Abstract
Objective:
To test the null hypothesis that there are no statistically significant differences between flowables and an orthodontic adhesive tested in terms of shear bond strength (SBS) and pullout resistance.
Materials and Methods:
To test the SBS of Light Bond, FlowTain, Filtek Supreme, and Tetric Flow were applied to the enamel surfaces of 15 teeth. Using matrices for application, each composite material was cured for 40 seconds and subjected to SBS testing. To test pullout resistance, 15 samples were prepared for each composite in which a wire was embedded; then the composite was cured for 40 seconds. Later, the ends of the wire were drawn up and tensile stress was applied until the resin failed. Findings were analyzed using an ANOVA and a Tukey HSD test.
Results:
The SBS values for Light Bond, FlowTain, Filtek Supreme, and Tetric Flow were 19.0 ± 10.9, 14.7 ± 9.3, 22.4 ± 16.3, and 16.8 ± 11.8 MPa, respectively, and mean pullout values were 42.2 ± 13.0, 24.0 ± 6.9, 26.3 ± 9.4, and 33.8 ± 18.0 N, respectively. No statistically significant differences were found among the groups in terms of SBS (P > .05). On the other hand, Light Bond yielded significantly higher pullout values compared with the flowables Filtek Supreme and Flow-Tain (P < .01). However, there were no significant differences among the pullout values of flowables, nor between Light Bond and Tetric Flow (P > .05).
Conclusions:
The hypothesis is rejected. Light Bond yielded significantly higher pullout values compared with the flowables Filtek Supreme and FlowTain. However, flowable composites provided satisfactory SBS and wire pullout values, comparable to a standard orthodontic resin, and therefore can be used as an alternative for direct bonding of lingual retainers.
Keywords: Retention, Fixed retainer, Bonding, Flowable composite, Physical property
INTRODUCTION
The introductions of acid etch and direct bonding techniques were among the most important improvements in orthodontics in the last century. These techniques facilitated attachment of orthodontic appliances to the teeth, and made appliances more esthetic and popular. Newman1 was the first to report direct bonding of orthodontic attachments to tooth surfaces in 1965, and Kneirim2 published the first report of the use of this technique to construct bonded fixed retainers.
Traditionally, bonded retainers have been attached to the teeth with composite. Various composites have been described for use in this technique including both restorative and orthodontic bonding materials. Thinning of the composite was previously advised to obtain the best handling characteristics, but there was still some difficulty.3 Later, several companies developed adhesives for lingual retainer bonding and claimed that these adhesives offer ease of application and optimal handling characteristics to allow the clinician to shape and finish the adhesive around the lingual retainer wire for maximum patient comfort. These highly filled, light-cured resins are also reported to be a better choice when longevity and durability are required.4,5 However, time-consuming trimming and finishing are often necessary to obtain optimal results.6
Flowable resin composites have been made with a variety of formulas and viscosities for different uses.7–12 Recently, the use of flowable composites, which were originally created for restorative dentistry by increasing the resin content of traditional microfilled composites, have been suggested for bonding lingual retainers.6,13,14 These composites are claimed to be advantageous because no mixing is required, needle tips on the application syringes allow direct and precise composite placement, the composite is not sticky, and it flows toward the bulk of the material rather than away from it. No trimming and polishing are required and chair time is reduced.6
However, previous reports have demonstrated that flowable composites present lower shear bond strength (SBS) values when used for bonding metallic orthodontic brackets.15 This raises the question whether they can serve as well when they are used for lingual retainer bonding. Fixed lingual retainers are kept in place for long periods of time. This requirement calls for sound and durable retention at the enamel/composite and composite/wire interfaces. A review of the literature revealed that systematic information about the use of flowable composites was limited to a number of bracket bonding studies and a few anecdotal technique clinic papers.6,13,14 Information about the SBS of flowable composites, when used for lingual retainers, is missing.
Therefore, the first aim of this study was to investigate whether flowable composites, when used for bonding lingual retainers, are a good option in terms of bond strength. The second part of the study tested whether flowable composites yield wire pullout resistance comparable to a regular orthodontic resin. For the purposes of this study, the null hypothesis assumed that there are no statistically significant differences between flowable composites and an orthodontic adhesive in terms of SBS and pullout values.
MATERIALS AND METHODS
Materials
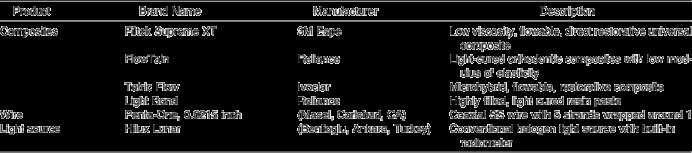
A range of materials was selected for use in this study to represent a broad cross-section of flowable composites available for clinical use in the construction of bonded retainers (Table 1). Three of these composites, Filtek Supreme XT (3M Espe, St. Paul, MN), FlowTain (Reliance, Itasca, IL), and Tetric Flow (Ivoclar, Schaan, Liechtenstein), and a control composite, Light Bond (Reliance, Itasca, IL), were selected for testing in this study.
Table 1.
Manufacturers and Properties of Materials Used
Methods
SBS testing
Sixty extracted sound human premolar teeth were used. Teeth with hypoplastic areas, cracks, or gross irregularities of the enamel structure were excluded from the study. The roots were mounted in a cubic mold using chemically cured acrylic resin (Vertex, Zeist, The Netherlands). The roots were mounted so that the labial surfaces of the crowns were perpendicular to the base of the molds. The teeth were then distributed into four experimental groups, each containing 15 teeth. A 37% orthophosphoric acid gel (3M Dental Products, St Paul, Minn) was used for acid etching of the teeth for 30 seconds, a common etching time in orthodontic bonding.15 The teeth were rinsed with water and dried with oil-free air for 10 seconds until the etched enamel exhibited a frosty, white appearance.
For each experimental group, respective adhesive primer was applied and light cured for 10 seconds. Then each composite resin was added to the surface by packing the material into cylindrical plastic matrices (Ultradent, South Jordan, Utah) with an internal diameter of 2.34 mm and height of 3 mm. Excess composite was carefully removed from the periphery of the matrix with an explorer, and the composite was cured with a halogen curing light (Hilux Lunar, Benlioglu, Ankara, Turkey) (Table 1) for 40 seconds (Figure 1).
Figure 1.
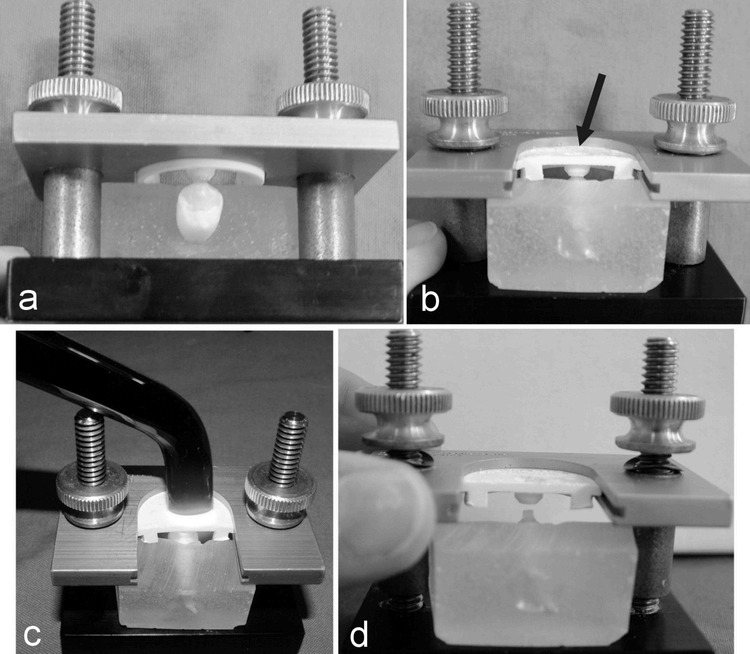
Preparation of the composite buildup on an enamel surface using the Ultradent matrix. (a) Matrix is adapted to the enamel surface. (b) Composite is packed into the mold (arrow). (c) Light curing. (d) Matrix is removed and the specimen is ready for testing.
The notched blade was placed directly over the resin stub flush against the tooth and, traveling at a crosshead speed of 1 mm/minute, was applied to each specimen at the tooth–composite interface until failure occurred (Figure 2).16 The force required to detach the composite block from the enamel surface was recorded in N and converted into MPa.
Figure 2.

Test setup used to determine the resistance of composites to pulling out the wire.
Wire pullout testing
Sixty cylindrical acrylic blocks, 25 mm in diameter and 10 mm deep, were prepared in molds to fit the universal testing machine. Fifteen blocks were allocated to each of the four test groups, and a hole 3 mm in diameter and 4 mm deep was drilled in the upper surface of each block, to represent the length of wire embedded in composite clinically in a bonded retainer. A 0.6 mm-wide groove was cut into the upper surface across the diameter of the block to accommodate the wire. The groove was cut to a depth of 1.0 mm in each test group to represent the total depth of the wire and composite material on the tooth surface. During the preparation phase, debris from the slot and center hole was cleaned manually and the slot and hole were dried using pressurized air.
A 10-cm length of 0.0215-inch Penta-One multistrand wire (Masel, Carlsbad, CA) (Table 1) was placed at the base of the groove and embedded in the respective composite material to be tested. The empty insert in the center of the slot was partially filled with the testing material using the appropriate syringe tip provided with the flowable resin package. Special precautions were taken so that the resin touched the walls of the center hole of the slot without the interference of air bubbles. The composite was then light cured for 40 seconds (Table 1).
The ends of the wire were drawn up and connected so that they could be secured using the attachment arm of the tensile load cell of the universal testing machine (TSTM 02500, Elista Ltd Sti, Istanbul, Turkey). With this arrangement, a force could be applied perpendicularly to the long axis of the embedded wire to cause wire pullout. A crosshead speed of 10 mm per minute was used, and the specimens were tested to failure.17 The force required to remove the wire from the composite was recorded in N (Figure 2).
Statistical Analysis
The raw data from all experiments were used to calculate group means and standard deviations. Analysis for statistically significant differences among groups was performed with one-way analysis of variance (ANOVA) with the SPSS (SPSS Inc., Chicago, IL) statistical analysis program. Differences between group means were tested for statistical significance at the 95% confidence level with the Tukey HSD range test.
RESULTS
SBS Testing
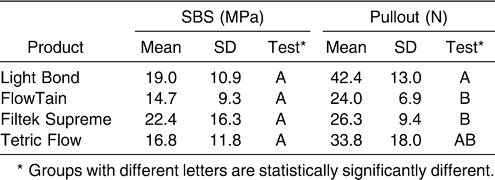
The results revealed that for Light Bond, FlowTain, Filtek Supreme, and Tetric Flow, the SBS values were 19.0 ± 10.9, 14.7 ± 9.3, 22.4 ± 16.3, and 16.8 ± 11.8 MPa, respectively (Table 2). Results of the ANOVA showed that there were no statistically significant differences among test groups (P > .05).
Table 2.
Means and Standard Deviations of SBS and Pullout Testing, and Statistical Results
Wire Pullout Testing
Results of the failure tests revealed that mean pullout forces for the test groups were 42.2 ± 13.0, 24.0 ± 6.9, 26.3 ± 9.4 and 33.8 ± 18.0 N for Light Bond, FlowTain, Filtek Supreme, and Tetric Flow, respectively (Table 2). Results of the ANOVA showed that there were statistically significant differences among test groups (P < .01). Therefore, the data were subjected to the Tukey HSD test for pair-wise comparison. The results demonstrated that Light Bond yielded statistically significantly higher detachment values compared with the flowable composites Filtek Supreme and FlowTain (P < .01); however, there were no statistically significant differences among the flowable composites or between Light Bond and Tetric Flow (P > .05) (Table 2).
DISCUSSION
A certain amount of relapse is almost inevitable following orthodontic therapy, particularly in the lower anterior segment. Therefore, the need for secure retention after orthodontic treatment is unquestioned, and the bonded wire retainer is the appliance of choice for the modern orthodontist.
With the advent of effective, new bonding materials, many orthodontists prefer to use canine-to-canine or premolar-to-premolar bonded retainers to obtain optimal retention of lower anterior teeth both functionally and esthetically.17–19 Recently use of flowable composites has been suggested for bonding lingual retainers,6,13,14 and almost every dental manufacturer now has its own flowable composite. Most of them show similar physical characteristics although they are marketed with claimed superiority to others. From a large range of composites available, three flowable composites (Filtek Supreme XT from 3M-Espe, Flow-Tain from Reliance, and Tetric Flow from Ivoclar) and a control composite (Light Bond, Reliance) were selected for testing. All these composites are widely used in dentistry and orthodontics.
The wire of choice for this testing procedure was 0.0215-inch Penta-One from Masel. This wire is also commonly used in orthodontics for lingual retainer fabrication. A study by Bearn et al17 showed that increasing the wire diameter from 0.0175 inch to 0.0215 inch increased the force required to pull the wire out of the composite, which was statistically significant (P < .05).
In the SBS part of the study, the samples were prepared using a standardized cylindrical mold from Ultradent to build up composite cores on the etched enamel surfaces, on which the composites were prepared directly. Since lingual retainers are bonded either directly or indirectly onto a tooth surface, the use of brackets was excluded from our experiment. If brackets had been used, another bonding interface, the adhesive-bracket interface, would have been created, making the results of the study vague. Even so, the bonded wire retainer is a complex system in which forces are exerted from different directions. It is difficult to perform a failure test that perfectly imitates the oral environment.20
Previous reports15 have demonstrated that flowable composites exhibit lower SBS values when they are used for bonding metallic orthodontic brackets. However, in this study we were unable to demonstrate any significant differences between the flowable composites and regular orthodontic adhesive. This difference may be a result of orthodontic attachments used in previous reports which was not the case in this study. Flowable composites may have been unsuccessful in adhering to the metallic bracket base failing to reveal actual enamel to flowable composite SBS.
The wire pullout-testing methodology was adopted from the study of Bearn et al.17 In that study, the method was used to evaluate the effect of composite type on retention of the wire. The total depth of the composite and the wire was selected as 1 mm, because Bearn showed that increasing the thickness to greater than 1.0 mm produced only a relatively small increase in force needed to detach the wire from the composite, so the increase was likely to give little clinical benefit.
The primary focus of the present study was to determine the resistance to failure when the wire is being pulled out of the composite, hopefully duplicating on a much larger scale the stress occurring when the area beneath the wire is being cleaned with dental floss. A question arising from an in vitro study is, Which forces must a retainer system withstand within the oral cavity under clinical conditions? The literature provides no data on clinically acceptable SBSs,20 but as for tensile loads, many studies cite Reynolds,21 who assumed that bonded orthodontic appliances should withstand 5–8 MPa. In his opinion, these forces are composed of chewing forces and other internal forces. According to Schulz et al,22 orthodontic bonds should be able to withstand 0.5–4 N. These loads consist—to a small extent—of chewing forces and—to a much greater extent—of forces required for the orthodontic movement of teeth through bone.
The average SBS of our study was around 20 MPa, which is well above that reported for many bracket SBS studies. Therefore, it can be claimed that, despite variations among them, the adhesives tested may be able to provide adequate SBS for successful clinical service. However, this statement should be evaluated with caution as no clinically acceptable SBS value has been previously reported for the retention of fixed lingual retainers. Also, physical surface characteristics such as hardness and surface roughness are other important factors that could affect the clinical effectiveness of the composites. Therefore, additional studies are needed to confirm these findings and prove the safety and dependability of flowable composites for use in orthodontic applications.
CONCLUSIONS
The flowable composites tested, FlowTain (Reliance), Filtek Supreme XT (3M), and Tetric Flow (Ivoclar) yielded comparable SBS values, and Tetric Flow exhibited wire pullout resistance values comparable with the control orthodontic composite, Light Bond (Reliance). Therefore, we believe it appropriate to advocate the use of these materials for bonded lingual retainers.
REFERENCES
- 1.Buonocore M. G. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955;34:849–853. doi: 10.1177/00220345550340060801. [DOI] [PubMed] [Google Scholar]
- 2.Kneirim R. W. Invisible lower cuspid to cuspid retainer. Angle Orthod. 1973;43:218–219. doi: 10.1043/0003-3219(1973)043<0218:ILCTCR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Zachrisson B. U. Third-generation mandibular bonded lingual 3-3 retainer. J Clin Orthod. 1995;29:39–48. [PubMed] [Google Scholar]
- 4.Usumez S, Buyukyilmaz T, Karaman A. Effect of a fast halogen and a plasma arc light on the surface hardness of orthodontic adhesives for lingual retainers. Am J Orthod Dentofacial Orthop. 2003;123:641–648. doi: 10.1016/S0889540603002014. [DOI] [PubMed] [Google Scholar]
- 5.Usumez S, Buyukyilmaz T, Karaman A. I, Gunduz B. Degree of conversion of two lingual retainer adhesives cured with different light sources. Eur J Orthod. 2005;27:173–179. doi: 10.1093/ejo/cjh085. [DOI] [PubMed] [Google Scholar]
- 6.Elaut J, Asscherickx K, Vande Vannet B, Wehrbein H. Flowable composites for bonding lingual retainers. J Clin Orthod. 2002;36:597–598. [PubMed] [Google Scholar]
- 7.Attar N, Tam L. E, McComb D. Flow, strength, stiffness and radiopacity of flowable resin composites. J Can Dent Assoc. 2003;69:516–521. [PubMed] [Google Scholar]
- 8.Bayne S. C, Thompson J. Y, Swift E. J, Jr, Stamatiades P, Wilkerson M. A characterization of first-generation flowable composites. J Am Dent Assoc. 1998;129:567–577. doi: 10.14219/jada.archive.1998.0274. [DOI] [PubMed] [Google Scholar]
- 9.Behle C. Flowable composites: properties and applications. Pract Periodontics Aesthet Dent. 1998;10:347–350. [PubMed] [Google Scholar]
- 10.Bonilla E. D, Yashar M, Caputo A. A. Fracture toughness of nine flowable resin composites. J Prosthet Dent. 2003;89:261–267. doi: 10.1067/mpr.2003.33. [DOI] [PubMed] [Google Scholar]
- 11.Labela R, Lambrechts P, Van Meerbeek B, Vanherle G. Polymerization shrinkage and elasticity of flowable composites and filled adhesives. Dent Mater. 1999;15:128–137. doi: 10.1016/s0109-5641(99)00022-6. [DOI] [PubMed] [Google Scholar]
- 12.Moon P. C, Tabassian M. S, Culbreath T. E. Flow characteristics and film thickness of flowable resin composites. Oper Dent. 2002;27:248–253. [PubMed] [Google Scholar]
- 13.Geserick M, Wichelhaus A. A color-reactivated flowable composite for bonding lingual retainers. J Clin Orthod. 2004;38:165–166. [PubMed] [Google Scholar]
- 14.Geserick M, Ball J, Wichelhaus A. Bonding fiber-reinforced lingual retainers with color-reactivating flowable composite. J Clin Orthod. 2004;38:560–562. [PubMed] [Google Scholar]
- 15.Uysal T, Sari Z, Demir A. Are the flowable composites suitable for orthodontic bracket bonding? Angle Orthod. 2003;74:697–702. doi: 10.1043/0003-3219(2004)074<0697:ATFCSF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Malkoc S, Demir A, Sengun A, Ozer F. The effect on shear bond strength of different antimicrobial agents after acid etching. Eur J Orthod. 2005;27:484–488. doi: 10.1093/ejo/cji032. [DOI] [PubMed] [Google Scholar]
- 17.Bearn D. R, McCabe J. F, Gordon P. H, Aird J. C. Bonded orthodontic retainers: the wire-composite interface. Am J Orthod Dentofacial Orthop. 1997;111:67–74. doi: 10.1016/s0889-5406(97)70304-4. [DOI] [PubMed] [Google Scholar]
- 18.Andenwalla S. T, Attarzadeh F. The bonded mandibular lingual retainer. Br J Orthod. 1986;13:159–163. doi: 10.1179/bjo.13.3.159. [DOI] [PubMed] [Google Scholar]
- 19.Bearn D. R. Bonded orthodontic retainers: a review. Am J Orthod Dentofacial Orthop. 1995;108:207–213. doi: 10.1016/s0889-5406(95)70085-4. [DOI] [PubMed] [Google Scholar]
- 20.Radlanski R. J, Zain N. D. Stability of the bonded lingual wire retainer: a study of the initial bond strength. J Orofac Orthop. 2004;65:321–335. doi: 10.1007/s00056-004-0401-4. [DOI] [PubMed] [Google Scholar]
- 21.Reynolds I. R. A review of direct orthodontic bonding. Br J Orthod. 1979;2:171–178. [Google Scholar]
- 22.Schulz R. P, Mayhew R. B, Oesterle L. J, Pierson W. P. Bond strengths of three resin systems used with brackets and embedded wire attachments. Am J Orthod. 1985;87:75–80. doi: 10.1016/0002-9416(85)90176-9. [DOI] [PubMed] [Google Scholar]


