Abstract
Objective:
To describe levels of loneliness in cancer caregivers over a 6 month time period, and to examine factors that influence changes in loneliness in caregivers over time.
Methods:
Prospective, repeated measures design was utilized to examine levels of loneliness and factors that influence loneliness in 129 family caregivers of individuals undergoing cancer treatment at three time points over a 6 month period. Measures included: PROMIS global health and sleep disturbance; NIH Toolbox loneliness, self-efficacy and perceived stress; Family Care Inventory mutuality scale; and Caregiver Reaction Assessment.
Results:
Approximately one third (30.2%, n = 39) of the caregivers had high levels of loneliness, and levels of loneliness did not change over the three time points (P = .985). For any given time point, caregivers who were not married (P = .008), not working (P = .027), with worse mental health (P = .015), more perceived-stress (P < .0001), and more caregiver burden (P = .003) reported higher levels of loneliness.
Conclusion:
This study provides guidance for clinicians attempting to identify at-risk caregivers by confirming the findings of previous research that caregivers with higher burden, stress and in poor mental health are at increased risk for loneliness. This study provides preliminary evidence that continuing to work during the caregiving trajectory may be beneficial to caregivers by reducing levels of loneliness. Future research is needed to confirm these findings and to examine novel interventions to reduce loneliness in cancer caregivers.
Keywords: cancer, caregiving, employment, loneliness, oncology, psycho-oncology
1 ∣. BACKGROUND
In 2015, an estimated 43.5 million adults in the United States served as an unpaid caregiver within the previous 12 months.1 Caregiving for a family member or friend with a chronic illness such as cancer entails the provision of emotional and physical support and may include a range of responsibilities including maintaining the home, preparing meals, administering medications, tending to medical needs, and coordinating medical care.2 Possibly because of the time demands of providing such care, caregivers often report feeling isolated from their usual support networks.3 This is problematic, because the stress of caregiving is associated with higher levels of caregiver burden and potential deterioration in physical and mental health,4,5 all of which may be improved with emotional support.6
Loneliness, an unpleasant psychological state associated with an unsatisfactory discrepancy between desired and achieved social relationships, can be debilitating.7 Social interaction is critical for health and well-being, as the quantity of social support and the quality of social relationships are important predictors of health.8 Social isolation is considered a form of “chronic stress” that is associated with cardiovascular disease, inflammation and impaired immune system function.9 Social isolation is the objective physical separation from other people, while loneliness is the subjective perception of being isolated or alone.7 The two are similar, but conceptually different, as it's possible to feel lonely while among other people, and one can be alone yet not feel lonely. Like social isolation, loneliness increases the risk of morbidity10,11 and all-cause mortality,12 comparable to the health risks associated with obesity13 or smoking up to 15 cigarettes a day.14
Caregivers report that the care recipient becomes their primary focus, and caregiving sometimes necessitates that caregivers withdraw from their normal activities and become isolated from their previous support systems.3 However, little research has examined loneliness in cancer caregivers to date. Identifying caregivers at risk for loneliness and understanding the factors that contribute to loneliness in cancer caregivers may guide interventions to enhance social connectedness and thereby reduce the negative effects of caregiving on caregiver's emotional and physical health. The purpose of this study is to describe levels of loneliness in cancer caregivers over a 6 month time period, and to examine factors that influence changes in loneliness in caregivers over time.
1.1 ∣. Research regarding loneliness in caregivers
Much of the research examining loneliness in caregivers has focused on caregivers of the elderly or individuals with dementia.15 In caregivers of the elderly and those with dementia, loneliness has been found to positively predict caregiver burden.16,17 In a review of 19 cancer caregiving studies, low social support was considered a hidden morbidity of caregiving, particularly for females.18 Surprisingly little is known about loneliness in cancer caregivers, although qualitative studies have provided rich details about the isolation and withdrawal from support systems that may occur during cancer caregiving.19-21 A few quantitative studies have provided some insight regarding loneliness in cancer caregivers, although loneliness was rarely the primary outcome examined. In a cross-sectional survey of 180 cancer caregivers, loneliness was an important predictor of fear of cancer recurrence.22 Segine et al found that higher levels of loneliness in breast cancer caregivers were associated with lower caregiver quality of life.23
Only two research studies, both cross-sectional, examined levels of loneliness as a primary outcome in cancer caregivers24,25 Sahin and Tan (2011) found that lower levels of social support and higher levels of depression were correlated with higher levels of loneliness in individuals with cancer and their caregivers24; interestingly, while both cancer patients and their caregivers experienced high levels of loneliness (n = 42, 70% and n = 38, 62%, respectively), caregivers reported significantly lower levels of family social support than did patients. Another study found that caregivers who were female, unmarried, less educated, and who were caring for terminally ill individuals had significantly higher levels of loneliness than did caregivers who were male, married, more educated, and caring for individuals who had advanced cancer25; the researchers also found levels of anxiety and depression to be significantly correlated with loneliness in all caregivers.
The research published to date has provided some insight into factors that influence levels of loneliness in caregivers in general, but there is a surprising paucity of research examining loneliness and its influencing factors in cancer caregivers. All of the studies examining loneliness in cancer caregivers known to us have utilized cross-sectional rather than longitudinal methodology.
2 ∣. METHODS
2.1 ∣. Study design
A prospective, repeated measures design was utilized to collect information about levels of loneliness and factors that influence loneliness in family caregivers of individuals beginning a new cancer treatment at the National Institutes of Health (NIH) Clinical Center over three time points: study enrollment (±14 days of the start of the patient's treatment) and three and 6 months after enrollment. Understanding the experience of caregivers during the trajectory of cancer care guided the study design. This included a variety of treatment settings (eg, inpatient, outpatient) and the impact of time, which could contribute to the caregiver's experience. The study took place between March 2014 and July 2016 and was part of a previously-published study assessing symptoms in cancer caregivers.26 All procedures performed in this study involving human participants were in accordance with the ethical standards of the NHLBI IRB (NCT01981538) and the U.S. Federal Policy for the Protection of Human Subjects.
2.2 ∣. Study population
Adults (>18 years) serving as an active caregiver for a NIH Clinical Center patient beginning cancer treatment (±14 days), having online/web access, and who were literate in English or Spanish were eligible to participate (Figure 1). Cancer patients preliminarily were assessed to determine if they were supported by an active caregiver during their treatment, defined as someone who would be providing emotional and/or physical support for at least 6 months during cancer treatment. Caregivers who were identified by the patient as being eligible and interested were subsequently recruited. Written informed consent was obtained from all participants prior to initiating any study procedures or data collection.
FIGURE 1.
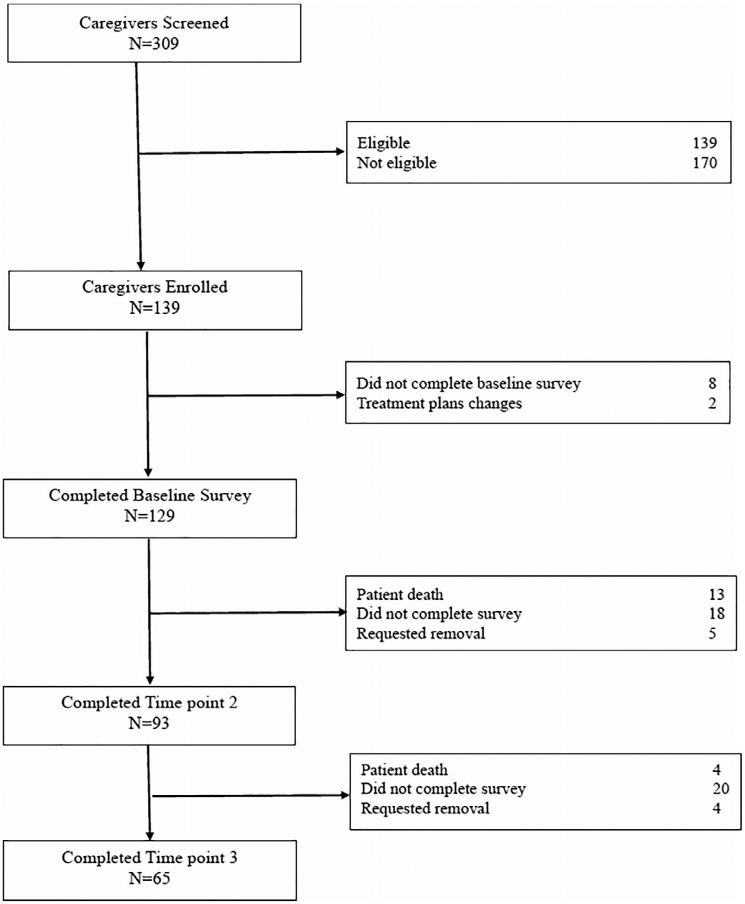
Diagram of enrollment and participation
Caregivers completed the initial online questionnaire within 1 week of study enrollment. For subsequent time points, caregivers were contacted by phone and/or email within ±2 weeks to remind them that their surveys were due. Subjects were removed from study if not able to complete the survey within 2 weeks of the due date.
2.3 ∣. Measures
2.3.1 ∣. Caregiver characteristics
The following self-report information was collected: age, caregiving hours per week, caregiver role (sole caregiver vs part of a caregiving team, and “double duty” caregiving for another individual in addition to the individual with cancer vs caring exclusively for the individual with cancer), education level, sex, employment status, income, living situation (lives with/apart from the patient, local vs distant [>100 miles] location) from NIH, marital status, race, and relationship to patient (spouse, parent, child, friend/other).
2.3.2 ∣. Patient characteristics
Patient information was obtained via hospital records including: age, cancer diagnosis, sex, hospital status (inpatient vs outpatient), patient type (pediatric/adult), and treatment type.
2.3.3 ∣. PROMIS and NIH Toolbox measures
The Patient-Reported Outcomes Measurement Information System (PROMIS) global physical/mental health and sleep disturbance, and NIH Toolbox loneliness, self-efficacy and perceived stress were used in analyses. PROMIS and NIH Toolbox are well-validated and reliable measures of self-reported health outcomes.27,28 Both generate T-scores, standardized scores that are normed to the general population with a mean of 50 and a standard deviation (SD) of 10. Individual items are rated using a five-point Likert scale, with higher scores indicative of higher levels of the concept, which can be positive (self-efficacy, physical/mental health) or negative (sleep disturbance, perceived stress, loneliness). NIH Toolbox loneliness was measured using a five-item fixed form, and PROMIS global physical and mental health were measured using an eight-item questionnaire. All other measures were delivered using Computer Adaptive Testing (CAT).
2.3.4 ∣. Family care inventory mutuality
The family care inventory (FCI) mutuality scale measures the strength of the relationship between the caregiver and patient, as self-reported by the caregiver.29 Originally developed for use in the elderly, it has been used in cancer populations as well.30,31 The 15-item scale addresses the relationship dimensions of love, reciprocity, shared pleasurable activities, and shared values between the care recipient and the caregiver. The measure uses a four-point Likert scale, with higher scores reflective of a better caregiver-patient relationship. The total mutuality score is the mean of all items in the scale, ranging from 0.0 to 4.0. In this study, the scale demonstrated a Cronbach's alpha of .95.
2.3.5 ∣. Caregiver reaction assessment
The Caregiver Reaction Assessment (CRA) is a 24-item self-administered scale that measures the positive and negative effects of caregiving in five domains: caregiver esteem, impact on finances, impact on health, impact on schedule, and lack of family support.32 This measure is a valid and reliable tool for use in caregivers of cancer patients.33 Responses are rated using a five-point Likert scale. The total mean score was used in analyses, (range = 1-5), after reversing self esteem questions, with higher total mean scores indicating greater caregiver burden. This instrument demonstrated a Cronbach's alpha of .86 in this study.
2.3.6 ∣. Health-promoting lifestyle behaviors-II
The health-promoting lifestyle behaviors-II (HPLP-II) is a 52-item questionnaire that assesses self-reported frequencies of current participation in health-promoting behaviors including: health responsibility (attending to/taking responsibility for one's own health), interpersonal support, nutrition, physical activity, spirituality, and stress management.34
Responses are rated using a four-point Likert scale (1 = never, 4 = routinely). The total score is the mean of all items in the scale and ranges from 0.0 to 4.0; higher scores indicate more engagement in health-promoting behaviors. Cronbach's alpha for this study was .94.
2.4 ∣. Statistical analyses
The distributions of all variables at each time-point were examined and appropriate descriptive statistics were computed (eg, mean and standard deviation [SD] for continuous variables and frequency and percentage for categorical variables). Baseline bivariate relationships were analyzed between all factors with loneliness by parametric and non-parametric tests (Chi-square test, Fisher's exact test, t test, or Wilcoxon signed rank test). A Three-level linear mixed model, based on full maximum likelihood (ML) estimation, was used to analyze the within-caregiver (level 1), between-caregiver (level 2), and between-patient (level 3) changes in loneliness scores over three time-points. Time point was treated as a categorical variable. First, unconditional models with and without time effect were built to estimate level 1, level 2, and level 3 variance components. Then, each time-invariant (caregiver age, sex, race/ethnicity, time in United States, location, education, relationship to patient, caregiving length, patient age, sex) and time-varying (income, work status, marital status, caregiving role, living status, caregiving hours, double-duty caregiving, hospital status, treatment type, PROMIS/NIH Toolbox T scores, and total scores for Mutuality, CRA, and HPLP-II) covariate was tested one-by-one to see whether it was a significant predictor of loneliness, as were time interactions. Finally, all the variables which were significant in the individual models were tested in the final model, and the forward stepwise method was used to select the predictors in the final model with entering criteria of 0.05 and removing criteria of 0.10. Aikake information criterion (AIC) and Bayesian information criterion (BIC) were used to compare and select models. Based on previous research, sex was controlled for in the final model. All data analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, North Carolina) or IBM SPSS Statistics (IBM Corp., Armonk, New York). A P < .05 was considered significant.
3 ∣. RESULTS
Of 309 caregivers screened, 129 were eligible and completed the survey at baseline, 93 at 3 months, and 69 at 6 months (Figure 1). Caregivers of adults (vs pediatric) were more likely to be completers at time points two and three; no other differences were noted between completers and non-completers. Descriptive characteristics and baseline outcomes are shown in Tables 1 and 2, respectively. Caregivers were predominantly female (67.4%, n = 87), non-Hispanic/white (71.1%, n = 91) and educated, with 61.2% (n = 79) having a bachelor's degree or higher. The types of cancers varied, with 62.2% (n = 67) of care recipients receiving biotherapies/immunotherapies (Table 1); nearly all were inpatient at baseline (87.3%, n = 107) and outpatient at time points two (88.2%, n = 82) and three (92.3%, n = 60). Mean levels of loneliness for this sample were within .5 SD of those levels found in the general population at all three time points (m = 54 ± 10.7, 53.9 ± 11.8, and 54.7 ± 11.4, respectively). However, 30.2% (n = 39) of the caregivers had baseline loneliness T scores considered “high” (≥60), more than twice the 15% prevalence of high levels of loneliness found in the general population.35 Based on the unconditional model, loneliness levels did not change over the three time points (P = .985). In the final model (Table 3), for any given time point, caregivers who were not married (P = .008), not working (P = .027), with worse mental health (P = .015), more perceived-stress (P < .0001), and more caregiver burden (P = .003) reported higher levels of loneliness.
TABLE 1.
Baseline demographic and descriptive characteristics of caregivers and patients
| Caregiver characteristics (n = 129) | Mean (SD) | Range |
|---|---|---|
| Age (years) | 48.6 (11.8) | 20 to 76 |
| Median | Range | |
| Months of Caregiving (n = 121) | 18.0 | 0.3 to 276 |
| n | % | |
| Sex | ||
| Female | 87 | 67.4 |
| Race and ethnicity (n = 128) | ||
| White and non-Hispanic | 91 | 71.1 |
| Non-White and Non-Hispanic | 18 | 14.1 |
| Hispanic/Latino | 19 | 14.8 |
| Education level | ||
| High School Graduate or below | 7 | 5.4 |
| Some College or Associate's Degree | 43 | 33.4 |
| Bachelor's Degree | 35 | 27.1 |
| Postgraduate Degree and above | 44 | 34.1 |
| Annual Household Income | ||
| <$50 000 | 35 | 27.6 |
| $50 000 to $89 000 | 32 | 25.2 |
| >$89 000 | 60 | 47.2 |
| Employment status | ||
| Full time | 74 | 57.4 |
| Part time | 21 | 16.3 |
| Not currently employed | 34 | 26.4 |
| Change in employment status | ||
| Yes | 65 | 50.4 |
| Left employment | 16 | 12.4 |
| Work fewer hours | 25 | 19.4 |
| Work more hours | 3 | 2.3 |
| Leave of absence | 21 | 16.3 |
| Marital status | ||
| Married | 107 | 83.6 |
| Relation to patient | ||
| Spouse/partner | 64 | 49.6 |
| Parent | 45 | 34.9 |
| Othera | 20 | 15.5 |
| Caregiver role | ||
| Sole caregiver | 59 | 45.7 |
| Part of a team | 70 | 54.3 |
| Double-duty Caregiverb | ||
| Yes | 43 | 33.6 |
| Does the caregiver live with the patient | ||
| Yes | 100 | 78.1 |
| Resides locallyc | 37 | 28.7 |
| Patient Characteristics (n = 111) | Mean (SD) | Range |
| Patient age (years) | 41.6 (18.6) | 4 to 76 |
| Patient Characteristics (n = 111) | n | % |
| Patient sex | ||
| Male | 61 | 55.0 |
| Patient type | ||
| Adult | 84 | 75.7 |
| Pediatric | 27 | 24.3 |
| Patient cancer typed | ||
| Carcinoma | 53 | 47.8 |
| Leukemia | 25 | 22.5 |
| Sarcoma | 23 | 20.7 |
| Lymphoma | 9 | 8.1 |
| Myeloma | 1 | 0.9 |
| Cancer treatment type | ||
| Biotherapy/immunotherapy | 69 | 62.2 |
| Allogeneic HSCTe | 11 | 9.9 |
| Chemotherapy | 10 | 9.0 |
| Surgery | 10 | 9.0 |
| Otherf | 11 | 9.9 |
| Hospital status | ||
| Inpatient | 92 | 83.6 |
Other: child (n = 10), sister (n = 5), other family (n = 3), and friend (n = 2).
Double-duty caregivers are caregivers who provide care to one or more people other than the cancer patient.
Resides locally = within 100 miles of NIH.
Type: Carcinoma: prostate, melanoma, anal, breast, lung, colon, liver, cervical, ovarian, adrenal cortical, pancreatic, kidney, thymus, thyroid and peritoneal cancer; Leukemia: chronic myelogenous leukemia, acute lymphocytic leukemia, acute myelogenous leukemia, and chronic lymphocytic leukemia; Sarcoma: brain, gastrointestinal stromal tumor and desmoid tumors; Lymphoma: Hodgkin's and non-Hodgkin's lymphoma; Myeloma: multiple myeloma.
HSCT = hematopoietic stem-cell transplantation.
Other treatments: Radiation (n = 3) and combination therapy (n = 8).
TABLE 2.
Baseline caregiver outcomes
| Outcomes | Baseline mean (SD) range (n) |
|---|---|
| Lonelinessa | 54 (10.7) |
| 37.1 to 85.2 (129) | |
| Physical healtha | 51.7 (7.8) |
| 19.9 to 67.7 (127) | |
| Mental healtha | 48.1 (8.3) |
| 21.2 to 67.6 (124) | |
| Perceived stressa | 52.0 (9.8) |
| 31.5 to 85.4 (129) | |
| Self-efficacya | 51.7 (9.4) |
| 17.3 to 68.4 (129) | |
| Sleep disturbancea | 54.0 (7.9) |
| 26.4 to 83.8 (129) | |
| Caregiver burdenb | 55.1 (12.0) |
| 28.0 to 103.0 (125) | |
| Mutualityc | 3.3 (0.7) |
| 0.3 to 4.0 (127) | |
| Health behaviorsd | 2.6 (0.5) |
| 1.4 to 3.8 (123) |
Measured using PROMIS and/or NIH Toolbox T Scores that are normed with average scores of 50 and a standard deviation of 10.
Caregiver Reaction Assessment total score.
Family Care Inventory Mutuality scale.
Health-Promoting Lifestyle Profile II total score.
TABLE 3.
Multilevel linear mixed model for predictors of loneliness over time
| Estimate | Standard error | P-value | Estimate | Standard error | P-value | |
|---|---|---|---|---|---|---|
| Timepoint a | ||||||
| Timepoint 1 | 0.0041 | 0.3877 | .9916 | 0.5169 | 0.5072 | .3103 |
| Timepoint 2 | −0.0514 | 0.3952 | .8966 | −0.0913 | 0.3501 | .7948 |
| Caregiver sexb | −0.0209 | 0.5226 | .9681 | |||
| Perceived stress | 0.1136 | 0.0246 | <.0001 | |||
| Caregiver burdenc | 0.0684 | 0.0225 | .0029 | |||
| Hospital statusd | −0.9034 | 0.4771 | .0608 | |||
| Mental healthe | −0.2098 | 0.0858 | .0160 | |||
| Mutualityf | −0.5666 | 0.3157 | .0752 | |||
| Marital statusg | −1.5215 | 0.5708 | .0088 | |||
| Employment statush | 0.9997 | 0.4490 | .0279 | |||
| Health behaviorsi | −1.0003 | 0.5826 | .0886 |
Timepoint was categorical (timepoint 3 = reference group).
Female = reference group.
Caregiver Reaction Assessment total score.
Dichotomized as inpatient and outpatient (reference group).
PROMIS global mental health.
Family Caregiver Inventory mutuality scale.
Dichotomized as married and unmarried (reference group).
Dichotomized as working and not working (reference group).
Health Promoting Lifestyle Profile-II total score.
4 ∣. CONCLUSIONS
A key finding of this study was that levels of loneliness started high and remained high throughout the 6 month trajectory of caregiving. Like past studies, caregiver burden16,17 and poor mental health24,25 were associated with higher levels of loneliness, while being married provided some protection against loneliness.25 Unlike past studies in cancer caregivers, this study found no relationship between sex and/or education levels and loneliness.25
A novel finding in this study is that caregivers who were employed reported lower levels of loneliness than their non-working peers. It is possible that individuals who are employed may receive workplace social support that is protective against loneliness. It is also possible that work may serve as a distraction, temporarily redirecting caregivers' attention away from the distress associated with caregiving, and this is somehow protective. Clearly, more research is needed to clarify if and precisely how being employed may shield caregivers from loneliness. If working truly is protective against loneliness, then there may be implications for the nearly 30% of caregivers in this study who left work after assuming their caregiving responsibilities.
Sahin et al found that patients reported receiving more social support than did caregivers.24 Understandably, friends and family rally around the cancer patient, and considerably less attention and support may be given to the caregiver. Particularly when the caregiver is the spouse, sibling and/or friend of the care recipient, cancer may have robbed the caregiver of their primary support system. In this case, the caregiver may be reluctant to share their suffering with the care recipient.19 In past studies, caregivers have discussed the need to prioritize the patient's needs over their own, while their own social networks and support systems may be shrinking.3 Our own past research has shown that roles change for the caregivers and individual with cancer during the treatment trajectory, when the cancer patient becomes the focus of treatment and support and the caregiver becomes the giver and protector.19
4.1 ∣. Study limitations
The strengths of this study include the availability of the survey in both English and Spanish and the longitudinal design, but several limitations exist. First, selection bias may be present because only caregivers referred by patients were recruited. Additionally, the self-reported nature of the study is vulnerable to recall or response bias. The NIH Clinical Center is a unique research setting, and individuals treated there may be different than those who receive cancer treatment in more traditional settings.
4.2 ∣. Clinical implications
This study provides guidance for clinicians by confirming the findings of previous research that showed that caregivers with higher burden, stress and in poor mental health are at increased risk for loneliness. Continuing to work may be beneficial to caregivers by reducing levels of loneliness, and clinicians might use this information when helping guide caregivers through the possible ramifications of leaving employment in order to provide care for the individual with cancer. Clinicians can become involved on a policy level by advocating for flexible family leave and alternative work schedules, not just for births and deaths but also for caregiving, so that caregivers are not forced against their will to leave employment in order to provide care.
Because accessing traditional support systems may be difficult for caregivers during cancer treatment, research suggests that the Internet, specifically online social support groups, may provide a valuable resource.36 Clinicians can encourage the use of the Internet using technology such as FaceTime or Skype that allows caregivers to visually connect with friends and family from a distance. Social networks such as Facebook and Instagram provide a platform for caregivers to obtain information, nurture existing social networks, and also develop new relationships by joining communities of interest (eg, for caregivers). Others, such as Caring Bridge (https://www.caringbridge.org/) help family and friends remain in communication during health crises by sending updates and activating/coordinating their community when assistance is needed. Web-based interventions for cancer caregivers can significantly reduce stress, burden, and improve mood,37 but additional research is needed to determine whether such interventions reduce loneliness and its sequela in this population. Moreover, even when social networks are available, a subset of caregivers, particularly those with a history of mental health needs, may need additional psychological help. Thus, caregivers should assess for more significant signs of distress including anxiety, depression, and suicidal ideation, and make appropriate referrals to spiritual care, social work and/or mental health providers.
ACKNOWLEDGEMENTS
This research was supported by the Intramural Research Program of the NIH Clinical Center. The authors wish to thank Sima Bedoya and Stephen Klagholz for their assistance with the study.
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
Data Citation
[Dataset] Ross A, Perez A, Wehrlen L, Lee J, Yang L, Cox R, Bevans M, Ding A, Wiener L, Wallen; 2020; Factors influencing loneliness in cancer caregivers: A longitudinal study. https://clinicaltrials.gov/ct2/show/ NCT01981538. The data that support the findings of this study are available from the corresponding author upon reasonable request.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.National Alliance for Caregiving. Caregiving in America; 2015; https://www.caregiving.org/research/caregivingusa/
- 2.Given BA, Given CW, Sherwood P. The challenge of quality cancer care for family caregivers. Semin Oncol Nurs. 2012;28(4):205–212. [DOI] [PubMed] [Google Scholar]
- 3.Gibbons SW, Ross A, Bevans M. Liminality as a conceptual frame for understanding the family caregiving rite of passage: an integrative review. Res Nurs Health. 2014;37(5):423–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Northouse L, Williams AL, Given B, McCorkle R. Psychosocial care for family caregivers of patients with cancer. J Clin Oncol. 2012;30(11):1227–1234. [DOI] [PubMed] [Google Scholar]
- 5.Bevans M, Sternberg EM. Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. JAMA. 2012;307(4):398–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elliott AF, Burgio LD, Decoster J. Enhancing caregiver health: findings from the resources for enhancing Alzheimer's caregiver health II intervention. J Am Geriatr Soc. 2010;58(1):30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Umberson D, Montez JK. Social relationships and health: a flashpoint for health policy. Health Soc Behav. 2010;51(Suppl):S54–S66. 10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steptoe A, Kivimaki M. Stress and cardiovascular disease: an update on current knowledge. Annu Rev Public Health. 2013;34:337–354. [DOI] [PubMed] [Google Scholar]
- 10.Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christiansen J, Larsen FB, Lasgaard M. Do stress, health behavior, and sleep mediate the association between loneliness and adverse health conditions among older people? Soc Sci Med. 2016;152:80–86. [DOI] [PubMed] [Google Scholar]
- 12.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227–237. [DOI] [PubMed] [Google Scholar]
- 13.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holt-Lunstad J The potential public health relevance of social isolation and loneliness: prevalence, epidemiology, and risk factors. Public Policy Aging Rep. 2018;27(4):127–130. [Google Scholar]
- 15.Gray TF, Azizoddin DR, Nersesian PV. Loneliness among cancer caregivers: a narrative review. Palliative & supportive care. 2020;18(3):359–67. [DOI] [PubMed] [Google Scholar]
- 16.Lee K, Martin P, Poon LW. Predictors of caregiving burden: impact of subjective health, negative affect, and loneliness of octogenarians and centenarians. Aging Ment Health. 2017;21(11):1214–1221. [DOI] [PubMed] [Google Scholar]
- 17.Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA. 2014;311(10):1052–1060. [DOI] [PubMed] [Google Scholar]
- 18.Li Q, Loke AY. A spectrum of hidden morbidities among spousal caregivers for patients with cancer, and differences between the genders: a review of the literature. Eur J Oncol Nurs. 2013;17(5):578–587. [DOI] [PubMed] [Google Scholar]
- 19.Gibbons SW, Ross A, Wehrlen L, Klagholz S, Bevans M. Enhancing the cancer caregiving experience: building resilience through role adjustment and mutuality. Eur J Oncol Nurs. 2019;43:101663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Totman J, Pistrang N, Smith S, Hennessey S, Martin J. You only have one chance to get it right: a qualitative study of relatives' experiences of caring at home for a family member with terminal cancer. Palliat Med. 2015;29(6):496–507. [DOI] [PubMed] [Google Scholar]
- 21.van Roij J, Brom L, Youssef-El Soud M, van de Poll-Franse L, Raijmakers NJH. Social consequences of advanced cancer in patients and their informal caregivers: a qualitative study. Supp Care Cance. 2019;27(4):1187–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maguire R, Hanly P, Balfe M, et al. Worry in head and neck cancer caregivers: the role of survivor factors, care-related stressors, and loneliness in predicting fear of recurrence. Nur Res. 2017;66(4):295–303. [DOI] [PubMed] [Google Scholar]
- 23.Segrin C, Badger TA, Sikorskii A. A dyadic analysis of loneliness and health-related quality of life in Latinas with breast cancer and their informal caregivers. J Psychosoc Oncol. 2019;37(2):213–227. [DOI] [PubMed] [Google Scholar]
- 24.Sahin ZA, Tan M. Loneliness, depression, and social support of patients with cancer and their caregivers. Clin J Oncol Nurs. 2012;16(2):145–149. [DOI] [PubMed] [Google Scholar]
- 25.Soylu C, Ozaslan E, Karaca H, Ozkan M. Psychological distress and loneliness in caregiver of advanced oncological inpatients. J Health Psychol. 2016;21(9):1896–1906. [DOI] [PubMed] [Google Scholar]
- 26.Klagholz SD, Ross A, Wehrlen L, Bedoya SZ, Wiener L, Bevans MF. Assessing the feasibility of an electronic patient-reported outcome (ePRO) collection system in caregivers of cancer patients. Psychooncology. 2018;27(4):1350–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cella D, Riley W, Stone A, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63(11):1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gershon RC, Wagster MV, Hendrie HC, Fox NA, Cook KF, Nowinski CJ. NIH toolbox for assessment of neurological and behavioral function. Neurology. 2013;80(11 Suppl 3):S2–S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Archbold PG, Stewart BJ, Greenlick MR, Harvath T. Mutuality and preparedness as predictors of caregiver role strain. Res Nurs Health. 1990;13(6):375–384. [DOI] [PubMed] [Google Scholar]
- 30.Schumacher KL, Stewart BJ, Archbold PG, Caparro M, Mutale F, Agrawal S. Effects of caregiving demand, mutuality, and preparedness on family caregiver outcomes during cancer treatment. Oncol Nurs Forum. 2008;35(1):49–56. [DOI] [PubMed] [Google Scholar]
- 31.Schumacher KL, Stewart BJ, Archbold PG. Mutuality and preparedness moderate the effects of caregiving demand on cancer family caregiver outcomes. Nurs Res. 2007;56(6):425–433. [DOI] [PubMed] [Google Scholar]
- 32.Given CW, Given B, Stommel M, Collins C, King S, Franklin S. The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health. 1992;15(4):271–283. [DOI] [PubMed] [Google Scholar]
- 33.Nijboer C, Triemstra M, Tempelaar R, Sanderman R, van den Bos GA. Measuring both negative and positive reactions to giving care to cancer patients: psychometric qualities of the caregiver reaction assessment (CRA). Soc SciMd. 1999;48(9):1259–1269. [DOI] [PubMed] [Google Scholar]
- 34.Walker SN, Sechrist KR, Pender NJ. The health-promoting lifestyle profile: development and psychometric characteristics. Nurs Res. 1987;36(2):76–81. [PubMed] [Google Scholar]
- 35.Slotkin J, Nowinski C, Hays R, et al. NIH Toolbox scoring and interpretation guide. Chicago: National Institutes of Health and Northwestern University; 2012. [Google Scholar]
- 36.Benson JJ, Oliver DP, Washington KT, et al. Online social support groups for informal caregivers of hospice patients with cancer. Eur J Oncol Nurs. 2020;44:101698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tang WP, Chan CW, So WK, Leung DY. Web-based interventions for caregivers of cancer patients: a review of literatures. Asia Pac J Oncol Nurs. 2014;1(1):9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


