Abstract
Objective:
To determine the surgery site dependency of root contact during drilling for orthodontic microimplant placement and to analyze the influence of clinicians' expertise on the results.
Materials and Methods:
Dental arches with resin teeth were mounted on a dental phantom (P-5/3 TS, Frasaco, Germany). Drilling was conducted in six locations frequently selected for microimplant placement: between the central incisors, between the maxillary first molar and second premolar, and between the mandibular first and second molars, bilaterally. The 28 qualified dentists who participated were divided into two groups based on their clinical experience. A total of 192 drillings were performed by the experienced group and 240 by the inexperienced group. The damaged root surfaces were classified as “moderate” or “severe.”
Results:
Significant differences in both overall and site-dependent rates of root contacts were found between the groups. Overall rates for the experienced and inexperienced groups were 13.5% and 21.3%, respectively. For the experienced group, the incidents occurred predominantly in the lower left (34.4%) and upper right (18.8%) posterior regions. The most susceptible teeth were numbers 36 and 16. In contrast, for the inexperienced group, all four posterior regions were susceptible.
Conclusions:
The surgery site and clinicians' expertise had significant effects on the rate as well as the pattern of root contacts.
Keywords: Microimplant, Root contact, Drilling
INTRODUCTION
Small-sized orthodontic microimplants allow easy placement with minimal anatomic limitations. Virtually all intraoral bony structures can host microimplants, and various sites have so far been tried for specific therapeutic purposes. For example, Kanomi1 and Costa et al2 implanted 1.2-mm- and 2-mm-diameter screws in the basal bone below the roots of teeth. The mandibular symphysis, midpalatal, infrazygomatic, alveolar process, sub-ANS, and retromolar areas have also been frequently selected. Among these, the interradicular bone in the alveolar process3 is biomechanically advantageous because of its proximity to the center of resistance of teeth. On the other hand, the risk of root contact or damage exists because of the narrow interradicular spaces and varying oral anatomies of individual patients.
Animal studies have demonstrated complete healing of minor damage to root tissue following implant removal, resulting in a normal periodontal structure.4,5 In contrast, heavily injured tissue did not heal completely,4 but left a bony ankylosed area on the root surface, which can have a negative impact on orthodontic tooth movement. Furthermore, microimplants in contact with root tissue are considered to be at a greater risk of failure. The force transfer from the tooth can jeopardize the implants' stability, leading to loosening and mobility that can worsen with time. Even root proximity has been reported as a primary risk factor for anchorage failure.6
Therefore, various methods to reduce the risk of root contact have been attempted, among which are anatomical maps for determining safer surgery locations and control of the microimplant insertion angle.3,7,8 Some researchers have recommended the use of a guide bar during periapical x-rays for preimplant assessment.9,10 However, these measures cannot always prevent root contact, so the clinical concern remains. Accordingly, in this study we investigated the frequency and pattern of root contact occurring during the drilling for orthodontic microimplant placement. Primary emphasis was placed on the influence of two factors: surgery site and the clinician's expertise.
MATERIALS AND METHODS
Upper and lower dental arch models with ideal arch forms were fabricated using plaster and sawdust at a ratio of 7∶3. Resin teeth with anatomically shaped roots (Il-Shin Co, Seoul, Korea) were placed mesial and distal to six drilling sites: between the central incisors, between the maxillary first molar and second premolar, and between the mandibular first and second molars bilaterally, resulting in a total of 12 resin teeth placed in a pair of upper and lower arch models: 11, 21, 31, 41, 15, 16, 25, 26, 36, 37, 46, and 47 (Figure 1). The root surfaces of the resin teeth were coated with red enamel paint as an aid in assessing root contact. The attached gingivae, the size of which was determined according to previous literature,11 was also colored red to display the drilling boundaries,
Figure 1.
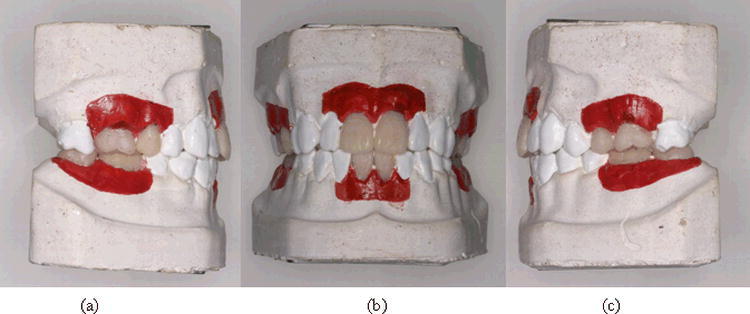
Dental arch model with resin teeth of anatomical root form placed at the mesial and distal of the six surgery sites. Red area represents the attached gingiva. (a) Right posterior, (b) anterior, and (c) left posterior areas.
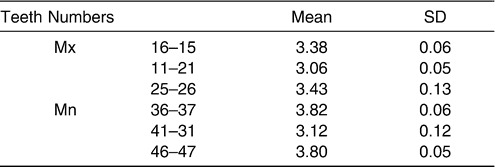
To confirm that the resin teeth were correctly positioned in the arch models, interroot distances were measured 7 mm apically from the cementoenamel junctions using a digital caliper with an accuracy of 0.01 mm. Means and standard deviations are presented in Table 1. The method error was calculated based on a repeat measurement of five randomly selected models after an interval of 2 weeks. Dahlberg's formula12 calculated the method error at 0.08, revealing it to be insignificant. Paired t-tests confirmed the result.
Table 1.
Means and Standard Deviations of Interradicular Distance Measured at the Six Drilling Sites of the Dental Arch Model (mm)
The arch model pairs were mounted in a dental phantom equipped with cheeks and movable TMJ (P-5/3 TS, Frasaco Co, Germany), maintaining Angle's Class I relationship. A total of 28 qualified dentists participated in the study, divided into two groups based on their level of expertise. The experienced group consisted of eight orthodontists with more than two years of experience in microimplant surgery. The inexperienced group consisted of 20 GPs who were either enrolled in—or had recently completed—their 1-year internship program on finishing their undergraduate DDS course. Precise instructions were given to all the participants regarding the position and direction (angulation) of the drill. The inexperienced participants were allowed one or two trial procedures at the six locations. In the experiment, each experienced participant worked on four upper and lower arch model pairs, while each inexperienced participant worked on two model pairs, resulting in a total of 192 drillings by the experienced participants and 240 by the inexperienced participants.
A pilot drill, 1 mm in diameter and 31 mm in length, was used with a slow-speed contra-angle handpiece. The occlusogingival and mesiodistal positions and angulation of the drill were as follows7: (1) in the maxillary molar region, on a line extending apically from the contact point of the second premolar and first molar and 8 mm apical to a line passing through the occlusogingival midpoints of the crowns (bracket position); and (2) in the mandible, the most apical position within the boundary of the attached gingiva on a line extending apically from the contact point of the first and second molars. The drill angulation was 45° for the upper and lower incisor areas, 30–40° and 20° in the maxillary and mandibular molar regions, respectively. The drilling depth for each site was 8 mm in the maxillary molar regions, 7 mm in the mandibular molar regions, and 6 mm in the anterior regions of both the mandible and maxilla. A colored band marked on the drills was used for depth control.
After drilling, the arch models were soaked in water for 6 hours and broken apart to expose and examine the roots. The drilled plaster materials were also examined to determine the drilling direction when root surface perforation was suspected. Damage to the root surface was classified as “moderate contact” or “severe contact” according to the size and pattern of the contact damage. Damage confined to the surface or indentations smaller than the drill radius were classified as moderate contact, whereas those greater than the drill radius or perforating the root surface were classified as severe contact (Figure 2).
Figure 2.
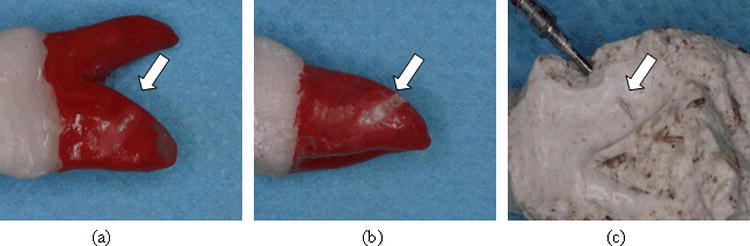
Assessment of the degree of root contact (white arrow). (a) Moderate contact. (b) Severe contact. (c) Perforated alveolar socket: an indication of root surface perforation.
The SAS 8.02 program (SAS Institute, Cary, NC, USA) was used for statistical analysis. Number of root contacts and their surgery-site dependence were analyzed and compared between the two groups. The Tukey test was used for post hoc comparison. Statistical significance was determined at P < .05.
RESULTS
The site and tooth-based summary of root contacts are given in Table 2. The overall rate for the experienced group was substantially lower than that of the inexperienced group, with statistical significance. Among the 192 drillings conducted by the former, 26 cases of root contact occurred, resulting in a rate of 13.5%, whereas the rate for the latter was 21.3% (51 contacts among 240 drillings). Note that the site-specific rate also differed significantly between the two groups, as presented in Figure 3. Unlike other sites, a higher rate was recorded for the experienced group on the lower left posterior area.
Table 2.
Number and Rate of Root Contacts in the Six Drilling Sites
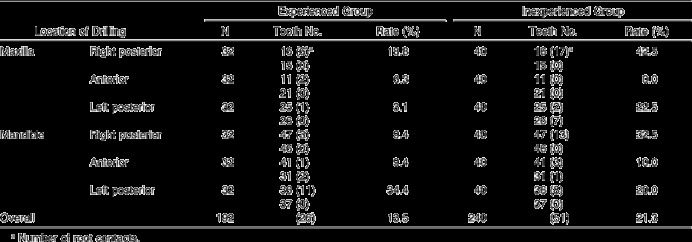
Figure 3.
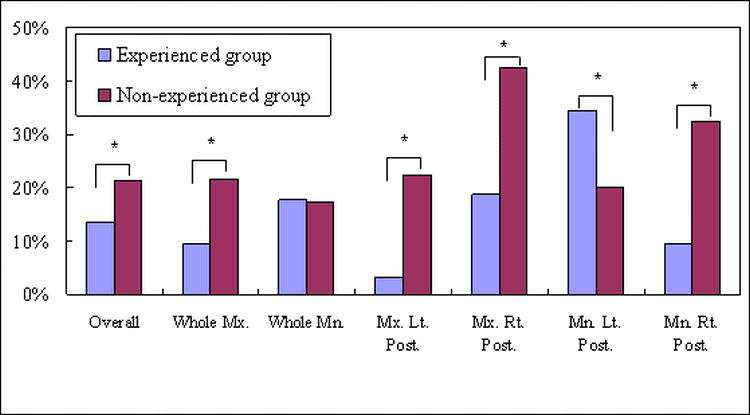
Comparison of the two groups. * Indicates statistical significance (P < .05).
Most of the root contacts were found in the posterior arches for both the groups. The experienced group operators caused root contacts predominantly in two sites: the lower left (between teeth 36 and 37; rate, 34.4%) and upper right (between 15 and 16; rate, 18.8%) areas. Statistical significance was found between these two sites. Meanwhile, for the inexperienced group, all four posterior regions were susceptible in the following order: upper right posterior (42.5%), lower right posterior (32.5%), upper left posterior (22.5%), and lower left posterior (20%). Differences were significant between the highest two and the lowest two sites, but not between the former two and between the latter two sites.
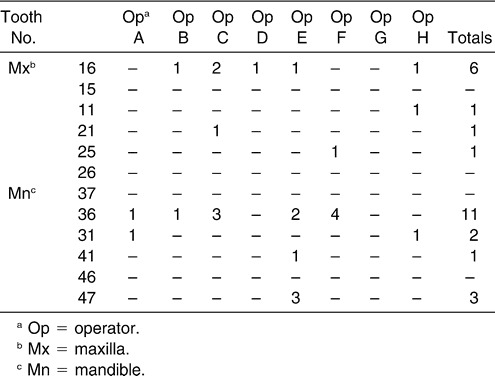
Table 3 displays the tooth-based distribution of the root contacts caused by each experienced group operator. Despite one participant's (operator E) making three root contacts at tooth 47, the statistical analysis results were not skewed. Although not presented here, root contacts made by the inexperienced group occurred in a more scattered fashion.
Table 3.
Distribution of Root Contacts Created by Experienced Group Operators
As the chi-square test revealed a significant difference in the overall and site-specific data between the two groups, further analysis was conducted for each group separately. And since the number of root contacts in the anterior regions was almost negligible compared with that in the posterior regions, only the data in the latter areas were analyzed.
Intragroup comparisons between the right and left arches are presented in Figure 4. The inexperienced group operators invaded more roots in the right-hand arches in both the maxilla and mandible, although it was not statistically significant. For the experienced group, right-vs-left bias was opposite between upper and lower jaws. Statistical significance in right-left difference existed only in the mandible. Upper and lower arch comparisons are presented in Figure 5, which reveals quite a different pattern between the two groups. For the experienced group, the overall rate was higher in the mandible, left posterior mandible, and right posterior maxilla, with statistical significance. However, for the inexperienced group, although the overall upper arch and its right and left posterior regions all showed a higher root contact rate than in the mandible, the differences were insignificant.
Figure 4.
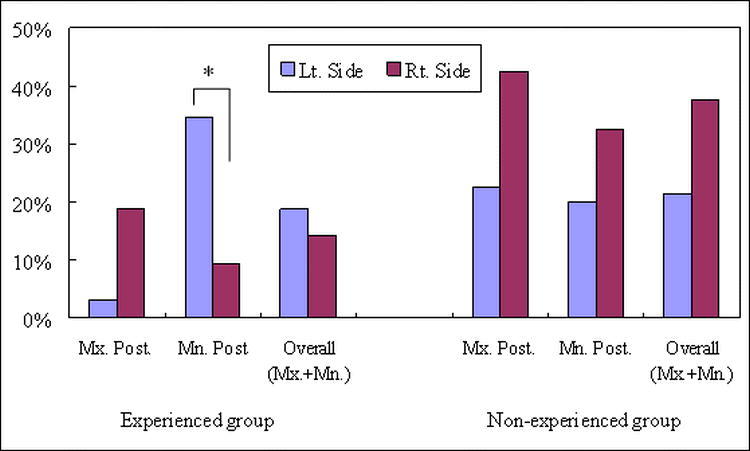
Comparison between right and left arches. * Indicates statistical significance (P < .05).
Figure 5.
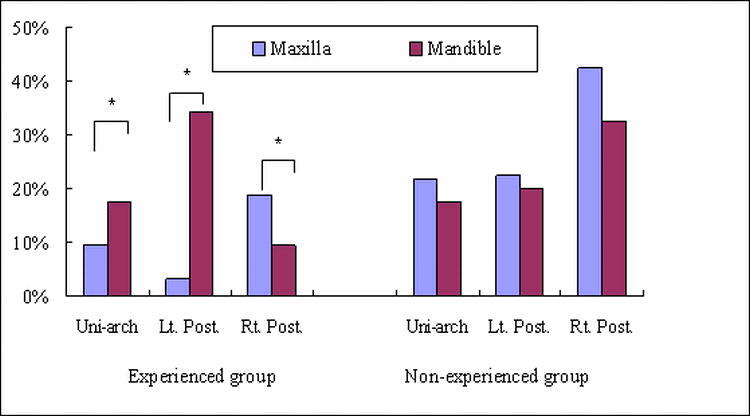
Comparison between upper and lower arches. * Indicates statistical significance (P < .05).
For the experienced group, severe contact occurred only at tooth 36. Of the 11 root contacts, four were classified as severe. For the inexperienced group, severe root contact was observed in a sporadic fashion: three instances at 16, two at 36, and one each at 26 and 46.
DISCUSSION
By selecting wider spaces, a clinician can reduce the risk of root contact. A 3D CT study7,8 has revealed that the widest interradicular distance in the maxilla was 3.18 mm, between the second premolar and first molar; in the mandible, it was 4.17 mm, between the first and second molars. These spaces would appear to be wide enough to host 1.2 mm- to 1.6 mm-diameter microimplants, sizes frequently used in orthodontic therapy. The risk can be further reduced by placing the microimplants at an angle with the root axis or with the alveolar bone surface. Actual insertion depth can be minimized while increasing cortical bone engagement. Selection of the drilling site and drilling angulation were based on these considerations. Even so, this study revealed that a significant number of root contacts can occur.
As expected, operator experience was a major factor in the root contact problem, which indicated that although a clinician might experience a high number of microimplant failures due to root contact in the initial trial period, the risk can be substantially lowered in subsequent years. Yet, it should be noted that the operator's habitual posture developed with clinical experience could have a negative impact, depending on the surgery site. Vulnerable sites were the maxillary right and mandibular left posterior regions (Figure 5). Two teeth, 36 and 16, were particularly susceptible. In the mandibular left, their contact rate was even highe than that of the inexperienced participants. This indicated that such operator factors as posture, view angle, and instrument access play more important roles than the interradicular space itself.
In the anterior arches, where visibility and accessibility were excellent, microimplants had a success rate of 100%, as opposed to 95% and 85.7% in the posterior regions.13,14 The experienced group tended to stick to their positions relative to the phantom with less movement, changing their posture less frequently throughout this experiment. All the participants in this study, with the exception of one operator in the experienced group, were right-handed; they conducted the drilling at positions between 9 o'clock and 12 o'clock, as appropriate.
Although there was right-vs-left bias in root contact results at each of the maxilla and mandible (experienced group), the combined rates were similar (Figure 4), that is, when the data in both upper and lower jaws were combined. Assuming a close correlation between clinical microimplant failure and root contact,6 this pattern is in overall agreement with previous clinical studies. Tseng et al,13 Cheng et al,14 and Park et al15 reported similar success rates of microimplant therapy in the right and the left posterior arches. When comparing upper and lower arches, higher failure rates recorded in the mandible in these clinical studies13–15 agree with the results exhibited by our experienced group (Table 2; Figure 5). A radiographic study by Kuroda et al6 supported this and showed that microimplant root contact was more frequent in the mandible (28.3% vs 25% in the maxilla). Mandibular microimplants also had a significantly higher failure rate. However, other studies reported similar success rates in the upper and lower arches, and an even lower rate in the mandible.16–17
In the left arches, most of the root contacts were mesial to the drilling: distal root surfaces of teeth 25 and 36 (with the exception of 26, the upper left posterior region for the inexperienced participants in Table 2). In the right arches, all the root contacts were distal to the drilling: mesial root surfaces of 16 and 47 for both groups. Therefore, it is apparent that both the angle and direction need to be carefully monitored and maintained throughout the course of drilling. The use of a surgical stent might be helpful, even for experienced operators, when drilling in the upper right or lower left posterior regions.
The incidence of severe root contact was low, with no case of root perforation. According to Andreasen et al,18,19 an injured root surface within 1.0 mm to 1.5 mm from a healthy periodontal ligament can undergo complete healing. Bae4 also reported that a damaged root surface can experience mild root resorption depending on the size of the injury, yet eventually heals to produce a healthy periodontal ligament. Since the most common drill and microimplant sizes are comparable to these dimensions, root damage from surgery would not be expected to be irreversible. A slow-speed drill can hardly perforate root tissue and, since an experienced clinician would ordinarily change the drilling direction when any resistance is felt, severe damage is unlikely. In a clinical situation, the patient's sensation could also help diagnose a root contact. Normally, the small dose, 0.5 mL–1.0 mL of lidocaine used for topical anesthesia, would not reach the adjacent PDL space to eliminate pain from intrusion of a foreign object, although the degree of anesthesia and referred pain from nearby nerve endings can make patient sensation an unreliable parameter.
Note that the mean root contact frequency of 13.5% recorded for the experienced group was similar to the commonly reported failure rate of microimplants.13–17,20 This might imply that a major portion of microimplant failures are related to the root contact problem. On the other hand, given that there are other risk factors involved (ie, implant size, mandibular angle, anatomical site of implant placement, bone quality, hygiene, soft tissue inflammation, and root proximity6,21), it might be that only some instances of root contact actually lead to microimplant failure. Therefore, a well designed clinical study is needed to clarify this issue.
CONCLUSIONS
Both the occurrence rate and the site-dependent pattern of root contacts during drilling for microimplant placement were affected by operator expertise.
Overall, the inexperienced operators generated a statistically significant higher frequency of root contacts (21.3%) than did the experienced group (13.5%; P < .05). The root contact rate of the experienced group was comparable to previously reported clinical microimplant failure rates.
For both groups, most root contacts occurred in the posterior regions. While the inexperienced participants generated contacts in all four posterior regions in a sporadic manner, the experienced operators' contacts occurred in two specific regions: the upper right and lower left posterior regions. The two most susceptible teeth were 16 and 36; thus, special attention is needed during drilling for microimplant placement to avoid mesial tilting for the former and distal tilting for the latter.
REFERENCES
- 1.Kanomi R. Mini-implant for orthodontic anchorage. J Clin Orthod. 1997;31:763–767. [PubMed] [Google Scholar]
- 2.Costa A, Raffini M, Melsen B. Microscrews as orthodontic anchorage. Int J Adult Orthod Orthogn Surg. 1998;13:201–209. [PubMed] [Google Scholar]
- 3.Park HS. Orthodontic Treatment Using Microimplant Clinical Applications of Microimplant Anchorage. Seoul, Korea: Daehan Nare Pub Co; 2006. pp. 5–33. [Google Scholar]
- 4.Bae SM. Daegu, Korea: Kyungpook National University; 2005. The repair of the root and pulp tissue after intentional root injury by the orthodontic microimplant in dog [PhD thesis] [Google Scholar]
- 5.Asscherickx K, Vannet BV, Wehrbein H, Sabzevar MM. Root repair after injury from mini-screw. Clin Oral Implants Res. 2005;16:575–578. doi: 10.1111/j.1600-0501.2005.01146.x. [DOI] [PubMed] [Google Scholar]
- 6.Kuroda S, Yamada K, Deguchi T, Hashimoto T, Kyung HM, Takano-Yamamoto T. Root proximity is a major factor for screw failure in orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2007;131(Suppl):S68–S73. doi: 10.1016/j.ajodo.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 7.Park HS. An anatomical study using CT image for the implantation of micro-implants. Kor J Orthod. 2002;32:435–441. Available at: http://www.koreamed.org/SearchBasic.php?RID=348360&DT=1&QY=%22Korean+J+Orthod%22+%5BJTI%5D Accessed May 30, 2009. [Google Scholar]
- 8.Hernández LC, Montoto G, Puente Rodríguez M, Galbán L, Martínez V. “Bone map” for a safe placement of miniscrews generated by computed tomography. Clin Oral Implants Res. 2008;19:576–581. doi: 10.1111/j.1600-0501.2007.01507.x. [DOI] [PubMed] [Google Scholar]
- 9.Bae SM, Park HS, Kyung HM, Sung JH. Micro-implant anchorage for treatment of skeletal Class I bialveolar protrusion. J Clin Orthod. 2001;35:417–422. [PubMed] [Google Scholar]
- 10.Bae SM, Park HS, Kyung HM, Kwon OW, Sung JH. J Clin Orthod. 2002: 36; Clinical application of micro-implant anchorage; pp. 298–302. [PubMed] [Google Scholar]
- 11.Lindhe J, Karring T, Lang NP. Clinical Periodontology and Implant Dentistry. Oxford, UK: Blackwell; 2003. pp. 5–8. [Google Scholar]
- 12.Dahlberg G. Statistical Methods for Medical and Biological Students. London: George Allen and Unwin; 1940. pp. 122–132. [Google Scholar]
- 13.Tseng YC, Hsieh CH, Chen CH, Shen YS, Huang, IY and Chen CM. The application of mini-implants for orthodontic anchorage. Int J Oral Maxillofac Surg. 2006;35:704–707. doi: 10.1016/j.ijom.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 14.Cheng SJ, Tseng IY, Lee JJ, Kok SH. A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorage. Int J Oral Maxillofac Implants. 2004;19:100–106. [PubMed] [Google Scholar]
- 15.Park HS, Jeong SH, Kwon OW. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006;130:18–25. doi: 10.1016/j.ajodo.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 16.Moon CH, Lee DG, Lee HS, Im JS, Baek SH. Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region. Angle Orthod. 2008;78:101–106. doi: 10.2319/121706-515.1. [DOI] [PubMed] [Google Scholar]
- 17.Luzi C, Verna C, Melsen B. A prospective clinical investigation of the failure rate of immediately loaded mini-implants used for orthodontic anchorage. Prog Orthod. 2007;8:192–201. [PubMed] [Google Scholar]
- 18.Andreasen JO, Rud J. Modes of healing histologically after endodontic surgery in 70 cases. Int J Oral Surg. 1972;1:148–160. doi: 10.1016/s0300-9785(72)80005-x. [DOI] [PubMed] [Google Scholar]
- 19.Andreasen JO, Kristerson L. The effect of limited drying or removal of the periodontal ligament. Periodontal healing after replantation of mature permanent incisors in monkeys. Acta Odontol Scand. 1981;39:1–13. doi: 10.3109/00016358109162253. [DOI] [PubMed] [Google Scholar]
- 20.Park HS. Clinical study on success rate of microscrew implants for orthodontic anchorage. Korean J Orthod. 2003;33:151–156. [Google Scholar]
- 21.Miyawaki S, Koyama I, Inoue M, Mishima K, Sugahara T, Takano-Yamamoto T. Factors associated with the stability of titanium screw placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2003;124:373–378. doi: 10.1016/s0889-5406(03)00565-1. [DOI] [PubMed] [Google Scholar]


