the participating nephrologists. Of 3,216 participants who received the first survey invitation from the American Medical Association, 322 opened the email and 112 clicked on the survey link. Of 2,892 participants who received the second survey invitation from the American Medical Association, 180 opened the email and 13 clicked on the survey link. Of 3,164 participants who received the third survey invitation, 396 opened the email and 45 clicked on the survey link. Of 901 and 906 participants who received an email invitation from the NKF, 50 and 37 clicked on the survey link, respectively. Additional public survey links were sent to individual colleagues in private practice and publicized via social media (Twitter). Survey participation was voluntary, and the participants were offered a discounted rate for NKF membership for 1 year upon survey completion. The survey was deemed exempt by institutional review boards at Vanderbilt University and Emory University (#190406 and #STUDY00000987, respectively). Informed consent was waived because of the information being deidentified. Links to resources for emotional well-being, such as the National Suicide Prevention Lifeline, were provided at survey completion. Funding was obtained from the NKF.
Burnout Measure
To facilitate survey completion and minimize participant burden, we used 2 validated, single-item measures of burnout adapted from the 22-item Maslach Burnout Inventory (MBI), which is considered the gold standard for burnout assessment.20 Our 2-item survey asked the participants to report, on a 7-point ordinal scale, how frequently they experienced emotional exhaustion (“‘burnout’ is defined as a combination of emotional exhaustion, depersonalization, and reduced personal accomplishment. Using this definition, how often do you feel burned out from your work as a nephrologist?”) and how frequently they had experienced depersonalization over the past year (“over the past year, how often have you felt callous toward people?”), with potential responses of “never,” “a few times a year or less,” “once a month or less,” “a few times a month,” “once a week,” “a few times a week,” or “every day.” Participants who selected “once a week” or more frequently as a response to either item were considered to be experiencing burnout. These question items have been validated against the full MBI, have been shown to have strong correlations with the full MBI (Spearman rho range, 0.61-0.83), and have been used in prior studies that measured burnout in health care professionals, including nephrology trainees.11,21,22
Quantitative Analyses
We used descriptive statistics as well as χ2 and Fisher exact tests to estimate the prevalence of burnout and compare categorical data and continuous variables based on burnout status. We used multivariable logistic regression analysis, with adjustment for age (<40, 40-59, and ≥60 years), sex (male vs female), race (White vs other), and international medical graduate status (yes vs no), to estimate the association of participant characteristics with burnout. We collapsed the race variable because of a limited number of non-White participants. Missing data were dropped (Table 1), and a complete case analysis was performed. A P value of <0.05 was considered statistically significant. Statistical analyses were performed using Stata, version 16 (StataCorp, College Station, TX), and SAS, version 9.4 (SAS, Cary, NC).
Table 1.
Self-Reported Demographic and Practice-Related Characteristics of Participants (N=457)
| Characteristic | Participants, N (%) |
|---|---|
| Age, y | |
| <40 | 136 (29.8) |
| 40-59 | 225 (49.2) |
| ≥60 | 94 (20.6) |
| Missing | 2 (0.4) |
| Sex | |
| Male | 296 (64.8) |
| Female | 154 (33.7) |
| Missing | 7 (1.5) |
| Racea | |
| Asian | 150 (32.8) |
| Black or African American | 15 (3.3) |
| White | 244 (53.4) |
| Other | 37 (8.1) |
| Missing | 11 (2.4) |
| Relationship statusb | |
| Married | 391 (85.6) |
| Other | 62 (13.6) |
| Missing | 4 (0.9) |
| Geographical region of practice | |
| Northeast or mid-Atlantic (CT, ME, MA, NH, RI, VT, NJ, NY, PA, DE, MD, DC) | 163 (35.7) |
| Midwest (IL, IN, MI, OH, WI, IA, KS, MN, MO, NE, ND, SD) | 64 (14.0) |
| South (FL, GA, NC, SC, VA, WV, AL, KY, MS, TN, AR, LA, OK, TX) | 131 (28.7) |
| West (AZ, CO, ID, MT, NV, NM, UT, WY, AK, CA, HI, OR, WA) | 82 (17.9) |
| Missing | 17 (3.7) |
| International medical graduate status | |
| Yes | 167 (36.5) |
| No | 285 (62.4) |
| Missing | 5 (1.1) |
| Years in practice | |
| 0-5 | 110 (24.1) |
| 6-20 | 219 (47.9) |
| >20 | 124 (27.1) |
| Missing | 4 (0.9) |
| Number of patients seen per wk | |
| ≤25 | 80 (17.5) |
| 26-75 | 217 (47.5) |
| >75 | 155 (33.9) |
| Missing | 5 (1.1) |
| Academic setting of practice | |
| Yes | 286 (62.6) |
| No | 167 (36.5) |
| Missing | 4 (0.9) |
| Occupies the majority of working time | |
| Patient care | 305 (66.7) |
| Other | 114 (25.0) |
| Missing | 38 (8.3) |
| Subject area(s) of practicea | |
| Pediatrics | 30 (6.7) |
| Transplantation | 173 (37.9) |
| Critical care | 198 (43.3) |
| Interventional nephrology | 22 (4.8) |
| Palliative care | 35 (7.7) |
| Dialysis | 362 (79.2) |
| Nondialysis kidney disease | 378 (82.7) |
| Missing | 20 (4.4) |
Abbreviations: AK, Alaska, AL, Alabama; AR, Arkansas; AZ, Arizona; CA, California; CO, Colorado; CT, Connecticut; DC, District of Columbia; DE, Delaware; FL, Florida; GA, Georgia; HI, Hawaii; IA, Iowa; ID, Idaho; IL, Illinois; IN, Indiana; KS, Kansas; KY, Kentucky; LA, Louisiana; MA, Massachusetts; MD, Maryland; ME, Maine; MI, Michigan; MN, Minnesota; MO, Missouri; MS, Mississippi; MT, Montana; NC, North Carolina; ND, North Dakota; NE, Nebraska; NH, New Hampshire; NJ, New Jersey; NM, New Mexico; NV, Nevada; NY, New York; OH, Ohio; OK, Oklahoma; OR, Oregon; PA, Pennsylvania; RI, Rhode Island; SC, South Carolina; SD, South Dakota; TN, Tennessee; TX, Texas; UT, Utah; VA, Virginia; VT, Vermont; WA, Washington; WI, Wisconsin; WV, West Virginia; WY, Wyoming.
Participants could select >1 answer.
No participants selected that they were widowed.
Qualitative Analyses
Two optional questions allowed for free text responses. These questions invited the respondents to elaborate on their choice of primary contributing factor to burnout and describe their experiences of (or satisfaction with) working as a nephrologist. We approached the free text responses with postpositivist framing using the qualitative content analysis.23 The approach outlined by Elo and Kyngäs24 was followed for preparing, organizing, and reporting the free text responses. Two researchers with expertise in qualitative methods (DN and LB) read through each response twice before choosing the unit of analysis (phrases or sentences). Using NVivo12 software (QSR International, Burlington, MA), LB grouped individual phrases and sentences into higher-order headings (codes). DN and LB reviewed the codes to develop more focused categories, quantify the frequency of the codes, and note themes. The codes often contributed to >1 category. The analysis was inductive in developing categories for felt causes of distress and deductive in applying these categories to the determinants of burnout identified using the Job Demands–Resources model and literature review.13
Results
Survey Participant Characteristics
Table 1 lists the demographic and practice-related characteristics of the participants. Of 462 nephrologists who responded, 461 answered at least 1 burnout-related question, and 457 answered both the burnout-related questions. Half of the participants were aged between 40 and 59 years (n=225; 49.2%); most were men (n=296; 64.8%), White (n=244; 53.4%), and married (n=391; 85.6%). Furthermore, most were US medical graduates (n=285; 62.4%) and practiced in academic settings (n=286; 62.6%); almost half cared for 26-75 patients per week (n=217; 47.5%).
Quantitative Results: Prevalence and Determinants of Burnout
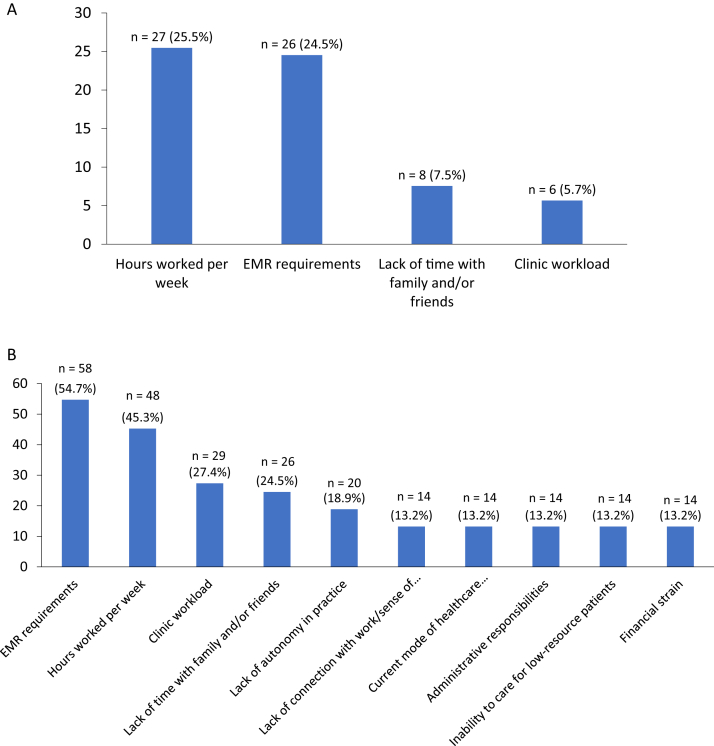
Overall, 106 (23.2%) participants reported burnout; 96 (21.0%) and 41 (9.0%) reported experiencing emotional exhaustion and depersonalization once a week or more, respectively, and 32 (7.0%) reported experiencing both emotional exhaustion and depersonalization once a week or more (Fig S1A and B; Item S2). Figure 1A shows the frequencies of reasons selected by the participants as the primary drivers of burnout, among those participants who met the criteria for burnout. The number of hours worked per week (n=27; 25.5%), electronic medical record requirements (n=26; 24.5%), lack of time with family and friends (n=8; 7.5%), and clinic workload (n=6; 5.7%) were the most frequently selected primary drivers of burnout. Figure 1B shows the frequencies of reasons selected by the participants as of 1 of the 3 top drivers of burnout. Electronic medical record requirements (n=58; 54.7%), the number of hours worked per week (n=48; 45.3%), clinic responsibilities (n=29; 27.4%), the lack of time with family and friends (n=26; 24.5%), a decreased sense of autonomy (n=20; 18.9%), lack of connection with work or lack of a sense of purpose (n=14; 13.2%), current mode of health care reimbursements (n=14; 13.2%), administrative responsibilities (n=14; 13.2%), the inability to care for low-resource patients (n=14; 13.2%), and financial strain (n=14; 13.2%) were most frequently reported.
Figure 1.
Frequencies of the most commonly reported drivers of burnout (among 106 participants who reported burnout, as defined by responding “once a week” or more frequently to either the question regarding emotional exhaustion or that regarding depersonalization). (A) Percentage of individuals reporting a reason as the primary driver of burnout. (B) Percentage of individuals reporting a reason being among the top 3 drivers of burnout. Abbreviation: EMR, electronic medical record.
Nephrologists who reported burnout were more likely than those without burnout to see >75 patients per week, practice in nonacademic settings, and spend majority of their time on direct patient care (Table 2). There were no significant differences in terms of demographics, relationship status, geographical region of practice, international medical graduate status, or years of practice. Table 3 shows unadjusted and adjusted odds ratios for associations between select provider- and practice-level characteristics and burnout. Caring for <25 versus 26-75 patients per week (odds ratio, 0.34; 95% confidence interval, 0.15-0.77), practicing in academic versus nonacademic settings (odds ratio, 0.33; 95% confidence interval, 0.21-0.54), and spending majority of time on other responsibilities versus patient care (odds ratio, 0.32; 95% confidence interval, 0.17-0.61) were each independently associated with nearly 70% lower odds of burnout after adjusting for age, sex, race, and international medical graduate status.
Table 2.
Characteristics of Participants by Burnout Status (N=457)
| Characteristic | Burnout Status, N (%)a |
Pb | |
|---|---|---|---|
| Yes | No | ||
| Total N | 106 (23.2) | 351 (76.8) | |
| Age, y | |||
| <40 | 29 (27.9) | 107 (30.5) | 0.43 |
| 40-59 | 57 (54.8) | 168 (47.9) | |
| ≥60 | 18 (17.3) | 76 (21.7) | |
| Sex | |||
| Male | 65 (61.9) | 231 (67.0) | 0.35 |
| Female | 40 (38.1) | 114 (33.0) | |
| Race | |||
| Asian | 31 (29.8) | 119 (34.8) | 0.77 |
| Black or African American | 4 (3.9) | 11 (3.2) | |
| White | 61 (58.7) | 183 (53.5) | |
| Other | 8 (7.8) | 29 (8.5) | |
| Relationship status | |||
| Married | 89 (84.8) | 302 (86.8) | 0.63 |
| Other | 16 (15.2) | 46 (13.2) | |
| Geographical region of practice | |||
| Northeast or mid-Atlantic (CT, ME, MA, NH, RI, VT, NJ, NY, PA, DE, MD, DC) | 36 (34.6) | 127 (37.8) | 0.74 |
| Midwest (IL, IN, MI, OH, WI, IA, KS, MN, MO, NE, ND, SD) | 13 (12.5) | 51 (15.2) | |
| South (FL, GA, NC, SC, VA, WV, AL, KY, MS, TN, AR, LA, OK, TX) | 33 (31.7) | 98 (29.2) | |
| West (AZ, CO, ID, MT, NV, NM, UT, WY, AK, CA, HI, OR, WA) | 22 (21.2) | 60 (17.9) | |
| International medical graduate status | |||
| Yes | 32 (30.5) | 135 (38.9) | 0.13 |
| No | 73 (69.5) | 212 (61.1) | |
| Years in practice | |||
| 0-5 | 23 (21.7) | 87 (25.1) | 0.44 |
| 6-20 | 57 (53.8) | 162 (46.7) | |
| >20 | 26 (24.5) | 98 (28.2) | |
| Number of patients seen per wk | |||
| ≤25 | 8 (7.6) | 72 (20.8) | <0.01 |
| 26-75 | 49 (46.7) | 168 (48.4) | |
| >75 | 48 (45.7) | 107 (30.8) | |
| Academic setting of practice | |||
| Yes | 49 (46.7) | 237 (68.1) | <0.01 |
| No | 56 (53.3) | 111 (31.9) | |
| Occupies the majority of working time | |||
| Patient care | 86 (85.2) | 219 (68.9) | <0.01 |
| Other | 15 (14.9) | 99 (31.1) | |
Abbreviations: AK, Alaska, AL, Alabama; AR, Arkansas; AZ, Arizona; CA, California; CO, Colorado; CT, Connecticut; DC, District of Columbia; DE, Delaware; FL, Florida; GA, Georgia; HI, Hawaii; IA, Iowa; ID, Idaho; IL, Illinois; IN, Indiana; KS, Kansas; KY, Kentucky; LA, Louisiana; MA, Massachusetts; MD, Maryland; ME, Maine; MI, Michigan; MN, Minnesota; MO, Missouri; MS, Mississippi; MT, Montana; NC, North Carolina; ND, North Dakota; NE, Nebraska; NH, New Hampshire; NJ, New Jersey; NM, New Mexico; NV, Nevada; NY, New York; OH, Ohio; OK, Oklahoma; OR, Oregon; PA, Pennsylvania; RI, Rhode Island; SC, South Carolina; SD, South Dakota; TN, Tennessee; TX, Texas; UT, Utah; VA, Virginia; VT, Vermont; WA, Washington; WI, Wisconsin; WV, West Virginia; WY, Wyoming.
Burnout is defined as responding “once a week” or more frequently to either the question regarding emotional exhaustion or that regarding depersonalization.
Using χ2 or Fisher exact test, as appropriate.
Table 3.
Associations of Select Participant Characteristics With Burnout (N=457)a
| Characteristic | Unadjusted OR (95% CI) | Adjusted OR (95% CI)b |
|---|---|---|
| Number of patients seen per wk | ||
| ≤25 | 0.38 (0.17-0.85) | 0.34 (0.15-0.77) |
| 26-75 | 1.00 (ref.) | 1.00 (ref.) |
| >75 | 1.54 (0.97-2.45) | 1.59 (0.98-2.58) |
| Academic setting of practice | ||
| Yes | 0.41 (0.26-0.64) | 0.33 (0.21-0.54) |
| No | 1.00 (ref.) | 1.00 (ref.) |
| Occupies majority of working time | ||
| Patient care | 1.00 (ref.) | 1.00 (ref.) |
| Other | 0.39 (0.21-0.70) | 0.32 (0.17-0.61) |
Abbreviations: CI, Confidence Interval; OR, odds ratio; ref, reference.
Burnout is defined as responding “once a week” or more frequently to either the question regarding emotional exhaustion or that regarding depersonalization.
Adjusted for age (<40, 40-59, and ≥60 years), sex (male vs. female), race (White vs other), and international medical graduate status (yes vs no).
Qualitative Results
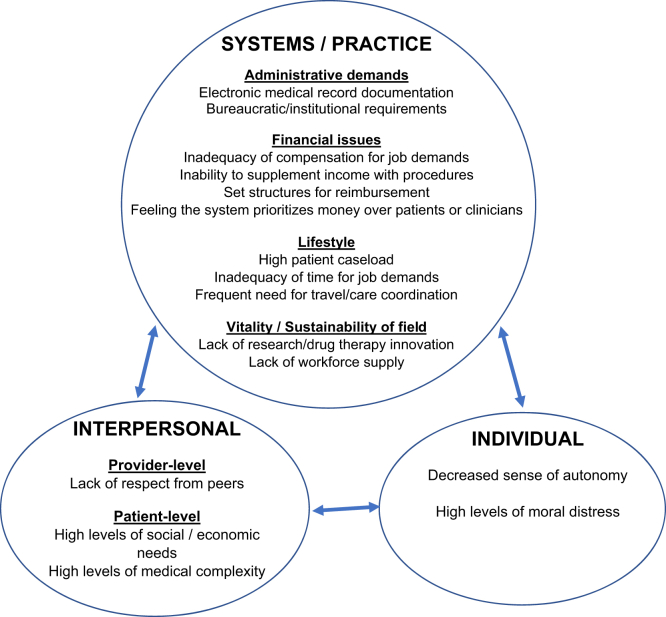
Of all the survey respondents, 144 (31.5%) participants provided free text responses. Themes were divided into individual, interpersonal, and system- or practice-level categories. The individual and interpersonal reasons for burnout included relationships with colleagues, challenges with accepting patients’ medical complexity, moral distress due to the inability to provide adequate care for patients with limited socioeconomic resources, and a need for a greater sense of autonomy related to work. The system-level themes included administrative demands, financial burdens, lifestyle intrusiveness, and concerns about innovation in the field. These themes and their interrelationships are illustrated in Fig 2, and exemplar quotes are highlighted below (Table 4; see Item S2 for the full data set).
Figure 2.
Conceptual framework of qualitative themes from free text responses.
Table 4.
Facilitator Source Levels, Qualitative Themes, and Quotes
| Theme | Example Quotes |
|---|---|
| Individual or interpersonal | |
| Felt inability to help patients: patients are too sick and their needs are too complex | “My patients are sick, even when they’re ‘well.’ The tools I have to test them with are often as toxic as the diseases, with flimsy evidence to support them.” - Male, age 50-59 y, academic nephrology “There is also a more recent surge in patient expectations that I respond directly to emails from them immediately for non-urgent questions (my nurses are happy to, but patients have started to expect it from the provider directly and often express frustration if they have to wait even more than a couple of hours for a response).” - Female, age 30-39 y, academic nephrology |
| Felt lack of appreciation | “I sense an overall lack of respect, less by my colleagues, more by patients/family members, and more egregiously from administrators…” - Male, age 60-69 y, academic nephrology “As an employed physician, I feel like I am paying for an administration who could care less if I am happy or not and would not really do anything to support me.” - Male, age 40-49 y, group multispecialty private practice “It’s a very hard field to practice, with no appreciation or feeling of fulfillment.” - Male, age 60-69 y, private practice |
| Systems or practice | |
| Too many tasks unrelated to patient care, electronic health record requirements | “Electronic records have pervaded my personal life and prevented [me] having full focus on the patient during clinic visits, which has contributed to my unhappiness with practicing medicine. Many of the tasks/clicks can be done by clinical support staff.” - Male, age 60-69 y, academic nephrology “It’s the continuous upgrades to the [electronic health record] and the continual accrual of physician ‘responsibilities’ for each patient encounter (ie, ‘Providers, this will just take a minute of your time!’). It’s workflow structured to maximize the ease of scheduling or the ease of quantifying productivity, with no consideration for the impact on the actual deliverer of care.” - Male, age 50-59 y, academic nephrology “The gap between the [electronic health record], requirements, and everything else [other facilitators of burnout listed in the survey] is huge.” - Male, age 70-79 y, private practice |
| Lack of autonomy caused by administrative bureaucracy | “It has become hard to do the ‘right things.’ There is too much bureaucracy. Physicians have no autonomy and are told how to work by administrators.” - Female, age 40-49 y, academic nephrology “Red tape [is not] allowing me to get authorizations for my patients to be sent to vascular surgeons.” - Female, age 40-49 y, private practice |
| United States health care system only cares about money | “There are other serious problems with current nephrology practice. The fact that we get paid more (or generate more relative value units) for putting a patient on dialysis (a ‘failure’) than for preventing [kidney disease] is a sad statement that is of a 1980s mentality.” - Male, age 60-69 y, academic nephrology |
| Concerns about vitality or sustainability of nephrology as a field | “I am concerned about the future of academic nephrology because the powers that be do not seem to realize the importance of facilitating research. We should do much more to fund research. Otherwise, young nephrologists will not pursue research.” - Male, age 60-69 y, academic nephrology “In terms of research progress, in addition to no new approaches to preventing/treating acute kidney injury and chronic kidney disease in over 50 years, we have worked hard over the past 30 years to ‘protect’ patients from contrast-induced nephropathy only to find out the entity may not really exist.” - Male, age 60-69 y, academic nephrology |
| Commercial dialysis company power | “My relationship with [the dialysis provider] is especially troubling because I am yoked to them by my medical director [with] non-competes, and they are manipulative.” - Male, age 60-69 y, group multispecialty private practice |
| Dissatisfaction with pay | “I felt compelled to decrease the number of patients I see per day to keep up with the current documentation requirements (it is not unusual to spend more time entering data then with the patient–so frustrating). Because my productivity has dropped, I have had to accept a significant reduction in my paycheck.” - Female, age 50-59 y, group multispecialty private practice “[It’s] better to be a hospitalist.” - Male, age 40-49 y, group multispecialty private practice |
Individual Reasons for Burnout: “It Has Become Hard to Do the Right Thing”
The individual reasons for burnout included a decreased sense of autonomy, frustration, and moral distress due to the inability to appropriately care for patients. One participant stated, “it has become hard to do the ‘right thing.’ There is too much bureaucracy. Physicians have no autonomy and are told how to work by administrators” (female, age 40-49 years, academic nephrology). Another reflected, “it is so rewarding to help patients and take care of them. This is what keeps us going. However, the loss of independence, respect, and the quality time with family due to increased burden from work that is not related to improving a patient’s health (like electronic medical record time, administrative work, etc) can cause damage to our profession. Taking autonomy away from physicians can kill innovation and creativity, which will be detrimental to healthcare eventually” (male, age 50-59 years, group multispecialty private practice).
The participants emphasized the complexity of care needed by patients with kidney disease (ie, physical, psychological, and social) and emphasized that although much of the coordination was left to nephrologists, limited appointment durations did not allow these issues to be adequately addressed. One participant noted, “complexity of patient illness and barriers to providing and receiving care, including medical (physical, psychological), social, financial, and support system (lack of). More and more, physicians are left to deal with all of these issues, but time given to address these issues continues to decrease” (female, age 40-49 years, group multispecialty private practice).
Interpersonal Reasons for Burnout: “I Sense an Overall Lack of Respect” and “My Patients are Sick, Even When They’re ‘Well’”
The participants described a decreased sense of respect, both from peers and their institutions as a whole. One participant expressed, “I sense an overall lack of respect, less by my colleagues, more by patients/family members, and more egregiously from administrators …. In addition the fact that we get paid more for putting a patient on dialysis (a ‘failure’) than for preventing end-stage renal disease is a sad statement” (male, age 60-69 years, academic nephrology).
Patient illness severity and complexity were cited as reasons for burnout, particularly when the respondents perceived the lack of recognition, support, and remuneration. The respondents emphasized the emotional burden of caring for severely ill patients. They referred to the physical toll that dialysis took on patients, as well as its noncurative nature, and the difficulties that some patients experienced in attempting to adhere to prescribed diets. One participant explained, “my patients are sick, even when they’re ‘well.’ The tools I have to [treat] them, which are often as toxic as [their] diseases … with flimsy evidence to support them” (male, age 50-59 years, academic nephrology).
System-Level Reasons for Burnout: “No One is Standing for Our Rights”
Most of the stated causes centered around system-level issues. Administrative tasks and demands and the burden of documentation in electronic medical records were frequently described and stated as frustrating by the respondents. One participant commented, “we became glorified internists. No one is standing for our rights. We run nursing home dialysis units, and [the Centers for Medicare & Medicaid Services] wants to apply ridiculous standards, with no common sense whatsoever. Enormous frustration” (male, age 50-59 years, group multispecialty private practice). Another expressed, “as an employed physician, I feel like I am paying for an administration who could care less if I am happy or not and would not really do anything to support me. Nephrology is dead as a profession …. comes down to how many visits per person on dialysis …. The dialysis portion of it is run by for-profit companies, which are publicly traded. Money for administrators, drug companies, dialysis companies, and insurance comes before patients” (male, age 40-49 years, group multispecialty private practice).
The participants also described frustrations with the inability to receive remuneration that was viewed as commensurate to their workload. Multiple comments referred to dissatisfaction with compensation, either by its own or in addition to other concerns. These comments referred to frustrations with dialysis provision being linked to Medicare payments and the inability to increase reimbursement through procedural interventions. One participant felt that from a financial perspective, it was “better to be a hospitalist.”
Other comments described concerns about commercial dialysis company power and their effect on practice. The respondents mentioned local monopolies or agreements between health care provider organizations and dialysis companies that limited locations for referrals. A few perceived the lack of cooperation by dialysis companies for patient-oriented research studies.
Multiple participants reported feeling that their employing organization, the wider US health care system, or both did not value them or the welfare of their patients. Some referred to payment structures that incentivized dialysis for kidney disease prevention. One participant stated, “we are the de facto primary care physicians for the patients …. The patients call us to go over every little change made by others or to get permission to start meds or undergo a test ordered by others. This is great—except we aren’t recognized for this work. You can’t bill for all those calls and emails” (male, age 40-49 years, private practice). Another participant commented, “there are other serious problems with current nephrology practice. The fact that we get paid more (or generate more RVUs) for putting a patient on dialysis (a ‘failure’) than for preventing ESRD is a sad statement that is of a 1980s mentality” (male, age 60-69 years, academic nephrology).
The participants lamented about their heavy clinical burden, which had resulted in decreased time for personal connections and with family. According to 1 participant, “nephrology has become a meat grinder. Our volumes are so high that, and I hate to say it, the last thing you want on a weekend is an interesting consult. I don’t have time to slow down and enjoy the medicine and personal connections anymore. There simply isn’t time to stop and think” (male, age 40-49 years, academic nephrology). Another participant had a similar perspective, “number of hours worked per week is linked with lack of time with family for me. I work a lot at home at night, so even though I’m ‘with my family,’ it reduces the amount of true quality time with them and time when I am truly present” (male, age 40-49 years, academic nephrology).
Finally, some respondents cited a perceived lack of research funding and innovation as the major sources of burnout. One participant observed, “it is becoming hard to continue productivity as a physician scientist as well as discharge responsibilities as a teacher and clinician in the academic setting. One major reason is the funding for research is so difficult either from the National Institutes of Health or from the Veterans Affairs Administration. I am concerned about the future of academic nephrology because the powers that be do not seem to realize the importance of facilitating research. We should do much more to fund research. Otherwise, young nephrologists will not pursue research” (male, age 60-69 years, academic nephrology). Another participant reflected, “these are among the many reasons trainees are not choosing nephrology … including too high a ratio of working hours: pay, lack of any new drug to prevent or improve acute kidney injury, the irreversibility of chronic kidney disease, the intensity duration of illness among dialysis patients (older and sicker). In terms of research progress, in addition to no new approaches to preventing/treating acute kidney injury and chronic kidney disease in over 50 years, we have worked hard over the past 30 years to ‘protect’ patients from contrast-induced nephropathy only to find out the entity may not really exist. Despite much research, progress in autosomal dominant polycystic kidney disease has been very slow and only produced a very expensive and potentially hepatotoxic therapy. Most of our therapies for glomerulonephritis are still way too toxic; so, patients can still die of the treatment. Hypertension guidelines are ridiculously numerous, constantly changing, and needlessly overcomplicated. Again, more ‘credit’ or payment for managing end-stage renal disease than thinking and being innovative in clinic is not a good system” (male, age 60-69 years, academic nephrology).
Respondents who used the free text questions to comment on the positive aspects of their work supported these facilitating factors in reverse. For example, those who described satisfaction with their schedule mentioned having control over the time spent on various aspects of work, including time for academic research, patient care, and teaching. They mentioned feeling appreciated by their employing organization and their colleagues, gratification because of the care they provided to their patients, and passion for intellectual aspects of the field.
Discussion
To our knowledge, this is the first study to explore the prevalence and potential drivers of burnout among practicing US nephrologists using validated instruments and the qualitative content analysis. Nearly one-quarter of the US nephrologists in our sample reported burnout. The quantitative and qualitative results demonstrated that administrative demands and clinical workload were strong drivers of burnout. Caring for fewer patients per week and practicing in academic settings were each independently associated with substantially lower (nearly 70%) odds of experiencing burnout.
Given the differences in instruments used to measure burnout among other health care professionals, it is difficult to compare the prevalence estimated among nephrologists in our sample with these estimates in other subspecialists, which range from 0% to 80%.25 Our results showed a prevalence of emotional exhaustion among US nephrologists in practice comparable with the prevalence of emotional exhaustion among nephrology trainees (23% and 30%, respectively).11
Our results did not demonstrate statistically significant associations between race and burnout in the multivariable analyses. In a cross-sectional analysis of 4,424 primary care and subspecialty physicians in the United States, burnout was more prevalent among those who self-identified as White, although the investigators extrapolated that this might have been the result of hesitancy of non-White physicians to report burnout.26 The small number of Black nephrologists in our sample limits the ability to capture differences in burnout by race or draw any conclusions related to this group.
Similarly, we did not find a statistically significant association between sex and burnout. In a cross-sectional analysis of 3,603 US primary care and subspecialty physicians, females reported a significantly higher prevalence of burnout compared with males.27 Similar results have been demonstrated in other studies.28 Because our respondents were predominantly male, the data might have been underpowered to detect statistically significant differences in burnout by sex, although it is also plausible that burnout is not differentially affected by sex in nephrology. There is mixed evidence regarding associations between age and burnout. Most studies have reported higher levels of burnout among younger-to-middle-aged physicians, but evidence from some surgical subspecialty fields indicates that older age is independently associated with burnout.29,30
In the quantitative analyses, electronic medical record requirements, the number of hours worked per week, the lack of time with family and friends, and clinic requirements were most frequently selected as the primary drivers of burnout. Caring for ≤25 versus 26-75 patients per week and practicing in academic versus nonacademic settings were each significantly associated with nearly 70% lower odds of burnout after adjusting for age, sex, race, and international medical graduate status. Increasing work requirements can deplete individuals’ capacity to meet other job-related demands and diminish their time spent with loved ones. Our results echo those of similar analyses among surgical subspecialists, advance practice nurses, and general internists, which also pointed toward clinical work hours and electronic medical record requirements as the determinants of burnout.31,32 Although burnout was not explicitly mentioned in an earlier analysis among medical students and residents, the respondents stated high clinical workload and poor work–life balance as deterrents to pursuing a nephrology fellowship. Thus, mitigating factors associated with burnout, such as clinical work hours during training, might be key to attracting prospective applicants to nephrology.33
In the qualitative analyses, the participants reported frustration with decreased financial remuneration, perceived decline in research innovation, and moral distress as the drivers of burnout. Although the perceived lack of research innovation has not been routinely demonstrated as a determinant of burnout in other specialties, perceptions of a decreased earning potential and the lack of research innovation in nephrology have previously been demonstrated in survey analyses among internal medicine trainees.34 Furthermore, educational debt has been shown to be a driver of trainee burnout.35 Given that kidney disease disproportionately affects those with limited social and economic resources in the United States, it is perhaps not surprising that the inability to provide care for those with a lack of resources, which may cause moral distress, emerged as a determinant of burnout in our sample.36,37 Moral distress has been demonstrated in nephrology as well as in an analysis of health care workers involved in caring for patients with hematopoietic stem cell transplants, and it might be possible that the medical complexity and resource needs of patients with stem cell transplants mirror those of patients with kidney disease.15,38 Compensating nephrologists in practice for the time spent at research conferences, involving nephrologists in health system-level decisions related to quality metrics and ways to align pay with performance, advocating for new payment models, developing and implementing models of care delivery that allow for concurrent hospice and dialysis services, and expanding Medicaid to cover dialysis for undocumented immigrants may be the requisite next steps to begin to address these issues.39,40
Institutional and organizational frameworks, including those of the National Academy of Medicine, outline multilevel strategies to reduce burnout in the general health care workforce. These frameworks involve reducing and/or redistributing workload, increasing the frequency of and opportunities for rewards, fostering community-building activities, ensuring equity in decision making and resource distribution, aligning organizational missions with employee values, and restoring an overall sense of control and purpose.41,42 The most robust evidence for interventions to reduce burnout has arisen from institutional, system-wide policies and culture changes, as opposed to personal coaching and resilience training. These include open forums for discussions between peers and institutional leaders, work hour modifications, physician extenders, career-coaching programs, and involving stakeholders in the development of electronic medical record changes and quality metrics.43,44
Our study has important limitations. Our sampling strategy to improve our sample size made it impossible to precisely capture the response rate. Our respondents were predominantly middle-aged, men, White, and married and had been in practice for 6-20 years. These specific demographics are not fully representative of the demographic makeup of the current nephrology workforce; as an example, our study was enriched with academic nephrologists.45 Only those determinants of burnout that were specified in our survey could be selected by the participants, although the free text responses helped mitigate this bias. Furthermore, only those participants who were already experiencing burnout might have chosen to respond to the survey, resulting in a selection bias. Although the 2-item MBI survey has been shown to produce the same results as the full 22-item survey, it asks only about emotional exhaustion and depersonalization. In the free text responses, many participants expressed their inability to achieve what they desired because of the lack of control over various situations and processes. This “lack of personal achievement” is the third component included in the original conceptualization of burnout by Maslach et al.1 As such, the 2-item MBI survey might not have captured the full spectrum of burnout experienced by our sample, resulting in a response bias. Further qualitative work is needed to more deeply explore the full spectrum of burnout. A sizable percentage of participants reported experiencing emotional exhaustion and depersonalization “a few times a month” (18% and 11%, respectively). Although these participants did not qualify as reporting burnout based on the validated definitions, these frequencies of emotional exhaustion and depersonalization might still signify meaningful intrusion on work–life satisfaction. Because the survey preceded the coronavirus disease 2019 pandemic, our estimate of burnout might underestimate its current prevalence in the postpandemic era. Furthermore, this survey preceded the publication of transformative clinical trials and widespread, equity-related changes in nephrology practice that may now affect the participants’ reported perceptions of innovation in the field.46,47
Regardless of the quantitative prevalence of burnout reported in this sample, the themes emphasized that the free text responses still highlighted that some practicing nephrologists face significant hindrances to their overall emotional well-being and job satisfaction. To pursue further analyses in this timely area, joint society-based databases are needed to systematically gather nephrologist-reported data, precisely determine the prevalence of burnout, comprehensively identify the demographics and practice patterns associated with burnout, and qualitatively interview individuals to rigorously explore the drivers of burnout. Nephrologists across diverse areas of practice, particularly those who practice in the community and may care for a large number of patients per week, must be included in the development of solutions. Nearly 1 in 4 nephrologists in our sample reported experiencing burnout, and nearly all emphasized the need for a widespread, system-level change. Now is the time to take the next steps to ultimately deliver stakeholder-developed, institutional, and organizational solutions to reduce burnout and increase job satisfaction in nephrology.
Article Information
National Kidney Foundation Education Committee Members
S. Soman, B. Jaar, K. Abdel-Kader, D. Adey, V. Agrawal, K. Beers, K. Cavanaugh, M.J. Choi, C.J. Diamantidis, M. Estrella, R. Greer, N. Krishnan, D. Nair, L. Plantinga, J. Schell, J. Simon, and J. Sperati.
Authors’ Full Names and Academic Degrees
Devika Nair, MD, MSCI, Laura Brereton, MSc, Courtney Hoge, MSPH, Laura C. Plantinga, PhD, Varun Agrawal, MD, Sandeep S. Soman, MD, Michael J. Choi, MD, and Bernard G. Jaar, MD, MPH, on behalf of the National Kidney Foundation Education Committee.
Authors’ Contributions
Research idea and study design: DN, LB, LCP, VA, SSS, MJC, BGJ; data acquisition: DN, LB, BGJ; data analysis/interpretation: DN, LB, CH, LCP, BGJ; statistical analysis: DN, LB, CH, LCP. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
This study was funded by the National Kidney Foundation Education Committee Project. The funders of this study had no role in the study design, data collection, data analysis or interpretation, writing of the report, or the decision to submit the report for publication.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Peer Review
Received June 18, 2021. Evaluated by 3 external peer reviewers, with direct editorial input from the Statistical Editor and the Editor-in-Chief. Accepted in revised form November 14, 2021.
Footnotes
Complete author and article information provided before references.
Complete author and article information (including a list of the members of the National Kidney Foundation Education Committee) provided before references.
Figure S1: Reported frequencies of (A) emotional exhaustion and (B) depersonalization among 457 respondents.
Item S1: Survey instrument.
Item S2: Data set.
Contributor Information
Bernard G. Jaar, Email: bjaar@jhmi.edu.
National Kidney Foundation Education Committee:
S. Soman, B. Jaar, K. Abdel-Kader, D. Adey, V. Agrawal, K. Beers, K. Cavanaugh, M.J. Choi, C.J. Diamantidis, M. Estrella, R. Greer, N. Krishnan, D. Nair, L. Plantinga, J. Schell, J. Simon, and J. Sperati
Supplementary Material
Figure S1; Item S1
Item S2.
References
- 1.Maslach C., Schaufeli W.B., Leiter M.P. Job burnout. Annu Rev Psychol. 2001;52(1):397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 2.Shanafelt T.D., Boone S., Tan L., et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 3.Tawfik D.S., Scheid A., Profit J., et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann Intern Med. 2019;171(8):555–567. doi: 10.7326/M19-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oreskovich M.R., Kaups K.L., Balch C.M., et al. Prevalence of alcohol use disorders among American surgeons. Arch Surg. 2012;147(2):168–174. doi: 10.1001/archsurg.2011.1481. [DOI] [PubMed] [Google Scholar]
- 5.Garcia C.D., Abreu L.C., Ramos J.L., et al. Influence of burnout on patient safety: systematic review and meta-analysis. Medicina. 2019;55(9):553. doi: 10.3390/medicina55090553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Han S., Shanafelt T.D., Sinsky C.A., et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784–790. doi: 10.7326/M18-1422. [DOI] [PubMed] [Google Scholar]
- 7.de Boer I.H. Nephrology at a crossroads. Clin J Am Soc Nephrol. 2018;13(2):324. doi: 10.2215/CJN.09070817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams A.W. Addressing physician burnout: nephrologists, how safe are we? Clin J Am Soc Nephrol. 2018;13(2):325–327. doi: 10.2215/CJN.06800617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roberts J.K. Burnout in nephrology: implications on recruitment and the workforce. Clin J Am Soc Nephrol. 2018;13(2):328–330. doi: 10.2215/CJN.09870917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin K.L. Medscape nephrologist lifestyle, happiness and burnout report 2020. Medscape; 2020. https://www.medscape.com/slideshow/2020-lifestyle-nephrologist-6012499#1
- 11.Agrawal V., Plantinga L., Abdel-kader K.A., et al. Burnout and emotional well-being among nephrology fellows: a national online survey. J Am Soc Nephrol. 2020;31(4):675–685. doi: 10.1681/ASN.2019070715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pawlowicz E., Nowicki M. Burnout syndrome among nephrologists—a burning issue—results of the countrywide survey by the Polish Society of Nephrology. BMC Nephrol. 2020;21(1):177. doi: 10.1186/s12882-020-01829-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bakker A.B., Demerouti E. The job demands-resources model: state of the art. J Manag Psychol. 2007;22(3):309–328. [Google Scholar]
- 14.Kroth P.J., Morioka-Douglas N., Veres S., et al. Association of electronic health record design and use factors with clinician stress and burnout. JAMA Network Open. 2019;2(8) doi: 10.1001/jamanetworkopen.2019.9609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ducharlet K., Philip J., Gock H., et al. Moral distress in nephrology: perceived barriers to ethical clinical care. Am J Kidney Dis. 2020;76(2):248–254. doi: 10.1053/j.ajkd.2019.09.018. [DOI] [PubMed] [Google Scholar]
- 16.Racial and ethnic categories and definitions for NIH diversity programs and for other reporting purposes. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/grants-and-training/funding-opportunities-and-contacts/all-funding-opportunity-announcements/racial
- 17.Statistical groupings of states and counties. United States Census Bureau. https://www2.census.gov/geo/pdfs/reference/GARM/Ch6GARM.pdf
- 18.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research Electronic Data Capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Medical marketing lists. Medical Marketing Service Inc. https://www.mmslists.com Accessed April 19, 2019.
- 20.Maslach C., Jackson S.E., Leiter M.P. In: Evaluating Stress: A Book of Resources. Zalaquett C.P., Wood R.J., editors. The Scarecrow Press; 1996. Maslach burnout inventory manual; pp. 191–218. [Google Scholar]
- 21.West C.P., Dyrbye L.N., Satele D.V., Sloan J.A., Shanafelt T.D. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27(11):1445–1452. doi: 10.1007/s11606-012-2015-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.West C.P., Dyrbye L.N., Sloan J.A., Shanafelt T.D. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24(12):1318–1321. doi: 10.1007/s11606-009-1129-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sandelowski M. What’s in a name? Qualitative description revisited. Res Nurs Health. 2010;33(1):77–84. doi: 10.1002/nur.20362. [DOI] [PubMed] [Google Scholar]
- 24.Elo S., Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 25.Rotenstein L.S., Torre M., Ramos M.A., et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320(11):1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garcia L.C., Shanafelt T.D., West C.P., et al. Burnout, depression, career satisfaction, and work-life integration by physician race/ethnicity. JAMA Netw Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.12762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chesak S.S., Cutshall S., Anderson A., Pulos B., Moeschler S., Bhagra A. Burnout among women physicians: a call to action. Curr Cardiol Rep. 2020;22(7):1–9. doi: 10.1007/s11886-020-01300-6. [DOI] [PubMed] [Google Scholar]
- 28.Obregon M., Luo J., Shelton J., Blevins T., MacDowell M. Assessment of burnout in medical students using the Maslach burnout inventory-student survey: a cross-sectional data analysis. BMC Med Educ. 2020;20(1):1–10. doi: 10.1186/s12909-020-02274-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kinslow K., Sutherland M., Mckenney M., Elkbuli A. Reported burnout among US general surgery residents: a surgery of the association of program directors in surgery members. Ann Med Surg. 2020;60:14–19. doi: 10.1016/j.amsu.2020.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou A.Y., Panagioti M., Esmail A., Agius R., Van Tongeren M., Bower P. Factors associated with burnout and stress in trainee physicians: a systematic review and meta-analysis. JAMA Netw Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.13761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coleman D.M., Money S.R., Meltzer A.J., et al. Vascular surgeon wellness and burnout: a report from the SVS Wellness Task Force. J Vasc Surg. 2021;73(6):1841–1850. doi: 10.1016/j.jvs.2020.10.065. [DOI] [PubMed] [Google Scholar]
- 32.Dyrbye L.N., West C.P., Kelsey E.A., Gossard A.A., Satele D., Shanafelt T. A national study of personal accomplishment, burnout, and satisfaction with work-life integration among advance practice nurses relative to other workers. J Am Assoc Nurse Pract. 2020;33(11):896–906. doi: 10.1097/JXX.0000000000000517. [DOI] [PubMed] [Google Scholar]
- 33.Nair D., Pivert K.A., Baudy A., Thakar C.V. Perceptions of nephrology among medical students and internal medicine residents: a national survey among institutions with nephrology exposure. BMC Nephrol. 2019;20(1):1–11. doi: 10.1186/s12882-019-1289-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McPeek-Hinz E., Boazak M., Sexton J.B., et al. Clinician burnout associated with sex, clinician type, work culture, and use of electronic health records. JAMA Netw Open. 2021;4(4) doi: 10.1001/jamanetworkopen.2021.5686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.West C.P., Shanafelt T.D., Kolars J.C. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306(9):952–960. doi: 10.1001/jama.2011.1247. [DOI] [PubMed] [Google Scholar]
- 36.Jameton A. Prentice-Hall; 1984. Nursing Practice: The Ethical Issues. [Google Scholar]
- 37.Norris K.C., Nissenson A.R. Race, gender, and socioeconomic disparities in CKD in the United States. J Am Soc Nephrol. 2008;19(7):1261–1270. doi: 10.1681/ASN.2008030276. [DOI] [PubMed] [Google Scholar]
- 38.Neumann J.L., Mau L.W., Virani S., et al. Burnout, moral distress, work-life balance, and career satisfaction among hematopoietic cell transplantation professionals. Bio Blood Marrow Transplant. 2018;24(4):849–860. doi: 10.1016/j.bbmt.2017.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schell J.O., Johnson D.S. Challenges with providing hospice care for patients undergoing long-term dialysis. Clin J Am Soc Nephrol. 2021;16(3):473–475. doi: 10.2215/CJN.10710720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rizzolo K., Novick T.K., Cervantes L. Dialysis care for undocumented immigrants with kidney failure in the COVID-19 era: public health implications and policy recommendations. Am J Kidney Dis. 2020;76(2):255–257. doi: 10.1053/j.ajkd.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Factors affecting clinician well-being and resilience: conceptual model. National Academy of Medicine. https://nam.edu/clinicianwellbeing/resources/factors-affecting-clinician-well-being-and-resilience-conceptual-model/
- 42.Shanafelt T.D., Noseworthy J.H. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129–146. doi: 10.1016/j.mayocp.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 43.West C.P., Dyrbye L.N., Erwin P.J., Shanafelt T.D. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 44.Robinson K.E., Kersey J.A. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Med (Baltim) 2018;97(38) doi: 10.1097/MD.0000000000012319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.The US adult nephrology workforce: developments and trends. The American Society of Nephrology. https://www.asn-online.org/education/training/workforce/Nephrology_Workforce_Study_Report_2016.pdf
- 46.Perkovic V., Jardine M.J., Neal B., et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–2306. doi: 10.1056/NEJMoa1811744. [DOI] [PubMed] [Google Scholar]
- 47.Inker L.A., Eneanya N.D., Coresh J., et al. New creatinine and cystatin C-based equations to estimate GFR without race. N Engl J Med. 2021;385(19):1737–1749. doi: 10.1056/NEJMoa2102953. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1; Item S1
Item S2.