Abstract
Diabetes and prediabetes are overwhelming public health concerns in Bangladesh. However, there is a paucity of the literature examining and measuring socioeconomic inequalities in the prevalence of diabetes in Bangladesh. To provide reliable data and contribute to a nationwide scenario analysis, this study aims to estimate the inequality in prevalence of diabetes and prediabetes and to identify factors potentially contributing to socioeconomic inequalities in Bangladesh. This study used data from the latest Bangladesh Demographic and Health Survey (BDHS) 2017–18, a nationally representative survey. A regression-based decomposition method was applied to assess the socioeconomic contributors to inequality. The prevalence of diabetes and prediabetes were about 10 and 15% among Bangladeshi adults, respectively. Both diabetes and prediabetes were significantly associated with age, wealth status, suffering from overweight or obesity and administrative divisions of the respondents (p < 0.001). Respondents’ household wealth status accounted for about 74 and 81% of the total inequality in diabetes and prediabetes in Bangladesh, respectively. Administrative region contributed 24.85% of the inequality in prediabetes and 12.26% of the inequality in diabetes. In addition, overweight or obesity status contributed 11.37% and exposure to television contributed 5.17% of the inequality in diabetes. Diabetes and prediabetes affect a substantial proportion of the Bangladeshi adult population. Therefore, these findings should be considered in the context of current and proposed policy decision making and for tracking its progression with economic development in Bangladesh.
Keywords: Diabetes, Prediabetes, Inequality, Decomposition, Bangladesh
Introduction
Diabetes is one of the fastest growing global health problems of the twenty-first century. Globally, in 2019 about 463 million people suffered from diabetes; 79.4% of cases occurred in low- and middle-income countries, including Bangladesh [1]. More than 4.2 million people died in 2019 due to diabetes-related complications [2]. However, a large number of people are unaware that they have diabetes, which leads to underestimation of the burden. According to a global report on diabetes, 1 in 2 people with diabetes were undiagnosed [2]. Further, the prevalence of prediabetes is increasing rapidly, and it is projected that at least 470 million people worldwide will be suffering from prediabetes in 2030 [3]. Diabetes is a chronic condition that occurs when the body cannot produce or use insulin effectively, while prediabetes is characterized by blood glucose levels which are above normal but below the threshold for diabetes, increasing the risk of developing diabetes [4].
Diabetes is a major public health burden that respects neither socioeconomic status nor national boundaries. Bangladesh is among the top-10 diabetes vulnerable countries in terms of adult diabetes as well as undiagnosed diabetes [1]. Indeed, diabetes is among the top-10 diseases in Bangladesh in terms of mortality and morbidity [5]. Individuals with diabetes often suffer from severe life-threatening complications, face declining health-related quality of life, require healthcare services, and cause undue financial and mental stress on households [6, 7]. Both diabetes and prediabetes are associated with premature mortality. For instance, a recent study indicated that in adults, diabetes was associated with a loss of 8 years of potential life, while prediabetes was associated with a loss of about 2 years of potential life [8]. Along with the burden of mortality and morbidity, the economic impact is substantial. The average annual cost of diabetes per person in Bangladesh was US $297 [9]. Further, the indirect costs of diabetes such as labor-force drop out, mortality, absenteeism, and presenteeism substantially impacts society [6]. A recent study indicated that the loss of productivity-adjusted life years per person was about US $16,987, an amount which could contribute to Bangladesh’s gross domestic product [10]. In 2017, about 55,703 individuals received in-hospital care due to diabetic-related complications, and about 2,641,000 outpatient visits occurred in Bangladesh [9]. A recent meta-analysis indicated the high prevalence of prediabetes (10.1%) in Bangladesh, with a significant difference between rural and urban areas and across socioeconomic status [11]. Per the latest report, the number of patients with diabetes in Bangladesh has reached around 8.4 million, posing a big challenge to the health system [12].
Diabetes and its complications can be prevented by maintaining an appropriate diet, physical exercise, and medication; however, few individuals in Bangladesh take these preventive actions [13]. As a consequence, the percentage of the population with diabetes and prediabetes is increasing every year [11]. It is crucial to assess the prevalence of diabetes and prediabetes with recent nationwide data and to identify its distribution among various groups. Although a few studies have focused on prevalence and risk factors of diabetes and prediabetes, inequality analysis using the decomposition technique is infrequent in Bangladesh [10, 11, 14, 15]. However, a number of studies have measured and analyzed socioeconomic inequalities in both developed and developing countries [16–19]. To provide reliable data and to perform a nationwide scenario analysis, this study aims to estimate the inequality of the prevalence of diabetes and prediabetes and to identify factors potentially contributing to socioeconomic inequalities in Bangladesh. Therefore, based on the published literature, we broke down inequality into a set of potential factors to determine their relative contributions [16–19]. The findings of this study can inform investment in strategies to control diabetes and its complications in Bangladesh and elsewhere with similar socioeconomic conditions.
Methods
Study population and data source
This study used data from the latest Bangladesh Demographic and Health Survey (BDHS) 2017–18, which is a nationally representative cross-sectional survey conducted by the Ministry of Health and Family Welfare. This was the second national survey in Bangladesh that incorporated the measurement of biomarker information, including blood pressure and fasting blood glucose (FBG), as well as sociodemographic characteristics of the participants [20].
Sampling method and sample size
The 2017–18 BDHS used a two-stage stratified cluster sampling frame to select households. In the first stage, the survey selected 675 enumeration areas (EAs) and conducted household listing for each EA in both rural and urban areas. In the second stage, an average of 30 households were selected systematically from each EA. Figure 1 represents an overview of the survey’s sampling procedure. The detailed sampling and data collection procedure has been described elsewhere [20]. The survey collected data on biomarkers and relevant information from a subsample of one-fourth (4864) of the selected households. These data were collected from all individuals aged 18 years and older of these households. Blood glucose was measured for a total of 12,257 respondents, comprised of 6971 women and 5286 men. We excluded 157 respondents due to missing values. Therefore, the analytic sample of this study is 12,100, with 6919 women and 5181 men. The survey was approved by the institutional review board of MEASURE DHS and the National Research Ethics Committee of the Bangladesh Medical Research Council. As per their procedure, informed consent was obtained from all participants.
Fig. 1.
Flow diagram of sampling procedure
Outcome variables
The main outcomes in this study were diabetes and prediabetes, which were determined based on the fasting plasma glucose (FPG) level. The HemoCue Glucose 201 DM system with plasma conversion was used to measure blood glucose. Provided that respondents had fasted overnight, capillary whole blood was taken from their ring or middle finger. The first two drops of blood were wiped away, and the third drop was taken for glucose measurement. Blood glucose level was measured in millimoles per liter (mmol/L). Individuals who had a FPG level of 7.0 mmol/L or above were considered as having diabetes [4]. For this study, individuals who were taking any prescribed medicines for diabetes were also considered as having diabetes. The term prediabetes was used for people with impaired glucose tolerance and/or impaired fasting glucose, which may lead to the development of diabetes and diabetes-related complications [1]. We considered individuals as having prediabetes if their FPG ranged between 6.1 mmol/L and 6.9 mmol/L that was used in various studies in Bangladesh and in other settings [14, 21–23].
For analysis, we categorized diabetes as ‘1’ if the respondents had a FPG level of 7.0 mmol/L or above or if they were taking any prescribed medicines for diabetes and ‘0’ otherwise. Likewise, after excluding the people with diabetes, we categorized prediabetes as ‘1’ if the respondents’ FPG ranged between 6.1 mmol/L and 6.9 mmol/L and ‘0’ otherwise [1].
Explanatory variables
Evidence from prior empirical studies suggests the existence of statistically significant associations between diabetes and prediabetes and various socioeconomic, demographic, and individual-level factors [7, 11, 15, 16]. In light of the previous literature, and after logistic regression analysis this study used explanatory variables such as age, sex, level of education, household wealth status, respondents’ working status, overweight or obesity status, smoking status, caffeinated drinks, exposure to mass media, region of residence, and administrative division in the decomposition analysis. We categorized age into four groups: 18–34 years, 35–49 years, 50–64 years, and 65 years and above. Level of education was categorized as ‘no formal education’, ‘primary education’, ‘secondary education’, and ‘higher education’. Household’s socioeconomic status was measured by wealth status. BDHS calculated household wealth status by using principal component analysis from households’ durable and non-durable assets [24]. Households were scored based on the consumer goods they possessed, which ranged from televisions to bicycles to cars, and housing characteristics such as toilet facilities, drinking water, floor materials, etc. The wealth index variable was categorized as ‘poorest’, ‘poor’, ‘middle’, ‘rich’, and ‘richest’. Working status was categorized as ‘yes’ if the respondent was currently working or ‘no’ otherwise. Individuals were categorized as overweight or obese if their body mass index (BMI) was greater than or equal to 25 (kg/m2) or higher as defined by the World Health Organization [25]. Exposure to mass media was proxied by whether the household had radio or television. In terms of community-level factors, the place of residence and administrative division of the country were considered. Place of residence was categorized as ‘urban’ and ‘rural’. Although BDHS 2017–18 does not have any specific information related to lifestyle, there was information on whether the individuals smoked/used tobacco and had any caffeinated drinks before blood pressure measurement. We included smoking/tobacco use status and whether had caffeinated drinks as two dummy variables. Division variable was categorized according to the eight administrative divisions in Bangladesh: Barisal, Chattogram, Dhaka, Khulna, Mymensingh, Rajshahi, Rangpur, and Sylhet. We used Barisal as the reference category as it is a middle ranged division in terms of various health indicators [26, 27].
Measurement and analysis
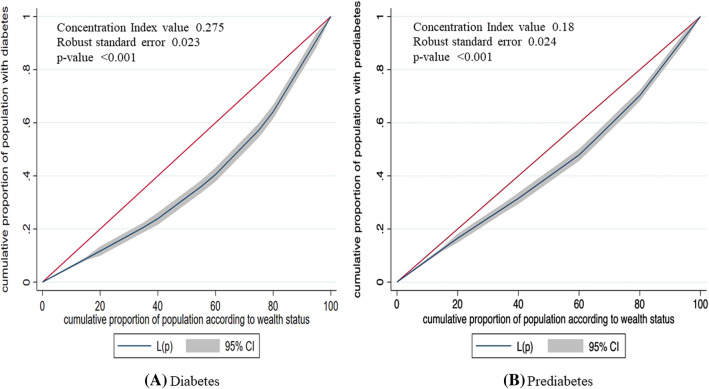
Descriptive bivariate analysis was performed using cross tables and chi-square tests to explore the determinants and the prevalence of diabetes and prediabetes in Bangladesh. The variables which were found significantly associated with diabetes and prediabetes from the chi-square tests were included in the logistic regression analysis to evaluate the association of diabetes and prediabetes with various factors, while statistical significance was determined with p values < 0.05. The adjusted odds ratios (AOR) and 95% confidence interval were also reported. To accomplish the objective of this study, the analyses were performed in several stages: plotting the concentration curves, examining the concentration indexes (CIs), and decomposition of the concentration index. First, we employed concentration curves to analyze the socioeconomic inequality of diabetes and prediabetes prevalence. Concentration curves measure inequality by plotting the cumulative percentage of respondents with diabetes (or prediabetes) against the cumulative percentage of respondents according to their socioeconomic status (wealth index). The 45° line shows the line of equality, which indicates the absence of socioeconomic inequality for diabetes (or prediabetes). If the concentration curve lies above the equality line, it indicates that the prevalence of diabetes (or prediabetes) is more concentrated among the poor respondents. If the concentration curve lies below the equality line, it indicates that the prevalence of diabetes (or prediabetes) is unequally distributed among the upper (rich) segment of the population.
Second, the CIs were calculated using the standard method developed by Kakwani et al. [28]. CIs summarize the graphical information (i.e., the area between the equality line and the concentration curve) generated by a concentration curve. A convenient simple computational formula for the concentration index can be written as:
where CI = concentration index; represents the (weighted) mean of the diabetes (or prediabetes); h is the diabetes (or prediabetes); r represents the fractional rank of the individual in the distribution of wealth index, and cov indicates the weighted covariance between h and r. The value of the concentration index ranges from -1 to + 1, where a negative index value is equivalent to a pro-poor concentration curve and a positive index corresponds to a pro-rich concentration curve. Moreover, a concentration index value of zero implies that there is no inequality for diabetes (or prediabetes) across people from different socioeconomic status.
Finally, to identify the contribution of various socioeconomic factors to the inequality in diabetes and prediabetes, we used a regression-based decomposition analysis as proposed by O’Donnell and colleagues [29]. Decomposition analysis indicates the effects and contributions of various socioeconomic and demographic factors of respondents to the wealth-related inequality. This technique can provide information about the responsiveness of diabetes and prediabetes to the change in the determinants variable which is crucial for prioritizing public health interventions [30]. For these purposes, the regression model for the health outcome Y (diabetes or prediabetes) with the set of k determinants ( can be written as:
where represents the selected explanatory (socioeconomic) variables, is the coefficient of , and is the stochastic error term. The CI for diabetes (or prediabetes) from the above regression (Y) can be decomposed as:
Here, CI is the concentration index; represents the mean of diabetes or prediabetes (Y); is the average of Kth socioeconomic variable(s) i.e., ; represents the concentration index of , and is the generalized concentration of the error term (); implies the elasticity of the prevalence of diabetes (or prediabetes) with respect to the explanatory variable. is the residual component that denotes the part of income-induced inequality in diabetes (or prediabetes) that cannot be explained by the explanatory variables. The findings from the decomposition approach were presented in elasticity, concentration index value, absolute contribution (same unit as the concentration index), and the percentage (relative) contribution. To adjust the complex sampling procedure of the BDHS study, we used the Stata svy command in this study. All analyses were performed using the statistical software package Stata (version 16.00; Stata Corp LP, College Station, Texas).
Patient and public involvement
No patients were involved in developing the research question, outcome measure and design of the study. We are unable to disseminate the results of the research directly to the study participants.
Results
Background characteristics of the study sample
The sociodemographic and health-related characteristics of the respondents and details of their households and communities are presented in Table 1. The highest percentage (44.75%) of respondents were in the 18–34 years age group, followed by the 35–49 years age group (28.4%). The majority of the respondents were female (57.18%) and employed (60.84%). About 30% of the respondents had primary education, while 26% had no formal education. About 25% of respondents were either overweight or obese. About half of the respondents (48.35%) had exposure to television, while only 1.55% had exposure to radio. About 23% of the respondents were living in Dhaka division, and the lowest percentage (5.52%) were in Barisal division. Among the respondents, about 14% had smoked/used tobacco and about 6% had caffeinated drinks before their blood pressure measurement.
Table 1.
Distribution of socioeconomic and individual-level characteristics of the study sample
| Number N | Percentage % | |
|---|---|---|
| Age | ||
| 18–34 | 5415 | 44.75 |
| 35–49 | 3436 | 28.4 |
| 50–64 | 2041 | 16.87 |
| 65 and above | 1208 | 9.98 |
| Sex | ||
| Male | 5181 | 42.82 |
| Female | 6919 | 57.18 |
| Level of education | ||
| No education | 3117 | 25.76 |
| Primary | 3620 | 29.92 |
| Secondary | 3562 | 29.44 |
| Higher | 1800 | 14.88 |
| Wealth index | ||
| Poorest | 2339 | 19.33 |
| Poor | 2391 | 19.76 |
| Middle | 2495 | 20.62 |
| Rich | 2409 | 19.91 |
| Richest | 2466 | 20.38 |
| Currently employed | ||
| No | 4738 | 39.16 |
| Yes | 7362 | 60.84 |
| BMI status | ||
| Underweight or normal | 9083 | 75.07 |
| Overweight or Obese | 3017 | 24.93 |
| Watching television (TV) | ||
| Yes | 5850 | 48.35 |
| No | 6250 | 51.65 |
| Exposure to radio | ||
| Yes | 188 | 1.55 |
| No | 11,912 | 98.45 |
| Smoked/used tobacco | ||
| Yes | 1708 | 14.12 |
| No | 10,392 | 85.88 |
| Caffeinated drink | ||
| Yes | 759 | 6.27 |
| No | 11,341 | 93.73 |
| Place of residence | ||
| Urban | 3211 | 26.54 |
| Rural | 8889 | 73.46 |
| Division | ||
| Barisal | 668 | 5.52 |
| Chattogram | 2084 | 17.22 |
| Dhaka | 2791 | 23.07 |
| Khulna | 1513 | 12.5 |
| Mymensingh | 990 | 8.18 |
| Rajshahi | 1751 | 14.47 |
| Rangpur | 1516 | 12.53 |
| Sylhet | 789 | 6.52 |
Prevalence of diabetes and prediabetes across background characteristics
Table 2 represents the prevalence of diabetes and prediabetes according to respondents’ background characteristics. This study found that 9.94 and 15.23% of the respondents had diabetes and prediabetes, respectively. The prevalence of diabetes was significantly associated with age (p < 0.001). The prevalence was the highest (16.25%) among respondents in the 50–64 age group, followed by those aged 65 and above (15.07%). The percentage of diabetes was slightly higher among males (10.52%) compared to females (9.50%), but this difference was not statistically significant. The prevalence of diabetes was slightly higher among educated participants. The prevalence was highest among the richest group (18.32%) and among individuals who were not employed (11.85%), watched television regularly (12.84%), and were overweight or obese (15.53%). The prevalence of diabetes was slightly higher among the respondents who were found as smoking/using tobacco compared to those who did not smoke/use tobacco (10.54% versus 9.84%). For those who had caffeinated drinks, the prevalence of diabetes was significantly higher (p = 0.002) compared to those who had no caffeinated drinks. The prevalence of diabetes was significantly higher in urban areas (13.26%) compared to rural areas (8.74%). Across administrative divisions, the prevalence of diabetes was highest in Dhaka division (14.32%) and lowest in Rangpur division (5.58%).
Table 2.
Prevalence of diabetes and prediabetes according to background characteristics (N = 12,100)
| Diabetes n (%) | Total participants (n) | Prediabetes n (%) | Total Participants (n) | |
|---|---|---|---|---|
| Age | ||||
| 18–34 | 284 (5.25) | 5415 | 687 (13.4) | 5130 |
| 35–49 | 404 (11.77) | 3436 | 517 (17.04) | 3032 |
| 50–64 | 332 (16.25) | 2041 | 292 (17.08) | 1709 |
| 65 and above | 182 (15.07) | 1208 | 164 (15.98) | 1026 |
| P value | < 0.001 | < 0.001 | ||
| Sex | ||||
| Male | 545 (10.52) | 5181 | 692 (14.93) | 4636 |
| Female | 657 (9.50) | 6919 | 968 (15.46) | 6262 |
| P value | p = 0.07 | p = 0.49 | ||
| Level of education | ||||
| No education | 307 (9.86) | 3177 | 452 (16.08) | 2809 |
| Primary | 370 (10.23) | 3620 | 468 (14.39) | 3250 |
| Secondary | 344 (9.67) | 3562 | 491 (15.27) | 3218 |
| Higher | 180 (10.02) | 1800 | 249 (15.36) | 1620 |
| P value | p = 0.92 | p = 0.51 | ||
| Wealth index | ||||
| Poorest | 134 (5.75) | 2339 | 273 (12.38) | 2204 |
| Poor | 143 (5.96) | 2391 | 242 (10.77) | 2248 |
| Middle | 198 (7.95) | 2495 | 283(12.31) | 2297 |
| Rich | 276 (11.44) | 2409 | 383 (17.93) | 2134 |
| Richest | 452 (18.32) | 2466 | 480 (23.81) | 2013 |
| P value | < 0.001 | < 0.001 | ||
| Currently working | ||||
| No | 561 (11.85) | 4738 | 702 (16.80) | 4177 |
| Yes | 641 (8.71) | 7361 | 958 (14.26) | 6720 |
| P value | < 0.001 | p = 0.003 | ||
| BMI status | ||||
| Normal | 734 (8.08) | 9083 | 1,166 (13.97) | 8349 |
| Overweight or obese | 468 (15.53) | 3017 | 494 (19.37) | 2548 |
| P value | < 0.001 | < 0.001 | ||
| Exposure to TV | ||||
| Yes | 751 (12.84) | 5850 | 906 (17.76) | 5798 |
| No | 451 (7.22) | 6250 | 754 (13.01) | 5099 |
| P value | < 0.001 | < 0.001 | ||
| Exposure to Radio | ||||
| Yes | 29 (15.65) | 188 | 29 (18.14) | 158 |
| No | 1173 (9.85) | 11,912 | 1631 (15.19) | 10,739 |
| P value | p = 0.036 | p = 0.47 | ||
| Smoked/used tobacco | ||||
| Yes | 180 (10.54) | 1708 | 223 (14.60) | 1528 |
| No | 1022 (9.84) | 10,392 | 1437 (15.33) | 9369 |
| P value | p = 0.438 | p = 0.489 | ||
| Caffeinated drink | ||||
| Yes | 102 (13.41) | 758 | 112 (17.08) | 656 |
| No | 1101 (9.71) | 11,342 | 1547 (15.11) | 10,241 |
| P value | p = 0.002 | p = 0.233 | ||
| Place of residence | ||||
| Urban | 426 (13.26) | 3211 | 548 (19.69) | 2785 |
| Rural | 777 (8.74) | 8889 | 1111 (13.7) | 8112 |
| P value | < 0.001 | < 0.001 | ||
| Administrative division | ||||
| Barisal | 64 (9.64) | 668 | 107 (17.69) | 603 |
| Chattogram | 233 (11.20) | 2084 | 296 (15.99) | 1850 |
| Dhaka | 400 (14.32) | 2791 | 596 (24.91) | 2392 |
| Khulna | 125 (8.28) | 1513 | 155 (11.22) | 1387 |
| Mymensingh | 78 (7.86) | 990 | 115 (12.64) | 912 |
| Rajshahi | 141 (8.05) | 1751 | 162 (10.05) | 1610 |
| Rangpur | 85 (5.58) | 1516 | 137 (9.58) | 1431 |
| Sylhet | 77 (9.73) | 789 | 91 (12.85) | 712 |
| P value | < 0.001 | < 0.001 | ||
| Total | 1,203 (9.94) | 12,100 | 1,660 (15.23) | 10,897 |
In terms of prediabetes, the prevalence was the highest (17.08%) among the age group 50–64 years, followed by the 35–49 years age group (17.04%). The prevalence of prediabetes was also high for young adults aged 18–34 years (13.4%). The prevalence of prediabetes was the highest among the richest group (23.81%), urban dwellers (19.69%), those who watched television (17.76%), those were overweight or obese (19.37%), and among those who lived in Dhaka division.
Factors associated with diabetes and prediabetes
Table 3 shows the risk factors associated with diabetes and prediabetes in the multivariate logistic regression model. We observed that respondents’ age, wealth status, suffering from overweight or obesity and administrative divisions were significant predictors of both diabetes and prediabetes in Bangladesh. Respondents aged 35–49, 50–64 and aged 65 and above had 2.42, 3.85 and 3.48 times higher odds of having diabetes compared to people in the age group 18–34, respectively, (p < 0.001). Respondents from households belonging to richer and the richest wealth quintile had 1.69 and 2.53 times higher odds of having diabetes compared to respondents from the poorest wealth quintile (p < 0.001). We found that respondents who were working at the time of data collection had significantly lower odds of suffering from diabetes (AOR = 0.83, p < 0.05) compared to their counterparts. Those who were suffering from overweight or obesity were found to have 70% higher odds of having diabetes (AOR = 1.70, p < 0.001) compared to those who were not overweight or obese. Respondents from Dhaka division had 30% greater odds of suffering from diabetes compared to those from Barisal (AOR = 1.30, p < 0.05). On the other hand, respondents from Khulna division had 26% lower odds (AOR = 0.74, p < 0.05) and respondents from Rangpur division had 37% lower odds of suffering from diabetes compared to those from Barisal. In terms of prediabetes, we found those who were in the age group 35–49 (AOR = 1.52, p < 0.001), 50–64 (AOR = 1.62, p < 0.001) and aged 65 and above (AOR = 1.45, p < 0.001) had significantly greater odds of having prediabetes compared to those in 18–34 years age group. We found that those who belongs to the richest and richer households had 78% (p < 0.001) and 34% (p < 0.01) greater odds of having prediabetes, respectively, compared to those from the poorest households. Respondents having overweight or obesity status was found to have significantly higher odds of having prediabetes (AOR = 1.29, p < 0.001) compared to their counterparts. Those who were from Dhaka division had 37% greater odds of having prediabetes compared to people from Barisal division while people from other divisions had significantly lower odds of having prediabetes.
Table 3.
Associated factors of diabetes and prediabetes in Bangladesh
| Diabetes | Prediabetes | |||||
|---|---|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | |||
| Lower limit | Upper limit | Lower limit | Upper limit | |||
| Age | ||||||
| 18–34 (ref) | ||||||
| 35–49 | 2.42*** | 2.06 | 2.85 | 1.52*** | 1.33 | 1.74 |
| 50–64 | 3.85*** | 3.24 | 4.57 | 1.62*** | 1.38 | 1.89 |
| 65 and above | 3.48*** | 2.83 | 4.29 | 1.45*** | 1.20 | 1.76 |
| Sex | ||||||
| Male (ref) | ||||||
| Female | 0.97 | 0.83 | 1.12 | – | – | – |
| Wealth index | ||||||
| Poorest (ref) | ||||||
| Poor | 0.96 | 0.75 | 1.24 | 0.89 | 0.74 | 1.08 |
| Middle | 1.25 | 0.98 | 1.61 | 0.97 | 0.80 | 1.19 |
| Richer | 1.69*** | 1.31 | 2.18 | 1.34** | 1.09 | 1.64 |
| Richest | 2.53*** | 1.93 | 3.30 | 1.78*** | 1.42 | 2.22 |
| Currently working | ||||||
| No | ||||||
| Yes | 0.83* | 0.71 | 0.97 | 0.94 | 0.83 | 1.05 |
| Overweight or obese | ||||||
| No (ref) | ||||||
| Yes | 1.70*** | 1.49 | 1.95 | 1.29*** | 1.13 | 1.46 |
| Exposure to TV | ||||||
| No | ||||||
| Yes | 1.08 | 0.91 | 1.27 | 0.97 | 0.84 | 1.12 |
| Exposure to radio | ||||||
| No (ref) | ||||||
| Yes | 1.11 | 0.71 | 1.72 | – | – | – |
| Caffeinated drink | ||||||
| No (ref) | ||||||
| Yes | 1.12 | 0.90 | 1.39 | – | – | – |
| Region of residence | ||||||
| Rural (ref) | ||||||
| Urban | 1.00 | 0.87 | 1.15 | 0.95 | 0.84 | 1.08 |
| Administrative division | ||||||
| Barisal (ref) | ||||||
| Chattogram | 0.94 | 0.74 | 1.21 | 0.76* | 0.62 | 0.94 |
| Dhaka | 1.30* | 1.02 | 1.66 | 1.37** | 1.12 | 1.67 |
| Khulna | 0.74* | 0.57 | 0.95 | 0.50*** | 0.40 | 0.62 |
| Mymensingh | 0.83 | 0.63 | 1.10 | 0.67*** | 0.54 | 0.84 |
| Rajshahi | 0.85 | 0.66 | 1.11 | 0.48*** | 0.38 | 0.60 |
| Rangpur | 0.63** | 0.47 | 0.83 | 0.49*** | 0.39 | 0.62 |
| Sylhet | 0.94 | 0.73 | 1.22 | 0.61*** | 0.49 | 0.77 |
***p < 0.001
**p < 0.01
*p < 0.05
Inequality in diabetes and prediabetes
We estimated the concentration curve and concentration index to represent the inequality in diabetes and prediabetes of Bangladeshi adults (Fig. 2). For both cases, the concentration curve lies below the line of equality (45º line), which implies a higher concentration of both diabetes and prediabetes towards individuals from the upper wealth quintiles.
Fig. 2.
Concentration curve for diabetes (A) and prediabetes (B). Here, red line shows the line of equality and CI denotes confidence interval
We found the value of the CIs for diabetes and prediabetes were 0.275 (p < 0.001) and 0.18 (p < 0.001), respectively (Fig. 2). Therefore, this study found a pro-rich socioeconomic inequality for diabetes and prediabetes in Bangladesh.
Decomposition of concentration index for diabetes and prediabetes
Table 4 represents the contribution of various socioeconomic and demographic factors to inequalities in diabetes and prediabetes. The column ‘Elasticity’ expresses the change in the dependent variable (socioeconomic inequality in diabetes or prediabetes) associated with a one-unit change in the explanatory variables. A positive or negative sign in elasticity indicates an increasing or decreasing change of diabetes or prediabetes in association with a positive change in the determinant [30]. The column ‘CI’ represents the distribution of the determinants with reference to wealth quintiles. The positive or negative sign of the CI indicates that the factors were more concentrated among the rich or poor households, respectively.
Table 4.
Decomposition of concentration index for diabetes and prediabetes
| Socio-economic variables | Diabetes | Prediabetes | ||||||
|---|---|---|---|---|---|---|---|---|
| Elasticity | CI | Contribution to overall CI = 0.275 | Elasticity | CI | Contribution to overall CI = 0.18 | |||
| Absolute contribution | Percentage contribution | Absolute contribution | Percentage contribution | |||||
| Age | ||||||||
| 18–34 (Ref) | ||||||||
| 35–49 | 0.228 | − 0.015 | − 0.003 | − 1.217 | 0.073 | − 0.015 | − 0.001 | − 0.597 |
| 50–64 | 0.205 | − 0.025 | − 0.005 | − 1.875 | 0.047 | − 0.025 | − 0.001 | − 0.667 |
| 65 and above | 0.112 | − 0.049 | − 0.006 | − 2.002 | 0.018 | − 0.049 | − 0.001 | − 0.501 |
| Total | − 0.014 | − 5.094 | − 0.003 | − 1.765 | ||||
| Sex | ||||||||
| Male (Ref) | ||||||||
| Female | − 0.067 | − 0.011 | 0.001 | 0.273 | 0.00004 | − 0.011 | − 4.666e − 07 | − 0003 |
| Level of education | ||||||||
| No education (Ref) | ||||||||
| Primary | 0.076 | − 0.186 | − 0.014 | − 5.082 | − 0.031 | − 0.186 | 0.006 | 3.182 |
| Secondary | 0.059 | 0.182 | 0.011 | 3.92 | − 0.036 | 0.182 | − 0.007 | − 3.672 |
| Higher | 0.015 | 0.467 | 0.007 | 2.614 | − 0.034 | 0.467 | − 0.016 | − 9.022 |
| Total | 0.004 | 1.452 | − 0.017 | − 9.512 | ||||
| Wealth index | ||||||||
| Poorest (Ref) | ||||||||
| Poor | − 0.006 | − 0.518 | 0.003 | 1.147 | − 0.027 | − 0.518 | 0.014 | 7.622 |
| Middle | 0.034 | − 0.015 | − 0.001 | − 0.186 | − 0.004 | − 0.015 | 0.0001 | 0.032 |
| Richer | 0.089 | 0.491 | 0.043 | 15.793 | 0.056 | 0.491 | 0.028 | 15.221 |
| Richest | 0.158 | 1.000 | 0.158 | 57.360 | 0.105 | 1.000 | 0.105 | 58.488 |
| Total | 0.203 | 74.114 | 0.1471 | 81.363 | ||||
| Currently working | ||||||||
| No (Ref) | ||||||||
| Yes | − 0.145 | − 0.177 | 0.026 | 9.328 | − 0.039 | − 0.177 | 0.007 | 3.881 |
| Overweight or obesity | ||||||||
| No (Ref) | ||||||||
| Yes | 0.095 | 0.327 | 0.031 | 11.372 | 0.04 | 0.327 | 0.013 | 7.225 |
| Watching television (TV) | ||||||||
| No (Ref) | ||||||||
| Yes | 0.020 | 0.715 | 0.014 | 5.175 | − 0.01 | 0.715 | − 0.007 | − 3.815 |
| Exposure to radio | ||||||||
| No (Ref) | ||||||||
| Yes | 0.004 | 0.292 | 0.001 | 0.476 | 0.001 | 0.292 | 0.0003 | 0.185 |
| Smoked/used tobacco | ||||||||
| No (ref) | ||||||||
| Yes | − 0.009 | − 0.160 | 0.001 | 0.502 | − 0.008 | − 0.160 | 0.001 | 0.687 |
| Caffeinated drink | ||||||||
| No (ref) | ||||||||
| Yes | 0.005 | 0.163 | 0.001 | 0.297 | 0.003 | 0.163 | 0.0004 | 0.236 |
| Place of residence | ||||||||
| Rural (Ref) | ||||||||
| Urban | 0.003 | 0.514 | 0.002 | 0.582 | 0.002 | 0.514 | 0.001 | 0.517 |
| Division | ||||||||
| Barisal (Ref) | ||||||||
| Chattogram | − 0.004 | 0.151 | − 0.001 | − 0.222 | − 0.038 | 0.151 | − 0.006 | − 3.180 |
| Dhaka | 0.050 | 0.314 | 0.016 | 5.665 | 0.044 | 0.314 | 0.014 | 7.676 |
| Khulna | − 0.034 | 0.059 | − 0.002 | − 0.737 | − 0.066 | 0.059 | − 0.004 | − 2.174 |
| Mymensingh | − 0.010 | − 0.229 | 0.002 | 0.834 | − 0.027 | − 0.229 | 0.006 | 3.443 |
| Rajshahi | − 0.018 | − 0.117 | 0.002 | 0.767 | − 0.08 | − 0.117 | 0.009 | 5.242 |
| Rangpur | − 0.048 | − 0.340 | 0.016 | 5.927 | − 0.071 | − 0.34 | 0.024 | 13.395 |
| Sylhet | − 0.002 | − 0.032 | 0.0001 | 0.022 | − 0.025 | − 0.032 | 0.001 | 0.443 |
| Total | 0.033 | 12.256 | 0.044 | 24.845 | ||||
| Explained CI | 0.303 | 110.733 | 0.187 | 100.847 | ||||
| Residual CI | − 0.028 | − 10.733 | − 0.007 | − 0.847 | ||||
The percentage contribution represents the relative contribution of each determinant included in the model to the overall socioeconomic-related inequality in diabetes or prediabetes. A positive percentage contribution denotes a factor that results in increasing the observed socioeconomic inequality of diabetes or prediabetes. In contrast, a negative percentage contribution indicates a factor that is likely to decrease the observed socioeconomic inequality of diabetes or prediabetes. Household wealth index was responsible for about 74% of the overall inequality in diabetes and 81% inequality in prediabetes. Overweight or obesity status of respondents explained 11.37% of the inequality in diabetes and about 7.23% of the inequality in prediabetes. Administrative division also made a significant contribution to inequality in prediabetes (24.85%) and diabetes (12.26%). Working status of respondents contributed about 9.33% of the inequality in diabetes and 3.88% of the inequality in prediabetes. Exposure to television contributed to 5.18% and level of education contributed to 1.45% of the overall inequality in diabetes among the respondents. The unexplained or residual contributing factors to the socioeconomic inequalities in diabetes and prediabetes accounted for − 10.73% and − 0.847%, respectively.
Discussion
Various non-communicable diseases (NCDs), including diabetes, are the largest global public health concern and a major challenge for the sustainable development goal of reducing premature deaths from NCDs by one-third by 2030. Socio-economic inequality analysis has become an important tool to influence policy based on inequalities. To the best of our knowledge, this is the first nationally representative study to quantify the socioeconomic inequality in diabetes and prediabetes and its determinants in Bangladesh. The findings showed that both diabetes and prediabetes were concentrated among the more affluent. Household wealth index, administrative region, being overweight or obese, working status, exposure to television, and living in urban areas were the major contributors to the pro-rich socioeconomic inequalities in both diabetes and prediabetes.
Diabetes is an emerging public health problem in Bangladesh. We observed that about 10% and 14% of the participants (aged 18 and above) had diabetes and prediabetes according to the latest BDHS survey. A recent systematic review and meta-analysis study indicated that the pooled prevalence of diabetes and prediabetes in the general population was 7.8% and 10.1%, respectively [11]. An earlier study using BDHS 2011 indicated that the prevalence of diabetes and prediabetes were 9.7% and 22.4%, respectively, among individuals aged 35 years or more in Bangladesh [14]. The authors observed that both diabetes and prediabetes were associated with age, wealth status, administrative divisions and overweight or obese people [14, 31]. Similar findings were also observed from another study in Bangladesh which indicated that in addition to these factors, hypertension and level of physical activity were significant predictors of the prevalence of diabetes among Bangladeshi adults [32]. However, nearly half of the population with diabetes may still be undiagnosed in Bangladesh, which leads to an underestimation of the real burden of the disease [33]. Lack of diagnosis is due to insufficient access to health care, insufficient diabetes screening materials, poor knowledge, social taboo, and poor health systems [26, 34]. This study observed that the prevalence of diabetes and prediabetes was positively associated with age, wealth status, living in urban areas, watching television regularly, being overweight or obese, and residing in a large administrative division like Dhaka, the capital of Bangladesh [7, 11, 15–17, 32]. Like the previous round of BDHS, we did not find any significant association with sex of the participants and the prevalence of diabetes and prediabetes [14]. Two decades earlier, a study observed that rural male respondents were at higher risk of diabetes than rural female in Bangladesh [23]. The same increasing pattern was also observed in rural India and rural Sri Lanka [35]. Indeed, the prevalence of both diabetes and prediabetes has been increasing rapidly in South Asia [11, 35]. The prevalence of diabetes were 7.7% in India, 19.9% in Pakistan, 9.5% in Nepal, 10.3% in Sri Lanka and 10.2% in Myanmar, respectively [1, 35–38]. A recent nationwide study in India indicated the overall prevalence of diabetes and prediabetes were 6.7 and 5.6%, respectively, where two-thirds of individuals with diabetes lived in urban areas [31]. In the south Asian context, the urban populations demonstrated a higher prevalence of diabetes, however, no distinct trend was observed regarding the prevalence of diabetes across sex of the population [35]. This study observed a pro-rich socioeconomic inequality, indicating that diabetes and prediabetes are concentrated among the more affluent households in Bangladesh. Our results are similar to those found in other settings, where the wealthiest people were more prone to diabetes and prediabetes [39]. A study in Sri Lanka observed that the prevalence of diabetes showed a more consistent pro-rich distribution in females compared to males [16]. Various studies have shown that the wealthiest households report significantly more morbidities in all categories of ailments and in-hospital admissions [15, 40, 41]. However, the opposite scenario, namely the pro-poor inequality in the prevalence of diabetes, has been observed in many high-income countries [42, 43]. Studies show that during times of economic transitions, adverse health behaviors are initially encountered among the wealthiest group and are later transmitted to the lower socioeconomic strata [16, 44]. The observed pro-rich pattern of diabetes and prediabetes may suggest that Bangladesh is in an economic transitional stage; the country recently received the United Nations’ recommendation for graduating from the category of a Least Developed Country to a developing country [45].
The key finding of the current study was that the household wealth index accounted for about 74 and 81% of the total inequality in diabetes and prediabetes in Bangladesh, respectively. Similar findings have been observed in many settings, indicating that people from the highest socioeconomic groups were more prone to diabetes and prediabetes [46–48]. Individuals in wealthier families have greater access to high-calorie food, including junk food, and are less involved in physical work, which might increase the risk of various NCDs [32, 49, 50]. However, individuals from lower socioeconomic status are more likely to have undiagnosed diabetes in Bangladesh [26]. These results are not surprising, as nutritional improvements were often observed among urban residents and those from the richest households [51]. Thus, we found undernutrition was more concentrated among the poorest people, while overweight or obese individuals were more likely to belong to the richest households in Bangladesh [51, 52].
This study indicated that being overweight or obese accounted for 11.37% of the total inequality in diabetes and about 7.22% of the inequality in prediabetes. In addition to making the largest contribution to socioeconomic inequalities in the prevalence of diabetes and prediabetes in various settings, being overweight and obese has become a public health concern [46, 52]. Recently, an increasing trend of being overweight or obese has been observed among urban and wealthier individuals in Bangladesh [52, 53]. Various reasons might contribute to increasing rates of overweight and obesity, such as the reduction in physical activity due to replacing physically intensive work with technologically intensive work, watching television, using social media and the internet, and other factors. Further, people from wealthier families in lower-income countries often have a greater risk of being overweight or obese due to a greater access to food and a lower level of physical activity due to increased leisure time [54, 55].
This study indicated that watching television and level of education contributed a significant portion of the overall inequality in diabetes among Bangladeshi adults. Therefore, interventions should prioritize the prevention of obesity, specifically by targeting the more affluent segment of society to reduce unhealthy diets and to increase physical activity. Further, we observed that the working status of people contributed about 9% of the inequality in diabetes and 4% of the inequality in prediabetes. Physical activity often increases oxygen consumption throughout the body and maintains blood glucose levels to preserve the central nervous system, which may reduce the risk of diabetes and other related NCDs [15, 56]. A study indicated that moderate to high levels of physical activity reduced morbidity and mortality in people with diabetes [32, 49, 50]. Therefore, policy and prevention programs must be tailored to the context of prevention, early diagnosis, adherence to treatment, and control of diabetes.
This study also observed that regional differences in diabetes and prediabetes significantly contributed to inequality in diabetes and prediabetes. Although the reasons are unclear, certain regions are expected to have high numbers of undiagnosed diabetes cases [26]. Some areas may have lower accessibility to healthcare services, religious conservatism, or low awareness of diabetes and prediabetes [57]. Although there was no significant socioeconomic differences (e.g., age, SES), each division had distinct characteristics. For example, Chattogram and Barisal division located in the coastal area of Bangladesh and people belonged to these divisions often consumes higher raw salts than other region in Bangladesh [15]. Again, greater accessibility to healthcare services and awareness were more common in Khulna Division [15, 58]. In Sylhet division. Various factors such as distance of health facilities, fragile communication system, hard-to-rich area and religious conservatism were significantly associated with the low healthcare service utilization [58]. Therefore, developing administrative region-specific policies should be considered for tackling diabetes and prediabetes in those areas. Further investigation of the risk factors underlying these regional differences in Bangladesh is warranted.
The study has several limitations. First, this study was based on cross-sectional data; therefore, this study only depicts associations between variables and cannot determine causation. Second, due to the unavailability of data on physical activity levels, dietary practices, and family history of diabetes and hypertension, this study could not control these factors, which were found as associated with prediabetes and diabetes in other studies [11, 59, 60]. Despite these limitations, the main strength of this study is its large, nationwide random sample, which allowed us to determine the nationwide prevalence and socioeconomic inequalities related to diabetes and prediabetes; thus, our findings are representative of the entire country.
Conclusion
Diabetes and prediabetes are an overwhelming public health problem in Bangladesh. This study has sketched inequalities in the prevalence of diabetes and prediabetes among Bangladeshi adults. This study indicated that household wealth index, administrative region, being overweight or obese, individual’s working status, exposure to television, and living in urban areas were the major contributors to the pro-rich socioeconomic inequalities in both diabetes and prediabetes in Bangladesh. Therefore, these study findings should be considered in the context of current and proposed policymaking. Finally, we believe that comprehensive national diabetes surveillance is urgently needed in Bangladesh.
Author contributions
ARS conducted the design of the study, interpretation of data, and writing of the initial manuscript. ARS and MK contributed to the statistical analysis plan and wrote the statistical methods section. ARS and MK reviewed the manuscript. ARS is the guarantor of this paper. All authors reviewed, contributed to, and approved the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
The electronic datasets can be freely downloaded from the DHS’s website through the following link: https://dhsprogram.com/data.
Declarations
Conflict of interest
Authors have no conflicts of interest.
Ethical approval
This study did not require ethical approval as it used unidentifiable secondary DHS dataset. According to the DHS, written informed consent was obtained from mothers/caretakers on behalf of the children enrolled in the survey. The DHS data are publicly accessible and were made available to us upon request by Measure DHS. No identifiable information was included in the dataset and no attempt was made to identify any individual interviewed in the survey.
Consent for publication
Not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Abdur Razzaque Sarker, Email: razzaque.sarker@gmail.com, Email: razzaque@bids.org.bd.
Moriam Khanam, Email: moriam.ihe@du.ac.bd.
References
- 1.IDF Diabetes atlas. Lancet. 2019 doi: 10.1016/S0140-6736(55)92135-8. [DOI] [Google Scholar]
- 2.IDF. Diabetes in South-East Asia. In: The International Diabetes Federation-the prevalence of diabetes [Internet]. 2019 [cited 10 Mar 2020]. Available: https://idf.org/our-network/regions-members/south-east-asia/diabetes-in-sea.html. Accessed 3 June 2021.
- 3.Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379:2279–2290. doi: 10.1016/S0140-6736(12)60283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ADA Classification and diagnosis of diabetes: standards of medical care in diabetes. Diabetes Care. 2018;41:S13–S27. doi: 10.2337/dc18-S002. [DOI] [PubMed] [Google Scholar]
- 5.IHME. What causes the most death and disability combined? In: Measuring what matters- Bangladesh [Internet]. 2020 [cited 18 Mar 2021]. Available: http://www.healthdata.org/bangladesh. Accessed 13 May 2021.
- 6.Bommer C, Heesemann E, Sagalova V, Manne-Goehler J, Atun R, Bärnighausen T, et al. The global economic burden of diabetes in adults aged 20–79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. 2017 doi: 10.1016/S2213-8587(17)30097-9. [DOI] [PubMed] [Google Scholar]
- 7.Barua L, Faruque M, Chowdhury HA, Banik PC, Ali L. Health-related quality of life and its predictors among the type 2 diabetes population of Bangladesh: a nation-wide cross-sectional study. J Diabetes Investig. 2021 doi: 10.1111/jdi.13331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rapoport M, Chetrit A, Cantrell D, Novikov I, Roth J, Dankner R. Years of potential life lost in pre-diabetes and diabetes mellitus: data from a 40-year follow-up of the Israel study on glucose intolerance, obesity and hypertension. BMJ Open Diabetes Res Care. 2021;9:1–8. doi: 10.1136/bmjdrc-2020-001981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sarker AR, Sultana M. Health and economic burden of diabetes in Bangladesh: priorities for attention and control. J Diabetes. 2017;12:1118–1119. doi: 10.1111/1753-0407.12587. [DOI] [PubMed] [Google Scholar]
- 10.Afroz A, Hird TR, Zomer E, Owen A, Chen L, Ademi Z, et al. The impact of diabetes on the productivity and economy of Bangladesh. BMJ Glob Heal. 2020;5:1–8. doi: 10.1136/bmjgh-2020-002420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akhtar S, Nasir JA, Sarwar A, Nasr N, Javed A, Majeed R, et al. Prevalence of diabetes and pre-diabetes in Bangladesh: a systematic review and meta-analysis. BMJ Open. 2020;10:e036086. doi: 10.1136/bmjopen-2019-036086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dhaka Tribune. Over 8 million people have diabetes in Bangladesh. Tribune Health Desk. 13 Nov 2020. Available: https://www.dhakatribune.com/health/2020/11/13/over-8-million-people-have-diabetes-in-bangladesh. Accessed 12 July 2021.
- 13.Islam SMS, Biswas T, Bhuiyan FA, Mustafa K, Islam A. Patients’ perspective of disease and medication adherence for type 2 diabetes in an urban area in Bangladesh: a qualitative study. BMC Res Notes. 2017;10:131. doi: 10.1186/s13104-017-2454-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akter S, Rahman MM, Abe SK, Sultana P. Prevalence of diabetes and prediabetes and their risk factors among Bangladeshi adults: a nationwide survey. Bull World Health Organ. 2014;92:204–213A. doi: 10.2471/BLT.13.128371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ali N, Akram R, Sheikh N, Sarker ARAR, Sultana M. Sex-specific prevalence, inequality and associated predictors of hypertension, diabetes, and comorbidity among Bangladeshi adults: results from a nationwide cross-sectional demographic and health survey. BMJ Open. 2019 doi: 10.1136/bmjopen-2019-029364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Silva AP, De Silva SHP, Haniffa R, Liyanage IK, Jayasinghe S, Katulanda P, et al. Inequalities in the prevalence of diabetes mellitus and its risk factors in Sri Lanka: a lower middle income country. Int J Equity Health. 2018 doi: 10.1186/s12939-018-0759-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Espelt A, Borrell C, Palència L, Goday A, Spadea T, Gnavi R, et al. Socioeconomic inequalities in the incidence and prevalence of type 2 diabetes mellitus in Europe. Gac Sanit. 2013 doi: 10.1016/j.gaceta.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Hosseinpoor AR, Bergen N, Kunst A, Harper S, Guthold R, Rekve D, et al. Socioeconomic inequalities in risk factors for non communicable diseases in low-income and middle-income countries: results from the world health survey. BMC Public Health. 2012 doi: 10.1186/1471-2458-12-912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Espelt A, Kunst AE, Palència L, Gnavi R, Borrell C. Twenty years of socio-economic inequalities in type 2 diabetes mellitus prevalence in Spain, 1987–2006. Eur J Public Health. 2012 doi: 10.1093/eurpub/ckr158. [DOI] [PubMed] [Google Scholar]
- 20.National Institute of Population Research and Training (NIPORT), and ICF. Bangladesh demographic and health survey 2017–18. Dhaka, Bangladesh, and Rockville, Maryland, USA: NIPORT and ICF. 2020.
- 21.Duc Son LENT, Kusama K, Hung NTK, Loan TTH, Van Chuyen N, Kunii D, et al. Prevalence and risk factors for diabetes in Ho Chi Minh City, Vietnam. Diabet Med. 2004 doi: 10.1111/j.1464-5491.2004.01159.x. [DOI] [PubMed] [Google Scholar]
- 22.Khambalia A, Phongsavan P, Smith BJ, Keke K, Dan L, Fitzhardinge A, et al. Prevalence and risk factors of diabetes and impaired fasting glucose in Nauru. BMC Public Health. 2011 doi: 10.1186/1471-2458-11-719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Unwin N, Shaw J, Zimmet P, Alberti K. Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. Diabet Med. 2002;19:708–723. doi: 10.1046/j.1464-5491.2002.00835.x. [DOI] [PubMed] [Google Scholar]
- 24.Rutstein SO, Johnson K. The DHS wealth index. DHS comparative reports No. 6. Calverton, Maryland, USA: ORC Macro, Maryland; 2004. Available: https://dhsprogram.com/pubs/pdf/cr6/cr6.pdf. Accessed 20 July 2021.
- 25.WHO. Obesity and overweight. In: Facts about overweight and obesity [Internet]. 2021 [cited 20 Mar 2021]. Available: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 15 July 2021.
- 26.Hasan MM, Tasnim F, Tariqujjaman M, Ahmed S. Socioeconomic inequalities of undiagnosed diabetes in a resource-poor setting: insights from the cross-sectional Bangladesh demographic and health survey 2011. Int J Environ Res Public Health. 2019;16:1–12. doi: 10.3390/ijerph16010115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sarker ARAR, Akram R, Ali N, Sultana M. Coverage and factors associated with full immunisation among children aged 12–59 months in Bangladesh: insights from the nationwide cross-sectional demographic and health survey. BMJ Open. 2019;9:e028020. doi: 10.1136/bmjopen-2018-028020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kakwani NC. Income inequality and poverty: methods of estimation and policy applications. Popul Dev Rev. 1980 doi: 10.2307/1972940. [DOI] [Google Scholar]
- 29.O’Donnell O, van Doorslaer E, Wagstaff A, Lindelow M, O’Donnell O, van Doorslaer E, et al. Analyzing health equity using household survey data. A guide to techniques and their implementation. Washington: The World Bank; 2008. [Google Scholar]
- 30.Shifti DM, Chojenta C, Holliday EG, Loxton D. Socioeconomic inequality in short birth interval in Ethiopia: a decomposition analysis. BMC Public Health. 2020;20:1–13. doi: 10.1186/s12889-020-09537-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chandrupatla SG, Khalid I, Muthuluri T, Dantala S, Tavares M. Diabetes and prediabetes prevalence among young and middle-aged adults in India, with an analysis of geographic differences: findings from the National Family Health Survey. Epidemiol Health. 2021 doi: 10.4178/epih.e2020065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Talukder A, Hossain MZ. Prevalence of diabetes mellitus and its associated factors in Bangladesh: application of two-level logistic regression model. Sci Rep. 2020;10:1–7. doi: 10.1038/s41598-020-66084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Latif ZA, Jain A, Rahman MM. Evaluation of management, control, complications and psychosocial aspects of diabetics in Bangladesh: DiabCare Bangladesh 2008. Bangladesh Med Res Counc Bull. 2011 doi: 10.3329/bmrcb.v37i1.7793. [DOI] [PubMed] [Google Scholar]
- 34.Manne-Goehler J, Atun R, Stokes A, Goehler A, Houinato D, Houehanou C, et al. Diabetes diagnosis and care in sub-Saharan Africa: pooled analysis of individual data from 12 countries. Lancet Diabetes Endocrinol. 2016 doi: 10.1016/S2213-8587(16)30181-4. [DOI] [PubMed] [Google Scholar]
- 35.Jayawardena R, Ranasinghe P, Byrne NM, Soares MJ, Katulanda P, Hills AP. Prevalence and trends of the diabetes epidemic in South Asia: a systematic review and meta-analysis. BMC Public Health. 2012 doi: 10.1186/1471-2458-12-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tandon N, Anjana RM, Mohan V, Kaur T, Afshin A, Ong K, et al. The increasing burden of diabetes and variations among the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Health. 2018 doi: 10.1016/S2214-109X(18)30387-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feng L, Naheed A, De Silva HA, Jehan I, Raqib R, Islam MT, et al. Regional variation in comorbid prediabetes and diabetes and associated factors among hypertensive individuals in rural Bangladesh, Pakistan, and Sri Lanka. J Obes. 2019 doi: 10.1155/2019/4914158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aung WP, Bjertness E, Htet AS, Stigum H, Kjøllesdal MKR. Trends in diabetes prevalence, awareness, treatment and control in Yangon region, Myanmar, between 2004 and 2014, two cross-sectional studies. Int J Environ Res Public Health. 2019 doi: 10.3390/ijerph16183461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Andrade FCD, López-Ortega M. Contextualizing health and aging in the Americas: effects of space, time and place. Springer; 2018. The magnitude of health inequalities among older adults in Brazil and Mexico; pp. 181–198. [Google Scholar]
- 40.Mahumud RA, Sarker AR, Sultana M, Islam Z, Khan J, Morton A. Distribution and determinants of out-of-pocket healthcare expenditures in Bangladesh. J Prev Med Public Health. 2017;50:91–99. doi: 10.3961/jpmph.16.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khan JAM, Ahmed S, Maclennan M, Sarker AR, Sultana M, Rahman H. Benefit incidence analysis of healthcare in Bangladesh – equity matters for universal health coverage. Health Policy Plan. 2016;32:1–7. doi: 10.1093/heapol/czw131. [DOI] [PubMed] [Google Scholar]
- 42.Espelt A, Borrell C, Roskam AJ, Rodríguez-Sanz M, Stirbu I, Dalmau-Bueno A, et al. Socioeconomic inequalities in diabetes mellitus across Europe at the beginning of the 21st century. Diabetologia. 2008 doi: 10.1007/s00125-008-1146-1. [DOI] [PubMed] [Google Scholar]
- 43.Al-Hanawi MK, Chirwa GC, Pulok MH. Socio-economic inequalities in diabetes prevalence in the Kingdom of Saudi Arabia. Int J Health Plan Manag. 2020 doi: 10.1002/hpm.2899. [DOI] [PubMed] [Google Scholar]
- 44.Blakely T, Hales S, Kieft C, Wilson N, Woodward A. The global distribution of risk factors by poverty level. Bull World Health Organ. 2005;83:118–126. [PMC free article] [PubMed] [Google Scholar]
- 45.Byron RK. Bangladesh gets UN recommendation for graduating from LDC status. The Daily Star. 27 Feb 2021. Available: https://www.thedailystar.net/business/news/bangladesh-gets-un-recommendation-graduating-ldc-status-2051857. Accessed 25 July 2021.
- 46.Mutyambizi C, Booysen F, Stokes A, Pavlova M, Groot W. Lifestyle and socio-economic inequalities in diabetes prevalence in South Africa: a decomposition analysis. PLoS ONE. 2019 doi: 10.1371/journal.pone.0211208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Corsi DJ, Subramanian SV. Socioeconomic gradients and distribution of diabetes, hypertension, and obesity in India. JAMA Netw Open. 2019 doi: 10.1001/jamanetworkopen.2019.0411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Adekanmbi VT, Uthman OA, Erqou S, Echouffo-Tcheugui JB, Harhay MN, Harhay MO. Epidemiology of prediabetes and diabetes in Namibia, Africa: a multilevel analysis. J Diabetes. 2019 doi: 10.1111/1753-0407.12829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mirhadyan L, Moradi L, Saeid P, Afsaneh K, Nejad LE. Junk food consumption and its associated factors in high school students in Rasht in 2017. J Res Dev Nurs Midwifery. 2020;17:52–66. doi: 10.29252/jgbfnm.17.1.52. [DOI] [Google Scholar]
- 50.Yin H, Wu Q, Cui Y, Hao Y, Liu C, Li Y, et al. Socioeconomic status and prevalence of chronic non-communicable diseases in Chinese women: a structural equation modelling approach. BMJ Open. 2017 doi: 10.1136/bmjopen-2016-014402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sarker AR, Sultana M, Sheikh N, Akram R, Ali N, Alam R, et al. Inequality of childhood undernutrition in Bangladesh: a decomposition approach. Int J Heal Plann Manag. 2019 doi: 10.1002/hpm.2918. [DOI] [PubMed] [Google Scholar]
- 52.Hasan E, Khanam M, Shimul SN. Socio-economic inequalities in overweight and obesity among women of reproductive age in Bangladesh: a decomposition approach. BMC Womens Health. 2020;20:1–11. doi: 10.1186/s12905-020-01135-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Banik S, Rahman M. Prevalence of overweight and obesity in Bangladesh: a systematic review of the literature. Curr Obes Rep. 2018 doi: 10.1007/s13679-018-0323-x. [DOI] [PubMed] [Google Scholar]
- 54.Chowdhury MAB, Adnan MM, Hassan MZ. Trends, prevalence and risk factors of overweight and obesity among women of reproductive age in Bangladesh: a pooled analysis of five national cross-sectional surveys. BMJ Open. 2018 doi: 10.1136/bmjopen-2017-018468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ghose B. Frequency of TV viewing and prevalence of overweight and obesity among adult women in Bangladesh: a cross-sectional study. BMJ Open. 2017 doi: 10.1136/bmjopen-2016-014399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.ADA Physical activity/exercise and diabetes. Diabetes Care. 2004;27:S73–S77. [Google Scholar]
- 57.Pulok MH, Uddin J, Enemark U, Hossin MZ. Socioeconomic inequality in maternal healthcare: an analysis of regional variation in Bangladesh. Health Place. 2018 doi: 10.1016/j.healthplace.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 58.Sarker AR, Sheikh N, Mahumud RA, Sultana M. Determinants of adolescent maternal healthcare utilization in Bangladesh. Public Health. 2018;157:94–103. doi: 10.1016/j.puhe.2018.01.010. [DOI] [PubMed] [Google Scholar]
- 59.Vakharia JD, Agrawal S, Molino J, Topor LS. Family history of diabetes is associated with increased risk of recurrent diabetic ketoacidosis in pediatric patients. Endocr Pract. 2020 doi: 10.4158/ep-2019-0351. [DOI] [PubMed] [Google Scholar]
- 60.Molla GJ, Ismail-Beigi F, Larijani B, Khaloo P, Moosaie F, Alemi H, et al. Smoking and diabetes control in adults with type 1 and type 2 diabetes: a nationwide study from the 2018 National Program for Prevention and Control of Diabetes of Iran. Can J Diabetes. 2020 doi: 10.1016/j.jcjd.2019.07.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The electronic datasets can be freely downloaded from the DHS’s website through the following link: https://dhsprogram.com/data.