Abstract
Background:
Second-hand smoking (SHS) is associated with many health problems. However, its prevalence in the community population aged 15 years and older in Vietnam is unknown.
Objectives:
To quantify the prevalence of SHS in Vietnamese communities aged 15 and above.
Methods:
This is a meta-analysis that reviewed studies of the prevalence of SHS in Vietnam published in MEDLINE, Scopus, Pubmed and the WHO library database between 1 January 2010 and 31 December 2019. MedCalc was used to perform all the analyses, and publication bias was determined using funnel plots and Egger regression asymmetry tests. Q-test and I2 statistic were used to identify heterogeneity across studies.
Results:
There were 7 articles that met our inclusion criteria 2 surveys at the national level, 3 Cross-sectional studies and 2 Case-control studies) involving 184 921 participants. According to the meta-analysis, the overall random-effects pooled prevalence of SHS was 54.6% (95% CIs: 44.900-64.154) with a high level of heterogeneity (P = .0001, Q = 2245.60, I2 = 99.73%). It is noteworthy that the pooled prevalence of SHS rose throughout the course of the survey years. Our research found no evidence of publication bias.
Conclusions:
Vietnam has ratified the implementation the WHO Framework Convention on Tobacco Control (FCTC) in 2004, there are still a large number of people who are adversely impacted by SHS. Given the tremendous cost that SHS imposes on health systems, our results underscore the critical need for the Vietnamese government to expedite an implementation of a set of stronger tobacco control practices, thus reducing the incidence of smoking-related illnesses and fatalities.
Keywords: Vietnam, smoking, secondhand smoking, passive smoking
Introduction
Despite the fact that the COVID-19 pandemic hit the world very hard that was unprepared, but preventable catastrophe as a decades-old pandemic of tobacco smoking has persisted unabated, continued claiming lives and making people ill since it is causally related to diseases affecting virtually all organs of the body. 1 Second-hand smoke (SHS) is a combination of smoke produced by the burning end of a cigarette and smoke exhaled by smokers. SHS is a complex combination comprising thousands of compounds, of which over 250 of which are known to be harmful and at least 69 of which are known to cause cancer. 2 According to solid scientific evidence, SHS contributes attributable to the premature deaths per year and serious illness of people who do not smoke. 1 The burden of tobacco-related disease weighs heavily on Vietnam, where tobacco is responsible for about 7.2 million deaths per year, including those caused by SHS, and is expected to continue growing at a frightening pace in the future. 3 Approximately 40 000 people each year in Vietnam die as a consequence of tobacco-related diseases, which include heart disease, stroke, and lung cancer. Cigarette smoking is responsible for 30 percent of all heart disease deaths in Vietnam. 4 In Vietnam, tobacco usage is currently common among nearly 1 out of every 2 adult males, according to the latest statistics (45.3%). As a result, about 34.5 million non-smokers are exposed to SHS in their residences as well as in public areas like as restaurants, hotels, and places of work, putting a significant number of people at risk for cardiovascular disease and other diseases. According to WHO, SHS raises the risk of heart disease and stroke in not just smokers, but also non-smokers who are exposed to harmful substances in tobacco smoke. 4
Toward the goal of reducing tobacco-related morbidity and mortality, Vietnam began implementing smoke-free policies, including ratifying the WHO FCTC in 2009, mandating smoking restrictions in indoor public places in 2010, 5 and enacting the comprehensive Law on Prevention and Control of Tobacco Harms in 2012. 6 Since the law has been endorsed, several associated initiatives have been undertaken to facilitate the implementation of smoke-free workplaces and public spaces. The exertion included, for example, publicizing the smoke-free provisions of the Law; creating and disseminating no-smoking signs at public places; initiating a public awareness campaign on the dangers of SHS; and instructing managers in both public and private areas about the dangers of SHS and how to create smoke-free workplaces and public spaces. 7
As of now, there has been very little study on changes in SHS levels in developing countries, notably in Vietnam, and there are little published review of changes in SHS levels following the adoption of the tobacco control law. Until 2020, the SHS concentration in a selection of public locations was measured by Tran K Long and his colleagues. According to the findings, the SHS concentration in restaurants, cafeterias, and coffee shops fell by about 45% after tobacco control regulations were implemented, indicating an improvement in air quality in these establishments. More enforcement of the country’s anti-smoking legislation is thus needed in order to eradicate SHS in public places due to the fact that partial bans are ineffective in Vietnam. 8
The different definitions of non-smokers used in each study, as well as the difficulties in precisely defining the sites where non-smokers are exposed to SHS, present challenges in assessing SHS. Furthermore, the magnitude of SHS in Vietnam has not been systematically summarized. Consequently, meta-analysis has been critical in determining the magnitude of SHS by statistically aggregating a number of individual original investigations.
Materials and Methods
Literature search
We conducted a systematic review and meta-analysis following the statements on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Comprehensive literature searches in MEDLINE, Scopus, Pubmed and the WHO library database for the relevant works published in any scientific field. The following search terms were used: “Passive smoking” or “Secondhand smoking” and “Vietnam.” Date filters were not used in order to get a comprehensive list of possible research.
Study selection
We considered studies to be eligible if they met all the following criteria: 1) a research that provides a precise definition of secondhand smoke or passive smoking, (2) the target population are non-smoker and aged 15 years and above, (3) the exposure to any kind of type and number of cigarettes or other tobacco products burned (4) a cross-sectional study or primary observational study with case-control or prospective cohort design which shown the result in the prevalence of SHS in Vietnam.
The following exclusion criteria were applied if they met any of the following criteria: (1) a study published in languages other than English, (2) a research conducted in vivo or in vitro, recommendations, expert statements, a case report, or a meta-analysis, (3) research conducted on the same demographic sample, and (4) overseas Vietnamese.
Because the information in this research was derived from publications that were already publicly available, there was no requirement for approval from an ethical committee or consent from participants.
Data extraction
With the help of Rayyan, we were able to identify duplicates (https://www.rayyan.ai). Separately, 2 investigators extracted and evaluated the quality of each eligible research by reading titles, abstracts, and full texts. We created organized spreadsheets in order to simplify the gathering of full and accurate data. Data collected included: first author, year of publication, participant characteristics (geographical location, gender, age, and sample size) and study methods (time of survey, type of survey, method of random sampling, and definition and measurement of passive smoking). Following a review of titles, iterative articles were omitted. Discussions were held to address disagreements and inconsistencies in the selection of studies and data extraction.
Quality assessment
After the relevant studies were determined in terms of title and content, JBI Critical Appraisal Checklist for Studies Reporting Prevalence Data was reviewed and the results are provided in Table 1. These criteria comprises 9 categories including the use of an appropriate sample frame, sampling method, sample size, description of research settings, sample coverage, measurement validity, data collection procedures, and statistical analysis techniques, as well as the generalizability of results. Each aspect was assessed using a single item, which may be classified as of high quality (scored as 1), low quality or unknown quality (scored as 0). The overall quality of each study was evaluated, and studies were divided into 3 categories: low level of quality (0-3), moderate level of quality (4-6), and high level of quality (7-9). The meta-analysis included only moderate- to high-quality studies. Two authors independently read and evaluated the included papers (TQD and NTTH).
Table 1.
JBI Critical appraisal checklist for studies reporting prevalence data.
| No. | Author | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | GATS 12 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| 2 | GATS 13 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| 3 | Ngo 14 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
| 4 | Rang 15 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 7 |
| 5 | Suzuki 16 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 6 | Dien 18 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 7 |
| 7 | Dang 17 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
Criteria for the critical appraisal of evidence:
Q1: Was the sample frame appropriate to address the target population?
Q2: Were study participants sampled in an appropriate way?
Q3: Was the sample size adequate?
Q4: Were the study subjects and the setting described in detail?
Q5: Was the data analysis conducted with sufficient coverage of the identified sample?
Q6: Were valid methods used for the identification of the condition?
Q7: Was the condition measured in a standard, reliable way for all participants?
Q8: Was there appropriate statistical analysis?
Q9: Was the response rate adequate, and if not, was the low response rate managed appropriately?
For system meta analysis on prevalence, there are several methods for evaluating the risk of bias or critical appraisal stage. 9 An internal working group of the Joanna Briggs Institute created JBI critical appraisal tool in 2014 which has been shown to be proven well-accepted by users and further refinements have been made to the tool based on their feedback. 10 Until 2020, the JBI critical appraisal is suggested based on the findings of systematic reviews of prevalence data, which have demonstrated that the tool has been officially assessed and is being increasingly utilized in these kinds of studies. 9
Statistical analysis
To analyze data, MedCalc Software (64-bits Windows) was used. The I2 statistic was used to determine the heterogeneity of estimates across studies, which quantifies the proportion of heterogeneity that is not due to sampling error. A score of I2 more than 75% implies a significant degree of heterogeneity. 11 Because anticipated a significant high degree of heterogeneity across studies, we decided to present the pooled and weighted estimate obtained from random effects models.
We conducted sensitivity analyses by omitting subgroups from the Meta-analyses and comparing the point estimates before and after eliminating groups of particular study. This allowed us to assess the impact of subgroups such as national survey and studies including all pregnancy participant.
Results
Literature search
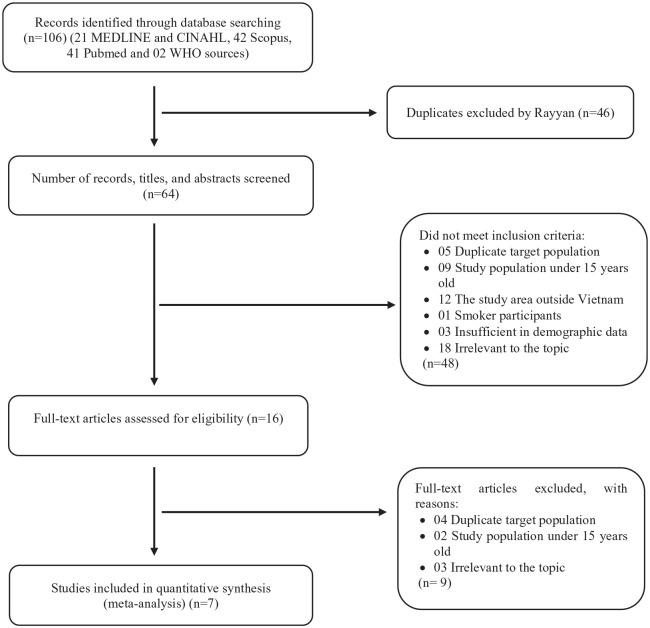
The process of study selection is shown in Figure 1. Our search yielded 21 studies from MEDLINE and CINAHL, 42 from Scopus, 41 from Pubmed databases and 2 WHO sources. Sixty-four studies remained after duplicates were removed. We reviewed the titles and abstracts of these studies and eliminated 48 records due to research categories that were inappropriate study types, according to our criteria. The remaining 16 full-text publications were evaluated for eligibility and only 7 of these met the eligible research were satisfactory.12-18
Figure 1.
Summary of the studies selection process.
Table 2 summarizes the characteristics and results of 7 articles included in this meta-analysis. Of the 7 studies, 2 surveys were conducted at the national level (Global Adult Tobacco Surveys (GATS)) and the remaining studies were conducted at the provincial level (3 Cross-sectional studies and 2 Case-control studies).
Table 2.
Description of the studies included in the meta-analysis.
| No. | Authors | Geographical location | Participant | Sample size | Research Method | Definition | Collection method | Gender | Mean age | Urban/Rural | Passive smoking percentage | Exposure Place/Source | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Urban | Rural | |||||||||||
| 1 | GATS 12 | All 63 provinces of Vietnam | ⩾15 year old | 6972 | Nationally representative survey | Exposure to SHS during previous 30 days in workplace | A two-stage random systematic sampling | 3326 (47.7%) | 2085 (29.9%) | Data was shown by category. Mean age not described. | 34.7% | 38.7% | 36.80% | At workplace |
| 2 | GATS 13 | All 63 provinces of Vietnam | ⩾15 year old | 7563 | Nationally representative survey | SHS at work is defined as the percentage of indoor workers age 15 and over who had been exposed to tobacco smoke at work in the past 30 days. | A two-stage random systematic sampling | 4750 (62.8%) | 3123 (41.3%) | Data was shown by category. Mean age not described. | 45.1% | 52.6% | 49% | At workplace |
| 3 | Chau Quy Ngo 14 | Obstetrics Department of Bach Mai Hospital, Hanoi, Vietnam | Pregnant women | 432 | Cross-sectional study | Whether they were exposed to SHS in the last 30 days | Convenience sampling | 0 | 432 (100%) | Not described. | 372 (86.1%) | 60 (13.9%) | 64.50% | Cafeterias and restaurants, workplace, home, and state authority offices |
| 4 | Nguyen N. Rang 15 | The Women’s and Children’s Hospital of An Giang, Vietnam | Pregnant women | 576 | Case-control study | Pregnant women who did not smoke but were exposed to husband or family members who smoked on a daily basis of more than 5 cigarettes a day at home. | Not described | 0 | 576 (100%) | Not described. | 419 (72.7%) | 157 (27.3%) | 341 (59.2%) | At home |
| 5 | Motoi Suzuki 16 | Khanh Hoa Province, central Vietnam | >20 year old | 167298 | Cross-sectional study | SHS exposure at home was defined as living with one or more indoor smokers. | Not described | 101 382 (60.6%) | 65 916 (51.7%) | Data was shown by category. Mean age not described. | Not described | Not described | 83763 (50.1%) | At home |
| 6 | Vu H. A. Dien 18 | National Hospital of Odonto-Stomatology in HCM City and Tu Du Hospital in HCM City | Pregnant women | 340 | Case-control study | Duration of passive cigarette smoking exposure was categorized using a cutoff of 15 min per day | Convenience sampling | 0 | 340 (100%) | Not described. | Not described | Not described | 86 (25.3%) | None |
| 7 | Anh Kim Dang 17 | Hanoi | Customer | 1740 | Cross-sectional study | “Being exposed to tobacco smoke in restaurants” was used to define customers who passively smoked in restaurants in the last 30 days. | A 2-stage random systematic sampling | 663 (38.1%) | 1077 (61.9%) | 34.6 ± 12.9 | Not described | Not described | 90.90% | Restaurants |
The overall sample volume of research was 184 921 individuals over the age of 15 years and the sample sizes were significantly different, ranging from 340 to 167 298 individuals. SHS was defined and age group of subjects was determined in all studies, except only one of the studies 16 (in most cases, it was more than 15 years of age, except for 1 case 16 in which age was higher than 19 years due to this article combine 10 to 19-year-old into a subgroup and this group age was eliminated since non-conformance with our selection criteria). The study region also varied, with 6 research investigating both urban and rural areas,12-15,17,18 while the other 1 study did not offer this figure. 16 Three surveys utilized a stratified multistage random sampling method to recruit participants and gather demographic data,12,13,17 while 2 used convenience sampling,14,18 2 did not specify particular sampling techniques.15,16 Three researches shown both males and females in their analyses,12,13,17100% of participants were pregnant female at hospitals among 3 researches14,15,18, 1 study has not yet provided a sex ratios among non-smokers. 16
The total prevalence of SHS in the studies included in this meta-analysis ranged from 25,3 percent in a research by Dien et al 17 (No incidence data are available for the exposure place) 18 to 90.9% in a study by Anh Kim Dang (at restaurants).
Quality assessment
The quality ratings of the systematic reviews included in this study were predominantly high, with no systematic studies being assessed as low or intermediate in quality, and as a result, none were omitted from consideration for quality concerns. Scores ranged from 7 to 9 on a scale of 9, with 9 being the highest attainable score. All systematic reviews have a properly and precisely stated definition of SHS in their methodology. Table 1 contains evaluations of methodological quality, as well as the outcomes of those evaluations.
SHS prevalence
Seven studies reported on the point prevalence of SHS and all of those were eligible for inclusion in the meta-analysis. It was discovered that the observed outcome was an estimated prevalence of SHS, which depicted the fractional frequency of SHS in each study plot. A total of 184,921 non-smokers had been exposed to passive smoke. The overall random-effects pooled prevalence of SHS was 54.6% (95% CIs: 44.900-64.154) with a high level of heterogeneity (due to the presence of heterogeneity between studies P = .0001, Q = 2245.60, I2 = 99.73%) (Table 3). Additionally, the pooled prevalence of passive smoking varied considerably throughout the survey years, with national surveys decreasing from 2010 to 2015 and but provincial and hospital surveys increasing significantly in recent years. The highest prevalence of passive smoking among Vietnamese population was in 2018 (90.9% [95% CI 89.5%-92.3%]) and lowest in 2019 (25.3 % [95% CI 20.8%-30.3%]).
Table 3.
Pooled prevalence of SHS prevalence. Test for heterogeneity.
| Study | Sample size | Proportion (%) | 95% CI | Weight (%) | |
|---|---|---|---|---|---|
| GATS 12 | 6972 | 36.804 | 35.671-37.949 | 14.49 |
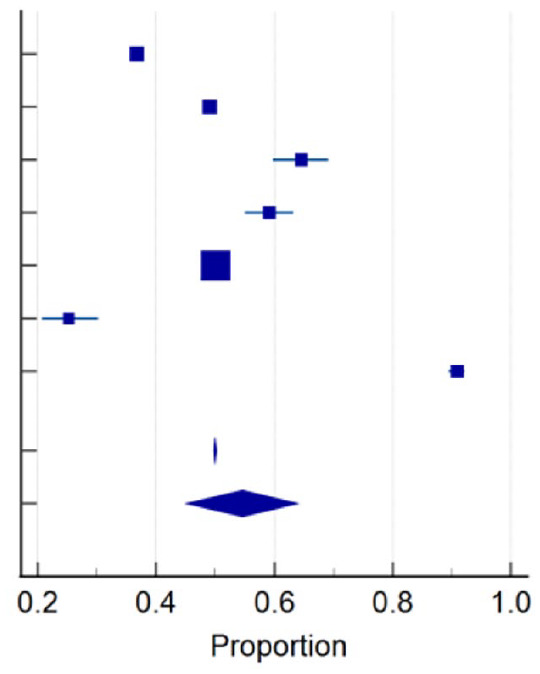
|
| GATS 13 | 7563 | 49.002 | 47.869-50.135 | 14.49 | |
| Chau Quy Ngo 14 | 432 | 64.583 | 59.870-69.096 | 14.04 | |
| Rang 15 | 576 | 59.201 | 55.062-63.246 | 14.16 | |
| Motoi Suzuki 16 | 167 298 | 50.068 | 49.828-50.308 | 14.52 | |
| Dien 18 | 340 | 25.294 | 20.759-30.265 | 13.92 | |
| Dang 17 | 1740 | 90.920 | 89.471-92.228 | 14.40 | |
| Total (random effects) | 184 921 | 54.614 | 44.900-64.154 | 100.00 |
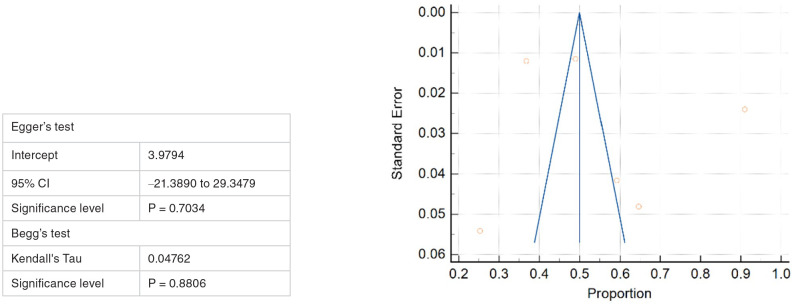
Publication bias
According to the visual examination of funnel plots in Figure 2, showing that there is no publication bias among the papers that were included, as well as the Begg (P = .8806) and Egger tests (P = .7034), there was no indication of publication bias in any of the estimates of prevalence.
Figure 2.
Funnel plot for assessing publication bias in Meta-analysis for SHS prevalence.
Sensitivity analysis
Based on the sensitivity analysis, the removal of subgroups did not significantly alter the findings, with pooled prevalence of SHS ranging from 59.235% (when excluding 2 national survey) and 58.297% (when excluding 3 studies including all pregnancy participant).
Discussion
The widespread scientific consensus is that exposure to secondhand smoke is detrimental to health, a significant public health concern, and the impetus for enacting smoke-free legislation. Nonetheless, the absence of a comprehensive meta-analysis of its frequency among nonsmokers is intriguing. The purpose of this research was to estimate the total prevalence of SHS among Vietnamese non-smokers aged 15 year old and over by examining previously published data and to the best of our knowledge, this is the first meta-analysis reporting the estimates of SHS in Vietnam. The findings of this study confirmed that a substantial upward tendency in terms of SHS exposure in resident publications over time.
This research comprised a total of 184 921 participants from among 07 eligible papers after a thorough screening process. All data was collected between 2010 and 2019. According to this meta-analysis, the pooled overall prevalence of SHS using the random effect model was 54.6% (95% CIs: 44.9-64.154) and a variation in the location of passive smoking exposure between urban and rural populations and stayed consistently high throughout the course of the research process. Our estimate of the prevalence of SHS in Vietnam appears to be greater than those published in China. 19 This data likely reflects the partial ineffective of anti-tobacco measures in protecting people who do not smoke from SHS harm. Several factors exist for this case. First, Vietnam has developed and effectively implemented a variety of smoke-free environment models, but recent study done in Vietnam indicates that there is a low perceived degree of compliance with smoke-free legislation by customers in restaurants 17 and inadequate degree of knowledge of SHS. 20 Second, the Tobacco Harm Prevention Law was promulgated in 2012 is only a partial ban, rather than a comprehensive ban as suggested by WHO Framework Convention on Tobacco Control. Conversely, evidence from Europe indicates that comprehensive smoking bans have a greater impact on policy support than partial smoking bans. 21 Third, the prohibition on smoking in public areas seems to have been less successful than anticipated due to “not strict enough” punishments from authorities. Despite the fact that smoking prohibition signs are placed across public spaces, smokers continue to disregard them in certain locations, and issuing a warning is insufficiently strict. 22 Finally, Vietnam is ranked among the countries with the highest smoking prevalence worldwide, there are still a scarcity of smoking cessation programs, despite the fact that Vietnam has ratified the WHO Framework Convention on Tobacco Control since 2004. 23
These are elements to consider from a policy perspective; however, there are relative strength factors to consider from the perspective of smokers as individuals, which have been demonstrated in several studies to contribute to the persistence of a high prevalence of SHS exposure among the Vietnamese population. First, the physical dependence on tobacco was shown to be common among Vietnamese adult males, despite the fact that the tobacco user had a strong desire to stop smoking. 24 And second, several studies have shown evidence of genetic impacts on nicotine dependency, for example, It is genetically predicated that Vietnamese male smokers with less MAOA expression would have greater nicotine dependency 25 and HTTLPR and STin2 VNTRs interact genetically to regulate nicotine dependence, with STin2 effects predominating. 26 It has potential benefits that an crucial step in transferring these genetic discoveries into clinical practice is discovering the genetic characteristics that influence smoking cessation in order to improve the effectiveness of existing smoking cessation therapies.
Since the knowledge gap is whether Vietnam has stringent regulations to protect the public from exposure to SHS or not. And there is no evidence of public health harm caused by the partial ban in the protection of non-smokers from SHS in Vietnam. Consequently, the higher prevalence of SHS among Vietnamese implies that further study is urgently needed to determine the efficacy of existing policies on reducing SHS exposure, such as smoking prohibitions in indoor and outdoor areas, and the health effects of SHS on individuals, particularly vulnerable groups. Together they have significant implications for our knowledge of the consequences of SHS exposure and the principles that guide our approach to policies to mitigate this exposure.
There are several limitations of this research that should be acknowledged that might influence our conclusions. First, the degree of heterogeneity across studies was substantial. Thus, even though we employed a random effects model to account for heterogeneity, our aggregate results should be taken cautiously. Second, the existence of heterogeneity posed a constraint since the sources of this heterogeneity could not be identified; its causes include the variations in participant characteristics and standardization of SHS measuring methods, including filling out questionnaires according to their perspectives, and the questions are asked differents on the frequency of exposure to SHS per day/month, the location of exposure, and the length of time spent exposed to SHS. The adoption of a consistent framework for study design, methodology, and variable definition in all similar studies in the future is strongly encouraged.
For a more accurate representation of our findings, we only included high-quality research, and there was no indication of publication bias, additional corroboration of our findings. Despite the limitations, this research has found evidence of significant public health importance and provides strong evidence in favor of immediate attention to the critical levels of SHS among Vietnamese and we should thus implement more public-health initiatives to better combat this trend.
Conclusions
This systematic review and meta-analysis revealed that SHS levels have been rising over time, and in recent years have become worse in Vietnam. This demonstrates the critical need of a more concentrated effort by the government to robust and enhance Vietnam’s tobacco control policies in order to provide a smoke-free and favorable environment for smokers to quit.
Supplemental Material
Supplemental material, sj-xlsx-1-sat-10.1177_11782218221086653 for Second-Hand Smoking Prevalence in Vietnamese Population Aged 15 and older: A Systematic Review and Meta-Analysis by Tran Quang Duc, Le Thi Kim Anh, Vu Thi Quynh Chi, Nguyen Thi Thanh Huong and Phan Ngoc Quang in Substance Abuse: Research and Treatment
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors’ Contributions: The initiative was launched thanks to TQD’s idea and action. The development of the search technique was coordinated by TQD, VTQC, PNQ and NTTH. The initial draft was finished by TQD and LTKA. All authors provided critical feedback on and then approved the final draft.
Availability of Data and Materials: All data regarding this research work is included in the manuscript.
Ethical Approval: This paper did not go through an ethical review since this was a literature review of already published studies, and no new data was acquired.
Informed Consent: Informed consent was not obtained since it was a literature review of already published data, and no new data was acquired.
ORCID iDs: Tran Quang Duc  https://orcid.org/0000-0002-7875-1985
https://orcid.org/0000-0002-7875-1985
Le Thi Kim Anh  https://orcid.org/0000-0003-4250-7507
https://orcid.org/0000-0003-4250-7507
Phan Ngoc Quang  https://orcid.org/0000-0003-1223-0914
https://orcid.org/0000-0003-1223-0914
Supplemental Material: Supplemental material for this article is available online.
References
- 1. World Health Organization. Tobacco [Internet]. 2020. Accessed July 9, 2021. https://www.who.int/news-room/fact-sheets/detail/tobacco
- 2. National Cancer Institute. Secondhand Smoke Exposure [Internet]. 2021. Accessed July 9, 2021. https://cancercontrol.cancer.gov/brp/tcrb/secondhand-smoke-exposure
- 3. World Health Organization. Noncommunicable diseases [Internet]. 2021. Accessed July 10, 2021. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- 4. World Health Organization. Smoking causes 40 000 deaths in Viet Nam each year. 2018. [Google Scholar]
- 5. Hoang VM, Tran TN, Vu QM, et al. Tobacco Control Policies in Vietnam: review on MPOWER Implementation Progress and Challenges. Asian Pac J Cancer Prev. 2016;17:1-9. [DOI] [PubMed] [Google Scholar]
- 6. National Assembly of Viet Nam. Law on Prevention and Control of Tobacco Harms. Government of Viet Nam; 2012. [Google Scholar]
- 7. Lam NT, Nga PTQ, Kashiwabara M, et al. Secondhand tobacco smoke exposure in indoor workplaces in Viet nam and associated factors: findings from two rounds of Global Adult Tobacco Surveys (GATS) 2010 and 2015. Asian Pac J Cancer Prev. 2020;21:33-38. [DOI] [PubMed] [Google Scholar]
- 8. Tran LK, Morawska L, Gartner CE, Huong LTT, Le HHTC, Thai PK. Secondhand smoke in public places in Vietnam: an assessment 5 years after implementation of the tobacco control law. Tob Control. 2021; 30:553-559. http://tobaccocontrol.bmj.com/content/early/2020/08/29/tobaccocontrol-2020-055753.abstract [DOI] [PubMed] [Google Scholar]
- 9. Borges Migliavaca C, Stein C, Colpani V, Barker TH, Munn Z, Falavigna M. How are systematic reviews of prevalence conducted? a methodological study. BMC Med Res Methodol [Internet]. 2020;20:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Heal policy Manag.2014;3:123–8. https://pubmed.ncbi.nlm.nih.gov/25197676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. https://pubmed.ncbi.nlm.nih.gov/12958120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vietnam Ministry of Health, Hanoi Medical University. General Office Statistics, World Health Organization. Global Adult Tobacco Survey (GATS) Vietnam 2015 [Internet]. 2015. Accessed July 11, 2021. https://www.who.int/tobacco/surveillance/survey/gats/vietnam-country-report-2015.pdf
- 13. Ministry of Health Vietnam, Medical University Hanoi. General Office Statistics, World Health Organization. Global Adult Tobacco Survey (GATS) Viet Nam 2010 [Internet]. 2010. Accessed July 9, 2021. https://www.who.int/tobacco/surveillance/en_tfi_gats_vietnam_report.pdf
- 14. Ngo CQ, Phan PT, Vu GV, et al. Prevalence and sources of second-hand smoking exposure among Non-Smoking pregnant women in an urban setting of Vietnam. Int J Environ Res Public Health. 2019;16:5022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rang NN, Hien TQ, Chanh TQ, Thuyen TK. Preterm birth and secondhand smoking during pregnancy: A case-control study from Vietnam. PLoS One. 2020;15:e0240289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Suzuki M, Thiem VD, Yoshida LM, Anh DD, Kilgore PE, Ariyoshi K. Who is exposed to smoke at home? A population-based cross-sectional survey in central Vietnam. Tob Control 2010;344–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dang A, Tran B, Nguyen L, et al. Customers’ perceptions of compliance with a tobacco control law in restaurants in Hanoi, Vietnam: A cross-sectional study. Int J Environ Res Public Health. 2018;15:1451. https://www.scopus.com/inward/record.uri?eid=2-s2.0-85050030074&doi=10.3390%2Fijerph15071451&partnerID=40&md5=54c4d456ca3ae427c5fe0060f85d48d5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dien VHA, McKinney CM, Pisek A, Pitiphat W. Maternal exposures and risk of oral clefts in South Vietnam. Birth Defects Res. 2018;110:527-537. http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=29322637&site=ehost-live [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zeng J, Yang S, Wu L, et al. Prevalence of passive smoking in the community population aged 15 years and older in China: a systematic review and meta-analysis. BMJ Open. 2016;6:e009847-e009847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Vu GV, Ngo CQ, Phan PT, et al. Inadequate knowledge, attitude and practices about second-hand smoke among Non-Smoking pregnant women in Urban Vietnam: the Need for Health Literacy Reinforcement. Int J Environ Res Public Health. 2020;17. 10.3390/ijerph17103744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mons U, Nagelhout GE, Guignard R, et al. Comprehensive smoke-free policies attract more support from smokers in Europe than partial policies. Eur J Public Health. 2012;22:10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nguyen VH, Do DA, Do TTH, et al. Smoke-free environment policy in Vietnam: what did people see and how did they react when they visited various public places? J Prev Med Hyg. 2019;60:E36-E42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jiang N, Siman N, Cleland CM, et al. Effectiveness of village health worker–delivered smoking cessation counseling in Vietnam. Nicotine Tob Res. 2019;21:1524-1530. https://pubmed.ncbi.nlm.nih.gov/30335180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kõks G, Tran HDT, Ngo NBT, et al. Cross-sectional study to characterise nicotine dependence in central Vietnamese men. Subst Abuse Res Treat. 2019;13:1178221818822979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kõks G, Prans E, Ho XD, et al. Genetic interaction between two VNTRs in the MAOA gene is associated with the nicotine dependence. Exp Biol Med. 2020;245:733-739. https://pubmed.ncbi.nlm.nih.gov/32241179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kõks G, Prans E, Tran HDT, et al. Genetic interaction between two VNTRs in the SLC6A4 gene regulates nicotine dependence in Vietnamese men. Front Pharmacol. 2018;9:1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-xlsx-1-sat-10.1177_11782218221086653 for Second-Hand Smoking Prevalence in Vietnamese Population Aged 15 and older: A Systematic Review and Meta-Analysis by Tran Quang Duc, Le Thi Kim Anh, Vu Thi Quynh Chi, Nguyen Thi Thanh Huong and Phan Ngoc Quang in Substance Abuse: Research and Treatment