Abstract
Many studies have investigated the impact of the COVID-19 pandemic on mental health. Throughout the pandemic, time spent at home increased to a great extent due to restrictive measures. Here we set out to investigate the relationship between housing conditions and the mental health of populations across European countries. We analyzed survey data collected during spring 2020 from 69,136 individuals from four cohorts from Denmark, France, and the UK. The investigated housing conditions included household density, composition, and crowding, access to outdoor facilities, dwelling type, and urbanicity. The outcomes were loneliness, anxiety, and life satisfaction. Logistic regression models were used, and results were pooled using random-effects meta-analysis. In the meta-analysis, living alone was associated with higher levels of loneliness (OR = 3.08, 95% CI 1.87–5.07), and lower life satisfaction (OR = 1.27, 95% CI 1.05–0.55), compared to living with others. Not having access to an outdoor space and household crowding were suggestively associated with worse outcomes. Living in crowded households, living alone, or lacking access to outdoor facilities may be particularly important in contributing to poor mental health during a lockdown. Addressing the observed fundamental issues related to housing conditions within society will likely have positive effects in reducing social inequalities, as well as improving preparedness for future pandemics.
Subject terms: Risk factors, Disease prevention, Epidemiology, Quality of life, Public health
Introduction
The COVID-19 pandemic transformed the everyday lives of millions of people worldwide. Public health measures such as stay-at-home recommendations, curfews, lockdown of educational activities, and remote working were implemented in most European countries during spring 2020; however, the severity of the pandemic and the stringency of public health recommendations and societal lockdowns varied throughout the pandemic.
A rapidly growing literature has investigated the effects of the COVID-19 pandemic and its associated societal lockdowns on populations’ mental health. Most of the findings from these studies indicated that the pandemic and associated societal lockdowns and periods of social isolation contributed to increased levels of loneliness, depression, and anxiety1–8, while a few studies examining changes in mental health indicated that some mental health outcomes improved, stayed the same, or worsened only slightly, compared to pre-pandemic years9–11. Considering that a national lockdown is one of the most effective non-pharmaceutical interventions to reduce the spread of COVID-19 and related deaths12, it is of utmost importance to understand which factors during a lockdown may lead to adverse psychological effects. Before the COVID-19 pandemic, European citizens already spent most of their time indoors13, but the time spent at home increased to a great extent due to the lockdowns. Individuals’ residences became the place for most of their private, work-related, and leisure activities. Robust evidence exists on housing as a determinant of health14,15. Thus, it is of interest to explore and quantify the relationship between the housing environment during COVID-19 related lockdowns and mental health indicators across Europe.
A few studies have assessed whether living conditions during the COVID-19 lockdowns influenced people’s mental health. For example, access to outdoor facilities has been found to be associated with lower levels of depression, stress16, anxiety17, and improved wellbeing18 in different studies. Increased house surface area was positively associated with wellbeing in a French study18 and a high prevalence of moderate-to-severe depressive symptoms was observed amongst Italian students living in dwellings < 60 m219. Furthermore, living alone was reported to be associated with greater loneliness20,21. To our knowledge, no previous studies have assessed the role of housing conditions during lockdowns on multiple mental health indicators in a multi-cohort study across Europe. Using data from four European cohorts, we examined and compared whether, and to what extent, housing conditions influenced the mental health of individuals during the first COVID-19 lockdown in spring 2020.
Methods
Study design
A two-stage meta-analysis22–25 was undertaken using individual participant data from four European cohorts. This study followed the reporting principles of the Strengthening the reporting of observational studies in epidemiology (STROBE) statement26.
Participating cohorts
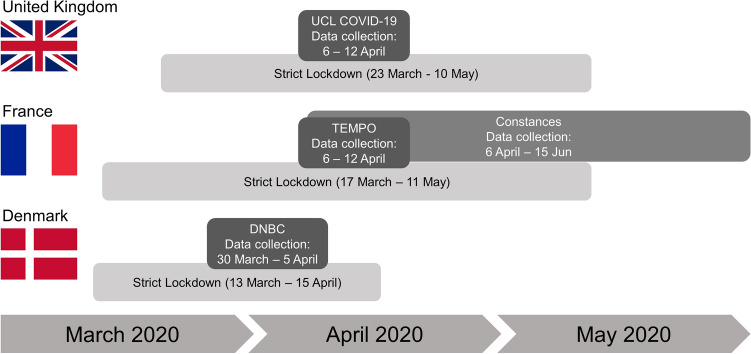
Four cohorts were included in this study: The Danish National Birth Cohort (DNBC, Denmark; n = 21,889)27, Constances (France, n = 28,171)28, TEMPO (France, n = 424)29 and the University College London COVID-19 Social Study (UCL COVID-19, United Kingdom [UK]; n = 18,652)20. The participating cohorts have collected data on housing environment and mental health outcomes and are part of the international COVID-MINDS network [https://www.covidminds.org/]. The participating cohorts, relevant ethical considerations, and a sample size flowchart for all cohorts, are presented in Supplementary Text S1. The four cohorts were divided into the following age and gender categories: (1) Young people 18–25 years; (2) Women above 25 years; (3) Men above 25 years. Young people were considered a separate category, as young adults between ages 18 and 25 have been consistently reported to be especially vulnerable and susceptible to symptoms of poor mental health during a lockdown30. This category was not further stratified by gender due to sample size considerations. While some cohort surveys provided options for self-reported gender other than men or women (e.g. other or prefer not to say), the resulting groups were too small to perform analysis on. The UCL COVID-19 cohort included all three populations, while only young people and women > 25 years were included in the DNBC, and only women and men > 25 years were included in the TEMPO and Constances cohorts. All four cohorts are longitudinal; however, for this analysis, only data from the Spring 2020 lockdown period were used (March 30–April 5, 2020, for the DNBC, April 6–June 15 for Constances, April 6–April 12, for TEMPO, and April 6–April 12 for UCL COVID-19) (Fig. 1). The combined sample size for our analyses was 69,136 individuals across the four cohorts.
Figure 1.
Data collection in the four participating cohorts.
Housing conditions
Access to outdoor facilities such as a garden, balcony, or yard was dichotomized as having access to any outdoor space (Yes or No). Household density was defined as the dwelling size (m2 floor area) divided by the number of persons living in the dwelling. The average floor area per person in the EU is 42.6 m2 per person31; hence the variable was dichotomized as < 43 m2 or ≥ 43 m2 per person. Household crowding32,33 was adapted from the Eurostat criteria34 with alterations due to data constraints. A minimal number of rooms for a given household was calculated as follows: (i) one room for the household; (ii) one room per couple in the household; (iii) one room for each adult single person; (iv) ½ room for each child. Household crowding was categorized as reference (minimal or minimal + 1), crowded (< minimal), and under-occupied (> minimal + 1). Based on previous literature33, household composition35 was categorized as households with children, adult-only households, and single-person households. Dwelling type was categorized as apartment versus house. In the UCL COVID-19 cohort, urbanicity was coded as urban (cities), semi-urban (large/small towns), and rural (village, hamlets, or other isolated dwellings) based on self-reported postal codes and EU standards of area of living36. In the Constances cohort, urbanicity was categorized as rural versus urban. Some of the exposures were ascertained differently across cohorts (e.g. see urbanicity definitions above); data harmonization was performed by re-categorizing survey responses to optimize the comparability of data from the four datasets.
Indicators of mental health and wellbeing
The UCLA short three-item T-ILS version loneliness scale was used in the DNBC, TEMPO, and UCL COVID-19 to assess the degree of loneliness of participants. The total score ranges from 3 to 9. Scores were dichotomized, and severe loneliness was defined as scores 7–937. In Constances, loneliness was measured by the question “How often have you felt lonely during the past week?”, collected on a 1–4 Likert scale from “Rarely or None of the Time (Less than 1 Day)” to “Most or All of the Time (5–7 Days)”. Scores were dichotomized, and severe loneliness was defined as score = 4.
Anxiety was measured using the GAD-7 scale38, ranging 0–21, in Constances and UCL COVID-19. Scores were dichotomized, and severe anxiety was defined as scores 15–21. In the DNBC, the SCL-ANX439 was used. Answers to five questions are collected on a Likert scales ranging 0–4 and are then dichotomized to 0 (not at all) or 1 (a little-extremely) and summed for each subscale. Thus, the summed score for anxiety ranges from 0–4. Severe anxiety was defined as ≥ 3 as suggested by the authors of the CMDQ39,40.
The ONS Life Satisfaction scale was used to measure life satisfaction in the UCL COVID-19 cohort, while the Cantril Self-Anchoring Striving Scale was used in the rest of the cohorts. Both scales range between 0 (not at all satisfied with life) and 10 (completely satisfied with life). Among young people, the scale was categorized as low (0–5), medium (6–8), and high (9–10) life satisfaction according to cut-offs used in previous literature41,42. Among women and men > 25 years, the scale was categorized as low (0–4), medium (5–6), and high (7–10) life satisfaction according to cut-offs used in previous surveys43. In line with our other analysis where severe loneliness and anxiety were used as outcomes, we dichotomized life satisfaction as low vs. medium or high life satisfaction. Thus, for all three outcomes, odds ratios above 1 infer that the exposure is associated with a poorer outcome (higher loneliness and anxiety, and lower life satisfaction).
Statistical analysis
Statistical analysis was performed using STATA for the DNBC and UCL COVID-19, SAS for Constances, and R for TEMPO.
Weighting was performed using the entropy balancing method44 for UCL COVID-19, and marginal calibration weighting45 for Constances to achieve more representative population-based samples. No weighting was performed for DNBC and TEMPO (Supplementary Text S1).
To describe the cohorts, means and standard deviations were used for normally distributed continuous variables, and medians and interquartile ranges (IQR) were used for non-normally distributed continuous variables. Frequencies and percentages were used for categorical variables.
Outcomes were used as binary variables, and binary logistic regression analyses were performed for each exposure and outcome combination within each cohort. Odds ratios (OR) and 95% confidence intervals (CI) are reported. Missing data (19.7%) was imputed using proc mi (SAS) in the Constances cohort. In all other cohorts, complete case analysis was performed, excluding individuals with information missing on any covariate (19% for DNBC, 43.5% for TEMPO, and 53% for UCL COVID-19). The analyses were performed separately for young people, women > 25 years, and men > 25 years. Confounders were identified using directed acyclic graphs (DAGs) and previous literature. Four models were tested:
-
(i)
Unadjusted model: testing the association between exposure (access to outdoor facilities, household density, crowding, and composition, dwelling type, urbanicity) and outcome (high levels of loneliness, anxiety, and low levels of life satisfaction);
-
(ii)
Model 1: Unadjusted model + age + educational attainment + sex (in the models for young people).
-
(iii)
Model 2: Model 1 + chronic disease status + mental illness status.
-
(iv)
Model 3: Model 2 + mutual adjustments for exposures
Age was defined as < 20 or 20-25 for young people and 25–34/35–44/45–54/55–64/65+ for women and men > 25. Educational attainment was categorized as Lower secondary education, ISCED 0–2; Upper secondary education, ISCED 3–4; Tertiary education, ISCED 5–8; Other education; Not currently studying. Chronic disease status and mental illness status were defined as Yes (ever had an illness) or No.
Results from the cohorts for each exposure-outcome combination using Model 3 were pooled using random-effects meta-analysis (metafor package in R), as heterogeneity was expected between the cohorts due to geographical differences, varying governmental restrictions, lockdown severities, and varying exposure and outcome ascertainment. Subgroup analyses by gender and age categories were undertaken. Subgroups analyses by country were also evaluated to investigate cross-country differences.
Ethics statement
Ethics statements from each participating cohorts are shown in Supplementary Text S1 in detail. All experimental protocols were approved by the Danish Data Protection Agency (DNBC, Denmark), the Committee on Health Research Ethics (DNBC, Denmark), the Department of Public Health at the University of Copenhagen (DNBC, Denmark), the French Data Protection Authority (Constances, France), the institutional review board of the National Institute for Medical Research (Constances, France), the Inserm ethics committee (Constances, France), the French National Committee for Data Protection (TEMPO, France), and the UCL Research Ethics Committee (UCL COVID-19 Social Study, UK). All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all participants.
Results
Descriptive statistics of the four cohorts can be found in Supplementary Table S1. All association results from the cohorts using the unadjusted model, Model 1, Model 2, and Model 3 (the fully adjusted model) are presented in Supplementary Table S2, Supplementary Table S3, Supplementary Table S4, and Supplementary Table S5, respectively. Forest plots showing the results from the random-effects meta-analyses for all exposure-outcome pairs, using Model 3, are shown in Supplementary Text S2. Below we present pooled and cohort-specific results using Model 3.
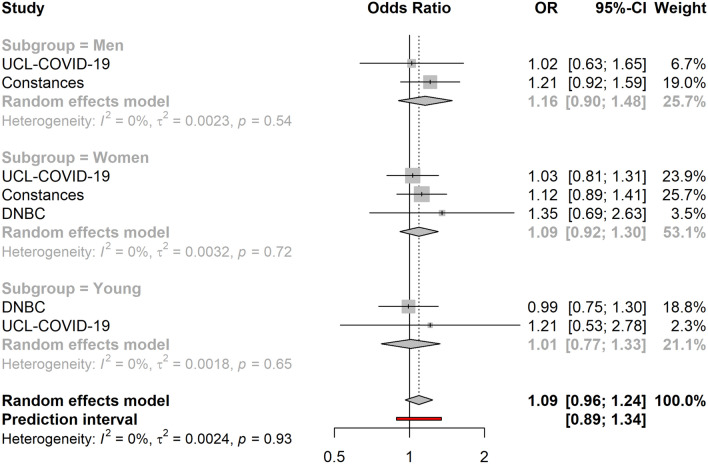
Access to outdoor space
Across all cohorts, not having access to outdoor space showed a suggestive association with higher levels of anxiety (OR = 1.09, 95% CI 0.96–1.24) (Fig. 2). Associations between access to outdoor space and loneliness (OR = 1.21, 95% CI 0.72–2.02) or life satisfaction (OR = 0.97, 95% CI 0.57–1.65) were not observed in the meta-analyses.
Figure 2.
Association between access to outdoor space (yes vs. no) and high levels of anxiety (N = 68,712). The cohort-specific estimates and 95% confidence intervals were obtained using binary logistic regression models. Age, educational attainment, gender, previously diagnosed chronic disease status and presence of previously diagnosed mental illness were used a covariates. In addition, the models included mutual adjustment for the other housing exposures. 95% CI 95% confidence interval, OR odds ratio.
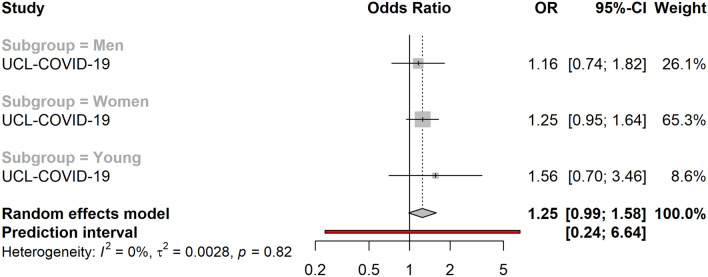
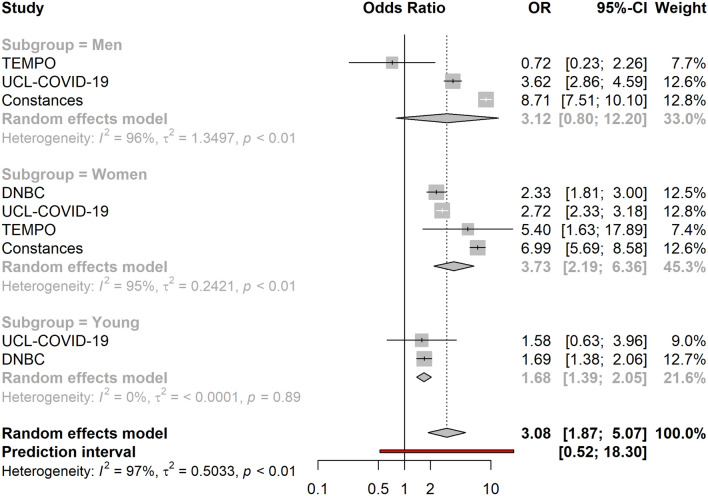
Household density, crowding, and composition
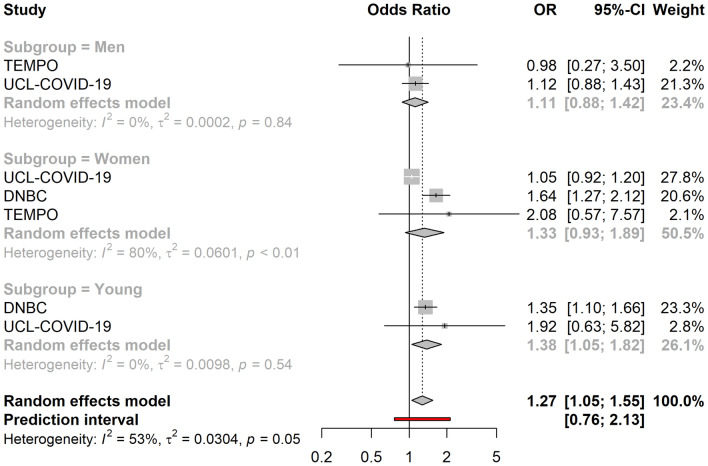
Living in under-occupied dwellings was associated with lower overall levels of loneliness (OR = 0.82, 95% CI 0.72–0.94). Similarly, living in crowded dwellings was suggestively associated with lower life satisfaction (OR = 1.25, 95% CI 0.99–1.58) (Fig. 3) and higher levels of loneliness in adult men (OR = 1.27, 95% CI 0.96–1.69) and women (OR = 1.26, 95% CI 1.01–1.58), while it was associated with lower levels of loneliness amongst young people (OR = 0.42, 95%CI: 0.21–0.84). Subgroup analyses showed that low household density, defined as having access to ≥ 43 m2 per person, was associated with higher levels of loneliness in men (OR = 1.36, 95% CI 1.18–1.57) and women (OR = 1.23, 95% CI 1.04–1.46) > 25 years, but lower levels of loneliness amongst the young (OR = 0.89, 95% CI 0.79–1.00). Similarly, low household density was associated with lower levels of anxiety amongst the young (OR = 0.76, 95% CI 0.67–0.86). However, living in under-occupied dwellings was associated with higher levels of anxiety in the young (OR = 2.36, 95% CI 1.08–5.17), while it was associated with lower levels of anxiety in adult men (OR = 0.77, 95% CI 0.56–1.04) and women (OR = 0.80, 95% CI 0.71–0.89). Living alone (vs. living with others) was associated with high overall levels of loneliness (OR = 3.08, 95% CI 1.87–5.07), (Fig. 4) and overall lower life satisfaction (OR = 1.27, 95% CI 1.05–0.55) (Fig. 5). While the association between living alone and loneliness was the association of the greatest magnitude that we observed in this study, no associations were detected between living alone and anxiety (OR = 0.86, 95% CI 0.59–1.25). Living with children was associated with higher levels of anxiety amongst women (OR = 1.10, 95% CI 1.00–1.22), but not in men (OR = 1.03, 95% CI 0.73–1.47), or the young (OR = 0.73, 95% CI 0.36–1.49).
Figure 3.
Association between household crowding and low life satisfaction (N = 18,652). The cohort-specific estimates and 95% confidence intervals were obtained using binary logistic regression models. Age, educational attainment, gender, previously diagnosed chronic disease status and presence of previously diagnosed mental illness were used a covariates. In addition, the models included mutual adjustment for the other housing exposures. 95% CI 95% confidence interval, OR odds ratio.
Figure 4.
Association between living alone (vs. living with others) and high levels of loneliness (N = 69,136). The cohort-specific estimates and 95% confidence intervals were obtained using binary logistic regression models. Age, educational attainment, gender, previously diagnosed chronic disease status and presence of previously diagnosed mental illness were used a covariates. In addition, the models included mutual adjustment for the other housing exposures. 95% CI 95% confidence interval, OR odds ratio.
Figure 5.
Association between living alone (vs. living with others) and low life satisfaction (N = 40,965). The cohort-specific estimates and 95% confidence intervals were obtained using binary logistic regression models. Age, educational attainment, gender, previously diagnosed chronic disease status and presence of previously diagnosed mental illness were used a covariates. In addition, the models included mutual adjustment for the other housing exposures. 95% CI 95% confidence interval, OR odds ratio.
Urbanicity and dwelling type
Living in a rural environment (vs. urban environment) was not associated with either loneliness (OR = 1.06, 95% CI 0.81–1.38), anxiety (OR = 0.97, 95% CI 0.83–1.13), or life satisfaction (OR = 0.96, 95% CI 0.72–1.28) in the meta-analyses or individual cohort subgroups. Similarly, living in an apartment (vs. house) also did not associate with loneliness (OR = 0.90, 95% CI 0.51–1.61), anxiety (OR = 0.93, 95% CI 0.68–1.26), or life satisfaction (OR = 0.83, 95% CI 0.50–1.40) in the meta-analyses or individual cohort subgroups.
Cross-country comparisons
For cross-country comparisons, we repeated our meta-analyses using countries as subgroups (Supplementary Text S3). These analyses revealed that low household density, defined as having access to ≥ 43 m2 per person, was associated with higher levels of loneliness in France (OR = 1.36, 95% CI 1.21–1.53), but not in other countries. Interestingly, living in crowded dwellings was suggestively associated with higher levels of loneliness in France (OR = 1.36, 95% CI 1.10–1.69), while living in under-occupied dwellings was associated with lower levels of loneliness (OR = 0.76, 95% CI 0.60–0.96) and anxiety (OR = 0.81, 95% CI 0.71–0.92). Having no access to outdoor spaces was suggestively associated with higher levels of anxiety in France (OR = 1.16, 95% CI 0.97–1.38), but not in the other countries. Living with children was suggestively associated with lower levels of loneliness in Denmark (OR = 0.90, 95% CI 0.81–1.00), while it tended to associate with higher levels of loneliness in other countries, especially amongst young people in the UK (OR = 2.87, 95% CI 1.39–5.92). Living with children was associated with higher levels of anxiety in France (OR = 1.15, 95% CI 1.01–1.31), but not in the other countries. Living alone was associated with lower life satisfaction in Denmark (OR = 1.47, 95% CI 1.20–1.80), and while directionally similar, this association did not reach statistical significance for other countries. Living alone was associated with lower levels of anxiety in the UK (OR = 0.50, 95% CI 0.31–0.80), whereas opposite trends were seen in Denmark (OR = 1.15, 95% CI 0.96–1.38) and France (OR = 1.18, 95% CI 0.71–1.96).
Discussion
We show results from an analysis of ~ 70,000 individuals from three European countries with available housing environment and mental health data during the first lockdown of the COVID-19 pandemic during spring 2020. As previous research shows that Europeans spend most of their life indoors13, which was the case to an even greater extent during lockdowns with curfews and stay at home recommendations, we set out to quantify the associations between various facets of the housing environment and the mental health and wellbeing of Europeans during the first severe lockdown of the pandemic.
Our key findings are as follows: (1) Living alone was consistently related to worse mental health during lockdown; (2) living in dwellings offering more rooms for a given household was related to better mental health, albeit with some differences by country and age groups; (3) having access to outdoor space appeared to be associated with lower levels of anxiety; (4) urbanicity and dwelling types were not associated with mental health status; (5) women’s mental health seemed to be more strongly associated with household composition than men’s.
Our results regarding poorer mental health, especially loneliness, amongst people living alone during the lockdown are consistent with other studies20,46. As suggested in the literature, lockdown situations heighten already existing risk factors of loneliness, such as living alone20. Therefore, as both social isolation and loneliness have been shown to be associated with increased mortality, impaired quality of life, and wellbeing47, people living alone might benefit from community support during lockdowns. With the rise in the proportion of people living alone across age-groups48, we also recommend piloting screening methods to identify the most vulnerable individuals in communities (e.g. those living alone) for the prioritization of additional support.
Our results indicate that living in under-occupied dwellings is associated with better mental health outcomes: lower levels of loneliness and anxiety, and higher life satisfaction. Another finding is that living in less dense environments (having access to more square meters per person) is associated with worse outcomes amongst adults > 25, but better outcomes in young adults < 25. While these findings seem counterintuitive, they appear to be largely driven by results from the French Constances cohort, where (1) both measures of household density and crowding were simultaneously available, so we were able to capture the difference between these determinants; (2) both low household density (vs. high household density) and living in more crowded dwellings (vs. ideal levels) were associated with worse outcomes, e.g. higher levels of loneliness. As Constances was the only cohort where both household density and crowding were measured, we were unable to verify these findings in other cohorts. However, as emphasized above, overall results from the meta-analyses show that living in under-occupied dwellings is generally associated with better mental health. These results are supported by a 2018 systematic review on household crowding49, which concluded that crowding may be associated with poor mental health. During a lockdown, it has been reported that people living in overcrowded dwellings were more likely to report poor mental health than people living in non-overcrowded housing50.
Our results suggest that lacking access to outdoor spaces is associated with higher levels of anxiety, but not with loneliness or quality of life. Evidence from previous studies suggests that access to outdoor green and blue spaces is beneficial for mental health51,52. During lockdowns, several studies also reported that access to natural green spaces was associated with better mental health53,54. Although having access to natural green spaces might be most beneficial for mental health55, this study suggests that having access to any type of outdoor spaces (e.g. balcony, garden, or yard) compared to none, may lower levels of anxiety during a lockdown. Consistently, results from our previous study among young people in Denmark have shown that individuals without access to outdoor spaces experienced greater decline in well-being during the COVID-19 pandemic21. Therefore, housing and urban design strategies should ensure access to outdoor spaces for all56.
In this study, no differences in mental health indicators were found by urbanicity or dwelling type. The relationship between urbanicity and mental health pre-pandemic is contradictory, with some reports showing a clear benefit of rural environments57, but some showing no difference between urban and rural environments58. However, recent evidence pointed towards a higher prevalence of poor mental health indicators, such as anxiety disorders and PTSD, in urban environments59. In line with this review, recent cross-cohort analyses from the UK reported that urban residents had a higher risk of being lonely both before and during the pandemic20. Similarly, it was reported in a Scottish cross-sectional study that urban residents were more psychologically distressed during the COVID-19 pandemic compared to rural residents60. The discrepancies between our results and the UK studies might have arisen due to differences in urbanicity classification. It may also be that our definition was too broad to be sensitive to certain aspects of urbanicity that would truly matter during lockdowns, such as the urban physical (e.g. noise pollution) and social (e.g. social cohesion) environments59. In line with these considerations, we expect a greater proportion of dwellings with direct access to outdoor space to be rural or semi-urban, thus, mutual adjustment for these factors is expected to result in attenuated estimates relative to urbanicity, which we do observe for some of our results.
Previous studies have shown that women, young people, and those with young children experienced the greatest increase in mental distress during the COVID-19 pandemic4,61. In this study, women living in households with children reported higher levels of anxiety compared to men and younger adults living with children. This result might be explained by a salient aspect of the COVID-19 crisis, which involved large-scale closures of daycare centers and schools, resulting in children staying at home and needing to be cared for and home-schooled62. Previous studies have shown that parents experienced high levels of stress, anxiety and depressive symptoms due to homeschooling during COVID-19 lockdowns63–65. As, globally, women are still responsible for most of the unpaid care work, such as raising children66, we recommend the prioritization of the provision of child care, especially for young children, as well as flexible working hours and paid sick leave for parents during lockdowns.
The collected data make it possible to compare associations between housing environment exposures and mental health outcomes across three European countries. The Oxford COVID-19: Government Response Tracker was developed to rank a range of governmental policies in response to the pandemic on a score from 0 to 100 according to their stringency. According to this stringency metric, France had the most stringent governmental response with a score of 88 out of 100 compared to 80 in the UK and 72 in Denmark three weeks into the respective national lockdowns in the spring of 202067. France and the UK likely had higher scores as both countries implemented curfews during this period, while more freedom of movement was allowed in Denmark. Thus, we expected that associations between certain characteristics of the household environment and negative mental health outcomes would be starker in France and the UK compared to Denmark. Our findings appear to be partly in line with this expectation, as a range of associations were most apparent in France and were likely driving some of the overall findings. The lack of differences in some of the examined associations can probably be attributed to the fact that the range of stringency levels in the three countries were still relatively close to each other; future comparisons with countries implementing less strict governmental responses—e.g. Sweden68—are warranted to explore the extent to which governmental stringency is relevant to the examined associations.
The importance of our results is threefold. First, our study can inform policy makers, authorities, and other stakeholders about the associations between various facets of the housing environment and mental health indicators in a period when citizens are encouraged or mandated to stay at home. Second, this study demonstrates that some living conditions (e.g. living alone, crowded households, lacking access to outdoor spaces) may be especially important to certain aspects of mental health during a lockdown; the identification of these factors might help to develop interventions, novel community-based support mechanisms and screening procedures to help those most affected by lockdowns. Third, while many of the reported inequalities have been observed before, it is likely that the COVID-19 pandemic and its lockdowns exacerbated some of these already existing associations. In the long term, this study might inform policy-makers and urban planners on these aspects with potential indications of specific requirements for different residents.
Important strengths of this study are its large sample size, the utilization of four cohorts from three European countries, and the availability of detailed harmonized information of housing environments, related factors and mental health outcomes during the first lockdown of the COVID-19 pandemic. Our sample includes individuals across a wide age range and from three European countries, enabling cross-country as well as sex- and age-specific comparisons.
The most important limitations of our study are the self-reported data on housing conditions and mental health outcomes, and that we did not have access to pre-pandemic data to undertake comparisons. Self-reported data are prone to various biases, and it is possible that these biases impacted our analysis. As complete-case analysis was used in most cohorts, missing data on exposures, outcomes or covariates might have also impacted our findings. This might be especially important regarding the mental health outcomes, where we expect those with the worst mental health to decide not to respond or underreport certain exposures; such biases would most likely attenuate findings. Another key limitation is that this study only included data from three Western and Northern European countries, and thus, our findings might not generalize to other settings. We consider cross-country comparisons suggestive and explorative; as results generally emanate from a single large cohort for all participating countries, it is hard to deduce whether larger, more comprehensive, and nationally representative samples would have produced different results. While weighting strategies were utilized in Constances and UCL COVID-19, where this was possible, TEMPO and DNBC were not designed to be representative of the general population. Last, in addition to our limitations regarding geographical generalizability, the cross-sectional nature of the data also limits our ability to generalize over time. Our results are based on self-reported data, which were collected at the beginning of the COVID-19 pandemic (spring 2020), at a time when most individuals likely experienced dynamic changes in their mental health in response to changing biological, societal, and political realities6,30.
In conclusion, we show that while urbanicity and household dwelling type was not associated with mental health, the other examined housing conditions, namely household composition, access to outdoor facilities, and household crowding and density, were associated with various aspects of mental health in three European countries during the first strict lockdowns of the COVID-19 pandemic, in spring 2020. Living alone, especially, was associated with severe loneliness and lower life satisfaction, but not with anxiety, while living with children was associated with higher levels of anxiety amongst women. These results pinpoint population groups that might need targeted interventions to ameliorate the negative mental health impact of the COVID-19 pandemic and its associated lockdowns.
Supplementary Information
Acknowledgements
The authors thank the INSERM-Versailles Saint Quentin en Yvelines University “Population-based Epidemiologic Cohorts Unit” (Cohortes épidémiologiques en population) which designed and manages the Constances Cohort Study. They also thank the National Health Insurance Fund (“Caisse nationale d’assurance maladie des travailleurs salaries,” CNAMTS) and its Health Screening Centres (“Centres d’examens de santé”), which are collecting a large part of the data, as well as the National Old-Age Insurance Fund (Caisse nationale d’assurance vieillesse) for its contribution to the constitution of the cohort, ClinSearch, Asqualab and Eurocell, which are conducting the data quality control.
Author contributions
Conceptualization: A.K., J.G., K.S., T.V.V.; Data curation: A.K., J.G., J.M., F.B., T.E.; Formal analysis: A.K., J.G., J.M., F.B., T.E., T.V.V.; Funding acquisition: D.F., M.Z., M.G., A.N., N.H.R., K.S.; Investigation: A.K., J.G., J.M., F.B., T.E., T.V.V.; Methodology: A.K., J.G., T.V.V.; Project administration: A.K.; Resources: D.F., M.Z., M.G., A.N., N.H.R., K.S.; Software: A.K., J.G., J.M., F.B., T.E., T.V.V.; Supervision: D.F., M.Z., M.G., A.N., N.H.R., K.S.; Validation: J.M., F.B., T.E.; Visualization: A.K., T.V.V.; Roles/Writing—original draft: A.K., T.V.V.; Writing—review & editing: A.K., J.G., J.M., F.B., T.E., D.F., M.Z., M.G., A.N., N.H.R., K.S., T.V.V.
Funding
This study was made possible by a grant from the RealDania Foundation (PRJ-2019-00020 ‘Indoor environment and child health…’). The DNBC was established with a significant grant from the Danish National Research Foundation. Additional support was obtained from the Danish Regional Committees, the Pharmacy Foundation, the Egmont Foundation, the March of Dimes Birth Defects Foundation, the Health Foundation and other minor grants. Follow‐up of mothers and children has been supported by the Danish Medical Research Council (SSVF 0646, 271‐08‐0839/06‐066023, O602‐01042B, 0602‐02738B), the Lundbeck Foundation (195/04, R100‐A9193), The Innovation Fund Denmark 0603‐00294B (09‐067124), the Nordea Foundation (02‐2013‐2014), Aarhus Ideas (AU R9‐A959‐13‐S804), a University of Copenhagen Strategic Grant (IFSV 2012) and the Danish Council for Independent Research (DFF—4183‐00594 and DFF—4183‐00152). Follow-up of mother and children in the COVID-19 data collection was supported by a grant from the Velux Foundation (grant number 36336, ‘Standing together at a distance—How Danes are living with the Corona Crisis’). The TEMPO cohort received funding from the French National Research Agency (ANR) including the Flash COVID-19 funding scheme; the French Institute for Public Health Research-IReSP (TGIR Cohortes); the French Inter-departmental Mission for the Fight against Drugs and Drug Addiction (MILDeCA); the French Institute of Cancer (INCa); and the Pfizer Foundation. The CONSTANCES COVID-19 Study was funded by: ANR (Agence Nationale de la Recherche, #ANR-20-COVI-000, #ANR-10-COHO-06), Fondation pour la Recherche Médicale (#20RR052-00), Inserm (Institut National de la Santé et de la Recherche Médicale, #C20-26). The CONSTANCES Cohort Study was supported and funded by the French National Health Insurance Fund (“Caisse nationale d’assurance maladie”, CNAM). The CONSTANCES Cohort Study is an “Infrastructure nationale en Biologie et Santé” and benefits from a grant from the French National Agency for Research (ANR-11-INBS-0002). CONSTANCES is also partly funded by Merck Sharp & Dohme (MSD), AstraZeneca, Lundbeck and L’Oréal. None of these funding sources had any role in the design of the study, collection and analysis of data or decision to publish. The Covid-19 Social Study was funded by the Nuffield Foundation [WEL/FR-000022583], but the views expressed are those of the authors and not necessarily the Foundation. The study was also supported by the MARCH Mental Health Network funded by the Cross-Disciplinary Mental Health Network Plus initiative supported by UK Research and Innovation [ES/S002588/1], and by the Wellcome Trust [221400/Z/20/Z]. DF was funded by the Wellcome Trust [205407/Z/16/Z]. The researchers are grateful for the support of a number of organisations with their recruitment efforts including: the UKRI Mental Health Networks, Find Out Now, UCL BioResource, SEO Works, FieldworkHub, and Optimal Workshop. The study was also supported by HealthWise Wales, the Health and Care Research Wales initiative, which is led by Cardiff University in collaboration with SAIL, Swansea University. The funders had no role in the study design, data collection, data analysis, interpretation, the writing of the report, and decisions on where to publish.
Data availability
Due to ethical reasons, investigators are not able to share individual level data. Summary data are shared in the Supplemental Material.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-09316-4.
References
- 1.Salari N, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health. 2020;16:1–11. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry. 2020;63:e32. doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pierce M, et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Essadek A, Rabeyron T. Mental health of French students during the Covid-19 pandemic. J. Affect. Disord. 2020;277:392–393. doi: 10.1016/j.jad.2020.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clotworthy A, et al. “Standing together - at a distance”: Documenting changes in mental-health indicators in Denmark during the COVID-19 pandemic. Scand. J. Public Health. 2020;49:79–87. doi: 10.1177/1403494820956445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pedersen MT, et al. Time trends in mental health indicators during the initial 16 months of the COVID-19 pandemic in Denmark. BMC Psychiatry. 2022;22:1–13. doi: 10.1186/s12888-021-03655-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. Lancet Psychiatry. 2021;8:141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andersen LH, Fallesen P, Bruckner TA. Risk of stress/depression and functional impairment in Denmark immediately following a COVID-19 shutdown. BMC Public Health. 2021;21:1–11. doi: 10.1186/s12889-021-11020-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Overbeck G, et al. Depression and anxiety symptoms in pregnant women in Denmark during COVID-19. Scand. J. Public Health. 2021;49:721–729. doi: 10.1177/14034948211013271. [DOI] [PubMed] [Google Scholar]
- 11.Sun Y, et al. Comparison of mental health symptoms prior to and during COVID-19: Evidence from a living systematic review and meta-analysis. medRxiv. 2021;17:65. [Google Scholar]
- 12.Flaxman S, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584:257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 13.European Commission . Indoor Air Pollution: New EU Research Reveals Higher Risks than Previously Thought. Joint Research Center; 2003. [Google Scholar]
- 14.Gibson M, et al. Housing and health inequalities: A synthesis of systematic reviews of interventions aimed at different pathways linking housing and health. Health Place. 2011;17:175–184. doi: 10.1016/j.healthplace.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krieger J, Higgins DL. Housing and health: Time again for public health action. Am. J. Public Health. 2002;92:758–768. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silva Moreira P, et al. Protective elements of mental health status during the COVID-19 outbreak in the Portuguese population. Int. J. Environ. Res. Public Health. 2021;18:1910. doi: 10.3390/ijerph18041910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bourion-Bédès S, et al. Psychological impact of the COVID-19 outbreak on students in a French region severely affected by the disease: Results of the PIMS-CoV 19 study. Psychiatry Res. 2021;295:113559. doi: 10.1016/j.psychres.2020.113559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haesebaert F, Haesebaert J, Zante E, Franck N. Who maintains good mental health in a locked-down country? A French nationwide online survey of 11,391 participants. Health Place. 2020;66:102440. doi: 10.1016/j.healthplace.2020.102440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amerio A, et al. Covid-19 lockdown: Housing built environment’s effects on mental health. Int. J. Environ. Res. Public Health. 2020;17:5973. doi: 10.3390/ijerph17165973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bu F, Steptoe A, Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31–34. doi: 10.1016/j.puhe.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Groot J, et al. Impact of housing conditions on changes in youth’s mental health following the initial national COVID-19 lockdown: A cohort study. Sci. Rep. 2020;12:1–10. doi: 10.1038/s41598-022-04909-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blettner M, Sauerbrei W, Schlehofer B, Scheuchenpflug T, Friedenreich C. Traditional reviews, meta-analyses and pooled analyses in epidemiology. Int. J. Epidemiol. 1999;28:1–9. doi: 10.1093/ije/28.1.1. [DOI] [PubMed] [Google Scholar]
- 23.Friedenreich CM. Methods for pooled analyses of epidemiologic studies. Epidemiology. 1993;4:295–302. doi: 10.1097/00001648-199307000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Steinberg K, et al. Comparison of effect estimates from a meta-analysis of summary data from published studies and from a meta-analysis using individual patient data for ovarian cancer studies. Am. J. Epidemiol. 1997;145:917–925. doi: 10.1093/oxfordjournals.aje.a009051. [DOI] [PubMed] [Google Scholar]
- 25.Burke DL, Ensor J, Riley RD. Meta-analysis using individual participant data: One-stage and two-stage approaches, and why they may differ. Stat. Med. 2017;36:855–875. doi: 10.1002/sim.7141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Von Elm E, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Bull. World Health Organ. 2007;85:867–872. doi: 10.2471/BLT.07.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olsen J, et al. The Danish National Birth Cohort–its background, structure and aim. Scand. J. Public Health. 2001;29:300–307. doi: 10.1177/14034948010290040201. [DOI] [PubMed] [Google Scholar]
- 28.Zins M, Goldberg M, team, C The French CONSTANCES population-based cohort: design, inclusion and follow-up. Eur. J. Epidemiol. 2015;30:1317–1328. doi: 10.1007/s10654-015-0096-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Redonnet B, Chollet A, Fombonne E, Bowes L, Melchior M. Tobacco, alcohol, cannabis and other illegal drug use among young adults: The socioeconomic context. Drug Alcohol Depend. 2012;121:231–239. doi: 10.1016/j.drugalcdep.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 30.Varga TV, et al. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: A longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg. Health Eur. 2021;2:10002. doi: 10.1016/j.lanepe.2020.100020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.European Commission. Housing Space per Person. https://ec.europa.eu/energy/content/housing-space-person_en.
- 32.Gray, A. Definitions of crowding and the effects of crowding on health. In A Literature Review Prepared for the Ministry of Social Policy (2001).
- 33.Hansen CB, Larsen CV, Bjerregaard P, Riva M. The effect of household crowding and composition on health in an Inuit cohort in Greenland. Scand. J. Public Health. 2020;49:921–930. doi: 10.1177/1403494820929496. [DOI] [PubMed] [Google Scholar]
- 34.Eurostat. Is Your Home Too Crowded?https://ec.europa.eu/eurostat/web/products-eurostat-news/-/DDN-20200422-1.
- 35.Eurostat. Household Composition Statistics. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Household_composition_statistics.
- 36.European Commission. Regional and Urban Policy. https://ec.europa.eu/info/departments/regional-and-urban-policy_en.
- 37.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Res. Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 39.Christensen KS, et al. A brief case-finding questionnaire for common mental disorders: the CMDQ. Fam. Pract. 2005;22:448–457. doi: 10.1093/fampra/cmi025. [DOI] [PubMed] [Google Scholar]
- 40.Larsen AR, Engsbro AL, Bytzer P. Screening instruments for anxiety and depression in patients with irritable bowel syndrome are ambiguous. Dan Med. J. 2014;61:A4785. [PubMed] [Google Scholar]
- 41.Due P, et al. Trends in high life satisfaction among adolescents in five Nordic countries 2002–2014. Nordisk välfärdsforskning| Nordic Welf. Res. 2019;4:54–66. [Google Scholar]
- 42.Mazur J, Szkultecka-Dębek M, Dzielska A, Drozd M, Małkowska-Szkutnik A. What does the Cantril Ladder measure in adolescence? Arch. Med. Sci. AMS. 2018;14:182. doi: 10.5114/aoms.2016.60718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boarini, R., Comola, M., Smith, C., Manchin, R. & De Keulenaer, F. What makes for a better life? The determinants of subjective well-being in OECD countries—Evidence from the Gallup World Poll. (2012).
- 44.Hainmueller J. Entropy balancing for causal effects: A multivariate reweighting method to produce balanced samples in observational studies. Polit. Anal. 2012;20:25–46. [Google Scholar]
- 45.Deville JC, Särndal CE. Calibration estimators in survey sampling. J. Am. Stat. Assoc. 1992;87:376–382. [Google Scholar]
- 46.Groarke JM, et al. Loneliness in the UK during the COVID-19 pandemic: Cross-sectional results from the COVID-19 Psychological Wellbeing Study. PLoS ONE. 2020;15:e0239698. doi: 10.1371/journal.pone.0239698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc. Natl. Acad. Sci. USA. 2013;110:5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Demey D, Berrington A, Evandrou M, Falkingham J. Pathways into living alone in mid-life: Diversity and policy implications. Adv. Life Course Res. 2013;18:161–174. doi: 10.1016/j.alcr.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 49.Shannon, H. et al. WHO Housing and health guidelines: Web annex A: Report of the systematic review on the effect of household crowding on health (2018).
- 50.National Housing Federation. Housing Issues During Lockdown: Health, Space and Overcrowding. https://www.housing.org.uk/globalassets/files/homes-at-the-heart/housing-issues-during-lockdown---health-space-and-overcrowding.pdf.
- 51.Gascon M, et al. Long-term exposure to residential green and blue spaces and anxiety and depression in adults: A cross-sectional study. Environ. Res. 2018;162:231–239. doi: 10.1016/j.envres.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 52.Kondo MC, et al. Momentary mood response to natural outdoor environments in four European cities. Environ. Int. 2020;134:105237. doi: 10.1016/j.envint.2019.105237. [DOI] [PubMed] [Google Scholar]
- 53.Pouso S, et al. Contact with blue-green spaces during the COVID-19 pandemic lockdown beneficial for mental health. Sci. Total Environ. 2021;756:143984. doi: 10.1016/j.scitotenv.2020.143984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dzhambov AM, et al. Does greenery experienced indoors and outdoors provide an escape and support mental health during the COVID-19 quarantine? Environ. Res. 2021;196:110420. doi: 10.1016/j.envres.2020.110420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shuda Q, Bougoulias ME, Kass R. Effect of nature exposure on perceived and physiologic stress: A systematic review. Complement. Ther. Med. 2020;53:10251. doi: 10.1016/j.ctim.2020.102514. [DOI] [PubMed] [Google Scholar]
- 56.Bird E, et al. Built and natural environment planning principles for promoting health: An umbrella review. BMC Public Health. 2018;18:1–13. doi: 10.1186/s12889-018-5870-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gruebner O, et al. Cities and mental health. Dtsch. Arztebl. Int. 2017;114:121. doi: 10.3238/arztebl.2017.0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Breslau J, Marshall GN, Pincus HA, Brown RA. Are mental disorders more common in urban than rural areas of the United States? J. Psychiatr. Res. 2014;56:50–55. doi: 10.1016/j.jpsychires.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 59.Ventimiglia I, Seedat S. Current evidence on urbanicity and the impact of neighbourhoods on anxiety and stress-related disorders. Curr. Opin. Psychiatry. 2019;32:248–253. doi: 10.1097/YCO.0000000000000496. [DOI] [PubMed] [Google Scholar]
- 60.Hubbard G, et al. Are rurality, area deprivation, access to outside space, and green space associated with mental health during the covid-19 pandemic? A cross sectional study (charis-e) Int. J. Environ. Res. Public Health. 2021;18:3869. doi: 10.3390/ijerph18083869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pieh C, Budimir S, Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020;136:110186. doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Alon T, Doepke M, Olmstead-Rumsey J, Tertilt M. The Impact of COVID-19 on Gender Equality. National Bureau of Economic Research; 2020. [Google Scholar]
- 63.Thorell LB, et al. Parental experiences of homeschooling during the COVID-19 pandemic: Differences between seven European countries and between children with and without mental health conditions. Eur. Child Adolesc. Psychiatry. 2021;7:1–13. doi: 10.1007/s00787-020-01706-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fong VC, Iarocci G. Child and family outcomes following pandemics: A systematic review and recommendations on COVID-19 policies. J. Pediatr. Psychol. 2020;45:1124–1143. doi: 10.1093/jpepsy/jsaa092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Calvano C, et al. Families in the COVID-19 pandemic: parental stress, parent mental health and the occurrence of adverse childhood experiences—Results of a representative survey in Germany. Eur. Child Adolesc. Psychiatry. 2021;1:1–13. doi: 10.1007/s00787-021-01739-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Power K. The COVID-19 pandemic has increased the care burden of women and families. Sustain. Sci. Pract. Policy. 2020;16:67–73. [Google Scholar]
- 67.Hale T, Webster S. Oxford COVID-19 government response tracker. Nat. Hum. Behav. 2020;5:529–538. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- 68.Saunes, I. S. et al. Nordic responses to Covid-19: Governance and policy measures in the early phases of the pandemic. Health Policy5, S0168–8510(21)00222-0 (2021). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Due to ethical reasons, investigators are not able to share individual level data. Summary data are shared in the Supplemental Material.