Abstract
Background and objectives
Hydatid disease of the lung, caused by Echinococcus granulosus, is an unusual parasitic disease. The aim of the current review for managing pulmonary hydatid cysts by uniportal video-assisted thoracoscopic surgery (u-VATS), and their complications, the size of hydatid cyst, length of hospital stay, surgery time, the rate of conversion from u-VATS to thoracotomy or mini-thoracotomy, follow-up, and outcomes.
Methods
We conduct the platform searches on the PubMed and Google Scholar electronic databases from inception to January 20, 2022, among patients diagnosed with pulmonary hydatid cyst (PHC) who underwent the u-VATS approach.
Results
This systematic review comprised five studies reporting 85 cases of PHC underwent (u-VATS) approach. Most patients were adults. The most common location of pulmonary hydatid cyst was the right lower lobe followed by the left lower lobe. The average size of PHC was 8.41 cm in all studies. The length of hospital stay was 3.85 days. The duration of operation time based on the means of the included studies was 86.19 min for each patient. Furthermore, the overall complication occurred in 9.35% of patients (n = 11) from 85 cases. The most complication was emphysema and prolonged air leak. The recurrence of pulmonary hydatid cyst did not occur in all studies.
Conclusion
The feasibility of the video-assisted thoracoscopic surgery (VATS) approach has been proven globally in terms of reducing the overall complication, shorter chest tube duration, shorter surgery time, reduce postoperative pain, shorter chest tube duration, lower chest tube drainage, and less required to pain killers postoperatively.
Keywords: Uniportal VATS, Single port VATS, Hydatid cyst, Single incision, Pulmonary, Minimally invasive surgery
Highlights
-
•
This systematic review comprised five studies reporting 85 cases of pulmonary hydatid cyst underwent (u-VATS) approach.
-
•
The median surgery time was 86.19 min and complications rate were 9.35%.
-
•
Uniportal video-assisted thoracoscopic surgery (u-VATS) is simple, safe and feasible for removal of pulmonary hydatid cysts.
1. Introduction
Hydatid disease of the lung, caused by Echinococcus granulosus, is an unusual parasitic disease observed most commonly in sheep and cattle-raising regions around the world, most notably in Australia, South Africa, New Zealand, South America, and the Mediterranean countries of Africa, Asia and Europe [1,2].
The liver is most affected (75%), then the lungs (20%), and other organs are affected at varying frequencies [3]. The single organ involvement occurs in 85–90% of cases, with a single cyst shown in 70% of cases [4].
The gold standard treatment of pulmonary hydatid cysts is surgical intervention. Parenchymal sparing surgery can be performed without the need for resection of lung tissue in most cases, but segmentectomy, lobectomy, or wedge resection should be considered, for example, for adherent cysts [[5], [6], [7], [8], [9]].
There has been an important revival in thoracoscopic surgery over the last two decades. Numerous papers have been published that describe performing complex operations using the uniportal VATS method via the intercostal and subxiphoid strategies [[10], [11], [12], [13], [14]]. We discovered only a few publications in the literate describing the method of uniportal VATS as a surgical treatment for pulmonary hydatid cysts [[15], [16], [17], [18], [19]]. The uniportal thoracoscopic technique requires only one skin incision and does not require the use of a rib separator. The incision is varying between 2 and 8 cm long [6]. The uniportal video-assisted thoracoscopic surgery (u-VATS) has superiority to thoracotomy in terms of reduced complications, shorter hospitalization, and surgery time was also shorter in the u-VATS group.
The present paper aims to review published articles related to the management of pulmonary hydatid cysts using uniportal video-assisted thoracoscopic surgery (u-VATS) and the benefits of this approach compared thoracotomy method.
2. Methods
2.1. Review objectives
The aim of the current systematic review for managing pulmonary hydatid cysts by uniportal video-assisted thoracoscopic surgery (u-VATS), and how many cases underwent the u-VATS approach worldwide for removal of pulmonary hydatid cyst and their complications, the size of hydatid cyst, length of hospital stay, surgery time, the rate of conversion from u-VATS to thoracotomy or mini-thoracotomy, follow-up and outcomes.
2.2. Protocol of the study
The work has been reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 criteria [20]. This study was also assessed using the AMSTAR-2 checklist, which determined that it was to be a high-quality review [21]. Ethical approval was not required for this review article.
2.3. Search strategy
A comprehensive search was conducted on major electronic databases (PubMed and google scholar) to obtain all publications on January 20, 2022. The search was conducted using the following keywords ("uniportal video-assisted thoracoscopic surgery" OR “minimally invasive" OR "UVATS" OR "single port VATS" AND " pulmonary hydatid cyst") Filters: (English, Humans) as shown in (Supplementary material 1) for detailed search strategy. The references of eligible papers were also screened to ensure that the search was comprehensive.
2.4. Eligibility criteria
Studies that reported on a human patient, diagnosed with pulmonary hydatid cyst, and underwent uniportal video-assisted thoracoscopic surgery (u-VATS) were included in this review. Narrative studies or systematic reviews, opinions, congress abstracts, meta-analyses, full-text unavailability, or editorials were excluded. Furthermore, patients who underwent (two, three, or four ports using video-assisted thoracoscopic surgery (VATS), patients who underwent thoracotomy and mini-thoracotomy for removal of pulmonary hydatid cysts were also excluded. Moreover, articles other than English were excluded in this review, and no date limitations were placed.
2.5. Data extraction and selection process
All steps of data extraction were conducted following PRISMA 2020 guidelines. The two independent authors (SKA and DHB) used the Rayyan website to screen abstract and full text-published articles based on inclusion and exclusion criteria [22]. Discrepancies between the two independent authors were resolved by the second author (RAE). Data were extracted and entered into a standardized form created in Microsoft Excel to collect the necessary information. The following data were extracted from each study: author names, year of publication, sample size, methods of study, the age of patients, location of pulmonary hydatid cyst, Diameter of Cyst (cm), the duration of hospital stays, conversion to complete thoracotomy or mini-thoracotomy, surgery time/min, complications, follow up and outcome.
2.6. Critical appraisal
We used the Joanna Briggs Institute's critical appraisal tool for non-randomized control studies and case reports to evaluate the quality of all included studies [23]. The evaluation was performed by two independent authors (SKA and DHB) for each article. Disagreements among authors about the evaluation of the paper were resolved through discussion or resolved by the second author (RAE). Articles with an average score of 50% or higher were included in the data extraction. Additionally, AMSTAR 2 criteria were used to rate the quality of our systematic review [21]. According to the Assessment of Multiple Systematic Reviews 2 (AMSTAR 2) tool, the quality of our systematic review is “Medium”.
2.7. Data synthesis and analysis
The data of the current systematic review was extracted and pooled from all included articles. The data collected and reported included (author names, year of publication, sample size, methods of study, age of patients, location of pulmonary hydatid cyst, Diameter of Cyst (cm), the duration of hospital stays, conversion to complete thoracotomy or mini-thoracotomy, surgery time/min, complications, follow-up, and outcome). We extracted the data based on eligibility studies. Furthermore, all patients diagnosed with pulmonary hydatid cyst and undergone uniportal video-assisted thoracoscopic surgery (u-VATS) were reported.
3. Results
3.1. Selection of studies
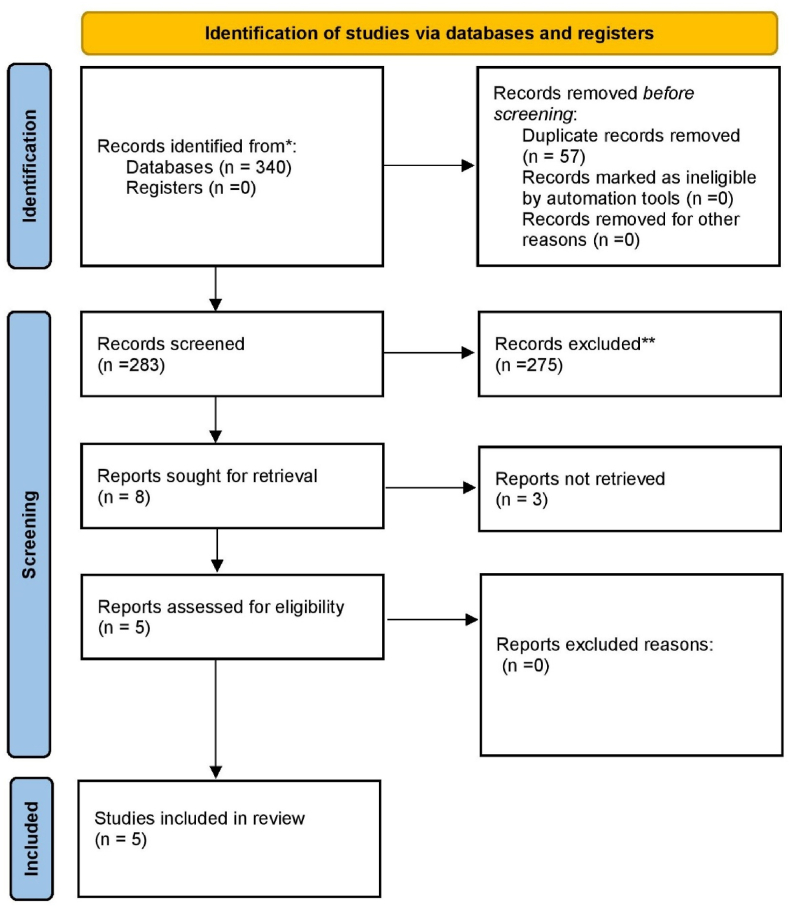
A comprehensive search was conducted on January 20.2022 from the major databases (PubMed, Google scholar) and we found 340 relevant published articles. Then, the references were transferred to the citation manager tool (Mendeley) and 57 articles were automated removed due to duplication. Then, 283 articles were screened for title, abstract and full text, and 275 articles were excluded based on inclusion criteria. Furthermore, 8 articles sought to be retrieval but 3 articles were excluded due to our inclusion criteria. Finally, 5 articles remained for the current systematic review (Fig. 1).
Fig. 1.
Prisma follow diagram.
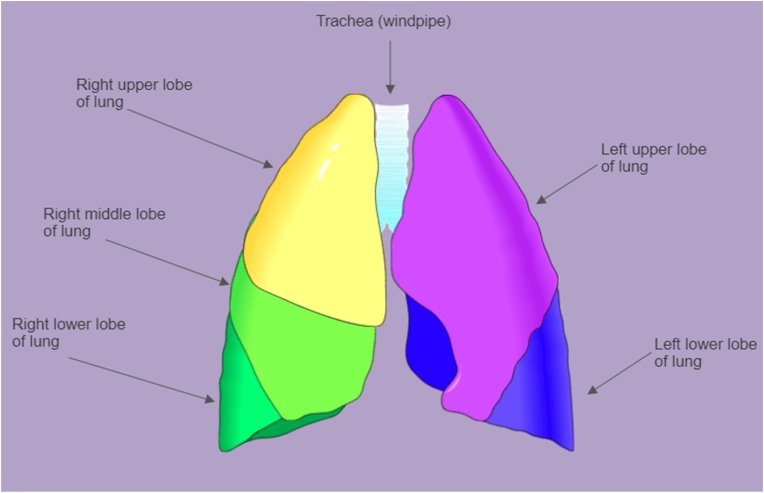
3.2. Characteristics of the included studies
Overall, the five studies including 85 cases participated in this systematic review; 23 cases from Palestine [15], and 62 cases from Turkey [[16], [17], [18], [19]]. All patients were diagnosed with pulmonary hydatid cysts and underwent uniportal video-assisted thoracoscopic surgery. Most patients were adults. The most common location of pulmonary hydatid cyst was the right lower lobe followed by the left lower lobe (Fig. 2). The average size of pulmonary hydatid cyst was 8.41 cm in all studies and the largest cyst were removed by uniportal video-assisted thoracoscopic surgery was 15.6 cm. The length of hospital stay was 3.85 days. In Cenk batla's 2019 study, the u-VATS approach was converted to mini-thoracotomy in 3 of 20 cases, and the second port incision was required in 6 cases to control air leaks adequately, and the same author conducted another study in 2020 in this study the u-VATS approach was converted to mini-thoracotomy in 4 cases, and in 8 cases the surgery was required to the second camera port.
Fig. 2.
Surface anatomy of lungs with lobes indicated by differing colors. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
However, the duration of operation time based on the means of the included studies was 86.19 min for each patient. Furthermore, the overall complication occurred in 9.35% of patients undergone u-VATS approach for pulmonary hydatid cyst (n = 11) from 85 cases, emphysema occurred in 3 cases, Atelectasis in 2 cases, failure of lung expansion in 1 case, a prolonged air leak in 1 case and wound infection occurred in 1 case, but three cases in the Cenk Balta et al., 2020 study unreported which type of complication occurred. Finally, the follow-up of patients who underwent uiportal video assisted-thoracoscopic surgery (u-VATS) ranged from 1 month to 22 months, and the recurrence of pulmonary hydatid cyst does not occur in all studies (Table 1).
Table 1.
Characteristics of included studies.
| Author/Year of publication | Sample size | Methods | Age Mean |
Location of cyst | Diameter of Cyst (cm) | Hospital Stay (MeanDays) |
Conversion to mini thoracotomy or complete thoracotomy | Complications | Surgery time/min | Follow up/months | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Abu akar et al., 2019 [15] | N = 23 | Retrospective Comparative cohort study | Mean age 31.39 years | The most common location was right lower lobe followed by left lower lobe | Average size of cysts was 5.78 cm | 3.65 days in average | NA | Complication occurred in n = 3 (13%) patients, the most common complication was emphysema | Mean 84 min (range, 25–210 min) | nor 30-day mortality recorded | No recurrence |
| Ocakcioglu et al., 2018 [19] | N = 18 | Retrospective Comparative study | Mean (SD) 25.86 ± 9.42 years |
NA | 7.07 ± 3.73 cm | (4.07 ± 0.73) days | All thoracoscopic procedures were concluded successfully, and conversion to open surgery was not required. |
N = 2 (11.1%) 1 case prolonged air leak and 1 case wound infection occurred |
Mean/SD 80.71 ± 13.28min |
18-month | No recurrence |
| Cenk Balta 2019 [17] | N = 20 | Retrospective study | Mean 21.45(5–63) years | RUL 15%(n = 3) RLL 45%(n = 9) LUL 20%(n = 4) LLL 20%(n = 4) |
Mean size of cysts were 6.91 cm (Min-max: 2.4–15.6 cm). | mean time of hospitalization was 3.55 days (min-max: 2–7 days). |
conversion to mini thoracotomy in 3 (15%) cases and required a second port incision in 6 (30%) cases to control air leaks adequately |
N = 3 (15%) Failure of lung expansion (n = 1) Atelectasis (n = 2 |
Mean 91.25 min (Min-max: 45–175 min |
Patients were followed up by chest x-rays at postoperative 1, 2, 3 and 6th months. All the patients received albendazole treatment 10 mg/kg/day for 3 months |
No recurrence |
| Cenk Balta et al., 2020 [16] | N = 23 | Retrospective multicenter descriptive study | median age of the participants was 20 years (14–33 years) |
The most common location was right lower lobe followed by left lower lobe | The median diameter of the cysts was 7.3 cm (5.2–9.75 cm) | Median hospitalization time was 4 days (3–4 days) | The surgery was completed with a second camera port in 8 patients (34.78%) and with a 5-cm extension of the incision (mini-thoracotomy) in 4 patients (17.39%). |
Complication occurred in n = 3 (13%) | The duration of surgery was 85 min (70–90 min) | NA | No recurrence |
| Ocakcioglu 2016 [18] | N = 1 | Case report | A 27-year-old male | right lower lobe | 15-cm cystic lesion with air-fluid level | 4 days remain postoperatively | NA | NA | Total surgery time was 90 min | 22-month follow-up | No recurrence |
4. Discussion
Nowadays, uniportal video-assisted thoracoscopic surgery (u-VATS) has been widely accepted for thoracic surgeries. According to the results of the current systematic review, we conclude that the u-VATS approach is safe and feasible for the removal of pulmonary hydatid cysts smaller than 15 cm. The success rate of this technique depends on the experienced cardiothoracic and vascular surgeons and the quality of surgery instruments. To the best of our knowledge, this is the first systematic review for managing pulmonary hydatid cyst using a uniportal video-assisted thoracoscopic surgery (u-VATS). We believe that pulmonary hydatid cysts should be removed by surgeons who was performed more than 100 different surgeries by the u-VATS approach.
The goal of surgical treatment of pulmonary cysts is to remove the germinative membrane, capitonnage, and evacuation of the cystic content. Echinococcal cyst surgery is associated with low morbidity and mortality [[24], [25], [26]]. In 1994, Becmeur and collages described minimally invasive treatment for pulmonary hydatid cysts for the first time [27]. After that, in 1996, the VATS was used for pediatric patients, then became popular in adults for removal of pulmonary hydatid cyst [[28], [29], [30], [31], [32], [33]].
The most common method for removing pulmonary hydatid cysts is thoracotomy, it has been replaced by VATS recently due to benefits such as a shorter time to the hospital stay, less postoperative pain, reduce complications, and better cosmetic outcomes [34,35]. The two major reasons why surgeons did not prefer attempting VATS in pulmonary hydatid cysts were difficulty in managing the residual cavity and the fear of thoracic cavity contamination with cystic fluid. Some more recently published articles demonstrated some techniques for overcoming these technical challenges [[36], [37], [38]].
The feasibility of the video-assisted thoracoscopic surgery (VATS) approach has been proven by many global researchers in terms reduce postoperative pain, shorter surgery time, shorter chest tube duration, lower chest tube drainage, less intraoperative blood loss [19,28,29,31,33,36,[38], [39], [40], [41], [42], [43], [44], [45]]. For this reason, VATS has now become a novel standard of thoracic surgery. However, due to the risk of contamination of the chest cavity during surgery, and difficulties associated with captonnage and bronchial fistula closure, it has not been widely disseminated [38,46,47]. The u-VATS has also been reported to be contraindicated in patients with pulmonary hydatid cysts larger than 10 cm, cysts located in the hilum, multiple cysts in one lung, and single lung ventilation difficulties in children under 10 years of age [33,48]. However, it was later found that large cysts can be removed after aspiration [17], and multiple or intrathoracic cysts can be operated on with certain difficulties [49]. Localization of cysts smaller than 2 cm is relatively more difficult to detect, but this problem can be addressed with proper radiographic mapping.
The surgery time for removal of pulmonary hydatid cyst using uniportal video-assisted thoracoscopic surgery was shorter in comparision to thoracotomy or mini-thoracotomy groups [[15], [16], [17], [18], [19],33,46]. Additionally, the postoperative hospitalization was shorter in the VTAS groups comparison to thoracotomy or mini-thoracotomy [16,17,33,37,46]. According to previously published articles, patients who underwent uniportal video-assisted thoracoscopic surgery (u-VATS) have better cosmetic outcomes and less required to pain killers postoperatively compared to patients who underwent thoracotomy. The limitations in this review are only two databases were searched for relevant published articles, and excluded some studies due to the unavailability of full texts [50,51]. Furthermore, because the u-VATS remain a challenge for cardiothoracic and vascular surgeons for removal of pulmonary hydatid cyst there are a few publications reported in the literature.
5. Conclusion
The uniportal video-assisted thoracoscopic surgery (u-VATS) safe and feasible technique for the removal of pulmonary hydatid cysts smaller than 15 cm with experienced hand surgeons. While many previous researchers removed pulmonary hydatid cysts by thoracotomy, mini-thoracotomy, video-assisted thoracoscopic surgery using two or three ports; early studies revealed that a single incision (uniportal) could be performed. In comparison to thoracotomy, the u-VATS approach has many benefits such as reduced overall complication, shorter chest tube duration, shorter surgery time, reduced postoperative pain, shorter chest tube duration, lower chest tube drainage, less intraoperative blood loss, better cosmetic outcomes, and less required to pain killers postoperatively.
Ethical approval
Ethical approval does not require for systematic reviews.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
Sirwan K. Ahmed: Conception and design, execution, analysis and interpretation of data, involved in drafting the article, revised it critically for important intellectual content, read and approved the final version of the manuscript.
Rawand A. Essa: Conception and design, execution, analysis and interpretation of data, involved in drafting the article, revised it critically for important intellectual content, read and approved the final version of the manuscript.
Dunya H. Bapir: involved in drafting the article, revised it critically for important intellectual content, read and approved the final version of the manuscript.
Trial registry number
Not applicable.
Guarantor
Sirwan Khalid. Ahmed.
Email: sirwan.ahmed1989@gmail.com.
Consent
Not Applicable.
Author agreement statement
We declare that this manuscript is original, has not been published before and is not currently being considered for publication elsewhere. We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We confirm that the order of authors listed in the manuscript has been approved by all of us. We understand that the Corresponding Author is the sole contact for the Editorial process. He is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs.
Data availability statement
All relevant data are within the manuscript and its supporting information files.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
There is no conflict to be declared.
Acknowledgments
Not applicable.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.103474.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Burgos R., Varela A., Castedo E., Roda J., Montero C.G., Serrano S., Téllez G., Ugarte J. Pulmonary hydatidosis: surgical treatment and follow-up of 240 cases. Eur. J. Cardio. Thorac. Surg. 1999;16:628–635. doi: 10.1016/s1010-7940(99)00304-8. [DOI] [PubMed] [Google Scholar]
- 2.Auldist A.W., Blakelock R. Pediatr Thorac Surg. Springer; 2009. Pulmonary hydatid disease; pp. 161–167. [Google Scholar]
- 3.McManus D.P., Gray D.J., Zhang W., Yang Y. Diagnosis, treatment, and management of echinococcosis. BMJ. 2012;344 doi: 10.1136/bmj.e3866. e3866–e3866. [DOI] [PubMed] [Google Scholar]
- 4.Agudelo Higuita N.I., Brunetti E., McCloskey C. Cystic echinococcosis. J. Clin. Microbiol. 2016;54:518–523. doi: 10.1128/JCM.02420-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halezeroglu S., Celik M., Uysal A., Senol C., Keles M., Arman B. Giant hydatid cysts of the lung. J. Thorac. Cardiovasc. Surg. 1997;113:712–717. doi: 10.1016/S0022-5223(97)70228-9. [DOI] [PubMed] [Google Scholar]
- 6.Migliore M., Calvo D., Criscione A., Borrata F. Uniportal video assisted thoracic surgery: summary of experience, mini-review and perspectives. J. Thorac. Dis. 2015;7:E378–E380. doi: 10.3978/j.issn.2072-1439.2015.07.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Doğan R., Yüksel M., Cetin G., Süzer K., Alp M., Kaya S., Unlü M., Moldibi B. Surgical treatment of hydatid cysts of the lung: report on 1055 patients. Thorax. 1989;44:192–199. doi: 10.1136/thx.44.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xanthakis D., Efthimiadis M., Papadakis G., Primikirios N., Chassapakis G., Roussaki A., Veranis N., Akrivakis A., Aligizakis C.J. Hydatid disease of the chest: report of 91 patients surgically treated. Thorax. 1972;27:517–528. [Google Scholar]
- 9.Nahmias J., Goldsmith R., Soibelman M., El-On J. Three-to 7-year follow-up after albendazole treatment of 68 patients with cystic echinococcosis (hydatid disease) Ann. Trop. Med. Parasitol. 1994;88:295–304. doi: 10.1080/00034983.1994.11812870. [DOI] [PubMed] [Google Scholar]
- 10.Rocco G., Martucci N., La Manna C., Jones D.R., De Luca G., La Rocca A., Cuomo A., Accardo R. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann. Thorac. Surg. 2013;96:434–438. doi: 10.1016/j.athoracsur.2013.04.044. [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez D., Delgado M., Paradela M., Fernandez R. Uni-incisional video-assisted thoracoscopic left lower lobectomy in a patient with an incomplete fissure. Innovations. 2011;6:45–47. doi: 10.1097/IMI.0b013e31820b0862. [DOI] [PubMed] [Google Scholar]
- 12.Gonzalez-Rivas D., Paradela M., Fernandez R., Delgado M., Fieira E., Mendez L., Velasco C., de la Torre M. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann. Thorac. Surg. 2013;95:426–432. doi: 10.1016/j.athoracsur.2012.10.070. [DOI] [PubMed] [Google Scholar]
- 13.Hernandez-Arenas L.A., Lin L., Yang Y., Liu M., Guido W., Gonzalez-Rivas D., Jiang G., Jiang L. Initial experience in uniportal subxiphoid video-assisted thoracoscopic surgery for major lung resections. Eur. J. Cardio. Thorac. Surg. 2016;50:1060–1066. doi: 10.1093/ejcts/ezw189. [DOI] [PubMed] [Google Scholar]
- 14.Essa R.A., Ahmed S.K., Bapir D.H., Rasul S.A., Abubakr C.P., Khdir A.A., Mina S.B., M-Amin P.K. Resection of esophageal duplication cyst in a 6-month child: a surgical challenge by video-assisted thoracoscopic surgery VATS. IJS Glob Heal. 2021;4:e63. [Google Scholar]
- 15.Akar F.A., Gonzalez-Rivas D., Shaqqura B., Salman W., Ismail M., Safadi T., Adwan R., Al-Hassan H., Rumman N., Hijjeh N. Uniportal video assisted thoracoscopy versus open surgery for pulmonary hydatid disease—a single center experience. J. Thorac. Dis. 2020;12:794. doi: 10.21037/jtd.2019.12.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Balta C., Karacaoglu I.C., Iliklerden D.M., Yekdes A.C. Comparison of videothoracoscopy and thoracotomy in surgical treatment of pulmonary hydatid cyst disease. J Coll Physicians Surg JCPSP. 2020;30:1063–1068. doi: 10.29271/jcpsp.2020.10.1063. [DOI] [PubMed] [Google Scholar]
- 17.Balta C. Uniportal-single incision thoracoscopic access for pulmonary hydatid cysts. Curr. Respir. Med. Rev. 2019;15:39–44. [Google Scholar]
- 18.Ocakcioglu I. Single-port thoracoscopic surgery for a hudge hydatid cyst. Gen Thorac Cardiovasc Surg. 2017;65:235–238. doi: 10.1007/s11748-016-0654-z. [DOI] [PubMed] [Google Scholar]
- 19.Ocakcioglu I., S F. Uniportal thoracoscopic approach for pulmonary hydatid cyst: preliminary results. Surg. Laparosc. Endosc. Percutaneous Tech. 2018;28:298–302. doi: 10.1097/SLE.0000000000000560. -S. Laparoscopy, & E., U. 2018. [DOI] [PubMed] [Google Scholar]
- 20.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int. J. Surg. 2021;88:105906. doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- 21.Shea B.J., Reeves B.C., Wells G., Thuku M., Hamel C., Moran J., Moher D., Tugwell P., Welch V., Kristjansson E. Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Bmj. 2017;358 doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst. Rev. 2016;5:1–10. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moola S., Munn Z., Tufanaru C., Aromataris E., Sears K., Sfetcu R., Currie M., Qureshi R., Mattis P., Lisy K. vol. 5. Joanna Briggs Inst Rev Manual Joanna Briggs Inst; 2017. https://synthesismanual.jbi.global/ (Chapter 7: Systematic Reviews of Etiology and Risk). [Google Scholar]
- 24.Ulkü R., Yilmaz H.G., Onat S., Ozçelik C. Surgical treatment of pulmonary hydatid cysts: report of 139 cases. Int. Surg. 2006;91:77–81. [PubMed] [Google Scholar]
- 25.Karaoglanoglu N., Kurkcuoglu I.C., Gorguner M., Eroglu A., Turkyilmaz A. Giant hydatid lung cysts. Eur. J. Cardio. Thorac. Surg. 2001;19:914–917. doi: 10.1016/s1010-7940(01)00687-x. [DOI] [PubMed] [Google Scholar]
- 26.Yalcinkaya I., Er M., Ozbay B., Ugras S. Surgical treatment of hydatid cyst of the lung: review of 30 cases. Eur. Respir. J. 1999;13:441–444. doi: 10.1183/09031936.99.13244199. [DOI] [PubMed] [Google Scholar]
- 27.Becmeur F., Chaouachi B., Dhaoui R., Kaabar N., Popperova N., Bientz J., Sauvage P. Video-assisted thoracic surgery of hydatid cysts of the lung in children. J. Chir. 1994;131:541–543. [PubMed] [Google Scholar]
- 28.Parelkar S., Gupta R., Shah H.…S B. Experience with video-assisted thoracoscopic removal of pulmonary hydatid cysts in children. J. Pediatr. Surg. 2009;44:836–841. doi: 10.1016/j.jpedsurg.2008.11.029. -J. of pediatric, U. 2009. [DOI] [PubMed] [Google Scholar]
- 29.Paterson H.S., Blyth D.F. Thoracoscopic evacuation of dead hydatid cyst. J. Thorac. Cardiovasc. Surg. 1996;111:1280–1281. doi: 10.1016/s0022-5223(96)70231-3. [DOI] [PubMed] [Google Scholar]
- 30.Tullu M.S., Lahiri K.R., Kumar S., Oak S.N. Minimal access therapy in pediatric pulmonary hydatid cysts. Pediatr. Pulmonol. 2005;40:92–95. doi: 10.1002/ppul.20231. [DOI] [PubMed] [Google Scholar]
- 31.Chowbey P., Shah S., Khullar R.…S A. Minimal access surgery for hydatid cyst disease: laparoscopic, thoracoscopic, and retroperitoneoscopic approach. J. Laparoendosc. Adv. Surg. Tech. 2003;13:159–165. doi: 10.1089/109264203766207672. -… & A.S., U. 2003. [DOI] [PubMed] [Google Scholar]
- 32.Mallick M.S., Al-Qahtani A., Al-Saadi M.M., Al-Boukai A.A.A. Thoracoscopic treatment of pulmonary hydatid cyst in a child. J. Pediatr. Surg. 2005;40 doi: 10.1016/j.jpedsurg.2005.08.036. e35–e37. [DOI] [PubMed] [Google Scholar]
- 33.Alpay L., Lacin T., Ocakcioglu I.…E S. Is video-assisted thoracoscopic surgery adequate in treatment of pulmonary hydatidosis? Ann. Thorac. Surg. 2015;100:258–262. doi: 10.1016/j.athoracsur.2015.03.011. -T.A. of thoracic, U. 2015. [DOI] [PubMed] [Google Scholar]
- 34.Essa R.A., Ahmed S.K., Bapir D.H. Uniportal video-assisted thoracoscopic right lower and middle sleeve bilobectomy for a neglected carcinoid tumor. Ann Med Surg. 2022;75:103359. doi: 10.1016/j.amsu.2022.103359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Essa R.A., Ahmed S.K. Uniportal video-assisted thoracoscopic surgery for retained shrapnel in the thoracic cavity: an update surgical approach for removal of foreign body. Ann Med Surg. 2022;75:103402. doi: 10.1016/j.amsu.2022.103402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alpay L., Lacin T., Atinkaya C., Kıral H., Demir M., Baysungur V., Okur E., Yalcınkaya I. Video-assisted thoracoscopic removal of pulmonary hydatid cysts. Eur. J. Cardio. Thorac. Surg. 2012;42:971–975. doi: 10.1093/ejcts/ezs338. [DOI] [PubMed] [Google Scholar]
- 37.Mehta K.D., Gundappa R., Contractor R., Sangani V., Pathak A., Chawda P. Comparative evaluation of thoracoscopy versus thoracotomy in the management of lung hydatid disease. World J. Surg. 2010;34:1828–1831. doi: 10.1007/s00268-010-0581-6. [DOI] [PubMed] [Google Scholar]
- 38.Findikcioglu A., Karadayi S., Kilic D., Hatiopoglu A. Video-assisted thoracoscopic surgery to treat hydatid disease of the thorax in adults: is it feasible? J. Laparoendosc. Adv. Surg. Tech. 2012;22:882–885. doi: 10.1089/lap.2012.0272. [DOI] [PubMed] [Google Scholar]
- 39.Razok A., Ali M.M.B. Primary mediastinal hydatidosis successfully treated with combined medical therapy and VATS (Video-assisted thoracoscopic surgery) IDCases. 2021;23 doi: 10.1016/j.idcr.2020.e01008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ulusoy A., Baytemir C.A., Kavas M., Bekir S.A., Ersöz E., Bilek S., Yalçınkaya İ. Fibrin glue and partial capitonnage in giant hydatid cyst in a pediatric patient. Ann. Thorac. Surg. 2021:S0003–S4975. doi: 10.1016/j.athoracsur.2021.07.013. [DOI] [PubMed] [Google Scholar]
- 41.Uchikov A.P., Shipkov C.D., Prisadov G. Treatment of lung hydatidosis by VATS: a preliminary report. Can. J. Surg. 2004;47:380–381. [PMC free article] [PubMed] [Google Scholar]
- 42.Joshi D., Chowdhury A.…S M. Complicated bilateral pulmonary hydatid cysts. J Cardiothorac Surg Ther. 2020;4:52–56. doi: 10.36959/582/422. -J.C.S., U. 2020. [DOI] [Google Scholar]
- 43.Mallick M.S., Al-Qahtani A., Al-Saadi M., Amer A., Al-Boukai A. Thoracoscopic treatment of pulmonary hydatid cyst in a child. J. Pediatr. Surg. 2005;40:e35–e37. doi: 10.1016/j.jpedsurg.2005.08.036. [DOI] [PubMed] [Google Scholar]
- 44.Ma J., Wang X., Mamatimin X., Ahan N., Chen K., Peng C., Yang Y. Therapeutic evaluation of video-assisted thoracoscopic surgery versus open thoracotomy for pediatric pulmonary hydatid disease. J. Cardiothorac. Surg. 2016;11:1–7. doi: 10.1186/s13019-016-0525-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eroglu A., Aydin Y., A B. Video-assisted thoracoscopic surgery is safe and effective in the treatment of pulmonary hydatid cyst. Ann. Thorac. Surg. 2016;101:P829. doi: 10.1016/j.athoracsur.2015.07.015. -T.A. of Thoracic, U. 2016. [DOI] [PubMed] [Google Scholar]
- 46.Meng D., Fu L., Wang L., Dai Y., Lv W., Zhang J., Hu J. Video-assisted thoracoscopic surgery versus open thoracotomy in pulmonary metastasectomy: a meta-analysis of observational studies. Interact. Cardiovasc. Thorac. Surg. 2016;22:200–206. doi: 10.1093/icvts/ivv309. [DOI] [PubMed] [Google Scholar]
- 47.Amine K., Samia B., Jamila C.…M B. Thoracoscopic treatment of pulmonary hydatid cyst in children: a report of 25 cases. Tunis. Med. 2014;92:341–344. -L. tunisie, U. 2014. [PubMed] [Google Scholar]
- 48.Abbas N., Addeen S.…A F. Video-assisted Thoracoscopic Surgery (VATS) with mini-thoracotomy for the management of pulmonary hydatid cysts. J. Cardiothorac. Surg. 2018;13:1–6. doi: 10.1186/s13019-018-0716-7. -J. of, U. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schewitz I. Uniportal Nuss procedure for pectus excavatum, where to place the camera?-but we’ve always done it this way. J. Vis. Surg. 2017;3:42. doi: 10.21037/jovs.2017.03.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Akar F.A., Shaqqura B., Hijjeh N. Uniportal video-assisted thoracoscopic approach for pulmonary hydatid cyst. Chest. 2019;155:32A. [Google Scholar]
- 51.Ali H.A., Shihadeh B. Uniportal VATS for large hydatid cyst of the lung. 2017. https://www.ctsnet.org/article/uniportal-vats-large-hydatid-cyst-lung
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data are within the manuscript and its supporting information files.