Abstract
Objective:
To determine the variation in prevalence of temporomandibular disorders (TMD), other side effects, and technical complications during 5 years of sleep apnea treatment with a mandibular advancement device.
Materials and Methods:
Forty patients diagnosed with obstructive sleep apnea received an adjustable appliance at 70% of the maximum protrusion. The protrusion was then progressively increased. TMD (diagnosed according to the Research Diagnostic Criteria for TMD), overjet, overbite, occlusal contacts, subjective side effects, and technical complications were recorded before and a mean of 14, 21, and 58 months after treatment and analyzed by the Wilcoxon test (P < .05).
Results:
Fifteen patients still used the oral appliance at the 5-year follow-up, and no significant variation in TMD prevalence was observed. Subjective side effects were common, and a significant reduction was found in overjet, overbite, and in the number of occlusal contacts. Furthermore, the patients made a mean of 2.5 unscheduled dental visits per year and a mean of 0.8 appliance repairs/relines per year by a dental technician. The most frequent unscheduled visits were needed during the first year and were a result of acrylic breakage on the lateral telescopic attachment, poor retention, and other adjustments to improve comfort.
Conclusions:
Five-year oral appliance treatment does not affect TMD prevalence but is associated with permanent occlusal changes in most sleep apnea patients during the first 2 years. Patients seek several unscheduled visits, mainly because of technical complications.
Keywords: Sleep-disordered breathing, Oral appliance, Craniomandibular disorders, Adverse effects, Device failure
INTRODUCTION
Obstructive sleep apnea (OSA) is a common respiratory disorder characterized by recurrent upper airway obstruction during sleep. Treatment options for OSA include behavioral modification, continuous positive airway pressure (CPAP), surgery, and oral appliances. Although CPAP appears to be most effective in improving OSA, oral appliances may be a good alternative for patients with mild to moderate symptoms who prefer oral appliances to CPAP or for those who are unable to tolerate CPAP therapy.1
Mandibular advancement devices (MAD) are the most common class of oral appliance used to treat snoring and OSA. Although there are several MAD designs, all devices protrude the mandible and induce changes in the anterior position of the tongue, soft palate, lateral pharyngeal walls, and mandible, resulting in improved airway patency.2 Increasing evidence suggests that MAD improves sleep-disordered breathing.1 However, response to MAD is variable and normally depends on the MAD design and patient characteristics. The acceptance rate of MAD after 1 year ranged from 55% to 82%, and there was a declining trend over time.2 The most common reasons for discontinuing MAD use are lack of efficacy, side effects, and complications.3
Subjective side effects are common, and the most frequently reported include temporomandibular joint (TMJ) pain, myofascial pain, tooth pain, salivation, TMJ sounds, dry mouth, gum irritation, and morning-after occlusal changes.4–7 Most of these side effects are minor and well-tolerated and tend to be resolved in a short period. However, objective side effects such as tooth movement, skeletal changes, and occlusal alteration have also been reported.5,8–17 Temporomandibular disorders (TMD) have been associated with the use of MAD, and this disorder is one of the exclusion criteria for many clinical studies. The majority of studies used the Helkimo Index or signs and symptoms to assess TMD.9,16,18 TMD are a cluster of heterogeneous disorders of the masticatory muscles and TMJs. The myogenous and arthrogenous disorders may be further subclassified into myofascial and arthrogenous pain, disc displacements, and degenerative joint disease as the most common conditions. The Research Diagnostic Criteria for TMD (RDC/TMD) were developed for research use and are a successful diagnostic and classification system.19
Appliances are usually worn every night indefinitely for symptomatic relief. The type and frequency of technical complications of MADs should be considered before treatment. However, technical complications with MADs, such as clasp breakages, repeated adjustments to optimize retention, or replacement of the device, have been reported in only a few studies.4,11,18,20,21 Technical complications may affect the cost for the patient and compliance with the treatment.22
The aim of this study was to evaluate variations in prevalence of TMD in OSA patients, as well as other side effects and technical failures, during 5 years of use of MADs.
MATERIALS AND METHODS
Forty-one adult patients with mild to severe OSA were recruited from the Sleep Unit of the Bellvitge University Hospital, Barcelona, Spain, between April 2002 and May 2004. All patients were diagnosed with OSA, based on the presence of OSA symptoms (snoring, apnea, and sleepiness) and overnight polysomnography (Apnea-Hypopnea Index > 10/h). Polysomnography was scored manually according to standard criteria.23 Patients were excluded if severe periodontal disease was present or if there were insufficient teeth to fit the MAD. All patients gave written informed consent to participate in the study, which was approved by the ethics committee of Bellvitge University Hospital. One patient was excluded because he did not have the minimum number of healthy teeth needed to retain the oral appliance. Therefore, 40 OSA patients participated in this prospective case series.
The MAD consisted of two full-coverage acrylic splints connected by two lateral telescopic attachments (Herner Guiding Telescopes, Iserlohn, Germany), allowing mouth breathing and a degree of side-to-side, protrusive, and opening movements of the mandible. Polyvinylsiloxane impressions of the maxillary and mandibular arches were used to manufacture dental plaster casts. The George Gauge (Great Lakes Orthodontic Lab, Tonowanda, NY) was used to measure the maximum mandibular protrusion capacity and then to make an interocclusal record of the desired anteroposterior and vertical mandibular position to be achieved by the MAD. The amount of mandibular advancement was initially set at 70% of the maximum and was then progressively increased over the following weeks until the patient stopped snoring or side effects appeared. All MADs were fabricated by the same dental technician and fitted and adjusted by a specialist dentist. The patients were instructed to use the MAD every night during sleep.
Before treatment was initiated, one dental clinician examined all patients, applied the RDC/TMD, and recorded the occlusal characteristics. Following the RDC/TMD algorithms, all subjects were assigned to the non-TMD group or to one of the three main groups (group I, myofascial pain; group II, TMJ disc displacement; group III, TMJ arthralgia/osteoarthritis/osteoarthrosis).19 Multiple diagnoses per subject were also possible. Overjet and overbite were measured by means of a digital caliper (Absolute; Vogel Germany, Kevelaer, Germany). Intraoral tooth contact in the intercuspal position was recorded using occlusal registration strips (Bausch Articulating Paper, Köln, Germany), and the recording was drawn on the protocol sheet.24 The number of occlusal contacts and the number of teeth in contact were recorded in both the anterior and posterior regions.
The follow-up visits were planned to be performed 6 weeks after the last increase in mandibular advancement, 6 months later, and 5 years after starting the therapy. The first checkup visit was performed after an average of 14 months from the start of treatment, the second checkup was performed after an average of 21 months from the start of treatment, and the third checkup took place after 4.8 years (range, 3.6 to 5.8 years). Follow-up visits consisted of occlusal registration, application of the RDC/TMD protocol, and a questionnaire to record the side effects reported by the patients. When patients referred to TMD-related symptoms, the RDC/TMD protocol was performed again. To evaluate the MAD treatment outcome, polysomnography was repeated close to the time of the first checkup for patients wearing the oral appliance during the night. Patients whose polysomnographs showed a lack of response were advised to discontinue MAD use.
During the treatment, patients with technical complications of the MAD and side effects involving the masticatory system were seen by a dentist. The number of additional dental visits, the reason for each extra visit, and the number of MAD repairs in the dental laboratory were recorded. Routine checkups and visits to increase the amount of mandibular advancement were excluded from this analysis.
Occlusal characteristics, TMD prevalence, and subjective side effects data at baseline and at each follow-up were compared using the Wilcoxon test for paired samples. P < .05 was regarded as statistically significant.
RESULTS
Thirty-one men and nine women were included in the study. The mean age was 54.1 years (SD 8.7; range, 35 to 70). Of these 40 patients, five did not attend the first checkup, four were lost, and another patient was affected by repetitive acrylic breakages on the lateral telescopic attachment of the oral appliance. This patient was included in the technical complications analysis but not in the side effects analysis. Between the first and the second checkup, 17 patients stopped using the MAD, 11 of them because polysomnography showed that it was ineffective, three because of side effects (arthralgia, myofascial pain, or discomfort), and the other three because it was considered that the appliance was no longer necessary, oral cancer, or dental modifications. Between the second and third checkups, three more patients were excluded: one because of multiple breakages, the second because of discomfort, and the third because he lost weight and the MAD was no longer needed. Therefore, 15 patients still used the MAD at the 5-year checkup. The mean mandibular advancement at the first checkup was 9.4 mm (83% of the maximum protrusion), and an increase in vertical dimension of 9.2 mm was observed at the incisal level.
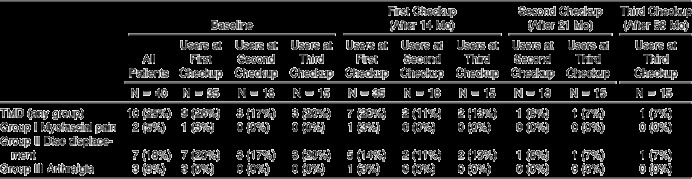
At baseline, 10 patients were diagnosed with TMD according to the RDC/TMD (Table 1). Of these, three were classified as presenting myofascial pain (group I), seven presented disc displacement with reduction (group II), and two presented arthralgia (group III). Two patients diagnosed as belonging to group II were also diagnosed as belonging to either group I or group III, given that the diagnostic groups were not mutually exclusive. Three of the five patients initially diagnosed as disc displacement with reduction still used the MAD at the 5-year follow-up, and only one of these patients was still diagnosed as disc displacement. Two patients who were initially diagnosed as disc displacement and five initially diagnosed as myofascial pain or arthralgia stopped using the MAD because it was ineffective, rather than as a result of problems with the masticatory system. No significant differences were observed in the prevalence of any TMD diagnosis group before treatment and at each checkup. During advancement of MAD, four patients reported mandibular pain. Three of these cases were diagnosed as arthralgia and the other as myofascial pain. Two of these four patients had not been diagnosed with TMD at baseline.
Table 1.
Number (Percentage) of Patients Diagnosed with Temporomandibular Disorders (TMD) for Each Diagnosis Group According to RDC/TMD at Each Checkup
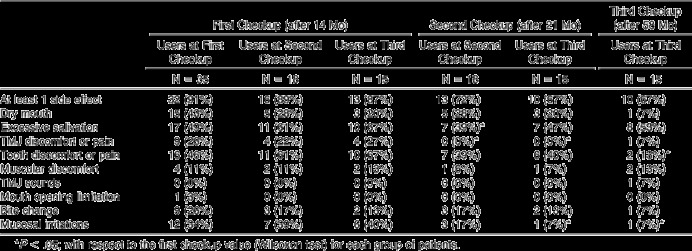
The number of occlusal contacts on the posterior teeth was reduced significantly during the 5 years of MAD treatment, and the greatest reduction was observed at the second checkup (Table 2). No significant differences in occlusal contacts or in the number of teeth in contact in the anterior region were observed during MAD treatment (Figure 1). Overbite and overjet were also significantly reduced during all treatments. Only 9%, 28%, and 33% of patients reported no side effects at the first, second, and last checkups, respectively (Table 3). Four patients stopped using the MAD because of side effects. The percentage of patients who reported tooth discomfort or mucosal irritations was significantly lower at the last checkup than at the first checkup.
Table 2.
Variations in Occlusal Characteristics (Means ± SDs) in Patients Before Oral Appliance Treatment and at Each Checkup
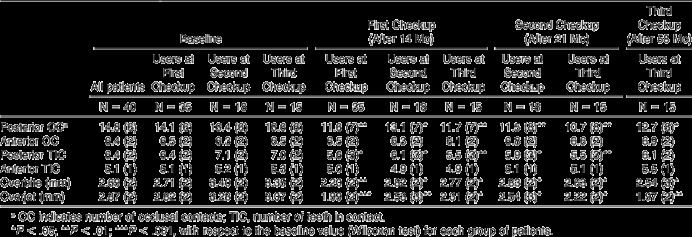
Figure 1.
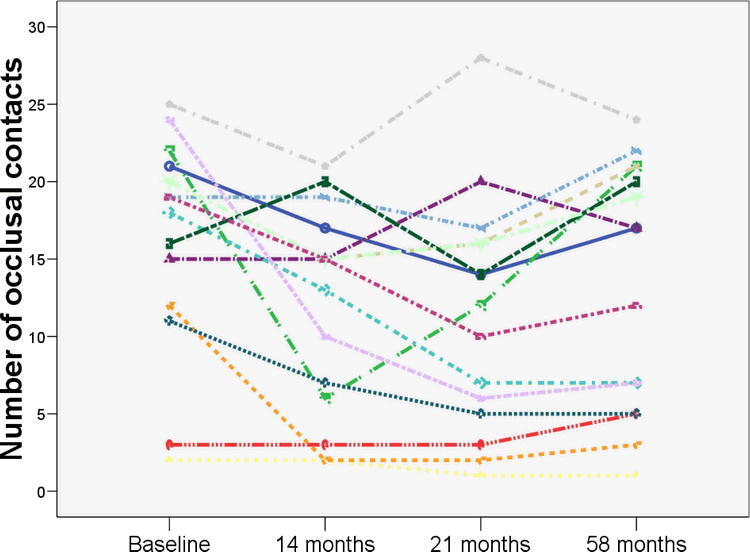
Individual number of occlusal contacts in the posterior teeth (n = 15) at baseline and at each checkup.
Table 3.
Number of Patients (Percentage) Who Reported Side Effects Related to the Use of the Oral Appliance at Each Follow-Up
Only eight patients did not request an extra visit to the dentist; four of these still used the MAD at the 5-year checkup. During the observational period, the patients made 160 extra visits to the dentist, and 54 appliance modifications were performed by the dental technician (Table 4). This corresponds to a mean of 2.5 unscheduled dental visits per year and a mean of 0.8 appliance repairs/relines per year by a dental technician. The most frequent unscheduled visits were needed during the first year because of acrylic breakage on the lateral telescopic attachment (Figure 2), poor retention, and other adjustments to improve comfort. Forty appliance repairs (32 because of acrylic breakage and eight relines because of MAD loosening) were made by the dental technician during the first 14 months.
Table 4.
Number of Additional Visits with the Corresponding Reason and the Number of Appliance Repairs During Oral Appliance Treatment
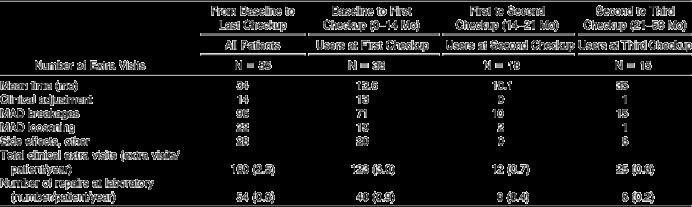
Figure 2.

Acrylic breakage on the lateral telescopic attachment.
DISCUSSION
The results of the present study confirm the reduction of overbite and overjet associated with the use of MAD reported in other long-term follow-up studies.13,14 Furthermore, the number of posterior occlusal contacts and number of posterior teeth in contact were significantly reduced during the first 2 years of MAD use. However, this tendency reversed during the period of 2 to 5 years of treatment, in agreement with another long-term study.8 It has been reported that the occlusal contact area and bite force of patients were reduced in the first months of wearing MAD.15 This was also demonstrated in a long-term study.17 Since bite force and occlusal contact area are the main factors that explain masticatory performance in dentate subjects,25 and the asymmetry of these factors is related to masticatory laterality,26 it appears that a reduction in masticatory performance can be expected in these patients. However, a direct relationship between the use of MAD and a worsening of masticatory efficiency is not demonstrated; this could be the subject of further research.
The results of this study suggest that 5 years of MAD treatment did not modify TMD prevalence in OSA patients. This is the first study in which TMD was diagnosed according to the RDC/TMD and classified as myofascial pain, disc displacement, and TMJ arthralgia/arthrosis in OSA patients in long-term therapy with MAD. Furthermore, OSA patients initially diagnosed with TMD were not excluded from this study. Although it has been stated that active TMD is a contraindication for MAD treatment,27 the results of this study, in agreement with other studies,9,10,16 suggest that the presence of disc displacement with reduction in the TMJ may not be a contraindication to treatment with a MAD. Furthermore, it has been found by means of magnetic resonance imaging that MAD appears to be innocuous to the TMJ in OSA patients, even in those with anterior disc displacement with or without reduction.28 The onset of arthrogenous or myogenous pain during advancement of MAD does not seem to be related to the presence of TMD before treatment.
We observed that MAD breakages, mainly on the lateral telescopic attachment, were the most frequent reason for seeking an unscheduled visit to the dentist. Such complications could be explained by errors made by the technician, maladjustments made by the dentist, and functional overload caused by nocturnal bruxism. These complications not only led to discontinuation of the use of MAD in two patients but also increased the cost of treatment and delayed effective treatment for OSA. Therefore, technicians and dentists should make the maximum effort to give patients the most comfortable and robust appliance. Although many studies have been published about the efficacy and side effects of MAD therapy, only a few reports have dealt with technical failure and the maintenance costs of these devices.4,11,18,20–22 In a previous study, 60% of subjects had experienced Herbst breakage and 40% received a replacement appliance after 3.6 years of treatment.11 When a monoblock MAD was used, technical complications were reported infrequently during the first year of treatment.18 However, six of nineteen patients had their monoblock device replaced by a new one in a 5-year follow-up study.20 Monoblock devices could be more robust and cost effective, but an adjustable appliance allows the mandible to be protruded incrementally and permits a degree of side-to-side, protrusion, and opening movement of the mandible.
The present study has several limitations. First, no control group was used, and a cause-and-effect relationship between the results of the present study and the use of MAD should be assumed with caution. Furthermore, we cannot know whether some adverse effects were related to the use of an intraoral appliance and/or to fact that the jaw was protruded for 6 to 8 hours per day. Second, the sample size might not have been large enough to find significant comparisons or relationships, such as in the prevalence of TMD.
CONCLUSIONS
In most OSA patients, 5-year oral appliance treatment is associated with mild, temporary subjective side effects and permanent occlusal changes mainly during the first 2 years.
The use of the oral appliance does not affect TMD prevalence.
Patients often seek several unscheduled visits, mainly because of technical complications.
Acknowledgments
The authors are grateful to the dental technician Santi Ferreres for performing the oral appliances and for repairing some of them. The authors also thank Robin Rycroft for language assistance.
REFERENCES
- 1.Lim J, Lasserson T. J, Fleetham J, Wright J. Oral appliances for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006 Jan 25;(1):CD004435. doi: 10.1002/14651858.CD004435.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cistulli P. A, Gotsopoulos H, Marklund M, Lowe A. A. Treatment of snoring and obstructive sleep apnea with mandibular repositioning appliances. Sleep Med Rev. 2004;8:443–457. doi: 10.1016/j.smrv.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Ferguson K. A, Cartwright R, Rogers R, Schmidt-Nowara W. Oral appliances for snoring and obstructive sleep apnea: a review. Sleep. 2006;29:244–262. doi: 10.1093/sleep/29.2.244. [DOI] [PubMed] [Google Scholar]
- 4.Shadaba A, Battagel J. M, Owa A, Croft C. B, Kotecha B. T. Evaluation of the Herbst mandibular advancement splint in the management of patients with sleep-related breathing disorders. Clin Otolaryngol Allied Sci. 2000;25:404–412. doi: 10.1046/j.1365-2273.2000.00411.x. [DOI] [PubMed] [Google Scholar]
- 5.Fritsch K. M, Iseli A, Russi E. W, Bloch K. E. Side effects of mandibular advancement devices for sleep apnea treatment. Am J Respir Crit Care Med. 2001;164:813–818. doi: 10.1164/ajrccm.164.5.2003078. [DOI] [PubMed] [Google Scholar]
- 6.de Almeida F. R, Lowe A. A, Tsuiki S, et al. Long-term compliance and side effects of oral appliances used for the treatment of snoring and obstructive sleep apnea syndrome. J Clin Sleep Med. 2005;1:143–152. [PubMed] [Google Scholar]
- 7.Marklund M, Franklin K. A. Long-term effects of mandibular repositioning appliances on symptoms of sleep apnoea. J Sleep Res. 2007;16:414–420. doi: 10.1111/j.1365-2869.2007.00615.x. [DOI] [PubMed] [Google Scholar]
- 8.Pantin C. C, Hillman D. R, Tennant M. Dental side effects of an oral device to treat snoring and obstructive sleep apnea. Sleep. 1999;22:237–240. doi: 10.1093/sleep/22.2.237. [DOI] [PubMed] [Google Scholar]
- 9.Bondemark L, Lindman R. Craniomandibular status and function in patients with habitual snoring and obstructive sleep apnoea after nocturnal treatment with a mandibular advancement splint: a 2-year follow-up. Eur J Orthod. 2000;22:53–60. doi: 10.1093/ejo/22.1.53. [DOI] [PubMed] [Google Scholar]
- 10.Fransson A. M, Tegelberg A, Johansson A, Wenneberg B. Influence on the masticatory system in treatment of obstructive sleep apnea and snoring with a mandibular protruding device: a 2-year follow-up. Am J Orthod Dentofacial Orthop. 2004;126:687–693. doi: 10.1016/j.ajodo.2003.10.040. [DOI] [PubMed] [Google Scholar]
- 11.Battagel J. M, Kotecha B. Dental side-effects of mandibular advancement splint wear in patients who snore. Clin Otolaryngol. 2005;30:149–156. doi: 10.1111/j.1365-2273.2004.00944.x. [DOI] [PubMed] [Google Scholar]
- 12.Hou H. M, Sam K, Hägg U, et al. Long-term dentofacial changes in Chinese obstructive sleep apnea patients after treatment with a mandibular advancement device. Angle Orthod. 2006;76:432–440. doi: 10.1043/0003-3219(2006)076[0432:LDCICO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Marklund M. Predictors of long-term orthodontic side effects from mandibular advancement devices in patients with snoring and obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2006;129:214–221. doi: 10.1016/j.ajodo.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Almeida F. R, Lowe A. A, Otsuka R, Fastlicht S, Farbood M, Tsuiki S. Long-term sequelae of oral appliance therapy in obstructive sleep apnea patients: part 2. Study-model analysis. Am J Orthod Dentofacial Orthop. 2006;129:205–213. doi: 10.1016/j.ajodo.2005.04.034. [DOI] [PubMed] [Google Scholar]
- 15.Otsuka R, de Almeida F. R, Lowe A. A. The effects of oral appliance therapy on occlusal function in patients with obstructive sleep apnea: a short-term prospective study. Am J Orthod Dentofacial Orthop. 2007;131:176–183. doi: 10.1016/j.ajodo.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 16.Hammond R. J, Gotsopoulos H, Shen G, Petocz P, Cistulli P. A, Darendeliler M. A. A follow-up study of dental and skeletal changes associated with mandibular advancement splint use in obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2007;132:806–814. doi: 10.1016/j.ajodo.2005.08.047. [DOI] [PubMed] [Google Scholar]
- 17.Ueda H, Almeida F. R, Lowe A. A, Ruse N. D. Changes in occlusal contact area during oral appliance therapy assessed on study models. Angle Orthod. 2008;78:866–872. doi: 10.2319/100107-470.1. [DOI] [PubMed] [Google Scholar]
- 18.Tegelberg A, Wilhelmsson B, Walker-Engstrom M. L, et al. Effects and adverse events of a dental appliance for treatment of obstructive sleep apnoea. Swed Dent J. 1999;23:117–126. [PubMed] [Google Scholar]
- 19.Dworkin S. F, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–355. [PubMed] [Google Scholar]
- 20.Marklund M, Sahlin C, Stenlund H, Persson M, Franklin K. A. Mandibular advancement device in patients with obstructive sleep apnea: long-term effects on apnea and sleep. Chest. 2001;120:162–169. doi: 10.1378/chest.120.1.162. [DOI] [PubMed] [Google Scholar]
- 21.Walker-Engstrom M. L, Tegelberg A, Wilhelmsson B, Ringqvist I. 4-year follow-up of treatment with dental appliance or uvulopalatopharyngoplasty in patients with obstructive sleep apnea: a randomized study. Chest. 2002;121:739–746. doi: 10.1378/chest.121.3.739. [DOI] [PubMed] [Google Scholar]
- 22.Loube M. D, Strauss A. M. Survey of oral appliance practice among dentists treating obstructive sleep apnea patients. Chest. 1997;111:382–386. doi: 10.1378/chest.111.2.382. [DOI] [PubMed] [Google Scholar]
- 23.American Academy of Sleep Medicine Task Force Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22:667–689. [PubMed] [Google Scholar]
- 24.Caro A. J, Peraire M, Martinez-Gomis J, Anglada J. M, Samsó J. Reproducibility of lateral excursive tooth contact in a semi-adjustable articulator depending on the type of lateral guidance. J Oral Rehabil. 2005;32:174–179. doi: 10.1111/j.1365-2842.2004.01287.x. [DOI] [PubMed] [Google Scholar]
- 25.Lujan-Climent M, Martinez-Gomis J, Palau S, Ayuso-Montero R, Salsench J, Peraire M. Influence of static and dynamic occlusal characteristics and muscle force on masticatory performance in dentate adults. Eur J Oral Sci. 2008;116:229–236. doi: 10.1111/j.1600-0722.2008.00530.x. [DOI] [PubMed] [Google Scholar]
- 26.Martinez-Gomis J, Lujan-Climent M, Palau S, Bizar J, Salsench J, Peraire M. Relationship between chewing side preference and handedness and lateral asymmetry of peripheral factors. Arch Oral Biol. 2009;54:101–107. doi: 10.1016/j.archoralbio.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 27.Clark G. T. Mandibular advancement devices and sleep disordered breathing. Sleep Med Rev. 1998;2:163–174. doi: 10.1016/s1087-0792(98)90019-3. [DOI] [PubMed] [Google Scholar]
- 28.de Almeida F. R, Bittencourt L. R, de Almeida C. I, Tsuiki S, Lowe A. A, Tufik S. Effects of mandibular posture on obstructive sleep apnea severity and the temporomandibular joint in patients fitted with an oral appliance. Sleep. 2002;25:507–513. [PubMed] [Google Scholar]


