Abstract
Objectives:
To test the hypothesis that there is no correlation in the interrelationships of skeletal and soft tissue points A and B with anterior teeth retraction.
Materials and Methods:
Thirty adult Class I bimaxillary protrusion patients treated with preadjusted appliances after first premolar extraction were included. Pretreatment and posttreatment variables were compared using paired t-test, and the relationship of soft and hard tissue variables was studied using Pearson correlation coefficient and linear regression equation.
Results:
Mean point A and soft tissue point A (sA) were retracted 2.7 mm (P < .001) and 1.7 mm (P < .001), and mean point B and soft tissue point B (sB) were retracted 2.1 mm (P < .001) and 1.2 mm (P < .001), respectively. Mean ratio of retraction of point A with sA and point B with sB was 1.5∶1 and 1.7∶1, respectively. A significant degree of correlation existed between retraction of point A and soft tissue point A (r = 0.648, P < .01) and point B and soft tissue point B (r = 0.806, P < .01). Linear regression analysis used to predict the changes in sA and sB showed significant relationship between point A and sA (r = 0.543, F = 11.7, R2 = 0.29, P < .001) and point B and sB (r = 0.825, F = 59.7, R2 = 0.68, P < .001). Decreases in hard and soft tissue convexity were due to the retraction of the skeletal and soft tissue points A and B in addition to the lips retraction.
Conclusions:
The hypothesis is rejected. Retraction of skeletal point A and B lead to retraction of sA and sB under controlled root positions. Nearly proportionate changes existed in the skeletal points and overlying corresponding soft tissue points.
Keywords: Point A, Point B, Soft tissue point A, Soft tissue point B, Bimaxillary protrusion
INTRODUCTION
Dentoalveolar flaring of the anterior teeth with resultant protrusion of lips and convexity of the face are unique features of bimaxillary protrusion. Protrusive lips and a convex facial profile usually result in poor facial esthetics because of the forwardly placed dentoalveolar segments. Because of poor facial esthetics and the negative perception of protrusive dentition and lips in society, most patients with bimaxillary protrusion seek orthodontic treatment to reduce the protrusive lips.1 Thus, the patient, despite having Class I normal occlusion and meeting the criteria of Andrew's keys to normal occlusion, still wishes to undergo an orthodontic treatment that involves extraction of first premolars to improve the facial esthetics. Treatment of these cases involves backward movement of anterior teeth with a certain amount of uprighting of the incisors to correct excessive proclination so that a straighter profile is achieved. Since the objective of treating bimaxillary protrusion cases is to achieve an esthetically superior profile and harmonious lip relationship, it is important to study the changes in relationship of soft tissues to skeletal and dental structures that actually define the treatment outcome with orthodontic tooth movement.2
Soft tissue analyses by Holdaway,3 Ricketts,4 and Burstone5 have contributed greatly to the fundamental literature on the soft tissue relationship with dentoskeletal structures. Reidel6 stressed that the soft tissue profile is closely related to the skeletal and dental structures. Subtelny7 indicated that not all parts of soft tissue profile directly follow the underlying skeletal profile. Burstone5 suggested that a direct relationship may not always exist because of variation in the thickness of the soft tissue covering the skeletal face.8
Bimaxillary protrusion is a commonly seen malocclusion in eastern Nepal. However, in Class I bimaxillary protrusion cases treated with first premolar extraction, a paucity of literature exists regarding the relationship of skeletal point A and B with soft tissue point A (sA) and B (sB) following orthodontic treatment in the indexed literature. Thus, this study was undertaken to relate the skeletal point A and B changes with the soft tissue points A and B of Nepalese Class I bimaxillary protrusion patients treated with extraction and fixed mechanotherapy so that a clinician's attention is drawn more towards the apical bases and the tooth apices than the daily clinical scenario. The aim of this study was to test the hypothesis that there is no correlation in the interrelationships of skeletal and soft tissue points A and B with anterior tooth retraction.
MATERIALS AND METHODS
Pretreatment and posttreatment lateral cephalograms of 30 adults having Class I bimaxillary protrusion (15 girls, 15 boys) of mean age 18.4 years, treated at the Department of Orthodontics, College of Dental Surgery, B.P. Koirala Institute of Health Sciences were selected for this study. A written consent was obtained before treatment after patients agreed to the treatment planning. This study was approved and certified for its completion by the research committee of the B.P. Koirala Institute of Health Sciences, Dharan, Nepal.
Sample selection criteria included:
Minimum age 16 years
Class I first molar, canine, and premolar relationship
Well aligned arches with no or minimal crowding
Protrusive upper and lower lips
Pre and post radiographs with good hard and soft tissue outlines and teeth in full occlusion, lips resting in natural position.
All pretreatment and posttreatment cephalograms were taken from the same machine in the standard position by the same operator.
All patients were treated with 0.022- × 0.028-inch Roth, preadjusted appliances after extraction of first premolars. All patients were treated with maximum anchorage mechanics using palatal and lingual arches or second molars banding or headgears, depending upon the patient compliance. Mild palatal root torque in the upper arch and lingual root torque in the lower arch were incorporated in the incisor retraction wire to prevent labial movement of the roots and compensate for any wire play with the brackets. Since all patients had passed their 16th birthday, it was presumed that the influence of growth on point A and B changes would be clinically insignificant and have minimal effects on the treatment results. Posttreatment radiographs were taken after removal of fixed appliances.
A constructed Frankfort horizontal (FH) plane, drawn at an inferior angle of 7 degrees to SN plane through point “S”, was referred to as a modified plane and denoted by “FH”. Frankfort horizontal perpendicular was constructed perpendicular to the FH plane through point “S” and denoted by “FHp.” The linear measurements were done from FHp plane to skeletal and soft tissue points A and B (Figure 1, Table 1). A maximum of four cephalograms per day were analyzed. Linear parameters were measured with digital vernier caliper and angular parameters with a protractor, which recorded up to 0.01 mm and 0.5 degrees, respectively.
Figure 1.
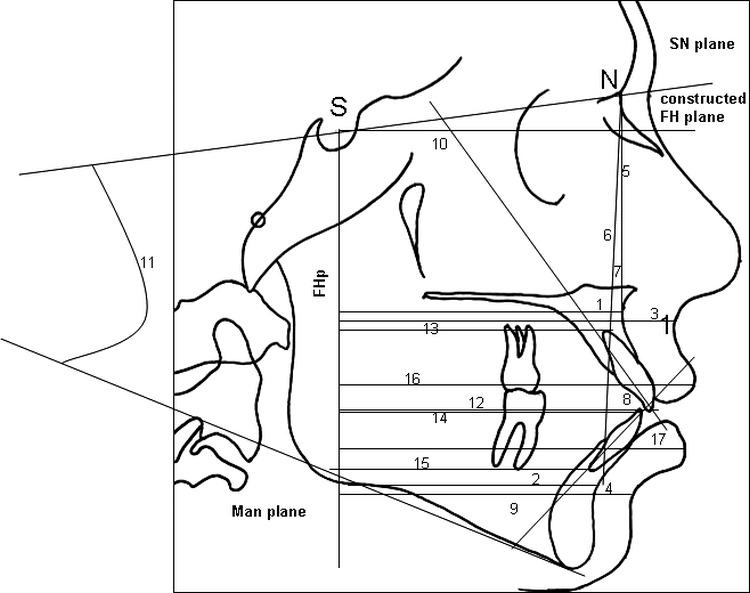
Cephalometric landmarks, measurements, and reference planes. (1) AFHp. (2) BFHp. (3) ssFHp. (4) siFHp. (5) SNA. (6) SNB. (7) ANB. (8) IIA. (9) IMPA. (10) U1SN. (11) SN-Go-Gn. (12) TUIFHp. (13) AUIFHp. (14) TLIFHp. (15) ALIFHp. (16) lsFHp. (17) liFHp.
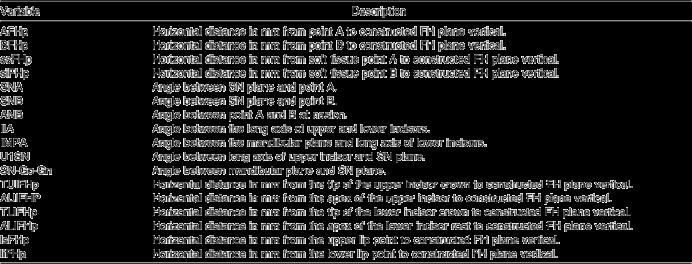
Table 1.
Cephalometric Measurements Used
The data were entered in Microsoft Excel and a master file was created in the spreadsheet. Descriptive statistics for mean, median, mode, standard deviation, range, and frequencies were calculated using the SPSS program version 11.5 (SPSS Inc, Chicago, Ill). The cephalometric values of pretreatment and posttreatment cephalograms were evaluated using paired t-test because the distribution of the data was approximately normal. Independent t-test was used to see any sexual differences in the outcome variables. P < .05 was considered significant in the study. A linear regression equation model to predict the changes in the soft tissue points A and B was calculated using the formula: Y = a + bX (where Y = dependent variable, sA or sB, and X = independent variable, point A or B).
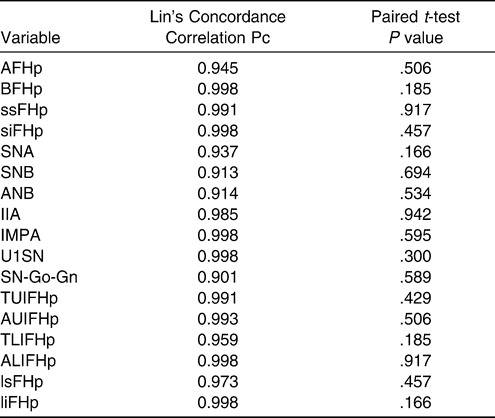
For the purpose of testing the intra-investigator error, 20 cephalograms were retraced after 8 weeks by the same operator. The tracings were analyzed using paired t-test and then Lin's concordance method9 for any significant difference between the two tracings.
RESULTS
No statistically significant differences were found between the observations made at two different times for the purpose of error testing using the paired t-test and Lin's concordance coefficient (Table 2). Mean age was 18.4 years (range 16–27 years) at the start of treatment. No statistically significant sexual differences were noted between the male and female samples when compared for each variable using independent t-test.
Table 2.
Summary Table for the Error of Study Analyses (n = 20)
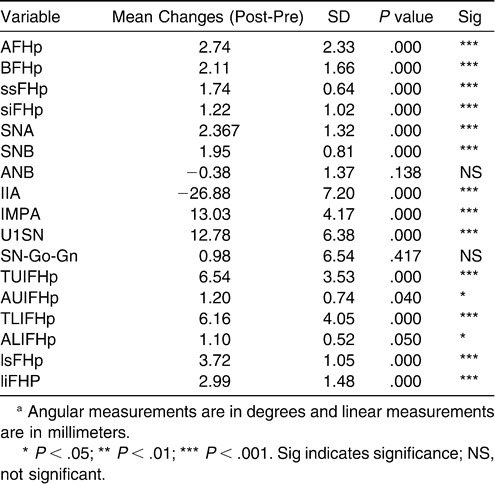
Upon incisor retraction, the mean point A retracted by 2.7 mm (P < .001) and mean sA retracted by 1.7 mm (P < 0.001). Similarly, the point B retracted by 2.1 mm (P < .001) and sB retracted by 1.2 mm (P < .001). The Pearson correlation coefficient (r) for A and sA was 0.648 (P < .001) and that of point B and sB was 0.806 (P < .001), showing a statistically significant relationship between these points. Linear regression analysis used to predict the changes in sA and sB showed significant relationship between point A and sA (r = 0.543, F = 11.7, P < .001). The coefficient of determination R2 was 0.29. Similarly for point B and sB, the relationship was significant (r = 0.825, F = 59.7, P < .001). The coefficient of determination R2 was 0.68.
Angle SNA retracted by 2.3 degrees and angle SNB retracted by 1.9 degrees. The ANB angle and the mandibular plane angle (SN-Go-Gn) did not show any significant changes. The mean interincisal angle increased from 105.9 degrees to 132.8 degrees. The IMPA decreased from 107.0 degrees to 94.1 degrees. The mean posttreatment U1 to SN angle was 103.4 degrees. The tip of the upper incisor retracted by 6.5 mm and the tip of the lower incisor retracted by 6.1 mm. Apices of upper and lower incisors showed 1.2 mm and 1.1 mm retraction following treatment. The upper and lower lips retracted at ls and li by 3.7 mm and 3.6 mm, respectively. The changes in the above parameters were statistically significant (Tables 3 through 5). The detrimental effects of orthodontic treatment in the periodontium were minimal after treatment except for mild blunting of the root apices in three cases under study.
Table 3.
Pretreatment Cephalometric Readings (n = 30)a
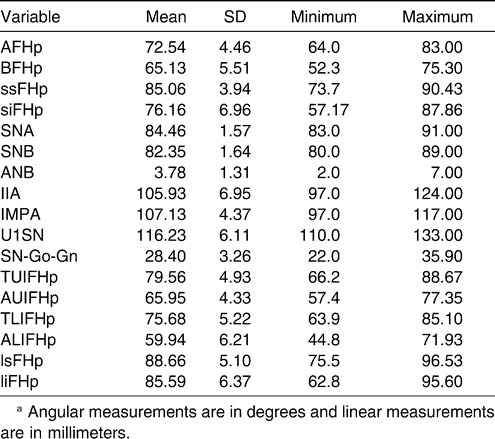
Table 4.
Posttreatment Cephalometric Readings (n = 30)a
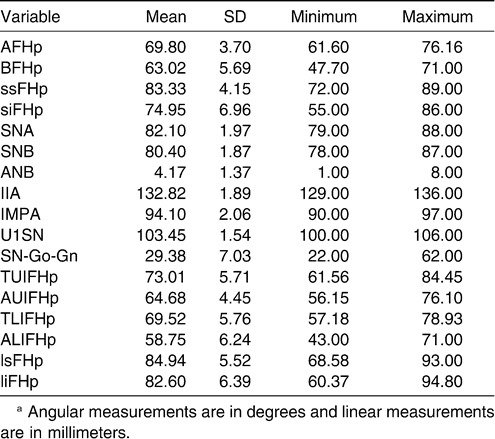
Table 5.
Mean Cephalometric Changes After Treatment (n = 30)a
DISCUSSION
In the present study, there was a significant relationship between retraction of skeletal point A (A) and soft tissue point A (sA) following incisor retraction. The skeletal point A retracted 2.7 mm (P < .001) and soft tissue point A retracted 1.7 mm (P < .001), establishing a ratio of 1.5∶1 (r = 0.648, P < .001). Skeletal point B retracted 2.1 mm (P < .001) and soft tissue point B retracted 1.2 mm (P < .001), establishing a ratio of 1.7∶1 (r = 0.806, P < .001). Linear regression analysis used to predict the changes in sA and sB showed significant relationship between point A and sA (r = 0.543, F = 11.7, R2 = 0.29, P < .001). Similarly for point B and sB, the relationship was significant (r = 0.825, F = 59.7, R2 = 0.68, P < .001).
The statistically significant correlation between these points indicated that with the backward movement of the skeletal points A and B, the soft tissue overlying these osseous points followed them, thus contributing to changes in the lip positions at the bases (Figures 2 through 4). The upper lip response was slightly higher when compared with the lower lip. This finding was slightly different from the findings of LaMastra,10 where skeletal point A moved back by 2.34 mm, soft tissue point A moved back by 1.75 mm, skeletal point B moved back by 1.89 mm, and soft tissue point B moved back by 1.73 mm. Thus, the ratio for the changes of skeletal point A to soft tissue point A in his study in Class II division 1 malocclusion was 1.4∶1 (r = 0.812, P < .001) and that of point B and soft tissue point B was 1.09∶1 (r = 0.96, P < .001). The difference could be related to the difference in the amount of tooth movement in the maxilla and mandible in Class II division 1 cases unlike Class I bimaxillary protrusion cases in the present study where they all were high anchorage cases for both arches. Roos11 in Class II malocclusion found the ratio of point A and point B retraction to corresponding soft tissue point A and B retraction to be 1∶1.4 (r = 0.58) and 1.2∶1 (r = 0.69), respectively.
Figure 2.
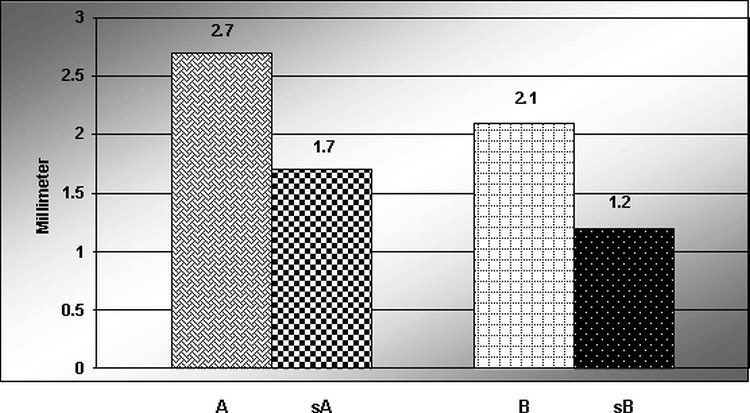
Mean changes in point A, soft tissue A, point B, and soft tissue point B after treatment.
Figure 3.
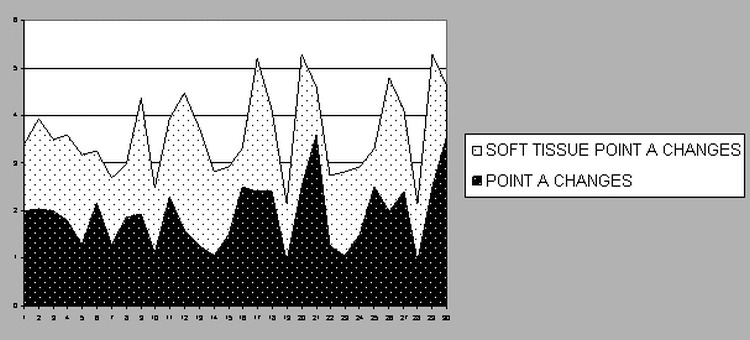
Point A and soft tissue point A changes (n = 30).
Figure 4.
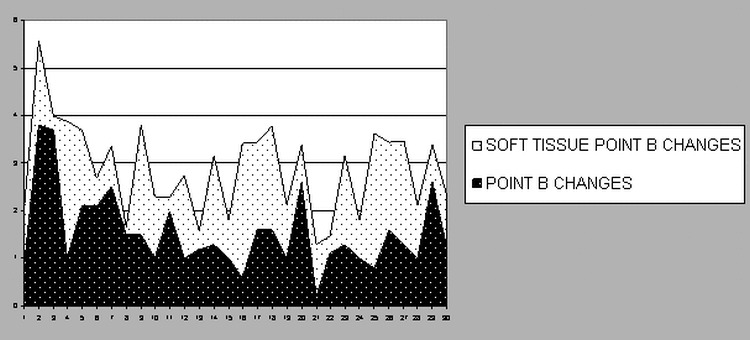
Point B and soft tissue point B changes (n = 30).
Bimaxillary protrusion cases generally have perfectly good occlusion. Patients are undergoing orthodontic treatment solely for the correction of protrusive profile and to improve the facial esthetics.
The clinical relevance of this study is that the clinicians must position the incisors in the most esthetic position by initial up-righting and some bodily movement. Thus, they must be cautious to prevent the reciprocal movement of the roots of anterior teeth labially during treatment. Therefore, it is very important to maintain the root positions and retract the incisors in this malocclusion group. With the labial movement of the roots, the skeletal convexity increases due to the forward movement of the skeletal points, which could become a factor for undesirable treatment results.12 A further study with a larger sample size including the sexual variation and the differentiation of thick and thin lips is recommended.
CONCLUSIONS
Retraction of skeletal points A and B leads to retraction of sA and sB under controlled root positions.
Lip retraction and retraction of the skeletal and soft tissue points A and B improved the soft tissue profile and decreased the soft tissue convexity.
Nearly proportionate changes in the skeletal and soft tissue points A and B existed with slightly better response in the upper lip than the lower lip.
Acknowledgments
Dr Kiran Kumar HK, Assistant Professor of Orthodontics and Dr D.D. Baral, Assistant Professor, Department of Biostatistics.
REFERENCES
- 1.Bills D. A, Handelman C. S, BeGole E. A. Bimaxillary protrusion: traits and orthodontic correction. Angle Orthod. 2005;75:333–339. doi: 10.1043/0003-3219(2005)75[333:BDPTAO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Diels R. M, Kalra V, Deloach N, Powers M, Nelson S. Changes in soft tissue profile of African-Americans following extraction treatment. Angle Orthod. 1995;65:285–292. doi: 10.1043/0003-3219(1995)065<0285:CISTPO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Holdaway R. A. A soft tissue cephalometric analysis and its use in orthodontic treatment planning. Part I. Am J Orthod. 1983;84:1–28. doi: 10.1016/0002-9416(83)90144-6. [DOI] [PubMed] [Google Scholar]
- 4.Ricketts R. M. Foundation for Cephalometric Communication. Am J Orthod. 1960;46:330–357. [Google Scholar]
- 5.Burstone C. J. Lip posture and its significance in treatment planning. Am J Orthod. 1967;53:262–284. doi: 10.1016/0002-9416(67)90022-x. [DOI] [PubMed] [Google Scholar]
- 6.Reidel R. A. An analysis of dentofacial relationships. Am J Orthod. 1957;43:103–119. [Google Scholar]
- 7.Subtelny J. D. A longitudinal study of soft tissue facial structures and their profile characteristics, defined in relation to underlying skeletal structure. Am J Orthod. 1959;45:481–507. [Google Scholar]
- 8.Bloom L. A. Perioral profile changes in orthodontic treatment. Am J Orthod. 1961;47:371–379. [Google Scholar]
- 9.Lin L. I. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45:255–268. [PubMed] [Google Scholar]
- 10.LaMastra S. J. Relationships between changes in skeletal and integumental points A and B following orthodontic treatment. Am J Orthod. 1981;79:416–423. doi: 10.1016/0002-9416(81)90383-3. [DOI] [PubMed] [Google Scholar]
- 11.Roos N. Soft tissue profile changes in Class II treatment. Am J Orthod. 1977;72:165–175. doi: 10.1016/0002-9416(77)90057-4. [DOI] [PubMed] [Google Scholar]
- 12.Goldin B. Labial root torque: effect on the maxilla and incisor root apex. Am J Orthod Dentofacial Orthop. 1989;95:208–219. doi: 10.1016/0889-5406(89)90051-6. [DOI] [PubMed] [Google Scholar]


