We read with great interest the recent findings in the study by Zampogna et al. 1 entitled “Time course of exercise capacity in patients recovering from COVID-19-associated pneumonia.” The central objective of the study was to evaluate the exercise capacity of patients four weeks after hospital discharge and after a three-month follow-up period. To that end, the authors divided the patients into two groups using the cutoff point of 75% of the predicted value for the six-minute walk distance. The main finding of that study 1 was that both groups recovered their exercise capacity and functional status after three months of follow-up. The study premise is interesting (functional assessment of patients who recovered from COVID-19) and provides the reader with important information about pulmonary rehabilitation strategies, which is one of the main challenges for COVID-19 survivors. However, some aspects of the study are subject to criticism.
Patients with COVID-19 and prolonged length of hospital stay can suffer from various functional limitations after discharge. Post-COVID symptoms include neuromusculoskeletal disorders, such as neuropathy and muscle weakness; dyspnea; severe hypoxemia; anxiety and/or depression; significant weight loss; and cardiovascular sequelae. 2 , 3 Therefore, these functional limitations need to be explored not only after discharge, but also during early rehabilitation in the convalescence phase. 4 In this context, a mobility team combined with interdisciplinary assistance 5 are essential to make the functionality of such patients to improve progressively, resulting in better quality of life and enabling the patients to return to their work activities. 6 , 7 However, it is necessary to consider some concerns related to that study. 1 There was a lack of clarity regarding the time course of the functional assessments performed, the importance and objective of the functional tests selected, and some details about the proposed rehabilitation program carried out during the follow-up. A more consistent description of the methodology should have rigorously been carried out. In this context, the study has its originality, importance, and clinical applicability jeopardized.
Considering that the mean length of ICU stay was 43 days, it is expected that the patients presented with pronounced limitations in functionality and performance of activities of daily living (ADL) and required to be followed up after discharge. The study started the evaluations approximately four weeks after discharge (4 ± 1 weeks), that is, they were extremely late, variability was high, and no details regarding the functional recovery process between discharge and beginning of follow-up were provided. In this context, it is highly recommended and desirable that rehabilitation programs that encourage functional recovery of these long-hospitalized patients should and can be started during hospitalization and need to be continued immediately after hospital discharge. 8 In addition, it is not clear in that study 1 whether the patients who were recruited after discharge had been admitted to different hospitals and, therefore, whether they had received equivalent pulmonary rehabilitation during hospitalization, which could impact their functionality after discharge.
The study has a bias in its own design, because the individuals were selected on the basis of their functional capacity and there was an imbalance in the number of individuals in each group that underwent a rehabilitation program (73% and 33% of the individuals in the <75% and ≥75% groups, respectively), evidencing a heterogeneous load of exercise training between the groups. It is highly likely that functional recovery in the <75% group was mainly due to the rehabilitation program implemented in which the patients were inserted than simply due to the time course. In addition, the study proved to be precarious since it did not present the rehabilitation structure in which the patients were submitted to from the standpoint of location (home or rehabilitation center), frequency, intensity, modality of exercise and supervision (face-to-face, telerehabilitation, unsupervised, or a combination of those). 8 In addition, heterogeneous compliance of patients in rehabilitation programs may compromise the results of the functional outcomes investigated. 9 The authors should have explored all of these aspects in more details, and, therefore, that study lacks reproducibility. 1
Regarding functional assessments, the authors mentioned that the six-minute walk test was used in order to assess lower extremity function, but COVID-19 patients report increased dyspnea and fatigue symptoms associated with impaired performance of ADL, particularly those who survived hospitalization. 10 In this context, most of ADL require elevation of both arms, with and without support. 11 Therefore, because the assessment of ADL also requires the assessment of the functionality of the upper limbs, that would be highly recommended, since therapies aimed at improving this function can also contribute to reducing dyspnea and muscle fatigue in those patients and to helping select a physical training program that can improve muscle dysfunction especially targeted for promoting functional independence for performing daily tasks in the home environment. Following this line of reasoning, it is highly recommended to assess the mechanisms of upper extremity muscle dysfunction, which can be measured and confirmed by different tests. 12
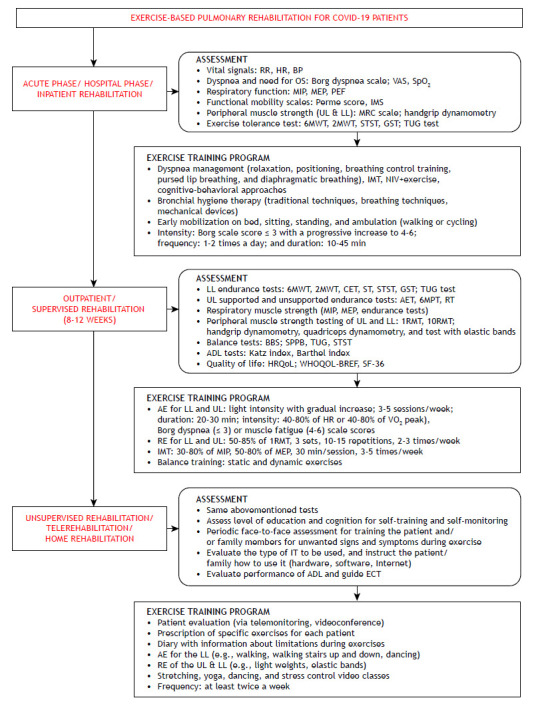
In conclusion, despite the relevance of the study by Zampogna et al., 1 given that the temporal evolution of functional capacity in patients affected by COVID-19 can be impacted by early and late rehabilitation, the conclusion of the study needs to be analyzed with caution. The assessment of functional capacity is important and should be directed to the phase of pulmonary rehabilitation (Figure 1). In addition, the absence of differences in the functional recovery of those individuals after a three-month period, considering that different loads of pulmonary rehabilitation were applied in both groups and no information regarding the protocol of physical exercise (intensity, duration, and number of sessions) were described, indicates that the results of that study should be evaluated with reservations. Therefore, it would be fair to assume that, above all, if the two groups were to receive equally exercise-based rehabilitation, the results would be likely to be different. Finally, we strongly recommend that a broader assessment of ADL should include activities that incorporate the upper limbs, because they are strongly associated with improvements in ADL, symptoms, and, consequently, quality of life in COVID-19 survivors.
Figure 1. Recommendations for assessment and physical training during different phases of pulmonary rehabilitation in COVID-19 patients. BP: blood pressure; OS: oxygen supplementation; VAS: visual analog scale; Perme: Perme Intensive Care Unit Mobility Score; IMS: ICU mobility scale; UL: upper limbs; LL: lower limbs; MRC: Medical Research Council scale; 6MWT: six-minute walk test; 2MWT: two-minute walk test; STST: sit-to-stand test; GST: gait speed test; TUG: timed up and go; IMT: inspiratory muscle training; NIV: noninvasive ventilation; CET: cycle ergometer test; ST: step test; AET: arm ergometer test; 6MPT: six-minute pegboard test; RT: ring test; 1RMT: one-repetition maximum test; 10RMT: ten-repetition maximum test; BBS: Berg balance scale; SPPB: Short Physical Performance Battery; ADL: activities of daily living; HRQoL: health-related quality of life; WHOQOL-BREF: World Health Organization Quality of Life Instrument, brief version; SF-36: Medical Outcomes Study 36-item Short-Form Health Survey; AE: aerobic exercise; RE: resistance exercise; IT: information technology; and ECT: energy conservation techniques.
REFERENCES
- 1.Zampogna E, Ambrosino N, Saderi L, Sotgi G, Bottini P, Pignatti P. Time course of exercise capacity in patients recovering from COVID-19-associated pneumonia J Bras. Pneumol. 2021;47(4):20210076–20210076. doi: 10.36416/1806-3756/e20210076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martillo M, Dangayach N, Tabacof L, Spielman LA, Dams-O'Connor K, Chan CC, et al. Postintensive Care Syndrome in Survivors of Critical Illness Related to Coronavirus. Disease. 2019:Cohort–Cohort. doi: 10.1097/CCM.0000000000005014. [DOI] [PubMed] [Google Scholar]
- 3.Wiertz CMH, Vints WAJ, Maas GJCM, Rasquin SMC, van Horn YY, Dremmen MPM. COVID-19 Patient Characteristics in the First Phase of Postintensive Care Rehabilitation. Arch Rehabil Res Clin Transl. 2021;3(2):100108–100108. doi: 10.1016/j.arrct.2021.100108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silva RN, Goulart CDL, Oliveira MR, Tacao GY, Back GD, Severin R, et al. Cardiorespiratory and skeletal muscle damage due to COVID-19: making the urgent case for rehabilitation [published online ahead of print, 2021 Mar 4] Expert Rev Respir Med. 2021:1–14. doi: 10.1080/17476348.2021.1893169. [DOI] [PubMed] [Google Scholar]
- 5.Gemelli Against COVID-19 Post-Acute Care Study Group Post-COVID-19 global health strategies the need for an interdisciplinary approach. Aging Clin Exp Res. 2020;32(8):1613–1620. doi: 10.1007/s40520-020-01616-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reina-Gutiérrez S, Torres-Costoso A, Martínez-Vizcaíno V, Núñez de Arenas-Arroyo S, Fernández-Rodríguez R, Pozuelo-Carrascosa DP. Effectiveness of Pulmonary Rehabilitation in Interstitial Lung Disease, Including Coronavirus Diseases: A Systematic Review and Meta-analysis. Arch Phys Med Rehabil. 2021 doi: 10.1016/j.apmr.2021.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tozato C, Ferreira BFC, Dalavina JP, Molinari CV, Alves VLDS. Cardiopulmonary rehabilitation in post-COVID-19 patients case series. Rev Bras Ter Intensiva. 2021;33(1):167–171. doi: 10.5935/0103-507X.20210018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gautam AP, Arena R, Dixit S, Borghi-Silva A. Pulmonary rehabilitation in COVID-19 pandemic era The need for a revised approach. Respirology. 2020;25(12):1320–1322. doi: 10.1111/resp.13946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goulart CDL, Silva RN, Oliveira MR, Guizilini S, Rocco IS, Mendez VMF, et al. Lifestyle and rehabilitation during the COVID-19 pandemic: guidance for health professionals and support for exercise and rehabilitation programs [published online ahead of print, 2021 Apr 28] Expert Rev Anti Infect Ther. 2021:1–12. doi: 10.1080/14787210.2021.1917994. [DOI] [PubMed] [Google Scholar]
- 10.Belli S, Balbi B, Prince I, Cattaneo D, Masocco F, Zaccaria S. Low physical functioning and impaired performance of activities of daily life in COVID-19 patients who survived hospitalisation. Eur Respir J. 2020;56(4):2002096–2002096. doi: 10.1183/13993003.02096-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Panka GF, Oliveira MM, França DC, Parreira VF, Britto RR, Velloso M. Ventilatory and muscular assessment in healthy subjects during an activity of daily living with unsupported arm elevation. Rev Bras Fisioter. 2010;14(4):337–344. doi: 10.1590/S1413-35552010005000013. [DOI] [PubMed] [Google Scholar]
- 12.Marklund S, Bui KL, Nyberg A. Measuring and monitoring skeletal muscle function in COPD current perspectives. Int J Chron Obstruct Pulmon Dis. 2019;14:1825–1838. doi: 10.2147/COPD.S178948. [DOI] [PMC free article] [PubMed] [Google Scholar]


