Abstract
Mental health in young people is a public health challenge worldwide, with around one-fifth of university students suffering from a 12-month mental disorder. In low- and middle-income countries (LMICs) of Southeastern Asia, resources for mental health are limited and counseling services are not regularly established at universities. This review aims to determine the prevalence of mental health problems among university students in six ASEAN (Association of Southeast Asian Nations) countries (Cambodia, Laos, Malaysia, Myanmar, Thailand, and Vietnam) and to identify the determinants of mental health. A systematic database search (PubMed, CINAHL, PsycINFO, PubPsych, and Scopus) for peer-reviewed, English language articles, published 2010-2020, reporting prevalence data based on standardized screening instruments resulted in 335 articles; 108 were eligible for full-text analysis, of which 34 could be included in the review. Median point prevalence was 29.4% for depression, 42.4% for anxiety, 16.4% for stress, and 13.9% for disordered eating. Current suicidality was present in 7% to 8% of students. There was a high rate of psychiatric comorbidity. Despite the high prevalence of mental health problems, the willingness to seek professional help was comparatively low. Implications for mental health promotion and prevention in university settings are discussed.
Keywords: anxiety, depression, epidemiology, mental health, prevalence, Southeastern Asia, students, universities
What We Already Know
Three-fourths of all mental disorders start by the mid-20s. Yet, mental health problems in young people are often left unrecognized, with adverse consequences for their academic success, productivity, general health, and social relationships.
Globally, one-fifth of university students suffer from a mental disorder in every given year.
In Southeastern Asia, mental health problems are highly stigmatized and mental health literacy is comparatively low, even in university settings.
What This Article Adds
This article systematically presents data on the prevalence of mental health problems among university students from six selected ASEAN (Association of Southeast Asian Nations) countries.
Determinants of mental health problems within this population are explored.
Recommendations for mental health promotion in university settings are derived from the results.
Introduction
Worldwide, mental health conditions gained in importance, currently accounting for one in five years lived with disability. 1 Good mental health is increasingly recognized as a prerequisite for individual health and the sustainable development of nations and was thus included in the Sustainable Development Goals (SDGs).2,3 Notwithstanding, mental health has been a low priority in Southeastern Asia, where the awareness for mental health is low and prejudices and public stigma are widespread.4,5 The Association of Southeast Asian Nations (ASEAN) countries are home to 670 million people, about 8.6% of the world’s population. 6 The subregion is characterized by its diversity, in terms of culture, ethnicity, and income. Many ASEAN countries face significant mental health challenges, with rapid urbanization, increasing income inequality, and social and cultural change playing a key role. Mental health spending is no more than 2% of the health budget, with 80% to 90% going to mental hospitals. 7 Many ASEAN countries lack mental health legislation, effective policies, and strategic plans to address mental health needs across communities and for specific populations, particularly young people.2,4,8,9
The mental health of university students presents a major public health challenge. According to the World Health Organization (WHO) World Mental Health (WMH) Surveys, three-fourths of mental disorders have their onset before the age of 24. 10 A national mental health survey in Singapore found a median age of onset of 22 years, with the highest incidence of mental illness between the age of 18 and 24 years. 11 The transition to adulthood, stressful academic life, sometimes accompanied by part-time employment, and experience of financial burden are unique challenges for university students.12-14 Thus, compared with the general adult population, university students may experience higher levels of psychological distress. In the midst of the COVID-19 pandemic, student status was found to be a significant risk factor for developing depressive symptoms, compared with people with other occupational statuses (e.g. employment or retirement). 15
According to the WHO WMH Surveys across 21 countries, one-fifth (20.3%) of college students screened positive for a 12-month mental disorder. 16 Only 16% of these students had received any treatment during the previous 12 months. Based on the WMH International College Students Project, Mortier et al 17 estimated a prevalence of 22.3% for lifetime suicidal ideation, plans, and attempts among college students. Untreated mental illness in university students may have significant implications for academic success, productivity, substance use, and social relationships, and thus impede the human capital of any country. 12
Several studies have reviewed mental health problems among university students, mostly in high-income Western countries.18,19 Other reviews focused on a single disorder and/or on a specific student population, mostly medical students.20-24 There is, however, a paucity of research with a wider scope from ASEAN countries, where most of the member countries are low- and middle-income countries (LMICs), adversity is most prevalent, and the impact of mental health problems may be more detrimental.
The objective of this systematic review is to review the existing literature to understand the prevalence of mental health problems and the determinants of mental health among university students in selected ASEAN countries (Cambodia, Laos, Malaysia, Myanmar, Thailand, and Vietnam). The review would help to inform the planning of an international mental health promotion project for university students in the above-named ASEAN countries.
Methods
For conducting this systematic review, a review protocol was developed (see Supplemental Material). We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines 25 and the recommendations of the Joanna Briggs Institute (JBI) for systematic reviews of prevalence and incidence. 26
Inclusion and Exclusion Criteria
Inclusion criteria were defined, using the CoCoPop scheme:
Condition: Mental health problems, assessed by standardized screening instruments.
Context: Private and public universities (colleges) in six upper and lower middle-income countries of Mainland Southeast Asia: Cambodia, Laos, Malaysia, Myanmar, Thailand, and Vietnam. All countries are members of the ASEAN and are potential partners for the mental health promotion project mentioned above.
Population: University (college) students from different faculties and programs.
Only peer-reviewed articles reporting quantitative data from cross-sectional studies were included. We only included articles in the English language that were published between 2010 and present.
Exclusion criteria were as follows:
lack of validated instruments
lack of prevalence data
low representativeness of the study population (response rate <70% or sample size <250)
wrong publication type (eg, review, intervention study, qualitative study)
wrong publication date
Search Strategy
The search terms are presented as Supplemental Material, Table 1.
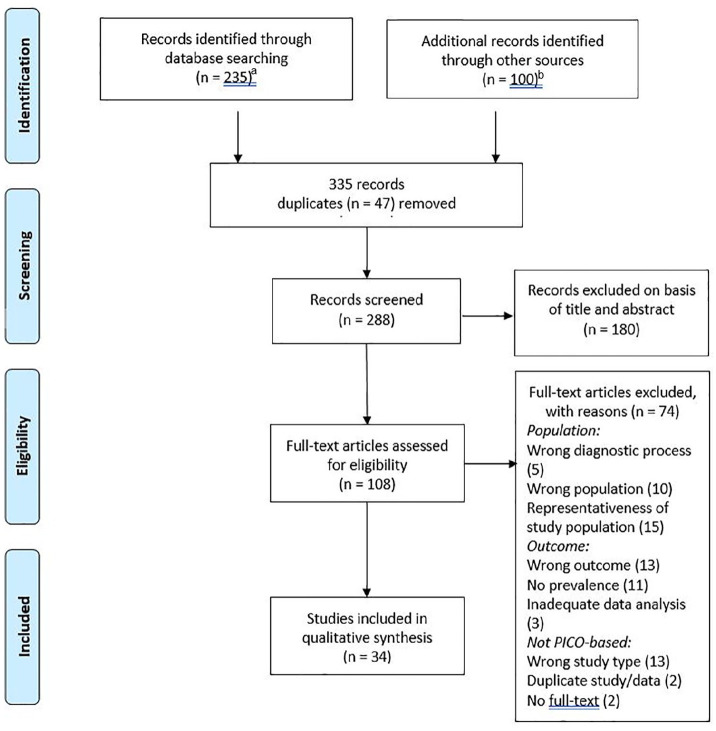
The database search was conducted between April and June 2020 in PubMed, CINAHL, PsycINFO, PubPsych, and Scopus. A PubMed alert with the above-mentioned search terms was run until August 2020. Additional articles were mainly retrieved through reference lists and citations, some through Google Scholar and conference websites (Figure 1). The database search revealed 235 articles; 100 additional articles were retrieved through other sources. After removal of duplicates, 288 articles were left for the screening of title and abstract. At this stage, articles were mainly excluded due to wrong type of population, country beyond the scope of the review, or wrong publication type or date; 108 articles were left for full-text analysis, of which 34 could be included in the review. The inclusion and exclusion of articles were done according to the PICO-based taxonomy. 27 Reasons for exclusion are given in Figure 1. A full list of the excluded articles is provided in the Supplemental Material.
Figure 1.
PRISMA flow diagram.
Abbreviation: PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PICO = Population, Intervention, Comparison, Outcome.
aPubMed (80), CINAHL (26), Scopus (34), PsycINFO (35), and PubPsych (60).
bReference lists and citations (34), Google Scholar (65), and conference websites (1).
Quality Assessment
Risk of bias was assessed using the JBI Checklist for prevalence studies. 28 Each article was critically appraised by two independent researchers from Germany and Vietnam. Discrepancies in the quality assessment were discussed until a mutual agreement was reached.
Data Extraction and Analysis
For data extraction, an extraction sheet was used, covering author, title, and year of the publication; description of study settings and participants; date of the survey; sampling method; sample size; response rate; gender and age of participants; screening instruments; prevalence of mental health variables; aims and outcomes of the study; statistical analysis; and associated variables.
Because of the heterogeneity of studies, a meta-analysis seemed not rational. Data were pooled and analyzed, using box-plots. Associated variables with a p-value <.05 were also included in the analysis. Data synthesis was done narratively.
Results
Of the 34 articles found, 27 studies were conducted in single nations, and seven were multinational studies. Most of the studies assessed depression, anxiety, and stress.
Study Setting and Study Populations
The single nation studies were conducted in Malaysia (18), Thailand (5), Vietnam (3), and Cambodia (1) (Supplemental Material, Table 2). There were no articles found from Laos and Myanmar, though data from these countries were reported within the multinational studies. Sample sizes ranged between 254 and 2970 participants. Eleven studies only focused on medical students. The mean age of participants ranged between 20.2 and 22.8 years. The majority of studies included more females than males (55%-77% females).
The sample sizes of the multinational studies ranged between 2643 and 20 222 (Supplemental Material, Table 3). The mean age of participants ranged between 20.5 and 21.3 years. Females were slightly overrepresented (54%-63%). Only subsamples from the multinational studies could be included in the review.
Psychological Distress
Common psychiatric symptoms and/or psychological distress were reported by four of the studies, encompassing 5141 students (Supplemental Material, Table 4). The prevalence ranged between 11.2% and 57%, with different cutoffs being employed.29-32
Depression, Anxiety, and Stress
Depression was assessed by 21 of the studies, encompassing data from 15 859 students (Supplemental Material, Table 4). The median point prevalence of depression was 29.4% (minimum: 0.0, maximum: 67.0, interquartile range [IQR] = 16-38.7). For severe depression, the median point prevalence was 7.6% (minimum: 0.0, maximum: 20.7, IQR: 3.2-16.8). Analysis showed that the different screening instruments led to different results, with a higher median point prevalence found by the Center for Epidemiological Studies–Depression (CES-D; 43.2%), compared with the Depression Anxiety Stress Scales–21 (DASS-21; 22.8%) and Patient Health Questionnaire–9 (PHQ-9; 25.1%) (Supplemental Material, Figures 2 and 3).
Anxiety was assessed by 10 of the studies, reporting data from 5351 students (Supplemental Material, Table 4 and Figure 4). Median point prevalence for anxiety was 42.4% (minimum: 0.6, maximum: 63.0, IQR: 21.5-55.1) and for severe anxiety 18.9% (minimum: 0.3, maximum: 29.9, IQR: 4-28). Eight studies assessed stress among university students, including data of 3898 students (Supplemental Material, Table 4 and Figure 4). Half of them were performed among medical students.33-36 Median point prevalence was 16.4% (minimum: 0.0, maximum: 23.7, IQR: 12.9-23.2) and for severe stress 5.1% (minimum: 0.0, maximum: 6.9, IQR: 3.2-6.1).
Suicidality
Suicidality was assessed by 6 studies (Supplemental Material, Table 4). Two multinational studies37,38 reported a lifetime prevalence between 0.9% and 16.3% for suicidal ideation and between 0.9% and 5.3% for suicidal attempts. For their whole sample (n = 4675), Peltzer et al 37 reported a prevalence of 11.7%/2.4% for suicidal ideation/behavior. The four single nation studies reported a 12-month prevalence of 3.9%/0.9% and 8.7%/1.3% for suicidal ideation/behavior39,40 and a point prevalence of 7% and 7.7%.41,42
Eating Disorder
Eating disorder was assessed by five different studies (Supplemental Material, Table 4 and Figure 5). Data from 5497 students could be included in the analysis. Median point prevalence for all students was 13.9% (minimum: 6.8, maximum: 20.6, IQR: 9.6-19.8), 13.4% in males and 13.9% in females The mean prevalence among females was higher (15.1% vs 12.3%).
Posttraumatic Stress Disorder (PTSD)
Posttraumatic stress disorder was only assessed as a predictor variable, but not as a primary outcome. Chan et al. 43 found a PTSD prevalence of 19.8% among all the students, with a higher prevalence (30.5%) among the students at risk for eating disorders. Two of the multinational studies37,44 reported a PTSD prevalence of 24.2% and 23.9% among students from different ASEAN countries.
Health Risk Behavior
Three studies assessed problematic Internet use or Internet addiction (Supplemental Material, Table 4). Balhara et al 45 reported a prevalence of 11.7% for problematic Internet use. Boonvisudhi and Kuladee 46 assessed possible Internet addiction (24.4%) and found a higher prevalence among females (27.8% vs 20.4%). Manaf et al 47 identified 56.5% of students as problematic users and 7.8% as addictive users. Males represented only 38.5% of the problematic users, but 64% of the addictive users. In summary, males were 2.43 times more likely to be problematic or addictive users, compared with females (Supplemental Material, Table 5).
Alcohol use was assessed by two multinational studies (Supplemental Material, Table 4). Peltzer and Pengpid 48 explored heavy drinking among university students (n = 17 590) from 24 countries across Asia, Africa, and the Americas. Only data for Laos could be included, where 46.5% of male students and 26.3% of female students were screened as heavy drinkers. Yi et al 49 assessed binge drinking among students (n = 8809) from 9 ASEAN countries and reported a pooled prevalence of 12.8%/6.4% for infrequent/frequent binge drinking for their whole sample. Frequent binge drinking was significantly more prevalent among males, compared with females in all countries except Malaysia (Supplemental Material, Table 5).
Determinants of Mental Health and Psychiatric Comorbidities
Determinants of mental health were assessed by all of the included studies. As the multinational studies all referred to their whole sample, only findings from the multinational ASEAN studies37,44,49 were included in the data analysis. Most of the studies tested associations between mental health variables and sociodemographic and study-related variables (age, gender, ethnicity, religion, year of study, academic success, economic background, residence or living arrangement), some included health status and health behavior (smoking, drinking, drug use, overweight, physical inactivity). Fewer studies included psychiatric comorbidities, psychological variables (self-perception, self-esteem, motivation, coping strategies), personal problems, stressful life events, or adverse childhood experiences in their analysis.
For most of the sociodemographic variables, findings were non-significant or contradictory between the studies. Exceptions were lower economic status/perceived financial struggle and poor academic performance which were positively correlated with mental health problems in nearly all the studies. Gender differences were found for anxiety, stress, and disordered eating which were more prevalent in females (Supplemental Material, Table 5). Heavy drinking and binge drinking was more prevalent in males, while findings for depression, suicidality, and Internet addiction were contradictory.
Internalizing problems were correlated with health status40,46,50 and health risk behavior.30,41,50,51 Positive correlations were also found for personal problems with peers, family, or partner30,40,42,46,52 and inadequate social support, while connectedness was negatively correlated with internalizing problems. 39 Among the psychological variables, negative self-perception played a role in depression 50 and disordered eating.43,44,53 Self-esteem was negatively correlated with anxiety and depression. 39 Having a history of mental health problems was associated with suicidality 42 and depression and anxiety. 39
There was high comorbidity between depression, anxiety, and stress54-56 and also between depression and suicidality.37,39,42 Disordered eating was correlated with PTSD in one study, 43 and with depression in other studies.44,53,55 Internet addiction/pathological use was identified as a predictor for depression 46 and eating disorder. 44 On the contrary, high scores of anxiety and depression predicted problematic Internet use. 45
Help-Seeking and Treatment Use
Only two of the included studies evaluated help-seeking. According to Aida et al., 33 most of the students preferred help-seeking from informal sources like family or friends. Help-seeking from formal sources was significantly associated with anxiety in this study. Musumari et al. 39 evaluated mental health service use among university students in Thailand. Around 6% of students had a history of mental health service use.
Discussion
Mental health in university students presents a major public health challenge. This review describes the prevalence of common mental health problems among students in six ASEAN countries and explores the determinants of mental health among this population. While student mental health is a priority in university settings of high-income countries (HIC), with counseling services regularly available at campuses, this is not the case in the low- and middle-income countries (LMICs) of Southeastern Asia. Non-availability of student-friendly mental health services, poor mental health literacy, and stigma may prevent students from help-seeking, even if they require support. The prevalence of mental health problems among university students in ASEAN countries was high, with depression and anxiety being the most prominent problems.
The depression prevalence found in this review was 29.4% and 7.6% for severe depression, which is in the same range as was reported by other reviews and meta-analyses on student mental health. Ibrahim et al. 18 reported a prevalence of 30.6% from 24 studies that were mostly conducted in Western countries. A recent meta-analysis 57 that focused on LMIC reported an overall prevalence of 24.4%. Two reviews20,22 that focused on medical students reported a depression prevalence of 28% and 27.2%. Peltzer and Pengpid 58 reported an overall depression prevalence of 36.8% (24% for moderate and 12.8% for severe depression) from studies in 26 high-, middle-, and low-income countries, with students from low-income countries reporting a higher prevalence (14.5%), compared with students from lower middle-income (12.9%) or upper middle-income and high-income countries (12%).
For anxiety, the median point prevalence was 42.4%, for severe anxiety, the median point prevalence was 18.9%. A global meta-analysis 21 of studies among medical students reported a pooled anxiety prevalence of 33.8%, with studies from Asia and Middle East reporting a higher prevalence (35.2% and 42.4%).
Suicidality prevalence ranged between 0.9% to 16.3% (lifetime prevalence) and 3.9% to 8.7% (current to 12-month prevalence). Rotenstein et al. 22 reported a pooled prevalence of 11% for suicidal ideation (past 2 weeks to past 12 months) among medical students worldwide. Mortier et al. 17 reported an estimated lifetime prevalence of suicidal ideation, plans, and attempts of 22.3% and a 12-month prevalence of 10.6% from a meta-analysis of 36 college student samples all over the world. Globally, suicidality is a concern among young people, and suicide is one of the three major causes of death among youth aged 15 to 29 worldwide. 59
Disordered eating was present in 13.9% of students. A systematic review and meta-analysis 23 reported a pooled prevalence of 10.4% among university students from nine countries, with a higher prevalence (13.7%) reported by the studies with female samples (n = 7).
The prevalence of possible Internet addiction/problematic use varied between 11.7% and 56.5%, and 7.8% of students were considered addicted. A meta-analysis among medical students 60 found a much higher prevalence of Internet addiction (30.6%). On the contrary, Balhara et al 45 reported a prevalence of only 8.4% for problematic Internet use among students from Asia and Europe, with a significantly higher prevalence (10.8%-12.6%) reported from the Asian students.
For alcohol abuse, the prevalence substantially varied between countries, with high rates reported from Laos and Thailand and lower rates reported from the other ASEAN countries. 49 In their multinational survey among students from 24 countries, Peltzer and Pengpid 48 found large between-country differences and an association with country per capita alcohol consumption, which is considerably lower in Muslim-majority countries.
Determinants of Mental Health
Many sociodemographic variables did not show consistent associations with mental health. Exceptions were poor economic background or perceived financial struggle and poor academic performance which were associated with mental health problems in most of the studies. Female gender was associated with disordered eating, anxiety, and stress. Associations were also found with psychological variables, relationships with parents and peers, social support, health status, and health risk behavior. The importance of connectedness and healthy relationships for student mental health has been highlighted by other large surveys, for example, the multinational study by Peltzer and Pengpid. 58 A recent study among first-year students from universities in Europe, Asia, Western Pacific, and the Americas found significant associations between depression and social capital. 61 Students with lower social capital on the individual level (trust in other people, having close friends, engaging in community activities) or on the macro level (country income level) had higher odds of depressive symptoms.
Another finding was the high rate of comorbidity between mental health problems, for example, between depression, anxiety, and stress, and also between depression and suicidality. High rates of psychiatric comorbidity are known from previous research. Data from the WMH International College Students Project showed that out of the 31.4% of students who screened positive for any mental disorder, roughly half of them screened positive for more than one disorder. Alonso, Mortier and Auerbach, 2018. 63
Heterogeneity Between the Studies
All of the included studies used validated screening instruments, which was an inclusion criterion. Although most of the instruments had been previously employed in Southeast Asia, not every instrument was validated in the specific context where it was used. While validation studies had been conducted in Vietnam,64,65 Malaysia,66,67 or Thailand, 68 similar studies from Laos or Cambodia are absent.69,70 Altogether, there were 17 different screening instruments employed (Supplemental Material, Table 4), most often the CES-D (8 studies), DASS-21 (8 studies), PHQ-9 (4 studies), GHQ-12 (12-item General Health Questionnaire; 4 studies), and EAT-26 (26-item Eating Attitudes Test; 5 studies). The use of different screening instruments and different cut-offs is a cause of heterogeneity. Our data showed that for depression, the mean point prevalence varied, according to the instrument that was used. Previous reviews also revealed differences in prevalence for the same mental health variable, depending on the employed instrument.22,23
Another issue is the cultural adaptation or non-adaptation of instruments. Only three out of 34 studies used culturally adapted instruments, with further two using a mix of adapted and non-adapted instruments (Supplemental Material, Table 4). Using instruments in a different cultural context has limitations. For instance, how mental health symptoms are experienced, interpreted, and communicated may vary widely between cultures. This may introduce a bias and limit the validity of the instrument across different cultural settings.71,72 Other problems often associated with the use of Western instruments in LMIC, like low levels of literacy or linguistic diversity, 73 have minor importance in university settings.
Treatment Use and Help-Seeking for Mental Health
Our data showed that treatment rates were low and students preferred informal help-seeking to help-seeking from counselors, psychologists, or psychiatrists. A low likelihood of formal help-seeking was also found by Kamimura et al 62 who compared perceptions of mental health between Vietnamese and US students. Stigma, perceived need, social context, and cultural competence of the service provider were identified as important determinants of help-seeking by prior research.74,75 While recent data from the United States 76 showed increasing rates of service use among students, data from other parts of the world show a different picture: The WHO WMH Surveys reported that only 16% of students suffering from a 12-month mental disorder received minimal treatment, 16 with substantially higher treatment rates in high-income countries (23.1%), compared with upper middle-income (11.4%) and lower middle-income and low-income countries (6.7%). Rotenstein et al 22 found that only 16% of medical students with a positive depression screening sought treatment. Low treatment rates in LMICs are not only due to low rates of help-seeking, but they also reflect the non-availability of easily accessible student-friendly services.
Limitations
There are several limitations to consider. First, this review identified studies from only four out of six focus countries, with an overrepresentation of studies from Malaysia. Therefore, mental health strategies developed from this review could not be overgeneralized to other ASEAN countries and settings. Second, there were methodological differences regarding sample size, screening instruments, associated factors/variables, and statistic analysis, which explained why a meta-analysis was not feasible. Third, the use of self-report measures goes along with a risk of underreporting due to internal stigma and social desirability. Fourth, this review was carried out during the COVID-19 pandemic, with its impacts on students’ mental health. Because the database search was finalized in June 2020, studies regarding the psychological impacts of the pandemic could not be included. Fifth, the review focused on English language journals which may limit findings from other language journals (e.g. in Vietnamese, Thai, Malay). Finally, there is a possible bias as five databases (PubMed, CINAHL, PsycINFO, PubPsych and Scopus) were selected for this review.
Recommendations
The findings of this review have important implications for mental health policy-making and practice in this subregion. The prevalence of internalizing problems and addiction among university students in ASEAN countries is high, suggesting the urgent need for comprehensive and systematic development and implementation of mental health services for students. At the level of institutional governance and policy-making, mental health services and counseling should be considered a priority and a compulsory component of the university infrastructure. This is in line with the concept of “Healthy Universities,” in which the health and well-being of students and staff are part of the universities core business.77-79 Regarding service implementation, a multitier approach to mental health promotion, prevention, early identification, and support should be developed in university settings. Finally, universities should offer opportunities and structured support for students to ensure that they are connected to peers, feel supported by staff, and settle into their new environment. 80
The impact of the COVID-19 pandemic on student mental health and possible mental health support during lockdown situations could be topics for future research. Recent literature indicates negative influences on the mental health of students, particularly on anxiety and stress,81-84 with financial constraints, uncertainties regarding academic performance and career perspectives, effects on daily life, and isolation being key issues.
Conclusion
The review shows the high burden of mental health problems among university students of six ASEAN countries, with depression, anxiety, and addictive behaviors being the most prominent problems. Although mental health problems are common among young people, the willingness to seek help from professionals is low and many settings lack counseling facilities or student-friendly mental health care. Apart from scaling up counseling facilities, mental health stigma needs to be addressed to encourage help-seeking for mental health problems. Re-orientating universities toward an enabling and supportive environment for students and staff could be preventive.
Supplemental Material
Supplemental material, sj-docx-1-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-10-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-11-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-2-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-3-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-4-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-5-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-6-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-7-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-8-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-9-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Gunter Groen  https://orcid.org/0000-0001-9947-8722
https://orcid.org/0000-0001-9947-8722
Supplemental Material: Supplemental material for this article is available online.
References
- 1. World Health Organization. Health Topics: Mental Health. Accessed December 16, 2020. https://www.who.int/health-topics/mental-health#tab=tab_2.
- 2. World Health Organization. Special Initiative for Mental Health (2019-2023). World Health Organization; 2019. Accessed September 21, 2020. https://eupha.org/repository/EUPHW/Resources/The_WHO_Special_Initiative_for_Mental_Health_2019-2023.pdf. [Google Scholar]
- 3. UN Department of Economic and Social Affairs. Sustainable Development. The 17 Goals. Accessed December 16, 2020. https://sdgs.un.org/goals.
- 4. Anwar N, Thamarangsi T. Care for mental disorders and promotion of mental well-being in South-East Asia. WHO South East Asia J Public Health. 2017;6(1):1-4. doi: 10.4103/2224-3151.206157. [DOI] [PubMed] [Google Scholar]
- 5. Chong SA, Abdin E, Picco L, et al. Recognition of mental disorders among a multiracial population in Southeast Asia. BMC Psychiatry. 2016;16:121. doi: 10.1186/s12888-016-0837-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Worldometer. Population of South-Eastern Asia. Published 2020. Accessed December 16, 2020. https://www.worldometers.info/world-population/south-eastern-asia-population/.
- 7. Maramis A, Van Tuan N, Minas H. Mental health in southeast Asia. Lancet. 2011;377(9767):700-702. doi: 10.1016/S0140-6736(10)62181-2. [DOI] [PubMed] [Google Scholar]
- 8. World Health Organization. Mental Health Action Plan 2013-2020. Geneva: World Health Organization; 2013. [Google Scholar]
- 9. World Health Organization. Mental Health Atlas 2017. Geneva: World Health Organization; 2018. [Google Scholar]
- 10. Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustün TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 2007;20(4):359-364. doi: 10.1016/S0140-6736(10)62181-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vaingankar JA, Rekhi G, Subramaniam M, Abdin E, Chong SA. Age of onset of life-time mental disorders and treatment contact. Soc Psychiatry Psychiatr Epidemiol. 2013;48(5):835-843. doi: 10.1007/s00127-012-0601-y. [DOI] [PubMed] [Google Scholar]
- 12. Hunt J, Eisenbeg D. Mental health problems and help-seeking behavior among colleges. J Adolesc Health. 2010;46(1):3-10. doi: 10.1016/j.jadohealth.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 13. Rückert H-W. Students′ mental health and psychological counselling in Europe. Ment Health Prev. 2015;3:34-40. doi: 10.1016/j.mhp.2015.04.006. [DOI] [Google Scholar]
- 14. Stallman HM. Psychological distress in university students: a comparison with general population data. Aust Psychol. 2010;45(4):249-257. doi: 10.1080/00050067.2010.482109. [DOI] [Google Scholar]
- 15. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55-64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Auerbach RP, Alonso J, Axinn WG, et al. Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychol Med. 2016;46(14):2955-2970. doi: 10.1017/S0033291716001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mortier P, Cuijpers P, Kiekens G, et al. The prevalence of suicidal thoughts and behaviours among college students: a meta-analysis. Psychol Med. 2018;48(4):554-565. doi: 10.1017/S0033291717002215. [DOI] [PubMed] [Google Scholar]
- 18. Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. 2013;47(3):391-400. doi: 10.1016/j.jpsychires.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 19. Pedrelli P, Nyer M, Yeung A, Zulauf C, Wilens T. College students: mental health problems and treatment considerations. Acad Psychiatry. 2015;39(5):503-511. doi: 10.1007/s40596-014-0205-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Puthran R, Zhang MWB, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50(4):456-468. doi: 10.1111/medu.12962. [DOI] [PubMed] [Google Scholar]
- 21. Quek TT-C, Tam WW-S, Tran BX, et al. The global prevalence of anxiety among medical students: a meta-analysis. Int J Environ Res Public Health. 2019;16:2735. doi: 10.3390/ijerph16152735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rotenstein LS, Ramos MA, Torre M, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316(21):2214-2236. doi: 10.1001/jama.2016.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jahrami H, Sater M, Abdulla A, Faris M, AlAnsari A. Eating disorders risk among medical students: a global systematic review and meta-analysis. Eat Weight Disord. 2019;24(3):397-410. doi: 10.1007/s40519-018-0516-z. [DOI] [PubMed] [Google Scholar]
- 24. Cuttilan AN, Sayampanathan AA, Ho RC-M. Mental health issues amongst medical students in Asia: a systematic review [2000-2015]. Ann Transl Med. 2016;4(4):72. doi: 10.3978/j.issn.2305-5839.2016.02.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Int J Surg. 2010;8(5):336-341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 26. Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Chapter 5: systematic reviews of prevalence and incidence. In: Joanna Briggs Institute Reviewer’s Manual., 2017. The Joanna Briggs Institute; 2017. Accessed December 10, 2018. https://reviewersmanual.joannabriggs.org/. [Google Scholar]
- 27. Edinger T, Cohen AM. A large-scale analysis of the reasons given for excluding articles that are retrieved by literature search during systematic review. AMIA Annu Symp Proc. 2013;2013:379-387. [PMC free article] [PubMed] [Google Scholar]
- 28. Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and incidence data. Int J Evid Based Healthc. 2015;13(3):147-153. [DOI] [PubMed] [Google Scholar]
- 29. Pensuksan WC, Lertmaharit S, Lohsoonthorn V, et al. Relationship between poor sleep quality and psychological problems among undergraduate students in the Southern Thailand. Walailak J Sci Technol. 2016;13(4):235-242. [PMC free article] [PubMed] [Google Scholar]
- 30. Talwar P, Rahman MFbA. Factor structure of General Health Questionnaire and assessment: a cross-sectional study among university students in Malaysia. J Psychiatry. 2015;16(2):232-240. [Google Scholar]
- 31. Haregu A, Gelaye B, Pensuksan WC, et al. Circadian rhythm characteristics, poor sleep quality, daytime sleepiness and common psychiatric disorders among Thai college students. Asia Pac Psychiatry. 2015;7(2):182-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yusoff MSB, Abdul Rahim AF, Yaacob MJ. Prevalence and sources of stress among Universiti Sains Malaysia medical students. Malays J Med Sci. 2010;17(1):30-37. [PMC free article] [PubMed] [Google Scholar]
- 33. Aida J, Hizlinda T, Siti Fatima S, et al. Psychological disorders and help seeking behaviour among Malaysian medical students in their clinical years. Med Health (Universiti Kebangsaan Malaysia). 2014;9(2):114-123. [Google Scholar]
- 34. Masiran R, Ismail SIF, Ibrahim N, et al. Associations between coping styles and psychological stress among medical students at Universiti Putra Malaysia. Curr Psychol. 2018:1-5. doi: 10.1007/s12144-018-0049-7. [DOI] [Google Scholar]
- 35. Ngan SW, Chern BCK, Rajarathnam DD, Balan J, Hong TS, Tiang K-P. The relationship between eating disorders and stress among medical undergraduate: a cross-sectional study. Open J Epidemiol. 2017;07(02):85-95. doi: 10.4236/ojepi.2017.72008. [DOI] [Google Scholar]
- 36. Teh CK, Ngo CW, Zulkifli RA, binti Vellasamy R, Suresh K. Depression, anxiety and stress among undergraduate students: a cross-sectional study. Open J Epidemiol. 2015;05(04):260-268. doi: 10.4236/ojepi.2015.54030. [DOI] [Google Scholar]
- 37. Peltzer K, Yi S, Pengpid S. Suicidal behaviors and associated factors among university students in six countries in the Association of Southeast Asian Nations (ASEAN). Asian J Psychiatr. 2017;26:32-38. doi: 10.1016/j.ajp.2017.01.019. [DOI] [PubMed] [Google Scholar]
- 38. Eskin M, AlBuhairan F, Rezaeian M, et al. Suicidal thoughts, attempts and motives among university students in 12 Muslim-majority countries. Psychiatr Q. 2019;90(1):229-248. doi: 10.1007/s11126-018-9613-4. [DOI] [PubMed] [Google Scholar]
- 39. Musumari PM, Tangmunkongvorakul A, Srithanaviboonchai K, et al. Grit is associated with lower level of depression and anxiety among university students in Chiang Mai, Thailand: a cross-sectional study. PLoS One. 2018;13(12):e0209121. doi: 10.1371/journal.pone.0209121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Quynh AT, Dunne MP, Ngoc HL. Well-being, depression and suicidal ideation among medical students throughout Vietnam. Vietnam J Med & Pharm. 2014;6(3):23-30. [Google Scholar]
- 41. Pham T, Bui L, Nguyen A, et al. The prevalence of depression and associated risk factors among medical students: an untold story in Vietnam. PLoS One. 2019;14(8):e0221432. doi: 10.1371/journal.pone.0221432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tan ST, Sherina MS, Rampal L, Normala I. Prevalence and predictors of suicidality among medical students in a public university. Med J Malaysia. 2015;70(1):1-5. [PubMed] [Google Scholar]
- 43. Chan YL, Samy AL, Tong WT, Islam MA, Low WY. Eating disorder among Malaysian university students and its associated factors. Asia Pac J Public Health. 2020;32:334-339. doi: 10.1177/1010539520947879. [DOI] [PubMed] [Google Scholar]
- 44. Pengpid S, Peltzer K. Risk of disordered eating attitudes and its relation to mental health among university students in ASEAN. Eat Weight Disord. 2018;23(3):349-355. doi: 10.1007/s40519-018-0507-0. [DOI] [PubMed] [Google Scholar]
- 45. Balhara YPS, Doric A, Stevanovic D, et al. Correlates of problematic internet use among college and university students in eight countries: an international cross-sectional study. Asian J Psychiatr. 2019;45:113-120. doi: 10.1016/j.ajp.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 46. Boonvisudhi T, Kuladee S. Association between Internet addiction and depression in Thai medical students at Faculty of Medicine, Ramathibodi Hospital. PLoS One. 2017;12(3):e0174209. doi: 10.1371/journal.pone.0174209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Manaf RA, Sham SM, Azri MK, Ragubathi MN. Internet addiction among undergraduate students: evidence from a Malaysian public university. Int Med J Malaysia. 2018;17(2):41-48. [Google Scholar]
- 48. Peltzer K, Pengpid S. Heavy drinking and social and health factors in university students from 24 low, middle income and emerging economy countries. Community Ment Health J. 2016;52(2):239-244. [DOI] [PubMed] [Google Scholar]
- 49. Yi S, Ngin C, Peltzer K, Pengpid S. Health and behavioral factors associated with binge drinking among university students in nine ASEAN countries. Subst Abuse Treat Prev Policy. 2017;12:1-10. doi: 10.1186/s13011-017-0117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ngin C, Pal K, Tuot S, Chhoun P, Yi R, Yi S. Social and behavioural factors associated with depressive symptoms among university students in Cambodia: a cross-sectional study. BMJ Open. 2018;8(9)e:019918. doi: 10.1136/bmjopen-2017-019918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Tuyen NTH, Dat TQ, Nhung HTH. Prevalence of depressive symptoms and its related factors among students at Tra Vinh University, Vietnam in 2018. AIMS Public Health. 2019;6(3):307-319. doi: 10.3934/publichealth.2019.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Talwar P, Othman MK, Othman AEA, Mustaffa MS, Mughal YH. Socio-demographic determinants and prevalence of depression, anxiety, and stress among Malaysian university students. J Indian Acad Appl Psychol. 2017;43(2):296-304. [Google Scholar]
- 53. Chin YS, Appukutty M, Kagawa M, et al. Comparison of factors associated with disordered eating between male and female Malaysian university students. Nutrients. 2020;12(2):318. doi: 10.3390/nu12020318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Francis B, Gill JS, Yit Han N, et al. Religious coping, religiosity, depression and anxiety among medical students in a multi-religious setting. Int J Environ Res Public Health. 2019;16(2):259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Gan WY, Mohd Nasir MT, Zalilah MS, Hazizi AS. Disordered eating behaviors, depression, anxiety and stress among Malaysian university students. College Student J. 2011;45(2):296. [Google Scholar]
- 56. Saravanan C, Wilks R. Medical students’ experience of and reaction to stress: the role of depression and anxiety. Sci World J. 2014;2014:737382. doi: 10.1155/2014/737382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Akhtar P, Ma L, Waqas A, et al. Prevalence of depression among university students in low and middle income countries (LMICs): a systematic review and meta-analysis. J Affect Disord. 2020;274:911-919. doi: 10.1016/j.jad.2020.03.183. [DOI] [PubMed] [Google Scholar]
- 58. Peltzer K, Pengpid S. Depressive symptoms and social demographic, stress and health risk behaviour among university students in 26 low-, middle- and high-income countries. Int J Psychiatry Clin Pract. 2015;19(4):259-265. doi: 10.3109/13651501.2015.1082598. [DOI] [PubMed] [Google Scholar]
- 59. World Health Organization. Suicide in the world. Global health estimates. Geneva, Switzerland: World Health Organization; 2019. [Google Scholar]
- 60. Zhang MWB, Lim RBC, Lee C, Ho RCM. Prevalence of internet addiction in medical students: a meta-analysis. Acad Psychiatry. 2018;42(1):88-93. doi: 10.1007/s40596-017-0794-1. [DOI] [PubMed] [Google Scholar]
- 61. Backhaus I, Varela AR, Khoo S, et al. Associations between social capital and depressive symptoms among college students in 12 countries: results of a cross-national study. Front Psychol. 2020;11:644. doi:10.3389/fpsyg.2020.00644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kamimura A, Trinh HN, Johansen M, et al. Perceptions of mental health and mental health services among college students in Vietnam and the United States. Asian J Psychiatr. 2018;37:15-19. doi: 10.1016/j.ajp.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 63. Alonso J, Mortier P, Auerbach RP, et al. Severe role impairment associated with mental disorders: results of the WHO World Mental Health Surveys International College Student Project. Depress Anxiety. 2018;35(9):802-814. doi: 10.1002/da.22778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Tran TD, Tran T, Fisher J. Validation of the Depression Anxiety Stress Scales (DASS) 21 as a screening instrument for depression and anxiety in a rural community-based cohort of northern Vietnamese women. BMC Psychiatry. 2013;13(1):24. doi: 10.1186/1471-244X-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Tran TD, Tran T, Fisher J. Validation of three psychometric instruments for screening for perinatal common mental disorders in men in the north of Vietnam. J Affect Disord. 2012;136(1-2):104-109. doi: 10.1016/j.jad.2011.08.012. [DOI] [PubMed] [Google Scholar]
- 66. Sherina MS, Arroll B, Goodyear-Smith F. Criterion validity of the PHQ-9 (Malay version) in a primary care clinic in Malaysia. Med J Malaysia. 2012;67(3):309-315. [PubMed] [Google Scholar]
- 67. Musa R, Fadzil MA, Zain Z. Translation, validation and psychometric properties of Bahasa Malaysia version of the Depression Anxiety and Stress Scales (DASS). ASEAN J Psychiatry. 2007;8:82-89. [Google Scholar]
- 68. Lotrakul M, Sumrithe S, Saipanish R. Reliability and validity of the Thai version of the PHQ-9. BMC Psychiatry. 2008;8:46. doi: 10.1186/1471-244X-8-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Mughal AY, Devadas J, Ardman E, Levis B, Go VF, Gaynes BN. A systematic review of validated screening tools for anxiety disorders and PTSD in low to middle-income countries. BMC Psychiatry. 2020;20:338. doi: 10.1186/s12888-020-02753-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ali G-C, Ryan G, De Silva MJ. Validated screening tools for common mental disorders in low- and middle-income countries: a systematic review. PLoS One. 2016;11(6):e0156939. doi: 10.1371/journal.pone.0156939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Sharan P, Sagar R, Kumar S. Mental health policies in South-East Asia and the public health role of screening instruments for depression. WHO South East Asia J Public Health. 2017;6(1):5-11. doi: 10.4103/2224-3151.206165. [DOI] [PubMed] [Google Scholar]
- 72. Oei TPS, Sawang S, Goh YW, Mukhtar F. Using the Depression Anxiety Stress Scale 21 (DASS-21) across cultures. Int J Psychol. 2013;48(6):1018-1029. doi: 10.1080/00207594.2012.755535. [DOI] [PubMed] [Google Scholar]
- 73. Kagee A, Tsai AC, Lund C, Tomlinson M. Screening for common mental disorders in low resource settings: reasons for caution and a way forward. Int Health. 2013;5(1):11-14. doi: 10.1093/inthealth/ihs004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Eisenberg D, Hunt J, Speer N. Help seeking for mental health on college campuses: review of evidence and next steps for research and practice. Harv Rev Psychiatry. 2012;20(4):222-232. doi: 10.3109/10673229.2012.712839. [DOI] [PubMed] [Google Scholar]
- 75. Eisenberg D, Speer N, Hunt JB. Attitudes and beliefs about treatment among college students with untreated mental health problems. Psychiatr Serv. 2012;63(7):711-713. doi: 10.1176/appi.ps.201100250. [DOI] [PubMed] [Google Scholar]
- 76. Eisenberg D, Lipson SK. The Healthy Minds Study. 2018-1019 Date Report. Accessed October 18, 2021. https://healthymindsnetwork.org/wp-content/uploads/2019/09/HMS_national-2018-19.pdf.
- 77. AUN Health Promotion Network. AUN Healthy University Framework. Mahidol: Mahidol University; 2017. [Google Scholar]
- 78. Cawood J, Dooris M, Powell S. Healthy universities: shaping the future. Perspect Public Health. 2010;130(6):259-260. doi: 10.1177/1757913910384055. [DOI] [PubMed] [Google Scholar]
- 79. Holt M, Powell S. Healthy Universities: a guiding framework for universities to examine the distinctive health needs of its own student population. Perspect Public Health. 2017;137(1):53-58. doi: 10.1177/1757913916659095. [DOI] [PubMed] [Google Scholar]
- 80. Macaskill A. The mental health of university students in the United Kingdom. Brit J Guid Couns. 2013;41(4):426-441. doi: 10.1080/03069885.2012.743110. [DOI] [Google Scholar]
- 81. Cao W, Fang Z, Hou G, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Du C, Zan MCH, Cho MJ, et al. Increased resilience weakens the relationship between perceived stress and anxiety on sleep quality: a moderated mediation analysis of higher education students from 7 countries. Clocks Sleep. 2020;2(3):334-353. doi: 10.3390/clockssleep2030025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Kamaludin K, Chinna K, Sundarasen S, et al. Coping with COVID-19 and movement control order (MCO): experiences of university students in Malaysia. Heliyon. 2020;6(11):e05339. doi: 10.1016/j.heliyon.2020.e05339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Sundarasen S, Chinna K, Kamaludin K, et al. Psychological impact of COVID-19 and lockdown among university students in Malaysia: implications and policy recommendations. Int J Environ Res Public Health. 2020;17(17). doi: 10.3390/ijerph17176206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-10-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-11-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-2-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-3-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-4-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-5-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-6-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-7-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-8-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health
Supplemental material, sj-docx-9-aph-10.1177_10105395211055545 for Mental Health of University Students in Southeastern Asia: A Systematic Review by Anja Susanne Dessauvagie, Hoang-Minh Dang, Thi Anh Thu Nguyen and Gunter Groen in Asia Pacific Journal of Public Health