As we pass the first anniversary of the COVID-19 pandemic, there has been greater attention on and concern about the impact of the pandemic on the mental health of Canadians. 1 This is understandable given that the pandemic has increased risk factor exposure (social isolation, financial stress, anxiety related to infection risk, etc.) for all Canadians. It is likely that these circumstances have increased the prevalence of mental disorders and therefore the need for mental health services. That said, there is a dearth of information to accurately determine whether there is in fact increased mental illness burden and an associated increased need for services. Without such information, the impact of the pandemic on population-based mental health need is unknown and policymakers and planners will struggle to meaningfully respond to increased need if it exists. Moreover, access to mental health services prior to the pandemic was poor such that any increase in demand will likely go unmet, and individuals will have even longer wait times for services.
The need for useful information to help plan for population-based mental health need is the focus of the study by Vigo et al. (ref). In this study, the authors propose a conceptual framework for measuring population-based prevalence estimates and then measure the variation in prevalence obtained from the various methods they use to determine the best approach. In Canada, prevalence estimates of the most common mental disorders have relied on population-based surveys by Statistics Canada. 2 The mental illness–specific surveys have occurred every 10 years (in 2002 and 2012) but have yielded stable prevalence estimates between these 2 time periods. Thus, we have known the prevalence of some of the most common disorders for nearly 20 years, but it is unclear whether this information has been used for planning purposes in any province. The framework and methods proposed by Vigo et al. may provide increased confidence in the accuracy of prevalence data. However, prevalence data alone is not sufficient to guide policy and planning.
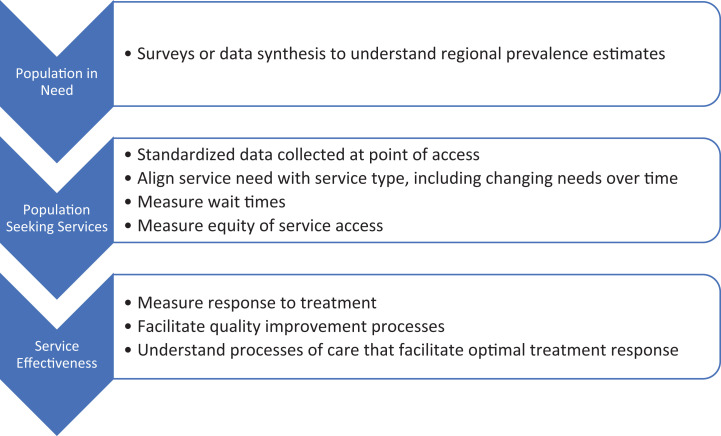
It is important to further consider the processes of a highly functioning health system and the information required to support the functioning of a health system. The idea of a need to understand and plan for mental health services is not new, with the concept being described more than 2 decades ago in the United Kingdom, 3 and the importance of routine outcome monitoring in mental health described in Australia nearly a decade ago. 4 To plan for and address population-based need for mental health services, there are 3 areas of information reflecting different attributes of a mental health system that are required (Figure 1):
Figure 1.
Information needs, required methods, and expected outcomes to facilitate mental health system policy and planning.
Population-based Prevalence Estimates
This information is necessary, but not sufficient, to understand the estimate of service need within the population. Diagnoses are likely useful in aligning clinical populations with treatment that is supported by evidence based on clinical trials, or care that is supported by clinical guidelines or the development of care pathways. With their conceptual framework, Vigo et al. (ref) have developed a proposed method to provide this information. The need to understand the prevalence of populations is obvious for planning purposes. Prevalence estimates are likely needed regionally as there is evidence that need varies geographically based on regional variation in demographics, among other factors. Measuring prevalence variation regionally requires a sampling strategy and adequate sample size and is likely to be costly, particularly when one factors in the need to understand variability in severity and the degree of comorbidity that occurs for any given disorder.
The Needs of Individuals Who Are Seeking Services
While prevalence estimates provide an important, but incomplete, perspective on needs, additional information obtained at point of care could contribute to a better understanding of the subset of individuals who seek help. Such information would be especially useful at regional levels, where population characteristics and related services may differ. A mental health system should be accountable to all individuals who need services, but should, at minimum, meet the needs of individuals who are seeking treatment since these are the individuals who are currently visible to the system. Moreover, evidence would suggest that our existing mental health systems in Canada are not meeting the needs of the subset of individuals with disorder who are seeking services. 5,6 Efforts to increase help-seeking among individuals with disorder without a plan to increase capacity will simply overwhelm the current, under-resourced system. There are many other important functions of understanding the populations seeking services, and this information is often routinely available in administrative data or could easily be incorporated into such data. For example, if populations seeking services are measured over time, planners would be able to monitor trends and respond to needs dynamically. In Ontario, we have seen a dramatic rise in the use of emergency departments for mental health and addictions-related issues, 7 including a large proportion who appear to be using the emergency department as a point of “first contact” within the broader system, 8 suggesting a population that would benefit from more, and better coordinated, services. If measurement frameworks are established regionally (e.g., regional centralized access points where information at the point of referral is routinely captured), information about regional variation in need would be available to align services with need at a regional level. Information about demographics, including variables related to equity, diversity, and inclusion, can also be incorporated to measure, over time, whether certain populations are not being served. This would create opportunities to systematically reach out to racialized communities that have historically been underserved by existing mental health services and to measure iteratively whether engagement strategies to improve access to underserved populations are successful. Finally, measuring the time of referral at this “front door” is the first step in developing a mental health and substance-related wait time strategy critical for system-level accountability.
The Effectiveness of Services
With rare exceptions, in most provincial mental health systems in Canada, outcomes are not routinely measured when services are provided to individuals. Without outcome measurement, individuals who receive services and clinicians who provide services have no objective way to determine whether the services are effective. The same outcome measures are also important to understand the impact of services provided across an organization and an entire system in aggregate. There are very few examples of systematic outcome measurement being used for system performance monitoring. Indeed, the challenges of estimating need for psychiatric hospitalization beds regionally in Australia has been described recently. 9 One successful example is the use of outcome monitoring in the Improving Access to Psychological Therapies (IAPT) program in England, a program to provide evidence-based psychotherapies (e.g., cognitive behavioural therapy) to individuals with depression and anxiety-related disorders. 10 Outcome measures are captured on 98% of individuals who receive services, and through routine outcome measurement, IAPT has been able to achieve good outcomes, and to determine how processes of care impact outcomes. IAPT is a learning health system, in which “science, informatics, incentives, and culture are aligned for continuous improvement and innovation, with best practices seamlessly embedded in the delivery process and new knowledge captured as an integral by-product of the delivery experience.” 11 For example, by measuring variation in average wait times (information captured in the second level of routine information—the needs of individuals who are seeking services, Figure 1), the IAPT program learned that longer wait times, independent of the quality of therapy, resulted in reduced treatment response. They also used this information to engage in quality improvement such that in 2019/20, 88% of individuals who initiated treatment within IAPT did so within 6 weeks, which likely contributed to the observed 51.1% of individuals who recovered. IAPT was established based on an understanding of the high prevalence (and burden) of depression and anxiety-related disorders, but the success of the program was based on the establishment of robust measurement systems that allowed the program to iteratively learn how to achieve outcomes iteratively.
Understanding population-based prevalence is important for understanding need for services, but for Canadians to have truly responsive mental health systems, we need to build comprehensive, problem-oriented data measurement and data analytic systems that will allow us to learn how to more accurately align services with need and to understand how to optimize the effectiveness of services.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Paul Kurdyak, MD, PhD https://orcid.org/0000-0001-8115-7437
Scott Patten, MD, PhD https://orcid.org/0000-0001-9871-4041
References
- 1. Vigo D, Patten S, Pajer K, et al. Mental health of communities during the COVID-19 Pandemic. Can J Psychiatry. 2020;65(10):681–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dobson K, Vigod S, Mustard C, Smith P. Trends in the prevalence of depression and anxiety disorders among working-age Canadian adults between 2000 and 2016. Health Rep. 2020;31(12):12–23. [DOI] [PubMed] [Google Scholar]
- 3. Thornicroft G, Strathdee G, Thornicroft G. Commissioning mental health services. Great Britain: H. M. Stationery Office; 1996. [Google Scholar]
- 4. Burgess P, Coombs T, Clarke A, Dickson R, Pirkis J. Achievements in mental health outcome measurement in Australia: reflections on progress made by the Australian mental health outcomes and classification network (AMHOCN). Int J Ment Health Syst. 2012;6(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Goldner EM, Jones W, Fang ML. Access to and waiting time for psychiatrist services in a Canadian urban area: a study in real time. Can J Psychiatry. 2011;56(8):474–480. [DOI] [PubMed] [Google Scholar]
- 6. Statistics Canada. Mental health care needs, 2018. Published 2019. Accessed March 14, 2021. https://www150.statcan.gc.ca/n1/pub/82-625-x/2019001/article/00011-eng.htm
- 7. Chiu M, Gatov E, Fung K, Kurdyak P, Guttmann A. Deconstructing the rise in mental health-related ed visits among children and youth In Ontario, Canada. Health Aff (Millwood). 2020;39(10):1728–1736. [DOI] [PubMed] [Google Scholar]
- 8. Gill PJ, Saunders N, Gandhi S, et al. Emergency department as a first contact for mental health problems in children and youth. J Am Acad Child Adolesc Psychiatry. 2017;56(6):475–482. e4. [DOI] [PubMed] [Google Scholar]
- 9. Allison S, Bastiampillai T, Looi JCL, Copolov D. Australia’s national mental health service planning framework: are opinion-based algorithms driving mental health policy? Aust N Z J Psychiatry. 2020;54(12):1149–1151. [DOI] [PubMed] [Google Scholar]
- 10. Clark DM, Canvin L, Green J, Layard R, Pilling S, Janecka M. Transparency about the outcomes of mental health services (IAPT approach): an analysis of public data. Lancet. 2018;391(10121):679–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Institute of Medicine. Digital infrastructure for the learning health system: the foundation for continuous improvement in health and health care. In: McGinnis JM, Powers B, Grossmann C, editors. The foundation for continuous improvement in health and health care workshop series summary. Washington (DC): National Academies Press; 2011:1–311. [PubMed] [Google Scholar]