Abstract
Background
We previously reported high in-hospital mortality for ST-segment elevation myocardial infarction (STEMI) patients with COVID-19 treated in the early phase of the pandemic.
Objectives
The purpose of this study was to describe trends of COVID-19 patients with STEMI during the course of the pandemic.
Methods
The NACMI (North American COVID-19 STEMI) registry is a prospective, investigator-initiated, multicenter, observational registry of hospitalized STEMI patients with confirmed or suspected COVID-19 infection in North America. We compared trends in clinical characteristics, management, and outcomes of patients treated in the first year of the pandemic (January 2020 to December 2020) vs those treated in the second year (January 2021 to December 2021).
Results
A total of 586 COVID-19–positive patients with STEMI were included in the present analysis; 227 treated in Y2020 and 359 treated in Y2021. Patients’ characteristics changed over time. Relative to Y2020, the proportion of Caucasian patients was higher (58% vs 39%; P < 0.001), patients presented more frequently with typical ischemic symptoms (59% vs 51%; P = 0.04), and patients were less likely to have shock pre-PCI (13% vs 18%; P = 0.07) or pulmonary manifestations (33% vs. 47%; P = 0.001) in Y2021. In-hospital mortality decreased from 33% (Y2020) to 23% (Y2021) (P = 0.008). In Y2021, none of the 22 vaccinated patients expired in hospital, whereas in-hospital death was recorded in 37 (22%) unvaccinated patients (P = 0.009).
Conclusions
Significant changes have occurred in the clinical characteristics and outcomes of STEMI patients with COVID-19 infection during the course of the pandemic.
Key Words: COVID-19, heart attack, outcomes, STEMI
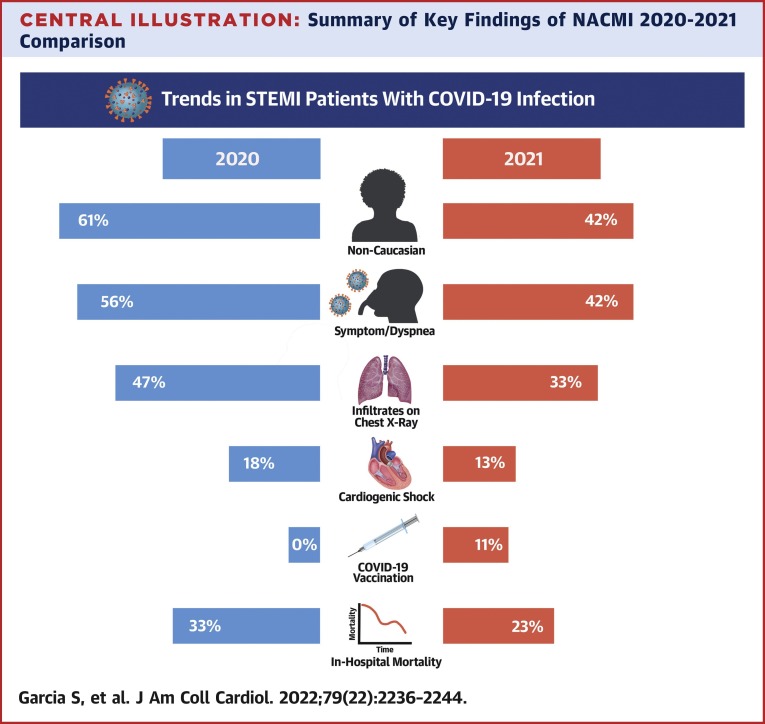
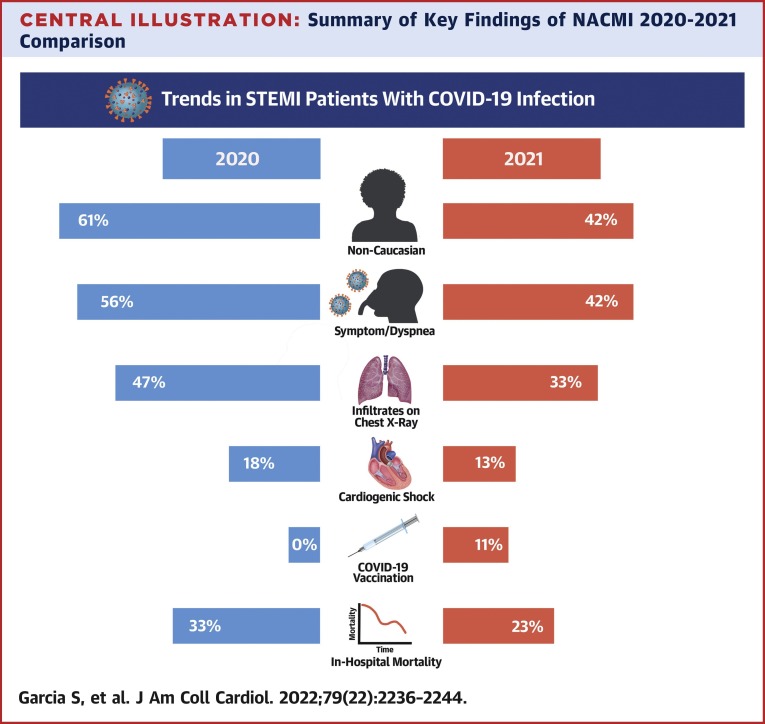
Central Illustration
The COVID-19 infection significantly increases the risk for both arterial and venous thromboembolic complications.1 The risk of myocardial infarction (MI) doubles within a week of receiving a COVID-19 diagnosis and is associated with higher odds of mortality.2 , 3 Patients presenting with ST-segment elevation myocardial infarction (STEMI) and COVID-19 constitute a high-risk subset with distinct clinical features, including preponderance of minority ethnicity, in-hospital presentation, cardiogenic shock, and very high in-hospital mortality.4, 5, 6, 7
Despite an increased number of COVID-19 cases worldwide, significant progress has been made in both disease prevention and management during the course of the pandemic, which has contributed to a marked reduction in mortality in selected countries.8, 9, 10 We previously reported very high (33%) in-hospital mortality for patients with STEMI and COVID-19 treated in North America during the early phase of the pandemic.4
The aim of this investigation is to examine trends in clinical characteristics, treatments, and outcomes of STEMI patients with COVID-19 infection using data from the NACMI (North American COVID-19 Myocardial Infarction) registry.
Methods
Study design
NACMI is a prospective, investigator-initiated, multicenter, observational registry of hospitalized STEMI patients with confirmed or suspected COVID-19 infection in North America. A detailed description of the study design has been previously published.4 , 11 A total of 64 sites were approved by the local ethics committees (12 Canadian and 52 U.S. sites).
Inclusion criteria
NACMI included 3 groups of STEMI patients (COVID-19–positive group, contemporary COVID-19–negative group, and a historical control group). The present analysis on trends focused on the COVID-19–positive and contemporary COVID-19–negative group. The COVID-19–positive group comprised adult patients (age ≥18 years) with: 1) ST-segment elevation in at least 2 contiguous leads (or new-onset left bundle branch block); 2) a clinical correlate of myocardial ischemia (eg, chest pain, dyspnea, cardiac arrest, shock, mechanical ventilation); and 3) confirmed COVID-19–positive by any commercially available test during, or 4 weeks before, the index STEMI hospitalization.
The COVID-19–negative group comprised adult patients with STEMI who were suspected positive on presentation but subsequently tested negative for COVID-19 infection (person under investigation [PUI]). The definition of PUI was left to the discretion of local hospitals but in general included a combination of possible COVID-19 signs and symptoms (fever or respiratory symptoms such as cough, shortness of breath, sore throat), or exposure to a confirmed case or cluster of suspected COVID-19 cases. With advancements in rapid COVID-19 testing and streamlined STEMI protocols, we anticipated the designation of PUI would be less relevant in Y2021 but presented this information to serve as a reference group to compare trends.
NACMI was designed in early 2020 before the commercialization of vaccines against COVID-19.12 , 13 Therefore, vaccine status was not routinely captured in the registry. However, once vaccines became commercially available in North America in 2021, the original protocol was amended to include immunization status including timing and type. The protocol amendment was approved by 20 enrolling sites at the time of this publication.
Primary endpoint
The primary endpoint for this analysis was in-hospital mortality. A composite of in-hospital death, stroke, or reinfarction was a secondary endpoint. Nonfatal events were defined using National Cardiovascular Data Registry (NCDR Cath PCI Registry version 4.4) definitions.
Data collection
We used standardized data collection forms, modeled after the American College of Cardiology National Cardiovascular Data Registry definitions, and a secure web-based application (REDCap, Research Electronic Data Capture) for data capture. The data coordinating center at the Minneapolis Heart Institute Foundation had full access to the dataset and performed the statistical analysis. The protocol was approved by each local Institutional Review Board. Informed consent was waived.
Statistical analysis
Discrete variables are summarized by counts (%), and continuous variables are summarized by mean ± SD if distributed symmetrically, or as median (25th percentile, 75th percentile) if skewed.
COVID-19–positive patients were divided into 2 groups according to the year of the STEMI presentation during the pandemic, ie, Y2020 group from March 1, 2020, to December 31, 2020; and Y2021 group from January 1, 2021, to December 31, 2021. These periods coincided with the commercial introduction of vaccines against COVID-19 in North America. Demographic, clinical, and outcome variables were compared between the groups using Pearson’s chi-square or Fisher exact test for categorical data and Student’s t-test or Wilcoxon rank sum test for continuous variables, as appropriate.
Given a relatively short hospital length of stay, in-hospital mortality is modeled as a binary variable, and the relative risk of death for Y2021 vs Y2020 group is estimated from a multivariate robust Poisson regression with a canonical log-link and robust sandwich estimator of variance to allow for overdispersion in the data. Model covariates include age, BMI, gender, race, diabetes, abnormal chest x-ray findings, and shock pre-percutaneous coronary intervention (PCI). More specifically, age originally collected as a 5-category variable is dichotomized as <66 or ≥66 years; and BMI categories are defined overweight/obese or not per Centers for Disease Control and Prevention definition. Furthermore, a proxy comorbidity index is defined to capture the pre-existing cardiovascular diseases/conditions as follows: a sum of indicators of hypertension and history of PCI, MI, coronary artery bypass graft, stroke, or CHF for each patient is dichotomized to index those with ≥3 pre-existing conditions. The choice of the variables and categories in the model is informed by existing literature, exploratory data analysis, sample size, and the number of adverse events considerations.4 , 14
Model parameters are estimated first from complete data, then using imputed data where missing values are approximated by sample medians that in case of categorical variables correspond to imputation by the most prevalent category. Model estimates are reported with their 95% CIs and P values.
COVID-19 vaccine data are available for 420 (71%) of patients in the study including 193 patients from the Y2021 cohort (54%). Of these 193 patients, only 22 (11%) were vaccinated against COVID-19 and 171 were unvaccinated. These data are described by summaries only, as in the previous text, because null number of adverse events did not allow for multivariate modeling.
Data were analyzed using R version 4.1.2 (R Foundation for Statistical Computing) in RStudio environment version 2021.09.1 (RStudio, PBC).
Results
A total of 586 COVID-19–positive patients with STEMI were included in the present analysis; 227 treated in Y2020 (United States: 93%; Canada: 7%) and 359 treated in Y2021 (United States: 91%; Canada: 9%). The baseline characteristics and clinical features at presentation are presented in Table 1 . Significant changes in patients’ characteristics occurred over time. Relative to patients treated in 2020, patients treated in 2021 were more likely to be Caucasian (58% vs 39%; P < 0.001), more likely to present with chest pain (59% vs 51%; P = 0.04) rather than dyspnea (42% vs 56%; P = 0.002), and less likely to have shock pre-PCI (13% vs 18%; P = 0.07) or infiltrates on chest x-ray (33% vs 47%; P = 0.001).
Table 1.
Trends in Baseline Characteristics and Clinical Features at Presentation
| Y2020 (n = 227) | Y2021 (n = 359) | P Valuea | |
|---|---|---|---|
| Age <66 y | 126 (56.0) | 201 (56.0) | 0.9 |
| Male | 163 (72.0) | 268 (75.0) | 0.4 |
| History of CAD | 51 (24.0) | 88 (28.0) | 0.3 |
| Non-Caucasian | 137 (61.0) | 142 (42.0) | <0.001 |
| Dyslipidemia | 98 (45.0) | 145 (46.0) | 0.9 |
| Diabetes mellitus | 102 (46.0) | 135 (42.0) | 0.4 |
| BMI, kg/m2 | 29 ± 8 | 27 ± 10 | 0.5 |
| Overweight/obese | 156 (72.0) | 253 (77.0) | 0.2 |
| Hypertension | 165 (74.0) | 223 (65.0) | 0.025 |
| History of heart failure | 33 (16.0) | 51 (16.0) | 0.9 |
| Aspirin on admission | 88 (39.0) | 127 (35.0) | 0.4 |
| Statin on admission | 88 (39.0) | 123 (34.0) | 0.3 |
| CVRF ≥3 | 43 (19.0) | 77 (21.0) | 0.5 |
| Symptoms at presentation | |||
| Dyspnea | 126 (56.0) | 152 (42.0) | 0.002 |
| Chest pain | 115 (51.0) | 212 (59.0) | 0.046 |
| Syncope | 6 (2.6) | 16 (4.5) | 0.3 |
| Infiltrates | 106 (47.0) | 120 (33.0) | 0.001 |
| Cardiac arrest pre-PCI | 23 (11.0) | 24 (7.9) | 0.2 |
| Shock pre-PCI | 37 (18.0) | 38 (13.0) | 0.079 |
| Ejection fraction, % | 43 (35, 55) | 45 (34, 55) | 0.5 |
| In-house presentation of MI | 13 (5.7) | 26 (7.4) | 0.4 |
Values are n (%), mean ± SD, or median (25th percentile, 75th percentile).
BMI = body mass index; CAD = coronary artery disease; CVRF = cardiovascular risk factors; MI = myocardial infarction; PCI = percutaneous coronary intervention.
Not adjusted for multiple comparisons.
Invasive angiography, revascularization strategies, and treatment times
The use of invasive angiography increased over time from 77% in 2020 to 86% in 2021 (P = 0.004). Among patients undergoing invasive angiography, revascularization strategies are listed in Table 2 . PCI (both primary and facilitated/rescue PCI) was the predominant revascularization modality used in >70% of cases with no significant differences between Y2020 and Y2021. Thrombolytics and coronary artery bypass graft surgery were infrequently used (<5% and 2%, respectively). Medical therapy alone was used in 19% of patients in Y2020 and 25% in Y2021 (P = 0.7) (primarily for patients with no culprit vessel).
Table 2.
Utilization of Invasive Angiography, Revascularization Strategies, and Antiplatelet Therapies at Discharge
| Y2020 (n = 227) | Y2021 (n = 359) | P Valuea | |
|---|---|---|---|
| No angiogram | 52 (23.0) | 49 (14.0) | 0.004 |
| Patients undergoing invasive angiography, n = 485 | |||
| Reperfusion strategy | 175 | 310 | 0.7 |
| CABG | 3 (1.7) | 5 (1.6) | |
| Facilitated/rescue PCI | 7 (4.0) | 11 (3.5) | |
| Medical therapy | 34 (19.0) | 78 (25.0) | |
| Primary PCI | 125 (71.0) | 206 (66.0) | |
| Thrombolytics | 6 (3.4) | 10 (3.2) | |
| Multivessel CAD | 69 (49.0) | 111 (49.0) | 0.9 |
| Primary PCI (survived to hospital discharge and complete antiplatelet data) | 89 (73.0) | 144 (73.0) | 0.45 |
| Clopidogrel | 31 (34.0) | 39 (27.0) | |
| Prasugrel | 10 (11.0) | 12 (8.0) | |
| Ticagrelor | 48 (53.0) | 93 (64.0) |
Values are n (%) or n.
CABG = coronary artery bypass graft surgery; other abbreviations as in Table 1.
Not adjusted for multiple comparisons.
Among patients undergoing primary PCI, the median door-to-balloon (D2B) time was 78 minutes (IQR: 50-122 minutes) in Y2020 and 70 minutes (IQR: 50-106 minutes) in Y2021 (P = 0.4). The proportion of patients meeting the metric of D2B time <90 minutes was 59% in Y2020 and 64% in Y2021 (P = 0.5).
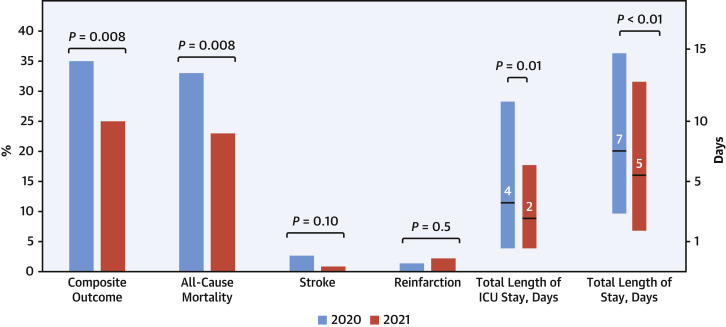
Clinical outcomes and length of stay
A marked reduction in mortality from 33% in Y2020 to 23% in Y2021 (P = 0.008) was observed with a trend for reduction in the incidence of stroke (Y2020 2.6% vs Y2021 0.8%; P = 0.10) but no difference in reinfarction (Y2020 1.3% vs Y2021 2.2%; P = 0.5) rates (Figure 1 ). The composite outcome of death, stroke, or reinfarction occurred in 80 of 227 (35%) patients in Y2020 and 90 of 359 (25%) patients in Y2021 (P = 0.008).
Figure 1.
In-Hospital Events in Patients With STEMI and COVID-19 Infection
Proportion (%) of major adverse cardiovascular events and length of intensive care unit (ICU) and hospital stay in expressed as median and IQR in hospitalized patients with ST-segment elevation myocardial infarction (STEMI) and COVID-19 infection according to year of treatment. The composite outcome includes death, stroke, or recurrent myocardial infarction.
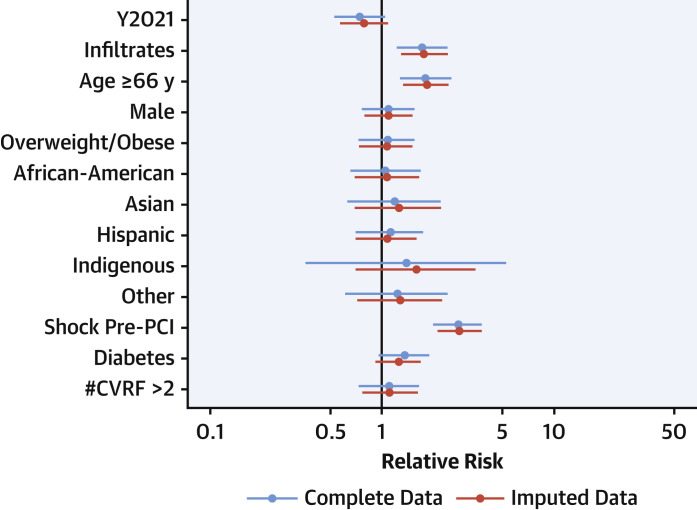
Length of stay decreased from 7 days (IQR: 3-15 days) in Y2020 to 5 days (IQR: 2-12 days) in Y2021 (P = 0.01), and intensive care unit stay decreased from 4 days (IQR: 1-11 days) in Y2020 to 2 days (IQR: 1-6 days) in Y2021 (P < 0.001). From multivariate analysis of complete data, the risk of in-hospital mortality for Y2021 patients was 25% lower (95% CI: −47 to 5; P = 0.01) than for Y2020. The risk of mortality was 1.7 (95% CI: 1.2-2.4; P = 0.002) times higher if infiltrates were observed and nearly 3 times higher (95% CI: 1.9-3.9; P < 0.001) if cardiogenic shock was present (Table 3 , Figure 2 ). Similar estimates were derived from imputed data (Supplemental Table 1).
Table 3.
Estimated Relative Risks of In-Hospital Mortality
| RR | 95% CI Lower Bound |
95% CI Upper Bound |
P Valuea | |
|---|---|---|---|---|
| 2021 | 0.751 | 0.534 | 1.055 | 0.101 |
| Infiltrates on chest x-ray | 1.721 | 1.224 | 2.434 | 0.002 |
| Age ≥66 y | 1.802 | 1.272 | 2.565 | 0.001 |
| Male | 1.089 | 0.757 | 1.589 | 0.652 |
| Overweight/obese | 1.069 | 0.737 | 1.585 | 0.731 |
| African American | 1.060 | 0.635 | 1.716 | 0.817 |
| Asian | 1.176 | 0.555 | 2.229 | 0.645 |
| Hispanic | 1.115 | 0.704 | 1.726 | 0.632 |
| Indigenous | 1.386 | 0.307 | 4.088 | 0.608 |
| Other ethnicity | 1.219 | 0.631 | 2.168 | 0.527 |
| Shock pre-PCI | 2.762 | 1.928 | 3.911 | 0.000 |
| Diabetes | 1.342 | 0.957 | 1.886 | 0.089 |
| CVRF ≥3 | 1.098 | 0.718 | 1.642 | 0.656 |
Baseline categories are: year 2020, no infiltrates on chest x-ray, age <66 years, female sex, BMI category not overweight/obese, Caucasian race, no shock pre-PCI, no diabetes, CVRF <2.
RR = relative risk; other abbreviations as in Table 1.
Not adjusted for multiple comparisons.
Figure 2.
Relative Risk of In-Hospital Death
Estimated relative risk of in-hospital mortality using original (blue) and imputed (red) data. Model covariates include age, body mass index, gender, race, diabetes, abnormal chest x-ray findings, and shock pre-percutaneous coronary intervention (PCI). Baseline categories are: Y2020, no infiltrates on chest x-ray, age <66 y, female gender, not overweight/obese, Caucasian race, no shock pre-PCI, no diabetes, cardiovascular risk factors (CVRF) <2.
Effect of COVID-19 vaccines on STEMI
Vaccine information was captured through a protocol amendment approved by the top 20 enrolling sites. These centers enrolled and provided vaccine data on 193 (54%) of 359 patients treated in Y2021. From these 193 patients hospitalized with STEMI and COVID-19, only 22 (11%) were vaccinated including 9 (45%) with BioNTech and Pfizer, 6 (30%) with Moderna, and 2 (10%) for each Johnson & Johnson and Janssen; in 3 patients, the vaccine type was unknown. The median time from vaccination to STEMI was 20 days (IQR: 6-132 days). The baseline characteristics and clinical features at presentation of vaccinated and unvaccinated patients in Y2021 are presented in Table 4 . Vaccinated patients were less likely to present with respiratory symptoms or infiltrates on chest x-ray. In Y2021, none of the 22 vaccinated patients expired in hospital, whereas in-hospital death was recorded in 37 (22%) of unvaccinated patients.
Table 4.
Baseline Clinical Characteristics and Outcomes of 2021 COVID-19–Positive STEMI Patients According to Vaccination Status
| Unvaccinated (n = 171) | Vaccinated (n = 22) | P Valuea | |
|---|---|---|---|
| Age <66 y | 104 (61.0) | 12 (55.0) | 0.572 |
| Overweight/obese | 128 (78.0) | 16 (89.0) | 0.372 |
| CVRF <3 | 137 (80.0) | 19 (86.0) | 0.579 |
| Dyspnea | 79 (46.0) | 6 (27.0) | 0.092 |
| Chest pain | 107 (63.0) | 15 (68.0) | 0.608 |
| Syncope | 6 (3.5) | 1 (4.5) | 0.577 |
| Infiltrates on chest x-ray | 64 (37.0) | 4 (18.0) | 0.075 |
| Pleural effusion | 11 (6.4) | 2 (9.1) | 0.647 |
| Cardiomegaly | 8 (4.7) | 0 (0.0) | 0.600 |
| Cardiac arrest pre-PCI | 8 (5.4) | 1 (5.0) | 1.0 |
| Shock pre-PCI | 20 (14.0) | 2 (10.0) | 1.0 |
| Ejection fraction, % | 45 (34, 55) | 45 (44, 54) | 0.404 |
| In-house presentation of MI | 19 (11.0) | 0 (0.0) | 0.137 |
| Clinical outcomes | |||
| Mortality | 37 (22.0) | 0 (0.0) | 0.009 |
| Stroke | 1 (0.6) | 0 (0.0) | 1.0 |
| Reinfarction | 3 (1.8) | 1 (4.5) | 0.386 |
| Composite endpoint | 38 (22.0) | 1 (4.5) | 0.052 |
Values are n (%) or median (25th percentile, 75th percentile).
CVD = cardiovascular disease; STEMI = ST-segment elevation myocardial infarction; other abbreviations as in Table 1.
Not adjusted for multiple comparisons.
COVID-19–negative patients
Trends in clinical characteristics and outcomes for patients who were suspected of having COVID-19 but subsequently tested negative (PUI) are presented in Table 5 . Unlike COVID-19–positive patients, we observed no differences in the baseline characteristics or in-hospital outcomes for COVID-19–negative patients (mortality Y2020 11% vs Y2021 9.5%; P = 0.231).
Table 5.
Trends in Baseline Characteristics and Outcomes for COVID-19–Negative Patients (Person Under Investigation)
| Y2020 (n = 495) | Y2021 (n = 298) | P Valuea | |
|---|---|---|---|
| Age ≥66 y | 200 (40.0) | 137 (46.0) | 0.124 |
| History of CAD | 127 (26.0) | 80 (30.0) | 0.275 |
| Non-Caucasians | 112 (24.0) | 83 (29.0) | 0.133 |
| Dyslipidemia | 277 (59.0) | 160 (59.0) | 0.976 |
| Diabetes mellitus | 151 (32.0) | 94 (33.0) | 0.675 |
| BMI, kg/m2 | 29 (25, 33) | 28 (25, 32) | 0.480 |
| Hypertension | 165 (74.0) | 223 (65.0) | 0.025 |
| History of heart failure | 45 (9.4) | 34 (13.0) | 0.118 |
| Aspirin on admission | 136 (27.0) | 95 (32.0) | 0.186 |
| Statin on admission | 172 (35.0) | 93 (31.0) | 0.306 |
| Clinical outcomes | |||
| Primary endpoint | 62 (14.0) | 29 (11.0) | 0.231 |
| Mortality | 54 (11.0) | 28 (9.5) | 0.501 |
| Stroke | 7 (1.6) | 2 (0.8) | 0.497 |
| Reinfarction | 5 (1.1) | 2 (0.8) | >0.099 |
Values are n (%) or median (25th percentile, 75th percentile).
Abbreviations as in Table 1.
Not adjusted for multiple comparisons.
Discussion
We conducted an analysis of trends in clinical characteristics, management strategies, and outcomes of STEMI patients with COVID-19 infection using the NACMI registry, which represents the largest prospective dataset worldwide. There are several important findings (Central Illustration ). First, in-hospital mortality decreased 25% (10 absolute points) in Y2021 compared with Y2020. Second, possible mediators of this reduction in mortality have been identified and include a lower risk profile of patients presenting with more typical ischemic symptoms, less cardiogenic shock, and pulmonary involvement. Third, a subgroup analysis of patients treated in Y2021 according to vaccination status revealed that vaccinated patients are significantly less likely to develop respiratory complications and none of them expired in the hospital, whereas in-hospital death was recorded in 22% of unvaccinated patients in Y2021. Finally, despite the logistical challenges imposed by the pandemic, PCI remains the dominant revascularization modality in North America with more than 70% of patients treated and 2 of 3 meeting the D2B time ≤90 minutes metric. In fact, we observed increased utilization of invasive angiography for risk stratification and management in Y2021 compared with Y2020. Taken together, our observations suggest that the clinical profile, management, and outcomes of STEMI patients with COVID-19 infection is evolving toward that of STEMI patients before the pandemic, although mortality remains high for unvaccinated patients.
Central Illustration.
Summary of Key Findings of NACMI 2020-2021 Comparison
Relative to Y2020, the proportion of Caucasian patients was higher, patients presented more frequently with typical ischemic symptoms, and were less likely to have shock pre-PCI or pulmonary manifestations of COVID-19 infection. In-hospital mortality decreased from 33% to 23%. Original created with BioRender.com. NACMI = North American COVID-19 STEMI Registry; PCI = percutaneous coronary intervention.
Our group and others have previously reported that patients with STEMI and COVID-19 infection have very high in-hospital mortality.3, 4, 5, 6, 7 Independent predictors of mortality in STEMI patients with COVID-19 infection are different than those without COVID-19.14 Risk models have identified respiratory variables such as tachypnea, hypoxemia, use of mechanical ventilation, and infiltrates on chest x-ray as significant predictors of mortality in patients with COVID-19 infection.15 In fact, respiratory variables accounted for ≥50% of the NACMI risk score.15 The introduction of vaccines has significantly reduced hospitalizations and mortality caused by COVID-19 infection.12 , 13 , 16, 17, 18 Our subgroup analysis according to vaccination status of STEMI patients treated in Y2021 suggests that prevention of severe respiratory illness is a likely mediator and provides additional support to current Centers for Disease Control and Prevention recommendations to vaccinate adults.19 In addition to lung infiltrates, age ≥66 years and cardiogenic shock pre-PCI are also associated with in-hospital mortality.
During the first wave of the pandemic, we reported a preponderance of minority ethnicity in patients with STEMI and COVID-19 infection. Crowded living conditions, frontline employment, health disparities, and higher prevalence of comorbidities may explain these findings.20 The present analysis demonstrates that, as the pandemic evolved, Caucasians became the predominant ethnic group in NACMI, which is consistent with prepandemic STEMI registries from North America.21, 22, 23
The NACMI registry was designed as a collaboration of 3 North American societies (Society for Cardiac Angiography and Interventions, Canadian Association of Interventional Cardiologists, and the American College of Cardiology Interventional Council) in response to an unprecedented reduction in cardiac catheterization laboratory activations and calls to deviate from the standard of care during the pandemic.24, 25, 26 The NACMI registry is the largest, prospective data set of STEMI patients with COVID-19 treated in 2021 and continues to demonstrate that PCI is feasible during the pandemic, with the majority of patients being treated within guideline-recommended times despite expected delays caused by testing and other logistical challenges posed by the pandemic. Educational efforts, such as the Society for Cardiac Angiography and Intervention’s Seconds Still Count Patient Awareness campaign, are helping reverse these trends.27 , 28
Study limitations
NACMI is the largest, prospective, multicentric STEMI COVID-19 registry to date. However, several limitations should be acknowledged. Common to observational registries, NACMI lacked independent event adjudication, core laboratory analysis, and pre-hospital data regarding total ischemic and transfer times for patients presenting to a non-PCI hospital. Angiographic and electrocardiographic core laboratory analysis are underway. Incomplete vaccination data as well as null number of deaths in vaccinated patients did not allow for estimating the association of vaccination with the risk of mortality while adjusting for underlying risk factors. The low proportion of vaccinated patients in a hospitalized cohort such as NACMI is consistent with the known protective effects against hospitalization, and other serious outcomes, of COVID-19 vaccines. Finally, our study did not capture information regarding COVID-19 variants. Omicron has shown signs of being less virulent than earlier variants, but it triggered record number of infections and a surge in deaths.29 Omicron was first reported in the United States on December 1, 2021, which is the very end of our study period.
Conclusions
Significant changes have occurred in the clinical characteristics, management strategies, and outcomes of STEMI patients with COVID-19 infection during the course of the pandemic. Notably, mortality is 25% lower for patients treated in Y2021 relative to Y2020 but remains high for unvaccinated patients.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE: Significant changes have occurred in the clinical characteristics, management strategies, and outcomes of STEMI patients with COVID-19 infection during the course of the pandemic. Mortality has decreased 25% but remains high for unvaccinated patients.
TRANSLATIONAL OUTLOOK: Efforts to educate the public on the beneficial effects of COVID-19 vaccines must continue.
Funding Support and Author Disclosures
This work Is supported by the American College of Cardiology Accreditation Grant and Saskatchewan Health Research Foundation (SHRF). The NACMI (North American COVID-19 STEMI) registry received financial support from Medtronic and Abbott Vascular. Dr Garcia has received institutional research grants from Edwards Lifesciences, BSCI, Medtronic, and Abbott Vascular; has served as a consultant for the American College of Cardiology, Medtronic, and BSCI; and has served as a proctor for Edwards Lifesciences. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgments
The authors thank the administrative and scientific personnel of the Society for Cardiovascular Angiography and Interventions, Minneapolis Heart Institute Foundation, Kiahltone R. Thao, and Logan Van Hon for their contributions to the NACMI registry.
Footnotes
Listen to this manuscript's audio summary by Editor-in-Chief Dr Valentin Fuster onwww.jacc.org/journal/jacc.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For a supplemental table, please see the online version of this paper.
Appendix
References
- 1.Ho F.K., Man K.K.C., Toshner M., et al. Thromboembolic risk in hospitalized and nonhospitalized COVID-19 patients: a self-controlled case series analysis of a nationwide cohort. Mayo Clin Proc. 2021;96:2587–2597. doi: 10.1016/j.mayocp.2021.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Luca G., Debel N., Cercek M., et al. Impact of SARS-CoV-2 positivity on clinical outcome among STEMI patients undergoing mechanical reperfusion: Insights from the ISACS STEMI COVID 19 registry. Atherosclerosis. 2021;332:48–54. doi: 10.1016/j.atherosclerosis.2021.06.926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kite T.A., Ludman P.F., Gale C.P., et al. International prospective registry of acute coronary syndromes in patients with COVID-19. J Am Coll Cardiol. 2021;77:2466–2476. doi: 10.1016/j.jacc.2021.03.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garcia S., Dehghani P., Grines C., et al. Initial findings from the North American COVID-19 Myocardial Infarction Registry. J Am Coll Cardiol. 2021;77:1994–2003. doi: 10.1016/j.jacc.2021.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saad M., Kennedy K.F., Imran H., et al. Association between COVID-19 diagnosis and in-hospital mortality in patients hospitalized with ST-segment elevation myocardial infarction. JAMA. 2021;326:1940–1952. doi: 10.1001/jama.2021.18890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stefanini G.G., Montorfano M., Trabattoni D., et al. ST-elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes. Circulation. 2020;141:2113–2116. doi: 10.1161/CIRCULATIONAHA.120.047525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bangalore S., Sharma A., Slotwiner A., et al. ST-segment elevation in patients with Covid-19 - a case series. N Engl J Med. 2020;382:2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Navaratnam A.V., Gray W.K., Day J., Wendon J., Briggs T.W.R. Patient factors and temporal trends associated with COVID-19 in-hospital mortality in England: an observational study using administrative data. Lancet Respir Med. 2021;9:397–406. doi: 10.1016/S2213-2600(20)30579-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madahar P., Wunsch H., Jha P., Slutsky A.S., Brodie D. Trends in COVID-19-related in-hospital mortality: lessons learned from nationwide samples. Lancet Respir Med. 2021;9:322–324. doi: 10.1016/S2213-2600(21)00080-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horwitz L.I., Jones S.A., Cerfolio R.J., et al. Trends in COVID-19 risk-adjusted mortality rates. J Hosp Med. 2021;16:90–92. doi: 10.12788/jhm.3552. [DOI] [PubMed] [Google Scholar]
- 11.Dehghani P., Davidson L.J., Grines C.L., et al. North American COVID-19 ST-Segment-Elevation Myocardial Infarction (NACMI) registry: rationale, design, and implications. Am Heart J. 2020;227:11–18. doi: 10.1016/j.ahj.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomas S.J., Moreira E.D., Jr., Kitchin N., et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine through 6 months. N Engl J Med. 2021;385:1761–1773. doi: 10.1056/NEJMoa2110345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baden L.R., El Sahly H.M., Essink B., et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N Engl J Med. 2021;384:403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morrow D.A., Antman E.M., Charlesworth A., et al. TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation. Circulation. 2000;102:2031–2037. doi: 10.1161/01.cir.102.17.2031. [DOI] [PubMed] [Google Scholar]
- 15.Dehghani P., Schmidt C., Garberich R., et al. TCT-63 North American COVID-19 Myocardial Infarction (NACMI) risk score for prediction of in-hospital mortality. J Am Coll Cardiol. 2021;78:B26. doi: 10.1016/j.jscai.2022.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haas E.J., McLaughlin J.M., Khan F., et al. Infections, hospitalisations, and deaths averted via a nationwide vaccination campaign using the Pfizer-BioNTech BNT162b2 mRNA COVID-19 vaccine in Israel: a retrospective surveillance study. Lancet Infect Dis. 2022;22(3):357–366. doi: 10.1016/S1473-3099(21)00566-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arbel R., Hammerman A., Sergienko R., et al. BNT162b2 vaccine booster and mortality due to Covid-19. N Engl J Med. 2021;385:2413–2420. doi: 10.1056/NEJMoa2115624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jara A., Undurraga E.A., González C., et al. Effectiveness of an inactivated SARS-CoV-2 vaccine in Chile. N Engl J Med. 2021;385:875–884. doi: 10.1056/NEJMoa2107715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rubin R. COVID-19 vaccines have been available in the US for more than a year—what’s been learned and what’s next? JAMA. 2022;327:513–516. doi: 10.1001/jama.2022.0106. [DOI] [PubMed] [Google Scholar]
- 20.Simon P., Ho A., Shah M.D., Shetgiri R. Trends in Mortality From COVID-19 and other leading causes of death among Latino vs White individuals in Los Angeles County, 2011-2020. JAMA. 2021;326:973–974. doi: 10.1001/jama.2021.11945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Henry T.D., Sharkey S.W., Burke M.N., et al. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116:721–728. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 22.Nallamothu B.K., Bates E.R., Wang Y., Bradley E.H., Krumholz H.M. Driving times and distances to hospitals with percutaneous coronary intervention in the United States: implications for prehospital triage of patients with ST-elevation myocardial infarction. Circulation. 2006;113:1189–1195. doi: 10.1161/CIRCULATIONAHA.105.596346. [DOI] [PubMed] [Google Scholar]
- 23.Yildiz M., Sharkey S., Aguirre F.V., et al. The Midwest ST-Elevation Myocardial Infarction Consortium: design and rationale. Cardiovasc Revasc Med. 2021;23:86–90. doi: 10.1016/j.carrev.2020.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garcia S., Albaghdadi M.S., Meraj P.M., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Daniels M.J., Cohen M.G., Bavry A.A., Kumbhani D.J. Reperfusion of ST-segment-elevation myocardial infarction in the COVID-19 era: business as usual? Circulation. 2020;141:1948–1950. doi: 10.1161/CIRCULATIONAHA.120.047122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xiang D., Xiang X., Zhang W., et al. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J Am Coll Cardiol. 2020;76:1318–1324. doi: 10.1016/j.jacc.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garcia S., Stanberry L., Schmidt C., et al. Impact of COVID-19 pandemic on STEMI care: An expanded analysis from the United States. Catheter Cardiovasc Interv. 2021;98:217–222. doi: 10.1002/ccd.29154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahmud E., Dauerman H.L., FGP Welt, et al. Management of acute myocardial infarction during the COVID-19 pandemic: a position statement from the Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP) J Am Coll Cardiol. 2020;76:1375–1384. doi: 10.1016/j.jacc.2020.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.SARS-CoV-2 B. 1.1.529 (Omicron) Variant—United States, December 1–8, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1731–1734. doi: 10.15585/mmwr.mm7050e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.