Summary
Arterial blood pressure is the driving force for organ perfusion. Although hypotension is common in acute care, there is a lack of accepted criteria for its definition. Most practitioners regard hypotension as undesirable even in situations that pose no immediate threat to life, but hypotension does not always lead to unfavourable outcomes based on experience and evidence. Thus efforts are needed to better understand the causes, consequences, and treatments of hypotension. This narrative review focuses on the heterogeneous underlying pathophysiological bases of hypotension and their impact on organ perfusion and patient outcomes. We propose the iso-pressure curve with hypotension and hypertension zones as a way to visualize changes in blood pressure. We also propose a haemodynamic pyramid and a pressure–output–resistance triangle to facilitate understanding of why hypotension can have different pathophysiological mechanisms and end-organ effects. We emphasise that hypotension does not always lead to organ hypoperfusion; to the contrary, hypotension may preserve or even increase organ perfusion depending on the relative changes in perfusion pressure and regional vascular resistance and the status of blood pressure autoregulation. Evidence from RCTs does not support the notion that a higher arterial blood pressure target always leads to improved outcomes. Management of blood pressure is not about maintaining a prespecified value, but rather involves ensuring organ perfusion without undue stress on the cardiovascular system.
Keywords: autoregulation, blood pressure, hypotension, organ perfusion, outcome, pathophysiology, perfusion
Editor's key points.
-
•
Hypotension has heterogenous underlying pathophysiological causes and organ-specific effects on tissue perfusion.
-
•
Hypotension does not always lead to organ hypoperfusion; in fact, it may not affect or may even increase organ perfusion.
-
•
The overall evidence from RCTs does not support the notion that a higher blood pressure target always leads to improved patient outcomes.
Arterial BP is perhaps the most commonly measured haemodynamic variable. It can increase or decrease acutely to produce hypertension or hypotension, respectively. Although the terms hypertension and hypotension have long been in use, widely accepted criteria defining them in acute care, including in the perioperative, intensive care, and emergency settings, have not been established. This is exemplified by the fact that although the diagnostic criteria for chronic hypertension are defined in chronic care,1,2 although diagnostic criteria have recently been revised,3similar clearly defined criteria for acute hypertension in acute care do not exist (but see Sessler and colleagues4 for recent efforts to establish such criteria). This review focuses on the discussion of acute hypotension, which is a more frequent occurrence than acute hypertension in acute care.
Hypotension currently lacks widely accepted criteria for diagnosis in acute care.5,6 A cohort study showed that both the threshold used to define hypotension and the method chosen to quantify hypotension affect the association between intraoperative hypotension and outcomes.7 This finding suggests that intraoperative hypotension studies based on different methodologies are not comparable and that it is challenging to apply the reported results in clinical practice. Although hypotension does not always appear to be hazardous based on both clinical experience and available evidence, most practitioners still regard it as undesirable, even in situations that pose no immediate threat to life. This incongruity implies that we may need to reflect on the fundamentals of hypotension, including its underlying pathophysiology and critical impact. Clarification of these fundamentals may improve our understanding of acute hypotension in acute care.
Hypotension and outcomes based on cohort studies
Most cohort studies show a consistent association between acute hypotension and unfavourable outcomes in acute care.8,9 For example cohort studies performed in noncardiac non-neurologic surgical patients show an association between perioperative hypotension and unfavourable outcomes, namely mortality,10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 all-cause morbidity,26 acute kidney injury,27, 28, 29, 30, 31, 32 myocardial injury,11,19,27,29,30,33, 34, 35, 36, 37, 38, 39 congestive heart failure,40 stroke,25,39,41 cognitive decline,42 delirium,43 poor liver8 and kidney44 graft function, and post-oesophagectomy leak.45 However, there are exceptions in which no association between hypotension and unfavourable outcomes was found for noncardiac non-neurologic surgical patients.46, 47, 48, 49, 50 Similarly, most cohort studies performed in cardiac surgical patients involving cardiopulmonary bypass show an association between perioperative hypotension and increased mortality,51,52 major morbidity,52 watershed stroke,53 early cognitive dysfunction,54 postoperative delirium,55 and acute kidney injury.56, 57, 58 However, there are exceptions in this patient population as well: one study failed to associate hypotension with postoperative delirium,59 and three studies failed to associate hypotension with acute kidney injury.60, 61, 62
The results of these cohort studies should be interpreted in light of their inherent limitations. The first limitation is related to the variety of thresholds used to define hypotension and the methods chosen to quantify the accumulative effects of hypotension (i.e. the exposure).5,7 The variety in exposure definitions affects the results of the association between intraoperative hypotension and outcomes.7 Moreover, the baseline BP used in retrospective studies might be unreliable as BP has a circadian fluctuation63 and also tends to be higher in clinical/hospital settings (white coat hypertension).64 The second limitation is related to the definition of outcomes. The outcomes, defined retrospectively, were not pre-specified, leading to variations in the timing, criteria, validity, relevance, and availability of the different outcome measures. The third limitation is related to confounder control. Hypotension has different underlying pathophysiological causes and effects on organ perfusion (see below), and organ perfusion, not the blood pressure per se, determines outcomes relevant to haemodynamics. Cohort studies investigating intraoperative hypotension do not normally consider flow/perfusion-related information (owing to the lack of routine measurement); therefore, these studies could be confounded by this unmeasured yet critical information. How hypotension is treated could also confound cohort studies because different treatments, although they may all increase BP, may have different effects on organ perfusion and other variables.65
Hypotension and outcomes based on randomised controlled trials
Among studies investigating the relationship between hypotension and outcomes, there is a conspicuous discrepancy between evidence based on cohort studies and evidence based on RCTs. Although an abundance of cohort studies have suggested an association between perioperative hypotension and unfavourable outcomes,4 RCTs have failed to demonstrate consistently improved outcomes from maintaining a higher BP (Table 1).66, 67, 68, 69, 70, 71, 72, 73 Assessing this body of evidence in surgical patients is limited by: (1) different surgeries, (2) different BP targets and different BP-related interventions, (3) different outcome measures, and (4) different flow/perfusion (including pump flow during cardiopulmonary bypass). In patients with septic shock requiring resuscitation, there was no significant difference in mortality between strategies targeting a higher (80–85 mm Hg) or lower (65–70 mm Hg) MAP.74 In critically ill older patients with vasodilatory hypotension, there was no significant difference in mortality between permissive hypotension (targeting an MAP of 60–65 mm Hg) and usual care (targeting a higher BP).75 These inconsistent findings, albeit likely to have multifactorial causes, suggest that we may need an improved approach toward understanding hypotension, including its definition, pathophysiology, and effects on organ perfusion and patient outcomes, in acute care. In other words, BP management is not as simple as merely targeting a prespecified BP value.
Table 1.
RCTs comparing a higher BP target with a lower BP target in perioperative care. ∗Early termination. CABG, coronary artery bypass grafting; CPB, cardiopulmonary bypass; DWI, diffusion-weighed magnetic resonance imaging.
| Year (Authors) | Surgery | Patients (n) | Higher BP target | Lower BP target | Outcomes | Conclusion |
|---|---|---|---|---|---|---|
| Noncardiac surgery | ||||||
| 1999 (Williams-Russo and colleagues)73 | Hip surgery under epidural anaesthesia | 235 | MAP=55–70 mm Hg | MAP=45–55 mm Hg | Cognitive, cardiac and renal complications | No difference |
| 2016 (Carrick and colleagues)66,∗ | Laparotomy or thoracotomy for trauma | 168 | MAP=65 mm Hg | MAP=50 mm Hg | 30 day mortality | No difference |
| 2017 (Futier and colleagues)67 | Major abdominal surgery | 292 | SBP=90–110% of resting value | SBP >80 mm Hg or 60% of resting value | A composite of systemic inflammatory response syndrome and organ dysfunction by day 7 after surgery | A higher BP target is beneficial |
| Cardiac surgery | ||||||
| 1995 (Gold and colleagues)68 | CABG with CPB | 248 | MAP=80–100 mm Hg during CPB | MAP=50–60 mm Hg during CPB | Mortality, cardiac, neurologic, and cognitive complications, and changes in quality of life | A higher MAP during CPB is beneficial |
| 2007 (Charlson and colleagues)70 | CABG with CPB | 412 | MAP target=80 mm Hg during CPB | MAP target=pre-bypass level during CPB | Mortality, major neurologic or cardiac complications, cognitive complications or deterioration in functional status | No difference |
| 2011 (Siepe and colleagues)69 | CABG with CPB | 92 | MAP=80–90 mm Hg during CPB | MAP=60–70 mm Hg during CPB | Early postoperative cognitive dysfunction and delirium | A higher MAP during CPB is beneficial |
| 2014 (Azau and colleagues)71 | Cardiac surgery with CPB | 300 | MAP=75–85 mm Hg during CPB | MAP=50–60 mm Hg during CPB | Acute kidney injury | No difference |
| 2018 (Vedel and colleagues)72 | Cardiac surgery with CPB | 197 | MAP=70–80 mm Hg during CPB | MAP=40–50 mm Hg during CPB | Cerebral infarcts detected by DWI | No difference |
Nature of blood pressure
Understanding the nature of BP helps to clarify when and why hypotension is worrisome. BP is the force exerted by the circulating blood that propels blood through the tissues and organs, that is organ perfusion, especially to the brain because it is at a higher level relative to the heart in sitting or standing individuals. Higher BP is required for the increased height difference between the brain and heart, as illustrated by the remarkably different baseline BP between standing giraffes and humans (systolic BP, ~300 vs ~120 mm Hg).76
Hypotension has different underlying pathophysiological mechanisms
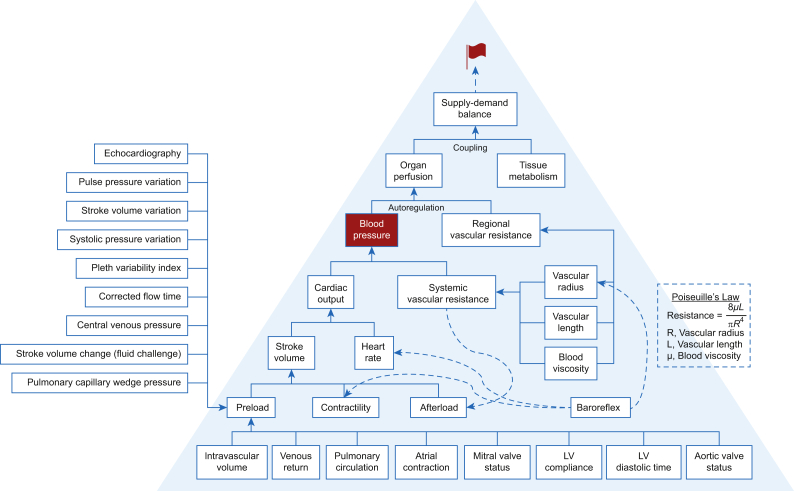
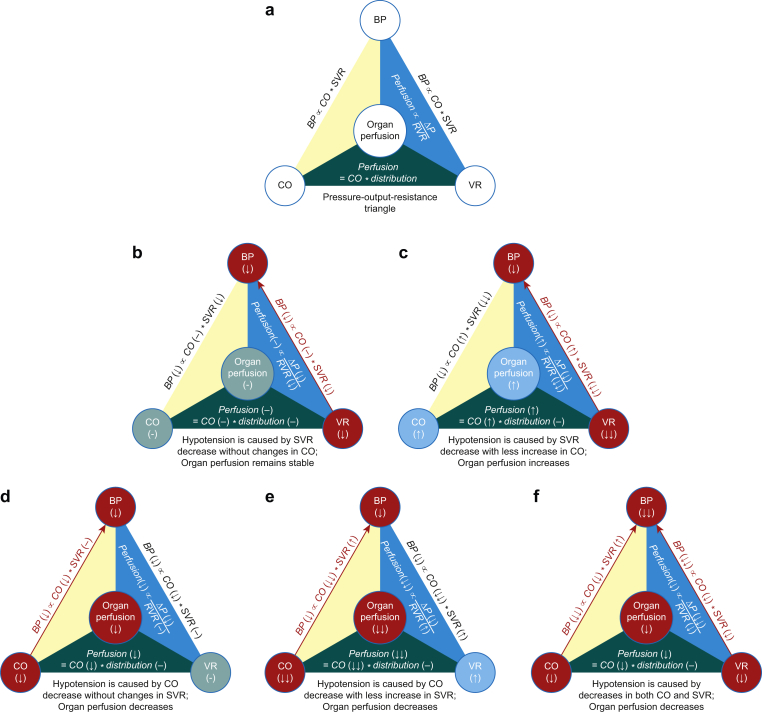
Arterial blood pressure is the result of multiple haemodynamic elements (Fig. 1).77 Therefore, hypotension is not always equivalent because it can have different underlying pathophysiological mechanisms as a result of different combinations of changes in relevant factors. The variety of potential underlying pathophysiological mechanisms based on the haemodynamic pyramid framework is presented in Figure 1. However, we use a simpler pressure–output–resistance triangle framework that regards BP as the product of cardiac output (CO) and systemic vascular resistance (SVR) (Fig. 2a).
Fig 1.
Haemodynamic pyramid. Venous blood must return to the heart and flow through the right heart, pulmonary vasculature, left atrium, and mitral valve to create the preload of the left ventricle. The magnitude of left ventricle preload is also dependent on atrial contraction, mitral valve status, aortic valve status (e.g. aortic valve regurgitation leading to augmented preload), and the compliance and diastolic time of the left ventricle. The magnitude of stroke volume is dependent on preload, myocardial contractility, and afterload. Blood pressure is dependent on cardiac output and systemic vascular resistance (SVR), whereas cardiac output is the product of stroke volume and heart rate. Afterload and SVR are related. SVR is proportional to the vascular length and blood viscosity and inversely proportional to vascular radius to the fourth power, a relationship described by the Hagen–Poiseuille equation. Organ perfusion is dependent on blood pressure (or perfusion pressure) and regional vascular resistance (RVR). The relationship between organ perfusion pressure and RVR is governed by pressure autoregulation. The match between organ perfusion and tissue metabolic activity determines perfusion adequacy and is one of the premises of organ well-being. Adequate organ perfusion is the primary goal of haemodynamic management. Baroreflex exerts its effects primarily on the vascular radius, heart rate, and myocardial contractility. Blood pressure (highlighted in red fonts) and heart rate are always monitored in acute care. The modern haemodynamic monitor enables the assessment of stroke volume and thus cardiac output or index. Tissue oximetry based on near-infrared spectroscopy enables assessing the balance between tissue oxygen consumption and supply. A variety of means and parameters assesses preload. Modern haemodynamic management has a variety of approaches with likely different effectiveness depending on the outcomes of interest.77, 78, 79 LV, left ventricle.
Fig 2.
The pressure–output–resistance triangle. Organ perfusion is in the centre of the triangle. This diagram is based on the following premises: (1) changes in systemic vascular resistance (determinant of blood pressure) and regional vascular resistance (determinant of organ perfusion) are concordant, and (2) the share of cardiac output among various organs remains stable. Blood pressure is proportional to cardiac output and systemic vascular resistance. Organ perfusion is proportional to perfusion pressure and inversely proportional to regional vascular resistance; it is also a percentage share of cardiac output (a). Hypotension can be caused by a decrease in systemic vascular resistance (close red circle and red arrow), and in this case, organ perfusion remains stable because of the proportional decreases in blood pressure and regional vascular resistance (b). Hypotension can be caused by a significant decrease in systemic vascular resistance (closed red circle and red arrow), although there is a lesser degree of increase in cardiac output (closed blue circle). In this case, organ perfusion is increased because of the lesser decrease in blood pressure than the decrease in regional vascular resistance (c). Hypotension can be caused by a decrease in cardiac output (closed red circle and red arrow), and in this case, organ perfusion is decreased because of decreased perfusion pressure in the face of an unchanged regional vascular resistance (d). Hypotension can be caused by a significant decrease in cardiac output (closed red circle and red arrow), although there is a lesser degree of increase in systemic vascular resistance (closed blue circle). In this case, organ perfusion has a significant decrease because of decreased perfusion pressure in the face of an increased regional vascular resistance (e). Hypotension can be caused by simultaneous decreases in cardiac output and systemic vascular resistance (closed red circles and red arrows). In this case, organ perfusion is decreased because of the more significant decrease in perfusion pressure than the decrease in regional vascular resistance (f). CO, cardiac output; VR, vascular resistance which can be either SVR (systemic vascular resistance) or RVR (regional vascular resistance) depending on the context; ΔP, perfusion pressure.
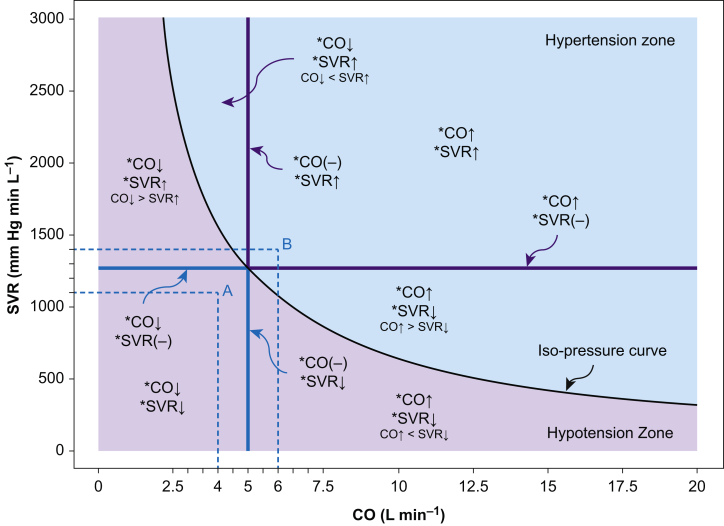
BP is determined primarily by stroke volume (or CO) and SVR at a given filling pressure, for example central venous pressure (CVP); the relationship among these variables is governed by the equation (Fig. 3).80 Thus BP can be the same for different CO and SVR values as long as the CO-SVR products are the same. For a constant CO-SVR product, the curve formed by different CO and SVR pairs (with different values) is referred to here as the iso-pressure curve (Fig. 3). The areas below and above the iso-pressure curve are referred to as the hypotension and hypertension zones, respectively (Fig. 3). The concepts of the iso-pressure curve and the hypotension and hypertension zones are explained in Figure 3. Hypotension has the following five exclusive underlying pathophysiological mechanisms based on different changes in CO and SVR (Fig 2, Fig 3):
-
•
SVR decreases whereas CO remains stable (Fig. 2b).
-
•
SVR decreases whereas CO increases, but the effect of the SVR decrease exceeds the effect of the CO increase (Fig. 2c).
-
•
CO decreases whereas SVR remains stable (Fig. 2d).
-
•
CO decreases whereas SVR increases, but the effect of the CO decrease surpasses the effect of the SVR increase (Fig. 2e).
-
•
Both CO and SVR decrease (Fig. 2f).
Fig 3.
Hypotension and hypertension zones divided by the iso-pressure curve. The abscissa indicates CO, and the ordinate indicates SVR. The following equation governs the relationship among different systemic haemodynamic variables: . The black curve is the iso-pressure curve; for a given pair of CO and SVR values, as long as the CO–SVR product equals the difference of MAP and CVP times 80, the point determined by the CO–SVR pair falls on the iso-pressure curve. In this case, we assume MAP is 85 mm Hg and the CVP is 5 mm Hg to exemplify the concept; the point representing a CO of 5 L min−1 and an SVR of 1280 mm Hg min L−1 falls on the black iso-pressure curve because the CO-SVR product equals the MAP–CVP difference times 80. The left lower purple area is called the hypotension zone because any point in this area, no matter what CO and SVR values it presents, leads to a smaller MAP–CVP difference than the MAP-CVP difference dictating the iso-pressure curve. For example, point A, determined by a CO of 4 L min−1 and an SVR of 1100 mm Hg min L−1, corresponds to a MAP–CVP difference of approximately 55 mm Hg; if assuming CVP equals 5 mm Hg, MAP is 60 mm Hg in this example. The combinations of different CO and SVR changes represent different underlying pathophysiologies of hypotension. The right upper blue area is called the hypertension zone because any point in this area, no matter what CO and SVR values it represents, leads to a larger MAP–CVP difference than the MAP–CVP difference dictating the iso-pressure curve. For example, point B, determined by a CO of 6 L min−1 and an SVR of 1400 mm Hg min L−1, corresponds to a MAP–CVP difference of approximately 105 mm Hg; if assuming CVP equals 5 mm Hg, the MAP is 110 mm Hg in this example. The combinations of different CO and SVR changes represent different underlying pathophysiologies of hypertension. CO, cardiac output; SVR, systemic vascular resistance; CVP, central venous pressure.
Although each of these mechanisms leads to hypotension, they have different impacts on organ perfusion, as discussed in the following section.
This simplified approach should not distract our attention from the causes of changes in CO and SVR as they themselves have different determinants (Fig. 1). CO is the product of HR and stroke volume (SV), with SV dependent on preload, myocardial contractility, and afterload. SVR is determined by the vascular radius, vascular length, and blood viscosity. Clinically, interventions such as the administration of vasopressors,65 beta-adrenergic antagonists,81 and calcium channel blockers82 and the use of pacemakers,83 can lead to changes in these haemodynamic aspects, and therefore BP changes.
Organ-specific impact of hypotension on perfusion
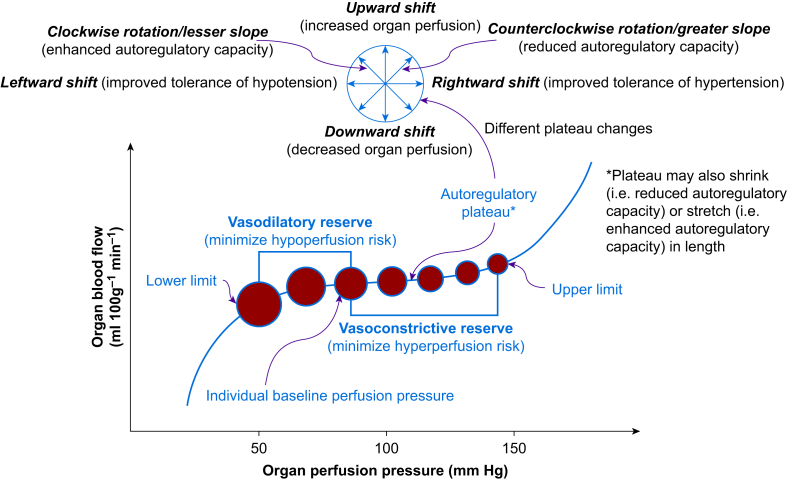
Hypotension, although usually leading to decreased perfusion pressure, does not always lead to organ hypoperfusion because organ perfusion is determined by the perfusion pressure divided by the regional vascular resistance (RVR). Based on Poiseuille's law, RVR is determined by the vascular radius, vascular length, and blood viscosity, although the vascular length rarely changes clinically. Multiple factors can change the vascular radius or vasomotor tone, for example age, atherosclerosis, blood pressure, hypercapnia, and vasoactive drugs (to name a few), and thus lead to RVR changes. The change in vasomotor tone secondary to a change in perfusion pressure is mediated by the myogenic mechanism and is the foundation of the pressure-dependent autoregulation of organ blood flow (Fig. 4). Depending on the relative direction and magnitude of changes in RVR as compared with perfusion pressure, hypotension can have the following three effects on organ perfusion:
-
•
Organ perfusion remains stable if the effects of the decreases in perfusion pressure and RVR are comparable, a scenario in which the underlying pathophysiology of hypotension is an SVR decrease without changes in CO (Fig. 2b). This impact is consistent with the conventional concept of pressure autoregulation, as discussed in the following section.
-
•
Organ perfusion increases if the effect of the perfusion pressure decrease is less than that of the RVR decrease, a scenario in which hypotension is secondary to an SVR decrease accompanied by a lesser degree of CO increase (Fig. 2c), as exemplified by the use of certain calcium channel blockers.82
-
•
Organ perfusion decreases if perfusion pressure decreases in the face of one of the following changes in RVR: (1) an unchanged RVR – that is a scenario in which the underlying pathophysiology of hypotension is a CO decrease without changes in SVR (Fig. 2d); (2) an increased RVR – that is a scenario in which hypotension is secondary to a CO decrease accompanied by a lesser degree of SVR increase (Fig. 2e); or (3) a decreased RVR, with the degree of the RVR decrease less than that of the perfusion pressure decrease – a scenario in which hypotension is secondary to a decrease in both CO and SVR (Fig. 2f).
Fig 4.
Pressure autoregulation of organ perfusion. The abscissa represents organ perfusion pressure whereas the ordinate represents organ blood flow. The relationship between organ perfusion pressure and blood flow is depicted by the autoregulation curve (blue curve), with the lower limit, upper limit, and plateau indicated. Organ blood flow remains relatively stable via active vasodilation or vasoconstriction (indicated by the closed red circles with different sizes) when organ perfusion pressure falls within the range between the lower and upper limits (i.e. the plateau). Each individual has a baseline blood pressure, and thus, a baseline perfusion pressure for each organ. When organ perfusion pressure decreases, organ vasculature responsible for flow resistance dilates to minimise hypoperfusion/ischaemia (vasodilatory reserve); otherwise, when organ perfusion pressure increases, organ vasculature responsible for flow resistance constricts to minimise hyperperfusion (vasoconstrictive reserve). The capacity of pressure autoregulation is organ-dependent. Multiple factors can affect the position and shape of the autoregulatory curve, as indicated by the compass.84
The overarching message is that hypotension does not inevitably lead to a decrease in organ perfusion; instead, its impact on organ perfusion is dependent on the direction of the change in RVR (i.e. no change, increase, or decrease) and, when RVR decreases, on the relative decrease in RVR in comparison with the decrease in perfusion pressure. The lack of organ perfusion appraisal may be a reason for the inconsistent results among the abovementioned studies investigating the relationship between hypotension and outcomes in acute care. After all, these studies were based on outcomes that were largely determined by organ perfusion.
Organ blood flow regulation
Organ blood flow regulation can be better explained at the level of tissue microcirculation. The regulation of tissue microcirculation takes place at the level of arterioles where capillary perfusion starts.85 Arterioles can dilate and constrict thanks to the smooth muscle in the arteriolar wall, which leads to changes in the arteriolar radius. This is a much more robust and efficient way of flow resistance adjustment compared with changes in vascular length or blood viscosity, because resistance is inversely proportional to vascular radius to the fourth power, but only directly proportional to vascular length and blood viscosity to the first power, per Poiseuille's law. Multiple factors regulate tissue perfusion via arteriolar dilation and constriction, including (1) perfusion pressure (i.e. pressure autoregulation), (2) the autonomic nervous system, (3) circulating hormones, (4) local metabolic activity, (5) endothelial products, and (6) flow-mediated diameter changes.85 The amalgamation of the effects exerted by these vasomotor tone modulators sets the flow resistance and regulates downstream capillary perfusion.
The capillary bed itself can also regulate its own perfusion. Endothelial cells possess contractile fibres and are able to regulate their volume in response to external stimuli.86 Evidence also suggests that capillaries respond to changes in BP, such that capillary diameter decreases during hypotension to the extent that red blood cell transit stops.87
Pressure autoregulation, which maintains relatively stable organ perfusion despite fluctuating perfusion pressure, is just one mechanism of organ blood flow regulation (Fig. 4).84,88,89 Viewing pressure autoregulation in the context of non-pressure regulatory mechanisms can be perplexing. There are two ways to consider the interplay between pressure autoregulation and non-pressure regulatory mechanisms. One way is to regard them as coexisting or parallel mechanisms, with organ perfusion as the end result of their summation. The other way is to consider non-pressure regulatory mechanisms as factors that modulate pressure autoregulation89; for example hypercapnia (i.e. a metabolite) regulates pressure autoregulation by shortening the plateau and shifting it upwards.88 Besides the interplay with non-pressure regulatory mechanisms, pressure autoregulation is also affected by physiological factors (e.g. age), chronic disease (e.g. hypertension and atherosclerosis), acute illness (e.g. traumatic brain injury), anaesthetics (e.g. sevoflurane), and drugs (e.g. calcium channel blockers).84 Moreover, different organs have different pressure autoregulation capacities, and what are commonly considered vital organs (brain, heart, and kidney) are equipped with robust autoregulatory capacities.84 Pressure autoregulation renders mammals, and especially their vital organs, more tolerant to acute hypotension and hypertension. During hypotension, the stable organ perfusion rendered by pressure autoregulation is consistent with the scenario described in Figure 2b (comparable reductions in perfusion pressure and RVR).
During sepsis and shock, macrocirculation and microcirculation are uncoupled despite the presence of normalised systemic haemodynamic variables.90 This concept is supported by the finding that sublingual capillary microvascular flow and the percentage of perfused capillaries remain unchanged despite an increase of MAP from 65 to 85 mm Hg using vasopressor infusion in septic shock patients.91,92 Microcirculatory dysfunction and mitochondrial depression are prominent pathophysiological features underlying the conditions of sepsis and shock and are responsible for refractory regional hypoxia and oxygen extraction deficit despite the correction of global oxygen delivery variables.93 Whether therapies aimed at microcirculation recruitment, such as using nitric oxide donors to open the hypoperfused capillary bed or increasing the opening pressure of microcirculation, or goal-directed therapy of microcirculation guided by tissue oxygen monitoring,94 improve outcomes remains to be determined.95
Importance of cardiac output to organ perfusion
The preceding discussion highlighted that CO is not only a determinant of BP but also associates with organ perfusion. Although BP decreases in every scenario, organ perfusion likely remains stable when CO remains stable (Fig. 2b), organ perfusion likely increases when CO increases (Fig. 2c), and organ perfusion likely decreases when CO decreases (Fig. 2d–f). This observation can be better comprehended if viewing organ perfusion as a percentage share of CO because CO is ultimately distributed to various tissues and organs and the summation of their perfusion shares equals CO.89 This view of the relationship between CO and organ perfusion enriches the traditional view regarding organ perfusion as the perfusion pressure divided by the RVR. It also highlights the importance of monitoring and maintaining CO when the ultimate goal is to ensure organ perfusion. However, we caution that this view of the relationship between CO and organ perfusion may not be applicable in conditions such as sepsis and shock, where microcirculatory dysfunction and the macrocirculation–microcirculation uncoupling are prominent features.
There is evidence suggesting the importance of maintaining CO in noncardiac surgical patients. In older adults (mean age 72 yr) with comorbid conditions undergoing elective total hip surgery with epidural anaesthesia, maintaining intraoperative MAP in the range of 45–55 mm Hg or 55–70 mm Hg did not lead to different outcomes (cognitive, cardiac, renal, and thromboembolic complications).73 One potential explanation for this result was the maintained CO in patients from both groups because all patients received a low-dose i.v. epinephrine infusion. Other studies showed that epinephrine infusion at rates of 1–5 μg min−1 preserves or augments CO despite significant hypotension.96,97 In high-risk patients aged 50 yr or older undergoing major gastrointestinal surgery, an RCT of the effects of usual care or perioperative CO-guided haemodynamic management on a composite of predefined 30 day moderate or major complications and mortality98 showed that CO-guided management through targeting a maximal SV via i.v. colloid infusion with a fixed low-dose dopexamine infusion (0.5 μg kg−1 min−1) led to reduction in the primary outcome (36.6%) compared with usual care (43.4%), although this difference did not reach a statistical significance (P=0.07).98
The importance of CO in organ perfusion was corroborated by an RCT performed in cardiac surgical patients,72 which showed that, targeting a higher MAP (70–80 mm Hg), compared with targeting a lower MAP (40–50 mm Hg), during cardiopulmonary bypass did not lead to significantly different volumes or numbers of new cerebral infarcts.72 A 40–50 mm Hg MAP is equivalent to a 30–40 mm Hg cerebral perfusion pressure assuming an intracranial pressure of 10 mm Hg (i.e. cerebral perfusion pressure equals MAP – intracranial pressure). A cerebral perfusion pressure of 30–40 mm Hg is much lower than 65 mm Hg, the widely quoted lower limit of cerebral autoregulation.88 Therefore, not seeing a worse cerebral outcome associated with this dangerously low MAP is counterintuitive. Amidst this perplexity, the most plausible explanation is how the pump flow (the equivalent of CO during cardiopulmonary bypass) was managed: it was fixed at 2.4 L min−1 m−2 irrespective of the target MAP. Therefore, if the pump flow's distribution to the brain remained unchanged, the brain would not become ischaemic despite a much lower MAP.
In contrast, an RCT performed in patients undergoing moderate-risk abdominal surgery showed that cardiac index and pulse pressure variation-guided haemodynamic therapy, on top of MAP-guided therapy, did not lead to improved composite outcomes compared with MAP-guided therapy only.99 There are several explanations for this finding. First, the intervention protocols (i.e. exposures) were not distinctively different between the groups. The end result of cardiac index and pulse pressure variation-guided care was the maintenance of the targeted BP via informed intravascular volume management; however, the same BP was also targeted and accomplished in the control group. Second, the composite outcome included complications with different severities and different relevance to haemodynamics, which may decrease the power of detecting a between-group difference.100 Third, the patients were undergoing moderate-risk abdominal surgery, and thus may have benefited from advanced haemodynamic therapy differently compared with patients undergoing high-risk surgeries.101 However a recent sub-analysis of the Crystalloid–Colloid Study found that the worse outcomes associated with hypotension were independent of cardiac index in noncardiac surgery patients.102
Proposed definition and classification of hypotension
In light of the preceding discussion, hypotension is a systemic haemodynamic abnormality, defined as a measured blood pressure that is lower than a prespecified threshold, that is directly caused by changes in CO, SVR, or both, and that may or may not lead to organ and tissue hypoperfusion. There are different working definitions of hypotension; we advocate a definition that is easy to apply and relevant to patient outcomes. Thus different hypotension criteria should be established for different patient populations.4,8
In light of the different effects of hypotension on organ perfusion, we propose further classification of hypotension as (1) concerning: hypotension that leads to decreased organ perfusion; (2) possibly concerning: does not lead to decreased organ perfusion; and (3) questionable: the impact on organ perfusion cannot be confidently determined. Although a number conventionally defines hypotension, the perfusion/demand match defines whether or not hypotension is concerning.
Organ perfusion assessment
Reliable assessment of organ perfusion facilitates hypotension management in acute care. However, organ perfusion assessment is challenging in clinical practice as no monitor exists that can directly quantify the blood flow to a specific organ. Instead, indirect methods are currently used for organ perfusion assessment (Supplementary Table S1). Signs and symptoms occur because of organ ischaemia, such as chest pain during myocardial ischaemia and dizziness during cerebral ischaemia; these are commonly used clinically for organ perfusion assessment. Monitoring and laboratory studies are available for diagnosing organ ischaemia with varying sensitivities and specificities, such as changes in electrocardiography and troponin elevation for myocardial ischaemia. An emerging technology is tissue oximetry based on near-infrared spectroscopy, which assesses the balance between tissue oxygen consumption and supply in the tissue bed illuminated by near-infrared lights.65,103 This monitor is noninvasive, continuous, portable, and can be applied to different organs.65,104,105 However, tissue oxygenation measured by near-infrared spectroscopy reflects tissue perfusion only when tissue metabolic rate of oxygen remains relatively stable.106 Other technologies, such as sidestream darkfield imaging91 and orthogonal polarisation spectral imaging,107 have also been used for microcirculation assessment.
Clinical scenarios involving hypotension
These examples highlight the complexity of real-world practice and underline the importance of the critical appraisal of hypotension in acute care.
Beta blocker-related hypotension
Perioperative use of beta blockers in noncardiac surgical patients is associated with increased incidence of hypotension.25,108,109 Reduced CO secondary to reduced HR and SV is primarily responsible for beta blocker-related hypotension, especially when using beta blockers that do not have intrinsic sympathomimetic activity.111 Although there may be a decrease in coronary perfusion pressure because of hypotension, beta blockers may augment coronary blood flow by increasing diastolic perfusion time via HR slowing112 or by coronary vasodilation.113 The level I recommendation for initiating oral beta blockers within the first 24 h in patients with non-ST-elevation acute coronary syndromes in the absence of heart failure, low-output state, risk of cardiogenic shock, or other contraindications highlights beta blockers' beneficial effect on the myocardial metabolic demand–supply balance.114 Propranolol can significantly reduce cerebral perfusion pressure and cerebral blood flow, although it also reduces cerebral metabolic rate of oxygen in baboons.115 In contrast, use of labetalol, metoprolol, oxprenolol, and sotalol did not lead to significant changes in cerebral blood flow in hypertensive patients.116 Perioperative use of beta blockers initiated 1 day or less before noncardiac surgery reduces non-fatal myocardial infarction but increases the risk of stroke and death.25,109 The role of hypotension in this outcome remains unclear.
Nicardipine-related hypotension
Nicardipine is widely used as an antihypertensive drug in acute care because of its efficiency, predictability, and titratability.82 Although it is a powerful arteriodilator and afterload/SVR/RVR modulator, nicardipine does not typically decrease preload or adversely affect myocardial contractility.82,117, 118, 119, 120 It increases CO because of an increase in HR and SV.82,117, 118, 119, 120 Nicardipine augments organ perfusion, as evidenced by increased coronary,119,120 cerebral,121 renal,122 vertebral,122 and skeletal muscle blood flow.82 In the face of decreased BP, the increased organ perfusion suggests that the degree of RVR decrease exceeds the degree of BP decrease (Fig. 2c). Whether nicardipine's haemodynamic profile leads to improved outcomes remains to be determined.
Hypotension related to angiotensin converting enzyme inhibitors or angiotensin II receptor blockers
Observational studies suggest that continuing angiotensin converting enzyme inhibitors (ACEIs) on the day of surgery poses an increased risk of intraoperative hypotension.123 Although some studies show a relatively stable CO,124,125 a meta-analysis noted a CO increase after ACEIs/angiotensin II receptor blockers (ARBs) administration,126 and there is evidence supporting both withholding127 and continuation128,129 of ACEIs/ARBs before surgery. A meta-analysis based on five RCTs and four cohort studies failed to demonstrate an association between perioperative use of ACEIs/ARBs and mortality or major cardiac events.123 The 2014 American College of Cardiology/American Heart Association guidelines recommend continuing these treatments throughout the perioperative period.130 Although continuation of ACEIs/ARBs perioperatively is associated with increased risk of hypotension, the overall evidence at present does not link this to unfavourable outcomes.
Neuraxial block-related hypotension
Hypotension is common after neuraxial block in obstetric and surgical patients. Neuraxial block-related hypotension is caused by a decrease in SVR, not CO. A study of patients undergoing elective Caesarean delivery showed that although systolic BP decreased 7% below baseline, CO increased 19% from baseline 20 min after the neuraxial block.131 In patients undergoing hip surgery under hypotensive epidural anaesthesia (maintaining MAP ≤50 mm Hg while infusing epinephrine to support circulation), an observational study showed that cerebral blood flow velocity was well maintained, despite MAPs well below the commonly accepted lower limit of cerebral autoregulation.132 However, there was considerable inter-individual heterogeneity, with 23% of patients having >20% reduction in cerebral blood flow velocity.133 In patients with severe coronary artery disease, an observational study showed that high thoracic epidural anaesthesia did not change coronary perfusion pressure or myocardial blood flow.133 This study also showed that thoracic epidural block increases the diameter of stenotic, but not non-stenotic, epicardial coronary artery segments.133 In patients with ischaemic heart disease, high thoracic epidural analgesia was able to partly normalise the myocardial blood flow response to sympathetic stimulation.134 When low-dose epinephrine was infused during epidural anaesthesia, patients who had a lower MAP (45–55 mm Hg) did not experience more complications than patients who had a higher MAP (55–70 mm Hg).73 A population-based cohort study, using data from propensity score-matched patients, concluded that epidural anaesthesia is associated with a small reduction in 30 day mortality.135 Therefore, the available evidence suggests that as long as extreme hypotension is avoided, neuraxial block-related hypotension does not appear to be harmful.
Acute anaemia-related hypotension
Acute anaemia leads to increased CO,136 increased cerebral blood flow,137 and increased coronary blood flow138 as a compensatory mechanism to boost oxygen delivery when arterial blood oxygen content is reduced.139 Acute anaemia also decreases blood viscosity and SVR.136 There appears to be an interplay between changes in blood viscosity and changes in CO during acute anaemia.136 Acute anaemia can lead to hypotension depending on the relative changes between CO and SVR. There was initially a concern that co-occurrence of anaemia and hypotension during cardiopulmonary bypass could be associated with an increased risk of postoperative acute kidney injury60; however, this was later refuted by a large cohort study.61 In high-risk patients undergoing hip fracture repair, liberal transfusion (maintaining a haemoglobin >100 g L−1) and restrictive transfusion (maintaining a haemoglobin no >80 g L−1 or keeping the patient free from anaemia-related symptoms) did not lead to different outcomes.140,141 At present, there is no evidence attesting to adverse effects associated with acute anaemia-related hypotension.
Propofol-related hypotension
Hypotension is common after anaesthesia induction using propofol.142 The effects of propofol on haemodynamics are mediated primarily via inhibition of sympathetic nervous activity, as opposed to direct vasomotor tone changes.142 Propofol impairs baroreflex,143 decreases SVR,144 decreases venous return,145 and can reduce CO.144,146 The impact of propofol on organ perfusion varies between brain and other organs. Propofol reduces cerebral perfusion but does not cause ischaemia because of the proportional reduction in cerebral metabolic activity.147, 148, 149 There is a lack of direct evidence on its effects on perfusion of non-brain organs, although indirect evidence suggests that it may not have adverse effects.150 Propofol may cause some degree of CO reduction144,146; however, this may not be consequential. As propofol can cause up to a 30% decrease in cerebral blood flow,147 it is likely that the reduced cerebral perfusion may be mainly responsible for the reduced CO because the brain accounts for up to 20% of CO.151 At present, there is no evidence attesting to an adverse effect exerted by propofol-related hypotension.
Septic shock-related hypotension
Septic shock is characterised by distributive organ hypoperfusion in the face of hypotension, vasodilation, and, frequently, increased CO.152, 153, 154, 155, 156 Several studies have found that when MAP is increased from 65 to 85 mm Hg using norepinephrine infusion in patients with septic shock, CO increases by 8–20%.91,157, 158, 159 However, the increase in CO does not consistently translate into an increase in organ perfusion. Some studies show that norepinephrine infusion, which increased MAP from 65 to 85 mm Hg, did not improve tissue perfusion.91,157,158 In contrast, other studies show that norepinephrine infusion leads to improved tissue perfusion.159,160 Among the multiple potential reasons for this discrepancy, flow redistribution may be responsible for the inconsistent changes in tissue perfusion.161,162 Even though an organ may appear to have sufficient gross perfusion, it can still undergo regional tissue ischaemia and hypoxia because of microcirculatory and mitochondrial dysfunction93 or unmet hypermetabolic activity.163 The challenges of treating haemodynamic abnormalities in septic shock were highlighted by a multicentre RCT,74 which showed that targeting MAP of 80–85 mm Hg, as compared with 65–70 mm Hg, did not lead to differences in mortality at either 28 or 90 days.74 Based on this, septic shock is neither caused by hypotension nor can it be cured by BP-increasing treatment.
Clinical implications
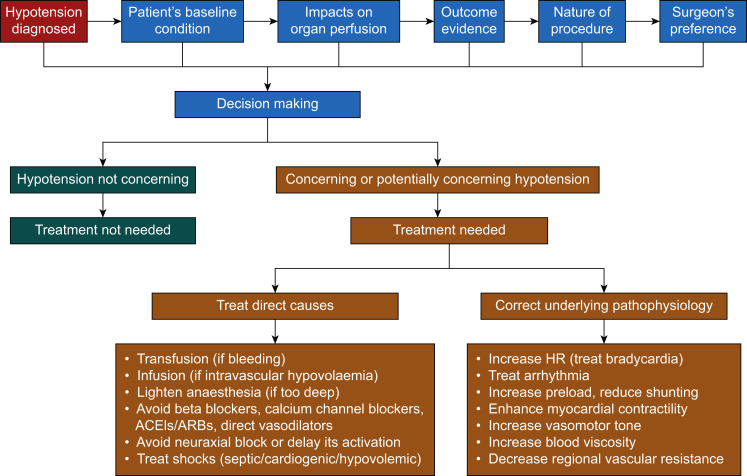
BP is the most common haemodynamic variable monitored in patient care (as a vital sign). Although HR is also monitored (as a vital sign), there is a consensus that it does not provide the same haemodynamic information as BP. The key message of the above discussion is the ‘heterogeneity’ of hypotension effects on underlying pathophysiology and its impact on organ perfusion and outcomes. The clinical management of hypotension follows the axis of diagnosis–decision-making–intervention (Fig. 5); it is critical to remember that the goal is to ensure organ perfusion, not to correct a number.
Fig 5.
The axis of diagnosis–decision-making–intervention for hypotension management. The first step is to diagnose hypotension based on both clinical experience and the available consensus.8 The second step is to decide to treat or not to treat hypotension, which is a complicated decision-making process that needs to take the patient's baseline condition, effects on organ perfusion, outcome evidence, and nature of the procedure. The third step is intervention if the decision is to treat hypotension. The intervention follows two approaches: one is to treat direct causes, and the other is to correct the underlying pathophysiology responsible for hypotension. These two lines of treatment approaches may sometimes overlap. ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker.
The first step in managing hypotension is to determine whether the BP decreases below a prespecified threshold. This can be challenging, as in perioperative care, the thresholds used to define hypotension are primarily experience-based owing to the lack of convincing RCT-based evidence.4,8 In critical care, the criteria for hypotension are also controversial and appear to depend on the patient population. The Surviving Sepsis Campaign recommends an initial target MAP of 65 mm Hg in patients with septic shock requiring vasopressors based on moderate-quality evidence.156 In contrast, patients with acute ischaemic stroke mandate a much higher BP for brain perfusion, although the minimal BP that is acceptable remains to be determined.164,165
The second step in managing hypotension is decision-making, that is deciding whether the diagnosed hypotension requires treatment. The decision-making process must take the patient's baseline condition, the impact on organ perfusion, outcomes evidence, the nature of the procedure, and the surgeon's preference into consideration. This is a complicated process, and there is no single criterion that fits all scenarios. Haemodynamics need to be meticulously managed in patients at risk of organ ischaemia because of either arterial stenotic disease (e.g. coronary artery disease) or the procedure itself (e.g. carotid artery clamping for endarterectomy). If the surgeon insists on lowering BP during signs of organ ischaemia, the situation should be discussed with the surgeon, and an observation should be made regarding whether improving CO or decreasing organ metabolic demand can reverse organ ischaemia. The outcome evidence upon which the decision-making process is based needs to be consistent and free from significant bias and limitations. At present, existing evidence does not consistently support the notion that a higher BP target leads to improved outcomes. Individualised BP management is promising,67 but challenges include what the baseline BP is and how to determine it.
It should be noted that different organs have different perfusion regulation and different tolerance of ischaemia.84 For example the brain cannot tolerate even a few minutes of ischaemia,166 whereas muscle can tolerate up to 2 h of ischaemia, as exemplified by the prevalent use of a tourniquet during limb procedures.167 Therefore, the impact of hypotension on organ perfusion is also organ-dependent, and organs that have poor tolerance of ischaemia should be closely monitored and prioritised in haemodynamic management.84
The third step is intervention if the decision is to correct the hypotension. There are two different lines of approach for treatment of hypotension. One addresses the cause of the hypotension, including – but not limited to – transfusion if there is active bleeding, infusion if there is intravascular volume depletion, lightening anaesthesia if it is too deep, avoiding beta blockers, calcium channel blockers, ACEIs/ARBs, and direct vasodilators, avoiding neuraxial blocks or delaying their activation, and treating septic, cardiogenic, or hypovolaemic shock. The other line is dealing with the haemodynamic changes that lead to hypotension by referring to the haemodynamic pyramid (Fig. 1) and the pressure–output–resistance triangle (Fig. 2). This approach includes the following treatments, depending on patient status: treat bradycardia, treat arrhythmia, increase preload, enhance myocardial contractility, increase vasomotor tone, and increase blood viscosity. The status of intravascular volume and preload can be assessed using dynamic indices, such as pulse pressure variation and stroke volume variation. However, performance of these dynamic indices may vary during hypotension or normotension, which deserves further investigation.
Conclusions
Hypotension has heterogenous underlying pathophysiological mechanisms and effects on organ perfusion and patient outcomes in acute care. Hypotension does not always lead to organ hypoperfusion; in fact, it may not affect or may even increase organ perfusion, depending on the relative changes between the perfusion pressure and the RVR and pressure autoregulation. Available outcome evidence should be interpreted recognising their various biases and limitations. Overall RCT evidence does not support the notion that a higher BP target always leads to improved outcomes. Management of hypotension follows the diagnosis–decision-making–intervention axis, and it is challenging to define hypotension using one threshold for different patient populations under different clinical situations. When dealing with hypotension, it is essential to consider how well the BP is driving organ perfusion rather than focusing on a fixed BP value. To treat or not to treat hypotension is a complicated decision-making process that needs to take into account the patient's baseline condition, effects on organ perfusion, outcome evidence, and the nature of the procedure. Treatment follows two approaches: treating the direct causes or correcting the underlying haemodynamic changes responsible for the hypotension. These two approaches may sometimes overlap. Hence, the focus is on the heterogeneity of hypotension's underlying pathophysiology, effects on organ perfusion and patient outcomes.
Handling editor: Hugh C Hemmings Jr
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bja.2021.06.048.
Declarations of interest
LM receives lecture fees from Edwards Lifesciences.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Williams B., Mancia G., Spiering W., et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 2.Whelton P.K., Carey R.M., Aronow W.S., et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 3.Foëx P., Sear J.W. Implications for perioperative practice of changes in guidelines on the management of hypertension: challenges and opportunities. Br J Anaesth. 2021 doi: 10.1016/j.bja.2021.05.006. Advance Access published on June 11. [DOI] [PubMed] [Google Scholar]
- 4.Sessler D., Bloomstone J.A., Aronson S., et al. Perioperative Quality Initiative consensus statement on intraoperative blood pressure, risk and outcomes for elective surgery. Br J Anaesth. 2019;122:563–574. doi: 10.1016/j.bja.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 5.Bijker J.B., van Klei W.A., Kappen T.H., van Wolfswinkel L., Moons K.G., Kalkman C.J. Incidence of intraoperative hypotension as a function of the chosen definition: literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology. 2007;107:213–220. doi: 10.1097/01.anes.0000270724.40897.8e. [DOI] [PubMed] [Google Scholar]
- 6.Brady K.M., Hudson A., Hood R., DeCaria B., Lewis C., Hogue C.W. Personalizing the definition of hypotension to protect the brain. Anesthesiology. 2020;132:170–179. doi: 10.1097/ALN.0000000000003005. [DOI] [PubMed] [Google Scholar]
- 7.Vernooij L.M., van Klei W.A., Machina M., Pasma W., Beattie W.S., Peelen L.M. Different methods of modelling intraoperative hypotension and their association with postoperative complications in patients undergoing non-cardiac surgery. Br J Anaesth. 2018;120:1080–1089. doi: 10.1016/j.bja.2018.01.033. [DOI] [PubMed] [Google Scholar]
- 8.Meng L., Yu W., Wang T., Zhang L., Heerdt P.M., Gelb A.W. Blood pressure targets in perioperative care. Hypertension. 2018;72:806–817. doi: 10.1161/HYPERTENSIONAHA.118.11688. [DOI] [PubMed] [Google Scholar]
- 9.Maheshwari K., Nathanson B.H., Munson S.H., et al. The relationship between ICU hypotension and in-hospital mortality and morbidity in septic patients. Intensive Care Med. 2018;44:857–867. doi: 10.1007/s00134-018-5218-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mascha E.J., Yang D., Weiss S., Sessler D.I. Intraoperative mean arterial pressure variability and 30-day mortality in patients having noncardiac surgery. Anesthesiology. 2015;123:79–91. doi: 10.1097/ALN.0000000000000686. [DOI] [PubMed] [Google Scholar]
- 11.Abbott T.E.F., Pearse R.M., Archbold R.A., et al. A Prospective international multicentre cohort study of intraoperative heart rate and systolic blood pressure and myocardial injury after noncardiac surgery: results of the VISION study. Anesth Analg. 2018;126:1936–1945. doi: 10.1213/ANE.0000000000002560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Monk T.G., Bronsert M.R., Henderson W.G., et al. Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. Anesthesiology. 2015;123:307–319. doi: 10.1097/ALN.0000000000000756. [DOI] [PubMed] [Google Scholar]
- 13.Monk T.G., Saini V., Weldon B.C., Sigl J.C. Anesthetic management and one-year mortality after noncardiac surgery. Anesth Analg. 2005;100:4–10. doi: 10.1213/01.ANE.0000147519.82841.5E. [DOI] [PubMed] [Google Scholar]
- 14.Sessler D.I., Sigl J.C., Kelley S.D., et al. Hospital stay and mortality are increased in patients having a "triple low" of low blood pressure, low bispectral index, and low minimum alveolar concentration of volatile anesthesia. Anesthesiology. 2012;116:1195–1203. doi: 10.1097/ALN.0b013e31825683dc. [DOI] [PubMed] [Google Scholar]
- 15.Sprung J., Abdelmalak B., Gottlieb A., et al. Analysis of risk factors for myocardial infarction and cardiac mortality after major vascular surgery. Anesthesiology. 2000;93:129–140. doi: 10.1097/00000542-200007000-00023. [DOI] [PubMed] [Google Scholar]
- 16.Willingham M.D., Karren E., Shanks A.M., et al. Concurrence of intraoperative hypotension, low minimum alveolar concentration, and low bispectral index is associated with postoperative death. Anesthesiology. 2015;123:775–785. doi: 10.1097/ALN.0000000000000822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pietropaoli J.A., Rogers F.B., Shackford S.R., Wald S.L., Schmoker J.D., Zhuang J. The deleterious effects of intraoperative hypotension on outcome in patients with severe head injuries. J Trauma. 1992;33:403–407. doi: 10.1097/00005373-199209000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Reich D.L., Wood R.K., Jr., Emre S., et al. Association of intraoperative hypotension and pulmonary hypertension with adverse outcomes after orthotopic liver transplantation. J Cardiothorac Vasc Anesth. 2003;17:699–702. doi: 10.1053/j.jvca.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 19.Sessler D.I., Meyhoff C.S., Zimmerman N.M., et al. Period-dependent associations between hypotension during and for four days after noncardiac surgery and a composite of myocardial infarction and death: a substudy of the POISE-2 trial. Anesthesiology. 2018;128:317–327. doi: 10.1097/ALN.0000000000001985. [DOI] [PubMed] [Google Scholar]
- 20.Goldman L., Caldera D.L., Southwick F.S., et al. Cardiac risk factors and complications in non-cardiac surgery. Medicine. 1978;57:357–370. doi: 10.1097/00005792-197807000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Ziser A., Plevak D.J., Wiesner R.H., Rakela J., Offord K.P., Brown D.L. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Anesthesiology. 1999;90:42–53. doi: 10.1097/00000542-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Willingham M., Ben Abdallah A., Gradwohl S., et al. Association between intraoperative electroencephalographic suppression and postoperative mortality. Br J Anaesth. 2014;113:1001–1008. doi: 10.1093/bja/aeu105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White S.M., Moppett I.K., Griffiths R., et al. Secondary analysis of outcomes after 11,085 hip fracture operations from the prospective UK Anaesthesia Sprint Audit of Practice (ASAP-2) Anaesthesia. 2016;71:506–514. doi: 10.1111/anae.13415. [DOI] [PubMed] [Google Scholar]
- 24.Cheng X.Q., Wu H., Zuo Y.M., et al. Perioperative risk factors and cumulative duration of "triple-low" state associated with worse 30-day mortality of cardiac valvular surgery. J Clin Monit Comput. 2017;31:387–395. doi: 10.1007/s10877-016-9856-2. [DOI] [PubMed] [Google Scholar]
- 25.Devereaux P.J., Yang H., Yusuf S., et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008;371:1839–1847. doi: 10.1016/S0140-6736(08)60601-7. [DOI] [PubMed] [Google Scholar]
- 26.Brunaud L., Nguyen-Thi P.L., Mirallie E., et al. Predictive factors for postoperative morbidity after laparoscopic adrenalectomy for pheochromocytoma: a multicenter retrospective analysis in 225 patients. Surg Endosc. 2016;30:1051–1059. doi: 10.1007/s00464-015-4294-7. [DOI] [PubMed] [Google Scholar]
- 27.Salmasi V., Maheshwari K., Yang D., et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology. 2017;126:47–65. doi: 10.1097/ALN.0000000000001432. [DOI] [PubMed] [Google Scholar]
- 28.Sun L.Y., Wijeysundera D.N., Tait G.A., Beattie W.S. Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology. 2015;123:515–523. doi: 10.1097/ALN.0000000000000765. [DOI] [PubMed] [Google Scholar]
- 29.Walsh M., Devereaux P.J., Garg A.X., et al. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology. 2013;119:507–515. doi: 10.1097/ALN.0b013e3182a10e26. [DOI] [PubMed] [Google Scholar]
- 30.Charlson M.E., MacKenzie C.R., Gold J.P., Ales K.L., Topkins M., Shires G.T. Intraoperative blood pressure. What patterns identify patients at risk for postoperative complications? Ann Surg. 1990;212:567–580. doi: 10.1097/00000658-199011000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hallqvist L., Granath F., Huldt E., Bell M. Intraoperative hypotension is associated with acute kidney injury in noncardiac surgery: an observational study. Eur J Anaesthesiol. 2018;35:273–279. doi: 10.1097/EJA.0000000000000735. [DOI] [PubMed] [Google Scholar]
- 32.Tallgren M., Niemi T., Poyhia R., et al. Acute renal injury and dysfunction following elective abdominal aortic surgery. Eur J Vasc Endovasc Surg. 2007;33:550–555. doi: 10.1016/j.ejvs.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 33.House L.M., Marolen K.N., St Jacques P.J., McEvoy M.D., Ehrenfeld J.M. Surgical Apgar score is associated with myocardial injury after noncardiac surgery. J Clin Anesth. 2016;34:395–402. doi: 10.1016/j.jclinane.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 34.Kim B.H., Lee S., Yoo B., et al. Risk factors associated with outcomes of hip fracture surgery in elderly patients. Kor J Anesthesiol. 2015;68:561–567. doi: 10.4097/kjae.2015.68.6.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Waes J.A., van Klei W.A., Wijeysundera D.N., van Wolfswinkel L., Lindsay T.F., Beattie W.S. Association between intraoperative hypotension and myocardial injury after vascular surgery. Anesthesiology. 2016;124:35–44. doi: 10.1097/ALN.0000000000000922. [DOI] [PubMed] [Google Scholar]
- 36.Alcock R.F., Kouzios D., Naoum C., Hillis G.S., Brieger D.B. Perioperative myocardial necrosis in patients at high cardiovascular risk undergoing elective non-cardiac surgery. Heart. 2012;98:792–798. doi: 10.1136/heartjnl-2011-301577. [DOI] [PubMed] [Google Scholar]
- 37.Hallqvist L., Martensson J., Granath F., Sahlen A., Bell M. Intraoperative hypotension is associated with myocardial damage in noncardiac surgery: an observational study. Eur J Anaesthesiol. 2016;33:450–456. doi: 10.1097/EJA.0000000000000429. [DOI] [PubMed] [Google Scholar]
- 38.von Knorring J. Postoperative myocardial infarction: a prospective study in a risk group of surgical patients. Surgery. 1981;90:55–60. [PubMed] [Google Scholar]
- 39.Sabate S., Mases A., Guilera N., et al. Incidence and predictors of major perioperative adverse cardiac and cerebrovascular events in non-cardiac surgery. Br J Anaesth. 2011;107:879–890. doi: 10.1093/bja/aer268. [DOI] [PubMed] [Google Scholar]
- 40.Charlson M.E., MacKenzie C.R., Gold J.P., Ales K.L., Topkins M., Shires G.T. Risk for postoperative congestive heart failure. Surg Gynecol Obstet. 1991;172:95–104. [PubMed] [Google Scholar]
- 41.Bijker J.B., Persoon S., Peelen L.M., et al. Intraoperative hypotension and perioperative ischemic stroke after general surgery: a nested case-control study. Anesthesiology. 2012;116:658–664. doi: 10.1097/ALN.0b013e3182472320. [DOI] [PubMed] [Google Scholar]
- 42.Yocum G.T., Gaudet J.G., Teverbaugh L.A., et al. Neurocognitive performance in hypertensive patients after spine surgery. Anesthesiology. 2009;110:254–261. doi: 10.1097/ALN.0b013e3181942c7a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang N.Y., Hirao A., Sieber F. Association between intraoperative blood pressure and postoperative delirium in elderly hip fracture patients. PloS One. 2015;10 doi: 10.1371/journal.pone.0123892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sandid M.S., Assi M.A., Hall S. Intraoperative hypotension and prolonged operative time as risk factors for slow graft function in kidney transplant recipients. Clin Transplant. 2006;20:762–768. doi: 10.1111/j.1399-0012.2006.00567.x. [DOI] [PubMed] [Google Scholar]
- 45.Fumagalli U., Melis A., Balazova J., Lascari V., Morenghi E., Rosati R. Intra-operative hypotensive episodes may be associated with post-operative esophageal anastomotic leak. Updates Surg. 2016;68:185–190. doi: 10.1007/s13304-016-0369-9. [DOI] [PubMed] [Google Scholar]
- 46.Bijker J.B., van Klei W.A., Vergouwe Y., et al. Intraoperative hypotension and 1-year mortality after noncardiac surgery. Anesthesiology. 2009;111:1217–1226. doi: 10.1097/ALN.0b013e3181c14930. [DOI] [PubMed] [Google Scholar]
- 47.Hsieh J.K., Dalton J.E., Yang D., Farag E.S., Sessler D.I., Kurz A.M. The association between mild intraoperative hypotension and stroke in general surgery patients. Anesth Analg. 2016;123:933–939. doi: 10.1213/ANE.0000000000001526. [DOI] [PubMed] [Google Scholar]
- 48.Hirsch J., DePalma G., Tsai T.T., Sands L.P., Leung J.M. Impact of intraoperative hypotension and blood pressure fluctuations on early postoperative delirium after non-cardiac surgery. Br J Anaesth. 2015;115:418–426. doi: 10.1093/bja/aeu458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kertai M.D., White W.D., Gan T.J. Cumulative duration of "triple low" state of low blood pressure, low bispectral index, and low minimum alveolar concentration of volatile anesthesia is not associated with increased mortality. Anesthesiology. 2014;121:18–28. doi: 10.1097/ALN.0000000000000281. [DOI] [PubMed] [Google Scholar]
- 50.Babazade R., Yilmaz H.O., Zimmerman N.M., et al. Association between intraoperative low blood pressure and development of surgical site infection after colorectal surgery: a retrospective cohort study. Ann Surg. 2016;264:1058–1064. doi: 10.1097/SLA.0000000000001607. [DOI] [PubMed] [Google Scholar]
- 51.Reich D.L., Bodian C.A., Krol M., Kuroda M., Osinski T., Thys D.M. Intraoperative hemodynamic predictors of mortality, stroke, and myocardial infarction after coronary artery bypass surgery. Anesth Analg. 1999;89:814–822. doi: 10.1097/00000539-199910000-00002. [DOI] [PubMed] [Google Scholar]
- 52.Ono M., Brady K., Easley R.B., et al. Duration and magnitude of blood pressure below cerebral autoregulation threshold during cardiopulmonary bypass is associated with major morbidity and operative mortality. J Thorac Cardiovasc Surg. 2014;147:483–489. doi: 10.1016/j.jtcvs.2013.07.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gottesman R.F., Sherman P.M., Grega M.A., et al. Watershed strokes after cardiac surgery: diagnosis, etiology, and outcome. Stroke. 2006;37:2306–2311. doi: 10.1161/01.STR.0000236024.68020.3a. [DOI] [PubMed] [Google Scholar]
- 54.Gottesman R.F., Hillis A.E., Grega M.A., et al. Early postoperative cognitive dysfunction and blood pressure during coronary artery bypass graft operation. Arch Neurol. 2007;64:1111–1114. doi: 10.1001/archneur.64.8.noc70028. [DOI] [PubMed] [Google Scholar]
- 55.Hori D., Brown C., Ono M., et al. Arterial pressure above the upper cerebral autoregulation limit during cardiopulmonary bypass is associated with postoperative delirium. Br J Anaesth. 2014;113:1009–1017. doi: 10.1093/bja/aeu319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kanji H.D., Schulze C.J., Hervas-Malo M., et al. Difference between pre-operative and cardiopulmonary bypass mean arterial pressure is independently associated with early cardiac surgery-associated acute kidney injury. J Cardiothorac Surg. 2010;5:71. doi: 10.1186/1749-8090-5-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hori D., Hogue C., Adachi H., et al. Perioperative optimal blood pressure as determined by ultrasound tagged near infrared spectroscopy and its association with postoperative acute kidney injury in cardiac surgery patients. Interact Cardiovasc Thorac Surg. 2016;22:445–451. doi: 10.1093/icvts/ivv371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ono M., Arnaoutakis G.J., Fine D.M., et al. Blood pressure excursions below the cerebral autoregulation threshold during cardiac surgery are associated with acute kidney injury. Crit Care Med. 2013;41:464–471. doi: 10.1097/CCM.0b013e31826ab3a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wesselink E.M., Kappen T.H., van Klei W.A., Dieleman J.M., van Dijk D., Slooter A.J. Intraoperative hypotension and delirium after on-pump cardiac surgery. Br J Anaesth. 2015;115:427–433. doi: 10.1093/bja/aev256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Haase M., Bellomo R., Story D., et al. Effect of mean arterial pressure, haemoglobin and blood transfusion during cardiopulmonary bypass on post-operative acute kidney injury. Nephrol Dial Transplant. 2012;27:153–160. doi: 10.1093/ndt/gfr275. [DOI] [PubMed] [Google Scholar]
- 61.Sickeler R., Phillips-Bute B., Kertai M.D., et al. The risk of acute kidney injury with co-occurrence of anemia and hypotension during cardiopulmonary bypass relative to anemia alone. Ann Thorac Surg. 2014;97:865–871. doi: 10.1016/j.athoracsur.2013.09.060. [DOI] [PubMed] [Google Scholar]
- 62.Kandler K., Jensen M.E., Nilsson J.C., Moller C.H., Steinbruchel D.A. Arterial pressure during cardiopulmonary bypass is not associated with acute kidney injury. Acta Anaesthesiol Scand. 2015;59:625–631. doi: 10.1111/aas.12484. [DOI] [PubMed] [Google Scholar]
- 63.Millar-Craig M., Bishop C., Raftery E. Circadian variation of blood-pressure. Lancet. 1978;311:795–797. doi: 10.1016/s0140-6736(78)92998-7. [DOI] [PubMed] [Google Scholar]
- 64.Pickering T.G., James G.D., Boddie C., Harshfield G.A., Blank S., Laragh J.H. How common is white coat hypertension? JAMA. 1988;259:225–228. [PubMed] [Google Scholar]
- 65.Meng L., Cannesson M., Alexander B.S., et al. Effect of phenylephrine and ephedrine bolus treatment on cerebral oxygenation in anaesthetized patients. Br J Anaesth. 2011;107:209–217. doi: 10.1093/bja/aer150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Carrick M.M., Morrison C.A., Tapia N.M., et al. Intraoperative hypotensive resuscitation for patients undergoing laparotomy or thoracotomy for trauma: early termination of a randomized prospective clinical trial. J Trauma Acute Care Surg. 2016;80:886–896. doi: 10.1097/TA.0000000000001044. [DOI] [PubMed] [Google Scholar]
- 67.Futier E., Lefrant J.Y., Guinot P.G., et al. Effect of individualized vs standard blood pressure management strategies on postoperative organ dysfunction among high-risk patients undergoing major surgery: a randomized clinical trial. JAMA. 2017;318:1346–1357. doi: 10.1001/jama.2017.14172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gold J.P., Charlson M.E., Williams-Russo P., et al. Improvement of outcomes after coronary artery bypass. A randomized trial comparing intraoperative high versus low mean arterial pressure. J Thorac Cardiovasc Surg. 1995;110:1302–1311. doi: 10.1016/S0022-5223(95)70053-6. discussion 11–4. [DOI] [PubMed] [Google Scholar]
- 69.Siepe M., Pfeiffer T., Gieringer A., et al. Increased systemic perfusion pressure during cardiopulmonary bypass is associated with less early postoperative cognitive dysfunction and delirium. Eur J Cardiothorac Surg. 2011;40:200–207. doi: 10.1016/j.ejcts.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 70.Charlson M.E., Peterson J.C., Krieger K.H., et al. Improvement of outcomes after coronary artery bypass II: a randomized trial comparing intraoperative high versus customized mean arterial pressure. J Card Surg. 2007;22:465–472. doi: 10.1111/j.1540-8191.2007.00471.x. [DOI] [PubMed] [Google Scholar]
- 71.Azau A., Markowicz P., Corbeau J.J., et al. Increasing mean arterial pressure during cardiac surgery does not reduce the rate of postoperative acute kidney injury. Perfusion. 2014;29:496–504. doi: 10.1177/0267659114527331. [DOI] [PubMed] [Google Scholar]
- 72.Vedel A.G., Holmgaard F., Rasmussen L.S., et al. High-target versus low-target blood pressure management during cardiopulmonary bypass to prevent cerebral injury in cardiac surgery patients: a randomized controlled trial. Circulation. 2018;137:1770–1780. doi: 10.1161/CIRCULATIONAHA.117.030308. [DOI] [PubMed] [Google Scholar]
- 73.Williams-Russo P., Sharrock N.E., Mattis S., et al. Randomized trial of hypotensive epidural anesthesia in older adults. J Am Soc Anesthesiol. 1999;91:926–935. doi: 10.1097/00000542-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 74.Asfar P., Meziani F., Hamel J.-F., et al. High versus low blood-pressure target in patients with septic shock. N Engl J Med. 2014;370:1583–1593. doi: 10.1056/NEJMoa1312173. [DOI] [PubMed] [Google Scholar]
- 75.Lamontagne F., Richards-Belle A., Thomas K., et al. Effect of reduced exposure to vasopressors on 90-day mortality in older critically ill patients with vasodilatory hypotension: a randomized clinical trial. JAMA. 2020;323:938–949. doi: 10.1001/jama.2020.0930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Goetz R.H., Warren J.V., Gauer O.H., et al. Circulation of the giraffe. Circ Res. 1960;8:1049–1058. doi: 10.1161/01.res.8.5.1049. [DOI] [PubMed] [Google Scholar]
- 77.Ackland G.L., Brudney C.S., Cecconi M., et al. Perioperative Quality Initiative consensus statement on the physiology of arterial blood pressure control in perioperative medicine. Br J Anaesth. 2019;122:542–551. doi: 10.1016/j.bja.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 78.Zhao X., Tian L., Brackett A., Dai F., Xu J., Meng L. Classification and differential effectiveness of goal-directed hemodynamic therapies in surgical patients: a network meta-analysis of randomized controlled trials. J Crit Care. 2020;61:152–161. doi: 10.1016/j.jcrc.2020.10.031. [DOI] [PubMed] [Google Scholar]
- 79.Zhao X., Zhang L., Brackett A., Dai F., Xu J., Meng L. Hemodynamic management and surgical site infection: network meta-analysis of randomized controlled trials. J Clin Anesth. 2020;67:110021. doi: 10.1016/j.jclinane.2020.110021. [DOI] [PubMed] [Google Scholar]
- 80.Cattermole G.N., Leung P.Y., Ho G.Y., et al. The normal ranges of cardiovascular parameters measured using the ultrasonic cardiac output monitor. Physiol Rep. 2017;5 doi: 10.14814/phy2.13195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hamer J., Sowton E. Cardiac output after beta-adrenergic blockade in ischaemic heart disease. Br Heart J. 1965;27:892–895. doi: 10.1136/hrt.27.6.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang J., McDonagh D.L., Meng L. Calcium channel blockers in acute care: the links and missing links between hemodynamic effects and outcome evidence. Am J Cardiovasc Drug. 2021;21:35–41. doi: 10.1007/s40256-020-00410-4. [DOI] [PubMed] [Google Scholar]
- 83.Ovsyshcher I., Zimlichman R., Katz A., Bondy C., Furman S. Measurements of cardiac output by impedance cardiography in pacemaker patients at rest: effects of various atrioventricular delays. J Am Coll Cardiol. 1993;21:761–767. doi: 10.1016/0735-1097(93)90110-m. [DOI] [PubMed] [Google Scholar]
- 84.Meng L., Wang Y., Zhang L., McDonagh D.L. Heterogeneity and variability in pressure autoregulation of organ blood flow: lessons learned over 100+ years. Crit Care Med. 2019;47:436–448. doi: 10.1097/CCM.0000000000003569. [DOI] [PubMed] [Google Scholar]
- 85.Bertuglia S., Colantuoni A., Intaglietta M. Textbook of angiology. Springer; New York: 2000. Regulation of vascular tone and capillary perfusion; pp. 439–454. [Google Scholar]
- 86.Boswell C.A., Majno G., Joris I., Ostrom K.A. Acute endothelial cell contraction in vitro: a comparison with vascular smooth muscle cells and fibroblasts. Microvasc Res. 1992;43:178–191. doi: 10.1016/0026-2862(92)90015-h. [DOI] [PubMed] [Google Scholar]
- 87.Mazzoni M., Borgström P., Intaglietta M., Arfors K.-E. Lumenal narrowing and endothelial cell swelling in skeletal muscle capillaries during hemorrhagic shock. Circ Shock. 1989;29:27–39. [PubMed] [Google Scholar]
- 88.Meng L., Gelb A.W. Regulation of cerebral autoregulation by carbon dioxide. Anesthesiology. 2015;122:196–205. doi: 10.1097/ALN.0000000000000506. [DOI] [PubMed] [Google Scholar]
- 89.Meng L., Hou W., Chui J., Han R., Gelb A.W. Cardiac output and cerebral blood flow: the integrated regulation of brain perfusion in adult humans. Anesthesiology. 2015;123:1198–1208. doi: 10.1097/ALN.0000000000000872. [DOI] [PubMed] [Google Scholar]
- 90.Ince C. Hemodynamic coherence and the rationale for monitoring the microcirculation. Crit Care. 2015;19:S8. doi: 10.1186/cc14726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dubin A., Pozo M.O., Casabella C.A., et al. Increasing arterial blood pressure with norepinephrine does not improve microcirculatory blood flow: a prospective study. Crit Care. 2009;13:R92. doi: 10.1186/cc7922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Morelli A., Donati A., Ertmer C., et al. Effects of vasopressinergic receptor agonists on sublingual microcirculation in norepinephrine-dependent septic shock. Crit Care. 2011;15:R217. doi: 10.1186/cc10453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ince C. The microcirculation is the motor of sepsis. Crit Care. 2005;9:S13–S19. doi: 10.1186/cc3753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Parker T., Brealey D., Dyson A., Singer M. Optimising organ perfusion in the high-risk surgical and critical care patient: a narrative review. Br J Anaesth. 2019;123:170–176. doi: 10.1016/j.bja.2019.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Buwalda M., Ince C. Opening the microcirculation: can vasodilators be useful in sepsis? Intensive Care Med. 2002;28:1208–1217. doi: 10.1007/s00134-002-1407-2. [DOI] [PubMed] [Google Scholar]
- 96.Sharrock N.E., Mineo R., Urquhart B. Hemodynamic response to low-dose epinephrine infusion during hypotensive epidural anesthesia for total hip replacement. Reg Anesth. 1990;15:295–299. [PubMed] [Google Scholar]
- 97.Sharrock N.E., Salvati E.A. Hypotensive epidural anesthesia for total hip arthroplasty: a review. Acta Orthop Scand. 1996;67:91–107. doi: 10.3109/17453679608995620. [DOI] [PubMed] [Google Scholar]
- 98.Pearse R.M., Harrison D.A., MacDonald N., et al. Effect of a perioperative, cardiac output-guided hemodynamic therapy algorithm on outcomes following major gastrointestinal surgery: a randomized clinical trial and systematic review. JAMA. 2014;311:2181–2190. doi: 10.1001/jama.2014.5305. [DOI] [PubMed] [Google Scholar]
- 99.Stens J., Hering J.-P., van der Hoeven C.W.P., et al. The added value of cardiac index and pulse pressure variation monitoring to mean arterial pressure-guided volume therapy in moderate-risk abdominal surgery (COGUIDE): a pragmatic multicentre randomised controlled trial. Anaesthesia. 2017;72:1078–1087. doi: 10.1111/anae.13834. [DOI] [PubMed] [Google Scholar]
- 100.Mascha E.J., Sessler D.I. Statistical grand rounds: design and analysis of studies with binary- event composite endpoints: guidelines for anesthesia research. Anesth Analg. 2011;112:1461–1471. doi: 10.1213/ANE.0b013e31821796d3. [DOI] [PubMed] [Google Scholar]
- 101.Voldby A.W., Brandstrup B. Fluid therapy in the perioperative setting—a clinical review. J Intensive Care. 2016;4:27. doi: 10.1186/s40560-016-0154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Maheshwari K., Pu X., Rivas E., et al. Association between intraoperative mean arterial pressure and postoperative complications is independent of cardiac index in patients undergoing noncardiac surgery. Br J Anaesth. 2021 doi: 10.1016/j.bja.2021.06.024. Advance Access published on July 16. [DOI] [PubMed] [Google Scholar]
- 103.Zhao X., Xiao H., Cai J., Meng L. Double standards: why is pulse oximetry standard care, whereas tissue oximetry is not? Curr Opin Anaesthesiol. 2020;33:619–625. doi: 10.1097/ACO.0000000000000910. [DOI] [PubMed] [Google Scholar]
- 104.Fan X., Lin L., Li G., et al. Do cerebral and somatic tissue oxygen saturation measurements correlate with each other during surgery? J Clin Monit Comput. 2020;34:483–490. doi: 10.1007/s10877-019-00339-3. [DOI] [PubMed] [Google Scholar]
- 105.Li G., Tian D.D., Wang X., et al. Muscular tissue oxygen saturation and posthysterectomy nausea and vomiting: the iMODIPONV randomized controlled trial. Anesthesiology. 2020;133:318–331. doi: 10.1097/ALN.0000000000003305. [DOI] [PubMed] [Google Scholar]
- 106.Meng L., Gruenbaum S.E., Dai F., Wang T. Physiology, intervention, and outcome: three critical questions about cerebral tissue oxygen saturation monitoring. Minerva Anestesiol. 2018;84:599–614. doi: 10.23736/S0375-9393.18.12476-X. [DOI] [PubMed] [Google Scholar]
- 107.Groner W., Winkelman J.W., Harris A.G., et al. Orthogonal polarization spectral imaging: a new method for study of the microcirculation. Nat Med. 1999;5:1209–1212. doi: 10.1038/13529. [DOI] [PubMed] [Google Scholar]
- 108.Bangalore S., Wetterslev J., Pranesh S., Sawhney S., Gluud C., Messerli F.H. Perioperative beta blockers in patients having non-cardiac surgery: a meta-analysis. Lancet. 2008;372:1962–1976. doi: 10.1016/S0140-6736(08)61560-3. [DOI] [PubMed] [Google Scholar]
- 109.Wijeysundera D.N., Duncan D., Nkonde-Price C., et al. Perioperative beta blockade in noncardiac surgery: a systematic review for the 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:2246–2264. doi: 10.1161/CIR.0000000000000104. [DOI] [PubMed] [Google Scholar]
- 111.Cruickshank J.M. Are we misunderstanding beta-blockers. Int J Cardiol. 2007;120:10–27. doi: 10.1016/j.ijcard.2007.01.069. [DOI] [PubMed] [Google Scholar]
- 112.Frishman W.H. Multifactorial actions of beta-adrenergic blocking drugs in ischemic heart disease: current concepts. Circulation. 1983;67:I11–I18. [PubMed] [Google Scholar]
- 113.Galderisi M., D'Errico A. Beta-blockers and coronary flow reserve: the importance of a vasodilatory action. Drugs. 2008;68:579–590. doi: 10.2165/00003495-200868050-00002. [DOI] [PubMed] [Google Scholar]
- 114.Amsterdam E.A., Wenger N.K., Brindis R.G., et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64:e139–e228. doi: 10.1016/j.jacc.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 115.Aqyagi M., Deshmukh V.D., Meyer J.S., Kawamura Y., Tagashira Y. Effect of beta-adrenergic blockade with propranolol on cerebral blood flow, autoregulation and CO2 responsiveness. Stroke. 1976;7:291–295. doi: 10.1161/01.str.7.3.291. [DOI] [PubMed] [Google Scholar]
- 116.Griffith D.N., James I.M., Newbury P.A., Woollard M.L. The effect of beta-adrenergic receptor blocking drugs on cerebral blood flow. Br J Clin Pharmacol. 1979;7:491–494. doi: 10.1111/j.1365-2125.1979.tb00991.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Rousseau M.F., Etienne J., Van Mechelen H., Veriter C., Pouleur H. Hemodynamic and cardiac effects of nicardipine in patients with coronary artery disease. J Cardiovasc Pharmacol. 1984;6:833–839. doi: 10.1097/00005344-198409000-00015. [DOI] [PubMed] [Google Scholar]
- 118.Silke B., Zezulka A.V., Verma S.P., Taylor S.H. Hemodynamic assessment of nicardipine alone and with atenolol in coronary artery disease using a modified echo-Doppler device. Am J Cardiol. 1989;64:28h–34h. doi: 10.1016/0002-9149(89)90978-8. [DOI] [PubMed] [Google Scholar]
- 119.Lambert C.R., Hill J.A., Nichols W.W., Feldman R.L., Pepine C.J. Coronary and systemic hemodynamic effects of nicardipine. Am J Cardiol. 1985;55:652–656. doi: 10.1016/0002-9149(85)90130-4. [DOI] [PubMed] [Google Scholar]
- 120.Lambert C.R., Pepine C.J. Effects of intravenous and intracoronary nicardipine. Am J Cardiol. 1989;64:8h–15h. doi: 10.1016/0002-9149(89)90974-0. [DOI] [PubMed] [Google Scholar]
- 121.Abe K., Iwanaga H., Inada E. Effect of nicardipine and diltiazem on internal carotid artery blood flow velocity and local cerebral blood flow during cerebral aneurysm surgery for subarachnoid hemorrhage. J Clin Anesth. 1994;6:99–105. doi: 10.1016/0952-8180(94)90004-3. [DOI] [PubMed] [Google Scholar]
- 122.Suzuki S., Ohtsuka S., Ishikawa K., Yamaguchi I. Effects of nicardipine on coronary, vertebral and renal arterial flows in patients with essential hypertension. Hypertens Res. 2003;26:193–199. doi: 10.1291/hypres.26.193. [DOI] [PubMed] [Google Scholar]
- 123.Hollmann C., Fernandes N.L., Biccard B.M. A systematic review of outcomes associated with withholding or continuing angiotensin-converting enzyme inhibitors and angiotensin receptor blockers before noncardiac surgery. Anesth Analg. 2018;127:678–687. doi: 10.1213/ANE.0000000000002837. [DOI] [PubMed] [Google Scholar]
- 124.Muiesan G., Alicandri C.L., Agabiti-Rosei E., et al. Angiotensin-converting enzyme inhibition, catecholamines and hemodynamics in essential hypertension. Am J Cardiol. 1982;49:1420–1424. doi: 10.1016/0002-9149(82)90354-x. [DOI] [PubMed] [Google Scholar]
- 125.Tarazi R.C., Bravo E.L., Fouad F.M., Omvik P., Cody R.J., Jr. Hemodynamic and volume changes associated with captopril. Hypertension. 1980;2:576–585. doi: 10.1161/01.hyp.2.4.576. [DOI] [PubMed] [Google Scholar]
- 126.Zou Z., Yuan H.B., Yang B., et al. Perioperative angiotensin-converting enzyme inhibitors or angiotensin II type 1 receptor blockers for preventing mortality and morbidity in adults. Cochr Database Syst Rev. 2016;2016 doi: 10.1002/14651858.CD009210.pub2. CD009210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Roshanov P.S., Rochwerg B., Patel A., et al. Withholding versus continuing angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers before noncardiac surgery: an analysis of the Vascular events in noncardiac Surgery patIents cOhort evaluatioN Prospective Cohort. Anesthesiology. 2017;126:16–27. doi: 10.1097/ALN.0000000000001404. [DOI] [PubMed] [Google Scholar]
- 128.Farag E., Liang C., Mascha E.J., et al. Association between use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers and postoperative delirium. Anesthesiology. 2020;133:119–132. doi: 10.1097/ALN.0000000000003329. [DOI] [PubMed] [Google Scholar]
- 129.Lee S.M., Takemoto S., Wallace A.W. Association between withholding angiotensin receptor blockers in the early postoperative period and 30-day mortality: a cohort study of the Veterans Affairs Healthcare System. Anesthesiology. 2015;123:288–306. doi: 10.1097/ALN.0000000000000739. [DOI] [PubMed] [Google Scholar]
- 130.Fleisher L.A., Fleischmann K.E., Auerbach A.D., et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:e278–e333. doi: 10.1161/CIR.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 131.Bray J.K., Fernando R., Patel N.P., Columb M.O. Suprasternal Doppler estimation of cardiac output: standard versus sequential combined spinal epidural anesthesia for cesarean delivery. Anesth Analg. 2006;103:959–964. doi: 10.1213/01.ane.0000231831.00032.97. [DOI] [PubMed] [Google Scholar]
- 132.Bombardieri A.M., Sharrock N.E., Ma Y., Go G., Drummond J.C. An observational study of cerebral blood flow velocity during hypotensive epidural anesthesia. Anesth Analg. 2016;122:226–233. doi: 10.1213/ANE.0000000000000985. [DOI] [PubMed] [Google Scholar]
- 133.Blomberg S., Emanuelsson H., Kvist H., et al. Effects of thoracic epidural anesthesia on coronary arteries and arterioles in patients with coronary artery disease. Anesthesiology. 1990;73:840–847. doi: 10.1097/00000542-199011000-00008. [DOI] [PubMed] [Google Scholar]
- 134.Nygård E., Kofoed K.F., Freiberg J., et al. Effects of high thoracic epidural analgesia on myocardial blood flow in patients with ischemic heart disease. Circulation. 2005;111:2165–2170. doi: 10.1161/01.CIR.0000163551.33812.1A. [DOI] [PubMed] [Google Scholar]
- 135.Wijeysundera D.N., Beattie W.S., Austin P.C., Hux J.E., Laupacis A. Epidural anaesthesia and survival after intermediate-to-high risk non-cardiac surgery: a population-based cohort study. Lancet. 2008;372:562–569. doi: 10.1016/S0140-6736(08)61121-6. [DOI] [PubMed] [Google Scholar]
- 136.Fowler N.O., Holmes J.C. Blood viscosity and cardiac output in acute experimental anemia. J Appl Physiol. 1975;39:453–456. doi: 10.1152/jappl.1975.39.3.453. [DOI] [PubMed] [Google Scholar]
- 137.Borgström L., Jóhannsson H., Siesjö B.K. The influence of acute normovolemic anemia on cerebral blood flow and oxygen consumption of anesthetized rats. Acta Physiol Scand. 1975;93:505–514. doi: 10.1111/j.1748-1716.1975.tb05842.x. [DOI] [PubMed] [Google Scholar]
- 138.Murray J.F., Rapaport E. Coronary blood flow and myocardial metabolism in acute experimental anaemia1. Cardiovasc Res. 1972;6:360–367. doi: 10.1093/cvr/6.4.360. [DOI] [PubMed] [Google Scholar]
- 139.Tuman K.J. Tissue oxygen delivery: the physiology of anemia. Anesthesiol Clin North Am. 1990;8:451–469. [Google Scholar]
- 140.Carson J.L., Sieber F., Cook D.R., et al. Liberal versus restrictive blood transfusion strategy: 3-year survival and cause of death results from the FOCUS randomised controlled trial. Lancet. 2015;385:1183–1189. doi: 10.1016/S0140-6736(14)62286-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Carson J.L., Terrin M.L., Noveck H., et al. Liberal or Restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365:2453–2462. doi: 10.1056/NEJMoa1012452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Robinson B.J., Ebert T.J., O'Brien T.J., Colinco M.D., Muzi M. Mechanisms whereby propofol mediates peripheral vasodilation in humans. Sympathoinhibition or direct vascular relaxation? Anesthesiology. 1997;86:64–72. doi: 10.1097/00000542-199701000-00010. [DOI] [PubMed] [Google Scholar]
- 143.Ebert T.J., Muzi M., Berens R., Goff D., Kampine J.P. Sympathetic responses to induction of anesthesia in humans with propofol or etomidate. Anesthesiology. 1992;76:725–733. doi: 10.1097/00000542-199205000-00010. [DOI] [PubMed] [Google Scholar]
- 144.Claeys M.A., Gepts E., Camu F. Haemodynamic changes during anaesthesia induced and maintained with propofol. Br J Anaesth. 1988;60:3–9. doi: 10.1093/bja/60.1.3. [DOI] [PubMed] [Google Scholar]
- 145.Muzi M., Berens R.A., Kampine J.P., Ebert T.J. Venodilation contributes to propofol-mediated hypotension in humans. Anesth Analg. 1992;74:877–883. doi: 10.1213/00000539-199206000-00017. [DOI] [PubMed] [Google Scholar]
- 146.Mulier J.P., Wouters P.F., Van Aken H., Vermaut G., Vandermeersch E. Cardiodynamic effects of propofol in comparison with thiopental: assessment with a transesophageal echocardiographic approach. Anesth Analg. 1991;72:28–35. doi: 10.1213/00000539-199101000-00006. [DOI] [PubMed] [Google Scholar]
- 147.Vandesteene A., Trempont V., Engelman E., et al. Effect of propofol on cerebral blood flow and metabolism in man. Anaesthesia. 1988;43:42–43. doi: 10.1111/j.1365-2044.1988.tb09067.x. [DOI] [PubMed] [Google Scholar]
- 148.Kaisti K.K., Långsjö J.W., Aalto S., et al. Effects of sevoflurane, propofol, and adjunct nitrous oxide on regional cerebral blood flow, oxygen consumption, and blood volume in humans. Anesthesiology. 2003;99:603–613. doi: 10.1097/00000542-200309000-00015. [DOI] [PubMed] [Google Scholar]
- 149.Meng L., Gelb A.W., McDonagh D.L. Changes in cerebral tissue oxygen saturation during anaesthetic-induced hypotension: an interpretation based on neurovascular coupling and cerebral autoregulation. Anaesthesia. 2013;68:736–741. doi: 10.1111/anae.12254. [DOI] [PubMed] [Google Scholar]
- 150.Lurati Buse G.A., Schumacher P., Seeberger E., et al. Randomized comparison of sevoflurane versus propofol to reduce perioperative myocardial ischemia in patients undergoing noncardiac surgery. Circulation. 2012;126:2696–2704. doi: 10.1161/CIRCULATIONAHA.112.126144. [DOI] [PubMed] [Google Scholar]
- 151.Xing C.Y., Tarumi T., Liu J., et al. Distribution of cardiac output to the brain across the adult lifespan. J Cereb Blood Flow Metab. 2017;37:2848–2856. doi: 10.1177/0271678X16676826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Rivers E., Nguyen B., Havstad S., et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 153.Peake S.L., Delaney A., Bailey M., et al. Goal-directed resuscitation for patients with early septic shock. N Engl J Med. 2014;371:1496–1506. doi: 10.1056/NEJMoa1404380. [DOI] [PubMed] [Google Scholar]
- 154.Yealy D.M., Kellum J.A., Huang D.T., et al. A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014;370:1683–1693. doi: 10.1056/NEJMoa1401602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Mouncey P.R., Osborn T.M., Power G.S., et al. Trial of early, goal-directed resuscitation for septic shock. N Engl J Med. 2015;372:1301–1311. doi: 10.1056/NEJMoa1500896. [DOI] [PubMed] [Google Scholar]
- 156.Rhodes A., Evans L.E., Alhazzani W., et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Crit Care Med. 2017;45:486–552. doi: 10.1097/CCM.0000000000002255. [DOI] [PubMed] [Google Scholar]
- 157.LeDoux D., Astiz M.E., Carpati C.M., Rackow E.C. Effects of perfusion pressure on tissue perfusion in septic shock. Crit Care Med. 2000;28:2729–2732. doi: 10.1097/00003246-200008000-00007. [DOI] [PubMed] [Google Scholar]
- 158.Bourgoin A., Leone M., Delmas A., Garnier F., Albanèse J., Martin C. Increasing mean arterial pressure in patients with septic shock: effects on oxygen variables and renal function. Crit Care Med. 2005;33:780–786. doi: 10.1097/01.ccm.0000157788.20591.23. [DOI] [PubMed] [Google Scholar]
- 159.Thooft A., Favory R., Salgado D.R., et al. Effects of changes in arterial pressure on organ perfusion during septic shock. Crit Care. 2011;15:R222. doi: 10.1186/cc10462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Jhanji S., Stirling S., Patel N., Hinds C.J., Pearse R.M. The effect of increasing doses of norepinephrine on tissue oxygenation and microvascular flow in patients with septic shock. Crit Care Med. 2009;37:1961–1966. doi: 10.1097/CCM.0b013e3181a00a1c. [DOI] [PubMed] [Google Scholar]
- 161.Lang C.H., Bagby G.J., Ferguson J.L., Spitzer J.J. Cardiac output and redistribution of organ blood flow in hypermetabolic sepsis. Am J Physiol. 1984;246:R331–R337. doi: 10.1152/ajpregu.1984.246.3.R331. [DOI] [PubMed] [Google Scholar]
- 162.Di Giantomasso D., May C.N., Bellomo R. Vital organ blood flow during hyperdynamic sepsis. Chest. 2003;124:1053–1059. doi: 10.1378/chest.124.3.1053. [DOI] [PubMed] [Google Scholar]
- 163.Tuchschmidt J., Fried J., Astiz M., Rackow E. Elevation of cardiac output and oxygen delivery improves outcome in septic shock. Chest. 1992;102:216–220. doi: 10.1378/chest.102.1.216. [DOI] [PubMed] [Google Scholar]
- 164.Powers W.J., Rabinstein A.A., Ackerson T., et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49:e46–e110. doi: 10.1161/STR.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 165.Hindman B.J. Anesthetic management of emergency endovascular thrombectomy for acute ischemic stroke: Part 1. Patient characteristics, determinants of effectiveness, and effect of blood pressure on outcome. Anesth Analg. 2019;128:695–705. doi: 10.1213/ANE.0000000000004044. [DOI] [PubMed] [Google Scholar]
- 166.Lee J.-M., Grabb M.C., Zipfel G.J., Choi D.W. Brain tissue responses to ischemia. J Clin Invest. 2000;106:723–731. doi: 10.1172/JCI11003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Lin L., Li G., Li J., Meng L. Tourniquet-induced tissue hypoxia characterized by near-infrared spectroscopy during ankle surgery: an observational study. BMC Anesthesiol. 2019;19:70. doi: 10.1186/s12871-019-0740-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.