Abstract
Objective:
To test the null hypothesis that there is no difference in facial profile shape, malocclusion class, or palatal morphology in Malay adults with and without obstructive sleep apnea (OSA).
Materials and Methods:
Subjects were 120 adult Malays aged 18 to 65 years (mean ± standard deviation [SD], 33.2 ± 13.31) divided into two groups of 60. Both groups underwent clinical examination and limited channel polysomnography (PSG). The mean OSA and control values were subjected to t-test and the chi square test.
Results:
Physical examination showed that 61.7% of the OSA patients were obese, and 41.7% of those obese patients had severe OSA. The mean body mass index (BMI) was significantly greater for the OSA group (33.2 kg/m2 ± 6.5) than for the control group (22.7 kg/m2 ± 3.5; P < .001). The mean neck size and systolic blood pressure were greater for the OSA group (43.6 cm ± 6.02; 129.1 mm Hg ± 17.55) than for the control group (35.6 cm ± 3.52; 114.1 mm Hg ± 13.67; P < .001). Clinical examination showed that the most frequent findings among OSA groups when compared with the control group were convex profiles (71.7%), Class II malocclusion (51.7%), and V palatal shape (53.3%), respectively; the chi square test revealed a significant difference in terms of facial profile and malocclusion class (P < .05), but no significant difference in palatal shape was found.
Conclusion:
The null hypothesis is rejected. A convex facial profile and Class II malocclusion were significantly more common in the OSA group. The V palatal shape was a frequent finding in the OSA group.
Keywords: Facial profile, Malocclusion, Adult, Palatal, Sleep apnea, Malay, Asian
INTRODUCTION
Despite progress in the discovery of several aspects of obstructive sleep apnea (OSA) pathogenesis over the past 25 years, its origin remains undefinable.1 The pathophysiology of OSA involves factors that relate to the anatomic dimensions of the upper airway, upper airway resistance, and upper airway muscle activity during sleep.2
However, it seems that many factors, alone or in combination, can contribute to the development of OSA, and these factors may vary between individuals.3 For example, factors such as upper airway anatomy, pharyngeal muscle control, and central control of respiration may independently influence the likelihood of developing OSA.4
Alternatively, craniofacial factors and obesity were reported to play an important role in the pathogenesis of OSA; this was particularly significant in Asian patients.5 Patients with OSA manifest a spectrum of craniofacial abnormalities and obesity that appear to promote upper airway obstruction during sleep.6 The contributions of skeletal abnormalities vary among patients and between ethnic groups. For example, Asians have more pronounced skeletal abnormalities and are less obese than white subjects.7 As well, obesity and a dolicocephalic facial pattern were identified as the most significant risk factors in Japanese men.8 A retrospective review of Asian and white patients showed that Asian patients had maxillomandibular protrusion, a narrower cranial base angle, a larger posterior airway space, and a more superiorly positioned hyoid bone as compared with white patients.9
However, clinical assessment alone is not sufficient to obtain an accurate diagnosis of OSA.10 It has been reported that when sleep experts based their diagnosis on history and examination alone, 50% of cases were wrongly diagnosed.11 Therefore, a range of mathematical formulas and models for the clinical prediction of OSA were developed. These models used body mass index, neck circumference, oxygen saturation, witnessed apneas, questionnaire data, and oral cavity measurements.12–14
Nevertheless, published literature regarding facial profile shape, malocclusion class, and palatal morphology and its association with OSA is minimal, especially in comparison with numerous articles describing the clinical and physical features of patients with OSA. Therefore, the aim of this study is to test the null hypothesis that no morphologic differences in terms of facial profile shape, malocclusion class, and palatal shape are present in adult Malays with and without OSA. Rejection of the null hypothesis might improve our understanding of the origin of OSA disorders in patients of diverse ethnicity.
MATERIALS AND METHODS
This multidisciplinary study took place in an otorhinolaryngology-head and neck surgery (ORL-HNS) clinic, Hospital Universiti Sains Malaysia (HUSM). After informed consent was obtained and the study was approved at the institutional level, 128 subjects were recruited for this study. However, only 120 subjects were able to complete sleep studies and clinical examinations (eight patients were unable to complete the sleep studies because of time constraints, as they were living out of town). A comparative, cross-sectional study design was employed. Inclusion criteria included age over 18 years, a diagnosis confirmed by limited polysomnography (PSG), and the presence of at least six teeth in each maxillary and mandibular arch, respectively. Exclusion criteria consisted of the presence of psychiatric illness, sedative and/or alcohol intake, patient-specific disorders (such as neuromuscular disorders), any craniofacial deformity (such as cleft lip and/or palate), and lack of informed consent or willingness to participate in the study.
The study sample was divided into two groups. The first group consisted of 60 patients with OSA diagnosed with limited PSG. The second group consisted of 60 healthy, non-OSA control subjects who did not have any apneic symptoms as evaluated by the attending physician and limited PSG. Both groups included in the study consisted of randomly selected subjects from ORL-HNS and the orthodontic clinic. In addition, individual nurses, medical/dental students, and university staff were asked to seek volunteers for the study. Each patient's age, sex, height, and weight was recorded. Body mass index (BMI) was calculated from the patient's height and weight in standard units (kg/m2), and neck circumference (NC) was measured at the level of the thyroid cartilage.
Assessment of Facial Profile Shape
The patient's facial profile was assessed by viewing the superficial facial features from the subject's left side while the subject was sitting in a comfortable upright position. The profile was assessed by joining the following two reference lines: a line joining the forehead and the soft tissue point A (deepest point in the curvature of upper lip), and a line joining point A and the soft tissue pogonion (most anterior point of the chin).15 Based on the relationship between these two lines, three facial profile shapes were recorded: a straight profile when the two lines form a nearly straight line, a convex profile when the two lines form an angle with concavity facing the tissue, and a concave profile when the two lines form an angle with convexity toward the tissue.15
Assessment of Malocclusion Class
Malocclusions were classified based on the British Standards Institute classification of incisor relationship.16 The categories defined by the British Standards Institute classification, which was used by the author and confirmed by a consultant orthodontist, are as follows: Class I malocclusion, when the lower incisor edges occlude with or lie immediately below the cingulum plateau of the upper central incisors; Class II malocclusion, when the lower incisor edges lie posterior to the cingulum plateau of the upper incisors (Class II subdivisions were combined because of the infrequent appearance of Class II division 2 in study subjects); and Class III malocclusion, when the lower incisor edges lie anterior to the cingulum plateau of the upper incisors.
Assessment of Palatal Morphology
Palatal morphology was investigated with the use of direct visualization while the patient was seated with the Frankfurt plane in a horizontal position. The shapes of the palate were classified as either “V” shape (narrow maxilla) or normal “U” shape.
Sleep Study
An overnight hospital type III sleep study was performed on each subject between 22:00 pm and 06:00 am. All variables were recorded with a portable diagnostic device (Embletta, Somnologica, Iceland) at the HUSM Sleep Science Laboratory. This device has been reported to be suitable for use both in hospitals and at home,17 and it has been validated against full PSG.18 The severity of OSA was classified according to the Apnea-Hypopnea Index (AHI) as mild (5 to 15/ h), moderate (15 to 30/h), or severe (>30/h). The control group included subjects whose AHI ranged from 0 to 4/h. Full details of the sleep study for the same group of patients can be found elsewhere.6,19
RESULTS
Table 1 shows the demographic profile of 120 subjects classified according to age and sex. The control group included 37 females and 23 males. The OSA group included 26 females and 34 males. According to gender and OSA severity, 9 patients were mild (3 males; 6 females), 17 patients were moderate (8 males; 9 females), and 34 patient were severe (23 males; 11 females; Table 2). Physical examination findings show that 61.7% of OSA patients were obese, and 41.7% of those obese patients had severe OSA (Table 3).
Table 1. .
Distribution of Study Subjects According to Age and Sexa
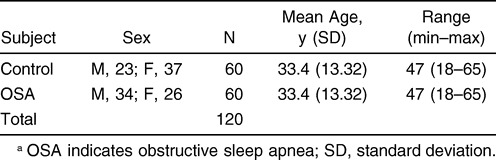
Table 2. .
Distribution of Study Subjects According to Gender and OSA Severitya
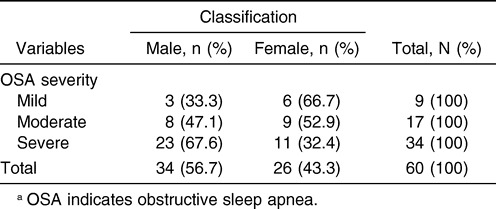
Table 3. .
Distribution of Study Subjects According to BMI and OSA Severitya
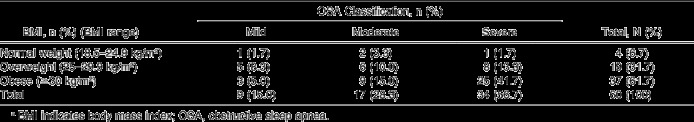
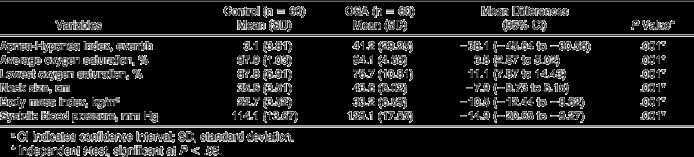
Table 4 shows the limited channels of PSG data and physical examination findings. PSG data show that the mean AHI was significantly greater for the OSA group (41.2/h ± 29.2) than for the control group (3.1/h ± 3.8; P < .001). As well, the average oxygen saturation and the lowest oxygen saturation were significantly lower for the OSA group (94.1% ± 4.6, 76.7% ± 10.8) than for the control group (97.9% ± 1.0, 87.8% ± 6.9; P < .001), respectively. Accordingly, the mean BMI was found to be significantly greater for the OSA group (33.2 kg/m2 ± 6.5) than for the control group (22.7 kg/ m2 ± 3.5; P < .001). In addition, the mean neck size and the systolic blood pressure were greater for the OSA group (43.6 cm ± 6.02; 129.1 mm Hg ± 17.55) than for the control group (35.6 cm ± 3.52; 114.1 mm Hg ± 13.67; P < .001). These results are summarized in Table 4.
Table 4. .
Polysomnography and Physical Examination Findingsa
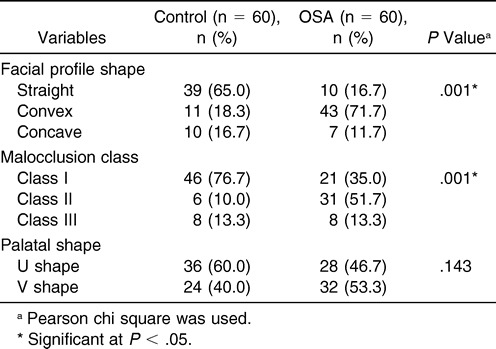
Clinical examination shows that the most frequent finding among OSA groups when compared with the control group were convex profiles (71.7%), Class II malocclusion (51.7%), and V palatal shape (53.3%), respectively; the chi square test revealed a significant difference among the facial profile and malocclusion class (P < .05), but no significance was found in terms of palatal shape. These results are summarized in Table 5.
Table 5. .
Clinical Observation of Facial Profile, Malocclusion Class, and Palatal Shape Variables
DISCUSSION
Results of this study indicate that OSA is more common in men (56.7%), and that men have a more severe type of OSA (67.6%) than women (32.4%). The results of this study are in line with the well-known Wisconsin Sleep Cohort study, which estimated the prevalence of OSA in men as almost three times higher than that in women.20 The reason for the higher prevalence of OSA in men is not completely understood. However, it may reflect the differences between men and women in bony configuration, fat deposition, and soft tissue structures that make the male upper airway more susceptible to collapse.21
The results of this current study also indicate that BMI and neck girth are significantly greater for the OSA group than for the control group. These findings support the view that obesity is one significant risk factor for Malay OSA patients that is in good agreement with findings obtained in the Chinese5 and Japanese populations.8
Clinical examination findings indicate that convex profiles, Class II malocclusion, and V shape palatal arch were the most frequent features among Malay OSA patients. It has been found that Japanese adults and children with OSA possess dolico facial patterns (long facial type) with retruded mandibles on Rickett's analysis.22 However, this facial pattern was noted at a lesser degree in children than in adults.23 Furthermore, the dolico facial pattern and obesity seen in Japanese men were the most important risk factors for OSA patients.8
The difference between our results and the above cited results is seen in two aspects. First, both reports used a cephalometric Rickett's type of analysis. According to this analysis, three facial patterns are seen: brachyo facial pattern (short face), mesio facial type (medium face), and dolico facial pattern (long face).22 In our study, we used a facial divergence sort of observation, and we classified subjects as having a straight, convex, or concave profile. Second, we do not know whether this type of facial profile can be considered a risk factor for OSA in Malay patients, and it is beyond the objective of the present study to determine this. However, it remains a promising area for future study.
On the other hand, the current study also found that Class II malocclusion was the most striking finding in the OSA group. Similarly Zonato et al24 examined 220 Brazilian OSA patients and reported that retrognathism was detected in 19.7% of patients, and Class II dental occlusion was observed in 26.3% of patients. One explanation for why OSA patients get this type of malocclusion could involve head position. As a compensation mechanism for a narrow airway, many OSA patients try to extend their head, and this may affect the mandibular rest position and cause retrusion of the mandible. As a result, prolonged head extension may be associated with development of a Class II malocclusion.25
In this current study, the palatal shape of Malay subjects was classified as normal U shape or narrow V shape. The V palatal shape was included as one predictive morphometric model for OSA,14 and the model illustrates the potential value of physical and dental examination.26
Using dental examination, we found that 53.3% of OSA patients presented with a V shape palatal arch, even though the chi square revealed no significance in terms of palatal shape.
However, for palatal size, we previously found that those patients with OSA had significantly narrower maxillary and mandibular arch widths with an increase in maxillary and mandibular arch length when compared with control subjects.19
In view of the fact that the roof of the mouth is also the floor of the nose, a narrow arch can infringe on the nasal cavity space. Therefore, maxillary dimensions, in addition to vascular and soft tissue factors, were reported as important for determining nasal airway properties.27 Besides contributing to high nasal resistance, maxillary constriction can contribute to lateral narrowing of the upper oral cavity and a low tongue posture, which consequently narrow the retroglossal region.28 This may provide a reasonable explanation for the narrowing of the posterior airway space seen in OSA patients.
In view of this contention, we believe that the clinical and morphologic features used in this study are good for developing clinical prediction formulae and prioritizing Malay OSA patients for PSG. In addition, because most Malay OSA subjects in this study tended to have a convex type of facial divergence, we suspect that the convex type of facial profile may be explained by a shorter anterior cranial base,29 reflecting their smaller anteroposterior facial dimensions. Thus, when the present results are taken into consideration, it may be necessary to apply somewhat modified treatment goals in obese orthodontic OSA patients. For instance, if the clinician were considering extraction-based therapy in those patients, less effect might be seen on the profile and on lip support.30
The current study could not overcome some methodologic limitations. First, generalization of the results to a larger population is limited because the sample subjects were care-seeking volunteers at a hospital clinic. This source of study subjects could introduce a potential selection bias into the investigation, making our results more applicable to hospital populations than to the general public. Second, this study examined patients with OSA during wakefulness. Nevertheless, abnormalities of upper airway anatomy and physiology in subjects with OSA during wakefulness have been clearly documented31 and still may provide some valuable information. Third, although every attempt was made to match patients with OSA and to control subjects for age and BMI, the OSA group was somewhat older and more obese. We believe these differences may explain the presence of OSA in this group of patients but did not affect our observations in terms of any differences noted on clinical examination.28 Fourth, the present study was based on single-night limited PSG, which may lead to underdiagnosis for some mild sleep apnea patients. Nevertheless, some studies failed to find differences in AHI between single- and two-night PSG in adults.32 With the disability associated with OSA patients and the global cost of PSG, a single night can still provide a valid diagnosis. Finally, generalization of the present results to different ethnicities, including other Malaysian populations, is limited because ethnic Malays may have unique craniofacial features. Additional studies are needed to find the best combination of anatomic, dental, and other clinical landmarks related to OSA.
CONCLUSIONS
Differences in facial profile shape and malocclusion class were observed in Malay adults with and without obstructive sleep apnea (OSA). A convex facial profile and Class II malocclusion were significantly more common in the OSA group. The V palatal shape was a frequent finding in the OSA group.
Acknowledgments
This study was funded by a short-term grant (304 PPSP 6131489), Universiti Sains Malaysia.
REFERENCES
- 1.Ryan C. M, Bradley T. D. Pathogenesis of obstructive sleep apnea. J Appl Physiol. 2005;99:2440–2450. doi: 10.1152/japplphysiol.00772.2005. [DOI] [PubMed] [Google Scholar]
- 2.Hudgel D. W. The role of upper airway anatomy and physiology in obstructive sleep apnea. Clin Chest Med. 1992;13:383–398. [PubMed] [Google Scholar]
- 3.Friedman M, Tanyeri H, La Rosa M et al. Clinical predictors of obstructive sleep apnea. Laryngoscope. 1999;109:1901–1907. doi: 10.1097/00005537-199912000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Jordan A. S, White D. P, Fogel R. B. Recent advances in understanding the pathogenesis of obstructive sleep apnea. Curr Opin Pulm Med. 2003;9:459–464. doi: 10.1097/00063198-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Hou H. M, Hägg U, Sam K et al. Dentofacial characteristics of Chinese obstructive sleep apnea patients in relation to obesity and severity. Angle Orthod. 2006;76:962–969. doi: 10.2319/081005-273. [DOI] [PubMed] [Google Scholar]
- 6.Banabilh S. M, Suzina A. H, Dinsuhaimi S, Samsudin A. R, Singh G. D. Craniofacial obesity in patients with obstructive sleep apnea. Sleep Breath. 2009;13:19–24. doi: 10.1007/s11325-008-0211-9. [DOI] [PubMed] [Google Scholar]
- 7.Li K. K, Kushida C, Powell N. B, Riley R. W, Guilleminault C. Obstructive sleep apnea syndrome: a comparison between Far-East Asian and white men. Laryngoscope. 2000;110:1689–1693. doi: 10.1097/00005537-200010000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Kubota Y, Nakayama H, Takada T et al. Facial axis angle as a risk factor for obstructive sleep apnea. Intern Med. 2005;44:805–810. doi: 10.2169/internalmedicine.44.805. [DOI] [PubMed] [Google Scholar]
- 9.Li K. K, Powell N. B, Kushida C, Riley R. W, Adornato B, Guilleminault C. A comparison of Asian and white patients with obstructive sleep apnea syndrome. Laryngoscope. 1999;109:1937–1940. doi: 10.1097/00005537-199912000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Schlosshan D, Elliott M. W. Sleep. 3: Clinical presentation and diagnosis of the obstructive sleep apnoea hypopnoea syndrome. Thorax. 2004;59:347–352. doi: 10.1136/thx.2003.007179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Viner S, Szalai J. P, Hoffstein V. Are history and physical examination a good screening test for sleep apnea? Ann Intern Med. 1991;115:356–359. doi: 10.7326/0003-4819-115-5-356. [DOI] [PubMed] [Google Scholar]
- 12.Rauscher H, Popp W, Zwick H. Model for investigating snorers with suspected sleep apnoea. Thorax. 1993;48:275–279. doi: 10.1136/thx.48.3.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoffstein V, Szalai J. P. Predictive value of clinical features in diagnosing obstructive sleep apnea. Sleep. 1993;16:118–122. [PubMed] [Google Scholar]
- 14.Kushida C. A, Efron B, Guilleminault C. A predictive morphometric model for the obstructive sleep apnea syndrome. Ann Intern Med. 1997;127:581–587. doi: 10.7326/0003-4819-127-8_part_1-199710150-00001. [DOI] [PubMed] [Google Scholar]
- 15.Rakosi T, Jonas I, Graber T. M. New York, NY: Thieme Medical; 1993. Orthodontic Diagnosis. [Google Scholar]
- 16.Mitchell L. New York, NY: Oxford University Press Inc; 2007. Introduction to Orthodontics. 3rd ed. [Google Scholar]
- 17.Dingli K, Coleman E. L, Vennelle M et al. Evaluation of a portable device for diagnosing the sleep apnoea/hypopnoea syndrome. Eur Respir J. 2003;21:253–259. doi: 10.1183/09031936.03.00298103. [DOI] [PubMed] [Google Scholar]
- 18.Skinner M. A, Choudhury M. S, Homan S. D, Cowan J. O, Wilkins G. T, Taylor D. R. Accuracy of monitoring for sleep-related breathing disorders in the coronary care unit. Chest. 2005;127:66–71. doi: 10.1378/chest.127.1.66. [DOI] [PubMed] [Google Scholar]
- 19.Banabilh S. M, Suzina A. H, Dinsuhaimi S, Samsudin A. R, Singh G. D. Dental arch morphology in south-east Asian adults with obstructive sleep apnoea: geometric morphometrics. J Oral Rehabil. 2009;36:184–192. doi: 10.1111/j.1365-2842.2008.01915.x. [DOI] [PubMed] [Google Scholar]
- 20.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 21.Malhotra A, Huang Y, Fogel R. B et al. The male predisposition to pharyngeal collapse: importance of airway length. Am J Respir Crit Care Med. 2002;166:1388–1395. doi: 10.1164/rccm.2112072. [DOI] [PubMed] [Google Scholar]
- 22.Kikuchi M, Higurashi N, Miyazaki S, Itasaka Y. Facial patterns of obstructive sleep apnea patients using Ricketts' method. Psychiatry Clin Neurosci. 2000;54:336–337. doi: 10.1046/j.1440-1819.2000.00703.x. [DOI] [PubMed] [Google Scholar]
- 23.Kikuchi M, Higurashi N, Miyazaki S, Itasaka Y, Chiba S, Nezu H. Facial pattern categories of sleep breathing-disordered children using Ricketts analysis. Psychiatry Clin Neurosci. 2002;56:329–330. doi: 10.1046/j.1440-1819.2002.01002.x. [DOI] [PubMed] [Google Scholar]
- 24.Zonato A. I, Bittencourt L. R, Martinho F. L, Junior J. F, Gregorio L. C, Tufik S. Association of systematic head and neck physical examination with severity of obstructive sleep apnea-hypopnea syndrome. Laryngoscope. 2003;113:973–980. doi: 10.1097/00005537-200306000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Pirila K, Tahvanainen P, Huggare J, Nieminen P, Lopponen H. Sleeping positions and dental arch dimensions in children with suspected obstructive sleep apnea syndrome. Eur J Oral Sci. 1995;103:285–291. doi: 10.1111/j.1600-0722.1995.tb00028.x. [DOI] [PubMed] [Google Scholar]
- 26.Schellenberg J. B, Maislin G, Schwab R. J. Physical findings and the risk for obstructive sleep apnea: the importance of oropharyngeal structures. Am J Respir Crit Care Med. 2000;162:740–748. doi: 10.1164/ajrccm.162.2.9908123. [DOI] [PubMed] [Google Scholar]
- 27.Cistulli P. A, Richards G. N, Palmisano R. G, Unger G, Berthon-Jones M, Sullivan C. E. Influence of maxillary constriction on nasal resistance and sleep apnea severity in patients with Marfan's syndrome. Chest. 1996;110:1184–1188. doi: 10.1378/chest.110.5.1184. [DOI] [PubMed] [Google Scholar]
- 28.Seto B. H, Gotsopoulos H, Sims M. R, Cistulli P. A. Maxillary morphology in obstructive sleep apnoea syndrome. Eur J Orthod. 2001;23:703–714. doi: 10.1093/ejo/23.6.703. [DOI] [PubMed] [Google Scholar]
- 29.Banabilh S. M, Suzina A. H, Dinsuhaimi S, Singh G. D. Cranial base and airway morphology in adult Malays with obstructive sleep apnoea. Aust Orthod J. 2007;23:89–95. [PubMed] [Google Scholar]
- 30.Neeley W. W. I. I, Gonzales D. A. Obesity in adolescence: implications in orthodontic treatment. Am J Orthod Dentofacial Orthop. 2007;131:581–588. doi: 10.1016/j.ajodo.2006.03.028. [DOI] [PubMed] [Google Scholar]
- 31.Pack A. I. Advances in sleep-disordered breathing. Am J Respir Crit Care Med. 2006;173:7–15. doi: 10.1164/rccm.200509-1478OE. [DOI] [PubMed] [Google Scholar]
- 32.Marzec M. L, Selwa L. M, Malow B. A. Analysis of the first night effect and sleep parameters in medically refractory epilepsy patients. Sleep Med. 2005;6:277–280. doi: 10.1016/j.sleep.2005.01.002. [DOI] [PubMed] [Google Scholar]


