Abstract
Objective:
Prostate cancer is the most common male cancer in the UK. In many hospitals, patients are now being referred for a multiparametric (mp) MRI scan of their prostate as part of an evaluation for the presence of prostate cancer, prior to an ultrasound-guided biopsy. Prostate Imaging Reporting and Data System (PI-RADS) score of 3 are defined as “equivocal” for the presence of prostate cancer. Thus, a PI-RADS 3 lesion does not confidently determine whether there is significant prostate disease or not.
Our aim is to determine the correlation of PI-RADS 3 prostatic lesions with histology proven, clinically significant cancer.
Methods:
We performed a retrospective review on a cohort of 143 consecutive patients. Each patient underwent a mp-MRI scan of their prostate given a PI-RADS score. PI-RADS 3 lesions were analysed further based on histology and categorised into malignant and non-malignant lesions. Prostate-specific antigen (PSA) results and prostatic volume of PI-RADS 3 lesions were also analysed.
Results:
We identified 45 patients with PI-RADS 3 lesions out of 143 patients. 32 patients subsequently underwent transrectal/transperineal ultrasound-guided biopsy. 43% of patients were found to have had a malignant prostatic adenocarcinoma on histology. The remaining 56% had non-malignant findings. Of those with malignant disease, there was a higher median PSA and lower mean prostatic volume.
Conclusion:
The study confirms that a score of PI-RADS 3 does not accurately differentiate between malignant and non-malignant lesions. Further investigations such as ultrasound-guided prostate biopsy and PSA parameters are required to accurately ascertain the nature of a prostate lesion with PI-RADS score 3.
Advances in knowledge:
An ultrasound-guided prostate biopsy in patients with PI-RADS 3 remains of paramount importance when distinguishing malignant vs non-malignant lesions. Multicentre data of MRI findings with PI-RADS 3 scores is required to yield a sample size large enough to carry out statistical analysis.
Background
Prostate cancer is the most common male cancer in the UK. 1 In many hospitals, patients are now being referred for a multiparametric (mp) MRI scan of their prostate as part of an evaluation for the presence of prostate cancer, prior to an ultrasound-guided biopsy. 2 The Prostate Imaging Reporting and Data System (PI-RADS) is an international reporting system designed to standardise the interpretation of prostate MR images. It provides a method of classifying prostates in order of suspicion for malignancy. 3 As per the classification, lesions with a PI-RADS score of 3 are defined as “equivocal” for the presence of prostate cancer (Figure 1). Thus, a PI-RADS 3 lesion does not confidently determine whether there is significant prostate disease or not (defined as a Gleason score of 7 or more). 5
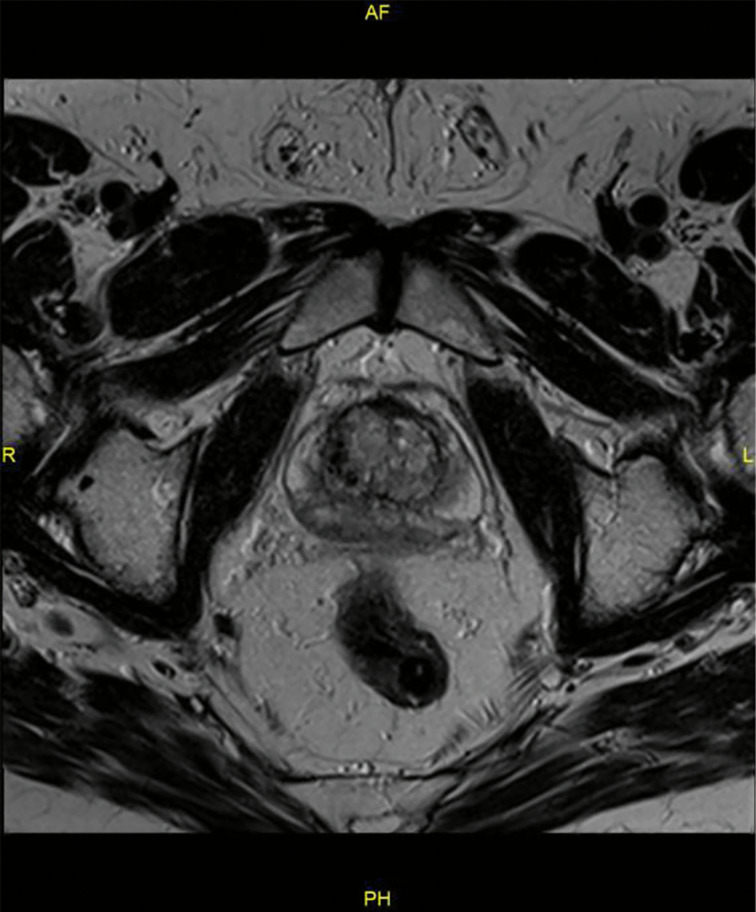
Figure 1.
PI-RADS-3 lesion. Prostate volume 35 ml. Proven at histology with bilateral medium-grade peripheral zone prostatic adenocarcinoma - Gleason 7b. Case courtesy of Dr Ian Bickle, Radiopaedia.org, rID: 8,6293. 4 PI-RADS, Prostate Imaging Reporting and Data System.
Objective
Our aim is to determine the correlation of PI-RADS 3 prostatic lesions with histology proven, clinically significant cancer.
Design, setting, and participants
We performed a retrospective review on a cohort of 143 consecutive patients between May 2018 to February 2020. All patients had been referred to a local district general hospital from primary care due to the presence of an elevated PSA and/or an abnormal digital rectal examination. Each patient underwent a mp-MRI scan of their prostate with contrast. All MRI prostate images were interpretated by experienced consultant radiologists.
We reviewed the demographic, clinical, MRI and biopsy data of each patient. We looked through all of the MRI reports for the patients and recorded PI-RADS score for each of the patients. Patients with PI-RADS 3 were analysed further. The number of abnormal lesions seen on MRI and their zone was recorded. Biopsy results were analysed to categorise PI-RADS 3 into malignant or non-malignant categories. We also looked at the patients’ Gleason score, PSA results and the prostatic volume.
Outcome measurements and statistical analysis
A total of 143 patients were retrospectively reviewed. We identified 45 patients with PI-RADS 3 lesions. The mean age of our patients was 69.4 years old (±SD 7.3). The median serum PSA was 7.3 ng ml−1 and median prostate volume was 42.0 ml.
Out of the 43 patients with identified PI-RADS 3 lesions, 32 patients subsequently underwent transrectal/transperineal ultrasound-guided biopsy. A review of their respective histology analyses revealed 18 patients had non-malignant disease, whereas 14 patients were harbouring prostatic adenocarcinoma (Figure 1). Amongst these, five patients had a combined Gleason score 6 (3 + 3); seven patient had a combined Gleason score 7 (3 + 4); and two patients had a combined Gleason score 9 (4 + 5) (Table 1.
Amongst the 18 patients with non-malignant disease, 1 had evidence of ASAP (atypical small acinar proliferation) and 1 had evidence of HGPIN (high grade prostatic intraepithelial neoplasia).
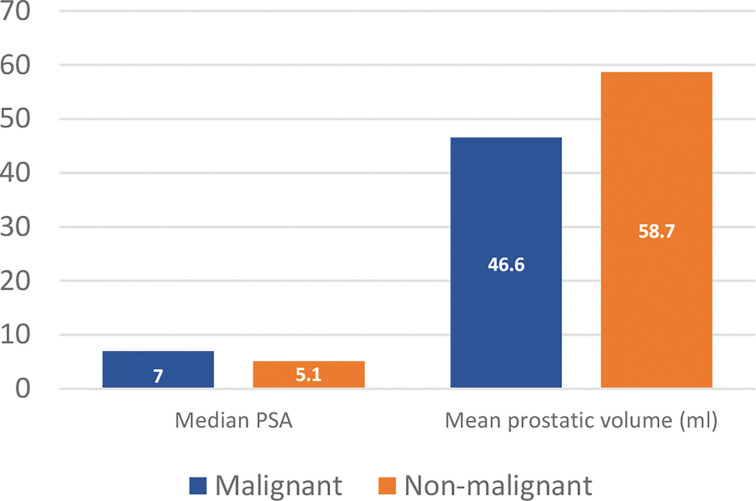
Mean PSA volume for patients with malignant lesions was on average higher (7.0) than patients with non-malignant lesions (5.1). Mean prostatic volume however was higher in patients with non-malignant lesions (58.7) than patients with malignant lesions (46.6) (Figure 2). The location of malignant and non-malignant lesions is seen in Figure 4.
Figure 2.
Number of patients.
The vast majority of the lesions seen on MRI scans were found to be in the peripheral zones of the prostate (Figure 3).
Figure 3.
Median PSA and mean prostatic volume in malignant and non-malignant cases. PSA, prostate-specific antigen.
Results and limitations
The clinical significance of PI-RADS 3 lesions and how best to manage them remains uncertain. In the literature, there is significant variability in terms of the detection rate of cancer in patients with PI-RADS 3 lesions. Within our cohort of 32 biopsied PI-RADS 3 patients, 43% of patients were found to have had a malignant prostatic adenocarcinoma on histology. The remaining 56% had non-malignant findings. Of those with malignant disease, there was a higher median PSA and lower mean prostatic volume.
Limitations
Margin of difference between malignant and non-malignant disease is small – hence, supporting/reinforcing the “equivocal” nature of PI-RADS 3 lesions
Small sample size – only 45 patients with PI-RADS 3 lesions were analysed
This was a single centre study and given the wide variation in the literature of the prevalence/likelihood of prostate cancer in biopsied PI-RADS 3 lesions, these findings cannot be generalised.
Patient factors not taken into account, e.g. frailty, functional status, past medical history, anticoagulants, risk factors - ?in comparison to other Trusts, do we a higher than average detection rate
Conclusions
Ultimately, an ultrasound-guided prostate biopsy in patients with PI-RADS 3 remains of paramount importance when distinguishing malignant vs non-malignant lesions. A multicentre data of MRI findings with PI-RADS 3 scores is required to yield a sample size large enough to carry out statistical analysis, and in turn produce data that may potentially be generalisable enough to influence future clinical guidelines and service provision. PSA and prostatic volume could be used to investigate correlations between PSA or prostatic volume and malignancy.
Figure 4.
Outcome measurements and statistical analysisLocation of lesion. Inner ring depicting malignant cases, outer ring depicting non-malignant cases.
Contributor Information
Sarmad Aslam, Email: sarmad.aslam@nhs.net.
Jeffrey Tsang, Email: jeffrey.tsang@nhs.net.
Ian Bickle, Email: ian.bickle@nhs.net.
Ali Saiepour, Email: Ali.saiepour@nhs.net.
REFERENCES
- 1. Cancer registration statistics, england - office for national statistics. [Internet]. OnsGovUk 2019. [Google Scholar]
- 2. mpMRI [Internet . Prostate Cancer UK. 2021. Available from: https://prostatecanceruk.org/about-us/projects-and-policies/mpmri
- 3. Choyke PL. A grading system for extraprostatic extension of prostate cancer that we can all agree upon? Radiol Imaging Cancer 2020; 2: e190088. doi: 10.1148/rycan.2019190088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bickle I. Diffuse prostate cancer - PIRADS 3 | Radiology Case | Radiopaedia.org [Internet]. 2021. Available from: https://radiopaedia.org/cases/diffuse-prostate-cancer-pirads-3?lang=gb
- 5. Ahdoot M, Lebastchi AH, Long L, Wilbur AR, Gomella PT, Mehralivand S, et al. Using prostate imaging-reporting and data system (pi-rads) scores to select an optimal prostate biopsy method: a secondary analysis of the trio study. Eur Urol Oncol 10, 2021: S2588-9311(21)00048-1. doi: 10.1016/j.euo.2021.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]