Abstract
Background
Regdanvimab has decreased the time to clinical recovery from coronavirus disease 2019 (COVID-19) and lowered the rate of oxygen therapy according to the results from phase 2/3 randomized controlled trial. More information is needed about the effects and safety of regdanvimab.
Methods
We analyzed data for patients with high-risk mild or moderate COVID-19 being admitted to Busan Medical Center between December 1, 2020 and April 16, 2021. A propensity score (PS) matched analysis was conducted to compare patients treated with and without regdanvimab. The primary outcome was in-hospital death or disease aggravation which means the need for oxygen therapy (low- or high-flow oxygen therapy and mechanical ventilation) and secondary outcomes comprised the length of hospital stay and adverse reactions.
Results
Among 1,617 selected patients, 970 (60.0%) were indicated for regdanvimab. Of these, 377 (38.9%) were administered with regdanvimab. Among a 1:1 PS-matched cohort of 377 patients each treated with and without regdanvimab, 19 (5%) and 81 (21.5%) reached the composite outcome of death, or disease aggravation, respectively (absolute risk difference, −16.4%; 95% confidence interval [CI], −21.1, −11.7; relative risk difference, 76.5%; P < 0.001). Regdanvimab significantly reduced the composite outcome of death, or disease aggravation in univariate (odds ratio [OR], 0.194; 95% CI, 0.112–0.320; P < 0.001) and multivariable-adjusted analyses (OR, 0.169; 95% CI, 0.095–0.289; P < 0.001). The hospital stay was shorter for the group with than without regdanvimab. Some hematological adverse reactions were more frequent in the group without regdanvimab, but other adverse reactions did not significantly differ between the groups.
Conclusion
Regdanvimab was associated with a significantly lower risk of disease aggravation without increasing adverse reactions.
Keywords: Regdanvimab, Monoclonal, Antibody, Mild-to-Moderate, COVID-19, Effectiveness
Graphical Abstract
INTRODUCTION
The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was identified at the end of 2019 as the cause of the outbreak of acute respiratory syndrome in Wuhan, Hubei Province, China.1 Thereafter, it spread rapidly around the world, causing a pandemic, and was named coronavirus disease 2019 (COVID-19).2 Vaccination against SARS-CoV-2 began in several countries from mid-December 2020, and by ≤ 11 months later, nearly half of the global population had received at least one dose of vaccine.3 However vaccine inequity is significant among nations, and only about 3.6% of the population in low-income countries have been vaccinated with even one dose.3 Globally, 2.9 million people per week contract COVID-19, and the number of new deaths is still > 49,000 per week.4 As of November 1, 2021, the global cumulative numbers of persons infected with COVID-19 and consequent deaths have exceeded 247 and 5 million, respectively.5 Various vaccines and treatments are being developed to overcome COVID-19, but more therapeutic strategies are needed. Furthermore, viruses mutate over time, which seems to affect viral transmission and disease severity, as well as vaccine and therapeutic efficacy.6,7,8,9,10 Until recently, the only drugs recommended by the World Health Organization (WHO) for treating patients with COVID-19 are corticosteroids and interleukin-6 receptor blockers (tocilizumab or sarilumab) in severe or critical patients.11 In the revised guidelines on September 24, 2021, the casirivimab/imdevimab combination was recommended in mild or moderate patients at the high risk of severe disease, and severe patients with seronegative status. Among antivirals, remdesivir has been approved by the U.S. Food and Drug Administration (FDA) for hospitalized patients with COVID-19 who require supplemental oxygen.12
Monoclonal antibodies (mAbs) targeting specific regions of viral surface proteins should be promising treatments against infectious diseases,13,14 and they are therapeutically effective against several viruses.15,16 Among the anti-SARS-CoV-2 mAbs for the treating COVID-19, combination therapies of bamlanivimab/etesevimab and casirivimab/imdevimab, and sotrovimab monotherapy have received emergency use authorization (EUA) from the FDA for outpatients with mild-to-moderate COVID-19 at high risk and they are recommended by the National Institutes of Health (NIH).12
Regdanvimab (CT-P59) is a recombinant neutralizing mAb constructed from the blood of convalescing patients with COVID-19, and it potently neutralizes the receptor-binding site of the SARS-CoV-2 spike protein as an antigen target.17 Results from a phase 2/3 randomized, double-blind, placebo-controlled clinical trial of outpatients with mild-to-moderate SARS-CoV-2 infection found that regdanvimab shortened the time to conversion to a negative real-time quantitative reverse transcriptase polymerase chain reaction (RT-PCR) result and clinical recovery without causing serious side effects or death, and lowered rates of oxygen therapy.18 Regdanvimab received product approval based on these results on February 5, 2021, under the condition of submitting the results of the phase 3 clinical trial thereafter, and it became available to improve clinical symptoms in patients aged ≥ 18 years at high-risk mild or moderate COVID-19 in Korea.19 High-risk was defined as age ≥ 60 years, or having ≥ 1 underlying disease such as cardiovascular or chronic respiratory diseases including asthma, hypertension, or diabetes, and moderate refers to patients with pneumonia.20 On March 26, 2021, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) concluded that regdanvimab could be used to treat adult patients with COVID-19 who do not require supplemental oxygen but are at high risk of progression to severity.21 Then, on September 17, 2021, the Ministry of Food and Drug Safety extended the scope of administration based on the results of the phase 3 clinical trial of regdanvimab and granted official product approval. Accordingly, the indications for regdanvimab were designated as high-risk mild and all moderate COVID-19 patients, and the high-risk included age > 50 years, body mass index (BMI) > 30 kg/m2, cardiovascular disease (including hypertension), chronic lung disease (including asthma), diabetes mellitus, chronic kidney disease (including dialysis), chronic liver disease, or immunosuppression due to disease or treatment.22
No drugs had been approved in Korea for treating mild-to-moderate COVID-19 until the conditional approval of regdanvimab.23 Therefore, regdanvimab is presently the only agent available in Korea that could prevent progression in patients at high-risk mild-to-moderate COVID-19. However, since the results of the phase 3 clinical trial have not yet been published and accumulated data are scant, the basis for judgment regarding treatment selection in routine clinical practice is insufficient.
Busan Medical Center (BMC) in Busan, the second largest city in Korea, is a currently operating, dedicated COVID-19 treatment facility. As of April 16, 2021, about 3,000 inpatients have been treated, and regdanvimab has been administered to > 400 patients since its approval. This study aimed to evaluate the effectiveness and safety of regdanvimab administered to patients at high-risk mild-to-moderate COVID-19 in real-world clinical practice. Given the lack of accumulated data about regdanvimab, we hope that the present results will serve as a meaningful basis for drug selection to treat patients with COVID-19.
METHODS
Patient population and data elements
This observational study retrospectively analyzed the medical records of adult patients (aged ≥ 18 years) with COVID-19 (confirmed by RT-PCR) who were admitted to BMC between December 1, 2020 and April 16, 2021. Each patient followed up until death or discharge. The study period ended on May 14, 2021, allowing for the last date of discharge in all patients. The patients with high-risk mild-to-moderate COVID-19 eligible for regdanvimab were extracted and assigned to groups that were treated or not with regdanvimab. Since regdanvimab was supplied and administered at BMC from February 19, 2021, all patients given regdanvimab were hospitalized after that date. The patients who were not treated with regdanvimab were admitted before February 19, 2021, and some who were hospitalized when regdanvimab became accessible refused to be treated with it.
Baseline characteristics including age, sex, BMI, comorbidities, and co-medications were analyzed. Comorbidities consisted of diabetes mellitus, hypertension, and cardiovascular, chronic lung, chronic kidney, and chronic liver diseases, as well as pneumonia, which is an indicator of moderate COVID-19. Co-medications included those that were presumed to affect COVID-19 treatment in previous studies, and those administered to treat comorbidities. These were classified as angiotensin-converting enzyme inhibitors (ACEIs)/angiotensin receptor blockers (ARBs),24,25 statins,26,27 aspirin,28,29 and immunomodulators.30,31 Immunomodulators include immunosuppressants and corticosteroids.
Several laboratory parameters at baseline that were also collected from electronic medical records (EMRs), included complete blood cell count, electrolytes, renal function, hepatic panel, C-reactive protein (CRP), lactate dehydrogenase (LDH), D-dimer, troponin I, ferritin, and creatine kinase.
Study exposure
The exposure in this study was regdanvimab. Regdanvimab administration was also identified in the EMRs. Regdanvimab was administered at the recommended dose of a single intravenous infusion of 40 mg/kg. Azithromycin, corticosteroids, hydroxychloroquine, lopinavir/ritonavir, and remdesivir, were evaluated as other treatment exposures of interest.
Study outcomes
The primary outcome was a composite of in-hospital death, or disease aggravation. Disease aggravation indicators included the need for oxygen therapy (low- or high-flow oxygen therapy, and mechanical ventilation) or transfer to a tertiary hospital for further invasive treatment. The secondary outcomes were length of hospital stay (days) and adverse reactions including fever or systemic pain, injection site reaction, hypersensitivity, and gastrointestinal, hematological, renal, and hepatic toxicity.
Statistical analysis
We assessed differences in demographic characteristics, baseline clinical characteristics, and co-medications between the groups. Summary statistics are presented as medians with interquartile ranges (IQRs) for continuous variables, and numbers and percentages for categorical variables. Between-group differences were examined using independent t-tests and χ2 tests, as appropriate. The low accuracy of χ2 tests was compensated for using Fisher exact tests.
Although the study was limited to patients suitable for regdanvimab administration, the baseline characteristics between the regdanvimab treated and untreated groups differed. Therefore, we balanced measured covariates by estimating propensity scores (PS) of regdanvimab administration using a multivariable logistic regression model, adjusted for the variables of age, sex, BMI, comorbidities, and disease severity. PSs were matched using the optimal method without designation of a caliper to prevent omission of the group treated with regdanvimab, and the results were confirmed. All baseline variables in the PS-matched cohort were descriptively analyzed. Detailed information on the modeling of PS matching was described in Appendix 1.
Differences in outcomes between groups with and without (reference) regdanvimab therapy in the PS-matched cohort and whether the estimated effect of regdanvimab remained consistent in the overall cohort were determined by multivariable logistic regression analyses. Variables in the multivariable analyses that affect the prognosis of COVID-19 were included as risk factors in the regdanvimab dosing criteria.21 Co-medications were included, and sex was added based on recent findings.32,33,34 To confirm the consistency of the results, we performed sensitivity analyses by changing the covariates included in the PS estimation model, changing the matching method, and adding covariates in the multivariable logistic regression model of analyzing matching data.
Missing data
Among the 970 patients included in the study, 73 (7.5%) had no BMI information and were excluded from analyses. Some of the 897 patients included in the analysis had missing baseline laboratory values, and Table 1 shows laboratory results after excluding them.
Table 1. Baseline characteristics in unmatched and propensity score matched cohorts of patients.
| Characteristics | Unmatched (n = 897) | Matched (n = 754) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No regdanvimab (n = 520, 58.0%) | Regdanvimab (n = 377, 42.0%) | P value | SMD | No regdanvimab (n = 377) | Regdanvimab (n = 377) | Matching | P value | SMD | |||
| Demographics | |||||||||||
| Age, yr | 65 (57–75) | 61 (53–68) | < 0.001 | 0.343 | 62 (55–69) | 61 (53–68) | Matched | 0.239 | 0.086 | ||
| Sex | 0.220 | 0.083 | Matched | 0.825 | 0.016 | ||||||
| Male | 205 (55.6) | 164 (44.4) | 161 (49.5) | 164 (50.5) | |||||||
| Female | 315 (59.7) | 213 (40.3) | 216 (50.4) | 213 (49.7) | |||||||
| BMI, kg/m2 | 23.5 (21.5–25.7) | 23.9 (22.3–26.1) | 0.003 | 0.198 | 24.0 (22.1–26.3) | 23.9 (22.3–26.1) | Matched | 0.465 | 0.053 | ||
| Comorbidities | |||||||||||
| Cardiovascular disease | 82 (73.9) | 29 (26.1) | < 0.001 | 0.253 | 27 (48.2) | 29 (51.8) | Matched | 0.781 | 0.020 | ||
| Chronic lung disease | 30 (78.9) | 8 (21.1) | 0.007 | 0.188 | 6 (42.9) | 8 (57.1) | Matched | 0.590 | 0.039 | ||
| Diabetes mellitus | 128 (59.8) | 86 (40.2) | 0.532 | 0.042 | 83 (49.1) | 86 (50.9) | Matched | 0.793 | 0.019 | ||
| Hypertension | 236 (61.0) | 151 (39.0) | 0.112 | 0.108 | 154 (50.5) | 151 (49.5) | Matched | 0.824 | 0.016 | ||
| Chronic kidney disease | 12 (75.0) | 4 (25.0) | 0.164 | 0.097 | 3 (42.9) | 4 (57.1) | Matched | 1.000a | 0.028 | ||
| Chronic liver disease | 14 (50.0) | 14 (50.0) | 0.385 | 0.058 | 11 (44.0) | 14 (56.0) | Matched | 0.542 | 0.044 | ||
| Pneumonia | 199 (54.1) | 169 (45.9) | 0.049 | 0.133 | 161 (48.8) | 169 (51.2) | Matched | 0.557 | 0.043 | ||
| Co-medications | |||||||||||
| ACEIs/ARBs | 144 (55.2) | 117 (44.8) | 0.277 | 0.073 | 97 (45.3) | 117 (54.7) | 0.106 | 0.118 | |||
| Statins | 148 (58.5) | 105 (41.5) | 0.841 | 0.014 | 92 (46.7) | 105 (53.3) | 0.281 | 0.079 | |||
| Aspirin | 59 (57.3) | 44 (42.7) | 0.880 | 0.010 | 27 (38.0) | 44 (62.0) | 0.034 | 0.155 | |||
| Immunomodulators | 6 (50.0) | 6 (50.0) | 0.573 | 0.038 | 5 (45.5) | 6 (54.5) | 0.761 | 0.022 | |||
Data are presented as number (%) or medians (interquartile range). Continuous variables were analyzed using Student t-tests. Categorical variables were analyzed using χ2 tests. Chronic kidney disease in matched cohorts was analyzed using Fisher exact test.
SMD = standardized mean difference, BMI = body mass index, ACEI = angiotensin-converting enzyme inhibitor, ARB = angiotensin-receptor blocker.
aFisher exact test.
All data were statistically using R version 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria), and values with P < 0.05 were considered significant.
Ethics statement
The Institutional Review Board (IRB) of Pusan National University approved this study (PNU IRB/2021_66_HR) and waived the requirement for informed consent. The data used in this study were anonymized after extracting patient data from the institution’s EMRs and did not contain any personally identifiable information.
RESULTS
Baseline patient characteristics
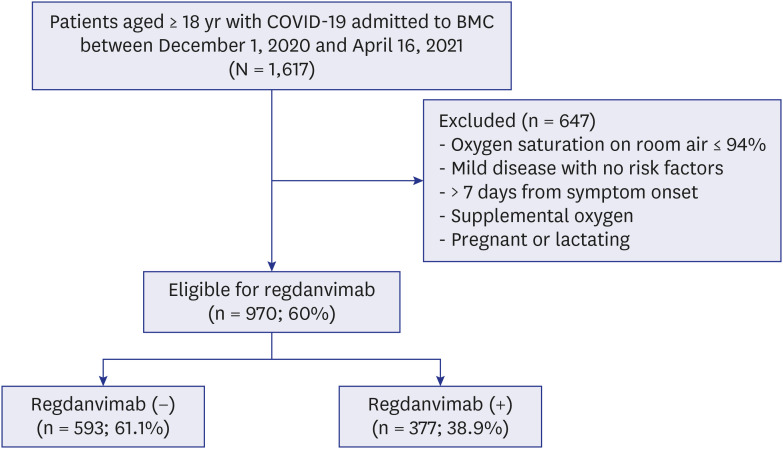
Among 1,617 patients with COVID-19 who were admitted during the study period, 970 (60.0%) were eligible for regdanvimab administration. These were assigned to receive treatment with (n = 377; 38.9%) or without (n = 593; 61.1%) regdanvimab (Fig. 1). Some immobile patients (n = 73) in the untreated group with missing height and weight records were excluded from analysis. Table 1 shows the baseline characteristics of the 897 patients. Patients in group without regdanvimab were older (median age 65 [IQR, 57–75] vs. 61 [53–68] years, P < 0.001), but sex did not significantly differ (P = 0.220). They had a lower BMI (23.5 [21.5–25.7] vs. 23.9 [22.3–26.1] kg/m2, P = 0.003), and a higher proportion of comorbid cardiovascular (73.9% vs. 26.1%, P < 0.001) and chronic lung (78.9% vs. 21.1%, P = 0.007) diseases. The proportion of patients with moderate COVID-19 (with pneumonia), was also higher in the untreated group (54.1% vs. 45.9%, P = 0.049). Other comorbidities (diabetes mellitus, hypertension, chronic kidney disease, and chronic liver disease) and co-medications (ACEIs/ARBs, statins, aspirin, and immunomodulators) did not significantly differ between the two groups.
Fig. 1. Flow chart of the study cohort.
COVID-19 = coronavirus disease 2019, BMC = Busan Medical Center.
Propensity-matched cohort characteristics
We created a PS-matched cohort of 754 patients, among whom, 377 were treated with regdanvimab and 377 were not. Demographics and comorbidities did not significantly differ between the PS-matched groups (Table 1). Among the co-medications that were not included in the matching variables, aspirin was prescribed to more patients in the regdanvimab group (Table 1). Supplementary Fig. 1 shows the distributions of covariates before and after PS matching. Differences in baseline characteristics were attenuated in the matched, compared with the unmatched cohort (Supplementary Fig. 2).
Patients in the PS-matched cohort who were treated with regdanvimab had significantly lower CRP (0.4 [0.4–1.8] vs. 0.7 [0.4–2.7] mg/dL, P < 0.001), LDH (206.0 [180.8–240.0] vs. 216.0 [190.5–257.0] IU/L, P = 0.011), and ferritin (169.0 [100.5–307.0] vs. 221.5 [124.3–378.3] ng/mL, P = 0.048] values, whereas D-dimer, troponin I, and creatine kinase values did not significantly differ (Table 2). Supplementary Table 1 shows details of the missing baseline laboratory data.
Table 2. Baseline laboratory data in propensity score-matched cohort.
| Laboratory marker | No regdanvimab (n = 377) | Regdanvimab (n = 377) | P value | SMD |
|---|---|---|---|---|
| WBC, 103/µL | 4.6 (3.7–5.9) | 4.6 (3.7–5.9) | 0.484 | 0.051 |
| Hemoglobin, g/dL | 13.5 (12.5–14.3) | 13.5 (12.5–14.4) | 0.444 | 0.056 |
| Platelet count, 103/µL | 187.0 (152.0–235.5) | 180.0 (149.0–216.0) | 0.005 | 0.205 |
| Absolute neutrophil count, /µL | 2,916 (2,154–3,926) | 2,834 (2,037–3,982) | 0.142 | 0.107 |
| Absolute lymphocyte count, /µL | 1,058 (790–1,431) | 1,206 (928–1,564) | < 0.001 | 0.243 |
| Na, mmol/L | 139.0 (137.0–140.5) | 139.0 (138.0–141.0) | 0.002 | 0.224 |
| K, mmol/L | 4.0 (3.8–4.2) | 4.0 (3.7–4.2) | 0.306 | 0.075 |
| Creatinine, mg/dL | 0.7 (0.6–0.9) | 0.7 (0.6–0.9) | 0.703 | 0.028 |
| GFR, mL/min | 97.2 (79.9–110.8) | 95.8 (80.0–110.6) | 0.626 | 0.036 |
| AST, IU/L | 28.0 (22.0–38.0) | 26.0 (21.0–32.0) | 0.202 | 0.093 |
| ALT, IU/L | 23.0 (17.0–36.0) | 23.0 (17.0–34.0) | 0.488 | 0.051 |
| Total bilirubin, mg/dL | 0.5 (0.4–0.7) | 0.6 (0.4–0.7) | 0.847 | 0.014 |
| CRP, mg/dL | 0.7 (0.4–2.7) | 0.4 (0.4–1.8) | < 0.001 | 0.255 |
| LDH, IU/L | 216.0 (190.5–257.0) | 206.0 (180.8–240.0) | 0.011 | 0.185 |
| D-dimer, ng/mL | 138.5 (95.8–224.5) | 146.0 (102.8–208.0) | 0.101 | 0.125 |
| Troponin I, ng/mL | 0.004 (0.002–0.009) | 0.004 (0.003–0.006) | 0.860 | 0.014 |
| Ferritin, ng/mL | 221.5 (124.3–378.3) | 169.0 (100.5–307.0) | 0.048 | 0.158 |
| Creatine kinase, U/L | 83.0 (58.0–123.2) | 79.0 (55.3–116.0) | 0.800 | 0.019 |
Data are presented as medians (interquartile range). Variables were analyzed using Student t-tests.
SMD = standardized mean difference, WBC = white blood cell, GFR = glomerular filtration rate, AST = aspartate transaminase, ALT = alanine transaminase, CRP = C-reactive protein, LDH = lactate dehydrogenase.
Regarding the use of other unapproved treatments for COVID-19, azithromycin, corticosteroids, lopinavir/ritonavir, and remdesivir were used significantly more in the regdanvimab-untreated group than in the regdanvimab-treated group throughout the entire hospital stay, and similar results were obtained except that remdesivir was not used in both groups, even if limited to administration before progressing to severe disease (Table 3).
Table 3. Use of other therapeutics in propensity score-matched cohort.
| Therapeutic drug | Total (N = 754) | No regdanvimab (n = 377) | Regdanvimab (n = 377) | P value | |
|---|---|---|---|---|---|
| Entire period | |||||
| Azithromycin | 256 (34.0) | 235 (62.3) | 21 (5.6) | < 0.001 | |
| Corticosteroids | 270 (35.8) | 180 (47.7) | 90 (23.9) | < 0.001 | |
| Hydroxychloroquine | 2 (0.3) | 1 (0.3) | 1 (0.3) | 1.000a | |
| Lopinavir/ritonavir | 59 (7.8) | 59 (15.6) | 0 (0.0) | < 0.001 | |
| Remdesivir | 72 (9.5) | 62 (16.4) | 10 (2.7) | < 0.001 | |
| Before progressing to severe disease | |||||
| Azithromycin | 240 (31.8) | 220 (58.4) | 20 (5.3) | < 0.001 | |
| Corticosteroids | 222 (29.4) | 141 (37.4) | 81 (21.5) | < 0.001 | |
| Hydroxychloroquine | 2 (0.3) | 1 (0.3) | 1 (0.3) | 1.000a | |
| Lopinavir/ritonavir | 53 (7.0) | 53 (14.1) | 0 (0.0) | < 0.001 | |
| Remdesivir | - | - | - | - | |
Data are presented as number (%). Variables were analyzed using χ2 tests.
aFisher exact test.
Clinical outcomes of PS-matched cohort
Table 4 shows the clinical outcomes in the PS-matched cohort. The composite outcome of death, or disease aggravation was reached by 19 (5%) and 81 (21.5%) patients treated with and without regdanvimab, respectively (absolute risk difference, −16.4%; 95% confidence interval [CI], −21.1, −11.7; relative risk difference [RRR], 76.5%; P < 0.001). Regdanvimab was also associated with a significant reduction in the composite outcome of death, or disease aggravation in univariate (odds ratio [OR], 0.194; 95% CI, 0.112, 0.320; P < 0.001) and multivariable-adjusted analyses (OR, 0.169; 95% CI, 0.095, 0.289; P < 0.001) (Supplementary Table 2). The secondary outcome, length of hospital stay, was shorter in the group treated with, than without regdanvimab (mean, 11.9 ± 3.3 vs. 13.7 ± 5.4 days; P < 0.001). The hematological adverse reactions of white blood cell abnormalities, thrombocytopenia, and lymphocytopenia were more frequent in the group that were not treated with regdanvimab, but other investigated adverse reactions did not significantly differ between the groups (Table 4).
Table 4. Clinical outcomes in propensity score-matched cohort.
| Clinical outcome | No regdanvimab (n = 377) | Regdanvimab (n = 377) | P value | ||
|---|---|---|---|---|---|
| Composite outcome of death, or disease aggravation | 81 (21.5) | 19 (5.0) | < 0.001 | ||
| Death | 0 | 0 | - | ||
| Disease aggravation | 81 (21.5) | 19 (5.0) | < 0.001 | ||
| Length of hospital stay, day | 13.7 ± 5.4 | 11.9 ± 3.3 | < 0.001 | ||
| Adverse reactions | |||||
| Fever or systemic pain | 62 (16.4) | 57 (15.1) | 0.617 | ||
| Injection site reaction | - | - | - | ||
| Hypersensitivity | 1 (0.3) | 1 (0.3) | 1.000a | ||
| Gastrointestinal toxicity | 13 (3.4) | 6 (1.6) | 0.104 | ||
| Abnormality of white blood cell | < 0.001 | ||||
| Elevation, > 10 × 103/µL | 45 (11.9) | 19 (5.0) | |||
| Decrease, < 4 × 103/µL | 56 (14.9) | 29 (7.7) | |||
| Decrease in hemoglobin, < 10.0 g/dL | 10 (2.7) | 5 (1.3) | 0.192 | ||
| Decrease in platelet, < 130 × 103/µL | 22 (5.8) | 9 (2.4) | 0.017 | ||
| Decrease in ANC | 0.188a | ||||
| Mild, 1,000–1,500/µL | 31 (8.2) | 23 (6.1) | |||
| Moderate, 500–1,000/µL | 12 (3.2) | 6 (1.6) | |||
| Severe, < 500/µL | 1 (0.3) | 0 (0.0) | |||
| Decrease in ALC, < 800/µL | 45 (11.9) | 11 (2.9) | < 0.001 | ||
| Abnormality of serum sodium | 0.373a | ||||
| Elevation, > 150 mmol/L | 0 (0.0) | 0 (0.0) | |||
| Decrease, < 130 mmol/L | 4 (1.1) | 1 (0.3) | |||
| Abnormality of serum potassium | 0.342a | ||||
| Elevation, > 5.5 mmol/L | 3 (0.8) | 0 (0.0) | |||
| Decrease, < 3 mmol/L | 2 (0.5) | 2 (0.5) | |||
| Renal toxicity | 6 (1.6) | 7 (1.9) | 0.780 | ||
| Liver toxicity | 12 (3.2) | 5 (1.3) | 0.086 | ||
Data are presented as number (%) or mean ± SD. Continuous and categorical variables were analyzed using Student’s t-tests and χ2 tests, respectively.
ANC = absolute neutrophil count, ALC = absolute lymphocyte count.
aFisher exact test.
Multivariable adjustment in the overall cohort
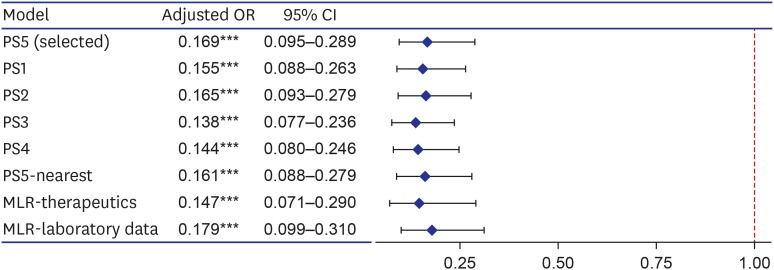
Regdanvimab was significantly associated with a reduction in the composite outcome of death, or disease aggravation in the overall cohort in the multivariable-adjusted analysis (OR, 0.148; 95% CI, 0.084, 0.247; P < 0.001) (Supplementary Table 2). Supplementary Table 2 shows the association between regdanvimab and the composite outcome of death, or disease aggravation among the analytical methods in the PS-matched and overall cohorts. These results were consistent with sensitivity analyses performed by various methods (Fig. 2).
Fig. 2. Forest plot for effects of regdanvimab on composite outcome of death, or disease aggravation in sensitivity analyses. Sensitivity analyses were performed by changing the covariates included in the PS estimation model (PS1–5), changing the matching method (PS5-nearest), and adding covariates in the multivariable logistic regression model of analyzing the matching data (MLR-therapeutics and laboratory data). The covariates included in each PS estimation model are as follows; PS5 included variables corresponding to the regdanvimab administration criteria of European Medicines Agency and gender according to clinical judgment (age, sex, BMI, cardiovascular disease, chronic lung disease, diabetes mellitus, hypertension, chronic kidney disease, chronic liver diseases, and pneumonia); PS1 included all measured covariates (age, sex, BMI, cardiovascular disease, chronic lung disease, diabetes mellitus, hypertension, chronic kidney disease, chronic liver diseases, pneumonia, ACEIs/ARBs, statins, aspirin, and immunomodulators); PS2 included variables that were statistically significant for both exposure and outcome, and significant for outcome (age, cardiovascular disease, hypertension, chronic kidney disease, and pneumonia); For PS3, variables corresponding to the Korean regdanvimab administration criteria were included according to clinical judgment (age, cardiovascular disease, chronic lung disease, diabetes mellitus, hypertension, and pneumonia); PS4 included variables of PS3 and what significant for outcome (age, cardiovascular disease, chronic lung disease, diabetes mellitus, hypertension, chronic kidney disease, and pneumonia). PS5-nearest was the result of performing nearest matching by designating a caliper, which was 0.094 (0.2 of the standard deviation of the logit of the PS). MLR-therapeutics was the result of adding other treatment exposures (azithromycin, corticosteroids, hydroxychloroquine, lopinavir/ritonavir, and remdesivir), and MLR-laboratory data was that of adding the baseline laboratory data (C-reactive protein, lactate dehydrogenase, D-dimer, troponin I, ferritin, and creatine kinase).
OR = odds ratio, CI = confidence interval, PS = propensity score, MLR = multivariable logistic regression, BMI = body mass index, ACEI = angiotensin-converting enzyme inhibitor, ARB = angiotensin-receptor blocker.
Variables of significance (***P < 0.001).
DISCUSSION
This retrospective analysis evaluated the effects and safety of regdanvimab in a PS-matched cohort of patients with mild-to-moderate COVID-19. Regdanvimab reduced disease aggravation by ≤ 77% in the PS-matched cohort compared with conventional treatment (RRR, 76.5%; P < 0.001), without increasing adverse outcomes, and this effect was also evident in the result of multivariate model considering other influencing factors (OR, 0.169; 95% CI, 0.095, 0.289; P < 0.001). The results were consistent across analytical or matching methods, and disease aggravation in the overall cohort was consistently reduced. In terms of mortality, none of the patients died in the PS-matched cohort, but in the overall cohort, 17 (3.3%) of 520 without regdanvimab treatment died compared with none in the regdanvimab group (Supplementary Table 3).
The results from part one of a phase 2/3 randomized clinical trial of patients with mild-to-moderate COVID-19 found that regdanvimab 40 mg/kg reduced the need for hospitalization or oxygen therapy by > 50% compared with placebo a (4.0% vs. 8.7%). It was more effective in patients with moderate COVID-19 (6.5% vs. 15.8%) and even more effective in moderate COVID-19 aged ≥ 50 years (7.5% vs. 23.7%).18 Although the results of the phase 3 clinical trial of regdanvimab have not yet been published, press releases state that it reduces the incidence of hospitalization or death by 72% among high-risk patients and by 70% in all patients.35,36 Here, we presumed that the regdanvimab effect on preventing the disease aggravation was somewhat greater because we targeted patients with high-risk mild or moderate COVID-19 who were indicated for regdanvimab.
The present results are comparable to those of other studies of neutralizing mAbs. Although some administration protocols differed, the results of the phase 3 BLAZE-1 study showed that bamlanivimab 700 mg and etesevimab 1,400 mg reduced COVID-19 related hospitalization or death by 87% compared with a placebo (0.8% vs. 6%, P < 0.001).37,38 Moreover, four patients given a placebo died, whereas no-one given bamlanivimab and etesevimab died (P = 0.010).37,38 The number of medically attended visits was reduced by 49% by neutralizing antibody mixture comprising 1,200 mg each of casirivimab and imdevimab compared with a placebo in all study subjects,39 and by 67% in a post-hoc analysis of high-risk patients.40,41 Sotrovimab, a single agent neutralizing mAb, was approved for EUA by FDA in May 2021.42 According to the unpublished interim results from phase 1/2/3 COMET-ICE study, a single dose of 500 mg of sotrovimab reduced the rate of hospitalization or death by day 29 by about 79% compared with a placebo in adult patients with mild or moderate COVID-19 with risk factors.43 In Korea, until recently, all confirmed COVID-19 patients were hospitalized regardless of severity. Therefore, in this study, death or disease aggravation was defined as a composite primary outcome instead of hospitalization or death as used in other studies. In other studies, hospitalization was defined as a case of hospitalization for more than 24 hours due to acute treatment or requiring oxygen therapy or mechanical ventilation, so it could be considered as similar outcome.
Fewer adverse reactions occurred in the group with, than without regdanvimab, which is presumably because more alternative therapeutic agents were administered to the latter group. Moreover, although not included in this paper, in the sensitivity analysis results that included alternative therapeutics administered before severe transition as covariates in the multivariate model, none of these (azithromycin, corticosteroids, lopinavir/ritonavir) had a significant effect on the composite outcome of death, or disease aggravation. None of the alternative therapeutics have been proven to be effective in treating mild-to-moderate COVID-19, but in the absence of established therapeutics, it may have been an unavoidable choice for treating patients. However, it should be noted that the use of these drugs increases the side effects without increasing the effectiveness.
This study has some limitations. We reduced bias in the observational studies using PS-matched and multivariable logistic regression analyses, but the possibility that unmeasured confounding factors might remain cannot be ruled out. Other factors that might affect outcomes, such as insurance type and income level, were not included. The entire cost of COVID-19 treatment is covered by the Korean government, so insurance type or income level was not considered as an influencing factor in the present study. However, these should be considered an important factor in other countries. Vaccination was not included in the investigation because no breakthrough infection occurred after vaccination among our study participants. In addition, since only a few mutant virus infections were confirmed, this study did not consider them as influencing factors and did not include them. However, breakthrough infection is also likely to increase as rates of vaccination and mutant virus infection increase, so these might also become important factors affecting treatment outcomes. The secondary outcomes were somewhat ambiguous. In terms of hospitalization, since BMC manages non-critical COVID-19 patients and some patients suffering from deterioration involve in transfer to a tertiary hospital rather than stay, the length of the hospital stay in BMC might partly reflect deterioration of the patient’s clinical status. In addition, discharge was delayed for some patients due to reasons unrelated to the progress of COVID-19, such as those who were guardians of pediatric patients or had unrelated comorbidities. Therefore, the length of the hospital stay might be difficult to equate with the clinical status of patients. Unlike other countries, patients diagnosed with COVID-19 have been mostly hospitalized regardless of severity in Korea. Therefore, the meaning of hospitalization or length of the hospital stay may differ from that in other countries. The adverse reactions of fever or systemic pain, injection site inflammation, hypersensitivity, and gastrointestinal toxicity were retrospectively identified based on EMRs; thus, minor symptoms might have been omitted or not closely followed up. Other adverse events identified based on laboratory data only included those during hospitalization, and not for longer periods.
Despite these limitations, the present findings have several important implications. Regdanvimab is the only neutralizing mAb against SARS-CoV-2 available in Korea, and it has shown significant clinical effectiveness as a single agent. However, the results of the phase 3 clinical trials await publication, and sufficient evidence for its routine clinical application is lacking. We hope that the real-world evidence provided herein, along with the results of the phase 3 clinical trials, will serve as a basis for effectively treating COVID-19. Controlling the transition to severe disease will prevent the collapse of medical systems in a pandemic situation where large number of patients are affected, and will also have important economic implications. The use of therapeutics cannot be overlooked, as COVID-19 continues to thrive despite vaccination.
Studies on the therapeutic effects of neutralizing antibodies, including regdanvimab, on mutated variants are currently in progress.44,45,46 Further studies of the regdanvimab effectiveness in actual clinical practice are needed on breakthrough or mutant virus infection.
In conclusion, regdanvimab was significantly associated with lower odds of disease aggravation in 754 PS-matched patients at a 1:1 ratio who were administered with regdanvimab or not (n = 377 each; OR, 0.169; 95% CI, 0.095, 0.289; P < 0.001) without increasing adverse reactions.
ACKNOWLEDGMENTS
According to the national COVID-19 response policy, and under the management of the Korea Disease Control and Prevention Agency (KDCA), Celltrion (Incheon, Korea) supplied Regkirona® Inj. (regdanvimab 960 mg/16 mL vial) free of charge to this hospital designated for COVID-19 treatment. This study did not receive research funding, and the results are not associated with Celltrion.
Appendix 1
Propensity score (PS) matching
Factors collected in this study that were likely to affect treatment assignment or outcome were age, sex, body mass index (BMI), cardiovascular disease, chronic lung disease, diabetes mellitus, hypertension, chronic kidney disease, chronic liver diseases, pneumonia, angiotensin-converting enzyme inhibitors (ACEIs)/angiotensin receptor blockers (ARBs), statins, aspirin, and immunomodulators. Among them, to select variables to be included in the PS estimation model, we used both statistical method and clinical judgment, and gave priority to clinical judgment over statistical significance. As a statistical method, differences between groups were compared for each factor and treatment assignment or outcome, and it was judged to be significant if P < 0.05. As a result of the analysis, age, BMI, cardiovascular disease, chronic lung disease, and pneumonia were significantly different for treatment assignment, and age, cardiovascular disease, hypertension, chronic kidney disease, and pneumonia were significantly different for outcome. Factors that showed significant differences in both treatment assignment and outcome were age, cardiovascular disease, and pneumonia. In clinical judgment, all variables corresponding to the regdanvimab administration criteria, which were assumed to be related to both treatment assignment and outcome, were included, and this was extended to include not only Korean administration criteria at that time but also that of the European Medicines Agency (EMA). In addition, sex was also added based on the results of recent studies. Since covariates included in the PS estimation model should not be affected by treatment assignment and should be measured before assignment, the agents administered for the coronavirus disease 2019 (COVID-19) treatment after hospitalization were excluded.
Accordingly, the modeling of the PS estimation was performed using the following variable selection methods.
∘ All covariates collected (PS1): age, sex, BMI, cardiovascular disease, chronic lung disease, diabetes mellitus, hypertension, chronic kidney disease, chronic liver diseases, pneumonia, ACEIs/ARBs, statins, aspirin, immunomodulators
∘ Variables that were statistically significant for both treatment assignment and outcome, and significant for outcome (PS2): age, cardiovascular disease, hypertension, chronic kidney disease, pneumonia
∘ Variables corresponding to Korean regdanvimab administration criteria according to clinical judgment (PS3): age, cardiovascular disease, chronic lung disease, diabetes mellitus, hypertension, pneumonia
∘ Variables corresponding to Korean regdanvimab administration criteria according to clinical judgment, and variables that were statistically significant in the outcome (PS4): age, cardiovascular disease, chronic lung disease, diabetes mellitus, hypertension, chronic kidney disease, pneumonia
∘ Based on clinical judgment, the variables corresponding to EMA’s regdanvimab administration criteria, and sex (PS5): age, sex, BMI, cardiovascular disease, chronic lung disease, diabetes mellitus, hypertension, chronic kidney disease, chronic liver diseases, pneumonia
For each variable selection method, multivariable logistic regression analysis was performed to estimate the PS, and matching was performed using the calculated PS. To check the balance after matching, standardized mean difference (SMD) was used. If the absolute value of SMD > 0.1, it means that there is an imbalance of the covariate between the two groups.
As a result of 1:1 optimal matching, the absolute SMD of age exceeded 0.1 only in PS1, and the absolute SMD values of all covariates were within 0.1 in other matching cohorts. So, we selected PS5, which is a balanced model for all covariates while including as many variables as possible according to clinical judgment, and then additionally performed 1:1 nearest matching with calipers. The caliper was designated as 0.2 times the standard deviation of the logit of the PS as it was known to be suitable for estimating the treatment effect. In the result of caliper-designated nearest matching, the absolute SMD values further decreased, but 25 patients in the treatment group were excluded and only 352 pairs of matching data were derived. In order to rule out the possibility that patients with a specific tendency were excluded, we selected the optimal matching result with sufficient balance without omission of patients in the treatment group as the final matching cohort. In addition, sensitivity analysis was performed for PS1-4 and PS5-nearest.
Among the baseline laboratory data, C-reactive protein, lactate dehydrogenase, D-dimer, troponin I, ferritin, and creatine kinase have not been clearly proven as prognostic factors for COVID-19, but have been reported to be significantly elevated in severe COVID-19 patients. Matching variables should have no missing values, and since many of the study subjects were missing these values, the laboratory data were excluded from the matching variables. However, these laboratory data may have influenced the outcome, so we added them as covariates in the sensitivity analysis. Similarly, azithromycin, corticosteroids, hydroxychloroquine, lopinavir/ritonavir, and remdesivir administered for the purpose of treating COVID-19 after hospitalization may have affected the outcome, so these were also added as covariates in the sensitivity analysis.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Park S, Je NK, Heo J.
- Data curation: Kim DW, Park M, Heo J.
- Formal analysis: Park S, Je NK.
- Visualization: Park S.
- Writing - original draft: Park S.
- Writing - review & editing: Park S, Je NK, Kim DW, Park M, Heo J.
SUPPLEMENTARY MATERIALS
Missing baseline laboratory data in propensity score-matched cohort
Associations between regdanvimab and primary endpoint in PS-matched and overall cohorts
Clinical outcomes in overall cohort
Distribution of covariates before and after propensity matching study patients who were and were not treated with regdanvimab.
Standardized mean differences in unadjusted and adjusted cohorts.
References
- 1.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Director-general's remarks at the media briefing on 2019-nCoV on 11 February 2020. [Updated 2020]. [Accessed November 1, 2021]. http://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 .
- 3.Our World in Data. Statistics and research coronavirus (COVID-19) vaccinations. [Updated 2021]. [Accessed November 1, 2021]. https://ourworldindata.org/covid-vaccinations .
- 4.World Health Organization. COVID-19 weekly epidemiological update. [Updated 2021]. [Accessed November 1, 2021]. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---26-october-2021 .
- 5.Johns Hopkins Coronavirus Resource Center. COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) [Updated 2021]. [Accessed November 1, 2021]. https://coronavirus.jhu.edu/map.html .
- 6.World Health Organization. Tracking SARS-CoV-2 variants. [Updated 2021]. [Accessed November 1, 2021]. https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/
- 7.Yi S, Kim JM, Choe YJ, Hong S, Choi S, Ahn SB, et al. SARS-CoV-2 delta variant breakthrough infection and onward secondary transmission in household. J Korean Med Sci. 2022;37(1):e12. doi: 10.3346/jkms.2022.37.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee JJ, Choe YJ, Jeong H, Kim M, Kim S, Yoo H, et al. Importation and transmission of SARS-CoV-2 B.1.1.529 (Omicron) variant of concern in Korea, November 2021. J Korean Med Sci. 2021;36(50):e346. doi: 10.3346/jkms.2021.36.e346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jia Z, Gong W. Will mutations in the spike protein of SARS-CoV-2 lead to the failure of COVID-19 vaccines? J Korean Med Sci. 2021;36(18):e124. doi: 10.3346/jkms.2021.36.e124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ryu BH, Hong SI, Lim SJ, Cho Y, Hwang C, Kang H, et al. Clinical features of adult COVID-19 patients without risk factors before and after the nationwide SARS-CoV-2 B.1.617.2 (Delta)-variant outbreak in Korea: experience from Gyeongsangnam-do. J Korean Med Sci. 2021;36(49):e341. doi: 10.3346/jkms.2021.36.e341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Therapeutics and COVID-19: living guideline. [Updated 2022]. [Accessed November 1, 2021]. https://www.who.int/publications/i/item/therapeutics-and-covid-19-living-guideline .
- 12.National Institutes of Health. COVID-19 treatment guidelines panel. Coronavirus disease 2019 (COVID-19) treatment guidelines. [Updated 2021]. [Accessed November 1, 2021]. https://www.covid19treatmentguidelines.nih.gov/ [PubMed]
- 13.Wang C, Li W, Drabek D, Okba NM, van Haperen R, Osterhaus AD, et al. A human monoclonal antibody blocking SARS-CoV-2 infection. Nat Commun. 2020;11(1):2251. doi: 10.1038/s41467-020-16256-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jahanshahlu L, Rezaei N. Monoclonal antibody as a potential anti-COVID-19. Biomed Pharmacother. 2020;129:110337. doi: 10.1016/j.biopha.2020.110337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saphire EO, Schendel SL, Gunn BM, Milligan JC, Alter G. Antibody-mediated protection against Ebola virus. Nat Immunol. 2018;19(11):1169–1178. doi: 10.1038/s41590-018-0233-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prabakaran P, Zhu Z, Xiao X, Biragyn A, Dimitrov AS, Broder CC, et al. Potent human monoclonal antibodies against SARS CoV, Nipah and Hendra viruses. Expert Opin Biol Ther. 2009;9(3):355–368. doi: 10.1517/14712590902763755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim C, Ryu DK, Lee J, Kim YI, Seo JM, Kim YG, et al. A therapeutic neutralizing antibody targeting receptor binding domain of SARS-CoV-2 spike protein. Nat Commun. 2021;12(1):288. doi: 10.1038/s41467-020-20602-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eom JS, Ison M, Streinu-Cercel A, Săndulescu O, Preotescu LL, Kim YS, et al. Efficacy and safety of CT-P59 plus standard of care: a phase 2/3 randomized, double-blind, placebo-controlled trial in outpatients with mild-to-moderate SARS-CoV-2 infection. Res Sq. doi: 10.21203/rs.3.rs-296518/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ministry of Food and Drug Safety. Approval of Regkirona® Inj., an antibody treatment for COVID-19. [Updated 2021]. [Accessed November 1, 2021]. https://www.mfds.go.kr/brd/m_99/view.do?seq=45029&srchFr=&srchTo=&srchWord=&srchTp=0&itm_seq_1=0&itm_seq_2=0&multi_itm_seq=0&company_cd=&company_nm=&Data_stts_gubun=C1009&page=2 .
- 20.Ministry of Food and Drug Safety. Pharmaceutical product information: Regkirona® Inj. 960 mg (regdanvimab) [Updated 2021]. [Accessed November 1, 2021]. https://nedrug.mfds.go.kr/pbp/CCBBB01/getItemDetail?itemSeq=202101124 .
- 21.European Medicines Agency. EMA issues advice on use of regdanvimab for treating COVID-19. [Updated 2021]. [Accessed November 1, 2021]. https://www.ema.europa.eu/en/news/ema-issues-advice-use-regdanvimab-treating-covid-19 .
- 22.Ministry of Food and Drug Safety. Official approval of Regkirona® Inj., an antibody treatment for COVID-19. [Updated 2021]. [Accessed November 1, 2021]. https://www.mfds.go.kr/brd/m_99/view.do?seq=45778&srchFr=&srchTo=&srchWord=&srchTp=0&itm_seq_1=0&itm_seq_2=0&multi_itm_seq=0&company_cd=&company_nm=&Data_stts_gubun=C1009&page=1 .
- 23.Kim SB, Ryoo S, Huh K, Joo EJ, Kim YJ, Choi WS, et al. Revised Korean Society of Infectious Diseases/National Evidence-based Healthcarea collaborating agency guidelines on the treatment of patients with COVID-19. Infect Chemother. 2021;53(1):166–219. doi: 10.3947/ic.2021.0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lam KW, Chow KW, Vo J, Hou W, Li H, Richman PS, et al. Continued in-hospital angiotensin-converting enzyme inhibitor and angiotensin ii receptor blocker use in hypertensive COVID-19 patients is associated with positive clinical outcome. J Infect Dis. 2020;222(8):1256–1264. doi: 10.1093/infdis/jiaa447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fosbøl EL, Butt JH, Østergaard L, Andersson C, Selmer C, Kragholm K, et al. Association of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use with COVID-19 diagnosis and mortality. JAMA. 2020;324(2):168–177. doi: 10.1001/jama.2020.11301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gupta A, Madhavan MV, Poterucha TJ, DeFilippis EM, Hennessey JA, Redfors B, et al. Association between antecedent statin use and decreased mortality in hospitalized patients with COVID-19. Nat Commun. 2021;12(1):1325. doi: 10.1038/s41467-021-21553-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Daniels LB, Sitapati AM, Zhang J, Zou J, Bui QM, Ren J, et al. Relation of statin use prior to admission to severity and recovery among COVID-19 inpatients. Am J Cardiol. 2020;136:149–155. doi: 10.1016/j.amjcard.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osborne TF, Veigulis ZP, Arreola DM, Mahajan SM, Röösli E, Curtin CM. Association of mortality and aspirin prescription for COVID-19 patients at the Veterans Health Administration. PLoS One. 2021;16(2):e0246825. doi: 10.1371/journal.pone.0246825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chow JH, Khanna AK, Kethireddy S, Yamane D, Levine A, Jackson AM, et al. Aspirin use is associated with decreased mechanical ventilation, intensive care unit admission, and in-hospital mortality in hospitalized patients with coronavirus disease 2019. Anesth Analg. 2021;132(4):930–941. doi: 10.1213/ANE.0000000000005292. [DOI] [PubMed] [Google Scholar]
- 30.Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146(1):110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pastor-Nieto M, Checa-Díaz P, González-Muñoz P, Martín-Fuentes A, Vergara-Sánchez A, Sánchez-Herreros C, et al. Prior treatment with immunosuppressants among COVID-19 inpatients at one hospital in Spain. J Eur Acad Dermatol Venereol. 2020;34(12):e760–e762. doi: 10.1111/jdv.16798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scully EP, Haverfield J, Ursin RL, Tannenbaum C, Klein SL. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat Rev Immunol. 2020;20(7):442–447. doi: 10.1038/s41577-020-0348-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R, Klein SL. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ. 2020;11(1):29. doi: 10.1186/s13293-020-00304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moon Hj, Kim K, Kang EK, Yang HJ, Lee E. Prediction of COVID-19-related mortality and 30-day and 60-day survival probabilities using a nomogram. J Korean Med Sci. 2021;36(35):e248. doi: 10.3346/jkms.2021.36.e248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Clinical Trials Arena. Celltrion's COVID-19 drug regdanvimab meets Phase III endpoints. [Updated 2021]. [Accessed November 1, 2021]. https://www.clinicaltrialsarena.com/news/celltrion-regdanvimab-phaseiii-data/
- 36.Monoclonal regdanvimab cuts COVID progression risk in placebo trial. IDWeek, September 29-October 3, 2021. [Updated 2021]. [Accessed November 1, 2021]. https://www.natap.org/2021/IDWeek/IDWeek_43.htm .
- 37.An EUA for bamlanivimab and etesevimab for COVID-19. Med Lett Drugs Ther. 2021;63(1621):49–50. [PubMed] [Google Scholar]
- 38.FDA. Fact sheet for health care providers. Emergency Use Authorization (EUA) of bamlanivimab and etesevimab. [Updated 2021]. [Accessed November 1, 2021]. https://bit.ly/3qfS6DN .
- 39.Weinreich DM, Sivapalasingam S, Norton T, Ali S, Gao H, Bhore R, et al. REGN-COV2, a neutralizing antibody cocktail, in outpatients with COVID-19. N Engl J Med. 2021;384(3):238–251. doi: 10.1056/NEJMoa2035002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.An EUA for casirivimab and imdevimab for COVID-19. Med Lett Drugs Ther. 2020;62(1614):201–202. [PubMed] [Google Scholar]
- 41.FDA. Fact sheet for health care providers. Emergency Use Authorization (EUA) of casirivimab and imdevimab. [Updated 2021]. [Accessed November 1, 2021]. http://e-lactancia.org/media/papers/casirivimabimdevimab-DS-FDA-Regeneron2020.pdf .
- 42.Orders M. An EUA for sotrovimab for treatment of COVID-19. Med Lett Drugs Ther. 2021;63(1627):97–xx98. [PubMed] [Google Scholar]
- 43.FDA. Fact sheet for health care providers. Emergency Use Authorization (EUA) of sotrovimab. [Updated 2021]. [Accessed November 1, 2021]. https://www.fda.gov/media/149534/download .
- 44.Hurt AC, Wheatley AK. Neutralizing antibody therapeutics for COVID-19. Viruses. 2021;13(4):628. doi: 10.3390/v13040628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baum A, Fulton BO, Wloga E, Copin R, Pascal KE, Russo V, et al. Antibody cocktail to SARS-CoV-2 spike protein prevents rapid mutational escape seen with individual antibodies. Science. 2020;369(6506):1014–1018. doi: 10.1126/science.abd0831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ryu DK, Song R, Kim M, Kim YI, Kim C, Kim JI, et al. Therapeutic effect of CT-P59 against SARS-CoV-2 South African variant. Biochem Biophys Res Commun. 2021;566:135–140. doi: 10.1016/j.bbrc.2021.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Missing baseline laboratory data in propensity score-matched cohort
Associations between regdanvimab and primary endpoint in PS-matched and overall cohorts
Clinical outcomes in overall cohort
Distribution of covariates before and after propensity matching study patients who were and were not treated with regdanvimab.
Standardized mean differences in unadjusted and adjusted cohorts.