Abstract
Objective:
To test the frictional resistance forces (FRS) generated between several archwires and (1) interactive self-ligating (ISL) brackets and (2) conventionally ligated (CL) brackets.
Materials and Methods:
Frictional forces produced between three different archwire combinations and self-ligating (SL) brackets (ceramic and metal-slot or all-metal) and CL brackets (metal or ceramic) were evaluated in a dry environment. The three ISL brackets tested were In-Ovation-C, In-Ovation-R, and Damon 3. The three CL brackets were Mystique with Neo Clip, Clarity, and Ovation. Each bracket was tested with 0.020″ SS, 0.019″ × 0.025″ SS and 0.018″ × 0.018″ coated SS.
Results:
The ISL brackets generally exhibited the lowest frictional forces irrespective of the bracket material and the wire size, and CL brackets exhibited consistently higher frictional forces. Mystique with Neo Clip produced the lowest frictional resistance of all brackets. The In-Ovation-C brackets demonstrated significantly lower frictional resistance than the SL brackets In-Ovation-R and Damon 3 as well as the CL brackets Clarity and Ovation.
Conclusions:
The ISL ceramic brackets produced the lowest frictional resistance of all the self-ligating brackets. The CL ceramic brackets produced the greatest friction.
Keywords: Ceramic-injection-molding, Interactive self-ligation, Friction reduction
INTRODUCTION
Interactive self-ligation (ISL) ceramic brackets are relatively new and little evidence-based data have reported thus far. Despite this, the frequency of use of ISL brackets is growing exponentially worldwide (Figures 1 and 2).1 A major reason for this is the increased patient demand for high esthetics in treatment. Consequently, there is a need for evidence-based research on the properties of esthetic, ceramic ISL and the frictional resistance (FRS) of ISL compared with conventionally ligated (CL) brackets. This is particularly true as lower FRS has recently been associated with significant reductions in overall treatment duration.2 In addition, another study demonstrated that passive brackets have no improvement during initial alignment compared with conventional brackets.3
Figure 1.
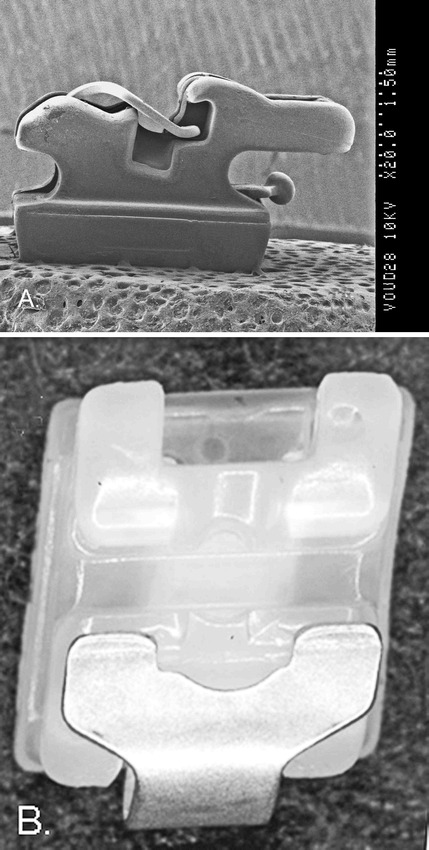
(A) SEM, 20× magnification of a side view of an interactive bracket (In-Ovation-C*). A smooth, glasslike texture is observed with the new ceramic-injection-molded (CIM) processed slot. The closed clip is compressed producing a curved shape. This produces a passive-active clip that curves toward the depth of the 0.022″ × 0.028 archwire slot to actively seat wires that are ≥0.020″ round SS for controlled sliding. Chamfered slot end(s) to reduce couples (binding) during tipping. (B) Light stereomicroscopy of the facial view of the maxillary left canine In-Ovation-C bracket and clip in an open-slot position demonstrates glasslike slot smoothness. The anodized rhodium-coated clip provides an esthetic, pearlescent color blending esthetically with the CIM
Figure 2.
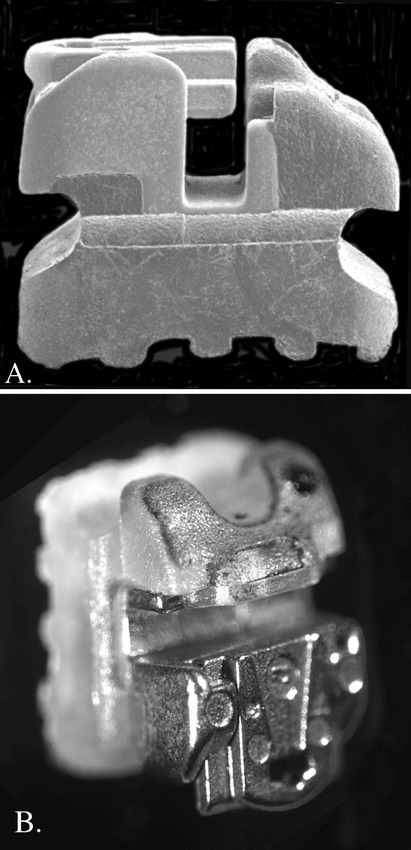
(A) SEM, 25× magnification of side view of the passive SL system Damon 3** of the maxillary left canine is shown with a polycarbonate upper 1/2, and a metal slot-clip assembly in the lower one-half. In this side view, there is no clip curvature to seat archwires toward the base of the slot making it passive. (B) Light, stereomicroscopy is used to examine the Frontal-¾ perspective of the passive metal clip in the open position demonstrating the metal slot-clip assembly is inserted into the polycarbonate material in the open position
Furthermore, ISL (also referred to as a passive-active system) attempts to satisfy two functional replacement criteria of elastomers.4 This includes both locking (passive) and seating (active) the archwire into the base of the slot with low functional friction so as to fully express the prescription.5,6 In contrast, passive systems do not fully seat the archwire for early full torque and in-out control as advocated by Roth.7 The low FRS found with self-ligation is clinically relevant for early alignment and sliding retraction of canines. Light force application may also contribute to the potential prevention of root resorption and anchorage loss.
The FRS is a critical factor in determining the efficiency of biological tooth movement during sliding mechanics. Many factors have been implicated in influencing friction in orthodontic systems, including wire size,4,8–12 bracket slot material,11,13,14 and method of ligation.4,11,15–20 One ISL bracket study demonstrated lower friction than CL brackets irrespective of the sliding angulations with the archwire.21 Other studies have found that increasing the archwire dimension is not significant;8 and some have found that smaller dimension archwires actually produce the highest FRS friction.12 Several studies have shown stainless steel (SS) brackets have less FRS during sliding than ceramic and other esthetic brackets.11,13,14,22,23 Finally, investigations of ligation methods have shown that ISL brackets reduces friction to minimal levels resulting in better efficiency compared with CL brackets.4,16–18
The purpose of this study was to evaluate the frictional forces generated between several archwires and ISL brackets made of ceramic, polycarbonate-metal, and all-metal brackets and to compare these frictional forces to metal and ceramic-metal brackets with elastomeric ligatures and ceramic with modified ligatures (Table 1). Three SS wire-size combinations with the six brackets were tested in vitro.
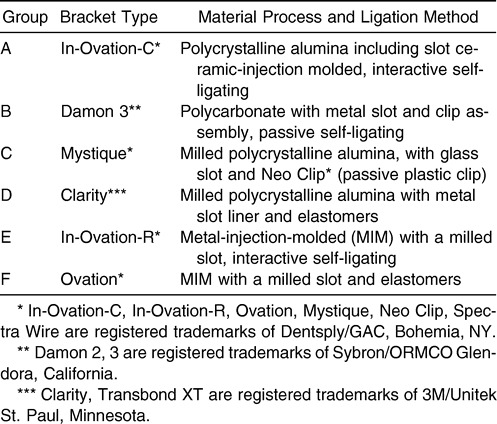
Table 1. .
Groups of Brackets and Ligation Method
MATERIALS AND METHODS
Sample Sizes
FRS was tested by the same operator in a standard laboratory setting using 0.022″ × 0.028″ maxillary left canine brackets and a Roth prescription. They were combined with 0.020″ SS and 0.019″ × 0.025″ SS archwires (Highland Metals, San Jose, Calif) and 0.018″ × 0.018″ esthetic SS archwires (Spectra Wire, Dentsply/GAC, Bohemia, NY) coated with polytetrofluoroethylene (PTFE). The brackets tested were:
ISL
Group A4—In-Ovation-C (Dentsply/GAC, Bohemia, NY)
Group E4—In-Ovation-R (Dentsply/GAC, Bohemia, NY)
Group B4—Damon 3 (Sybron/ORMCO, Glendora, Calif)
CL
Group C4—Mystique (Dentsply/GAC, Bohemia, NY)
Group D4—Clarity (3M/Unitek, St Paul, Minn)
Group F4—Ovation, (Dentsply/GAC, Bohemia, NY)
The three different archwires were held in the Clarity and Ovation brackets with elastomeric ligatures (Dentsply/GAC, Bohemia, NY) and tested in a dry environment. The specimen population totaled 180 bracket and archwire specimen combinations (6 groups × 10 sample brackets × 3 archwire sizes). Each bracket was pulled along a section of a 50-mm wire only once to eliminate the influence of wear. The elastomeric modules were tied with a ligature gun (Straight-Shooter, T-P Orthodontics, La Porte, Ind). This method limited possible stretching differences between the elastomeric modules. All elastomers, and all Neo Clips for Mystique, were placed over the bracket-archwire assembly and left for 24 hours before testing to allow for relaxation and adaptation.
Measurement Technique
A testing machine (Chatillon, TCD 200, CSC Force Measurement, Agawam, Mass) with a 1 Newton tension load cell was set on a range of 1 lb and calibrated from 0 to 1000 g in this experiment (Figure 3A). The brackets were bonded (Transbond XT, 3M/Unitek, St Paul, Minn) on plastic bracket pedestals, then wiped with alcohol and air dried. Straight wires were inserted into individual brackets (Figure 3B). The upper and lower part of the wire was then fixed in the C-shaped acrylic rod. The C-shape rod was held from the crosshead of the testing machine (Figure 3C).
Figure 3.
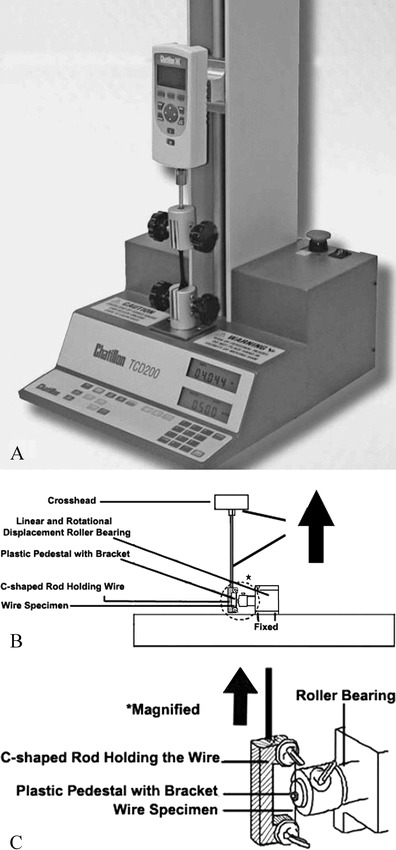
(A) The frictional resistance testing apparatus. (B) The bracket-wire setup is shown. (C) A magnified illustration of the C-shaped rod holding the wire
Each bracket was placed in a custom-designed testing apparatus that was fixed to the base of the testing machine. The plastic bracket pedestal was connected through roller bearing to allow for linear and rotational displacement of each bracket. Thus, the bracket and the wire specimen were perfectly aligned during each run to prevent a notching or binding effect due to excessive angulation of the bracket relative to the wire.
The rate of movement was 12.7 mm/min, and each test was carried out for 1.0 mm to minimize wear and to simulate canine retraction between monthly appointments. Ten nonrepeated evaluations for each bracket-archwire combination were tested. The load cell registered the force values, as measured by a digital force gauge (Model Chatillon DFA Series, ItinScale Co, Brooklyn, NY) and were transmitted to a computer disk as a DC analog voltage signal. The load cell voltage signals were transmitted to the computer file through a data acquisition board and accompanying software (Nexygen FM, Low Force Application Measurement software Version 4.2, ItinScale Co, Brooklyn, NY). The data were entered into a statistical analysis system (Statistics Toolbox for MATLAB, Mathworks Inc, Natick, Mass).
Data Analysis
Mean and standard error were calculated from 10 readings of dynamic friction. A nonrepeated analysis of variance was used to analyze differences among groups, and Tukey's test was used to identify differences among means of different groups for a bracket and wire dimension. Significance was set at α = .01.
RESULTS
Comparison of Frictional Forces by Bracket Type
The highest statistically significant friction was shown by the 0.020″ SS wire and the Clarity bracket (Group D) (mean 72.55g; Table 2). The Ovation bracket (Group F) produced the second-highest friction (mean 62.55g). The Mystique (Group C), In-Ovation-C (Group A), Damon 3 (Group B), and In-Ovation-R (Group E) brackets produced the lowest mean frictional forces (Figure 4). The differences between Clarity and Mystique and the differences between Ovation and In-Ovation-R were statistically significant at (P < .01).
Table 2. .
Means and Standard Deviations (SDs) of Frictional Force in Gramsa
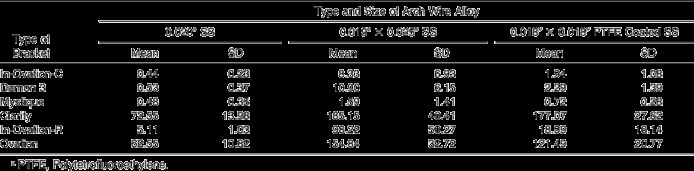
Figure 4.
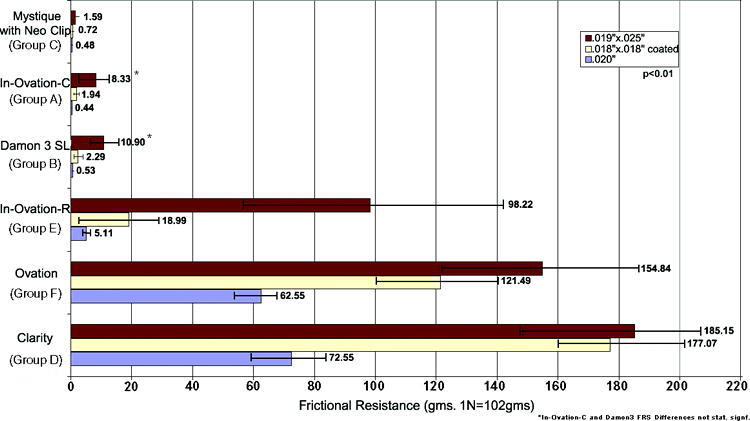
Mean frictional resistances with standard deviations are shown for ceramic, polycarbonate-metal, and all-metal SL brackets compared with CL ceramic and metal brackets ligated with elastomers and using three different arch wire sizes
For the 0.019″ × 0.025″ SS wire, the Clarity (Group D) and Ovation (Group F) brackets produced the greatest friction with mean values of 185.15g and 154.84g, respectively. The differences between these two were not statistically significant. However, the differences between Clarity and Mystique were statistically significant (P < .01). In-Ovation-R brackets demonstrated a mean value for FRS of 98.22g which is statistically significantly lower than Ovation and Clarity brackets (P < .01). The lowest frictional forces were produced by Mystique with Neo Clip, In-Ovation-C, and Damon 3 brackets with mean values of 1.59g, 8.33g, and 10.90 g, respectively. In-Ovation-C produced less FRS than Damon 3, but these differences were not statistically significant.
For the 0.018″ × 0.018″ SS esthetic coated (Spectra*) wire the Clarity bracket had the highest frictional forces (mean, 177.07g). The Ovation bracket produced the second-highest friction (mean, 121.49g). The lowest frictional forces were shown by Mystique with Neo Clip (mean, 0.72g), In-Ovation-C (mean, 1.94g), Damon 3 (mean, 2.29g), and In-Ovation-R (mean, 18.99g). The difference between the In-Ovation-R metal bracket and the Ovation bracket was statistically significant (P < .01).
Comparison by Wire Size and Mode of Ligation
The lowest mean frictional force was noted for the 0.020″ SS wire, and the highest mean frictional forces were demonstrated for the 0.019″ × 0.025″ SS wire. The 0.018″ × 0.018″ SS esthetic coated wire generally showed significantly higher friction (up to 2× to 5× greater) than the 0.020″ SS wires. Overall, ISL brackets showed significantly lower FRS whereas elastomeric ligation produced significantly higher FRS (with the exception of Mystique and NeoClip).
DISCUSSION
The elimination of elastomers and metal ligatures ties has dramatically improved chairside efficiency4,24 and the potential for good oral hygiene.6,25 Additionally, ISL brackets result in a gradual decreasing interactivity. Friction is produced from the time of initial archwire insertion, producing light, continuous forces optimal for biological tooth movement.4,5 It is important to note that other factors can affect friction.26
The Effect of Bracket Material, Wire Size, and Ligation Method on Kinetic Friction
The results presented here showed that significant differences were found between ISL esthetic and metal brackets. ISL and SL metal brackets produced similar, lower statistically significant kinetic FRS than CL brackets (P < .01). This is contrary to the conventionally accepted concept that all ceramic brackets have higher friction than metal brackets.
On preliminary observation, the CL ceramic brackets generally exhibited the highest frictional forces and these results agreed with several other studies.13,14,26–28 However, from a clinical perspective, the most significant finding was that an ISL bracket with an all-ceramic slot (In-Ovation-C) demonstrated lower friction than an interactive metal self-ligating (SL) bracket (In-Ovation-R). The similar Cr-Co clips within In-Ovation-C showed more freedom within the bracket body compared with In-Ovation-R. The reduction in the curved shape of the In-Ovation-C clip may have also resulted in lower seating forces, which appears to be related to lower friction. In-Ovation-C consistently demonstrated lower friction than a passive ISL bracket system (Damon 3). Random retesting of bracket-wire combinations confirmed these results.
The aforementioned two findings may be attributable to the new ceramic-injected molding technique that produced a smoother, glass-like slot in In-Ovation-C. Additionally, in clinical settings, a ceramic slot is free of the metal oxide micro-corrosions observed when the metal slots are exposed to saliva.29 The chamfers at the ends of the In-Ovation-C slot may have contributed to reduction in wire binding (Figure 1). In-Ovation-C also showed a smoother vertical slot, possibly allowing easier movement of the interactive clip during the initial light seating of the wire toward the slot base. With respect to direct comparisons of In-Ovation-C vs Damon 3, although the differences were not statistically significant at P = .01, In-Ovation-C consistently and for all the tested wires, produced lower FRS.
For control of tooth movement, some frictional resistance must be present. Low friction appears to meet this requirement ideally because it produces earlier rotational corrections and faster initial alignment compared with passive systems.4 In the middle stages of treatment, interactive friction is used during canine sliding retraction on 0.018″ or 0.020″ round SS to prevent distal rotation. In the final stage of treatment, active torque control is observed with the ISL brackets.30 Passive systems lack seating action on the archwire toward the base of the slot.30 Based on our testing and clinical observations, the realistic objective appears to be low interactive friction to seat the wire while producing light, continuous forces for optimal biological tooth movement.4 The corollary to this is that low interactive friction has the potential to optimize transeptal fiber pull during various tooth movements. From our empirical observations we suggest that the wire seating maximizes skeletal expansion, including after rapid maxillary expansion, when expanded archwires and headgear are applied.
It was expected that an increase in wire size dimension would produce higher frictional forces, as reported in several other studies.8,9,13,21,31,32 The 0.020″ SS wire was found to be associated with significantly lower levels of FRS followed by the 0.018″ × 0.018″ esthetic coated wire that may cause “nudging” dental movements.32 The standard deviations found in this friction investigation are consistent with other friction studies. The ISL esthetic and metal brackets generally produced approximately a 10-fold significantly lower frictional force compared with CL metal and esthetic brackets with elastomers on a 0.020″ SS. (Our findings support those of previous studies that found that metal SL brackets generated lower FRS than did CL metal and CL esthetic brackets.21,33,34)
CONCLUSIONS
The ISL brackets produced the lowest FRS irrespective of bracket material and wire size, whereas the CL brackets exhibited the highest frictional forces, except for Mystique with Neo Clip.
A ceramic ISL bracket In-Ovation-C showed lower friction than all brackets with metal slots tested.
The wire size associated with the least friction was 0.020″ round SS confirming its indication for ISL sliding biomechanics, followed by 0.018″ × 0.018″ SS esthetic coated and 0.019″ × 0.025″ SS wires.
REFERENCES
- 1.Keim R. G, Gottlieb E. L, Nelson A. H, Vogels D. S., III JCO study of orthodontic diagnosis and treatment procedures. Part 2: breakdowns of selected variables. J Clin Orthod. 2008;2008;42:609–710. [PubMed] [Google Scholar]
- 2.Pandis N, Polychronopoulou A, Eliades T. Self-ligating vs. conventional brackets in the treatment of mandibular crowding: a prospective clinical trial of treatment duration and dental effects. Am J Orthod Dentofacial Orthop. 2007;132:208–215. doi: 10.1016/j.ajodo.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 3.Miles P. G, Weyant R. J, Rustveld L. A clinical trial of Damon 2TM vs conventional twin brackets during initial alignment. Angle Orthod. 2006;76:480–485. doi: 10.1043/0003-3219(2006)076[0480:ACTODV]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Voudouris J. C. Interactive edgewise mechanisms: form and function comparison with conventional edgewise brackets. Am J Orthod Dentofacial Orthop. 1997;11:119–140. doi: 10.1016/s0889-5406(97)70208-7. [DOI] [PubMed] [Google Scholar]
- 5.Voudouris J. C. Flow Mechanics and Biological Tooth Movement. Excellence and Efficiency Interactive Twin Self-Ligation: Orthopedic-Muscle and Gnathological Biomechanics in Clinical Orthodontics. In: Kuftinec MM, editor. Toronto, On: ISL and Dentofacial Orthopedic Publications Co; 2007. pp. 13–17. [Google Scholar]
- 6.Voudouris J. C. Seven clinical principles of interactive twin mechanisms. J Clin Orthod. 1997;31:55–65. [PubMed] [Google Scholar]
- 7.Roth R. H. Five-year clinical evaluation of the Andrews' straight-wire appliance. J Clin Orthod. 1976;10:836–850. [PubMed] [Google Scholar]
- 8.Tidy D. C. Frictional forces in fixed appliances. Am J Orthod Dentofacial Orthop. 1989;96:249–254. doi: 10.1016/0889-5406(89)90462-9. [DOI] [PubMed] [Google Scholar]
- 9.Garner L. D, Allai W. W, Moore B. K. A comparison of frictional forces during simulated canine retraction of a continuous edgewise archwire. Am J Orthod Dentofacial Orthop. 1986;90:199–203. doi: 10.1016/0889-5406(86)90066-1. [DOI] [PubMed] [Google Scholar]
- 10.Andreasen G. F, Quevedo F. R. S. Evaluation of friction forces in the 0.022 × 0.028 edgewise bracket in vitro. J Biomech. 1970;3:151–160. doi: 10.1016/0021-9290(70)90002-3. [DOI] [PubMed] [Google Scholar]
- 11.Riley J. L, Garrett S. G, Moon P. C. Frictional forces of ligated plastic and metal edgewise brackets [abstract] J Dent Res. 1979;58:98. [Google Scholar]
- 12.Baker K. L, Nieberg L. G, Weimer A. D, Hanna M. Frictional changes in force values caused by saliva substitution. Am J Orthod Dentofacial Orthop. 1987;91:316–320. doi: 10.1016/0889-5406(87)90173-9. [DOI] [PubMed] [Google Scholar]
- 13.Pratten D. H, Popli K, Germane N, Gunsolley J. C. FRSS of ceramic and stainless steel orthodontic brackets. Am J Orthod Dentofacial Orthop. 1990;98:398–403. doi: 10.1016/S0889-5406(05)81647-6. [DOI] [PubMed] [Google Scholar]
- 14.Tselepis M, Brockhurst P, West V. C. The dynamic FRSS between orthodontic brackets and archwires. Am J Orthod Dentofacial Orthop. 1994;106:131–138. doi: 10.1016/s0889-5406(94)70030-3. [DOI] [PubMed] [Google Scholar]
- 15.Nicolls J. Frictional forces in fixed orthodontic appliances. Dent Pract. 1968;18:362–366. [PubMed] [Google Scholar]
- 16.Hain M, Dhopatkar A, Rock P. The effect of ligation method on friction in sliding mechanics. Am J Orthod Dentofacial Orthop. 2003;123:416–422. doi: 10.1067/mod.2003.14. [DOI] [PubMed] [Google Scholar]
- 17.Berger J. A. The influence of the SPEED bracket's self-ligating design on the force levels in tooth movement a comparative in vitro study. Am J Orthod Dentofacial Orthop. 1990;97:219–228. doi: 10.1016/S0889-5406(05)80055-1. [DOI] [PubMed] [Google Scholar]
- 18.Shivapuja P. K, Berger J. A. Comparative study of conventional ligation and self ligation bracket systems. Am J Orthod Dentofacial Orthop. 1994;106:472–480. doi: 10.1016/S0889-5406(94)70069-9. [DOI] [PubMed] [Google Scholar]
- 19.Echols P. M. Elastic ligatures binding forces and anchorage taxation. Am J Orthod. 1975;67:219–220. doi: 10.1016/0002-9416(75)90146-3. [DOI] [PubMed] [Google Scholar]
- 20.Baccetti T, Franchi L. Friction produced by types of elastomeric ligatures in treatment mechanics with the preadjusted appliance. Angle Orthod. 2006;76:211–216. doi: 10.1043/0003-3219(2006)076[0211:FPBTOE]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Thorstenson G. A, Kusy R. P. Resistance to sliding of self-ligating brackets versus conventional stainless steel twin brackets with second-order angulation in the dry and wet (saliva) states. Am J Orthod Dentofacial Orthop. 2001;120:361–370. doi: 10.1067/mod.2001.116090. [DOI] [PubMed] [Google Scholar]
- 22.Cha J-Y, Kim K-S, Hwang C-J. Friction of conventional and silica-insert ceramic brackets in various bracket-wire combinations. Angle Orthod. 2007;77:100–107. doi: 10.2319/092705-333R.1. [DOI] [PubMed] [Google Scholar]
- 23.Kusy R, Whitley J. FRSSs of metal-lined ceramic brackets versus conventional stainless steel brackets and development of 3-D friction maps. Angle Orthod. 2001;71:364–374. doi: 10.1043/0003-3219(2001)071<0364:FROMLC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Maijer R, Smith D. C. Time savings with self-ligating brackets. J Clin Orthod. 1990;24:29–31. [PubMed] [Google Scholar]
- 25.Forsberg C. M, Brattstrom V, Malmberg E, Nord C. E. Ligature wires and elastomer rings: two methods of ligation, and their association with microbial colonization of Streptococcus mutans and Lactobacilli. Eur J Orthod. 1991;13:416–420. doi: 10.1093/ejo/13.5.416. [DOI] [PubMed] [Google Scholar]
- 26.Braun S, Bluestein M, Moore B. K, Benson G. Friction in perspective. Am J Orthod Dentofacial Orthop. 1999;115:619–627. doi: 10.1016/s0889-5406(99)70286-6. [DOI] [PubMed] [Google Scholar]
- 27.Keith O, Kusy R. P, Whitley J. Q. Evaluation of zirconia brackets. Am J Orthod Dentofacial Orthop. 1994;106:605–614. doi: 10.1016/S0889-5406(94)70085-0. [DOI] [PubMed] [Google Scholar]
- 28.Kemp D. W. A Comparative Analysis of Frictional Forces between Self-ligating and Conventional Edgewise Orthodontic Brackets [thesis] 1992 Toronto, Canada: Department of Orthodontics, University of Toronto. [Google Scholar]
- 29.Matasa G. C. Attachment corrosion and its testing. J Clin Orthod. 1995;29:16–23. [PubMed] [Google Scholar]
- 30.Voudouris J. C, Kuftinec M. M, Bantleon H. P, Muhs S, A Perscheck. Selbsligierende Twin-Brackets [Teil I]—ist weniger mehr? Inf Orthod Kieferorthop. 2003;35:13–18. [Google Scholar]
- 31.Kapila S, Angolkar P. V, Duncanson M. G, Nanda R. S. Evaluation of friction between edgewise stainless steel brackets and orthodontic wires of four alloys. Am J Orthod Dentofacial Orthop. 1990;98:117–126. doi: 10.1016/0889-5406(90)70005-W. [DOI] [PubMed] [Google Scholar]
- 32.Kusy R. P, Whitley J. Q, Mayhew M. J, Buckthal J. E. Surface roughness of orthodontic arch wires via laser spectroscopy. Angle Orthod. 1988;58:33–45. doi: 10.1043/0003-3219(1988)058<0033:SROOA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 33.Pizzoni L, Ravnholt G, Melsen B. Frictional forces related to self-ligating brackets. Eur J Orthod. 1998;20:283–291. doi: 10.1093/ejo/20.3.283. [DOI] [PubMed] [Google Scholar]
- 34.Thorstenson G. A, Kusy R. P. Comparison of resistance to sliding between different self-ligating brackets with second order angulation in the dry and saliva states. Am J Orthod Dentofacial Orthop. 2002;121:472–482. doi: 10.1067/mod.2002.121562. [DOI] [PubMed] [Google Scholar]


