Abstract
Background
Physical activity is a commonly prescribed medicine for people with conditions such as obesity and diabetes who are also at increased risk of being hospitalized or severely ill from COVID-19. However, many people are reporting challenges in engaging in a healthy dose of physical activity amid the pandemic.
Objective
This rapid review synthesizes the current empirical evidence about the impacts of COVID-19 on people’s outdoor physical activity and sedentary behavior while highlighting the role of community environments in promoting or hindering physical activity during the pandemic.
Methods
Literature searches were conducted using keywords related to COVID-19: physical activity, mobility, and lifestyle behaviors. Eligibility criteria were peer-reviewed empirical and quantitative studies published in English, addressing COVID-19 and using physical activity and/or sedentary behavior as the study outcomes.
Results
Out of 61 eligible studies, the majority (78.3%) were conducted in Asian and European countries, with only four (6.7%) being US studies. The results showed that COVID-19 was linked with significant decreases in mobility, walking, and physical activity, and increases in sedentary activity. A few studies also reported contradicting results including increased uses of parks/trails and increased recreational activity among certain groups of population.
Conclusions
Evidence suggests an overall negative impact of COVID-19 on physical activity, with differential effects across different sub-populations. Significant knowledge gaps are also found in the roles of social and physical attributes that can promote physical activity during pandemics with reduced safety risks.
The spread of coronavirus disease 2019 (COVID-19), classified as a pandemic by the World Health Organization on March 11, 2020, has greatly impacted people’s daily lives globally [1]. The COVID-19 Community Mobility Reports from Google indicate that compared to the pre-COVID-19 baseline (the median value of the five weeks from January 3, 2020 to February 6, 2020), mobility trends during COVID-19 (as of March 9, 2021) showed decreases in most locations including retail and recreation (-14%), transit stations (-34%), grocery stores and pharmacies (-5%), and workplaces (-31%); however, increases have been witnessed in parks (+9%) and residential places (+9%) [2]. This suggests that while people spent more time at home, they also visited parks and open spaces (eg, national parks, public gardens, dog parks) more frequently during the pandemic [2].
Outdoor physical activity holds strong potential as an effective coping and preventive strategy given its many well-documented physical, social, and mental health benefits for people of all ages, especially those with or at risk of developing chronic diseases [3,4]. Many empirical studies suggest that physical activity can prevent chronic diseases (eg, cardiovascular disease, diabetes, and obesity), improve brain health and conditions, promote mental health (eg, reduced depression and anxiety), and reduce falls or fall-related injuries [5,6]. For those with existing health conditions such as diabetes and obesity, physical activity is even more critical as a remedy to treat and manage the conditions [7]. Recognizing these health benefits, many efforts have been initiated by organizations like America Walks and World Health Organization to promote physical activity, which increasingly recognize the importance of environmental approaches. The Surgeon General’s Call to Action to Promote Walking and Walkable Communities released in 2015 by the US Department of Health and Human Services recognizes the importance of active lifestyles and creating walkable environments to support active living [8]. A large body of physical activity literature recognizes the significant roles of community environments (eg, streetscape, esthetics, roads and traffic, neighborhood parks, and activity zones) in promoting physical activity and reducing sedentary behavior [9,10].
While considering health-promotion strategies and interventions, Stokols (1992) emphasized the nature of individuals’ interactions with physical and sociocultural environments from an ecological perspective, focusing on the need of addressing environmental factors to change/promote health-related behaviors [11]. Ecological models have been popularly used as the foundation to understand and develop multilevel approaches of promoting health behaviors. Bronfenbrenner (1994) introduced the ecological systems model, which focused on the impact of the environment on individual development. He saw individual development influenced by multi-layered exposures to various environmental factors over time, categorized into five systems, including microsystem, mesosystem, exosystem, macrosystem, and chronosystem [12]. The quality of each layer can either enhance or restrict individuals’ health-related behaviors.
COVID-19 has brought a new layer of challenges to our health and healthy behaviors. People worldwide are reporting challenges in engaging in a healthy dose of physical activity amid the pandemic, with up to a 50% decrease of physical activity in some areas. This decline is in part due to the limited and inequitable availability of safe outdoor community resources (eg, parks, trails, sports facilities, sidewalks) that support physical activity [13]. Despite the growing recognition of the negative impacts of COVID-19 on people’s health, only a small amount of literature has explored the roles of environmental factors such as neighborhood infrastructure and recreational resources that can help promote or hinder physical activity. Recent reviews showed that the personal, behavioral, and social changes during the pandemic have led to mental distress and illness [14-16]. Reviews of work on children and older adults emphasized the environmental associations of anxiety, depression, and other psychological outcomes (eg, worry, grief) during the COVID-19 pandemic [14,16]. Usher et al. (2020) also conducted a rapid review highlighting the psychological distress (eg, fear, stress, anger, and frustration) associated with behavioral changes (isolation and quarantine) and restricted social interactions (social distancing) [15]. Facing the new normal of everyday life, Megahed & Ghoneim (2020) suggested research areas and questions related to five scopes of post-coronavirus architecture and urbanism (post-pandemic urbanism, public spaces, housing, office spaces, and building and construction technology) that researchers need to address to prevent the virus from spreading [17].
This rapid review aims to show whether COVID-19 has impacted people’s outdoor physical activity and sedentary behavior during the early phases of the pandemic, by synthesizing the current empirical evidence on this topic, and highlighting the roles of community environments in promoting or hindering physical activity during the pandemic. Going beyond the scope of previous literature reviews on COVID-19, this study includes multiple and specific physical activity outcomes (eg, walking and biking), and summarizes several environmental factors shown to be important for promoting physical activity amid the pandemic. By providing a comprehensive and critical examination of the current body of literature on this topic, we aim to provide empirical guidance for policymakers, researchers, and practitioners. This guidance can support those in various professions toward investigating the full range of environmental facilitators and barriers to promoting active living, as an effective way to cope with emotional or mental distress during pandemics like COVID-19.
METHODS
Eligibility criteria
We selected studies that met the following four criteria: 1) addressing the impact of COVID-19, 2) including physical activity (eg, step counts, weekly minutes of physical activity, time spent outdoors) and/or sedentary behavior (eg, screen/sitting time, total sedentary time) as study outcomes, 3) peer-reviewed empirical and quantitative studies including both cross-sectional and longitudinal studies, and 4) studies written in English. We excluded studies on health care facilities and professional athletes, given their unique and narrow focuses that are different from our main study aim targeting general populations in their everyday residential communities.
Search strategy
Literature searches were conducted in PubMed on October 23, 2020, using pre-developed keywords related to COVID-19, physical activity, mobility, and lifestyle behaviors. COVID-19 related search terms included “coronavirus” or “COVID-19” or “coronavirus disease 2019” or “SARS-COV-2” or “Severe Acute Respiratory Syndrome Coronavirus 2”. Physical activity related search terms encompassed “physical activity” or “walk” or “bike” or “sedentary” or “exercise” or “active living” or “transport” or “mobility” (Table 1). The PubMed search limiter included articles being published between 2019 and 2020. Additional searches were conducted in Google Scholar on November 1, 2020, to validate and supplement the PubMed search results.
Table 1.
PubMed search string
| Domains | Search string |
|---|---|
| COVID-19 |
((wuhan[tw] AND (coronavirus[tw] OR corona virus[tw])) OR coronavirus*[ti] OR COVID*[tw] OR nCov[tw] OR 2019 ncov[tw] OR novel coronavirus[tw] OR novel corona virus[tw] OR covid-19[tw] OR SARS-COV-2[tw] OR Severe Acute Respiratory Syndrome Coronavirus 2[tw] OR coronavirus disease 2019[tw] OR corona virus disease 2019[tw] OR new coronavirus[tw] OR new corona virus[tw] OR new coronaviruses[all] OR novel coronaviruses[all] OR “Severe Acute Respiratory Syndrome Coronavirus 2”[nm] OR 2019 ncov[tw] OR nCov 2019[tw] OR SARS Coronavirus 2[all]) AND (2019[dp]:2020[dp]))) |
| Active living | (Physical activit*) or walk* or sedentary or (moderate activit*) or (vigorous activit*) or exercise or bike or biking or bicycle or bicycling or cycling or recreation* or (active living) or running or jogging or strolling or (screen time) or (sedentary behavior) or play or transport* or transit or bus or (light rail) or travel or trip or mobility or (outdoor time) or leisure* |
Selection process
Eligible studies were selected in two phases using Covidence (www.covidence.org), which is a web-based systematic review software for screening and data extraction. First, studies searched in PubMed were screened based on the titles and abstracts. Second, articles selected from the title and abstract screening went through the full-text sorting. Two researchers completed the screening process independently, and all disagreements were resolved through consensus discussions with a third researcher.
Quality assessment
Two researchers independently conducted the quality assessment of each study selected from the title and abstract screening and the full-text sorting, using a pre-developed quality assessment tool adapted from established tools for quantitative studies [18,19]. The methodological quality was assessed on a rating scale of zero to six based on the following six criteria: 1) study design (cross-sectional vs longitudinal studies), 2) sample representativeness, 3) large sample size, 4) measurement tool for outcome variables, 5) confounders, and 6) statistical methods. The studies were classified as low-quality, middle-quality, and high-quality based on the rating scores of 0 to 2, 3 to 4, and 5 to 6, respectively.
Data extraction
Using a pre-established data extraction template, we synthesized the study characteristics related to the fields of publication, study designs, study locations and settings, study participants, confounding/control variables, environmental factors, physical activity outcomes, statistical study findings, and quality assessment results (Table S1 in the Online Supplementary Document). Two researchers extracted the data from the selected studies and cross-checked the extracted data. Two other researchers further reviewed the quality of the extracted data.
RESULTS
Study identification
Figure 1 displays the search and selection process that follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A total of 5059 records were identified from the PubMed database search. A total of 872 duplicates and 4061 irrelevant records were removed after the title and abstract screening. The remaining 126 articles were further screened based on the full text, which identified 70 ineligible articles. In addition, 5 studies were identified through Google Scholar. This led to the final total of 61 eligible studies for the data extraction and synthesis.
Figure 1.
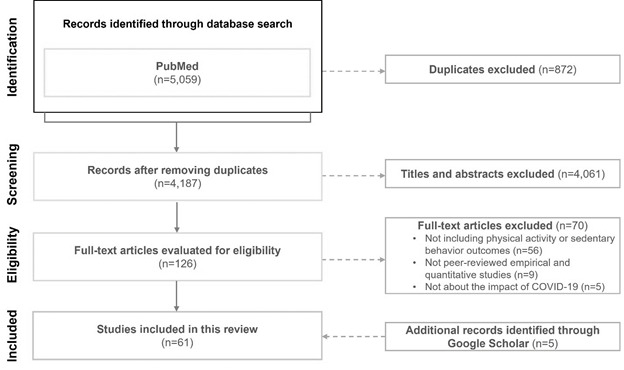
PRISMA flow chart.
Characteristics of the included studies
Of the 61 reviewed studies summarized in Table 2, the majority were cross-sectional studies (n = 52, 85.2%). Popular fields of publication were health-related (n = 54, 88.5%) including public/global health, medical, and nutrition/physical activity. Most of the studies were conducted in Europe (n = 27, 44.3%), North America (n = 13, 21.3%), or Asia (n = 13, 21.3%). The sample sizes of the reviewed studies ranged between 24 and 7420 000, and over two thirds had a sample of at least 400. The study population covered children and/or adolescents (n = 8, 13.1%), adults (n = 43, 70.5%), and older adults (n = 2, 3.3%). Five domains of physical activity-related outcomes were measured in the reviewed studies: walking and biking (n = 13, 8.1%), physical activity (n = 92, 57.5%), mobility (n = 17, 10.6%), sedentary behavior (n = 37, 23.1%), and total energy expenditure (n = 1, 0.6%).
Table 2.
Study characteristics
| Study characteristics | No. | % |
|---|---|---|
|
Study designs:
| ||
| Cross-sectional |
52 |
85.2 |
| Longitudinal |
9 |
14.8 |
|
Fields of publication:
| ||
| Ecology |
2 |
3.3 |
| Economics |
1 |
1.6 |
| Public/global health |
36 |
59.0 |
| Medical |
12 |
19.7 |
| Nutrition and physical activity |
6 |
9.8 |
| Psychology |
2 |
3.3 |
| Sustainability |
1 |
1.6 |
| Transportation |
1 |
1.6 |
|
Regions of study locations:
| ||
| Oceania |
3 |
4.9 |
| Europe |
27 |
44.3 |
| North America |
13 |
21.3 |
| Asia |
13 |
21.3 |
| Africa |
1 |
1.6 |
| Multiple |
4 |
6.6 |
|
Study settings:
| ||
| General/not specified |
46 |
75.4 |
| Urban only |
9 |
14.8 |
| Urban and suburban |
2 |
3.3 |
| Urban and rural |
4 |
6.6 |
|
Gender:
| ||
| Both male and female |
60 |
98.4 |
| Female only |
1 |
1.6 |
|
Populations:
| ||
| Children/adolescents/youth (under 18) |
8 |
13.1 |
| Adults (18+) |
43 |
70.5 |
| Older adults (65+) |
2 |
3.3 |
| Children and adults |
1 |
1.6 |
| Not applicable |
7 |
11.5 |
|
Specific groups:*
| ||
| Adults with specific conditions |
10 |
16.4 |
| Children with specific conditions |
1 |
1.6 |
| Older adults with specific conditions |
1 |
1.6 |
|
Sample sizes:†: | ||
| <400 |
18 |
29.5 |
| 400-4999 |
35 |
57.4 |
| 5000+ |
8 |
13.1 |
|
Physical activity outcome measures:
| ||
| Subjective measures |
45 |
73.8 |
| Objective measures |
13 |
21.3 |
| Both subjective and objective measures |
3 |
4.9 |
|
Physical activity outcome domains:
| ||
| Walking and/or biking |
13 |
8.1 |
| Physical activity |
92 |
57.5 |
| Mobility |
17 |
10.6 |
| Sedentary behavior |
37 |
23.1 |
| Total energy expenditure | 1 | 0.6 |
*Specific groups of population include adults with chronic conditions, with chronic coronary syndromes, of pregnant women, of eating disorder group, and of runners and cyclists; children with congenital heart disease (CHD); older patients with implantable cardioverter-defibrillators (ICD), with type 2 diabetes, subscribers of Leave No Trace (LNT) center for outdoor ethics, a non-profit organization.
†Sample sizse range from 24-4742 000 in the included 61 studies. 18 studies [20-37] with sample sizes lower than 400 and 8 studies [13,38-44] with sample sizes greater than 5000.
Changes in physical activity amid COVID-19
Table 3 displays the significant impacts of COVID-19 on walking and biking, physical activity, mobility, sedentary behavior, and total energy expenditure. Most of the reviewed studies showed that the COVID-19 outbreak limited walking and biking, physical activity, and mobility, while increasing sedentary behavior across all age groups worldwide.
Table 3.
Impact of COVID-19 on physical activity*
| Negative | Positive | Not significant | Not reported | |||
|---|---|---|---|---|---|---|
|
1
|
Walking and biking
|
|
|
|
|
|
|
|
1.01 |
Walking |
[20-23,45-49] |
|
[50] |
|
|
|
1.02 |
Walking and biking |
|
[38]* |
|
[40,51]D |
|
2
|
Physical activity
|
|
|
|
|
|
|
|
2.01 |
Light physical activity |
[52]* |
|
|
|
|
|
2.02 |
Moderate physical activity |
[20-24,45,46,48,50] |
[29] |
|
|
|
|
2.03 |
Vigorous physical activity |
[20,22,23,45,46,48,50,52,53] |
[29] |
[47] |
|
|
|
2.04 |
Moderate to vigorous physical activity |
[52,53]* |
|
|
[54]D, [55] |
|
|
2.05 |
Meeting the recommended physical activity |
47,56] |
|
|
[57]D, [51,58] |
|
|
2.06 |
Meeting the 24-h movement recommendation |
|
|
|
[51],[57]* |
|
|
2.07 |
Overall time outdoors |
|
|
|
[57]D |
|
|
2.08 |
Total physical activity |
[20,25-28,46,50,55,56,58-65] |
[59] |
|
[35,36,42,66]D, [67], [68]D |
|
|
2.09 |
Step counts |
[21,26,30,31,39,53,69]* |
|
|
[15]D |
|
|
2.1 |
Outdoor physical activity |
[70] |
|
|
[51,57,71]D |
|
|
2.11 |
Outdoor play |
[70] |
|
|
[51,57]D |
|
|
2.12 |
Physical activity with family |
|
[62] |
|
[57]D |
|
|
2.13 |
Exercise/sports |
[26]*, [32,49,64,72] |
|
|
[34,42], [37,73,74]D |
|
|
2.14 |
Housework (light, moderate, or heavy) |
|
|
|
[34] |
|
|
2.15 |
Labor/physical working (eg, gardening) |
|
[49] |
|
[34] |
|
|
2.16 |
Type of physical activity |
|
|
|
[55] |
|
|
2.17 |
Time spent to relax/Leisure activities |
|
[64] |
|
[75] |
|
|
2.18 |
Locations of physical activity |
|
|
|
[25], [38]* |
|
|
2.19 |
Outdoor recreation |
[76] |
[38]* |
|
|
|
3
|
Mobility
|
|
|
|
|
|
|
|
3.01 |
Overall trips |
|
|
|
[20,77]D |
|
|
3.02 |
Travel mode/behaviors |
|
|
|
[77]D |
|
|
3.03 |
Trip purpose |
|
|
|
[43,44,77]D |
|
|
3.04 |
Use of transportation/Total time spent in transport/Energy expenditure |
[48,64] |
|
|
[77]D |
|
|
3.05 |
Bike sharing system usage |
|
[41] |
|
|
|
|
3.06 |
Distance travelled |
[76] |
|
|
[69]* |
|
|
3.07 |
Ridership |
[36] |
|
|
|
|
|
3.08 |
Moving habits |
|
|
|
[78]D |
|
|
3.09 |
Frequency of outings |
|
|
|
[66] |
|
|
3.10 |
Park/green space visitation |
|
[38]* |
|
[79]D |
|
4
|
Sedentary behavior
|
|
|
|
|
|
|
|
4.01 |
Time spent sitting |
|
[20-22,25,29,45,46] |
[50] |
[54]D |
|
|
4.02 |
Screen time (eg, video games, TV watching, computer use) |
|
[22,32,33,48,49,62] |
[61] |
[35,36,51,54,57,71]D |
|
|
4.03 |
Family sedentary behavior |
|
|
|
[57]D |
|
|
4.04 |
Use of/time spent on social media |
|
[27], [69]* |
|
[51,57]D |
|
|
4.05 |
Total sedentary behavior/time |
|
[48,49,58,59] |
|
[66] |
|
|
4.06 |
Non-screen based sedentary activities |
|
|
|
[51]D |
|
|
4.07 |
Homestay duration |
|
[69]† |
|
|
|
|
4.08 |
E-working time |
|
[48,62] |
|
|
|
|
4.09 |
Resting heart rate |
[53]† |
|
|
|
|
5
|
Composite
|
|
|
|
|
|
| 5.01 | Total energy expenditure | [20] | ||||
*Subjective Data (no symbol), Objective Data (†), Descriptive Only (D)
Of the 10 studies reporting significant changes in walking and biking during the COVID-19 pandemic, one study that focused on runners and cyclists demonstrated that daily pedestrian (ie, running, walking, and hiking) and cycling recreational activity increased by 291% in Oslo, Norway during the COVID-19 lockdown [38]. The other nine studies indicated significant decreases in walking during confinement [20-23,45-49].
The overall physical activity levels dropped significantly worldwide during COVID-19, including decreases in light [52], moderate and/or vigorous [20-24,45,46,48,50,52], and total physical activity [20,25-28,46,50,55,56,58-65], although one study showed an increase in moderate, vigorous, and total physical activity among university students during confinement [29]. Other studies suggested a significant decrease in the proportion [47] or the number [56] of participants who met the recommended physical activity level (for adults, at least 150 minutes of moderate-intensity aerobic activity according to the Centers for Disease Control and Prevention) during the pandemic, confirming the significant impact of COVID-19 on public health. Further, COVID-19 has resulted in significant decreases in daily step counts [26,30,31,39,52,53,69], outdoor physical activity and outdoor play [70], and exercise/sports [26,32,49,64,72], while several studies indicated significant increases in physical activity with family [62], labor/physical working (eg, gardening) [49], and time spent in leisure activities [64]. Inconsistent impacts of COVID-19 were reported on outdoor recreational activities in two studies. One US study demonstrated a significant decrease in outdoor recreation participation [76], while another European study reported a significant increase in outdoor recreational activity during the pandemic [38].
Studies on mobility showed significant decreases in total time spent in transport [48,64], distances traveled for outdoor recreation [76], subway ridership [40], and the frequency of outings [66]. However, two other studies reported that the COVID-19 outbreak increased the use of the Public Bike Sharing System in South Korea [41] and park and green space visits in Norway [38].
Physical inactivity and sedentary behavior became more prevalent during the COVID-19 pandemic. The reviewed studies showed significant increases in time spent sitting [20-22,25,29,45,46], screen time (eg, video games, TV watching, and computer use) [27,32,33,48,49,62], time spent on social media [27,69], total sedentary time [48,49,58,59], homestay duration [69], and e-working time [48,62]. Another study reported a significant decline in the resting heart rate [53].
Only one study investigated the influence of the COVID-19 pandemic on total energy expenditure. It revealed a significant decrease in energy expenditure among physiotherapy professionals and students during the COVID-19 lockdown [20].
The roles of community environments
In general, physical activity and trips for all purposes (eg, commuting, shopping, and social/recreational) decreased remarkably since the start of the pandemic. Despite the recognition that supportive community environments are important for promoting active lifestyles, only a small number (n = 11 including three studies with descriptive statistics only, 18%) of the included studies investigated the roles of community environments (Table 4) [25,30,34,35,38,42,43,51,55,57,79]. Most of the abovementioned studies were from Europe (n = 5) followed by Canada (n = 3), the US (n = 2), and Asia (n = 1). Although not directly evaluating the environmental effects, 10 additional mobility-related articles (16%) examined the changes in people’s transportation habits (eg, locations they visited) and purposes since COVID-19 [40,41,43,48,64,66,69,76-78]. Four domains of community environments have emerged from these studies to be important for supporting physical activity during the COVID-19 pandemic, including regional locations, dwelling types and density, nature and green spaces, and neighborhood infrastructure (Table 4).
Table 4.
Environmental factors
| Associations with physical activity | |
|---|---|
| Regional locations (urban) |
35 (–), 38 (NI), 43 (NI) |
| Dwelling types and density |
30 (living in a flat rather than in a house –; dwelling density NS), 34 (dwelling density NS), 51 (house residence +; dwelling density –), 57 (house residence +) |
| Nature and green spaces† |
25 (–), 51 (–), 55 (+), 66 (+), 79 (+) |
| Neighborhood infrastructure§ | 25 (sidewalks and roads, +), 42 (closed infrastructure, no good environments; NI), 51 (proximity to major roads, +) |
*Associations with physical activity – Positive (+), Negative (–), Not significant (NS), Not indicated/descriptive (NI).
†Two studies with negative results are for children. and others with positive results are for adults.
§Neighborhood infrastructure excluding nature and green spaces (eg, parks, trails).
Three of the reviewed studies examined regional locations such as urban and rural areas based on inhabitants and ecosystem conditions (ie, vegetation density and canopy covers). One study investigated the relationship between different regional settings (urban, suburban, and rural) and the changes in older adults’ physical activity during the pandemic, which reported a significantly greater decrease in physical activity among those living in urban areas [35]. Another study also reported a rapid decrease in physical activity and the increase in unhealthy behaviors (eg, smoking and alcohol consumption) in both urban (>2000 inhabitants) and rural patient populations with chronic coronary syndromes [38]. However, the decrease in physical activity was greater in urban patients than in rural ones. Descriptively, another US study showed that people in rural areas exhibited less decline in activities at locations such as workplace, transit, retail, and grocery store, but greater decreases in park visits than urban residents [43]. A consistent trend was revealed in a mobility-related article, which found that urban residents with limited access to outdoor recreation/leisure amenities were significantly more impacted by COVID-19 than their rural counterparts [76].
Of the three studies considering dwelling types (detached house vs apartment or flat), two Canadian studies focusing on children and youth populations showed a notable increase in outdoor activities (ie, walking, biking, playing) and overall time spent outdoors among those living in detached houses, compared to residents of apartments [51,57]. The third study conducted in Czech found that heart failure patients living in flats had significant decreases in daily step counts since the onset of the COVID-19, while those living in houses with gardens had less decrease [30]. Additionally, three studies assessed the relationships between residential or dwelling density and changes in physical activity [30,34,51]. Mitra et al. [51] indicated that the outdoor activities of children living in areas with high dwelling density decreased more significantly than those residing in low dwelling density areas. However, the other two studies showed that the changes in physical activity were not associated with residential density [30,34].
Five articles focusing on the association of nature and green spaces with the changes in physical activity during the COVID-19 pandemic showed inconsistent results [25,38,51,55,79]. Two North American studies relating to the child population showed a significant decrease in park visits and outdoor activities in parks or trails [25,51]. The remaining three articles involving adults, or the general population, showed a positive relationship between having/visiting nature or green spaces and physical activity [38,55,79]. Compared to inactive populations, active populations had significantly greater connectedness to nature and nature-relatedness during COVID-19 [55].
In terms of neighborhood infrastructure, three articles considered neighborhood environmental conditions (eg, major roads, sidewalks, and neighborhood amenities) to examine their relationships with the changes in physical activity [25,42,51]. According to Constandt et al. (2020), people in Belgium reported closed infrastructure and the lack of places to exercise as the barriers to exercising since the onset of the pandemic [42]. Dunton et al. (2020) demonstrated that US children had significant increases in physical activity on sidewalks and roads in their neighborhoods, while their physical activity time at parks or trails significantly decreased since the pandemic began [25]. Mitra et al. (2020) showed the proximity to major roads was a barrier to Canadian children, decreasing the odds of participating in outdoor activities. The same study also indicated that access to parks was negatively associated with parent-reported changes in physical activity among children [51].
DISCUSSION
This rapid review suggested that COVID-19 greatly impacted people’s daily mobility and physical activity patterns. Overall, people worldwide showed decreases in daily physical activities and increases in sedentary time (eg, watching TV, using electronic devices) and time spent at home, compared to the pre-COVID times. As increasing evidence confirms that sedentary behavior, independent of the physical activity levels, accompanies multiple health risks including chronic diseases, obesity, depression, and anxiety [80-83], further efforts are needed to develop effective intervention strategies to break down prolonged sitting time and reduce sedentary lifestyles. On the contrary, specific groups such as undergraduate students and runners/cyclists who used the Strava application showed significant increases in physical activity [29,38]. Housing and neighborhood environments have also been shown to play meaningful roles, with some evidence suggesting their potential to mitigate the negative impact of the pandemic.
Knowledge gaps recognized from the reviewed studies
Given the time-sensitive nature of published studies on this topic, about a quarter of all the reviewed studies (15 out of 61) relied on descriptive statistics to examine changes in walking, physical activity, sedentary behavior, and mobility behavior, without any statistical tests. Nine out of the 61 (15%) articles included were longitudinal studies comparing the data collected from two different periods before and during COVID-19. Most of the reviewed studies used self-reported or parent-reported survey data asking whether participants’ physical activity had decreased, increased, or remained constant. Seventeen out of the 61 (30%) included studies had limited sample sizes of fewer than 400, ranging from 24 to 315. Even for the articles with larger samples (n ≥400), only 20 studies were representative of the population by using random sampling methods. Lastly, this review identified a limited number of studies (11 out of 61) targeting vulnerable populations such as older adults and children.
While we emphasize the importance of future research on vulnerable populations, the review identified the lack of studies on highlighting the roles of community environments in physical activity and health-related outcomes across different populations in terms of age, gender, income, and health conditions amid COVID-19. For this review, about half (n = 6, 55%) of the eleven environment-related articles focused on specific populations including children (n = 3), older adults (n = 2), and heart failure patients (n = 1). This may highlight the benefits of the community environment for those specific populations who may have limited access to out-of-neighborhood destinations/opportunities. In addition, many existing studies emphasized the importance of neighborhood-level built environments where residents’ daily activities occur (eg, sidewalks and public spaces) on health-related outcomes; and the environmental impacts on those outcomes tend to differ across different populations [84-87]. For example, accessibility to freely available neighborhood resources (eg, walking/biking trails and green spaces) have been shown to impact residents’ behaviors, physical health, and mental health [88,89].
Built environments and active living during COVID-19
This review identified four environmental factors, including regional locations, dwelling types and density, nature and green spaces, and neighborhood infrastructure related to changes in physical activity. In addition to their community strategies supporting physical activity, the Centers for Disease Control and Prevention provided guidelines on how to be physically active during COVID-19 by visiting parks, pools, or recreation facilities. Although the number of empirical studies on COVID-19 that consider the roles of built environments is small, many leading organizations/initiatives, such as the American Association of Retired Persons (AARP), National Association of City Transportation Officials (NACTO), and professional design groups (eg, MASS, ARUP) have published design guidelines with implementable environmental strategies (eg, curbside seating and increased bike lanes) to cope with the “new normal” following the coronavirus pandemic. These publications address the design conflicts, dilemmas faced, and the potential solutions (eg, tactical urbanism) to provide better outdoor spaces for everyone to stay healthy and engaged, while ensuring safety from infection. For example, NACTO released a resource (ie, Streets for Pandemic Response and Recovery) that includes detailed strategies to redesign and adapt streets for new uses amid COVID-19. AARP published design briefs responding to the impact of COVID-19 on commercial areas, informing local leaders to make their communities more livable and protect their residents from COVID-19 [90]. Their design briefs include Open Streets programs to encourage walking and bicycling to dining and retail areas. A non-profit organization called Bike & Walk Montclair launched a campaign to respond to the pandemic mobility challenges by weighing bike lanes and opening more spaces for pedestrians and bicyclists [91].
Recommendations for future practice and research
Based on the knowledge gaps mentioned above, longitudinal studies utilizing more vigorous sampling strategies and objective measures of physical activity can help increase the study generalizability and reduce the survey recall bias. More work is needed to investigate the long-term effects of COVID-19 on physical activity and health-related outcomes to further explore how people are recovering from COVID-19. Moreover, further research is needed to investigate the impact of COVID-19 on vulnerable populations (eg, older adults and children) and identify potential social and environmental strategies for promoting active living of everyone after COVID-19.
Given the significance of community environments in maintaining and promoting health behaviors and health outcomes, and ith the limited empirical evidence on the roles of community environments amid COVID-19, more studies are needed to explore how they can help people cope with COVID-19 and how the design dilemma can be addressed in the future. Stronger collaborations between public health and urban planning/design sectors are needed to identify locally implementable environmental strategies that can help respond to the multiple public health challenges that this global pandemic has brought. Drawing from the findings of this review, environmental strategies needing further collaborative efforts include the following.
Consider potential negative impacts of urbanization and compact developments on physical activity (decreases in physical activity) and health (rapid spread of infections) during pandemics like COVID-19.
Highlight the importance of providing free and accessible outdoor spaces for all populations (equity).
Consider shared backyards for residents of high-density dwelling types such as apartments and public/affordable housing, where provision of private outdoor spaces is difficult.
Consider transforming community vacant land into small parks/green spaces in areas lacking safe outdoor resources to support physical activity and help people cope with mental health problems.
Consider the importance of safe neighborhood streets and sidewalks to serve as health infrastructure supporting healthy physical activity, especially when other physical activity resources may be unsafe or closed during pandemics like COVID-19.
In addition, many of the pandemic-responsive design/planning strategies proposed and implemented by various organizations and communities have not been examined for their effectiveness. Future research that documents and quantifies the specific benefits and costs of the various pandemic-responsive strategies is needed to develop evidence-based intervention strategies to enable our cities to be better prepared for future pandemics and other public health challenges. In addition to those environmental strategies, educational or promotional programs/events or the use of walking/cycling applications can be encouraged to promote engagement in physical activity.
Limitations of this rapid review
This rapid review has two major limitations. First, we only used one database for the comprehensive database searches to ensure a timely review. However, Google Scholar searches were also conducted as a supplemental approach to help reduce the possibility of omitting important studies. Second, this review was limited to peer-reviewed quantitative studies in English, which may result in missing relevant qualitative studies and those written in other languages and/or not peer-reviewed. We, however, provided a brief discussion on the grey literature highlighting a few published guidelines most relevant to this review.
CONCLUSION
Evidence suggests an overall negative impact of COVID-19 on physical activity, with differential effects across different sub-populations. Significant knowledge gaps are also found in the roles of community environments that can promote healthy outdoor activities during the pandemic with reduced safety risks. A major paradigm shift is expected in planning and design to address the dilemma of creating compact and sustainable built environments while providing sufficient protection from infectious diseases and flexibility to accommodate the dynamic needs of outdoor activities during and beyond the pandemic.
Additional material
Acknowledgments
Availability of data and materials: The data extraction material (search terms and data extraction table) are attached as a supplementary table. All papers included in our review are cited.
Footnotes
Funding: There is no funding to declare for this study.
Authorship contributions: AP: Conceptualization, Methodology, Validation, Writing – Original Draft, Writing – Review & Editing, Project Administration. SZ: Conceptualization, Methodology, Data Curation, Writing – Review & Editing. HY: Data Extraction, Validation. JJ: Data Extraction, Validation. CL: Conceptualization, Writing – Review & Editing, Supervision. All authors approved the final version for submission.
Competing interests: The authors have completed the ICMJE Declaration of Interest Form (available upon request from the corresponding author), and declare no conflicts of interest.
REFERENCES
- 1.World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020 2020. Available: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020. Accessed: 10 July 2021.
- 2.Google LLC. Google COVID-19 Community Mobility Reports 2021 [Available from: https://www.google.com/covid19/mobility/. Accessed: 31 Oct 2021.
- 3.Centers for Disease Control and Prevention. Benefits of Physical Activity 2021. Available: https://www.cdc.gov/physicalactivity/basics/pa-health/index.htm. Accessed: 10 July 2021.
- 4.Reiner AM, Jekauc D, Niermann C, Woll A.Long-term health benefits of physical activity–a systematic review of longitudinal studies. BMC Public Health. 2013;13:813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peluso MAM.Andrade LHSGd. Physical activity and mental health: the association between exercise and mood. Clinics (São Paulo). 2005;60:61-70. 10.1590/S1807-59322005000100012 [DOI] [PubMed] [Google Scholar]
- 6.Anderson E, Durstine JL.Physical activity, exercise, and chronic diseases: A brief review. Sports Med Health Sci. 2019;1:3-10. 10.1016/j.smhs.2019.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hayes C, Kriska A.Role of physical activity in diabetes management and prevention. J Am Diet Assoc. 2008;108:S19-23. 10.1016/j.jada.2008.01.016 [DOI] [PubMed] [Google Scholar]
- 8.US Department of Health and Human Services. Step It Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities. 2015. [PubMed] [Google Scholar]
- 9.Committee on Environmental Health The built environment: designing communities to promote physical activity in children. Pediatrics. 2009;123:1591-8. 10.1542/peds.2009-0750 [DOI] [PubMed] [Google Scholar]
- 10.Sallis JF, Floyd MF, Rodríguez DA, Saelens BE.Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125:729-37. 10.1161/CIRCULATIONAHA.110.969022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stokols D.Establishing and maintaining healthy environments: toward a social ecology of health promotion. Am Psychol. 1992;47:6. 10.1037/0003-066X.47.1.6 [DOI] [PubMed] [Google Scholar]
- 12.Bronfenbrenner U. Ecological models of human development: Worth Publishers; 1994. 37-43 p. [Google Scholar]
- 13.Tison GH, Avram R, Kuhar P, Abreau S, Marcus GM, Pletcher MJ, et al. Worldwide effect of COVID-19 on physical activity: a descriptive study. Ann Intern Med. 2020;173:767-70. 10.7326/M20-2665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marques de Miranda D, da Silva Athanasio B, de Sena Oliveira AC, Silva ACS.How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disaster Risk Reduct. 2020;51:101845. 10.1016/j.ijdrr.2020.101845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Usher K, Jackson D, Durkin J, Gyamfi N, Bhullar N.Pandemic-related behaviours and psychological outcomes: A rapid literature review to explain COVID-19 behaviours. Int J Ment Health Nurs. 2020;29:1018-34. 10.1111/inm.12790 [DOI] [PubMed] [Google Scholar]
- 16.Vindegaard N, Benros ME.COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun. 2020;89:531-42. 10.1016/j.bbi.2020.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Megahed NA, Ghoneim EM.Antivirus-built environment: Lessons learned from Covid-19 pandemic. Sustain Cities Soc. 2020;61:102350. 10.1016/j.scs.2020.102350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Effective Public Health Practice Project. Quality Assessment Tool for Quantitative Studies 1998. Available: https://merst.ca/ephpp/. Accessed: 10 July 2021.
- 19.Zhong S, Lee C, Foster M, Bian J.Intergenerational communities: A systematic literature review of intergenerational interactions and older adults’ health-related outcomes. Soc Sci Med. 2020;264:113374. 10.1016/j.socscimed.2020.113374 [DOI] [PubMed] [Google Scholar]
- 20.Srivastav AK, Sharma N, Samuel AJ.Impact of Coronavirus disease-19 (COVID-19) lockdown on physical activity and energy expenditure among physiotherapy professionals and students using web-based open E-survey sent through WhatsApp, Facebook and Instagram messengers. Clin Epidemiol Glob Health. 2021;9:78-84. 10.1016/j.cegh.2020.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruiz-Roso MB, Knott-Torcal C, Matilla-Escalante DC, Garcimartín A, Sampedro-Nuñez MA, Dávalos A, et al. COVID-19 lockdown and changes of the dietary pattern and physical activity habits in a cohort of patients with type 2 diabetes mellitus. Nutrients. 2020;12:2327. 10.3390/nu12082327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Biviá-Roig G, La Rosa VL, Gómez-Tébar M, Serrano-Raya L, Am-Cuenca JJ, Caruso S, et al. Analysis of the impact of the confinement resulting from COVID-19 on the lifestyle and psychological wellbeing of Spanish pregnant women: an Internet-based cross-sectional survey. Int J Environ Res Public Health. 2020;17:5933. 10.3390/ijerph17165933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Di Stefano V, Battaglia G, Giustino V, Gagliardo A, D’Aleo M, Giannini O, et al. Significant reduction of physical activity in patients with neuromuscular disease during COVID-19 pandemic: the long-term consequences of quarantine. J Neurol. 2021;268:20-6. 10.1007/s00415-020-10064-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.López-Sánchez GF, López-Bueno R, Gil-Salmerón A, Zauder R, Skalska M, Jastrzębska J, et al. Comparison of physical activity levels in Spanish adults with chronic conditions before and during COVID-19 quarantine. Eur J Public Health. 2021;31:161-6. 10.1093/eurpub/ckaa159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dunton GF, Do B, Wang SD.Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the US. BMC Public Health. 2020;20:1351. 10.1186/s12889-020-09429-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Assaloni R, Pellino VC, Puci MV, Ferraro OE, Lovecchio N, Girelli A, et al. Coronavirus disease (Covid-19): how does the exercise practice in active people with type 1 diabetes change? A preliminary survey. Diabetes Res Clin Pract. 2020;166:108297. 10.1016/j.diabres.2020.108297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elran-Barak R, Mozeikov M.One month into the reinforcement of social distancing due to the COVID-19 outbreak: subjective health, health behaviors, and loneliness among people with chronic medical conditions. Int J Environ Res Public Health. 2020;17:5403. 10.3390/ijerph17155403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sassone B, Mandini S, Grazzi G, Mazzoni G, Myers J, Pasanisi G.Impact of COVID-19 pandemic on physical activity in patients with implantable cardioverter-defibrillators. J Cardiopulm Rehabil Prev. 2020;40:285. 10.1097/HCR.0000000000000539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Romero-Blanco C, Rodríguez-Almagro J, Onieva-Zafra MD, Parra-Fernández ML, Prado-Laguna MDC, Hernández-Martínez A.Physical activity and sedentary lifestyle in university students: changes during confinement due to the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17:6567. 10.3390/ijerph17186567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vetrovsky T, Frybova T, Gant I, Semerad M, Cimler R, Bunc V, et al. The detrimental effect of COVID-19 nationwide quarantine on accelerometer-assessed physical activity of heart failure patients. ESC Heart Fail. 2020;7:2093-7. 10.1002/ehf2.12916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hemphill NM, Kuan MT, Harris KC.Reduced physical activity during COVID-19 pandemic in children with congenital heart disease. Can J Cardiol. 2020;36:1130-4. 10.1016/j.cjca.2020.04.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pietrobelli A, Pecoraro L, Ferruzzi A, Heo M, Faith M, Zoller T, et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity (Silver Spring). 2020;28:1382-5. 10.1002/oby.22861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Majumdar P, Biswas A, Sahu S.COVID-19 pandemic and lockdown: cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol Int. 2020;37:1191-200. 10.1080/07420528.2020.1786107 [DOI] [PubMed] [Google Scholar]
- 34.Suzuki Y, Maeda N, Hirado D, Shirakawa T, Urabe Y.Physical activity changes and its risk factors among community-dwelling Japanese older adults during the COVID-19 epidemic: associations with subjective well-being and health-related quality of life. Int J Environ Res Public Health. 2020;17:6591. 10.3390/ijerph17186591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cransac-Miet A, Zeller M, Chagué F, Faure AS, Bichat F, Danchin N, et al. Impact of COVID-19 lockdown on lifestyle adherence in stay-at-home patients with chronic coronary syndromes: Towards a time bomb. Int J Cardiol. 2021;323:285-7. 10.1016/j.ijcard.2020.08.094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carroll N, Sadowski A, Laila A, Hruska V, Nixon M, Ma DW, et al. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients. 2020;12:2352. 10.3390/nu12082352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ghosh A, Arora B, Gupta R, Anoop S, Misra A.Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes Metab Syndr. 2020;14:917-20. 10.1016/j.dsx.2020.05.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Venter ZS, Barton DN, Gundersen V, Figari H, Nowell M.Urban nature in a time of crisis: recreational use of green space increases during the COVID-19 outbreak in Oslo, Norway. Environ Res Lett. 2020;15:104075. 10.1088/1748-9326/abb396 [DOI] [Google Scholar]
- 39.Pépin JL, Bruno RM, Yang R-Y, Vercamer V, Jouhaud P, Escourrou P, et al. Wearable activity trackers for monitoring adherence to home confinement during the COVID-19 pandemic worldwide: data aggregation and analysis. J Med Internet Res. 2020;22:e19787. 10.2196/19787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Park J.Changes in subway ridership in response to COVID-19 in Seoul, South Korea: Implications for social distancing. Cureus. 2020;12:e7668. 10.7759/cureus.7668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Park S, Kim B, Lee J.Social Distancing and Outdoor Physical Activity During the COVID-19 Outbreak in South Korea: Implications for Physical Distancing Strategies. Asia Pac J Public Health. 2020;32:360-2. 10.1177/1010539520940929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Constandt B, Thibaut E, De Bosscher V, Scheerder J, Ricour M, Willem A.Exercising in times of lockdown: an analysis of the impact of COVID-19 on levels and patterns of exercise among adults in Belgium. Environ Resour Econ (Dordr). 2020;17:4144. 10.3390/ijerph17114144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sehra ST, George M, Wiebe DJ, Fundin S, Baker JF.Cell phone activity in categories of places and associations with growth in cases of COVID-19 in the US. JAMA Intern Med. 2020;180:1614-20. 10.1001/jamainternmed.2020.4288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Saha J, Barman B, Chouhan P.Lockdown for COVID-19 and its impact on community mobility in India: An analysis of the COVID-19 Community Mobility Reports, 2020. Child Youth Serv Rev. 2020;116:105160. 10.1016/j.childyouth.2020.105160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Castañeda-Babarro A, Arbillaga-Etxarri A, Gutiérrez-Santamaría B, Coca A.Physical activity change during COVID-19 confinement. Int J Environ Res Public Health. 2020;17:6878. 10.3390/ijerph17186878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Effects of COVID-19 home confinement on physical activity and eating behaviour Preliminary results of the ECLB-COVID19 international online-survey. Nutrients. 2020;12:1583. 10.3390/nu12061583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gallo LA, Gallo TF, Young SL, Moritz KM, Akison LK.The impact of isolation measures due to COVID-19 on energy intake and physical activity levels in Australian university students. Nutrients. 2020;12:1865. 10.3390/nu12061865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zheng C, Huang WY, Sheridan S, Sit CH-P, Chen X-K, Wong SH-S.COVID-19 pandemic brings a sedentary lifestyle in young adults: a cross-sectional and longitudinal study. Int J Environ Res Public Health. 2020;17:6035. 10.3390/ijerph17176035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pišot S, Milovanović I, Šimunič B, Gentile A, Bosnar K, Prot F, et al. Maintaining everyday life praxis in the time of COVID-19 pandemic measures (ELP-COVID-19 survey). Eur J Public Health. 2020;30:1181-6. 10.1093/eurpub/ckaa157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yang Y, Koenigstorfer J.Determinants of physical activity maintenance during the Covid-19 pandemic: a focus on fitness apps. Transl Behav Med. 2020;10:835-42. 10.1093/tbm/ibaa086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mitra R, Moore SA, Gillespie M, Faulkner G, Vanderloo LM, Chulak-Bozzer T, et al. Healthy movement behaviours in children and youth during the COVID-19 pandemic: Exploring the role of the neighbourhood environment. Health Place. 2020;65:102418. 10.1016/j.healthplace.2020.102418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Di Sebastiano KM, Chulak-Bozzer T, Vanderloo LM, Faulkner G.Don’t walk so close to me: physical distancing and adult physical activity in Canada. Front Psychol. 2020;11:1895. 10.3389/fpsyg.2020.01895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ong JL, Lau T, Massar SA, Chong ZT, Ng BK, Koek D, et al. COVID-19-related mobility reduction: heterogenous effects on sleep and physical activity rhythms. Sleep. 2021;44:a179. 10.1093/sleep/zsaa179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Meyer J, McDowell C, Lansing J, Brower C, Smith L, Tully M, et al. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int J Environ Res Public Health. 2020;17:6469. 10.3390/ijerph17186469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lesser IA, Nienhuis CP.The impact of COVID-19 on physical activity behavior and well-being of Canadians. Int J Environ Res Public Health. 2020;17:3899. 10.3390/ijerph17113899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.López-Bueno R, Calatayud J, Andersen LL, Balsalobre-Fernández C, Casaña J, Casajús JA, et al. Immediate impact of the COVID-19 confinement on physical activity levels in Spanish adults. Sustainability. 2020;12:5708. 10.3390/su12145708 [DOI] [Google Scholar]
- 57.Moore SA, Faulkner G, Rhodes RE, Brussoni M, Chulak-Bozzer T, Ferguson LJ, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. 2020;17:85. 10.1186/s12966-020-00987-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gallè F, Sabella EA, Ferracuti S, De Giglio O, Caggiano G, Protano C, et al. Sedentary behaviors and physical activity of Italian undergraduate students during lockdown at the time of CoViD− 19 pandemic. Int J Environ Res Public Health. 2020;17:6171. 10.3390/ijerph17176171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Qi M, Li P, Moyle W, Weeks B, Jones C.Physical activity, health-related quality of life, and stress among the Chinese adult population during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17:6494. 10.3390/ijerph17186494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gilic B, Ostojic L, Corluka M, Volaric T, Sekulic D.Contextualizing Parental/Familial influence on physical activity in adolescents before and during COVID-19 pandemic: a prospective analysis. Children (Basel). 2020;7:125. 10.3390/children7090125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.López-Bueno R, Calatayud J, Casaña J, Casajús JA, Smith L, Tully MA, et al. COVID-19 confinement and health risk behaviors in Spain. Front Psychol. 2020;11:1426. 10.3389/fpsyg.2020.01426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Azizi A, Achak D, Aboudi K, Saad E, Nejjari C, Nouira Y, et al. Health-related quality of life and behavior-related lifestyle changes due to the COVID-19 home confinement: Dataset from a Moroccan sample. Data Brief. 2020;32:106239. 10.1016/j.dib.2020.106239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ruíz-Roso MB, de Carvalho Padilha P, Matilla-Escalante DC, Brun P, Ulloa N, Acevedo-Correa D, et al. Changes of physical activity and ultra-processed food consumption in adolescents from different countries during Covid-19 pandemic: An observational study. Nutrients. 2020;12:2289. 10.3390/nu12082289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bourdas DI, Zacharakis ED.Evolution of changes in physical activity over lockdown time: Physical activity datasets of four independent adult sample groups corresponding to each of the last four of the six COVID-19 lockdown weeks in Greece. Data Brief. 2020;32:106301. 10.1016/j.dib.2020.106301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sánchez-Sánchez E, Ramírez-Vargas G, Avellaneda-López Y, Orellana-Pecino JI, García-Marín E, Díaz-Jimenez J.Eating habits and physical activity of the Spanish population during the COVID-19 pandemic period. Nutrients. 2020;12:2826. 10.3390/nu12092826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gallè F, Sabella EA, Da Molin G, De Giglio O, Caggiano G, Di Onofrio V, et al. Understanding knowledge and behaviors related to CoViD–19 epidemic in Italian undergraduate students: the EPICO study. Int J Environ Res Public Health. 2020;17:3481. 10.3390/ijerph17103481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yamada K, Yamaguchi S, Sato K, Fuji T, Ohe T.The COVID-19 outbreak limits physical activities and increases sedentary behavior: A possible secondary public health crisis for the elderly. J Orthop Sci. 2020;25:1093. 10.1016/j.jos.2020.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cancello R, Soranna D, Zambra G, Zambon A, Invitti C.Determinants of the lifestyle changes during COVID-19 pandemic in the residents of Northern Italy. Int J Environ Res Public Health. 2020;17:6287. 10.3390/ijerph17176287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sun S, Folarin AA, Ranjan Y, Rashid Z, Conde P, Stewart C, et al. Using smartphones and wearable devices to monitor behavioral changes during COVID-19. J Med Internet Res. 2020;22:e19992. 10.2196/19992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.de Lannoy L, Rhodes RE, Moore SA, Faulkner G, Tremblay MS.Regional differences in access to the outdoors and outdoor play of Canadian children and youth during the COVID-19 outbreak. Can J Public Health. 2020;111:988-94. 10.17269/s41997-020-00412-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Colley RC, Bushnik T, Langlois K.Exercise and screen time during the COVID-19 pandemic. Health Rep. 2020;31:3-11. [DOI] [PubMed] [Google Scholar]
- 72.Đogaš Z, Lušić Kalcina L, Pavlinac Dodig I, Demirović S, Madirazza K, Valić M, et al. The effect of COVID-19 lockdown on lifestyle and mood in Croatian general population: a cross-sectional study. Croat Med J. 2020;61:309-18. 10.3325/cmj.2020.61.309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schnitzer M, Schöttl SE, Kopp M, Barth M.COVID-19 stay-at-home order in Tyrol, Austria: sports and exercise behaviour in change? Public Health. 2020;185:218-20. 10.1016/j.puhe.2020.06.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Phillipou A, Meyer D, Neill E, Tan EJ, Toh WL, Van Rheenen TE, et al. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. Int J Eat Disord. 2020;53:1158-65. 10.1002/eat.23317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fong BY, Wong M, Law VT, Lo MF, Ng TK, Yee HH, et al. Relationships between physical and social behavioural changes and the mental status of homebound residents in Hong Kong during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17:6653. 10.3390/ijerph17186653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rice WL, Mateer TJ, Reigner N, Newman P, Lawhon B, Taff BD.Changes in recreational behaviors of outdoor enthusiasts during the COVID-19 pandemic: analysis across urban and rural communities. J Urban Econ. 2020;6:a020. 10.1093/jue/juaa020 [DOI] [Google Scholar]
- 77.Beck MJ, Hensher DA.Insights into the impact of COVID-19 on household travel and activities in Australia–The early days under restrictions. Transp Policy (Oxf). 2020;96:76-93. 10.1016/j.tranpol.2020.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nguyen DV, Pham GH, Nguyen DN.Impact of the Covid-19 pandemic on perceptions and behaviors of university students in Vietnam. Data Brief. 2020;31:105880. 10.1016/j.dib.2020.105880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Day BH.The value of greenspace under pandemic lockdown. Environ Resour Econ (Dordr). 2020;76:1-25. 10.1007/s10640-020-00489-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Booth FW, Roberts CK, Laye MJ.Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2:1143. 10.1002/cphy.c110025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Centers for Disease Control and Prevention. Lack of Physical Activity. Atlanta, GA: CDC; 2019. [Google Scholar]
- 82.Tanha T, Wollmer P, Thorsson O, Karlsson MK, Lindén C, Andersen LB, et al. Lack of physical activity in young children is related to higher composite risk factor score for cardiovascular disease. Acta Paediatr. 2011;100:717-21. 10.1111/j.1651-2227.2011.02226.x [DOI] [PubMed] [Google Scholar]
- 83.Saxena S, Van Ommeren M, Tang K, Armstrong T.Mental health benefits of physical activity. J Ment Health. 2005;14:445-51. 10.1080/09638230500270776 [DOI] [Google Scholar]
- 84.Yen IH, Michael YL, Perdue L.Neighborhood environment in studies of health of older adults: a systematic review. Am J Prev Med. 2009;37:455-63. 10.1016/j.amepre.2009.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kerr J, Rosenberg D, Frank L.The role of the built environment in healthy aging: Community design, physical activity, and health among older adults. J Plann Lit. 2012;27:43-60. 10.1177/0885412211415283 [DOI] [Google Scholar]
- 86.Christian H, Zubrick SR, Foster S, Giles-Corti B, Bull F, Wood L, et al. The influence of the neighborhood physical environment on early child health and development: A review and call for research. Health Place. 2015;33:25-36. 10.1016/j.healthplace.2015.01.005 [DOI] [PubMed] [Google Scholar]
- 87.Saelens BE, Handy SL.Built environment correlates of walking: a review. Med Sci Sports Exerc. 2008;40(7 Suppl):S550. 10.1249/MSS.0b013e31817c67a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Freedman VA, Grafova IB, Rogowski J.Neighborhoods and chronic disease onset in later life. Am J Public Health. 2011;101:79-86. 10.2105/AJPH.2009.178640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tomey K, Roux AVD, Clarke P, Seeman T.Associations between neighborhood characteristics and self-rated health: a cross-sectional investigation in the Multi-Ethnic Study of Atherosclerosis (MESA) cohort. Health Place. 2013;24:267-74. 10.1016/j.healthplace.2013.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.American Association of Retired Persons. Helping Commercial Districts Manage and Respond to COVID-19. 2020. Available: https://www.aarp.org/livable-communities/tool-kits-resources/info-2020/main-street-america-covid-briefs.html. Accessed: 10 July 2021.
- 91.Martin J. Montclair weighing bike lanes, street closures during pandemic. 2020. Available: https://www.northjersey.com/story/news/essex/2020/06/03/montclair-nj-weighing-bike-lanes-street-closures-during-pandemic/5258260002/. Accessed: 10 July 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


