Abstract
Background
Physical restraints (PR) are commonly used in geriatric long‐term care. Restraint‐free care should be the aim of high quality nursing care.
Objectives
To evaluate the effectiveness of interventions to prevent and reduce the use of physical restraints in older people who require long‐term nursing care (either in community nursing care or in residential care facilities).
Search methods
The Cochrane Dementia and Cognitive Improvement Group’s Specialized Register, MEDLINE, EMBASE, CINAHL, PsycINFO, LILACS, a number of trial registers and grey literature sources were searched on 7 September 2009. The following search terms were used: "physical restraint*", bedrail*, bedchair*, "containment measure*, elderly, "old people", geriatric*, aged, "nursing home*", "care home*", "geriatric care", "residential facilit*".
Selection criteria
Individual or cluster‐randomised controlled trials comparing an intervention aimed at reducing the use of physical restraints with usual care in long‐term geriatric care settings.
Data collection and analysis
Two reviewers independently assessed the retrieved articles for relevance and methodological quality and extracted data. Critical appraisal of studies addressed risk of bias through selection bias, performance bias, attrition bias, and detection bias, as well as critera related to cluster designa. We contacted study authors for additional information where necessary. PR were defined heterogeneously throughout the studies. Not all studies offered sufficient data for aggregated data meta‐analysis, and therefore study results are presented in a narrative form.
Main results
Five cluster‐randomised controlled studies met the inclusion criteria. All of them investigated educational approaches. Two studies offered consultation in addition and two other studies offered guidance for nursing staff in addition. Four studies examined nursing home residents and one study residents in group dwelling units. No studies in community settings were included. Three studies included only one or two nursing homes per study condition. Overall, methodological quality of studies was low.
The studies revealed inconsistent results. One study in the nursing home setting documented an increase of PR use in both groups after eight months, while the other three studies found reduced use of PR in the intervention groups after seven and 12 months of follow up respectively. The single study examining residents in group dwelling units found no change in PR use in the intervention group after six months whereas PR use increased significantly in the control group.
Authors' conclusions
There is insufficient evidence supporting the effectiveness of educational interventions targeting nursing staff for preventing or reducing the use of physical restraints in geriatric long‐term care.
Plain language summary
Interventions for preventing and reducing the use of physical restraints in long‐term geriatric care
In geriatric long‐term care, physical restraints (PR) such as bedrails and belts in bed or chair are commonly used. Nurses justify them as safety measures, primarily for the prevention of falls, for controlling disruptive behaviour and for the safe use of medical devices. However, it is questionable whether PR are effective and safe devices. There is evidence of various adverse effects such as injuries, reduced psychological well‐being or decreased mobility related to the use of PR. Therefore, restraint‐free care should be the aim of high quality nursing care. We reviewed whether interventions aimed at preventing and reducing the use of PR in geriatric long‐term care settings are effective. We identified five small‐sized randomised controlled studies suitable for inclusion. All studies examined educational interventions targeted at nursing staff. Four studies investigated residents in nursing homes and one in group dwelling units. The methodological quality of all studies was limited. Results of the studies were inconsistent. One study with higher methodological quality showed no reduction in PR use. Three other studies with lower methodological quality found their intervention to be effective. Thus, current evidence on interventions for the reduction or prevention of PR use in long‐term geriatric care does not support a clear conclusion. Ongoing and unpublished research might alter the results of the review.
Background
The use of physical restraints (PR) with older people has been reported as common practice in different countries (de Vries 2004). Many international studies have investigated the frequency of PR use in institutional long‐term nursing care facilities. Recently, epidemiological studies demonstrated pronounced variation among centres both between and within countries (Feng 2009; Meyer 2009). Limited knowledge exists about the number and type of PR used in community nursing care for older people (de Veer 2009).
PR include any devices, equipment or aids designed to confine a resident’s bodily movements or free body movement to a preferred position, e.g. bilateral bedrails, limb or trunk belts, and fixed tables on a chair or chairs that prevent persons from getting up (Evans 2002a). The use of PR is usually justified by nurses as a safety measure, primarily for the prevention of falls Evans 2002a, Hamers 2005. Control of disruptive behaviour, safe use of medical devices and other reasons have also been reported (Hamers 2005). On the other hand, questions have been raised about the justification for and consequences of the use of PR in older people. Considering the current evidence, it is questionable whether PR use can be justified in terms of controlling psychomotor agitation, reducing the risk of falling or fall‐related injuries and whether PR are effective and safe devices. Observational studies have suggested that PR are associated with various adverse effects (Evans 2002a). Case reports and case series have described direct injuries and mortality related to PR use, for example by falls due to bedrail failure or by fatal entrapment (Healey 2008). Social and psychosocial adverse events such as reduced psychological well‐being or decreased mobility have been reported to be associated with PR (Castle 2009; Engberg 2008; Evans 2002a). However, the validity of these analyses is weak (Healey 2008). Several determinants of PR use have been suggested. Cognitive impairment and disruptive behaviour have been reported consistently as being associated with PR use (Huizing 2007; Karlsson 1996; Meyer 2009; Sullivan‐Marx 1999; Tinetti 1991). It is unclear whether institutional characteristics, such as staff mix, significantly influence decisions on PR use (Huizing 2007; Meyer 2009). The “philosophy” of care (i.e. attitudes) and the beliefs of nursing staff are suspected to be powerful determinants of PR use as a routine measure (Meyer 2009).
A restraint‐free nursing care environment has been recommended as the standard of care, while anything less has been claimed to be substandard (Flaherty 2004). Accordingly, in recent decades efforts have been made to reduce the use of PR. Programmes to reduce the use of physical restraints with older people were first introduced in the US in the 1980s (Castle 1998). A number of studies have been conducted in hospitals and nursing homes. The systematic review by Evans 2002b analysed 13 studies, including only one randomised controlled trial (RCT). Since then, a number of randomised controlled studies have been conducted (Capezuti 2007; Huizing 2009a; Testad 2005; Testad 2010). All interventions were designed as complex interventions, consisting of different components including educational sessions aimed at changing nurses’ attitudes to PR use and information about and implementation of alternatives to the use of physical restraints. Some interventions targeted members of different professions, e.g. physicians, nurses and social workers. Most studies addressed nurses only (Evans 2002b).
Objectives
To evaluate the effectiveness of interventions for preventing and reducing the use of physical restraints in older people who require long‐term nursing care (either in community nursing care or in residential care facilities).
To evaluate these complex interventions by retrieving detailed data on implementation.
To highlight the quality and quantity of research evidence available and to set an agenda for future research.
Methods
Criteria for considering studies for this review
Types of studies
All individual or cluster‐randomised controlled trials in which older adults or groups of older adults requiring long‐term nursing care were allocated either to a restraint reduction programme or usual care (control group). Studies comparing two types of programmes were also included.
Types of participants
Older people of either gender requiring long‐term nursing care irrespective of their cognitive status.
Types of interventions
All interventions or groups of interventions comprising a restraint reduction or prevention programme. Interventions containing drug therapy were excluded. Interventions were categorised as follows:
1. Educational interventions: These interventions included either direct‐to‐caregiver programmes or programmes addressing disseminators who distributed the programmes’ contents. We expected a range of different approaches varying, for example, in terms of length and content. Educational programmes included all or any of the following content: impact of PR, residents’ rights and autonomy, myths and misconceptions about the use of physical restraints, ethical issues, legal aspects, restraint minimisation, risks and adverse outcomes of physical restraint use, reasons for and management of specific behavioural problems (reasons and/or management), and alternatives to physical restraints (Evans 2002b). Following the ‘framework for design and evaluation of complex interventions’, it was not possible to extract the effective or ineffective components of the educational programmes (Craig 2008); therefore, components of included programmes were analysed in detail if possible.
2. Organisational interventions: Organisational approaches included interventions aimed at changing organisational policies, for example through introduction of special ‘physical restraint nurses’, counselling by nurse specialists, increased involvement of family members, or simply limiting access to PR equipment.
3. Interventions providing restraint alternatives: These interventions included the provision of any device, material or other intervention to be used instead of PR or to reduce the need for PR. Comprehensive lists of potential alternatives have been published previously (Joanna Briggs Institute 2002).
4. Other interventions: All other interventions which did not fit into one of the three categories mentioned above; also interventions comprising a combination of these categories.
For the purposes of this review, PR was defined as: "any device, material or equipment attached to or near a person’s body and which cannot be controlled or easily removed by the person and which deliberately prevents or is deliberately intended to prevent a person’s free body movement to a position of choice and/or a person’s normal access to their body" (Evans 2002a; Retsas 1998). The use of psychotropic medication aiming to control disruptive behaviour (‘chemical’ restraint) was beyond the scope of this review, since the mode of action is considerably different.
Types of outcome measures
Primary outcomes
Number or proportion of residents with at least one PR,
Prevention of PR (i.e. preventing the introduction of new PR),
Reduction of PR (i.e. withdrawing previously‐used PR).
Secondary outcomes
Type of PR
Duration of PR use
Prescription of psychotropic drugs
Residents' and caregivers' quality of life
Adverse effects of the interventions employed
Duration of effect of the interventions
Injuries and deaths during the study period
Search methods for identification of studies
See Cochrane Dementia and Cognitive Improvement Group methods used in reviews.
The Cochrane Dementia and Cognitive Improvement Group’s Specialized Register, MEDLINE, EMBASE, CINAHL, PsycINFO, LILACS, a number of trial registers and grey literature sources were searched on 18 September 2008 and updated on 7 September 2009. The Specialized Register contains records from MEDLINE, EMBASE, CINAHL, PsycINFO, LILACS, many trial databases and grey literature sources and is updated regularly. In addition, reference lists of retrieved articles were checked for additional trials. Experts in the field were contacted to identify unpublished or ongoing studies. Hand search for abstracts of the following scientific congresses was performed in order to retrieve unpublished studies: IAGG World Congress of Gerontology & Geriatrics, The Gerontological Society of America’s Annual Scientific Meeting, Congress of the European Union Geriatric Medicine Society, European Congress of Gerontology.
The following search terms were used: ((physical restraint*) OR bedrail* OR bedchair* OR containment measure*) AND ((elderly OR (Old people) OR geriatric* OR aged OR (nursing home) OR (care home) OR (geriatric care) OR (residential facilit*)) AND ((randomized controlled trial) OR (controlled clinical trial) OR randomized OR groups)). See Appendix 1 for the MEDLINE search strategy.
Data collection and analysis
Selection of studies
Titles and abstracts of citations obtained from the search were examined independently by two review authors and obviously irrelevant articles were discarded. The two authors independently assessed the retrieved articles for inclusion in the review according to the inclusion criteria mentioned above. Disagreements were resolved by discussion or, if necessary, referred to a third review author.
Quality assessment
Quality criteria were developed by the authors of the review, following the Cochrane Handbook for Systematic Reviews of Interventions version 5.0.2 (Higgins 2009). Two authors independently assessed methodological quality of studies in order to identify any potential sources of systematic bias. Criteria for appraisal of studies were internal validity and low risk of bias through selection bias, performance bias, attrition bias, and detection bias. Since cluster‐randomised trials were considered for inclusion, design‐related criteria for these types of studies were applied (Campbell 2004; Hahn 2005; Puffer 2003). The following main criteria were assessed (for a complete list of items assessed for quality assessment see Appendix 2).
Sequence generation
Allocation concealment
Recruitment bias
Baseline imbalance between groups
Outcome assessors blinded to treatment allocation
Loss to follow‐up of clusters
Methods of analysis adequate for cluster‐randomised controlled trials.
If the description of the items was unclear or missing, the corresponding author of the trial was contacted to obtain the required data. Study validity was determined by categorising individual studies into low, moderate, or high risk of bias.
Data extraction
Data were extracted from the publications by two independent reviewers using a standardised form and were checked for accuracy. The results were discussed and in case of disagreement a third reviewer was called in to reach consensus. If necessary, study authors were contacted to obtain additional data for enhanced risk of bias assessment.
Data analysis
A data check revealed a pronounced clinical heterogeneity in terms of definitions of PR (for details see ‘Definition of physical restraints and methods of data collection’). Also, the components of the tested interventions and the duration and frequencies of educational sessions differed between studies. Two studies revealed pronounced baseline differences in prevalence of PR between groups. In one study the results were published as mean number of PR per week. Given these inconsistencies, we considered a meta‐analysis on published data was not feasible. Thus, we tried to conduct an individual patient data (IPD) meta‐analysis. We invited the authors to make their individual patient data accessible. All authors agreed to participate. However, only two were able to deliver their data in time and three others notified us that their data would be available at a later date. Additional data from an ongoing study (Haut 2009) are expected in autumn 2010. Consequently, we decided to prepare a first version of this review in a narrative form alongside ongoing collection of IPD in order to prepare a prompt update of this review.
Results
Description of studies
Results of the search
The following results were retrieved from the searches:
| Source | Date Range Searched | Hits Retrieved |
| Medline (Pubmed) | Searched 7 September 2009 | 68 |
| Embase (Ovid SP) | Searched 7 September 2009 | 34 |
| PsycInfo (Ovid SP) | Searched 7 September 2009 | 7 |
| Cinahl (Ovid SP) | Searched 7 September 2009 | 11 |
| Lilacs (Bireme) | Searched 7 September 2009 | 0 |
| CDCIG SR | Searched 7 September 2009 | 71 |
| CENTRAL (The Cochrane Library) | Issue 4 2009 | 34 |
| ISTP Conference Proceedings http://portal.isiknowledge.com/portal.cgi | Searched 7 September 2009 | 4 |
| Australian Digital Theses Program http://adt.caul.edu.au/ |
Searched 7 September 2009 | 0 |
| Canadian Theses and Dissertations http://www.collectionscanada.ca/thesescanada/index‐e.html |
Searched 7 September 2009 | 2 |
| DATAD http://www.aau.org/datad/backgrd.htm |
Searched 7 September 2009 | 0 |
| WHO trials register http://www.who.int/ictrp/search/en/ | Searched 7 September 2009 | 9 |
| Current Controlled trials: Meta Register of Controlled trials (mRCT) http://www.controlled‐trials.com/ |
Searched 7 September 2009 | 6 |
| ISRCTN Register |
Searched 7 September 2009 together with mRCT | 0 |
| Nederlands Trial Register http://www.trialregister.nl/trialreg/index.asp | Searched 7 September 2009 | 1 |
| ClinicalTrials.gov http://www.ClinicalTrials.gov |
Searched 7 September 2009 with mRCT | 0 |
| IPFMA Clinical Trials Register www.ifpma.org/clinicaltrials.html |
Searched 7 September 2009 | 0 |
| UMIN Japan Trial Register http://www.umin.ac.jp/ctr/ |
Searched 7 September 2009 | 0 |
| ISI Web of Knowledge | Searched 7 September 2009 | 49 |
A total of 160 titles and abstracts were screened for relevance, and 27 full text publications were reviewed. Four publications fulfilled the eligibility criteria (Evans 1997; Huizing 2009a; Huizing 2009b; Testad 2005). Two publications (Huizing 2009a; Huizing 2009b) reported on the same study. The final report was used as primary source of data Huizing 2009a. One ongoing trial was identified in a trial register. The senior investigator of this study made the manuscript available before publication (Pellfolk 2010). One study author informed us about another study by his working group which had been accepted for publication and made the manuscript available (this study was not listed the trial registers searched) (Testad 2010). We identified one unpublished study (Koczy 2005). Despite repeated requests, the authors did not make the study results accessible. Two studies (Gulpers 2010; Haut 2009) were still ongoing. Thus, we finally included five studies in this review.
Included studies
Four studies were conducted in nursing homes, and one study (Pellfolk 2010) in group dwelling units. No studies were identified that investigated older people in community dwellings. In all studies nursing homes (Evans 1997; Testad 2005; Testad 2010), nursing home wards (Huizing 2009a) or group dwelling units (Pellfolk 2010) were randomised to either an intervention or a control group. In three out of five studies (Evans 1997; Testad 2005; Testad 2010) study groups consisted of only one or two nursing homes. One study compared two intervention groups with one control group (Evans 1997). Two studies were carried out in Norway, one in the Netherlands, one in Sweden, and one in the United States. A total of 802 residents was allocated to the intervention and 749 to the control groups.
Duration of follow‐up
Follow‐up ranged from six (Pellfolk 2010) to 12 months (Evans 1997, Testad 2010) (see Figure 1).
1.
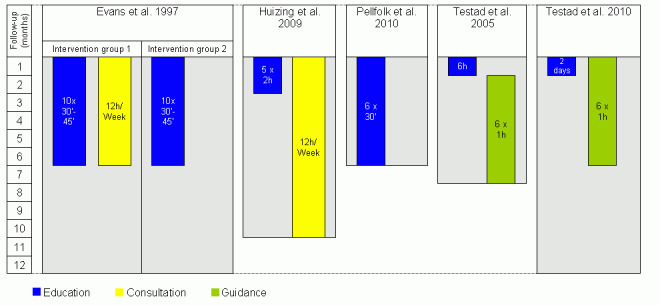
Overview of the components of the interventions.
Definition of physical restraints and methods of data collection
Definitions of PR were heterogeneous among studies. Evans 1997 and Pellfolk 2010 counted all measures as PR that inhibit a person’s free physical movement, e.g. belts or chairs with tables, whereas bedrails were excluded. Testad 2005, Testad 2010 and Huizing 2009a defined PR more comprehensively as any limitation of an individual’s freedom of movement, including belts or chairs with fixed tables, but also restrictive clothes (e.g. sleeping suits) and electronic measures which could restrict a person's movement (e.g. sensor mats or motion alarm systems). Testad 2010 defined two different modes of action in the use of RP: structural and interactional restraints. Structural restraints were defined as PR aiming at protecting the resident through structural measures and not linked to treatment or care giving activities, e.g. locked doors on the ward, electronic surveillance, bedrails and belts. Interactional restraints were linked to treatment or care giving activities, e.g. force or pressure in medical examination, treatment, or in activity of daily living procedures. Since the underlying concept of interactional restraints is related more to elder abuse than to PR, we included only structural restraints for this review.
In the study by Evans 1997 PR use was surveyed by trained observers (n=18), visiting all residents 18 times within 72 hours. The visits covered all three shifts and the order of visits was randomised to prevent PR removal by staff. In the study by Huizing 2009a trained observers (n=11) rated the use of PR by visiting wards four times (morning, afternoon, evening, night) within 24 hours. Visits were unannounced. Testad 2005, Testad 2010 rated the use of PR during the previous seven days through standardised interviews with the residents’ nurse in charge conducted by a trained research nurse (Kirkevold 2004). In Pellfolk 2010 nurses documented PR using a special documentation sheet.
Setting and participants
Evans 1997 included nursing homes in the area of Philadelphia, USA. All residents aged 60 years and older were included. Huizing 2009a included gerontopsychiatric nursing home wards, where almost all residents had a dementia diagnosis. Residents with Korsakoff’s Syndrome or psychiatric disorders were excluded. Testad 2005 included four nursing homes and claimed that these nursing homes were representative of all Norwegian nursing homes in terms of size and organisation. Only residents with a dementia diagnosis, determined by the Clinical Dementia Rating Scale (CDR), were included. Testad 2010 included four nursing homes (all seven nursing homes in a defined region were invited and four agreed to participate). All residents with dementia, defined as a Functional Assessment Staging (FAST) score ≥ 4, were included. The study by Pellfolk 2010 was conducted in group dwelling units for people with dementia. These were designed as homelike environments for six to eight residents with dementia, including private rooms and communal dining and living rooms. The units were generally locked to prevent residents from leaving. Such units can be organised as single or multiple units, or integrated into nursing homes. Staffing levels are higher than in other long‐term care facilities (staff resident ratio was 0.78 ± 0.12 in the intervention and 0.83 ± 0.18 in the control group).
Description of interventions
In all studies (Evans 1997; Huizing 2009a; Pellfolk 2010; Testad 2005; Testad 2010) the interventions comprised an educational programme. In addition, consultation (Evans 1997; Huizing 2009a) or guidance (Testad 2005; Testad 2010) for nursing staff was offered in four out of five studies. Evans 1997 provided two intervention groups; one offered solely the educational programme (RE group) and one (REC group) offered additional consultation for nursing staff (see Figure 1).
Educational Programmes
Underlying concepts of educational programmes
The educational programme by Huizing 2009a was developed on the basis of a previous educational programme for restraint reduction in hospitals (Dielis‐van Houts 2004). The educational programme by Pellfolk 2010 was based on previous research and the clinical experience of experts in geriatric medicine and nursing. The educational programme by Testad 2010 was based on the ‘practical framework for staff to reduce agitation and use of restraint in the interaction with residents with dementia’; this framework has been developed through clinical practice. Two studies (Evans 1997; Testad 2005) provided no information as to whether their educational programme referred to any underlying theory or was based on an already established programme.
Educational programmes' content and delivery
The educational programmes were administered over a period of one to six months. The total amount of education ranged from six to ten hours, with a different number of educational sessions ranging from one to ten sessions. The duration of individual educational sessions ranged from 30 – 45 minute sessions to full day seminars (for details see Figure 1). Testad 2010 offered a seminar lasting two days. The exact number of hours was not mentioned.
The study by Testad 2010 offered insufficient information on the content of the educational programmes.
Educational programmes covered the following topics:
Information on dementia, aggression and challenging behaviour (Pellfolk 2010; Testad 2005)
Strategies for analysing and handling aggression or challenging behaviour (Evans 1997; Huizing 2009a; Pellfolk 2010)
Information on PR, e.g. legal issues, adverse events, experiences of being restrained, correct use (Evans 1997; Huizing 2009a; Pellfolk 2010)
Decision‐making processes and alternatives to use of PR (Huizing 2009a; Pellfolk 2010; Testad 2005)
Falls and fall prevention (Evans 1997; Pellfolk 2010).
Consultation
Two interventions (Evans 1997, Huizing 2009a) comprised consultation delivered by a nurse specialist at registered nurse (RN) level (Huizing 2009a) or a master’s‐prepared gerontological nurse specialist (Evans 1997). Evans offered six months' consultation for the corresponding intervention group, and Huizing 2009a eight months.
The consultations included:
Multidisciplinary meetings, evaluating the use of physical restraints on individual residents, discussing difficulties in achieving PR free care and stimulating the use of PR alternatives or less restrictive measures (Huizing 2009a).
Discussions about residents with challenging behaviour or history of multiple falls (Evans 1997).
Guidance
Two studies (Testad 2005; Testad 2010) offered a monthly one‐hour guidance session over sixth months following the single educational session. Guidance in the study by Testad 2005 addressed the development of care plans for individual residents, taking into account the content of the educational session. Guidance in the study by Testad 2010 addressed the implementation and reinforcement of new skills.
Control group
In all studies (Evans 1997; Huizing 2009a; Pellfolk 2010; Testad 2005; Testad 2010), no intervention was offered in the control group (usual care). Characteristics of usual care were not reported in any of the studies.
Feasibility/pilot test
None of the studies provided any information on a pilot test or a feasibility test of the intervention.
Implementation of interventions
The educational sessions by Testad 2005; Testad 2010 followed a curriculum. Pellfolk 2010 based the educational sessions on videotapes and used group discussion of clinical vignettes. Evans 1997 audiotaped and reviewed randomly selected educational sessions in order to explore standardised administration. No information on the implementation strategy was published by Huizing 2009a. None of the studies evaluated process of implementing the interventions.
Nurse attendance at educational sessions
Huizing 2009a reported that 90% of staff attended at least four out of five educational sessions. Evans 1997 reported that 81% of nursing staff in intervention group 1 and 78% in intervention group 2 attended at least one out of ten educational sessions, whereas 42% of intervention group 1 and 39% of intervention group 2 attended five or more sessions. In the study by Testad 2010, all the nursing staff attended all the educational and guidance sessions. Pellfolk 2010 and Testad 2005 gave no information on the proportion of nurses attending the educational session.
Nursing staff turnover
Attrition rates of nursing staff were reported in two studies. Testad 2010 reported that 56 staff members (53.8%) in the intervention group and 53 (57.0%) in the control group were still employed at the end of the follow‐up period. Reasons for attrition included retirement, pregnancy, long‐term sick leave, and moving or changing job. In Testad 2005 nursing staff attrition is only presented as the number of nurses who left the study, without reporting the corresponding proportion.
Excluded studies
Studies were excluded because they were not randomised controlled trials or did not meet the inclusion criteria relating to the main outcomes, the participants or the intervention.
Risk of bias in included studies
Authors of all studies were contacted and asked to deliver further information on methodological details not reported in their publications. All authors responded to our requests.
Overall, the methodological quality of the studies was low to moderate. The results of the assessment of methodological quality for the individual studies are presented in the risk of bias tables (see Figure 2; Figure 3) and in Appendix 2 (including information requested from the study authors).
2.
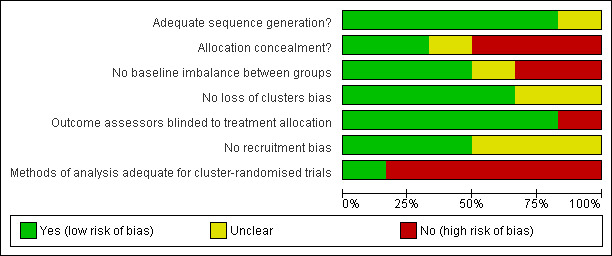
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
3.
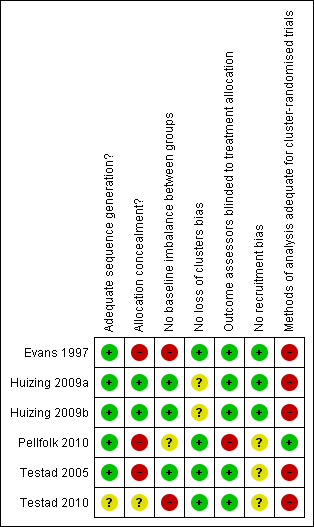
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Sequence generation and allocation concealment
Sequence generation was adequate in four studies (Evans 1997; Huizing 2009a; Pellfolk 2010; Testad 2005); in one study the generation of the randomisation sequence is unclear (Testad 2010). Allocation concealment was adequate in one study (Huizing 2009a).
Recruitment bias
In two studies participants were included before random allocation of clusters (Evans 1997; Huizing 2009a), whereas three studies allocated clusters first (Pellfolk 2010; Testad 2005; Testad 2010).
Baseline imbalance between groups
In the study by Evans 1997 statistically significant differences in baseline characteristics emerged concerning the prevalence of PR (32% in the first intervention group vs. 23% for the second vs. 49% in the control group) and the dependency level of participants (participants in the first intervention group were significantly less dependent than participants in the second intervention and the control group). In Testad 2010 there were differences in prevalence of PR (60% in the intervention vs. 13% in the control group of structural restraints), in the use of psychotropic medications (28% in the intervention vs. 9% in the control group), and in mean agitation scores. In the study by Pellfolk 2010, differences in baseline characteristics were documented for age of participants (mean (SD) intervention group 80.5 ± 9.1 vs. 83.4 ± 6.4 control group; P=0.02) and wandering behaviour (48.6% intervention group vs. 35.0% control group; P=0.02); however, it remains unclear whether these differences constitute a clinically‐relevant imbalance between groups.
Outcome assessors blinded to treatment allocation
In four studies outcome assessors were blinded to group allocation (Evans 1997; Huizing 2009a; Testad 2005; Testad 2010).
Loss of clusters
In four studies none of the clusters were lost to follow‐up (Evans 1997; Pellfolk 2010; Testad 2005; Testad 2010). One cluster out of 15 clusters dropped out of the study by Huizing 2009a.
Methods of analysis adequate for CRCTs
Four of the studies did not consider the cluster design effect in any of their statistical analyses (Evans 1997; Huizing 2009a; Testad 2005; Testad 2010). Only one study (Pellfolk 2010) adjusted the likelihood of being restrained to the cluster design. Intra‐cluster correlation coefficients were not reported in any of the studies.
Effects of interventions
Since we were not able to conduct a meta‐analysis, we decided to prepare this review in a narrative form. All studies presented the proportion of residents with PR as primary outcome. None of the studies reported the number of residents with newly applied or withdrawn PR. The effects of interventions on the primary outcome were presented according to the type of intervention (see ‘Description of interventions’). One study (Pellfolk 2010) presented data from participants with data both at baseline and follow‐up as well as from all participants (including participants admitted during the study follow‐up). For this study, results of both groups will be presented. Secondary outcomes were reported differently according to type. Not all of the studies offered data on all secondary outcomes.
Primary outcome‐ Physical restraints use
Educational programme plus consultation
In the study by Evans 1997, the prevalence in the first intervention group, offering an educational programme and consultation, decreased after twelve months by 18 percentage points (from 32% to 14%). In the control group, prevalence decreased by 6 percentage points (49% to 43%). No information is available regarding whether these changes were statistically significant. Huizing 2009a found a significant increase in PR use in both study groups after ten months. PR use increased in the intervention group by 10 percentage points (from 54% to 64%; P=0.02) and in the control group by 11 percentage points (from 49% to 60%; P=0.007).
Educational programme plus guidance
Testad 2005 documented a decrease in the mean number of PR per week and resident after seven months from 3.3 to 1.5 in the intervention group compared to an increase from 3.1 to 3.7 in the control group, a statistically significant difference between study groups (P= 0.016).
Testad 2010 documented a decrease of restraints by 42 percentage points (from 60% at baseline to 18% after twelve months) in the intervention group, while restraint frequency remained unchanged in the control group (13% at baseline as well as 13% at follow‐up visit).
Educational programme
Evans 1997 showed an absolute decrease of PR use after twelve months by 4 percentage points (23% to 19%) in the second intervention group. In the control group, PR use decreased by 6 percentage points (49% to 43%). No information is available regarding whether these changes were statistically significant.
For participants with data at both baseline and follow‐up (n=288), the study by Pellfolk 2010 showed an almost unchanged proportion of PR use after 6 months in the intervention group (21.5% to 20.1%), while PR use increased significantly in the control group (from 20.1% to 38.1%; P<0.001). The difference between the study groups was statistically significant (P=0.001). Residents in the intervention group were less likely to be physically restrained at follow‐up (OR 0.21; 95% CI 0.08‐0.57; P= 0.002). For all participants (baseline n=353/ follow‐up n=350), PR use decreased significantly in the intervention group (25.7 to 16.8; P=0.03) and increased non‐significantly in the control group (24.7 to 33.3). The difference between groups was statistically significant (P=0.001).
Secondary outcomes
Types of restraints
Only one study presented results on types of restraints (Huizing 2009a). In this study, bilateral bedrails were the most commonly used measures (45%). Other measures used were belts in chairs (10%), belts in beds (9%), and restraining sleep suits (8%). At baseline, study groups did not differ significantly with regard to the type of PR measures. In the intervention group the use of deep or tipped chairs increased significantly from baseline to follow‐up from 6% to 20% (P=0.001). The use of infrared systems also increased significantly from 2% at baseline to 9% at follow‐up (P=0.004). In the control group, the use of bilateral bedrails increased significantly from baseline to follow‐up (45% to 52%; P=0.004). The use of sleeping suits differed significantly between groups at follow‐up (4% in the intervention group vs. 17% in the control group).
Multiple restraints
Only one study reported results for multiple restraints. Huizing 2009a documented 17% of the participants with two different types of PR, 10% with three and 2% with four different measurements within 24 hours (mean types of PR per resident 0.93 ± 1.10). No significant difference in the frequency of multiple restraints was found between study groups at baseline and follow‐up. In both groups multiple restraints significantly increased (P= 0.04 respectively P=0.002).
Restraint intensity
Restraint intensity indicates the number of observations per resident with PR in 24 hours. Only one study by Huizing 2009a provided data on this outcome measure. The mean number of observations per resident with PR in a 24‐hour period at baseline was 1.36 ± 1.62. During follow‐up PR intensity increased significantly in both study groups (P=0.001 for both groups).
Psychotropic medications
A further publication (Siegler 1997) about Evans 1997 reported a non‐significant increase in residents with at least one neuroleptic medication in both intervention groups from baseline to follow‐up (RE from 13.5% to 15.5%, REC from 18.2% to 19.0%). In the control group, the proportion of residents with at least one neuroleptic medication decreased significantly from 18.6% to 11.3% (P=0.014). Benzodiazepines significantly decreased in all study groups (RE from 37.2% to 27.0%, REC from 22.3% to 18.2 %, and control group from 32.8% to 26.6%). In the study by Testad 2005 psychotropic medication decreased in the intervention group from 71% to 55% and in the control group from 61% to 52%. Pellfolk 2010 documented no difference in benzodiazepines and neuroleptics between study groups. In the intervention group psychotropic medication was unchanged from baseline to follow‐up (benzodiazepine from 31.7% to 31.9% and neuroleptics from 48.6% to 47.9%). In the control group, the use of psychotropic medication decreased non‐significantly (benzodiazepine from 30.2% to 22.8% and neuroleptics from 43.9% to 38.6%). In the study by Testad 2010, study groups showed significant baseline differences in the frequency of participants with at least one psychotropic medication (28% intervention vs. 9% control group; P=0.03). At follow‐up, psychotropic medication remained nearly unchanged in both study groups (intervention group from 28% to 31.8%, control group from 8.6 to 8.7%).
Falls and fall‐related injuries
In the study by Evans 1997 the control group showed a significantly lower baseline rate of residents with at least one fall event (control 20.1% vs. REC 33.1% and RE 37.5%; P=0.001). At follow‐up the control group had a statistically significant higher number of residents with at least one fall event compared with both intervention groups (control group 53.3% vs. REC 37.8% and RE 32.2; P<0.001). The total number of residents with fall‐related injuries during follow‐up was small. In the REC group no serious fall‐related injuries occurred, in the RE group eight residents experienced at least one fall‐related injury (5.3%), compared with four residents in the control group (2.2%). Pellfolk 2010 assessed the proportion of residents with falls during a one‐month period before and after the intervention in both study groups and documented a non‐significant decrease (intervention group from 11.4% to 10.1%, control group from 14.4% to 8.6%).
No other studies reported on falls and fall‐related injuries.
Adverse outcomes
Some adverse outcomes associated with PR use were included as study outcomes, e.g. falls and fall‐related injuries or psychotropic medication. No further physical or psychological adverse outcomes were reported or discussed in any of the studies.
Discussion
Summary of main results
Five cluster‐randomised controlled trials were included in this review, showing inconsistent results.
One out of four studies investigating nursing homes (Huizing 2009a) documented an increase of PR use in both groups after follow‐up, while the other three studies (Evans 1997; Testad 2005; Testad 2010) found that their interventions reduced the use of PR. The reporting of the study by Huizing 2009a indicated a high methodological quality. The other studies (Evans 1997; Testad 2005; Testad 2010) included only one (Evans 1997) or two (Testad 2005; Testad 2010) nursing homes per study group; therefore, centre effects might have influenced the results. While Testad 2005; Testad 2010 and Huizing 2009a used comparable definitions of PR, Evans 1997 used a more narrow definition (i.e. excluding bedrails). Two studies (Evans 1997; Testad 2010) showed a statistically significant baseline imbalance in PR use between study groups. In summary, the reviewed evidence is inconsistent. Studies of weak methodological quality indicate an effect whereas one study of good quality did not find a reduction in PR. There is insufficient evidence supporting the effectiveness of educational interventions targeting nursing staff for preventing or reducing the use of PR in long‐term geriatric care. Further high quality research is needed.
The fifth study by Pellfolk 2010, investigating an educational restraint reduction approach in group dwelling units, showed an almost unchanged proportion of PR in the intervention group compared to an increase in the control group. The intervention showed a statistically significant effect after including all residents admitted consecutively to the clusters during follow up. Thus, the study suggests a preventive rather than a reductive effect. However, the results of the study were difficult to interpret and comparable studies investigating group dwelling units are lacking.
No studies investigating the community setting could be included.
Overall completeness and applicability of evidence
The number of studies included in this review was small and all studies exhibited at least some methodological shortcomings. Four out of five studies were published after 2005 and we identified one unpublished study (Koczy 2005) and two ongoing studies (Gulpers 2010; Haut 2009). Thus, research activities in the field of restraint reduction should be accelerated.
The included studies demonstrated significant clinical heterogeneity in terms of PR definition and components of the intervention. We were not able to prepare a meta‐analysis based on published aggregated data, and individual patient data was not yet available for all studies. Consequently, we decided to prepare a first version of this review in a narrative form whilst data collection for an IPD is ongoing for a first update of this review.
All studies investigated interventions of a complex nature. Overall reporting of underlying theories, modelling of components, piloting of feasibility and acceptability, and standardised introduction of the intervention in different centres was insufficient or even entirely missing. Usual care, which was the comparator in all studies, was not explained in any study. Therefore, the replicability of the studies and the applicability of the results are limited (MRC 2008).
Studies in the community were lacking.
Quality of the evidence
Overall methodological quality of the studies was low to moderate. Three out of five studies were especially prone to bias since the study groups included only one or two nursing homes. The cluster design of the studies was consistently disregarded. Thus, a unit of analysis bias would have emerged (Hahn 2005; Puffer 2003). It remains unclear to what extent centre effects have influenced the results.
Two studies (Evans 1997; Testad 2010) indicated heterogeneity among study centres due to statistically significant differences in baseline PR prevalence.
Potential biases in the review process
Efforts to minimise the risk of bias have been made throughout the review process. Publication bias is unlikely to affect the results since an intensive literature search covering electronic databases (Cochrane Dementia and Cognitive Improvement Group’s Specialized Register, Medline, Embase, Cinahl, PsycInfo, Lilacs) and trial registers, guided by the Cochrane Dementia and Cognitive Improvement Group, was performed. We tried to obtain unpublished studies via hand searching of abstract books from scientific congresses and through contact with authors of included studies and other experts in the field. Selection of studies, quality appraisal and data extraction were conducted by two independent review authors.
Agreements and disagreements with other studies or reviews
There are no other systematic reviews using high quality methods focusing on interventions aimed at prevention and reduction of PR use in long‐term geriatric care.
Authors' conclusions
Implications for practice.
There is insufficient evidence to support the effectiveness of interventions for preventing or reducing the use of PR in geriatric long‐term care. The review is based on a limited number of studies with various methodological shortcomings.
Implications for research.
The studies showed significant clinical heterogeneity in terms of the components of the interventions and the definitions of PR applied. Bedrails were not always counted as PR. However, bedrails are the most commonly used devices in nursing homes (Meyer 2009). A consensus statement for conducting clinical trials aimed at PR reduction comparable to those published for fall injury prevention trials (Lamb 2005) or hip protectors trials (Cameron 2010) could help overcome the arbitrariness of research methods and PR definition.
Only one study investigated group dwelling units for persons with dementia and no studies in the community setting could be identified. For both settings further studies are needed.
Researchers in the field of PR reduction are urgently requested to put more weight on the careful development of their complex interventions including theory‐based modelling of components and pilot testing of feasibility and acceptability.
Evaluation studies should adhere to the best available methodological standards, especially in terms of placing more emphasis on well‐designed cluster‐randomised controlled trials with rigorous statistical methods adjusting for cluster design.
Reporting of complex interventions should comply with existing reporting statements, e.g. CONSORT Statement for randomised trials of non‐pharmacological interventions (Boutron 2008) or cluster‐randomised controlled trials (Campbell 2004), as well as with reporting guidelines specific to complex interventions (Lenz 2007; MRC 2008; Shepperd 2009).
What's new
| Date | Event | Description |
|---|---|---|
| 10 March 2011 | Amended | Figures 1 and 2 corrected |
Acknowledgements
We acknowledge the contributions of the consumer editors Johanna Waßmuß (Nurse Manager, Max‐Brauer‐Nursing Home, Hamburg, Germany) and Helga Schneider‐Schelte (German Alzheimer Society, Berlin, Germany) to the development of the protocol. We also thank Pia von Lützau for her contributions to the development process of the review, in particular for handsearching the abstract books and data preparation.
We would also like to acknowledge the Cochrane dementia and cognitive improvement review group for their support.
Appendices
Appendix 1. Sources searched and search strategies used
| Source | Search strategy |
| Medline (Ovid SP) | 1. physical restraint*.mp. 2. (bedrail* or "bed rail*").mp. 3. (bedchair* or "bed chair*").mp. 4. "containment measure*".mp. 5. exp Restraint, Physical/ 6. Education, Nursing/ 7. 6 or 4 or 1 or 3 or 2 or 5 8. elderly.mp. 9. ("old people" or "old person*").mp. 10. geriatric*.mp. 11. aged.mp. 12. ("nursing home*" or nursinghome).mp. 13. "care home*".mp. 14. ("residential home*" or "residential facilit*").mp. 15. Aged/ 16. Residential Facilities/ 17. 11 or 9 or 12 or 15 or 14 or 8 or 16 or 10 or 13 18. 7 and 17 19. randomized controlled trial.pt. 20. controlled clinical trial.pt. 21. randomi?ed.ab. 22. randomly.ab. 23. trial.ab. 24. groups.ab. 25. 22 or 21 or 24 or 23 or 19 or 20 26. (animals not (humans and animals)).sh. 27. 25 not 26 28. 27 and 18 29. (200809* or 200810* or 200811* or 200812*).ed. 30. 2009*.ed. 31. 30 or 29 32. 28 and 31 |
| Embase (Ovid SP) | 1. (Physical restraint*).mp. 2. bedrail*.mp. 3. bedchair*.mp. 4. (Containment measure*).mp. 5. 1 OR 2 OR 3 OR 4 6. elderly.mp. 7. (old people).mp. 8. geriatric*.mp. 9. aged.mp. 10. (nursing home).mp. 11. (care home).mp. 12. (geriatric care).mp. 13. (residential facility*).mp. 14. 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 15. (randomized controlled trial).mp. 16. (controlled clinical trial).mp. 17. randomized.mp. 18. groups.mp. 19. 200809*.em. OR 200810*.em. OR 200811*.em. OR 200812*.em. 20. 2009*.em. 21. 19 OR 20 22. 15 OR 16 OR 17 OR 18 23. 22 AND 14 AND 5 24. 23 AND 21 |
| Psycinfo (Ovid SP) | 1. Physical restraint*.mp. 2. bedrail*.mp. 3. "bed rail*".mp. 4. (bedchair* or "bed chair*").mp. 5. Containment measure*.mp. 6. 4 or 1 or 3 or 2 or 5 7. exp Physical Restraint/ 8. 6 or 7 9. elderly.mp. 10. ("old people" or "old person*").mp. 11. geriatric*.mp. 12. aged.mp. 13. ("nursing home*" or nursinghome).mp. 14. "care home*".mp. 15. ("residential home*" or "residential facilit*").mp. 16. exp Residential Care Institutions/ 17. 11 or 9 or 12 or 15 or 14 or 10 or 13 or 16 18. exp Clinical Trials/ 19. randomized controlled trial.mp. 20. controlled clinical trial.mp. 21. randomized.mp. 22. groups.mp. 23. (sep or oct or nov or dec).mo. and "2008".mp. [mp=title, abstract, heading word, table of contents, key concepts] 24. "2009".yr. 25. (sep or oct or nov or dec).mo. and "2008".yr. 26. 25 or 24 27. 22 or 21 or 18 or 19 or 20 28. 27 and 8 and 17 29. 28 and 26 |
| Cinahl (Ebsco host) | S1 TX physical restraint* S2 TX bedrail* S3 TX bedchair* S4 TX “containment measure*” S5 S1 OR S2 OR S3 OR S4 S6 TX elderly S7 TX “old people” or “old person*” S8 TX geriatric* S9 TX aged S10 TX “nursing home*” or nursinghome S11 TX “care home*” S12 TX “residential home*” or “residential facility*” S13 S6 or S7 or S8 or S9 or S10 or S11 or S12 S14 S5 and S13 S15 TX “randomized controlled trial” S16 TX “controlled clinical trial” S17 AB random* S18 AB trial S19 AB groups S20 S15 or S16 or S17 or S18 or S19 S21 S14 and S20 S22 EM 2008 S23 EM 2009 S24 S22 or S23 S25 S14 and S24 |
| Lilacs (Bireme) | (“physical restraint*” AND (elderly OR geriatr$)) AND (2008 OR 2009) |
| CDCIG SR | (“physical restraint*” OR “containment measure*”) AND (2008 OR 2009) |
| Meta Register of Controlled Trials (mRCT): includes ‐ ISRCTN Register; Action Medical Research; Medical Research Council (UK); National Health Service Research and Development Health Technology Assessment Programme (HTA); National Institutes of Health (NIH) ‐ randomized trial records held on NIH ClinicalTrials.gov website; The Wellcome Trust; UK Clinical Trials Gateway | “physical restrain%” AND (2008 or 2009) |
| Umin Japan Trial Register | “physical restraints” OR “physical restraint” OR “bedrail” OR “trunk belts” |
| WHO Portal: includes ‐ Australian New Zealand Clinical Trials Registry; ClinicalTrials.gov; ISRCTN; Chinese Clinical Trial Register; Clinical Trials Registry ‐ India; German Clinical Trials Register; Iranian Registry of Clinical Trials; Sri Lanka Clinical Trials Registry; The Netherlands National Trial Register | “physical restraints” |
| CENTRAL (The Cochrane Library) | #1 “physical restraint*” #2 bedrail* #3 bedchair* #4 “containment measure*” #5 #1 or #2 or #3 or #4 #6 elderly #7 “old people” #8 geriatric* #9 aged #10 “nursing home*” #11 “care home*” #12 “geriatric care” #13 “residential facit*” #14 #6 or #7 or #8 or #9 or #10 or #12 or #13 #15 #5 and #14 #16 #15 [clinical trials] [date: 2008‐2009] |
| Australasian Digital Theses | “physical restraint*” |
| ISI Web of Knowledge | 1. ((physical restraint*) OR bedrail* OR bedchair* OR containment measure*) AND ((elderly OR (Old people) OR geriatric* OR aged OR (nursing home) Or (care home) OR (geriatric care) Or (residential facilit*)) AND ((randomized controlled trial) OR (controlled clinical trial) OR randomized OR groups)) 2. #1 AND (2008‐2009) [Year Published] |
Appendix 2. Items for quality assessment of included stuidies
| Item | Evans et a. 1997 | Testad et al. 2005 | Huizing et al. 2009 a+b | Pellfolk et al. 2010 | Testad et al. 2010 |
| METHOD | |||||
| Allocation sequence adequately generated | Yes* | Yes* | Yes* | Yes* | Unclear* |
| Allocation adequately concealed | No* | No* | Yes* | No | Unclear* |
| No evidence for cluster imbalance | No | Yes | Yes | Yes | No |
| Clusters lost to follow‐up | 0/3 | 0/4 | 1/15 | 0/40 | 0/4 |
| Participants identified before randomisation | Yes | No* | Yes | No* | No* |
| If no: no evidence for biased selection of participants | ‐‐‐ | Unclear | ‐‐‐ | Unclear | Unclear |
| PARTICIPANTS | |||||
| Inclusion/ exclusion criteria for participants clearly defined | Yes* | Yes* | Yes* | Yes* | Yes |
| Inclusion/ exclusion criteria for clusters clearly defined | Unclear* | Yes* | Yes* | Yes* | Yes* |
| Sample size calculation | Yes* | No* | No* | Yes | Yes* |
| Adequate sample size calculation using methods for cluster randomisation | No* | No* | No* | No* | No* |
| No relevant differences between groups after randomisation | No | Yes | Yes | Unclear | No |
| Loss to follow‐up less 5% of participants | Unclear | Yes | No | Unclear | No |
| Were incomplete data adequately explained | Yes* | Yes* | Yes | No* | Yes |
| INTERVENTIONS | |||||
| 41. All groups treated equally, except of intervention or control | Yes | Yes | Yes | Yes | Yes |
| OUTCOMES | |||||
| Primary outcome clearly stated? | Yes | Yes | Yes | Yes | Yes |
| Method of primary outcome assessment adequate | Yes | Yes | Yes | Yes | Yes |
| Outcome assessors blinded to group allocation | Yes | Yes | Yes | No | Yes |
| Data collection started immediately after randomisation | No* | Unclear* | No* | No* | Yes* |
| RESULTS | |||||
| Intention to treat analysis | Yes | Yes | Yes | Yes | No* |
| Complete reporting of outcome (as scheduled) | Yes | Yes | Yes | Yes | Yes |
| Methods of analysis adequate for cluster‐randomised trials | No | No | No | Yes (partial)* | No* |
| Coefficient of intra‐cluster correlation reported | No | No | No | No* | No* |
| MISCELLANEOUS | |||||
| No evidence for interpretation bias | Yes | Yes | Yes | Yes | Yes |
| Conflicts of interest mentioned | No | No | No | No | Yes |
| Requests to authors required | Yes | Yes | Yes | Yes | Yes |
| * Items marked with an asterisk have been answered by the study authors following personal request. | |||||
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Evans 1997.
| Methods | Cluster‐randomised controlled trial | |
| Participants | Country: USA 3 nursing homes in the area of Philadelphia All residents in each participating nursing home Inclusion criteria: age 60+, non‐comatose, and conversant in English |
|
| Interventions | Intervention 1: educational intervention plus consultation Intervention 2: educational intervention Control: usual care |
|
| Outcomes | Physical restraints status, serious fall‐related injuries, psychotropic medications | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | High risk | |
| No baseline imbalance between groups | High risk | |
| No loss of clusters bias | Low risk | |
| Outcome assessors blinded to treatment allocation | Low risk | |
| No recruitment bias | Low risk | |
| Methods of analysis adequate for cluster‐randomised trials | High risk | |
Huizing 2009a.
| Methods | Cluster‐randomised controlled trial | |
| Participants | Country: The Netherlands 14 nursing home wards from seven nursing homes; region: Kerkrade, Landgraaf and Bocholtz All residents of each participating nursing home ward Exclusion criteria: residents with Korsakoff’s Syndrome and psychiatric diseases. |
|
| Interventions | Intervention: educational intervention plus consultation Control: usual care |
|
| Outcomes | Physical restraint status | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | |
| No baseline imbalance between groups | Low risk | |
| No loss of clusters bias | Unclear risk | One out of 15 clusters was lost to follow‐up |
| Outcome assessors blinded to treatment allocation | Low risk | |
| No recruitment bias | Low risk | |
| Methods of analysis adequate for cluster‐randomised trials | High risk | |
Huizing 2009b.
| Methods | Cluster‐randomised controlled trial | |
| Participants | Country: The Netherlands 14 nursing home wards from seven nursing homes; region: Kerkrade, Landgraaf and Bocholtz All residents newly admitted within study follow‐up. Exclusion criteria: Exclusion criteria: residents with Korsakoff’s Syndrome and psychiatric diseases. |
|
| Interventions | Intervention: educational intervention plus consultation Control: usual care |
|
| Outcomes | Physical restraint status | |
| Notes | Secondary source: Part of the study published in Huizing et al. 2009a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | |
| No baseline imbalance between groups | Low risk | |
| No loss of clusters bias | Unclear risk | One out of 15 clusters was lost to follow‐up |
| Outcome assessors blinded to treatment allocation | Low risk | |
| No recruitment bias | Low risk | |
| Methods of analysis adequate for cluster‐randomised trials | High risk | |
Pellfolk 2010.
| Methods | Cluster‐randomised controlled trial | |
| Participants | Country: Sweden 40 group dwelling units for people with dementia All residents of the included group dwelling units |
|
| Interventions | Intervention: educational intervention Control: usual care |
|
| Outcomes | Residents: physical restraint status, falls, benzodiazepine and neuroleptics' use Staff: knowledge, attitudes (The Perceptions of Restraints Use Questionnaire (PRUQ)) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | High risk | |
| No baseline imbalance between groups | Unclear risk | Unclear |
| No loss of clusters bias | Low risk | |
| Outcome assessors blinded to treatment allocation | High risk | |
| No recruitment bias | Unclear risk | Unclear |
| Methods of analysis adequate for cluster‐randomised trials | Low risk | Only for the likelihood of being restrained, not for sample size calculation, no intra‐cluster correlation coefficient was calculated. |
Testad 2005.
| Methods | Cluster‐randomised controlled trial | |
| Participants | Country: Norway 4 nursing homes Participants: persons with dementia diagnosis (measured by Clinical Dementia Rating Scale) |
|
| Interventions | Intervention: educational intervention plus guidance Control: usual care |
|
| Outcomes | Physical restraints status Agitation (Brief Agitation Rating Scalse, BARS) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | High risk | |
| No baseline imbalance between groups | Low risk | |
| No loss of clusters bias | Low risk | |
| Outcome assessors blinded to treatment allocation | Low risk | |
| No recruitment bias | Unclear risk | Unclear |
| Methods of analysis adequate for cluster‐randomised trials | High risk | |
Testad 2010.
| Methods | Cluster‐randomised controlled trial | |
| Participants | Country: Norway 4 nursing homes; region Rogaland. Participants: persons with dementia diagnosis (Functional Assessment Staging (FAST) score ≥ 4) |
|
| Interventions | Intervention: educational intervention plus guidance Control: usual care |
|
| Outcomes | Physical restraints status (separated in interactional and structural restraints), Agitation (CMAI) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Unclear risk | Not reported |
| No baseline imbalance between groups | High risk | |
| No loss of clusters bias | Low risk | |
| Outcome assessors blinded to treatment allocation | Low risk | |
| No recruitment bias | Unclear risk | Unclear |
| Methods of analysis adequate for cluster‐randomised trials | High risk | |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Branitzki 2005 | Study protocol without results |
| Capezuti 1998 | Primary outcome not physical restraints |
| Capezuti 2007 | No randomised controlled trial |
| Choi 2009 | No randomised controlled trial and not long‐term care setting |
| Dewey 2000 | No randomised controlled trial |
| Ejaz 1994 | No randomised controlled trial |
| Evans 2002b | No randomised controlled trial |
| Frank 1996 | No randomised controlled trial |
| Healey 2008 | No randomised controlled trial |
| Huizing 2006 | Preliminary results |
| Koczy 2005 | Study protocol without results |
| Kotynia‐English 2005 | Aim of the intervention was not the reduction or prevention of the use of physical restraints |
| Levine 1995 | No randomised controlled trial |
| Levine 2000 | No randomised controlled trial |
| McCallion 1999 | Aim of the intervention was not the reduction or prevention of the use of physical restraints |
| Moretz 1995 | Description of the development of an physical restraint reduction program, no results |
| Patterson 1995 | No results |
| Ralphs‐Thibodeau 2006 | No randomised controlled trial |
| Rovner 1996 | Aim of the intervention was not the reduction or prevention of the use of physical restraints |
| Schnelle 1992 | No randomised controlled trial |
| Si 1999 | Not long‐term care setting |
| Siegler 1997 | Primary outcome not physical restraints |
| Steinert 2009 | No randomised controlled trial |
| Toseland 1997 | Aim of the intervention was not the reduction or prevention of the use of physical restraints |
| Woods 2005 | Aim of the intervention was not the reduction or prevention of the use of physical restraints |
Characteristics of ongoing studies [ordered by study ID]
Gulpers 2010.
| Trial name or title | Belt restraint reduction in nursing homes: design of a quasi‐experimental study |
| Methods | Quasi‐experimental longitudinal study |
| Participants | 720 psychogeriatric nursing home residents in 26 wards in 13 dutch psychogeriatric nursing homes |
| Interventions | Educational intervention for nursing home staff, policy change (belt use is prohibited by the nursing home management), nurse specialist and nursing home manager as consultants, availability of alternative interventions |
| Outcomes | Primary outcome: proportion of residents with a belt Secondary outcomes: other types of physical restraints (e.g. bilateral full enclosure bedrails, deep or overturned chairs, chairs with a locked tray table, chairs on a board), psychoactive drug use, number of falls and fall‐related injuries, the use of alternative interventions, cognitive level, activities of daily living (ADL)‐status, ADL‐dependency, and mobility |
| Starting date | 01/10/2008 |
| Contact information | m.gulpers@zw.unimaas.nl |
| Notes |
Haut 2009.
| Trial name or title | Evaluation of an evidence‐based guidance on the reduction of physical restraints in nursing homes: a cluster‐randomised controlled trial |
| Methods | Cluster‐randomised controlled trial |
| Participants | A total of 36 nursing home clusters including approximately 3000 residents will be recruited. Inclusion criteria for clusters: prevalence of at least 20% of physical restraints at baseline |
| Interventions | A structured information programme for nursing staff, information materials for legal guardians and residents' relatives and a one‐day training workshop for nominated nurses |
| Outcomes | Primary outcome: number of residents with at least one physical restraint Secondary outcome: number of falls and fall‐related fractures |
| Starting date | 15/04/2009 |
| Contact information | Gabriele.Meyer@uni‐wh.de |
| Notes |
Contributions of authors
GM and SK initially planned the study; RM, SK, and GM wrote the study protocol. RM and TR selected studies for inclusion/exclusion, evaluated the methodological quality of included trials and extracted data. RM and GM interpreted the study data. RM corresponded with the study authors and wrote the drafts of the review with major contributions by GM. RM and GM started collecting individual patient data from the study authors. GM, SK, and TR contributed to all drafts of the review.
Sources of support
Internal sources
Department of Nursing Science, Faculty of Health, Witten/Herdecke University, Germany.
Unit of Health Sciences and Education, University of Hamburg, Germany.
External sources
Ministry of Education and Research, Germany.
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Evans 1997 {published data only}
Huizing 2009a {published data only}
- Huizing A, Hamers J, Gulpers M, Berger M. A cluster‐randomized trial of an educational intervention to reduce the use of physical restraints with psychogeriatric nursing home residents. Journal of the American Geriatrics Society 2009;57(7):1138‐48. [DOI] [PubMed] [Google Scholar]
Huizing 2009b {published data only}
- Huizing A, Hamers J, Gulpers M, Berger M. Preventing the use of physical restraints on residents newly admitted to psycho‐geriatric nursing home wards. International Journal of Nursing Studies 2009;46(4):459‐69. [DOI] [PubMed] [Google Scholar]
Pellfolk 2010 {published data only}
- Pellfolk T, Gustafson Y, Bucht G, Karlsson S. Effects of a Restraint Minimization Program on Staff Knowledge, Attitudes, and Practice: A Cluster Randomized Trial. Journal of the American Geriatrics Society 2010;58:62‐9. [DOI] [PubMed] [Google Scholar]
Testad 2005 {published data only}
- Testad I, Aasland A, Aarsland D. The effect of staff training on the use of restraint in dementia: a single‐blind randomised controlled trial. International Journal of Geriatric Psychiatry 2005;20:587‐90. [DOI] [PubMed] [Google Scholar]
Testad 2010 {published data only}
- Testad I, Ballard C, Brønnick K, Aarsland D. The effect of staff training on agitation and use of restraint in nursing home residents with dementia: a single‐blind, randomized controlled trial. Journal of Clinical Psychiatry 2010;71(1):80‐6. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Branitzki 2005 {published data only}
- Branitzki S, Koczy P. [ReduFix‐ a study of reducing physical restraint: preventing risk of injury]. Pflege Zeitschrift 2005;58(5):310‐3. [PubMed] [Google Scholar]
Capezuti 1998 {published data only}
- Capezuti E, Strumpf NE, Evans LK, Grisso JA, Maislin G. The relationship between physical restraint removal and falls and injuries among nursing home residents. The journals of gerontology. Series A, Biological sciences and medical sciences 1998;53(1):M47‐52. [DOI] [PubMed] [Google Scholar]
Capezuti 2007 {published data only}
- Capezuti E, Wagner L, Brush B, Boltz M, Renz S, Talerico K. Consequences of an intervention to reduce restrictive side rail use in nursing homes. Journal of the American Geriatrics Society 2007;55:334‐41. [DOI] [PubMed] [Google Scholar]
Choi 2009 {published data only}
- Choi K, Kim J. Effects of an educational program for the reduction of physical restraint use by caregivers in geriatric hospitals. Journal of Korean Academy of Nursing 2009;39(6):769‐80. [DOI] [PubMed] [Google Scholar]
Dewey 2000 {published data only}
- Dewey K, Brill C. Decrease in restraint use in a study of a geropsychiatric unit. Journal of Psychosocial Nursing and Mental Health Services 2000;38(10):14‐8, 44‐5. [DOI] [PubMed] [Google Scholar]
Ejaz 1994 {published data only}
- Ejaz FK, Jones JA, Rose MS. Falls among nursing home residents: an examination of incident reports before and after restraint reduction programs. Journal of the American Geriatrics Society 1994;42(9):960‐4. [DOI] [PubMed] [Google Scholar]
Evans 2002b {published data only}
- Evans D, Wood J, Lambert L. A review of physical restraint minimization in the acute and residential care settings. Journal of Advanced Nursing 2002;40:616‐25. [DOI] [PubMed] [Google Scholar]
Frank 1996 {published data only}
- Frank C, Hodgetts G, Puxty J. Safety and efficacy of physical restraints for the elderly. Review of the evidence. Canadian Family Physician 1996;42:2402‐9. [PMC free article] [PubMed] [Google Scholar]
Healey 2008 {published data only}
- Healey F, Oliver D, Milne A, Connelly J. The effect of bedrails on falls and injury: a systematic review of clinical studies. Age and Ageing 2008;37:368‐78. [DOI] [PubMed] [Google Scholar]
Huizing 2006 {published data only}
- Huizing A, Hamers J, Gulpers M, Berger M. Short‐term effects of an educational intervention on physical restraint use: a cluster randomized trial. BMC Geriatrics 2006;26:6‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koczy 2005 {published data only}
- Koczy P, Klie T, Kron M, Bredthauer D, Rissmann U, Branitzki S, et al. Effectiveness of a multifactorial intervention to reduce physical restraints in nursing home residents with dementia [Effektivität einer multifaktoriellen Intervention zur Reduktion von körpernaher Fixierung bei demenzkranken Heimbewohnern]. Zeitschrift für Gerontologie und Geriatrie 2005;38:33‐9. [DOI] [PubMed] [Google Scholar]
Kotynia‐English 2005 {published data only}
- Kotynia‐English R, McGowan H, Almeida OP. A randomized trial of early psychiatric intervention in residential care: impact on health outcomes. International Psychogeriatrics 2005;17(3):475‐85. [DOI] [PubMed] [Google Scholar]
Levine 1995 {published data only}
- Levine JM, Marchello V, Totolos E. Progress toward a restraint‐free environment in a large academic nursing facility. Journal of the American Geriatrics Society 1995;43(8):914‐8. [DOI] [PubMed] [Google Scholar]
Levine 2000 {published data only}
- Levine JM, Hammond M, Marchello V, Breuer B. Changes in bedrail prevalence during a bedrails‐reduction initiative. Journal of the American Medical Directors Association 2000;1(1):34‐6. [PubMed] [Google Scholar]
McCallion 1999 {published data only}
- McCallion P, Toseland RW, Freeman K. An evaluation of a family visit education program. Journal of the American Geriatrics Society 1999;47(2):203‐14. [DOI] [PubMed] [Google Scholar]
Moretz 1995 {published data only}
- Moretz C, Dommel A, Deluca K. Untied: a safe alternative to restraints. Medsurg Nursing 1995;4(2):128‐32. [PubMed] [Google Scholar]
Patterson 1995 {published data only}
- Patterson JE, Strumpf NE, Evans LK. Nursing consultation to reduce restraints in a nursing home. Clinical Nurse Specialist 1995;9(4):231‐5. [DOI] [PubMed] [Google Scholar]
Ralphs‐Thibodeau 2006 {published data only}
- Ralphs‐Thibodeau S, Knoefel F, Benjamin K, Leclerc A, Pisterman S, Sohmer J, et al. Patient choice: an influencing factor on policy‐related research to decrease bedrail use as physical restraint. Worldviews Evid Based Nurs 2006;3(1):31‐9. [DOI] [PubMed] [Google Scholar]
Rovner 1996 {published data only}
- Rovner BW, Steele CD, Shmuely Y, Folstein MF. A randomized trial of dementia care in nursing homes. Journal of the American Geriatrics Society 1996;44(1):7‐13. [DOI] [PubMed] [Google Scholar]
Schnelle 1992 {published data only}
- Schnelle JF, Newman DR, White M, Volner TR, Burnett J, Cronqvist A, et al. Reducing and managing restraints in long‐term‐care facilities. Journal of the American Geriatrics Society 1992;40(4):381‐5. [DOI] [PubMed] [Google Scholar]
Si 1999 {published data only}
- Si M, Neufeld RR, Dunbar J. Removal of bedrails on a short‐term nursing home rehabilitation unit. Gerontologist 1999;39(5):611‐4. [DOI] [PubMed] [Google Scholar]
Siegler 1997 {published data only}
- Siegler EL, Capezuti E, Maislin G, Baumgarten M, Evans L, Strumpf N. Effects of a restraint reduction intervention and OBRA '87 regulations on psychoactive drug use in nursing homes. Journal of the American Geriatrics Society 1997;45(7):791‐6. [DOI] [PubMed] [Google Scholar]
Steinert 2009 {published data only}
- Steinert T, Bohnet U, Flammer E, Lüchtenberg D, Eisele F. Effects of a training of power and balance on the use of mechanical restraint among in‐patients with dementia [Effekte eines Kraft‐ und Bewegungstrainings auf die Fixierungshäufigkeit bei Demenzpatienten in der stationären gerontopsychiatrischen Versorgung]. Psychiatrische Praxis 2009;36(6):273‐8. [DOI] [PubMed] [Google Scholar]
Toseland 1997 {published data only}
- Toseland RW, Diehl M, Freeman K, Manzanares T, Naleppa M, McCallion P. The impact of validation group therapy on nursing home residents with dementia. Journal of Applied Gerontology 1997;16(1):31‐50. [Google Scholar]
Woods 2005 {published data only}
- Woods DL, Craven RF, Whitney J. The effect of therapeutic touch on behavioral symptoms of persons with dementia. Alternative Therapies in Health and Medicine 2005;11(1):66‐74. [PubMed] [Google Scholar]
References to ongoing studies
Gulpers 2010 {published data only}
- Gulpers MJ, Bleijlevens MH, Rossum E, Capezuti E, Hamers JP. Belt restraint reduction in nursing homes: design of a quasi‐experimental study. BMC Geriatrics 2010;10(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haut 2009 {published data only}
- Haut A, Köpke S, Gerlach A, Mühlhauser I, Haastert B, Meyer G. Evaluation of an evidence‐based guidance on the reduction of physical restraints in nursing homes: a cluster‐randomised controlled trial. BMC Geriatrics 2009;9:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Boutron 2008
- Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P, CONSORT Group. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Annals of Internal Medicine 2008;148(4):295‐309. [DOI] [PubMed] [Google Scholar]
Cameron 2010
- Cameron ID, Robinovitch S, Birge S, Kannus P, Khan K, Lauritzen J, Howland J, Evans S, Minns J, Laing A, Cripton P, Derler S, Plant D, Kiel DP. Hip protectors: recommendations for conducting clinical trials‐an international consensus statement (part II). Osteoporosis International 2010;21(1):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2004
- Campbell MK, Elbourne DR, Altman DG, CONSORT group. CONSORT statement: extension to cluster randomised trials. BMJ 2004;328(7441):702‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Castle 1998
- Castle N, Mor V. Physical restraint in nursing homes: a review of the literature since the nursing home reform act of 1987. Medical Care Research and Review 1998;55:139‐70. [DOI] [PubMed] [Google Scholar]
Castle 2009
- Castle NG, Engberg J. The health consequences of using physical restraints in nursing homes. Medical Care 2009;47(11):1164‐73. [DOI] [PubMed] [Google Scholar]
Craig 2008
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
de Veer 2009
- Veer AJ, Francke AL, Buijse R, Friele RD. The Use of Physical Restraints in Home Care in the Netherlands. Journal of the American Geriatrics Society 2009;57(10):1881‐6. [DOI] [PubMed] [Google Scholar]
de Vries 2004
- Vries O, Ligthart G, Nikolaus T, on behalf of the participants of the European Academy of Medicine of Ageing‐Course III. Differences in period prevalence of the use of physical restraints in elderly inpatients of European hospitals and nursing homes. Journals of Gerontology A, Biological Science Medical Science 2004;59:M922‐3. [DOI] [PubMed] [Google Scholar]
Dielis‐van Houts 2004
- Dielis‐van Houts A, Schuurmans M. The balance between safety, freedom of movement and use of restraints [Een balans tussen: Veiligheid, Vrijheid en Vrijheidsbeperking]. UMC‐Utrecht, Utrecht 2004.
Engberg 2008
- Engberg J, Castle N, McCaffrey D. Physical restraint initiation in nursing homes and subsequent resident health. Gerontologist 2008;48:442‐52. [DOI] [PubMed] [Google Scholar]
Evans 2002a
- Evans D, Wood J, Lambert L, Fitzgerald M. Physical Restraint in Acute and Residential Care. Adelaide, The Joanna Briggs Institute 2002.
Evans 2002b
- Evans D, FitzGerald M. Reasons for physically restraining patients and residents: a systematic review and content analysis. International Journal of Nursing Studies 2002;39(7):735‐43. [DOI] [PubMed] [Google Scholar]
Feng 2009
- Feng Z, Hirdes JP, Smith TF, Finne‐Soveri H, Chi I, Du Pasquier JN, Gilgen R, Ikegami N, Mor V. Use of physical restraints and antipsychotic medications in nursing homes: a cross‐national study. International Journal of Geriatric Psychiatry 2009;24(10):1110‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Flaherty 2004
- Flaherty J. Zero tolerance for physical restraints: difficult but not impossible. Journal of Gerontology 2004;59A:919‐20. [DOI] [PubMed] [Google Scholar]
Hahn 2005
- Hahn S, Puffer S, Torgerson D, Watson J. Methodological bias in cluster randomised trials. BMC Medical research methodology 2005;5(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamers 2005
- Hamers J, Huizing A. Why do we use physical restraints in the elderly?. Zeitschrift für Gerontologie und Geriatrie 2005;38:19‐25. [DOI] [PubMed] [Google Scholar]
Higgins 2009
- Higgins J, Greene S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.2. Available online: http://www.cochrane‐handbook.org. Accessed 01/06/2010. 2009.
Huizing 2007
- Huizing AR, Hamers JP, Jonge J, Candel M, Berger MP. Organisational determinants of the use of physical restraints: a multilevel approach. Social Science and Medicine 2007;65(9):924‐33. [DOI] [PubMed] [Google Scholar]
Joanna Briggs Institute 2002
- Joanna Briggs Institute. Physical Restraint ‐ Pt 2: Minimisation in Acute and Residential Care Facilities. Best Practice 2002;6(4):1‐6. [Google Scholar]
Karlsson 1996
- Karlsson S, Bucht G, Eriksson S, Sandman PO. Physical restraints in geriatric care in Sweden: prevalence and patient characteristics. Journal of the American Geriatrics Society 1996;44(11):1348‐54. [DOI] [PubMed] [Google Scholar]
Kirkevold 2004
- Kirkevold Ø, Engedal K. Prevalence of patients subjected to constraint in norwegian nursing homes. Scandinavian Journal of Caring Sciences 2004;18(3):281‐6. [DOI] [PubMed] [Google Scholar]
Lamb 2005
- Lamb SE, Jørstad‐Stein EC, Hauer K, Becker C, Prevention of Falls Network Europe and Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. Journal of the American Geriatrics Society 2005;53(9):1618‐22. [DOI] [PubMed] [Google Scholar]
Lenz 2007
- Lenz M, Steckelberg A, Richter B, Mühlhauser I. Meta‐analysis does not allow appraisal of complex interventions in diabetes and hypertension self‐management: a methodological review. Diabetologia 2007;50(7):1375‐83. [DOI] [PubMed] [Google Scholar]
Meyer 2009
- Meyer G, Köpke S, Haastert B, Mühlhauser I. Restraint use among nursing home residents: cross‐sectional study and prospective cohort study. Journal of Clinical Nursing 2009;18:981‐90. [DOI] [PubMed] [Google Scholar]
MRC 2008
- Medical Research Council. Developing and evaluating complex interventions: new guidance. Available online: www.mrc.ac.uk/complexinterventionsguidance. Accessed 01/06/2010 2008.
Puffer 2003
- Puffer S, Torgerson D, Watson J. Evidence for risk of bias in cluster randomised trials: review of recent trials published in three general medical journals. BMJ 2003;327(7418):785‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Retsas 1998
- Retsas A. Survey findings describing the use of physical restraints in nursing homes in Victoria, Australia. International Journal of Nursing Studies 1998;35:184‐91. [DOI] [PubMed] [Google Scholar]
Shepperd 2009
- Shepperd S, Lewin S, Straus S, Clarke M, Eccles MP, Fitzpatrick R, Wong G, Sheikh A. Can we systematically review studies that evaluate complex interventions?. PLoS medicine 2009;6(8):e1000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sullivan‐Marx 1999
- Sullivan‐Marx EM, Strumpf NE, Evans LK, Baumgarten M, Maislin G. Predictors of continued physical restraint use in nursing home residents following restraint reduction efforts. Journal of the American Geriatrics Society 1999;47(3):342‐8. [DOI] [PubMed] [Google Scholar]
Tinetti 1991
- Tinetti ME, Liu WL, Marottoli RA, Ginter SF. Mechanical restraint use among residents of skilled nursing facilities. Prevalence, patterns, and predictors. JAMA 1991;265(4):468‐71. [PubMed] [Google Scholar]


