Graphical abstract
Keywords: COVID-19, Perceived risk, Perception, Vaccine intent
Abstract
Background
COVID-19 pandemic has caused significant morbidity and mortality globally. As vaccines have been developed under expedited conditions, their safety and efficacy are being questioned by some populations leading to vaccine hesitancy, resulting in delayed vaccine uptake and herd immunity. This study aims to adopt a combination of Health Belief Model and other independent risk factors associated with high vaccine acceptance.
Methods
An anonymized cross-sectional survey was distributed between 15 January and 3 February 2021 across Singapore, Hong Kong and Australia among adult respondents through a certified online panel. Exploratory factor analysis and confirmatory factor analysis were carried out to assess perception constructs followed by multivariate regression modelling to assess factors associated with high vaccine acceptance against SARS_CoV-2.
Results
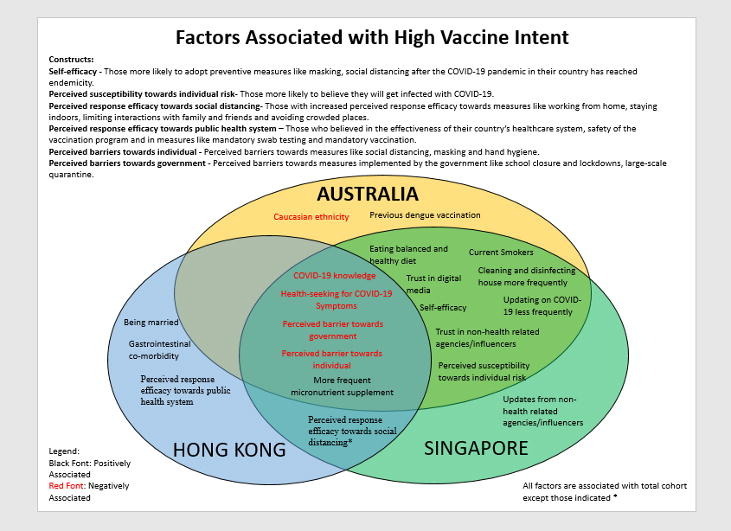
A total of 3,133 anonymised participants from Singapore (n = 1,009), Australia (n = 1,118) and Hong Kong (n = 1,006) completed the survey. While age and gender were not significantly associated, Asian ethnicity, current smokers and self-efficacy were significant associated factors of increased vaccine acceptance. While specific practices like taking micronutrients more frequently, cleaning and disinfecting their house more often were positively associated with increased vaccine acceptance, seeking medical help for COVID-19 symptoms like loss of smell/taste and overall COVID-19 knowledge score were negatively associated. Increased likelihood of vaccine acceptance was seen among those that obtained COVID-19 information less frequently and used digital media or non-health-related sources like influencers as a source of information. Among the eight perception constructs, perceived susceptibility and perceived response efficacy were positively associated, while perceived barriers were negatively associated with high vaccine acceptance.
Conclusion
While demographic parameters have weak association with vaccine acceptance, perceptions and practices parameters can help to better understand and influence vaccine acceptance. Study findings should provide guidance on the risk communication strategy to enhance vaccine acceptance for vaccination and boosters against new SARS-CoV-2 variants.
1. Introduction
In December 2019, a cluster of coronavirus disease 2019 (COVID-19) cases were first identified in Wuhan, China. The disease has since spread worldwide causing great concerns with countries imposing various degrees of lockdown and travel restrictions. On 11 December 2020, United States Food and Drug Administration (FDA) issued the first emergency use authorization (EUA) of Pfizer-BioNTech COVID-19 vaccine for use in United States [1]. EUA was issued on 14 December 2020 in Singapore and 25 January 2021 in Australia and Hong Kong [2], [3], [4] Subsequently, more vaccines such as Moderna, AstraZeneca, Sinovac and others have been authorized for emergency use across the world.
When COVID-19 vaccines were first approved, vaccine hesitancy and reluctance were observed in certain population, threatening the success of prevention measures against COVID-19. Since then, as vaccination campaigns continue, Australia, Hong Kong and Singapore have 94.1% (population aged 16 and above), 74.9 (population aged 12 and above) and 90% (total population) population vaccinated as of 17 February 2022 [7]. By understanding the risk factors and perceptions that affect people’s intention to get vaccinated may guide policy-decision making process to enhance risk communication so as to increase vaccination uptake. Vaccinating against COVID-19 can help prevent serious illness and death [8]. While studies have looked at cultural, political and racial differences to explain vaccine hesitancy, acceptance and likelihood, COVID-19 vaccination rate has been shown to vary across different phases of the pandemic in each affected country with introduction of newer variants and vaccine options [9], [10].
MacDonald et al. stated that, “Acceptance of vaccination is an outcome behaviour resulting from a complex decision-making process that can be potentially influenced by multiple factors”[11, p. 4162]” While there have been studies looking into various risk factors associated with vaccine uptake [12], a population-based study in Hong Kong concluded that Health Belief Model (HBM) constructs along with independent risk factors can provide an evidence-based model and help implement various vaccination strategies [13]. However, few studies have adopted a combination of this conceptual framework to assess the COVID-19 vaccine intent among population [13]. This study aims to identify key perception constructs and risk factors between residents with high and low COVID-19 vaccine intent from three countries: Australia, Hong Kong and Singapore.
2. Methods
2.1. Study setting and data collection
A cross-sectional anonymised survey was conducted in English in Australia and Singapore while participants in Hong Kong had an additional choice of answering in traditional Chinese. The survey was translated to Chinese using Google Translate and was back translated to English with help of a professional translator, fluent in Chinese and English. Online survey was distributed between 15th January 2021 to 3rd February 2021 to participants aged ≥ 21 years. Survey distribution was undertaken by an external vendor involving participants selected from an online panel belonging to Dynata, an international panel company [14]. The panel members are recruited by means of different sample sources such as panel, web intercept sample and specialty lists in order to target different population thereby increasing diversity and representativeness within each country.
2.2. Survey details
The survey had seven sections: 1) general/demographics, 2) health history, 3) practices, 4) knowledge on COVID-19, 5) perceptions of COVID-19, 6) source of information, and 7) self-efficacy (Supplementary Table 1 for the survey).
A total of 21-items related to practices were designed to understand what safety measures were undertaken by respondents to reduce the risk of contracting/spreading SARS-CoV-2 virus after the first case was detected in their country and before any measures were enforced/advised by their respective governments. Questions on perceptions were adapted from HBM and divided into 4 subsections: perceived susceptibility, perceived severity, perceived response efficacy and perceived barriers [15]. Sources of information were classified as traditional media (television, radio, newspapers), digital media (websites, social media, messaging platforms, emails), medical practitioners and health related governmental agencies and non-health related governmental agencies and people (family/friends, influencers, employers, religious groups). Health seeking behaviour, seen as important or sufficient comprised of 12-items further sub-categorised as: 1) general disease specific information related to self: how it is transmitted, how I can prevent its spread, how to recognize its symptoms, the probability of catching it in my country; 2) Seeking care/treatment: how I can protect myself and my family, how it is treated, the development of a vaccine or treatment against it, how I can take care of a person belonging to a high-risk group; 3) global COVID-19 information: the geographic areas where it is present, how it is different from other diseases such as influenza, the authorities’ decisions on new restrictions or relaxed measures, number of infected cases and the death toll. Self-efficacy was determined based on their compliance to adhere to preventive measures and likeliness to continue adopting them after the COVID-19 pandemic reaches endemicity.
2.3. Statistical analysis
Scores were obtained for practices, knowledge, health-seeking behaviour, self-efficacy and perception constructs and were analysed as continuous variables. A score of “1″ was given for every practice that was carried out and converted to percentage based on total number of applicable items for each participant. A similar approach was used to obtain the knowledge score. Health seeking behaviour had three categories with 4 items each and a score of “1” was given for every item that was important or sufficient. To assess self-efficacy, all responses were in a 7-point scale (0- least likely and 7 – very likely). The score for each item was totalled (sum score = 42) and averaged. Descriptive analysis included frequency and percentage for categorical variables and mean and standard deviation for continuous variables. Univariate analysis included Pearson Chi-square and fisher’s exact test for all categorical variables and independent t-test for continuous variables with significance measured at p-value < 0.01 for all sections except perception. All significant variables were assessed using univariate logistic regression with significance measured at p-value < 0.01 (Supplementary Table 2, 3, 4, 7).
Exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) were carried out for section on perceptions. While EFA was used to uncover underlying factorial structure of items under perception, CFA aimed to validate precision and validity of the presumed factorial structure. In rudimentary phase, four potential constructs were assumed to summarize four categories of perception: perceived susceptibility, perceived response efficacy, perceived barrier towards individual and perceived barrier towards government. However, this failed to gain the acceptable fit in CFA due to considerable number of items under perceived response efficacy construct, indicating further modification of assumption. EFA was then conducted using principal axis factoring with Promax rotation to obtain a glimpse at potential factors under the data and some items that had factor loadings lower than 0.4, were excluded. Number of factors were suggested by parallel analysis and based on EFA results, 8-factor model was examined using CFA with Robust ML estimator to test the new assumption of 8 sub-constructs. In this study, 4 types of fit indices were used to evaluate the CFA model: comparative fit indices (CFI), Tucker-Lewis index (TLI), standardized root mean square residual (SRMR) and root mean square error of approximation (RMSEA). The adequate model fit required CFI > 0.90, TLI > 0.90, SRMR < 0.08, RMSEA < 0.08. Internal consistency measures of reliability were Cronbach coefficient alpha, which considers value > 0.7 as acceptable (supplementary Fig. 1 and supplementary Table 5). Score of each construct added in subsequent logistic regression is denoted by an average score of questions under the construct. A total of 8 constructs were obtained for perception and details on items constituting these constructs is provided in supplementary Table 6.
For purpose of this analysis, the cohort was categorised into two groups: low and high intent towards COVID-19 vaccination. Participants that strongly agreed, agreed or somewhat agreed on a 7-point Likert scale that they will voluntarily get vaccinated for COVID-19, if not made mandatory by legislation, were categorised as those with high vaccine intent and the rest were categorised as those with low vaccine intent. All significant demographic and health history variables in univariate model along with knowledge and practice scores were put in a base multivariate model and then variable selection was conducted using stepwise AIC method. Given this base model, significant variables under source of information and self-efficacy that were significant at p-value < 0.01, were added along with all eight perception constructs in order to determine predictors of high intent towards COVID-19 vaccination. Significance in multivariate logistic regression model was considered at p-value < 0.05. Analysis was performed with IBM SPSS statistics software v26 (Chicago, IL, USA) (chi-square, regression analysis) and R 3.6.1 statistics (ECA, CFA).
2.4. Ethics
Electronic consent was obtained from participants who completed and returned the survey. Patient information sheet entailing the consent to use the collected information for research purpose upon completion of the questionnaire, was provided to respondents at start of the survey. Our study posed minimal risks to respondents as it was completely anonymous, and waiver of informed consent would not complicate the rights or welfare of study subjects. It qualified for exemption by National University of Singapore Institutional Review Board (NUS-IRB) from Saw Swee Hock School of Public Health Departmental Ethics Review Committee (SSHSPH-DERC) (SSHSPH-029 (PA1).
3. Results
A total of 3,133 participants from Australia (n = 1,118), Hong Kong (n = 1,006) and Singapore (n = 1,009) were involved in this survey. Females accounted for more than half the respondents in each country while the mean age of respondents was between 43 and 46 years. Respondents in Hong Kong (90%) and Singapore (96%) were primarily Asians, while respondents in Australia were Caucasians (76%). A substantial proportion of respondents were aged > 65 years in Australia (11%) compared to Hong Kong (2.5%) and Singapore (6%). Majority of respondents in Singapore were employed as either manager/directors or were professionals (35%) while 42% of respondents were white collared in Hong Kong while 36% of respondents in Australia were either unemployed, retired, homemaker or students. >50% of respondents in Hong Kong and Singapore had a university degree or higher compared to only 41% in Australia. All three countries had about 20% respondents who had children < 5 years living in the household while 36% in Hong Kong and Singapore had elderly aged > 65 years compared to only 20% in Australia. Proportion of respondents that were diagnosed or had family members diagnosed with COVID-19 was 14% in Australia, 18% in Hong Kong and 9% in Singapore (supplementary Tables 8, 9, 10).
3.1. KAP scores across Australia, Hong Kong and Singapore
Based on univariate regression, practice scores were not significantly associated with vaccine intent levels across all cohorts, although they showed some correlation based on AIC method (Table 1 ). Respondents in Hong Kong and Singapore with a higher mean knowledge score were more likely to have low vaccine intent (Hong Kong: mean 72.9 vs. 65.5; Singapore: mean 72 vs. 64) while those with higher mean self-efficacy score across all countries were more likely to have high vaccine intent (Australia: mean 27.7 vs 30; Hong Kong: mean 31.5 vs. 33; Singapore: mean 31.9 vs 33.5). Significant perception constructs varied across cohorts however those with higher perceived barriers were less likely to have high vaccine intent among respondents from all cohorts. Respondents with higher perceived susceptibility towards individual risk, were more likely to have high vaccine intent in Australia (2.53 vs. 3.10) and Singapore (3.12 vs. 3.51) while respondents with higher perceived response efficacy towards public health system were more likely to have high vaccine intent in Hong Kong (4.31 vs. 4.75) (Table 1).
Table 1.
Knowledge, Practice, Self-efficacy and Perception scores of low and high vaccine acceptances across countries.
| KAP scores | All | Low acceptance Mean (SD) | High acceptance Mean (SD) | p-value | All | Low acceptance Mean (SD) | High acceptance Mean (SD) | p-value | All | Low acceptance Mean (SD) | High acceptance Mean (SD) | p-value | All | Low acceptance Mean (SD) | High acceptance Mean (SD) | p-value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total cohort | Singapore | Hong Kong | Australia | |||||||||||||
| Practice | 64.6 (19.1) | 64 (19.1) | 65 (19.1) | 0.108 | 64.1 (19.6) | 63.4 (20.2) | 64.8 (18.9) | 0.248 | 66.1 (16.5) | 66.2 (16.2) | 66 (16.8) | 0.860 | 63.7 (20.7) | 63.1 (20) | 64.7 (21.7) | 0.220 |
| Knowledge | 68.3 (22.2) | 72 (21.4) | 64 (22.6) | <0.001 | 69.2 (21.9) | 72.9 (20.6) | 65.5 (22.7) | <0.001 | 64.3 (21.7) | 66 (21.7) | 62.6 (21.5) | 0.012 | 70.9 (22.5) | 74.4 (20.9) | 64.8 (23.9) | <0.001 |
| Self-efficacy | 31.1 (8.1) | 30 (8.1) | 32 (7.8) | <0.001 | 32.7 (7.3) | 31.9 (7.4) | 33.5 (7.2) | 0.001 | 32.2 (6.6) | 31.5 (6.8) | 33 (6.2) | <0.001 | 28.5 (9.3) | 27.7 (8.9) | 30 (9.7) | <0.001 |
| Perceived susceptibility towards government | 5.01 (1.55) | 5 (1.52) | 5.02 (1.58) | 0.600 | 4.69 (1.54) | 4.61 (1.5) | 4.78 (1.6) | 0.075 | 5.61 (1.34) | 5.70 (1.2) | 5.51 (1.4) | 0.025 | 4.76 (1.57) | 4.77 (1.56) | 4.73 (1.59) | 0.69 |
| Perceived susceptibility towards individual risk | 3.26 (1.45) | 3.05 (1.33) | 3.52 (1.56) | <0.001 | 3.31 (1.45) | 3.12 (1.3) | 3.51 (1.5) | <0.001 | 3.79 (1.31) | 3.71 (1.2) | 3.88 (1.4) | 0.039 | 2.74 (1.40) | 2.53 (1.20) | 3.10 (1.63) | <0.001 |
| Perceived response efficacy towards public health system | 5.14 (1.17) | 5.12 (1.18) | 5.17 (1.16) | 0.230 | 5.40 (0.97) | 5.38 (1.0) | 5.43 (1.0) | 0.45 | 4.53 (1.22) | 4.31 (1.2) | 4.75 (1.2) | <0.001 | 5.45 (1.07) | 5.50 (1.03) | 5.37 (1.14) | 0.042 |
| Perceived response efficacy towards social distancing | 5.42 (0.97) | 5.41 (0.98) | 5.44 (0.96) | 0.360 | 5.37 (0.94) | 5.31 (1.0) | 5.44 (0.9) | 0.034 | 5.39 (0.90) | 5.34 (0.9) | 5.44 (0.9) | 0.059 | 5.50 (1.05) | 5.53 (1.02) | 5.45 (1.11) | 0.2 |
| Perceived response efficacy towards mask wearing | 5.86 (1.25) | 5.84 (1.28) | 5.89 (1.21) | 0.300 | 6.08 (1.00) | 6.11 (1.0) | 6.05 (1.0) | 0.34 | 6.06 (1.10) | 6.09 (1.1) | 6.03 (1.1) | 0.41 | 5.49 (1.47) | 5.48 (1.46) | 5.52 (1.49) | 0.71 |
| Perceived response efficacy towards non-pharmaceutical intervention | 6.04 (0.84) | 6.07 (0.85) | 6 (0.82) | 0.021 | 6.09 (0.79) | 6.11 (0.8) | 6.07 (0.8) | 0.39 | 5.87 (0.82) | 5.87 (0.8) | 5.87 (0.8) | 0.98 | 6.14 (0.87) | 6.18 (0.86) | 6.08 (0.89) | 0.047 |
| Perceived barrier towards individual | 3.94 (1.68) | 4.67 (1.46) | 3.03 (1.49) | <0.001 | 3.90 (1.66) | 4.73 (1.4) | 3.06 (1.4) | <0.001 | 3.51 (1.58) | 3.98 (1.6) | 3.02 (1.5) | <0.001 | 4.35 (1.70) | 5.11 (1.23) | 3.01 (1.59) | <0.001 |
| Perceived barrier towards government | 3.62 (1.76) | 4.09 (1.73) | 3.03 (1.62) | <0.001 | 3.65 (1.75) | 4.27 (1.7) | 3.02 (1.6) | <0.001 | 3.63 (1.77) | 4.03 (1.8) | 3.21 (1.7) | <0.001 | 3.58 (1.77) | 4.00 (1.75) | 2.82 (1.55) | <0.001 |
3.2. Significant factors correlated with high vaccine intent
Following univariate regression, variables used as standard factors for adjustment were selected based on the AIC method (Table 2 ) for all four multivariate models (overall, Australia, Hong Kong and Singapore). Of the 11 factors correlated with high vaccine intent in the overall model, only ethnicity, marital status, diagnosis with COVID-19, smoking status, gastrointestinal co-morbidity, dengue vaccination and knowledge score were statistically significant.
Table 2.
Factors used as standard factors for adjustment based on the AIC method.
| Variables |
Total cohort |
Singapore |
Hong Kong |
Australia |
||||
|---|---|---|---|---|---|---|---|---|
| p-value |
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
OR (95% CI) |
|
| Ethnicity | 0.000 | 0.53 (0.44,0.63) | – | – | <0.001 | 0.48 (0.33, 0.70) |
||
| Age | 0.077 | 0.99 (0.98,1.00) | – | – | – | |||
| Occupation status | 0.054 | 1.21 (0.99,1.47) | – | – | – | |||
| Health care professionals | – | – | – | 0.088 | 1.51 (0.94, 2.44) |
|||
| Annual average salary (>USD 100,000) | – | – | 0.001 | 2.07 (1.35, 3.20) |
– | |||
| USD 50,001 – USD 100,000 | – | – | 0.001 | 1.68 (1.22, 2.32) |
– | |||
| Marital status (Married) | 0.000 | 1.45 (1.22,1.74) | – | 0.004 | 1.57 (1.16, 2.13) |
– | ||
| Diagnosed self with COVID-19 | 0.042 | 1.33 (1.01,1.76) | – | – | – | |||
| Smoking status (current smoker) | 0.012 | 1.29 (1.06,1.57) | 0.031 | 1.47 (1.04, 2.08) |
– | 0.006 | 1.64 (1.15, 2.34) |
|
| Co-morbidity - Diabetes | – | – | 0.011 | 2.36 (1.24, 4.70) |
– | |||
| Co-morbidity - Gastrointestinal disease | 0.004 | 1.69 (1.18,2.42) | – | 0.001 | 2.37 (1.42, 4.07) |
– | ||
| Persons over 65 years old living in your HH | – | 0.005 | 1.48 (1.13, 1.94) |
– | – | |||
| Children under the age of 5 in HH | – | – | – | 0.022 | 1.53 (1.06, 2.20) |
|||
| Vaccination (measles, dengue, flu) - none | – | 0.050 | 0.76 (0.57, 1.00) |
– | – | |||
| Vaccination - Measles | 0.050 | 1.34 (1.00,1.79) | – | – | 0.053 | 1.62 (0.99, 2.65) |
||
| Vaccination - Dengue | 0.001 | 2.22 (1.38,3.67) | – | – | <0.001 | 5.17 (2.16, 14.42) |
||
| Practice score | 0.095 | 1.00 (0.99,1.01) | 0.049 | 1.01 (1.00, 1.01) |
– | 0.054 | 1.01 (1.00, 1.01) |
|
| Knowledge score | <0.001 | 0.99 (0.98,0.99) | 0.000 | 0.99 (0.98, 0.99) |
0.031 | 0.99 (0.99, 1.00) |
<0.001 | 0.99 (0.98, 0.99) |
Of the significantly associated factors, only knowledge score was negatively associated with vaccine intent. Although age was correlated in the overall model, it showed no significant association with vaccine intent (p-value 0.077). In Australia, Caucasians are less likely to have high vaccine intent compared to Asian (OR 0.48; 95 %CI: 0.33, 0.70). Health care professionals in Australia showed a positive correlation with vaccine intent but was not statistically significant (p-value 0.88). Current smokers were significantly more likely to have high vaccine intent in total cohort (OR 1.29; 95 %CI: 1.06, 1.57). Similarly, this was observed in Australia (OR 1.64; 95 %CI: 1.15, 2.34) and in Singapore (OR 1.47; 95 %CI: 1.04, 2.08). Respondents in Singapore with elderly members aged > 65 years residing in the same household (HH) were significantly more likely to have high vaccine intent (OR 1.48; 95 %CI: 1.13, 1.94). On the contrary, respondents in Australia with children aged < 5 were significantly more likely to have high vaccine intent (OR 1.53; 95 %CI: 1.06, 2.20). COVID-19 knowledge score had significant negative association with vaccine intent in all four multivariate models while practice score had a positive association only in Singapore (Table 2).
3.3. Independent risk factors related to practises associated with high vaccine intent
Australians who wore a surgical mask (AdjOR 1.84; 95 %CI: 1.32, 2.56) and worked from home when not sick were positively associated with high vaccine intent (AdjOR 1.49; 95 %CI: 1.02, 2.19). Singaporeans who avoided public transport (AdjOR 1.65; 95 %CI: 1.23, 2.22) were positively associated with high vaccine intent while Hong Kong residents that avoided overseas trips to countries with COVID-19 cases were negatively associated (AdjOR 0.52; 95 %CI: 0.28, 0.94). Respondents who take micronutrient supplements frequently was positively associated with high vaccine intent across all cohorts, while respondents who clean and disinfect their house more often than before pandemic, and who have balanced and healthy diet were more likely to have high vaccine intent in total cohort (AdjOR 1.41; 95 %CI: 1.16, 1.72; AdjOR 1.32; 95 %CI: 1.10, 1.59), in Australia (AdjOR 1.69; 95 %CI: 1.18, 2.42; AdjOR 1.43; 95 %CI: 1.12, 2.17) and in Singapore (AdjOR 1.53; 95 %CI: 1.08, 2.16; AdjOR 1.56; 95 %CI: 1.12, 2.17), respectively. Respondents who sought medical help for COVID-19 related symptoms like loss of smell/taste was negatively associated with high vaccine intent across all cohorts (Table 3 ).
Table 3.
Independent Risk factors for high acceptance towards COVID-19 vaccine associated with Practices.
| Practices#(Total) |
Total cohort |
Singapore |
Hong Kong |
Australia |
||||
|---|---|---|---|---|---|---|---|---|
| p-value | AdjOR (95% CI) | p-value | AdjOR (95% CI) | p-value | AdjOR (95% CI) | p-value | ||
| Wore a surgical mask when I was not sick | 0.053 | 1.20 (0.99, 1.45) | 0.109 | 1.32 (0.94.1.85) | – | 0.000 | 1.84 (1.32, 2.56) |
|
| Wore a surgical mask when I was sick | 0.421 | 1.13 (0.84, 1.51) | – | – | 0.031 | 1.77 (1.05, 2.98) |
||
| Cleaned & disinfected my house more often than before | 0.001 | 1.41 (1.16,1.72) | 0.015 | 1.53 (1.08,2.16) | – | 0.005 | 1.69 (1.18, 2.42) |
|
| Avoided public transport | 0.083 | 1.17 (0.98,1.39) | 0.001 | 1.65 (1.23,2.22) | – | – | ||
| Worked from home even though I was fine | 0.138 | 1.15 (0.96,1.38) | – | – | 0.041 | 1.49 (1.02, 2.19) |
||
| Worked from home when I had a cold or cough | <0.001 | 1.46 (1.18,1.79) | – | – | 0.099 | 1.40 (0.94, 2.08) |
||
| Kept my children out of school even though school was still opened | 0.013 | 1.33 (1.06,1.66) | 0.014 | 1.62 (1.10,2.37) | – | 0.501 | 1.17 (0.75, 1.82) |
|
| Avoided overseas trips to countries with COVID-19 cases | – | – | 0.031 | 0.52 (0.28, 0.94) |
– | |||
| Had a more balanced and healthy diet | 0.003 | 1.32 (1.09,1.59) | 0.009 | 1.56 (1.12,2.17) | – | 0.035 | 1.43 (1.03, 1.99) |
|
| Took micronutrient supplements more frequently | <0.001 | 1.49 (1.27,1.77) | 0.033 | 1.37 (1.03,1.83) | 0.005 | 1.49 (1.23, 1.98) |
0.001 | 1.76 (1.25, 2.47) |
| Covered my mouth when I coughed or sneezed | 0.001 | 0.56 (0.40,0.79) | – | – | 0.012 | 0.41 (0.20, 0.83) |
||
| Used caution while opening letters or packages | 0.036 | 1.20 (1.01,1.43) | 0.216 | 1.21 (0.89,1.64) | – | 0.072 | 1.37 (0.97, 1.94) |
|
| Symptoms* | ||||||||
| Yes - Fever | 0.001 | 0.69 (0.56,0.86) | – | 0.076 | 0.70 (0.47, 1.04) |
– | ||
| Yes - Fatigue/lethargy | 0.433 | 0.93 (0.78,1.11) | – | – | – | |||
| Yes - Shortness of breath | 0.063 | 0.85 (0.72,1.01) | 0.030 | 0.71 (0.52,0.97) | – | 0.314 | 0.84 (0.60, 1.18) |
|
| Yes - Loss of smell | 0.000 | 0.63.(0.53,0.75) | 0.000 | 0.53 (0.38,0.73) | 0.028 | 0.71 (0.53, 0.96) | 0.000 | 0.49 (0.34, 0.70) |
| Yes - Loss of taste | 0.000 | 0.59 (0.50,0.72) | 0.000 | 0.53 (0.39,0.73) | 0.020 | 0.69 (0.50, 0.94) |
0.000 | 0.43 (0.30, 0.62) |
Practices were carried out by respondents to reduce the risk of contracting or spreading COVID-19 after the first case was detected and before safety measures were enforced or advised in their country.
To ensure you are not infected with COVID-19, for which of these symptoms would you seek medical help? (reference category: No).
3.4. Independent risk factors related to information seeking behaviour associated with high vaccine intent.
Respondents who do not update on COVID-19 frequently were more likely to show high vaccine intent in total cohort, in Australia and Singapore (Table 4 ). Respondents in total cohort, Australia and Singapore who have more trust towards non-health related agencies/people and digital media were significantly more likely to have high vaccine intent (Total: AdjOR 1.29; 95 %CI: 1.11, 1.51, Singapore: OR 1.38; 95 %CI: 1.06, 1.81). Health seeking behaviour was not significantly associated in Australia, however, respondents in Hong Kong who felt that sufficient information on care and treatment were provided, were significantly more likely to have high vaccine intent (AdjOR 1.13; 95% CI: 1.03,1.25). Singaporeans who are interested in general COVID-19 information (AdjOR 0.76; 95 %CI: 0.61,0.96) and perceived that seeking care/treatment (AdjOR 0.74; 95 %CI: 0.61, 0.91) was important, were significantly less likely to show high vaccine intent.
Table 4.
Independent Risk factors for high acceptance towards COVID-19 vaccine associated with Sources and type of information.
| Source of information |
Total cohort |
Singapore |
Hong Kong |
Australia |
||||
|---|---|---|---|---|---|---|---|---|
| p-value | AdjOR (95% CI) |
p-value | AdjOR (95% CI) |
p-value | AdjOR (95% CI) |
p-value | AdjOR (95% CI) |
|
| How often do you check for new updates on COVID-19? (reference: Daily*) | ||||||||
| Weekly | 0.193 | 1.14 (0.94,1.39) | 0.216 | 1.24 (0.88, 1.73) |
– | 0.791 | 0.96 (0.68, 1.34) |
|
| Monthly | 0.000 | 2.67 (1.63,4.35) | 0.005 | 3.52 (1.45, 8.57) |
– | 0.010 | 3.06 (1.30, 7.19) |
|
| Rarely/never | 0.094 | 1.31 (0.96,1.79) | 0.009 | 2.26 (1.23, 4.14) |
– | 0.162 | 0.69 (0.42, 1.16) |
|
| From which of the following sources and types of media do you frequently get updates on COVID-19? No* | ||||||||
| Non-health related agencies or people | 0.001 | 1.29 (1.11,1.51) | 0.016 | 1.38 (1.06, 1.81) |
0.113 | 1.26 (0.95, 1.67) |
0.197 | 1.21 (0.91, 1.63) |
| How much do you trust the following sources and types of media on their reporting about COVID-19? | ||||||||
| Medical practitioners or health related government agencies | – | – | 0.063 | 1.34 (0.98,1.81) | – | |||
| Non-health related agencies or people | <0.001 | 1.49 (1.24,1.82) | 0.027 | 1.48 (1.04,2.09) | 0.131 | 1.33 (0.92,1.93) | 0.007 | 1.65 (1.15,2.38) |
| Traditional | 0.330 | 1.07 (0.93,1.24) | – | – | – | |||
| digital | <0.001 | 1.32 (1.12,1.54) | 0.006 | 1.48 (1.12,1.94) | – | 0.004 | 1.59 (1.16,2.19) | |
| What information about COVID-19 has been important for you to be updated on during this pandemic? Not important* | ||||||||
| General disease specific information related to self | 0.002 | 0.83 (0.75,0.93) | 0.022 | 0.76 (0.61,0.96) | – | – | ||
| Seeking care/treatment | – | 0.003 | 0.74 (0.61,0.91) | – | – | |||
| Global COVID-19 information | – | – | – | – | ||||
| For each type of information about COIVD-19, was sufficient information provided by your government? Not sufficient* | ||||||||
| General disease specific information related to self | – | – | – | – | ||||
| Seeking care/treatment | – | – | 0.013 | 1.13 (1.03,1.25) | – | |||
| Global COVID-19 information | – | – | – | – | ||||
3.5. Independent risk factors related to perceptions and self-efficacy associated with high vaccine intent
Australians and Singaporeans with high self-efficacy were 1.02 times more likely to have high vaccine intent while respondents with high self-efficacy in Hong Kong were 1.04 times more likely to have high vaccine intent (supplementary Table 14).
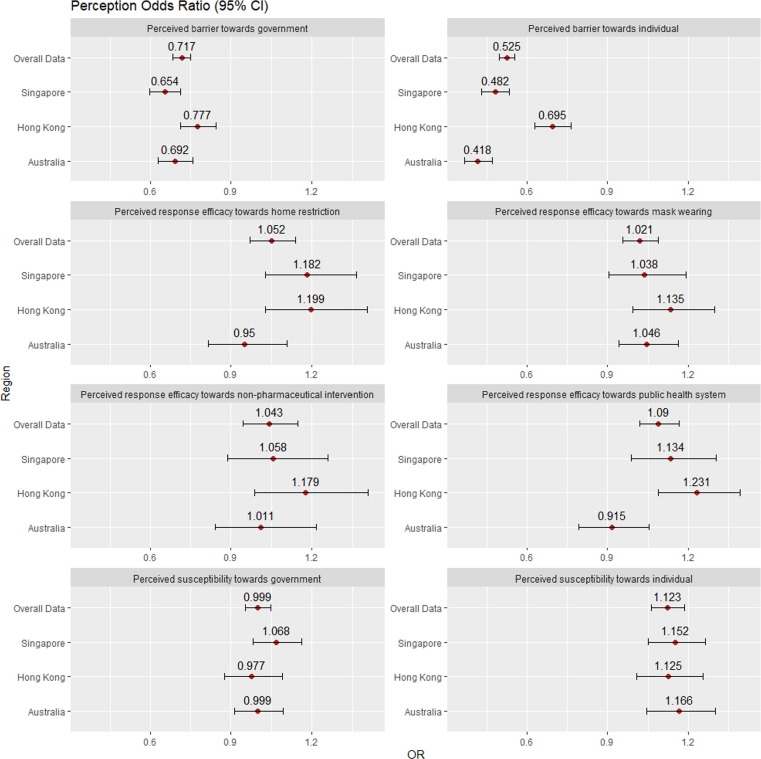
Of the eight perception constructs identified by ECA and CFA, three were significantly associated with high vaccine intent across all countries. Perceived susceptibility towards individual risk that addressed how likely respondents would be infected with COVID-19 in the next few months due to an outbreak at home or work, was positively associated with high vaccine intent (Total: AdjOR 1.12; 95 %CI: 1.06, 1.19, Australia: AdjOR 1.17; 95 %CI: 1.05, 1.30; Hong Kong: AdjOR 1.13; 95 %CI: 1.01, 1.26; Singapore: AdjOR 1.15; 95 %CI: 1.05, 1.26;). Perceived barrier towards self which addressed how difficult it was to perform or adhere to measures directed at individual level like avoiding crowded places, public transport, social distancing, masking, was negatively associated with high vaccine intent (Total: AdjOR 0.53; 95 %CI: 0.49, 0.56; Australia: AdjOR 0.42; 95 %CI: 0.37, 0.47; Hong Kong: AdjOR 0.69; 95 %CI: 0.63, 0.76; Singapore: AdjOR 0.48; 95 %CI: 0.43, 0.54). Finally, perceived barrier towards government that addressed how difficult it would be for measures like school closures, mass temperature screening, lockdown and large-scale quarantine to be implemented by government was also negatively associated with high vaccine intent (Total: AdjOR 0.72; 95 %CI: 0.68, 0.75; Australia: AdjOR 0.69; 95 %CI: 0.63, 0.76; Hong Kong: AdjOR 0.78; 95 %CI: 0.71, 0.84; Singapore: AdjOR 0.65; 95 %CI: 0.59, 0.71). (Fig. 1 , supplementary Table 14).
Fig. 1.
Perception constructs overall and country specific.
Perceived response efficacy towards social distancing which includes limiting physical contact with friends and family, staying indoors, avoiding public transport and crowded places, working from home, school closures was positively associated with high vaccine intent in Hong Kong (AdjOR 1.99; 95 %CI: 1.03, 1.40) and Singapore (AdjOR 1.18; 95 %CI: 1.03, 1.36), but not in Australia. Whereas perceived response efficacy towards public health system addressing mandatory swab testing and vaccination, agreeing if healthcare system in their country was effective and if vaccine would be safe, was positively associated with high vaccine intent in the total cohort (AdjOR 1.09; 95 %CI: 1.02, 1.17) and Hong Kong (AdjOR 1.23; 95 %CI: 1.09, 1.39). Although remaining three perception constructs: perceived susceptibility towards government, perceived response efficacy towards mask wearing and perceived response efficacy towards non-pharmaceutical interventions, were correlated across all countries, they were not significantly associated with high vaccine intent (supplementary Table 14).
4. Discussion
Our study aims to understand various practices and perceptions are associated with high vaccine intent in three countries which are similar in their approach towards managing the COVID-19 pandemic but are different in their population demographics. At the time of this survey distribution, Pfizer-BioNTech COVID-19 vaccine was approved in all three countries but only Singapore had initiated the vaccination program on 30th December 2020 [16]. Australia and Hong Kong initiated the vaccine program after the study period on 22nd – 23rd February 2020 respectively [5], [6].
4.1. Impact of demographic factors and health history
Gender was not found to be associated with high vaccine intent, which was also reported by an Australian survey by Faasse and Newby [17]. However, a systematic review on COVID-19 vaccine receptivity conducted between 1 January and 20 October 2020 found males to be more receptive to being vaccinated. While majority of the studies included in the systematic review were from USA, other studies have also observed a similar pattern among males possibly due to higher perceived risk of COVID-19 complications [19], [20]. Although our study did not find any association with age and high vaccine intent, a study carried out among nurses found younger age to be associated with stronger vaccine intent [21]. While an Indian study found older age groups > 45 years are more willing to take the COVID-19 vaccine [22], an Australian study found vaccine hesitancy to be associated with younger than 60 years of age [23]. Country based analysis found older people aged > 50 to be favorably disposed to vaccination in Europe, UK and Canada but reverse association was seen in China [18]. Therefore, this suggests that other factors like type of population and location of study may also play an important role in influencing vaccine intent. In addition, the population at risk were observed to be different when affected by the different variants of SARS-CoV-2 at different phases of the pandemic, which can also influence the association between age groups and vaccine intent [24].
Asians was observed to have a significantly higher vaccine intent compared to Caucasians which is concurrent with findings from studies in USA where vaccine acceptance amongst Asians was higher than other races [25], [26]. This suggests that difference in cultural and social background can also influence their vaccine intent. Being married was positively associated with high vaccine intent in Hong Kong while having children under 5 years and elderly members in the household were positively associated with high vaccine intent in Australia and Singapore respectively. This suggests that having vulnerable individuals residing within the same household is likely to influence vaccine intent. In addition, socio-economic status was positively associated with high vaccine intent in Hong Kong, similar to findings from a global survey conducted in 19 countries as well as from recent review published by Cascini et al. study in China [27], [28]. While education and socioeconomic status are known to be positively associated with determinants of positive health outcome [23], [26], [27] it can influence vaccine intent in any direction as explained by MacDonald et al., who concludes that various political and cultural factors can affect vaccine hesitancy and complacency [11]. Unique factors like political interference, political inclination and doubts towards expedited vaccine development have also been shown to have effect on COVID-19 vaccination [12], [18].
Current smokers were positively associated with high vaccine intent in Australia and Singapore but not in Hong Kong where there are extensive tobacco control measures and current smoking prevalence (10.8% smoking in persons aged over 15 in 2019) is one of the lowest across the world [29]. In addition, individuals with comorbidities were positively associated with high vaccine intent in Hong Kong, concurrent with findings from USA [30]. Smoking and comorbidities increase perceived susceptibility towards individual risk thereby potentially increasing their vaccination interest. Individuals who have had dengue vaccination was positively associated with high vaccine intent in Australia and Singapore, which is concurrent with evidence that prior vaccinations can influence vaccination compliance in other diseases such as influenza and dengue [31], [32], [33]. This suggests that investment in education and risk communication to encourage positive attitude towards vaccination against a specific disease is likely to have a positive impact on achieving high vaccine intent against other vaccine-preventable infectious diseases.
4.2. Impact of various practices and COVID-19 knowledge
4.2.1. Impact of lifestyle and health seeking behaviour
Respondents from all three countries that started taking micronutrient supplements more frequently were significantly more likely to show high vaccine intent. Those that cleaned and disinfected their house more often than before and those that had a healthy and balanced diet were also significantly more likely to show high vaccine intent in Australia and Singapore. This suggests that people who are diet and hygiene conscious will be more likely to have higher intention to get vaccinated. Respondents that sought help for symptoms like loss of taste and smell and shortness of breath were less likely to show high vaccine intent. These findings are possibly due to the behavioural patterns in individuals. It has been seen that individuals experiencing COVID-19 symptoms may refrain from visiting the doctors in fear of being exposed to the virus [34]. More studies are required to help understand these barriers and its association with vaccine intent.
4.2.2. Impact of masking and social distancing practises on vaccine intent
Masking irrespective of health status was seen to be significantly associated with high vaccine intent in Australia suggesting that people who were willing to wear masks would also be more willing to vaccinate however this was not observed in Hong Kong and Singapore. This can be attributed to masking being more prominent and a more habitual practice even before the pandemic in some Asian countries [35]. Since the SARS outbreak, many Asian countries would wear mask to protect against seasonal flu and common cold, as well as a mean of prevention from inhaling excessive amount of air pollutants [35], [36]. Singaporeans avoiding public transport and keeping their children out of school, and Australians working from home when not feeling well were all significantly associated with high vaccine intent. Moore et al., recently concluded that intrinsic factors like returning to normalcy was one of the key factors to drive vaccination behaviour [37]. While there haven’t been many studies looking at daily practices as risk factors for high vaccine intent, this study assessed and identified behaviours or practices that were seen amongst those with high intention to vaccinate against SARS-CoV-2.
4.2.3. Impact of knowledge on vaccine intent
Higher COVID-19 knowledge score was negatively associated with high vaccine intent indicating that increased knowledge on COVID-19 did not necessarily increase vaccine intent. This was validated by our findings on health seeking behaviour wherein respondents that thought specific COVID-19 information was important or sufficient were also associated with low vaccine intent. Similar findings have been concluded by Yan et al. [38], that found knowledge as a negative predictor for vaccine intention and speculated that there may be a more complicated relationship between knowledge and vaccine intention. Contrasting findings from Hong Kong have shown that inadequate knowledge is associated with vaccine hesitancy [39]. Furthermore, such knowledge-behaviour gap has been observed in other vaccines such as human papillomavirus [40]. Thus, it is not only important to provide COVID-19 information but to also introduce health promotion and disease prevention messages to increase vaccine intent.
4.3. Impact of information seeking behaviour
As online media is getting more popular over traditional print media, increasing number of individuals are seeking health information online [41]. This has increased tremendously during COVID-19 pandemic with digital media being used as a means of not only providing health information but also for crisis communication. Similar to findings by Liu et al. that found a positive correlation between seeking COVID-19-related information on digital media and practising preventive behaviours [42], our study found seeking information from digital sources and non-health related governmental agencies and family, friends and influencers to be positively associated with high vaccine intent. A USA based study suggested that vaccination uptake can be increased if one identifies with the political speaker who is endorsing it and they also found that a factually accurate message by an expert may not be effectual to increase vaccination uptake [43]. Bonnevie et al. found influencers to significantly increase beliefs on flu vaccine and they have been engaged to not only market products but also to promote vaccination [44]. While countries like Singapore have adopted social media and mobile messaging platforms to convey COVID-19 information to the public [45], the role of influencers was positively associated with high vaccine intent in all three countries. Influencers can be meaningfully engaged to motivate people to get vaccinated and follow other preventive measures.
4.4. Impact of perception constructs
Amongst eight constructs that were derived by cluster and factor analysis, three were significantly associated with vaccine intent across all countries; perceived susceptibility towards individual risk, perceived barrier towards measures directed towards self and government. Our findings with perceived susceptibility towards individual risk are in concordance with findings from survey related to HBM conducted in Israel that found higher perceived severity was associated with increased intent to get vaccinated [46]. Similarly, Macdonald et al reported that when perceived risks of vaccine-preventable diseases are low and vaccination is not considered a required preventive action, vaccination complacency exists [11]. Moreover, numerous studies concerning COVID-19 have shown similar pattern with perceived susceptibility, indicating that increased awareness of risk of infection can drive people towards vaccination as a form of prevention [19], [47], [48], [49]. While this has also been reported by Yan et al’s study in which respondents in Hong Kong displayed strong intention to vaccinate if they had a greater level of susceptibility [38], it contradicts the findings from another population-based study by Wong et al., wherein perceived susceptibility was not associated with acceptance of COVID-19 vaccine [13]. These findings could be linked to the different study time periods. While Wong et al.’s survey was conducted early on in the pandemic, between July-August 2020, Yan’s and our study periods were in early 2021. Change in people’s perception towards susceptibility changes over time and can also change with varying factors such as the type of variant, disease severity, availability of treatment and vaccines and extent of preventive measures. While perceived susceptibility towards individual risk may reduce over time with relaxing of rules and decreased severity of the variant, it can increase again with increased severity.
Perceived barrier has shown to have an inverse relation with vaccine willingness as also seen in our study for vaccine intent [13], [49]. However, perceived barriers have been construed differently across studies based on the vaccine type [50]. This study has determined two unique perceived barrier constructs associated with vaccine intent: first, perceived barriers towards preventive measures directed at an individual level, which include avoiding public transport, social distancing, travelling, self-isolation, masking and daily temperature monitoring; second, perceived barrier towards government measures which include quarantine, mass temperature screening, school closures and city lockdowns.
While Australia did not see any correlation with perceived response efficacy constructs, Singapore showed a positive correlation with perceived response efficacy towards social distancing. Hong Kong showed a positive correlation with perceived response efficacy towards social distancing and public health system construed by respondents’ belief in country’s healthcare system and vaccine safety. Studies have shown a negative correlation with vaccine harm which was validated by our finding on a positive correlation with vaccine safety [50], [51]. This suggests that residents who trust their health system efficacy would have a predilection for vaccination.
While our study saw a positive correlation with vaccine intent and respondents’ willingness to maintain social distancing and self-isolation, survey conducted by Wang et al., in Hong Kong observed a decrease in willingness to accept COVID-19 vaccine with growing compliance of personal protection behaviours [51]. Attitude towards COVID-19 vaccination has changed over the course of the pandemic with each wave showing different trends [23], [52]. Results from an online survey have shown a drop in intent to get vaccinated in most countries including Australia which saw a decrease from 88% to 79% in one month [52]. Understanding perceptions across different waves of the pandemic will thus help in understanding factors that can help to increase vaccine intent.
4.5. Impact of Self-efficacy
Individuals is likely to have higher degree of self-efficacy when exposed to higher degree of threat and in this case the exposure to SARS-CoV-2 virus [53]. Similar to our findings, Hao et al. identified self-efficacy to be positively associated with vaccination behaviour in China [54]. This study concludes that self-efficacy plays a key role in mediating between the effect of perceived susceptibility and perceived barrier on vaccine intent.
While vaccine development usually takes over 10–15 years to ensure safety and efficacy [55], [56], U.S. FDA gave its full approval to the first COVID-19 vaccine on 23rd August 2021, less than two years after SARS-CoV-2 was first identified. Despite proven safety and efficacy of COVID-19 vaccines, low vaccine intent or hesitancy can be attributed to side effects and hasty vaccine development [18], [57]. Perception towards long-term side-effects and the duration of vaccine effectiveness need to be studied to understand its impact on vaccine intent. Interventions to improve self-efficacy or studies trying to alter perceptions take time and have shown limited success [58]. Although the three countries surveyed are different demographically, culturally and politically, high vaccine intent may be achieved by some common approaches based on our study findings. Firstly, by increasing people’s perception towards COVID-19 susceptibility, especially among the more vulnerable subpopulation, by means of social media and influencers. Secondly, by implementing public health measures that are sustainable and manageable by the respective government and healthcare system to achieve trust and confidence among the population. Finally, by investing in risk communication as part of pandemic preparedness to reduce the perceived barriers and increase the self-efficacy of vaccination.
5. Strengths and limitations
One key strength of this study lies in validity and reliability of perception constructs that has been derived with a robust statistical method. A limiting factor of this study is the vaccine intent group classification, which was based on their willingness to voluntarily get vaccinated, but this may not necessarily imply they will ultimately get vaccinated. Other limitations are related to survey-based studies namely; 1. potential over-simplification of findings due to a lack of a longitudinal study design, 2. potential social desirability bias resulting from closed responses, 3. limited generalisability of findings due to potential skewed in respondents’ demographic, 4. potential recall bias due to questions related to the start of pandemic and 5. due to the nature of a cross-sectional study, the investigation of a causal relationship between the risk factors and vaccine intent is limited.
6. Conclusion
Understanding factors that drive high vaccine intent should guide policy and risk communication strategies to achieve more positive vaccine uptake behaviour. Our study found that perceived susceptibility and perceived response efficacy were positively associated with high vaccine intent for COVID-19. On the contrary, perceived barriers were negatively associated. While intent to get vaccinated is high among those that have an increased perceived susceptibility towards compliance with preventive measures, this may also decrease over time as perceived barriers increases at different phase of the COVID-19 pandemic.
7. Availability of data and materials
All data relevant to the study are included in the article or uploaded as supplementary information.
Author contributions
Concept and design: JP, SS, JYT, LKPS, SWCC.
Acquisition, analysis or interpretation of data: JP, HG, SS, CEYP, JYT, LKPS, SWCC.
Drafting of the manuscript: SS, HG, CEYP.
Critical revision of the manuscript for important intellectual content: JP, HG, CEYP, SS, JYT, LKPS, SWCC.
Statistical analysis: HG, SS.
Administrative, technical or material support: JP, SS, JYT, LKPS, SWCC.
Supervision: JP.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
We would like to acknowledge Ms. Katrina Dexter for working with us to translate and distribute the survey online in all the countries. We would also like to acknowledge Ms. Jiayun Koh and Mr. Nicholas Lau for their contribution in survey design and drafting of the study proposal.
Source of funding
1) NUS COVID-19 RESEARCH SEED FUNDING (NUSCOVID19RG-43) - JP,
2) Lloyd’s Register Foundation Institute for the Public Understanding of Risk (IPUR_FY2020_RES_02_PANG), National University of Singapore - JP The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2022.03.062.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.U.S. Food and Drug Adminstration. Comirnaty and Pfizer-BioNTech COVID-19 Vaccine 2021 [cited 2021 April 27]. Available from: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/comirnaty-and-pfizer-biontech-covid-19-vaccine#:∼:text=On%20December%2011%2C%202020%2C%20the,years%20of%20age%20and%20older.
- 2.Health Science Authority. HSA Grants Interim Authorisation for First COVID-19 Vaccine in Singapore 2020 [cited 2022 February 22]. Available from: https://www.hsa.gov.sg/announcements/press-release/interimauth-firstcovid19vaccine.
- 3.Australian Government Department of Health Therapeutic Goods Adminstration. COVID-19 vaccines undergoing evaluation 2022 [cited 2022 February 22]. Available from: https://www.tga.gov.au/covid-19-vaccines-undergoing-evaluation.
- 4.The Government of the Hong Kong Special Adminstrative Region. About the Vaccines 2022 [cited 2022 February 22]. Available from: https://www.covidvaccine.gov.hk/en/vaccine.
- 5.The Government of the Hong Kong Special Adminstrative Region. Hong Kong Vaccination Dashboard 2022 [cited 2022 February 17]. Available from: https://www.covidvaccine.gov.hk/en/dashboard.
- 6.Australian Government Department of Health. Vaccination numbers and statistics 2022 [cited 2022 February 17]. Available from: https://www.health.gov.au/initiatives-and-programs/covid-19-vaccines/numbers-statistics.
- 7.Ministry of Health Singapore. 2022 [cited 2022 February 17]. Available from: https://www.moh.gov.sg/covid-19/vaccination.
- 8.Centers for Disease Control and Prevention. Benefits of Getting a COVID-19 Vaccine 2022 [cited 2022 March 1]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/vaccine-benefits.html.
- 9.IPSOS. COVID-19 vaccination intent is decreasing globally 2021 [cited 2021 September 3]. Available from: https://www.ipsos.com/en/global-attitudes-covid-19-vaccine-october-2020.
- 10.Momplaisir F.M., Kuter B.J., Ghadimi F., Browne S., Nkwihoreze H., Feemster K.A., et al. Racial/Ethnic Differences in COVID-19 Vaccine Hesitancy Among Health Care Workers in 2 Large Academic Hospitals. JAMA Netw Open. 2021;4(8):e2121931. doi: 10.1001/jamanetworkopen.2021.21931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.MacDonald N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 12.Wang J., Jing R., Lai X., Zhang H., Lyu Y., Knoll M.D., et al. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines. 2020;8(3):482. doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong M.C.S., Wong E.L.Y., Huang J., Cheung A.W.L., Law K., Chong M.K.C., et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine. 2021;39(7):1148–1156. doi: 10.1016/j.vaccine.2020.12.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dynata. Dynata [cited 2022 March 1]. Available from: https://www.dynata.com/.
- 15.Costa M.F. Health belief model for coronavirus infection risk determinants. Rev Saude Publica. 2020;54:47. doi: 10.11606/s1518-8787.2020054002494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gov.sg. What you should know about the COVID-19 vaccine 2020 [cited 2022 March 1]. Available from: https://www.gov.sg/article/what-you-should-know-about-the-covid-19-vaccine.
- 17.Faasse K., Newby J. Public Perceptions of COVID-19 in Australia: Perceived Risk, Knowledge, Health-Protective Behaviors, and Vaccine Intentions. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.551004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin C., Tu P., Beitsch L.M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines (Basel) 2020;9(1) doi: 10.3390/vaccines9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dror A.A., Eisenbach N., Taiber S., Morozov N.G., Mizrachi M., Zigron A., et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Galbadage T., Peterson B.M., Awada J., Buck A.S., Ramirez D.A., Wilson J., et al. Systematic Review and Meta-Analysis of Sex-Specific COVID-19 Clinical Outcomes. Front Med (Lausanne) 2020;7:348. doi: 10.3389/fmed.2020.00348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kwok K.O., Li K.-K., Wei W.I., Tang A., Wong S.Y.S., Lee S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int J Nurs Stud. 2021;114 doi: 10.1016/j.ijnurstu.2020.103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumari A., Ranjan P., Chopra S., Kaur D., Kaur T., Upadhyay A.D., et al. Knowledge, barriers and facilitators regarding COVID-19 vaccine and vaccination programme among the general population: A cross-sectional survey from one thousand two hundred and forty-nine participants. Diabetes Metabolic Syndrome: Clin Res Rev. 2021;15(3):987–992. doi: 10.1016/j.dsx.2021.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rhodes A., Hoq M., Measey M.-A., Danchin M. Intention to vaccinate against COVID-19 in Australia. Lancet Infect Dis. 2021;21(5) doi: 10.1016/S1473-3099(20)30724-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ries J. What to Know About COVID-19, Variants, and Children Healthline2021 [cited 2021 May 24]. Available from: https://www.healthline.com/health-news/what-to-know-about-covid-19-variants-and-children.
- 25.Szilagyi P.G., Thomas K., Shah M.D., Vizueta N., Cui Y., Vangala S., et al. National Trends in the US Public’s Likelihood of Getting a COVID-19 Vaccine—April 1 to December 8, 2020. JAMA. 2021;325(4):396–398. doi: 10.1001/jama.2020.26419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26 doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cascini F., Pantovic A., Al-Ajlouni Y., Failla G., Ricciardi W. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: A systematic review. EClinicalMedicine. 2021;40 doi: 10.1016/j.eclinm.2021.101113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Census and Statistics Department Hong Kong Special Administrative Region. Thematic household Survey Report No. 70—Pattern of Smoking 2020 [cited 2021 October 26]. Available from: https://www.statistics.gov.hk/pub/B11302702020XXXXB0100.pdf.
- 30.Dalal R.S., McClure E., Marcus J., Winter R.W., Hamilton M.J., Allegretti J.R. COVID-19 Vaccination Intent and Perceptions Among Patients With Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2021;19(8):1730. doi: 10.1016/j.cgh.2021.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alqudeimat Y., Alenezi D., AlHajri B., Alfouzan H., Almokhaizeem Z., Altamimi S., et al. Acceptance of a COVID-19 Vaccine and Its Related Determinants among the General Adult Population in Kuwait. Medical Principles Practice. 2021;30(3):262–271. doi: 10.1159/000514636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harapan H., Fajar J.K., Sasmono R.T., Kuch U. Dengue vaccine acceptance and willingness to pay. Hum Vaccin Immunother. 2017;13(4):786–790. doi: 10.1080/21645515.2016.1259045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heo J.Y., Chang S.H., Go M.J., Kim Y.M., Gu S.H., Chun B.C. Risk Perception, Preventive Behaviors, and Vaccination Coverage in the Korean Population during the 2009–2010 Pandemic Influenza A (H1N1): Comparison between High-Risk Group and Non–High-Risk Group. PLoS ONE. 2013;8(5) doi: 10.1371/journal.pone.0064230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tan H.M.J., Tan M.S., Chang Z.Y., Tan K.T., Ee G.L.A., Ng C.C.D., et al. The impact of COVID-19 pandemic on the health-seeking behaviour of an Asian population with acute respiratory infections in a densely populated community. BMC Public Health. 2021;21(1):1196. doi: 10.1186/s12889-021-11200-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martinelli L., Kopilaš V., Vidmar M., Heavin C., Machado H., Todorović Z., et al. Face Masks During the COVID-19 Pandemic: A Simple Protection Tool With Many Meanings. Frontiers. Public Health. 2021;8 doi: 10.3389/fpubh.2020.606635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Health Hub. How to Protect Yourself Against the Haze 2021 [cited 2022 March 3]. Available from: https://www.healthhub.sg/live-healthy/1079/how-to-protect-yourself-against-haze.
- 37.Moore R., Purvis R.S., Hallgren E., Willis D.E., Hall S., Reece S., et al. Motivations to Vaccinate Among Hesitant Adopters of the COVID-19 Vaccine. J Community Health. 2021 doi: 10.1007/s10900-021-01037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yan E., Lai D.W.L., Lee V.W.P. Predictors of Intention to Vaccinate against COVID-19 in the General Public in Hong Kong: Findings from a Population-Based, Cross-Sectional Survey. Vaccines. 2021;9(7):696. doi: 10.3390/vaccines9070696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Luk T.T., Zhao S., Wu Y., Wong J.Y.-H., Wang M.P., Lam T.H. Prevalence and determinants of SARS-CoV-2 vaccine hesitancy in Hong Kong: A population-based survey. Vaccine. 2021;39(27):3602–3607. doi: 10.1016/j.vaccine.2021.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wegwarth O., Kurzenhäuser-Carstens S., Gigerenzer G. Overcoming the knowledge–behavior gap: The effect of evidence-based HPV vaccination leaflets on understanding, intention, and actual vaccination decision. Vaccine. 2014;32(12):1388–1393. doi: 10.1016/j.vaccine.2013.12.038. [DOI] [PubMed] [Google Scholar]
- 41.Yan Y.Y. Online Health Information Seeking Behavior in Hong Kong: An Exploratory Study. J Med Syst. 2010;34(2):147–153. doi: 10.1007/s10916-008-9226-9. [DOI] [PubMed] [Google Scholar]
- 42.Liu P.L. COVID-19 Information Seeking on Digital Media and Preventive Behaviors: The Mediation Role of Worry. Cyberpsychol Behav Soc Netw. 2020;23(10):677–682. doi: 10.1089/cyber.2020.0250. [DOI] [PubMed] [Google Scholar]
- 43.Robertson C.T., Bentele K., Meyerson B., Wood A.S.A., Salwa J. Effects of political versus expert messaging on vaccination intentions of Trump voters. PLoS ONE. 2021;16(9) doi: 10.1371/journal.pone.0257988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bonnevie E., Rosenberg S.D., Kummeth C., Goldbarg J., Wartella E., Smyser J. Using social media influencers to increase knowledge and positive attitudes toward the flu vaccine. PLoS ONE. 2020;15(10) doi: 10.1371/journal.pone.0240828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wong J.E.L., Leo Y.S., Tan C.C. COVID-19 in Singapore—Current Experience: Critical Global Issues That Require Attention and Action. JAMA. 2020;323(13):1243–1244. doi: 10.1001/jama.2020.2467. [DOI] [PubMed] [Google Scholar]
- 46.Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. 2021;21(1):804. doi: 10.1186/s12889-021-10816-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 2020;38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fisher K.A., Bloomstone S.J., Walder J., Crawford S., Fouayzi H., Mazor K.M. Attitudes Toward a Potential SARS-CoV-2 Vaccine : A Survey of U.S. Adults Ann Intern Med. 2020;173(12):964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Guidry J.P.D., Laestadius L.I., Vraga E.K., Miller C.A., Perrin P.B., Burton C.W., et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–142. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reiter P.L., Brewer N.T., Gottlieb S.L., McRee A.-L., Smith J.S. Parents' health beliefs and HPV vaccination of their adolescent daughters. Soc Sci Med. 2009;69(3):475–480. doi: 10.1016/j.socscimed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 51.Wang K., Wong E.L., Ho K.F., Cheung A.W., Yau P.S., Dong D., et al. Change of Willingness to Accept COVID-19 Vaccine and Reasons of Vaccine Hesitancy of Working People at Different Waves of Local Epidemic in Hong Kong, China: Repeated Cross-Sectional Surveys. Vaccines (Basel) 2021;9(1) doi: 10.3390/vaccines9010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.IPSOS. COVID-19 vaccination intent is decreasing globally 2020 [cited 2021 May 21]. Available from: https://www.ipsos.com/en/global-attitudes-covid-19-vaccine-october-2020.
- 53.Jones C.L., Jensen J.D., Scherr C.L., Brown N.R., Christy K., Weaver J. The Health Belief Model as an Explanatory Framework in Communication Research: Exploring Parallel, Serial, and Moderated Mediation. Health Commun. 2015;30(6):566–576. doi: 10.1080/10410236.2013.873363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen H., Li X., Gao J., Liu X., Mao Y., Wang R., et al. Health Belief Model Perspective on the Control of COVID-19 Vaccine Hesitancy and the Promotion of Vaccination in China: Web-Based Cross-sectional Study. J Med Internet Res. 2021;23(9) doi: 10.2196/29329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.The History of Vaccines. Vaccine Development, Testing, and Regulation 2018 [cited 2021 October 4]. Available from: https://www.historyofvaccines.org/content/articles/vaccine-development-testing-and-regulation.
- 56.Cleve M. What the lightning-fast quest for Covid vaccines means for other diseases. Nature. 2021;589 doi: 10.1038/d41586-020-03626-1. [DOI] [PubMed] [Google Scholar]
- 57.Griva K., Tan K.Y.K., Chan F.H.F., Periakaruppan R., Ong B.W.L., Soh A.S.E., et al. Evaluating Rates and Determinants of COVID-19 Vaccine Hesitancy for Adults and Children in the Singapore Population: Strengthening Our Community's Resilience against Threats from Emerging Infections (SOCRATEs) Cohort. Vaccines (Basel) 2021;9(12) doi: 10.3390/vaccines9121415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brewer N.T. What Works to Increase Vaccination Uptake. Acad Pediatr. 2021;21(4s):S9–s16. doi: 10.1016/j.acap.2021.01.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.