Abstract
Blunted facial affect is a transdiagnostic component of Serious Mental Illness (SMI) and is associated with a host of negative outcomes. However, blunted facial affect is a poorly understood phenomenon, with no known cures or treatments. A critical step in better understanding its phenotypic expression involves clarifying which facial expressions are altered in specific ways and under what contexts. The current literature suggests that individuals with SMI show decreased positive facial expressions, but typical, or even increased negative facial expressions during laboratory tasks. While this literature has coalesced around general trends, significantly more nuance is available regarding what components facial expressions are atypical and how those components are associated with increased severity of clinical ratings. The present project leveraged computerized facial analysis to test whether clinician-rated blunted affect is driven by decreases in duration, intensity, or frequency of positive versus other facial expressions during a structured clinical interview. Stable outpatients meeting criteria for SMI (N = 59) were examined. Facial expression did not generally vary as a function of clinical diagnosis. Overall, clinically-rated blunted affect was not associated with positive expressions, but was associated with decreased surprise and increased anger, sadness, and fear expressions. Blunted affect is not a monolithic lack of expressivity, and increased precision in operationally defining it is critical for uncovering its causes and maintaining factors. Our discussion focuses on this effort, and on advancing digital phenotyping of blunted facial affect more generally.
Keywords: Schizophrenia, Clinical Ratings, Discrete Emotions, Blunted Affect, Negative Symptoms
1. Introduction
Blunted facial affect, or a reduction in the facial expression of emotions, is a transdiagnostic component of Serious Mental Illness (SMI) (Cooper et al., 2013; Gaebel and Wölwer, 2004; Harati et al., 2020, 2016; Renneberg et al., 2005; Strauss and Cohen, 2017). Blunted facial affect is a primary component of blunted affect, which comprises reductions of expressions through many channels, including facial, vocal, and gestural expressions. Blunted affect is a negative symptom of schizophrenia (American Psychiatric Association, 2013) and is also common in mood disorders (e.g., psychomotor retardation in depression), autism-spectrum, and neurodegenerative disorders (Levenson et al., 2014; Strauss and Cohen, 2017). Blunted facial affect is associated with poor social and vocational functioning (Cohen et al., 2020a; Riehle and Lincoln, 2018; Troisi et al., 2007) and increased risk of suicide (Grigoriou and Upthegrove, 2020). At present, there are no known cures, or well-validated treatments for blunted facial affect. Moreover, the mechanisms underlying it are not well delineated, though it is clear that blunted facial affect does not necessarily reflect an experiential deficit (Kring et al., 1993; Kring and Neale, 1996). Given the importance of facial expressions in social functioning more generally (Chovil, 1991; Fridlund, 1991; Hess et al., 1995), understanding blunted facial affect is an unmet need for addressing SMI.
A critical step in understanding blunted facial affect involves more precisely defining its phenotypic expression. This is necessary for advancing assessment, for example, using digital phenotyping technologies based on automated computerized facial analysis (Cohen et al., 2020a, 2020b) and for spurring scientific discovery of its mechanisms and of potential interventions. Currently, blunted affect is typically assessed using clinical rating scales (Kilian et al., 2015). The explicit definitions in these scales focus on a wide range of facial expressions and potential disruptions (e.g., frequency and intensity) (Axelrod et al., 1993; Kirkpatrick et al., 2011, 2006; Kring et al., 2013; Ventura et al., 1993). Using these scales, SMI patients, notably those with schizophrenia, show severe levels of blunted affect compared to nonpsychiatric controls, on the order of three to six standard deviations in blunted vocal affect and global negative symptoms (Cohen et al., 2014b). However, the aspects of facial expression disruptions which influence clinical ratings are only partially understood.
Studies employing behavioral analysis of facial expressions based on type, intensity, frequently, or duration (Ekman et al., 2002; Kring and Sloan, 2007) suggest that expressive deficits are more nuanced. First, individuals with schizophrenia generally show blunted happy expressions, but similar or exaggerated negative expressions than nonpsychiatric control individuals. This has been demonstrated using manual coding (Kohler et al., 2008a, 2008b; Lotzin et al., 2013; Mandal et al., 1998; Mattes et al., 1995), computerized facial analysis (Alvino et al., 2007; Bishay et al., 2019) and electromyography (EMG) (Mattes et al., 1995; Sestito et al., 2013; Varcin et al., 2019, 2010) methods (but see Aghevli et al., 2003 for decreased negative expressions). Studies employing EMG suggest that these alterations are primarily driven by abnormalities in facial muscles related to smiling (i.e., zygomaticus major) (Mattes et al., 1995; Varcin et al., 2019, 2010). When individuals with schizophrenia “pose” facial expressions under controlled laboratory conditions, findings are even more nuanced. Individuals with schizophrenia can pose faces of happiness and sadness (Putnam and Kring, 2007; Schwartz et al., 2006), but are less effective at posing surprise (Putnam and Kring, 2007; Schwartz et al., 2006), and have mixed success posing expressions of anger and disgust (Putnam and Kring, 2007; Schwartz et al., 2006). The expressions which individuals with schizophrenia can produce consciously are the ones which they seem to be less effective at producing in the normal flow of conversation. Second, across the schizophrenia spectrum, higher clinical ratings of blunted affect have been associated with reduced happiness (Gupta et al., 2019; Kring et al., 2013), but increased negative (Cohen et al., 2020a; Gupta et al., 2019) expressions (but see decreased negative facial expressions overall in Kring et al., 2013). In a related vein, in individuals with depression, symptom severity has been related to reduced happiness and increased contempt expressions (Girard et al., 2013).
Finally, similar patterns have generally been identified transdiagnostically. On the whole, facial expression is relatively similar in patients with schizophrenia and major depressive disorder (Trémeau et al., 2005), mirroring findings that have been reported with vocal expression between these groups (Cohen et al., 2012). Individuals with depression and borderline personality disorder show reductions in positive expressions and either equal (Davies et al., 2016; Gehricke and Shapiro, 2000; Renneberg et al., 2005) or more intense negative expressions (Girard et al., 2013; Jaeger et al., 1986; Matzke et al., 2014; Sloan et al., 1997; Staebler et al., 2011) relative to nonpsychiatric control individuals. A slight difference is found in bipolar disorder. While individuals with bipolar disorder have shown reductions in facial expressions relative to controls (Bersani et al., 2013; Broch-Due et al., 2018), and increased negative expressions, particularly fear (Kjærstad et al., 2020), they have also shown more surprised and engaged facial expressions, which are not inherently valanced in either direction (Broch-Due et al., 2018).
In reviewing the extant literature, it seems that blunted facial affect generally reflects decreased positive facial expressions and that negative facial expressions are either spared or exaggerated. The latter finding warrants replication (because it diverges from the operational definition of blunted affect), and there are three limitations with the extant literature to consider. First, most prior studies have focused on differences between schizophrenia and nonpsychiatric groups. This is problematic because not all patients with schizophrenia present with blunted affect (Bobes et al., 2010) and blunted affect is not solely present in schizophrenia. Using diagnosis as a stand in for “blunted affect” elides degrees of severity and ignores the transdiagnostic nature of this criterion. Rather, examining how clinical ratings of blunted affect in diverse samples of individuals with SMI are associated with facial expressions allows for greater understanding of this transdiagnostic concept. Second, prior studies have been inconsistent about how they quantified facial expression, with studies examining various aspects of duration, intensity, and frequency of expression “events” (Bishay et al., 2019; Juckel et al., 2008; Lotzin et al., 2013; Putnam and Kring, 2007). This multi-component approach is important in light of evidence that patients may have more ambiguous and less distinctive facial expressions (Hamm et al., 2014; Putnam and Kring, 2007). Finally, most prior studies have examined facial expression during a controlled laboratory task; one that is temporally and contextually removed from when/where the behavioral sampling informing the clinical ratings occurred (i.e., during a clinical interview).
The present study leveraged computerized facial expression technology to understand how different features of facial expressions were related to blunted affect during a clinical interview in a sample of SMI outpatients. Specifically, automated codings of intensity, frequency, and duration of happy, surprised, sad, scared, disgusted, and angry facial expressions were analyzed as predictors of clinical ratings of blunted facial affect. Informed by the extant literature, we hypothesized that lower frequency, intensity, and duration of positive expressions would be related to clinical ratings of blunted facial affect, and that frequency, intensity, and duration of other facial expressions might be increased.
2. Methods
2.1. Participants.
Participants (N = 59) were stable outpatients meeting U.S. federal definitions of SMI (ADAMHA, 1992), aggregated from two previous data collections from our lab (Cohen et al., 2019, 2014a, 2012). This is the first study examining computerized facial expression from these data collections. All participants were receiving treatment for an SMI from a multidisciplinary team and were living in a group home facility. The sample was two-thirds men (n = 39) and one-third women (n = 20), and was roughly split between White (n = 31) and Black/African-American (n = 27) participants, with 1 Asian-American participant. Participants’ ages ranged from 18 to 63 years old (M(SD) = 43.47 (10.53)). Lifetime diagnoses, determined by clinical interviews (see below), included schizophrenia (n = 36), major depressive disorder (n = 11), bipolar 1 disorder (n = 10) and psychosis not otherwise specified (n = 2). Of the 59 participants, 41 had psychosis by history. Two of the participants with major depressive disorder were in a current episode. None of the participants with bipolar disorder were in an active episode. Participants were free from major medical or other neurological disorders that would be expected to impair compliance with the research protocol. Though substance use was endorsed by the participants, no participant endorsed clinically relevant substance use per the Alcohol Use Disorders Identification Test /Drug Use Disorders Identification Test (AUDIT/DUDIT) scores (Berman et al., 2005; Bush, 1998).
2.2. Clinical measures.
Preliminary diagnoses and symptom ratings were made individually by doctoral level students who were trained to criterion (intraclass correlation coefficient values >= .70 on gold standard video review). Diagnoses and ratings were based on information obtained from medical records, the patients’ treatment teams, structured clinical interviews (including the Structured Clinical Interview for DSM– IV–TR; First et al., 2002), and self-report and behavioral observations made during the research interviews. All diagnoses and ratings were videotaped and carefully reviewed by a secondary graduate student. The diagnosis and ratings were then discussed during a case conference meeting led by a licensed clinical psychologist with considerable diagnostic experience (Alex S. Cohen). The group ranged from four to seven members. Final ratings and diagnoses were recorded when full agreement by the case conference members was reached. Nearly all interviewers were White. They were evenly split between male and female and were blind to our computerized facial expression assessment. Clinically-rated blunted facial affect, our primary dependent variable, was measured using the “Blunted facial affect” item from the Scale for the Assessment of Negative Symptoms (SANS)(Andreasen, 1989). Twenty-eight of 59 SANS blunted facial affect scores were in the “absent” range, 11 were “questionable”, and the remaining 20 were “mild” or greater in severity (See supplemental Figure S1 for a histogram of scores). As some research suggests bias in negative symptom ratings, specifically that negative symptoms are rated higher in Black individuals than in White individuals (Trierweiler et al., 2000), a t test was conducted to assess potential racial disparities in this rating including only the Black and White participants. No significant difference in clinician rated blunted affect (t(56)= 1.159, p = 0.25) by racial group was found.
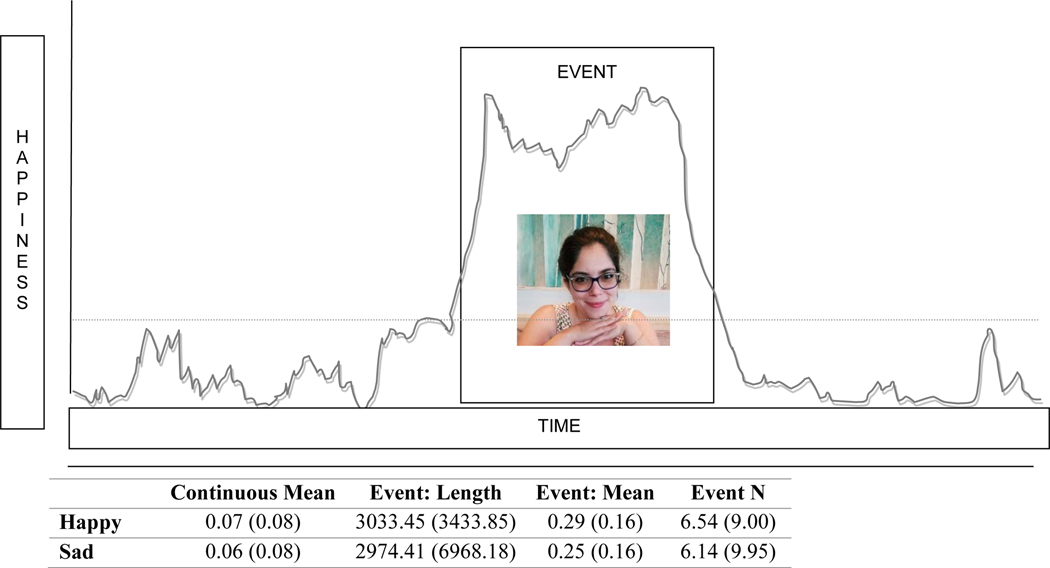
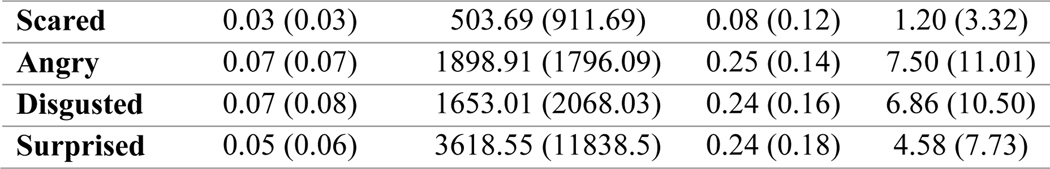
2.3. Computerized facial expression assessment (Figure 1).
Fig. 1.
Illustration of feature definition for a “Happy” event (above), with descriptive statistics (mean and standard deviations) for the emotion expression features (below)
Facial expressions were analyzed during video-recorded clinical interviews using FaceReader version 8.0 (Noldus, 2019). FaceReader is a commercially-available, automated facial expression analysis program, which has shown convergence with another automated program and human coding in prior work (Gupta et al., 2020). Scores were averaged across the first and last five-minute epochs of the interview (cf. (Gupta et al., 2020)) There were no significant differences between FaceReader scores from these five-minute epochs (i.e., all p’s > 0.05). FaceReader analyzes individual video frames and, using predefined algorithms which incorporate information from a subset of the action units from Ekman’s Facial Action Coding System (FACS) (Ekman et al., 2002), classifies different facial expression categories, including happy, sad, scared, angry, disgust and surprised facial expressions1 . Scores reflect a measure of confidence that an individual facial expression “category” is being shown, ranging from 0 (not at all) to 100 (perfect match). The most recent version of FaceReader, used in this study, was validated on a standardized set of images, each displaying one of eight facial emotions (van der Schalk et al., 2011). This validation set comprises images of North European (54.5%) and Mediterranean (Turkish and Moroccan) subjects (45.5%) and is largely male (54.5%). Relative to the current sample, the validation sample was less ethnically diverse (though also less White), and more male. We computed four measures for each expression category, the first based on all scores, and the remaining scores based on events (e.g., smiles) based on scores exceeding 0.26; a value corresponding to a Facial Action Coding System score of 2/B (i.e., slight) or greater. Our measures included: 1) Mean intensity (i.e., average score from all frames in the recording), 2) Mean event length (i.e., average length of facial expression event in milliseconds), 3) Mean event intensity (i.e., average score from frames during a facial expression event), and 4) N events (i.e., number of discrete facial expression events). These video recordings were originally made for interview fidelity and diagnostic/symptom reliability purposes, and were conducted in a variety of environments (e.g., conference rooms, group home living rooms) under a variety of lighting conditions. To ensure adequate data for analysis, video recordings with less than 10% of frames analyzable by FaceReader were excluded (as in (Cohen et al., 2017, 2013)). On average, 52.94% of frames were analyzable (SD = 30.76), with no significant differences between men and women or between White and Black/African-American participants (p’s > 0.45).
2.4. Analyses.
Analyses were conducted in two steps. We first conducted evaluation of the 24 facial expression features computed for this project, and their respective relationships to gender, race and age. Second, we compared diagnostic groups on these features. Given that blunted facial affect is a transdiagnostic feature of SMI, we expected these differences to be nonsignificant and small to negligible in effect size. Finally, we examined their relative relations to clinically-rated blunted facial affect. We computed linear regressions to compute the relative contributions of happy expressions (Step 1), and other expressions (Step 2) to clinically-rated blunted facial affect (dependent variable). These regressions were conducted “family-wise”, such that continuous mean, event mean, event length, and event number features were examined separately. Zero-order correlations between these variables were also computed. Analyses were conducted in R (R Core Team, 2019) using base, psych (Revelle, 2020), lme4(Bates et al., 2015), and ICC (Wolak et al., 2012)packages. All Variance Inflation Factor scores were below 2.50 (suggesting multi-collinearity was not an issue). Variables with skew > 2 were square root transformed, and all facial features scores were standardized and “trimmed” (i.e., values exceeding 3.50 standard deviations replaced with a value of 3.50).
3. Results
3.1. Preliminary analyses.
Per the computerized analysis, participants produced, on average, over 30 distinct facial expression events (Figure 1). The number of happy, sad, and disgusted events were fairly similar, and there were slightly more angry and fewer surprised events. Scared events were relatively infrequent. The length of these events varied, with happy, sad and surprised events lasting over 3 seconds, angry and disgusted events lasting approximately 1.5 seconds, and scared events lasting approximately 500 milliseconds. The intensity of these events, on average, was relatively similar.
Significant gender differences emerged for 7 of 24 facial expression features. Men showed more happy (i.e., with higher mean Intensity, and more frequent events), more angry (i.e., with higher mean intensity, and more, longer and more intense events) and less disgust (i.e., with less intense events) than women (p’s < 0.05, d’s > 0.49). Differences between Black/African-American and White individuals emerged for 5 of 24 facial expression features. Black/African-American individuals showed greater happiness (i.e., with higher mean intensity, and longer and more intense events) and less anger (i.e., with lower Mean Intensity, and fewer events) than White participants (p’s < 0.05, d’s > 0.58). Age was significantly correlated with 2 of 24 emotion expression features, with older age associated with greater happy (mean intensity (r = .33, p = 0.01) and fewer angry events ( r = −0.29, p = 0.02). Demographic variables were not significantly associated with the number of frames available for analysis.
3.2. Diagnostic differences.
Diagnostic differences were observed for only one of the emotion expression features. On average, patients with bipolar diagnoses showed significantly less intense happy events. The effect size was roughly equivalent when comparted to participants with depression (Cohen’s d = 1.06) or to participants with schizophrenia (Cohen’s d = 1.05).
3.3. Zero-order correlations (Supplemental Figure S2).
Clinically-rated blunted facial affect was significantly associated with 4 of 24 computerized facial expression features, including lower surprised (lower mean intensity, r= −0.34; mean event intensity scores; r= −0.31; number of events; r= − 0.38), and longer angry events (r= 0.31). The computer facial features were not redundant, as evidence by a relatively low average inter-correlation value (average r= 0.09), and only 7 of 576 possible correlation values exceeding 0.80.
3.4. Regression analyses (Table 1).
Table 1.
Linear regressions evaluating contributions from happy (step 1) and other emotional expressions (step 2) to clinically rated blunted facial affect (dependent variable).
| Measure of Emotional Expression | ||||||||
|---|---|---|---|---|---|---|---|---|
| Continuous Emotion: M | Event: M Length | Event: M Value | Event: N | |||||
| F | r2 | F | r 2 | F | r 2 | F | r 2 | |
| Step 1 | 2.83 | 0.03 | 2.75 | 0.03 | 2.46 | 0.02 | 1.52 | 0.01 |
| B (SE) | t | B (SE) | t | B (SE) | t | B (SE) | t | |
| Happy | −0.22 (0.13) | −1.68 | −0.22 | −1.66 | −0.20 | −1.57 | −0.16 | −1.23 |
| (0.13) | (0.13) | (0.13) | ||||||
| ΔF | Δ r 2 | ΔF | Δ r 2 | ΔF | Δ r 2 | ΔF | Δ r 2 | |
| Step 2 a | 2.47* | 0.11 | 3.97** | 0.21 | 2.42+ | 0.11 | 2.98* | 0.15 |
| B (SE) | t | B (SE) | t | B (SE) | t | B (SE) | t | |
| Happy | −0.25 (0.15) | −1.73 | −0.32 (0.13) |
− 2.38* |
−0.11 (0.14) |
−0.80 | −0.13 (0.14) |
0.18 |
| Sad | −0.08 (0.13) | −1.73 | 0.30 (0.14) |
2.13* | 0.10 (0.13) |
0.80 | 0.02 (0.13) | 0.18 |
| Scared | 0.24 (0.14) | 1.70 | 0.18 (0.14) |
1.32 | 0.21 (0.13) |
1.61 | 0.31 (0.14) | 2.27* |
| Angry | −0.02 (0.14) | −0.12 | 0.44 (0.13) |
3.35* * |
0.26 (0.14) |
1.89 | 0.05(0.14) | 0.34 |
| Disgusted | −0.04 (0.13) | −0.32 | −0.05 (0.13) |
−0.38 | −0.09 (0.14) |
−0.63 | −0.02 (0.13) |
−0.15 |
| Surprised | −0.47 (0.14) | −3.37** | −0.27 (0.16) |
−1.70 | −0.28 (0.13) |
− 2.13* |
−0.39 (0.13) |
− 3.06** |
NOTES: M = mean, N = Number. r2 = adjusted r2.
Also includes gender and ethnicity as covariates, ΔF and Δ r2 given relative to model including both happy and covariates.
= p = .05
= p < .05;
= p < .01
When predicting clinically-rated blunted affect, regression analyses showed that happy facial expressions made a significant contribution in one regression (i.e., mean event length). When happy expressions were included alone, they accounted for minimal variance (R2’s < 0.05). In contrast, the contributions of other facial expressions (i.e., in Step 2) were significant in three of four regressions, even when accounting for gender and ethnicity, and explained between 11% and 21% additional variance in clinical ratings. This primarily reflected decreased surprise expression (for 3 of 4 regressions), and increased anger, sadness, and scared emotion expression (for 1 of 4 regressions each), which emerged as predictors of clinically rated blunted affect.
4. Discussion
This study evaluated facial expressions during a clinical interview using automated facial expression technologies in a sample of outpatients with SMI. There were four notable findings. First and unexpectedly, decreased happy expressions were not generally related to clinical ratings of blunted facial affect. A significant relationship to clinically rated blunted affect emerged for only one of four measures of happy expression, and only in the model which also accounted for covariates and the other facial expressions. Second, decreased expressions of surprise were significantly related to clinical ratings of blunted affect. Surprise was a particularly important feature across regressions, spanning overall intensity, intensity during events, and number of events. Third, and converging with other studies, clinical ratings of blunted affect were related to increased expressions of anger, sadness, and fear. Finally, facial expression generally did not differ as a function of clinical diagnosis, highlighting the transdiagnostic consistency of this symptom.
Our findings join the mounting literature suggesting that blunted affect is not a monolithic lack of expressivity (Davies et al., 2016; Kohler et al., 2008a, 2008b; Mandal et al., 1998; Matzke et al., 2014; Staebler et al., 2011), which has important implications for understanding the potential mechanisms underlying blunted affect. It has been demonstrated elsewhere that blunted affect does not necessarily reflect a more global lack of emotional experience (e.g., Kring et al., 1993) or psychopharmacological treatment side effects (Kring and Earnst, 1999; Kring and Moran, 2008), and it seems unlikely that wholesale psychomotor deficits are responsible given that clinical ratings were associated with exaggerations in frequency, length and intensity for at least some facial expressions. Some researchers/theorists have proposed that blunted affect is primarily a symptom of social disconnectedness (e.g., Rümke, 1941; Sullivan, 1962), and it stands to reason that blunted facial affect arises as a function of social synchrony, reciprocity, and other interactive components with others (as discussed in affective and social sciences; Wheatley et al., 2012). In this manner, a patient who smiles during a clinical interview but fails to do so at contextually “appropriate” moments (e.g., when an interviewer tells a joke) may be judged as being clinically blunted. Similarly, a patient who shows increased anger expression in ways that are judged to disconnect from the interviewer may be rated as being clinically blunted, despite their motoric expressivity being increased. The potential causal roles that social synchrony, mimicry and interaction play in blunted facial affect have received limited attention to date, but have been observed in some (Dombrowski et al., 2014; Riehle et al., 2018; Sestito et al., 2013; Varcin et al., 2010), though not all (Riehle and Lincoln, 2018) previous studies.
The finding that decreased expressions of surprise were particularly important predictors of clinically-rated blunted affect may support the hypothesis that social connection is critical to blunted affect. Surprise is an interesting expression because it is not inherently valenced, but instead indicates engagement and arousal (Russell and Barrett, 1999). Indeed, lower levels of emotional engagement has been closely related to blunted affect (Stip et al., 2005), as has decreased clinician rated excitement (Ang et al., 2019). The central position of surprise in clinician rated blunted affect may have been missed in much of the past literature which has compared positive and negative emotions and side-stepped surprise (e.g. Alvino et al., 2007; Kohler et al., 2008a, 2008b). This finding does not generalize to deficits in facial expressions of high-arousal, as increased levels of high-arousal emotions, anger and fear, also were associated with clinician rated blunted affect. Looking at discrete emotions separately, rather than from a circumplex model, appears to be critical for understanding clinical ratings of blunted affect, and may offer unique insights into how blunted facial affect contributes to or is driven by motivational and functional deficits. For example, facial displays of different discrete emotions are thought to have unique adaptive significance, such as engaging different sensory systems and increasing the availability of sensory information (Susskind et al., 2008). Diminished facial expressivity may inhibit the acquisition of important sensory information and increases in certain kinds of expressions, like fear, may result in threatening information being overvalued.
It is clear from our results that it is important to evaluate intensity, duration, and frequency components of different affective expressions separately. Clinician ratings of blunted affect in this study seem to reflect longer duration of anger and sadness expressions combined with less intensity and frequency expression which suggest engagement. Updating rating scale manuals to emphasize discrete emotions and providing clinicians with direct training in how to assess facial displays in terms of intensity, duration, and frequency, may increase the validity of these measures. Recent symptom measures have included this level of nuance, including the Clinical Assessment Interview for Negative Symptoms (CAINS; (Kring et al., 2013) and the Brief Negative Symptom Scale (BNSS; (Strauss et al., 2012) which assess blunted affect based on frequency and intensity of expressions, but rate expressions broadly, rather than in terms of discrete emotions shown, or even valence. Systems for training raters in evaluating discrete emotional expressions exist, and have applied to undergraduates, school teachers, retail workers, and medical providers (Blanch-Hartigan, 2012; Endres and Laidlaw, 2009; Kemeny et al., 2012; Matsumoto and Hwang, 2011).
It is also noteworthy that, in our study, happy facial expressions were not related to clinically rated blunted facial affect. This could reflect that clinical interviews tend to focus on unpleasant content (e.g., psychiatric hospitalization, symptoms), and hence, happy expressions were less important in social connection between interviewee and interviewer. It is also possible that differentiating between genuine and nongenuine happy expressions, which fulfill different social roles (cf. Ekman and Friesen, 1982) might be important for understanding associated with blunted affect (cf. Ricard et al., 2021).
This study has several limitations. First, we were not able to explore the effects of various psychiatric medications on facial expressions, though in laboratory tasks antipsychotics were not shown to effect facial expressivity in schizophrenia (Kohler et al., 2008a). This sample was not specifically selected for high clinical ratings of blunted affect, and as such, as is typical in the literature (Bobes et al., 2010), only about 30% of the sample had clinically significant blunted affect. Range restriction could have impacted the results. Similarly, measurement error in either clinical ratings or computerized analyses of facial expression could also have impacted the results. Future research triangulating the effect of facial expressions on other outcome measures, such as measures of social functioning or clinician perceptions of engagement is needed. While these results suggest what informs clinician ratings of blunted affect, it is unknown whether similar features influence lay perceptions of blunted affect, or even whether the same features are influential in other situations outside of the clinical interview. While blunted affect may have effects on clinical care, it is important largely because of the effects it has on social interactions with laypeople outside of clinical settings (Hooley et al., 1987; Keltner and Kring, 1998; Riehle et al., 2018; Riehle and Lincoln, 2018). Future research should apply these same nuanced metrics of expressivity to videos gathered in more ecologically valid settings and with ratings made by untrained observers to ascertain whether surprise, anger, and sadness continue to influence others’ perceptions of individuals with SMI. Further, while this study had nearly equal representation from Black participants and White participants, there was less diversity in the clinicians who conducted the interviews, and no ability to explore expressive displays in other ethnic and racial groups or across cultures. Thus, the present data are informative for understanding interactions between White clinicians and Black and White participants, where we did not find racial differences in clinical ratings, but found differences in the facial expressions. Past studies have found that Asian American individuals with depression showing increased positive and negative expressions (Chentsova-Dutton et al., 2010, 2007), highlighting the importance of racial and ethnic diversity in future studies. There may have been unaddressed dynamics which influenced expressive displays, as racial differences between medical doctors and their patients can influence nonverbal displays (Lorié et al., 2017). Most of the studies in the literature thus far have either matched individuals with diagnoses and controls on ethnicity or have not addressed ethnicity at all. Further exploration of racial and ethnic differences in both expressions and how factors of expressivity relate to clinician ratings is warranted. Further, the algorithms used for computerized facial analyses may not yet be optimized for individuals with darker skin tones (Cowan et al., Under Review; Hitczenko et al., 2021), which may introduce noise in the data, though in the current study there was no difference by race in the algorithm’s ability to identify faces. Lastly, in identifying surprise as a crucial component of blunted affect, this study indicates reactivity may be crucial. Operationalizations of facial affect which directly address reactivity, like how long an expression takes to hit peak, or how quickly expressions change may be a fruitful future direction.
Supplementary Material
Acknowledgements
This project was funded by Grants from the National Institute of Mental Health (R03MH092622) and from the Louisiana Board of Regents to AC. The authors are grateful to Dr. Vijay Mittal for his suggestions. The authors acknowledge with gratitude all the participants who contributed to this study.
Funding
This project was funded by Grants from the National Institute of Mental Health (R03MH092622) and from the Louisiana Board of Regents to AC
Footnotes
Conflicts of Interest
G. P. Strauss is one of the original developers of the Brief Negative Symptom Scale (BNSS) and receives royalties and consultation fees from ProPhase LLC in connection with commercial use of the BNSS and other professional activities; these fees are donated to the Brain and Behavior Research Foundation. Dr. Strauss has received honoraria and travel support from ProPhase LLC for training pharmaceutical company raters on the BNSS. In the past two years, Dr. Strauss has consulted for and/or been on the speaker bureau for Minerva Neurosciences, Acadia, and Lundbeck pharmaceutical companies. No other others have conflicts to report.
FaceReader also provides scores for “contempt” which were not included in this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aghevli MA, Blanchard JJ, Horan WP, 2003. The expression and experience of emotion in schizophrenia: a study of social interactions. Psychiatry Res. 119, 261–270. 10.1016/S0165-1781(03)00133-1 [DOI] [PubMed] [Google Scholar]
- Alvino C, Kohler C, Barrett F, Gur RE, Gur RC, Verma R, 2007. Computerized measurement of facial expression of emotions in schizophrenia. J. Neurosci. Methods 163, 350–361. 10.1016/j.jneumeth.2007.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (Ed.), 2013. Diagnostic and statistical manual of mental disorders: DSM-5, 5th ed. ed. American Psychiatric Association, Washington, D.C. [Google Scholar]
- Andreasen NC, 1989. The Scale for the Assessment of Negative Symptoms (SANS): conceptual and theoretical foundations. Br. J. Psychiatry. Suppl. 49–58. [PubMed] [Google Scholar]
- Ang MS, Rekhi G, Lee J, 2019. Validation of the Brief Negative Symptom Scale and its association with functioning. Schizophr. Res. 208, 97–104. 10.1016/j.schres.2019.04.005 [DOI] [PubMed] [Google Scholar]
- Axelrod BN, Goldman RS, Alphs LD, 1993. Validation of the 16-item negative symptom assessment. J. Psychiatr. Res. 27, 253–258. 10.1016/0022-3956(93)90036-2 [DOI] [PubMed] [Google Scholar]
- Bates D, Mächler M, Bolker B, Walker S, 2015. Fitting Linear Mixed-Effects Models Using lme4. J. Stat. Softw. 67. 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- Berman AH, Bergman H, Palmstierna T, Schlyter F, 2005. Evaluation of the Drug Use Disorders Identification Test (DUDIT) in Criminal Justice and Detoxification Settings and in a Swedish Population Sample. Eur. Addict. Res. 11, 22–31. 10.1159/000081413 [DOI] [PubMed] [Google Scholar]
- Bersani FS, Bersani Polli, Valeriani G, Zullo D, Melcore C, Capra Quartini, Marino P, Minichino Bernabei, Robiony Liberati, 2013. Facial expression in patients with bipolar disorder and schizophrenia in response to emotional stimuli: a partially shared cognitive and social deficit of the two disorders. Neuropsychiatr. Dis. Treat. 1137. 10.2147/NDT.S46525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishay M, Palasek P, Priebe S, Patras I, 2019. SchiNet: Automatic Estimation of Symptoms of Schizophrenia from Facial Behaviour Analysis. IEEE Trans. Affect. Comput. 1–1. 10.1109/TAFFC.2019.2907628 [DOI] [Google Scholar]
- Blanch-Hartigan D, 2012. An effective training to increase accurate recognition of patient emotion cues. Patient Educ. Couns. 89, 274–280. 10.1016/j.pec.2012.08.002 [DOI] [PubMed] [Google Scholar]
- Bobes J, Arango C, Garcia-Garcia M, Rejas J, CLAMORS Study Collaborative Group, 2010. Prevalence of Negative Symptoms in Outpatients With Schizophrenia Spectrum Disorders Treated With Antipsychotics in Routine Clinical Practice: Findings From the CLAMORS Study. J. Clin. Psychiatry 71, 280–286. 10.4088/JCP.08m04250yel [DOI] [PubMed] [Google Scholar]
- Broch-Due I, Kjærstad HL, Kessing LV, Miskowiak K, 2018. Subtle behavioural responses during negative emotion reactivity and down-regulation in bipolar disorder: A facial expression and eye-tracking study. Psychiatry Res. 266, 152–159. 10.1016/j.psychres.2018.04.054 [DOI] [PubMed] [Google Scholar]
- Bush K, 1998. The AUDIT Alcohol Consumption Questions (AUDIT-C) An Effective Brief Screening Test for Problem Drinking. Arch. Intern. Med. 158, 1789. 10.1001/archinte.158.16.1789 [DOI] [PubMed] [Google Scholar]
- Chentsova-Dutton YE, Chu JP, Tsai JL, Rottenberg J, Gross JJ, Gotlib IH, 2007. Depression and emotional reactivity: Variation among Asian Americans of East Asian descent and European Americans. J. Abnorm. Psychol. 116, 776–785. 10.1037/0021-843X.116.4.776 [DOI] [PubMed] [Google Scholar]
- Chentsova-Dutton YE, Tsai JL, Gotlib IH, 2010. Further evidence for the cultural norm hypothesis: Positive emotion in depressed and control European American and Asian American women. Cultur. Divers. Ethnic Minor. Psychol. 16, 284–295. 10.1037/a0017562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chovil N, 1991. Social determinants of facial displays. J. Nonverbal Behav. 15, 141–154. 10.1007/BF01672216 [DOI] [Google Scholar]
- Cohen AS, Cowan T, Le TP, Schwartz EK, Kirkpatrick B, Raugh IM, Chapman HC, Strauss GP, 2020a. Ambulatory digital phenotyping of blunted affect and alogia using objective facial and vocal analysis: Proof of concept. Schizophr. Res. S0920996420301535. 10.1016/j.schres.2020.03.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen AS, Fedechko TL, Schwartz EK, Le TP, Foltz PW, Bernstein J, Cheng J, Holmlund TB, Elvevåg B, 2019. Ambulatory vocal acoustics, temporal dynamics, and serious mental illness. J. Abnorm. Psychol. 128, 97–105. 10.1037/abn0000397 [DOI] [PubMed] [Google Scholar]
- Cohen AS, McGovern JE, Dinzeo TJ, Covington MA, 2014a. Speech deficits in serious mental illness: A cognitive resource issue? Schizophr. Res. 160, 173–179. 10.1016/j.schres.2014.10.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen AS, Mitchell KR, Elvevåg B, 2014b. What do we really know about blunted vocal affect and alogia? A meta-analysis of objective assessments. Schizophr. Res. 159, 533–538. 10.1016/j.schres.2014.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen AS, Mitchell KR, Strauss GP, Blanchard JJ, Buchanan RW, Kelly DL, Gold J, McMahon RP, Adams HA, Carpenter WT, 2017. The effects of oxytocin and galantamine on objectively-defined vocal and facial expression: Data from the CIDAR study. Schizophr. Res. 188, 141–143. 10.1016/j.schres.2017.01.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen AS, Morrison SC, Callaway DA, 2013. Computerized facial analysis for understanding constricted/blunted affect: Initial feasibility, reliability, and validity data. Schizophr. Res. 148, 111–116. 10.1016/j.schres.2013.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen AS, Najolia GM, Kim Y, Dinzeo TJ, 2012. On the boundaries of blunt affect/alogia across severe mental illness: Implications for Research Domain Criteria. Schizophr. Res. 140, 41–45. 10.1016/j.schres.2012.07.001 [DOI] [PubMed] [Google Scholar]
- Cohen AS, Schwartz E, Le T, Cowan T, Cox C, Tucker R, Foltz P, Holmlund TB, Elvevåg B, 2020b. Validating digital phenotyping technologies for clinical use: the critical importance of “resolution.” World Psychiatry 19, 114–115. 10.1002/wps.20703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper SE, Miranda R, Mennin DS, 2013. Behavioral Indicators of Emotional Avoidance and Subsequent Worry in Generalized Anxiety Disorder and Depression. J. Exp. Psychopathol. 4, 566–583. 10.5127/jep.033512 [DOI] [Google Scholar]
- Cowan T, Cohen AS, Raugh IM, Strauss GP, Under Review. Ambulatory audio and video recording for digital phenotyping in schizophrenia: Adherence & data usability. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies H, Wolz I, Leppanen J, Fernandez-Aranda F, Schmidt U, Tchanturia K, 2016. Facial expression to emotional stimuli in non-psychotic disorders: A systematic review and metaanalysis. Neurosci. Biobehav. Rev. 64, 252–271. 10.1016/j.neubiorev.2016.02.015 [DOI] [PubMed] [Google Scholar]
- Dombrowski M, McCleery A, Gregory SW, Docherty NM, 2014. Stress Reactivity of Emotional and Verbal Speech Content in Schizophrenia: J. Nerv. Ment. Dis. 202, 608–612. 10.1097/NMD.0000000000000169 [DOI] [PubMed] [Google Scholar]
- Ekman P, Friesen WV, 1982. Felt, false, and miserable smiles. J. Nonverbal Behav. 6, 238–252. 10.1007/BF00987191 [DOI] [Google Scholar]
- Ekman P, Friesen WV, Hager JC, 2002. Facial Action Coding System. Manual and Investigator’s Guide. Research Nexus., Salt Lake City, UT. [Google Scholar]
- Endres J, Laidlaw A, 2009. Micro-expression recognition training in medical students: a pilot study. BMC Med. Educ. 9, 47. 10.1186/1472-6920-9-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J, 2002. Structured Clinical Interview for DSM-IV-TR Axis 1 Disorders, Research Version, Patient Edition. (SCID-I/P). Biometrics Research, New York State Psychiatric Institute., New York. [Google Scholar]
- Fridlund AJ, 1991. Sociality of Solitary Smiling: Potentiation by an Implicit Audience 12. [Google Scholar]
- Gaebel W, Wölwer W, 2004. Facial expressivity in the course of schizophrenia and depression. Eur. Arch. Psychiatry Clin. Neurosci. 254. 10.1007/s00406-004-0510-5 [DOI] [PubMed] [Google Scholar]
- Gehricke J-G, Shapiro D, 2000. Reduced facial expression and social context in major depression: discrepancies between facial muscle activity and self-reported emotion. Psychiatry Res. 95, 157–167. 10.1016/S0165-1781(00)00168-2 [DOI] [PubMed] [Google Scholar]
- Girard JM, Cohn JF, Mahoor MH, Mavadati S, Rosenwald DP, 2013. Social Risk and Depression: Evidence from Manual and Automatic Facial Expression Analysis. Proc. Int. Conf. Autom. Face Gesture Recognit. IEEE Int. Conf. Autom. Face Gesture Recognit. 1–8. 10.1109/FG.2013.6553748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigoriou M, Upthegrove R, 2020. Blunted affect and suicide in schizophrenia: A systematic review. Psychiatry Res. 293, 113355. 10.1016/j.psychres.2020.113355 [DOI] [PubMed] [Google Scholar]
- Gupta T, Haase CM, Strauss GP, Cohen AS, Mittal VA, 2019. Alterations in facial expressivity in youth at clinical high-risk for psychosis. J. Abnorm. Psychol. 128, 341–351. 10.1037/abn0000413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta T, Haase CM, Strauss GP, Cohen AS, Ricard JR, Mittal VA, 2020. Alterations in facial expressions of emotion: Determining the promise of ultrathin slicing approaches and comparing human and automated coding methods in psychosis risk. Emotion. 10.1037/emo0000819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamm J, Pinkham A, Gur RC, Verma R, Kohler CG, 2014. Dimensional Information-Theoretic Measurement of Facial Emotion Expressions in Schizophrenia. Schizophr. Res. Treat. 2014, 1–10. 10.1155/2014/243907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harati S, Crowell A, Huang Y, Mayberg H, Nemati S, 2020. Classifying Depression Severity in Recovery From Major Depressive Disorder via Dynamic Facial Features. IEEE J. Biomed. Health Inform. 24, 815–824. 10.1109/JBHI.2019.2930604 [DOI] [PubMed] [Google Scholar]
- Harati S, Crowell A, Mayberg H, Kong J, Nemati S, 2016. Discriminating clinical phases of recovery from major depressive disorder using the dynamics of facial expression, in: 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). Presented at the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), IEEE, Orlando, FL, USA, pp. 2254–2257. 10.1109/EMBC.2016.7591178 [DOI] [PubMed] [Google Scholar]
- Hess U, Banse R, Kappas A, 1995. The intensity of facial expression is determined by underlying affective state and social situation. J. Pers. Soc. Psychol. 69, 280–288. 10.1037/0022-3514.69.2.280 [DOI] [Google Scholar]
- Hitczenko K, Cowan HR, Goldrick M, Mittal VA, 2021. Racial and Ethnic Biases in Computational Approaches to Psychopathology. Schizophr. Bull. 10.1093/schbul/sbab131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooley JM, Richters JE, Weintraub S, Neale JM, 1987. Psychopathology and marital distress: The positive side of positive symptoms. J. Abnorm. Psychol. 96, 27–33. 10.1037/0021-843X.96.1.27 [DOI] [PubMed] [Google Scholar]
- Jaeger J, Borod JC, Peselow E, 1986. Facial expression of positive and negative emotions in patients with unipolar depression. J. Affect. Disord. 11, 43–50. 10.1016/01650327(86)90058-3 [DOI] [PubMed] [Google Scholar]
- Juckel G, Mergl R, Präßl A, Mavrogiorgou P, Witthaus H, Möller HJ, Hegerl U, 2008. Kinematic analysis of facial behaviour in patients with schizophrenia under emotional stimulation by films with “Mr. Bean.” Eur. Arch. Psychiatry Clin. Neurosci. 258, 186–191. 10.1007/s00406-007-0778-3 [DOI] [PubMed] [Google Scholar]
- Keltner D, Kring AM, 1998. Emotion, Social Function, and Psychopathology. Rev. Gen. Psychol. 2, 320–342. 10.1037/1089-2680.2.3.320 [DOI] [Google Scholar]
- Kemeny ME, Foltz C, Cavanagh JF, Cullen M, Giese-Davis J, Jennings P, Rosenberg EL, Gillath O, Shaver PR, Wallace BA, Ekman P, 2012. Contemplative/emotion training reduces negative emotional behavior and promotes prosocial responses. Emotion 12, 338–350. 10.1037/a0026118 [DOI] [PubMed] [Google Scholar]
- Kilian S, Asmal L, Goosen A, Chiliza B, Phahladira L, Emsley R, 2015. Instruments Measuring Blunted Affect in Schizophrenia: A Systematic Review. PLOS ONE 10, e0127740. 10.1371/journal.pone.0127740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkpatrick B, Fenton WS, Carpenter WT, Marder SR, 2006. The NIMH-MATRICS Consensus Statement on Negative Symptoms. Schizophr. Bull. 32, 214–219. 10.1093/schbul/sbj053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkpatrick B, Strauss GP, Nguyen L, Fischer BA, Daniel DG, Cienfuegos A, Marder SR, 2011. The Brief Negative Symptom Scale: Psychometric Properties. Schizophr. Bull. 37, 300–305. 10.1093/schbul/sbq059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kjærstad HL, Jørgensen CK, Broch-Due I, Kessing LV, Miskowiak K, 2020. Eye gaze and facial displays of emotion during emotional film clips in remitted patients with bipolar disorder. Eur. Psychiatry 63, e29. 10.1192/j.eurpsy.2020.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohler CG, Martin EA, Milonova M, Wang P, Verma R, Brensinger CM, Bilker W, Gur RE, Gur RC, 2008a. Dynamic evoked facial expressions of emotions in schizophrenia. Schizophr. Res. 105, 30–39. 10.1016/j.schres.2008.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohler CG, Martin EA, Stolar N, Barrett FS, Verma R, Brensinger C, Bilker W, Gur RE, Gur RC, 2008b. Static posed and evoked facial expressions of emotions in schizophrenia. Schizophr. Res. 105, 49–60. 10.1016/j.schres.2008.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kring AM, Earnst KS, 1999. Stability of emotional responding in schizophrenia. Behav. Ther. 30, 373–388. 10.1016/S0005-7894(99)80016-1 [DOI] [Google Scholar]
- Kring AM, Gur RE, Blanchard JJ, Horan WP, Reise SP, 2013. The Clinical Assessment Interview for Negative Symptoms (CAINS): Final Development and Validation. Am. J. Psychiatry 170, 165–172. 10.1176/appi.ajp.2012.12010109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kring AM, Kerr SL, Smith DA, Neale JM, 1993. Flat affect in schizophrenia does not reflect diminished subjective experience of emotion. J. Abnorm. Psychol. 102, 507–517. 10.1037/0021-843X.102.4.507 [DOI] [PubMed] [Google Scholar]
- Kring AM, Moran EK, 2008. Emotional Response Deficits in Schizophrenia: Insights From Affective Science. Schizophr. Bull. 34, 819–834. 10.1093/schbul/sbn071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kring AM, Neale JM, 1996. Do schizophrenic patients show a disjunctive relationship among expressive, experiential, and psychophysiological components of emotion? J. Abnorm. Psychol. 105, 249–257. 10.1037/0021-843X.105.2.249 [DOI] [PubMed] [Google Scholar]
- Kring AM, Sloan DM, 2007. The Facial Expression Coding System (FACES): Development, validation, and utility. Psychol. Assess. 19, 210–224. 10.1037/1040-3590.19.2.210 [DOI] [PubMed] [Google Scholar]
- Levenson RW, Sturm VE, Haase CM, 2014. Emotional and Behavioral Symptoms in Neurodegenerative Disease: A Model for Studying the Neural Bases of Psychopathology. Annu. Rev. Clin. Psychol. 10, 581–606. 10.1146/annurev-clinpsy-032813-153653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorié Á, Reinero DA, Phillips M, Zhang L, Riess H, 2017. Culture and nonverbal expressions of empathy in clinical settings: A systematic review. Patient Educ. Couns. 100, 411–424. 10.1016/j.pec.2016.09.018 [DOI] [PubMed] [Google Scholar]
- Lotzin A, Haack-Dees B, Resch F, Romer G, Ramsauer B, 2013. Facial emotional expression in schizophrenia adolescents during verbal interaction with a parent. Eur. Arch. Psychiatry Clin. Neurosci. 263, 529–536. 10.1007/s00406-012-0386-8 [DOI] [PubMed] [Google Scholar]
- Mandal MK, Pandey R, Prasad AB, 1998. Facial Expressions of Emotions and Schizophrenia: A Review. Schizophr. Bull. 24, 399–412. 10.1093/oxfordjournals.schbul.a033335 [DOI] [PubMed] [Google Scholar]
- Matsumoto D, Hwang HS, 2011. Evidence for training the ability to read microexpressions of emotion. Motiv. Emot. 35, 181–191. 10.1007/s11031-011-9212-2 [DOI] [Google Scholar]
- Mattes RM, Schneider F, Heimann H, Birbaumer N, 1995. Reduced emotional response of schizophrenic patients in remission during social interaction. Schizophr. Res. 17, 249–255. 10.1016/0920-9964(95)00014-3 [DOI] [PubMed] [Google Scholar]
- Matzke B, Herpertz SC, Berger C, Fleischer M, Domes G, 2014. Facial Reactions during Emotion Recognition in Borderline Personality Disorder: A Facial Electromyography Study. Psychopathology 47, 101–110. 10.1159/000351122 [DOI] [PubMed] [Google Scholar]
- Noldus, 2019. FaceReader. Noldus, Wageningen, the Netherlands. [Google Scholar]
- Putnam KM, Kring AM, 2007. Accuracy and intensity of posed emotional expressions in unmedicated schizophrenia patients: Vocal and facial channels. Psychiatry Res. 151, 67–76. 10.1016/j.psychres.2006.09.010 [DOI] [PubMed] [Google Scholar]
- R Core Team, 2019. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. [Google Scholar]
- Renneberg B, Heyn K, Gebhard R, Bachmann S, 2005. Facial expression of emotions in borderline personality disorder and depression. J. Behav. Ther. Exp. Psychiatry 36, 183–196. 10.1016/j.jbtep.2005.05.002 [DOI] [PubMed] [Google Scholar]
- Revelle W, 2020. psych: Procedures for Psychological, Psychometric, and Personality Research. R package version 2.0.12,. Northwestern University, Evanston, Illinois. [Google Scholar]
- Ricard JR, Gupta T, Vargas T, Haase CM, Mittal VA, 2021. Genuine and non-genuine smiles in individuals meeting criteria for a clinical high-risk syndrome. Early Interv. Psychiatry eip.13233. 10.1111/eip.13233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riehle M, Lincoln TM, 2018. Investigating the social costs of schizophrenia: Facial expressions in dyadic interactions of people with and without schizophrenia. J. Abnorm. Psychol. 127, 202–215. 10.1037/abn0000319 [DOI] [PubMed] [Google Scholar]
- Riehle M, Mehl S, Lincoln TM, 2018. The specific social costs of expressive negative symptoms in schizophrenia: reduced smiling predicts interactional outcome. Acta Psychiatr. Scand. 138, 133–144. 10.1111/acps.12892 [DOI] [PubMed] [Google Scholar]
- Rümke H, 1941. Das Kernsymptom der Schizophrenie und das “Praecox-Gefühl.” Z Gesamte Neurol Psychiatr 102, 168–75. [Google Scholar]
- Russell JA, Barrett LF, 1999. Core affect, prototypical emotional episodes, and other things called emotion: Dissecting the elephant. J. Pers. Soc. Psychol. 76, 805–819. 10.1037/0022-3514.76.5.805 [DOI] [PubMed] [Google Scholar]
- Schwartz BL, Mastropaolo J, Rosse RB, Mathis G, Deutsch SI, 2006. Imitation of facial expressions in schizophrenia. Psychiatry Res. 145, 87–94. 10.1016/j.psychres.2005.12.007 [DOI] [PubMed] [Google Scholar]
- Sestito M, Umiltà MA, De Paola G, Fortunati R, Raballo A, Leuci E, Maffei S, Tonna M, Amore M, Maggini C, Gallese V, 2013. Facial reactions in response to dynamic emotional stimuli in different modalities in patients suffering from schizophrenia: a behavioral and EMG study. Front. Hum. Neurosci. 7. 10.3389/fnhum.2013.00368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan DM, Strauss ME, Quirk SW, Sajatovic M, 1997. Subjective and expressive emotional responses in depression. J. Affect. Disord. 46, 135–141. 10.1016/S01650327(97)00097-9 [DOI] [PubMed] [Google Scholar]
- Staebler K, Renneberg B, Stopsack M, Fiedler P, Weiler M, Roepke S, 2011. Facial emotional expression in reaction to social exclusion in borderline personality disorder. Psychol. Med. 41, 1929–1938. 10.1017/S0033291711000080 [DOI] [PubMed] [Google Scholar]
- Stip E, Fahim C, Mancini-Marïe A, Bentaleb LA, Mensour B, Mendrek A, Beauregard M, 2005. Restoration of frontal activation during a treatment with quetiapine: an fMRI study of blunted affect in schizophrenia. Prog. Neuropsychopharmacol. Biol. Psychiatry 29, 21–26. 10.1016/j.pnpbp.2004.08.015 [DOI] [PubMed] [Google Scholar]
- Strauss GP, Cohen AS, 2017. A Transdiagnostic Review of Negative Symptom Phenomenology and Etiology. Schizophr. Bull. 43, 712–719. 10.1093/schbul/sbx066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss GP, Keller WR, Buchanan RW, Gold JM, Fischer BA, McMahon RP, Catalano LT, Culbreth AJ, Carpenter WT, Kirkpatrick B, 2012. Next-generation negative symptom assessment for clinical trials: Validation of the Brief Negative Symptom Scale. Schizophr. Res. 142, 88–92. 10.1016/j.schres.2012.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan HS, 1962. Schizophrenia as a human process. With Introduction and Commentaries by Helen Swick Perry. Norton, New York. [Google Scholar]
- Susskind JM, Lee DH, Cusi A, Feiman R, Grabski W, Anderson AK, 2008. Expressing fear enhances sensory acquisition. Nat. Neurosci. 11, 843–850. 10.1038/nn.2138 [DOI] [PubMed] [Google Scholar]
- Trémeau F, Malaspina D, Duval F, Corrêa H, Hager-Budny M, Coin-Bariou L, Macher J-P, Gorman JM, 2005. Facial Expressiveness in Patients With Schizophrenia Compared to Depressed Patients and Nonpatient Comparison Subjects. Am. J. Psychiatry 162, 92–101. 10.1176/appi.ajp.162.1.92 [DOI] [PubMed] [Google Scholar]
- Trierweiler SJ, Neighbors HW, Munday C, Thompson EE, Binion VJ, Gomez JP, 2000. Clinician attributions associated with the diagnosis of schizophrenia in African American and non-African American patients. J. Consult. Clin. Psychol. 68, 171–175. 10.1037/0022-006X.68.1.171 [DOI] [PubMed] [Google Scholar]
- Troisi A, Pompili E, Binello L, Sterpone A, 2007. Facial expressivity during the clinical interview as a predictor functional disability in schizophrenia. A pilot study. Prog. Neuropsychopharmacol. Biol. Psychiatry 31, 475–481. 10.1016/j.pnpbp.2006.11.016 [DOI] [PubMed] [Google Scholar]
- Varcin KJ, Bailey PE, Henry JD, 2010. Empathic deficits in schizophrenia: The potential role of rapid facial mimicry. J. Int. Neuropsychol. Soc. 16, 621–629. 10.1017/S1355617710000329 [DOI] [PubMed] [Google Scholar]
- Varcin KJ, Nangle MR, Henry JD, Bailey PE, Richmond JL, 2019. Intact spontaneous emotional expressivity to non-facial but not facial stimuli in schizophrenia: An electromyographic study. Schizophr. Res. 206, 37–42. 10.1016/j.schres.2018.12.019 [DOI] [PubMed] [Google Scholar]
- Ventura J, Lukoff D, Nuechterlein K, Liberman R, Green M, Shaner A, 1993. Appendix 1: Brief Psychiatric Rating Scale (BPRS) Expanded version (4.0) scales, anchor points and administration manual. Int. J. Methods Psychiatr. 3, 227–244. [Google Scholar]
- Wheatley T, Kang O, Parkinson C, Looser CE, 2012. From Mind Perception to Mental Connection: Synchrony as a Mechanism for Social Understanding: Mind Perception and Mental Connection. Soc. Personal. Psychol. Compass 6, 589–606. 10.1111/j.17519004.2012.00450.x [DOI] [Google Scholar]
- Wolak ME, Fairbairn DJ, Paulsen YR, 2012. Guidelines for estimating repeatability: Guidelines for estimating repeatability. Methods Ecol. Evol. 3, 129–137. 10.1111/j.2041210X.2011.00125.x [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.