Abstract
Background:
Femoroacetabular impingement (FAI) is a major cause of hip pain in young adults and athletes. Surgical treatment of FAI is recommended in cases of failed nonoperative treatment that have the typical clinical and radiographic findings. At present, the role of risk factors for revision surgery and progression to total hip arthroplasty (THA) in patients with FAI is still unclear.
Purpose:
To investigate the possible association between (1) rate of revision and progression to THA and (2) patient characteristics, type of lesion, family history of hip disease, type of intervention, radiographic parameters, physical examination, and pre- and postoperative scores.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
The present systematic review was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. In October 2020, the main online databases were accessed. All articles concerning surgical correction for selected patients with FAI were accessed. Patient characteristics, type of intervention, radiographic parameters, physical examination, and pre- and postoperative scores were assessed. The outcomes of interest were the possible association between these variables and the rate of revision and subsequent progression to THA using a multivariate analysis through the Pearson product-moment correlation coefficient.
Results:
Data from 99 studies (9357 procedures) were collected. The median follow-up was 30.9 months (interquartile range, 24.0-45.0). The mean ± SD age was 33.4 ± 9.3 years; mean body mass index (BMI), 24.8 ± 4.8; percentage right side, 55.8% ± 8.0%; and percentage female sex, 47.5% ± 20.4%. The overall rate of revision was 5.29% (351 of 6641 patients), while the rate of subsequent progression to THA was 3.78% (263 of 6966 patients). Labral debridement (P < .0001), preoperative acetabular index (P = .01), and BMI (P = .03) all showed evidence of a statistically positive association with increased rates of THA. No other statistically significant associations were found between patient characteristics, type of lesion, family history of hip disease, type of intervention, radiographic parameters, physical examination, or pre- and postoperative scores and the rate of revision and/or progression to THA.
Conclusion:
Although surgical procedures to treat FAI led to satisfactory outcomes, there was a revision rate of 5.29% in the 9357 procedures in the present systematic review. The rate of progression to THA after a median follow-up of 30 months was 3.78%. Patients who have a higher BMI and/or have a pathologic acetabular index and/or undergo labral debridement during correction of FAI are more at risk for a subsequent THA. We advocate additional education of this patient population in terms of expected outcomes and suggest surgical labral repair instead of debridement if needed.
Keywords: femoroacetabular impingement, revision surgery, total hip arthroplasty, risk factors
In patients with femoroacetabular impingement (FAI), anatomic abnormalities of the femoral head and/or the acetabulum produce pathologically high contact forces between the femur and the acetabulum. FAI can be a cause of activity limitation, decreased hip function, and significant hip pain, especially in young adults and athletes, because of cartilage and labral damage.38,39 These repetitive insults to the cartilage and labrum result in early hip degeneration and osteoarthritis 106 ; 79% of patients with osteoarthritis of the hip displayed subtle developmental changes on radiographs obtained before adulthood.38,48 FAI can be classified into 3 types depending on the origin of the pathology, being on the femur (cam), acetabulum (pincer), or both (mixed). In previous cross-sectional studies of 4151 individuals, 19.6% of men and 5.2% of women exhibited a pistol grip deformity of the proximal femur, which was defined by calculating the triangular index. 42 Surgery is indicated in symptomatic patients with clinical and radiographic findings of FAI whose nonoperative treatment has failed for a minimum of 3 months. 62 In these patients, surgical options include femoral osteochondroplasty to improve the femoral head-neck offset; debridement, repair, or reconstruction of the labrum; and/or removal of an excessive acetabular rim.31,66,79 Ganz et al 39 first described the technique of surgical hip dislocation for the treatment of FAI in 2003, and several studies have shown good clinical outcomes using this technique.5,91 Given the long operating and recovery time of open hip dislocation surgery, a mini-open anterior technique was developed by Clohisy and McClure, 20 who accessed the hip joint through a Hueter approach. Over the past few years, arthroscopic management of FAI has become popular, with a decrease in complications and faster recovery.60,83,97
All surgical interventions aim to improve patients’ activity levels, relieve hip pain, and restore natural hip function. The various surgical techniques for management of FAI are all successful (surgical hip dislocation, mini-open, arthroscopy), but data on rates of revision and progression to total hip arthroplasty (THA) are limited. So far, prognostic factors for surgical outcome for FAI are still unclear. Thus, the present systematic review investigated the risk factors for revision surgery and progression to THA in patients who underwent surgery for symptomatic FAI. A multivariate analysis was conducted to investigate the association between (1) rate of revision and progression to THA and (2) patient characteristics, type of lesion, type of intervention, radiographic parameters, physical examination, and pre- and postoperative scores.
Methods
Search Strategy
The present systematic review was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. 77 We followed the PICO protocol for the preliminary search:
P (problem): FAI
I (intervention): surgical correction
C (comparator): generalities, type of intervention, radiographic parameters, tests, scores
O (outcomes): revision rate and progression to THA
Literature Search
Two authors (F.M., A.B.) independently performed the literature search in October 2020, accessing the following databases with no time constraints: PubMed, Embase, Google Scholar, and Scopus. The following keywords were used in combination: hip, FAI, femoroacetabular impingement, arthroscopy, mini-open, open, surgery, dislocation, treatment, therapy, cam, pincer, mixed, labral, acetabulum, femur, pelvis, pain, debridement, repair, reconstruction, THA, complications, pain. The resulting titles and eventually the abstracts were screened by the 2 authors. The full text of the articles of interest was accessed. The references were also screened. Disagreements between the authors were solved by a third senior author (M.B.).
Eligibility Criteria
All the articles concerning surgical correction for patients with FAI were accessed. To be eligible for inclusion, articles had to report the rate of revision and/or progression to THA at last follow-up. Any kind of surgical intervention that did not involve THA was considered revision surgery. According to the authors language capabilities, articles in English, Italian, French, German, and Spanish were considered. Articles of level 1 to 4 according to the Oxford Centre of Evidenced-Based Medicine were considered. 55 Data from national registries were not considered. Reviews, letters, expert opinion, case reports, and editorials were not eligible. Animal, biomechanical, and cadaveric studies were also not considered. Articles regarding revision settings were not eligible. Studies with data based on combined treatments, as well as those focusing on rehabilitation protocols, were excluded. Studies including adjuvants or innovative surgical procedures were excluded. The studies were included regardless of the surgical exposure (arthroscopic, mini-open, open). Studies treating skeletally immature patients were included, as were those describing outcomes in patients who were obese. Studies with data on patients >60 years old or with clear evidence of advanced hip degeneration (Tönnis grade III) were not included. Case series of <10 patients were also excluded. Only studies reporting quantitative data under the outcomes of interest were analyzed.
Data Extraction
Data extraction was performed by 2 authors (F.M., A.B.). Data from the following endpoints were collected:
Generalities: author and publication year, journal, type of study, follow-up duration, number of patients and procedures, mean age, body mass index (BMI), sex, side of surgery, return to sport
Type of intervention: labral debridement, labral repair, labral reconstruction
Radiographic parameters: femoral offset (millimeters), acetabular inclination (Tönnis angle), α-angle (anteroposterior, groin-lateral), β-angle, sharp angle, center-edge angle, anterior center-edge angle, lateral center-edge angle, acetabular index, Tönnis grade, caudocranial femoral coverage (percentage), anterior coverage (percentage), posterior coverage (percentage), crossover sign, and joint space (medial, foveal, lateral)
Physical examination: range of motion (flexion, extension, abduction, adduction, internal and external); anterior, lateral, and posterior impingement test (percentage positive)
Pre- and postoperative scores: Harris Hip Score, modified Harris Hip Score, Non-arthritic Hip Score, 12-Item Short Form Health Survey (SF-12; physical and mental subscales), Hip Outcome Score (activities of daily living and sport-specific subscales), International Hip Outcome Tool–12 and −33, and visual analog scale
The present work investigated whether the aforementioned endpoints were associated with the rate of revision and subsequent progression to THA. Thus, every endpoint was independently analyzed, and its association with revision and progression to THA was assessed.
Methodological Quality Assessment
The methodological quality assessment was made through the Coleman Methodology Score (CMS). 23 The CMS analyzes studies under several items: number of patients, follow-up, type of surgical approach, and study design, as well as descriptions of diagnosis, surgical technique, and postoperative rehabilitation. Furthermore, outcome criteria, the procedure of assessing outcomes, and a description of the sample selection process are evaluated. The quality is scored from 0% (poor) to 100% (excellent), with values >60% considered satisfactory.
Statistical Analysis
The statistical analyses were performed by the main author (F.M.). For the analytical statistics, STATA software (Version 16; StataCorp) was used. The Shapiro-Wilk test was performed to investigate data distribution. For normal data, mean and standard deviation were calculated. For nonparametric data, median and interquartile range were calculated. Multiple pairwise correlations using the Pearson product-moment correlation coefficient (r) were performed to investigate the association between the endpoints were accomplished. According to the Cauchy-Schwarz inequality, the final effect ranks between +1 (positive linear correlation) and −1 (negative linear correlation). Values of 0.1 < | r | < 0.3 and 0.3 < | r | < 0.5 and | r | > 0.5 were considered to have poor, moderate, and strong correlation, respectively. Possible associations with the outcomes of interest were evaluated for each endpoint. Overall significance was evaluated using the χ2 test. A linear regression of the statistically significant correlations was made, and added-variable plots were displayed. Values of P > .05 were considered statistically significant.
Results
Search Results
The literature search resulted in 1174 articles. Initially, 509 articles were excluded because of duplication; 529 articles were then excluded because of the following: type of study (n = 187), nonoperative techniques (n = 91), combined treatments (n = 47), adjuvants and/ or innovative surgeries (n = 41), language limitations (n = 22), uncertain data (n = 7), or other (n = 134). A further 37 articles were excluded because they did not match the topic of interest or report quantitative data under the outcomes of interest. Finally, 99 articles were included for analysis: 3 randomized clinical trials, 36 prospective studies, and 60 retrospective studies. The literature flowchart is shown in Figure 1.
Figure 1.
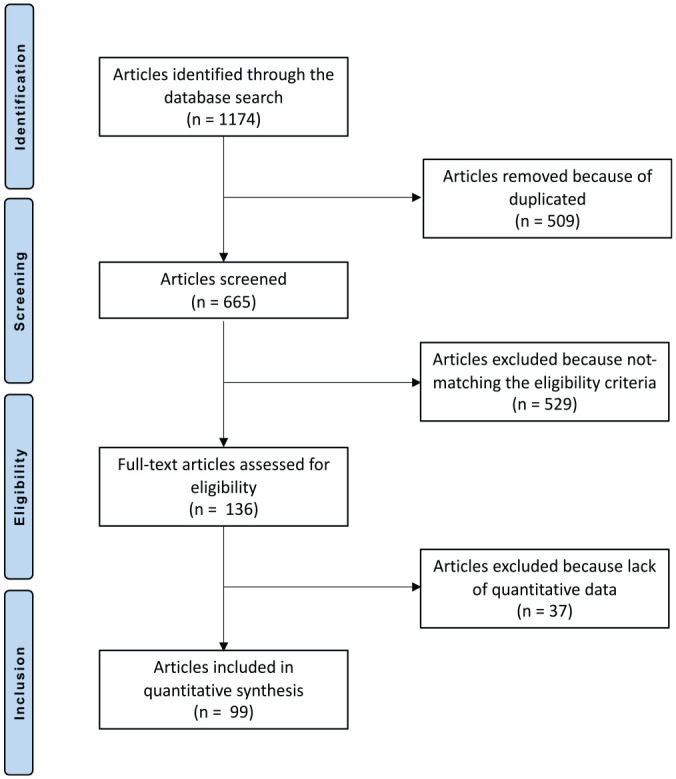
Flowchart of the literature search.
Methodological Quality Assessment
The CMS evidenced the overall limited quality of the studies. Indeed, 60% of studies were retrospective, 36% prospective, and only 3% were randomized trials. Eligibility criteria and rehabilitation protocols were frequently not indicated. General health measures were rarely cited. The procedure of assessing outcomes was often biased or not clearly described. The study size and mean follow-up were well-reported in most studies. The descriptions of diagnoses and surgical techniques were also commonly well-described. The overall CMS was 64.7 points (range, 40-85), attesting to the acceptable quality of the methodological assessment of the present study (Table 1).
Table 1.
Generalities of the Included Studies and Demographic Baseline of the Patients a
| First Author | Year | Journal | Study Design | CMS | Treatment | Mean Follow-up, mo | Procedures, No. | Mean Age, y | Female, % |
|---|---|---|---|---|---|---|---|---|---|
| Anwander 1 | 2017 | Clin Orthop Rel Res | Retrospective | 68 | Open | Resection, 156.0; reattachment, 144.0 | 60 (resection, 25; reattachment, 35) | Resection, 29; reattachment, 29 | Resection, 24; reattachment, 37 |
| Bardakos 2 | 2008 | J Bone Joint Surg Br | Retrospective | 61 | Arthroscopy | 12.0 | 71 | 34.3 | 47.9 |
| Beaulé 3 | 2007 | J Bone Joint Surg Am | Retrospective | 54 | Open | 37.2 | 37 | 40.5 | |
| Beck 4 | 2011 | J Bone Joint Surg Am | Retrospective | 53 | Open | 12.0 | 50 | 32.0 | 44.0 |
| Beck 5 | 2004 | Clin Orthop Rel Res | Retrospective | 40 | Open | 56.4 | 19 | 36.0 | |
| Bedi 6 | 2011 | Am J Sports Med | Prospective | 53 | Arthroscopy | 10.9 | 10 | 25.9 | |
| Bellotti 7 | 2016 | Hip Int | Retrospective | 53 | Mini-open | 104.4 | 296 | ||
| Boone 8 | 2012 | HSS J | Retrospective | 70 | Open | 46.8 | 22 | 44.0 | 31.8 |
| Botser 9 | 2014 | Am J Orthop | Prospective | 72 | Arthroscopy | 14.3 | 18 | 20.1 | 100.0 |
| Open | 16.2 | 5 | 18.1 | ||||||
| Bryan 10 | 2016 | Am J Sports Med | Prospective | 82 | Arthroscopy | Younger, 51.6; older, 46.8 | 201 | Younger, 37; older, 60 | 68.7 |
| Büchler 11 | 2013 | Arthroscopy | Retrospective | 61 | Arthroscopy | 15.0 | 66 | 33.8; | 74.2 |
| Open | 17.5 | 135 | 31.2 | 32.6 | |||||
| Byrd 12 | 2009 | Clin Orthop Relat Res | Prospective | 79 | Arthroscopy | 16.0 | 207 | 33.0 | 31.0 |
| Byrd 13 | 2011 | Am J Sports Med | Prospective | 76 | Arthroscopy | 19.0 | 200 | 28.6 | 26.0 |
| Byrd 15 | 2009 | Arthroscopy | Prospective | 70 | Arthroscopy | 120.0 | 26 | 46.0 | 50.0 |
| Byrd 16 | 2016 | Arthroscopy | Retrospective | 70 | Arthroscopy | 30.0 | 244 (122, study; 122, control) | Study, 15.9; control: 36.8 | Study, 53.3; control, 41.8 |
| Camenzind 17 | 2015 | J Hip Pres Surg | Retrospective | 66 | Open | Reconstruction: 38.0; control: 42.0 | 27 (reconstruction, 13; control, 14) | Reconstruction, 36; control, 25 | Reconstruction, 38.5; control 21.4 |
| Chaudhary 18 | 2015 | Indian J Orthop | Retrospective | 61 | Open | 24.8 | 16 | 28.3 | 31.3 |
| Cho 19 | 2015 | Hip Pelvis | Retrospective | 57 | Open / mini-open | >24 | 13 | 45.0 | 53.8 |
| Cohen 22 | 2012 | Am J Sports Med | Retrospective | 59 | Mini-open | 22 | 66 | 32.0 | 31.8 |
| Comba 25 | 2016 | Muscles Ligaments Tendons J | Prospective | 72 | Arthroscopy | 91.0 | 42 | 38.0 | 37.7 |
| Degen 26 | 2017 | Arthroscopy | Retrospective | 66 | Arthroscopy | Study, 36.1; control, 34.1 | 346 (study, 38; control, 306) | Study, 16; control, 31 | Study, 47; control, 46.3 |
| Domb 27 | 2017 | Am J Sports Med | Retrospective | 68 | Arthroscopy | Tönnis 0, 70.0; Tönnis 1, 72.6 | 124 (Tönnis 0, 62; Tönnis 1, 62) | Tönnis 0, 41.9; Tönnis 1, 42.3 | 59.7 |
| Domb 28 | 2014 | Am J Sports Med | Retrospective | 66 | Arthroscopy | Reconstruction, 26.4; resection, 30.0 | 33 (11, reconstruction; 22, resection) | Reconstruction, 33.0; resection, 38.8 | Reconstruction, 36.4; resection, 36.4 |
| Domb 29 | 2015 | Arthroscopy | Prospective | 77 | Arthroscopy | Study, 32.8; control, 33.1 | 104 (study, 52; control, 52) | Study, 54.8; control, 20.3 | 65.4 |
| Domb 30 | 2013 | Arthroscopy | Prospective | 68 | Open | 24.8 | 10 | 19.0 | 80.0 |
| Arthroscopy | 25.5 | 20 | 19.6 | 80.0 | |||||
| Espinosa 31 | 2006 | J Bone Joint Surg Am | Retrospective | 61 | Open | 24.0 | 60 | 30.0 | 36.5 |
| Ezechielia 32 | 2016 | Technol Health Care | Prospective | 63 | Mini-open | 15.0 | 72 (group A, 56; group B, 15) | Group A, 32.1; group B, 28.5 | 47.2 |
| Fabricant 33 | 2015 | J Bone Joint Surg Am | Retrospective | 67 | Arthroscopy | 21.0 | 37 | 28.0 | 41.0 |
| 149 | 30.0 | 50.0 | |||||||
| 57 | 29.0 | 58.0 | |||||||
| Flores 34 | 2018 | Orthop J Sports Med | Prospective | 72 | Arthroscopy | Early, 15.5; late, 13.1 | 60 (early, 30; late, 30) | Early, 37.2; late, 35.3 | Early, 50.0; late, 43.3 |
| Frank 35 | 2014 | Am J Sports Med | Retrospective | 64 | Arthroscopy | 29.9 | 64 (partial capsular closure, 32; complete capsular closure, 32) | 32.8 | 62.5 |
| Fukui 36 | 2015 | Arthroscopy | Retrospective | 75 | Arthroscopy | 40.0 | 102 | 35.0 | 50.0 |
| Fukui 37 | 2015 | Bone Joint J | Retrospective | 64 | Arthroscopy | 42.0 | 28 | 34.0 | 42.9 |
| Gedouin 40 | 2010 | Orthop Traum Surg Res | Retrospective | 58 | Arthroscopy | 15.6 | 38 | 36.0 | 13.2 |
| Gicquel 41 | 2014 | Orthop Traum Surg Res | Prospective | 64 | Arthroscopy | 55.2 | 53 | 31.0 | 62.7 |
| Gupta 44 | 2016 | Am J Sports Med | Prospective | 77 | Arthroscopy | 28.9 | 595 | 38.04 | 61.7 |
| Gupta 45 | 2014 | Am J Sports Med | Prospective | 71 | Arthroscopy | 28.3 | 47 | 37.18 | 40.4 |
| Haefeli 46 | 2017 | Clin Orthop Relat Res | Retrospective | 72 | Arthroscopy | 84.0 | 52 | 35.0 | 89.0 |
| Hartigan 49 | 2017 | J Hip Pres Surg | Retrospective | 64 | Arthroscopy | 42.0 | 69 | 43.6 | 36.9 |
| Hartmann 50 | 2009 | Arch Orthop Trauma Surg | Retrospective | 56 | Arthroscopy | 15.0 | 34 | 31.1 | 48.5 |
| Hatakeyama 51 | 2018 | Am J Sports Med | Retrospective | 69 | Arthroscopy | 42.5 | 45 | Success, 20; failure, 47 | Success, 59; failure, 91 |
| Honda 52 | 2020 | Knee Surg Sports Traumatol Arthrosc | Retrospective | 66 | Arthroscopy | Young, 31.8; middle, 30.9 | 84 | Younger, 30.9; middle, 56.7 | Young, 46; middle, 67 |
| Horisberger 53 | 2010 | Arthroscopy | Prospective | 56 | Arthroscopy | 36.0 | 20 | 47.3 | 20.0 |
| Horisberger 54 | 2010 | Clin Orthop Relat Res | Prospective | 69 | Arthroscopy | 27.6 | 105 | 40.9 | 30.5 |
| Hufeland 56 | 2016 | Arch Orthop Trauma Surg | Retrospective | 64 | Arthroscopy | 66.3 | 44 | 34.3 | 45.5 |
| Ilizaliturri 57 | 2007 | J Bone Joint Surg Br | Prospective | 61 | Arthroscopy | 30.0 | 14 | 30.6 | 53.8 |
| Ilizaliturri 58 | 2008 | J Arthroplasty | Prospective | 60 | Arthroscopy | 24.0 | 19 | 34.0 | 42.1 |
| Krych 61 | 2013 | Arthroscopy | Prospective, Randomized | 76 | Arthroscopy | 32.0 | 36 | Repair, 38; debridement, 39 | 100.0 |
| LaFrance 63 | 2015 | J Hip Pres Surg | Prospective | 71 | Arthroscopy | PRP, 18.5; control, 23.3 | 35 | PRP, 34.4; control, 34.9 | |
| Larson 64 | 2009 | Arthroscopy | Retrospective | 63 | Arthroscopy | Group 1, 21.4; group 2, 16.5 | 71 (group 1, 36; group 2, 39) | Group 1, 31; group 2, 27 | Group 1, 26.5; group 2, 37.8 |
| Larson 65 | 2012 | Am J Sports Med | Prospective | 79 | Arthroscopy | 42.0 | 94 | Group 1, 32; group 2, 28 | Group 1, 38.6; group 2, 42 |
| Levy 67 | 2017 | Am J Sports Med | Retrospective | 49 | Arthroscopy | 31.2 | 84 (atypical, 28; typical, 56) | Atypical 35.8; typical 35.2 | Atypical 64; typical 64 |
| Levy 68 | 2017 | Am J Sports Med | Retrospective | 67 | Arthroscopy | 24.0 | 51 | 26.3 | 56.7 |
| Maldonado 69 | 2018 | Am J Sports Med | Retrospective | 65 | Arthroscopy | IFL, 42.5; control, 43.9 | 743 (IFL, 351; control, 392) | IFL, 27.8; control, 34.1 | IFL, 82.3; control, 70.7 |
| Maldonado 70 | 2019 | Arthroscopy | Retrospective | 57 | Arthroscopy | CLT, 59.7; control, 51.4 | 72 (CLT, 18; control, 54) | CLT, 41.2; control, 41.1 | 50.0 |
| Mardones 72 | 2016 | Muscles Ligaments Tendons J | Retrospective | 61 | Arthroscopy | 48.0 | 17 | 33.5 | 73.3 |
| Matsuda 73 | 2015 | J Hip Pres Surg | Prospective | 69 | Arthroscopy | >24 | 145 (focal, 127; global, 18) | Focal, 39.8; global, 37.2 | Focal 52; global, 33 |
| McConkey 74 | 2019 | J Pediatr Orthop | Prospective | 60 | Arthroscopy | 24.0 | 36 (bilateral, 24; unilateral, 12) | Bilateral, 15.7; unilateral, 16.5 | Bilateral, 58.3; unilateral, 58.3 |
| Mohan 76 | 2017 | Arthroscopy | Retrospective | 69 | Arthroscopy | 34.0 | 57 | 17.8 | 66.0 |
| Moriya 78 | 2017 | J Orthop Surg Res | Retrospective | 61 | Arthroscopy | 28.0 | 23 | 59.3 | 73.9 |
| Murphy 79 | 2004 | Clin Orthop Relat Res | Prospective | 71 | Open | 62.4 | 23 | 35.4 | 43.5 |
| Naal 80 | 2012 | Am J Sports Med | Retrospective | 68 | Open | 60.7 | 233 | 30.0 | 40.0 |
| Naal 81 | 2011 | Am J Sports Med | Retrospective | 59 | Open | 45.1 | 30 | 19.7 | 0.0 |
| Nawabi 82 | 2016 | Am J Sports Med | Prospective | 62 | Arthroscopy | 31.3 | 207 (BD, 55; control, 152) | BD, 29.8; control, 29.6 | BD, 47.8; control, 55.7 |
| Nho 83 | 2011 | Am J Sports Med | Retrospective | 61 | Arthroscopy | 27.0 | 47 | 22.8 | 28.0 |
| Nielsen 84 | 2014 | BMC Musc Dis | Prospective | 72 | Arthroscopy | >24 | 117 | 37.0 | 59.0 |
| Novais 85 | 2014 | J Pediatr Orthop | Retrospective | 41 | Open | 21.6 | 29 | 17.0 | 31.0 |
| Palmer 87 | 2012 | Arthroscopy | Retrospective | 72 | Arthroscopy | 46.0 | 185 | 40.2 | 50.7 |
| Perets 88 | 2017 | Arthroscopy | Prospective | 67 | Arthroscopy | 35.7 | 11 | 14.7 | 100.0 |
| Perets 89 | 2018 | Arthroscopy | Retrospective | 62 | Arthroscopy | 49.1 | 60 | 19.5 | 80.0 |
| Perets 90 | 2018 | J Bone Joint Surg Am | Retrospective | 68 | Arthroscopy | Obese, 71.6; control, 71.3 | 148 (obese, 74; control, 74) | 44.2 | Obese, 60.8; control, 60.8 |
| Peters 91 | 2006 | J Bone Joint Surg Am | Prospective | 60 | Open | 32.0 | 30 | 31.0 | 44.8 |
| Peters 92 | 2010 | Clin Orthop Relat Res | Retrospective | 58 | Open | 26.0 | 96 | 28.0 | 41.5 |
| Philippon 93 | 2009 | J Bone Joint Surg Br | Prospective | 71 | Arthroscopy | 27.6 | 112 | 40.6 | 55.4 |
| Philippon 94 | 2012 | Arthroscopy | Retrospective | 64 | Arthroscopy | 36.0 | 60 | 15.0 | 69.0 |
| Philippon 95 | 2007 | Knee Surg Sports Traumatol Arthrosc | Retrospective | 65 | Arthroscopy | 19.2 | 45 | 31.0 | 6.7 |
| Philippon 96 | 2012 | Arthroscopy | Retrospective | 60 | Arthroscopy | 37.5 | 153 | 57.0 | 52.9 |
| Philippon 98 | 2010 | Am J Sports Med | Retrospective | 62 | Arthroscopy | 24.0 | 28 | 27.0 | 0.0 |
| Polesello 99 | 2014 | Hip Int | Retrospective | 62 | Arthroscopy | 73.2 | 26 | 34.6 | 12.5 |
| Polesello 100 | 2009 | Rev Bras Ortop | Retrospective | 48 | Arthroscopy | 27.0 | 28 | 34.0 | 33.0 |
| Rafols 101 | 2015 | Arthroscopy | Prospective, Randomized | 84 | Arthroscopy | 24.0 | 57 | Group 1, 34.2; group 2, 36.5 | 47.4 |
| Rego 102 | 2018 | Int Orthop | Retrospective | 62 | Arthroscopy | 44.0 | 102 | 34.0 | 47.0 |
| Open | 76.0 | 96 | 31.0 | 40.0 | |||||
| Rhee 103 | 2016 | Arch Orthop Trauma Surg | Prospective, Randomized | 85 | Arthroscopy | Group A, 32.3; group B, 31.8 | 37 (group A, 19; group B, 18) | Group A, 33.8; group B, 34.6 | 59.5 |
| Roos 104 | 2017 | Rev Bras Ortop | Retrospective | 60 | Arthroscopy | 29.1 | 41 | 36.1 | 13.0 |
| Open | 52.0 | 17 | 35.8 | 31.3 | |||||
| Sanders 105 | 2017 | Knee Surg Sports Traumatol Arthrosc | Retrospective | 65 | Arthroscopy | 30.0 | 46 | 42.4 | 67.4 |
| Sansone 107 | 2015 | Orthop J Sports Med | Retrospective | 72 | Arthroscopy | 12.3 | 115 | 25.0 | 18.0 |
| Sansone 108 | 2017 | Sc J Med Sci Sports | Prospective | 77 | Arthroscopy | 25.4 | 359 | 37.0 | 34.3 |
| Sansone 109 | 2016 | J Hip Pres Surg | Prospective | 74 | Arthroscopy | 12.8 | 80 | 47.0 | 23.0 |
| Singh 112 | 2010 | Arthroscopy | Prospective | 66 | Arthroscopy | 22.0 | 27 | 22.0 | |
| Sink 113 | 2013 | Clin Orthop Relat Res | Retrospective | 61 | Open | 27.0 | 52 | 16.2 | 84.1 |
| Skendzel 114 | 2014 | Am J Sports Med | Retrospective | 63 | Arthroscopy | 73.0 | 383 | 37.0 | |
| 63 | 46.0 | ||||||||
| Skowronek 115 | 2017 | Indian J Orthop | Retrospective | 66 | Open | 45.0 | 39 | 29.3 | 35.9 |
| Stake 116 | 2013 | Am J Sports Med | Prospective | 61 | Arthroscopy | 24.0 | 42 (WC, 21; control, 21) | 39.0 | WC, 15; control, 15 |
| Steppacher 117 | 2014 | Clin Orthop Relat Res | Retrospective | 70 | Open | 72.0 | 97 | 32.0 | 43.0 |
| Tjong 118 | 2016 | Orthop J Sports Med | Retrospective | 46 | Arthroscopy | 24.0 | 23 | Return, 44; not return, 43.7 | Return, 47; not return, 53 |
| Tjong 119 | 2017 | Arthroscopy | Prospective | 62 | Open | 37.2 | 106 | 38.1 | 58.0 |
| Tran 120 | 2013 | ANZ J Surg | Retrospective | 61 | Arthroscopy | 14.0 | 41 | 15.7 | 14.7 |
| Wang 121 | 2011 | Orthop Surg | Retrospective | 51 | Arthroscopy | 11.6 | 21 | 37.1 | 57.1 |
| Wu 122 | 2019 | J Orthop Surg Res | Retrospective | 55 | Mini-open | 44.0 | 39 | 43.6 | 47.2 |
| Zingg 123 | 2013 | Arch Orthop Trauma Surg | Prospective | 68 | Arthroscopy | 12.0 | 23 | 27.6 | 21.7 |
| Open | 12.0 | 15 | 28.9 | 26.7 |
BD, borderline dysplastic; CLT, complete labral tear; CMS, Coleman Methodology Score; IFL, iliopsoas fractional lengthening; PRP, platelet-rich plasma; WC, workers’ compensation.
Patient Demographics
Data from 9357 procedures (8897 patients) were collected. The median follow-up was 30.9 months (interquartile range, 24.0-45.0). The mean ± SD age was 33.4 ± 9.3 years; mean BMI, 24.8 ± 4.8; percentage right side, 55.8% ± 8.0%; and percentage female sex, 47.5% ± 20.4%. Baseline characteristics are shown in Table 1.
Outcomes of Interest
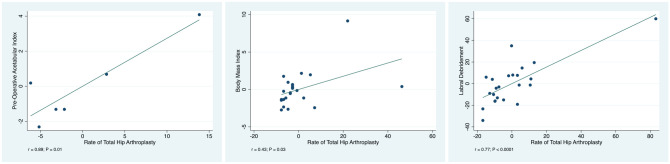
The overall rate of revision was 5.29% (351 of 6641 patients), while the rate of subsequent progression to THA was 3.78% (263 of 6966 patients). Labral debridement showed evidence of a statistically significant positive and strong association with an increased rate of progression to THA (r = 0.77; P < .0001). Equally, a higher preoperative acetabular index showed evidence of a statistically significant positive and strong association with an increased rate of progression to THA (r = 0.89; P = .01). The BMI at baseline showed evidence of a statistically significant positive and moderate association with an increased rate of THA (r = 0.43; P = .03). No other statistically significant associations were found between patient characteristics, type of lesion, type of intervention, radiographic parameters, physical examination, or pre- and postoperative scores and the rate of revision and/or progression to THA. The added-variable plots of these regressions are shown in Figure 2. The multivariate analysis including all the endpoints is shown in Appendix Table A1 (available in the online version of this article).
Figure 2.
Added-variable plots of the associations: acetabular index, body mass index, and labral debridement.
Discussion
FAI is a frequent and well-recognized cause for hip pain, joint damage, and early-onset osteoarthritis in young adults and athletes. Over the past few decades, better understanding of the pathophysiology and natural course of FAI has led to earlier identification and improved treatment options for this condition. The present study described the rates of revision and THA progression after surgical treatment of FAI, identifying some variables associated with increased rates of progression to THA. The overall revision rate after surgical treatment of FAI was 5.29%, and 3.78% of 9357 procedures progressed to THA. To date, this is the largest systematic review to analyze revision and progression rates after surgical treatment of FAI, including a total of 99 studies. According to the main results of the present study, BMI at baseline, labral debridement, and acetabular index were significantly associated with an increased rate of progression to THA. No other statistically significant associations were identified between patient characteristics, type of lesion, type of intervention, radiographic parameters, physical examination, or pre- and postoperative scores and the rate of revision and/or progression to THA.
Surgical hip dislocation for the treatment of FAI—including labral repair, labral debridement, femoral osteochondroplasty, and acetabuloplasty—leads to improvements in hip range of motion, radiographic parameters, and clinical outcomes comparable with those of hip arthroscopy.30,80,91,117 Surgical treatment for FAI, regardless of the technique, improves hip function, with 68% to 96% of patients reporting good to excellent results after a minimum follow-up of 2 years. 21
One of the main findings of our study was an overall revision rate of 5.29% after surgical treatment of FAI (open hip dislocation, mini-open, and arthroscopic). These findings are similar to those from a registry study from the United Kingdom, which showed a revision hip arthroscopy rate of 4.5% at a mean 1.7 years. 71 In a systematic review of >6000 patients, the reoperation rate was 6.3% at a mean 1.6 years, and the most common reason for revision surgery was progression to THA. 47
No or mild hip osteoarthritis, labral repair, young age, and limited cartilage damage have been associated with good clinical outcomes, with a progression to THA in 0% to 26% of the cases. 21 A systematic review compared outcomes and rates of progression to THA between surgical hip dislocation and arthroscopy 86 : 7% of the hips were converted to a THA after a maximum follow-up of 12 years in the open group, as compared with 9.5% after 8.1 years in the arthroscopic group, with no statistical difference between them. Byrd and Jones14,15 reported THA progression rates between 0% and 29% at 2 years after hip arthroscopy. Schairer et al 110 used population-level data of State Ambulatory Surgery Databases and State Inpatient Databases for California and Florida from 2005 to 2012 to examine the progression rate of THA within 2 years after hip arthroscopy. They found an overall progression rate of 12.4% within 2 years after hip arthroscopy, with a significant difference between age groups. In patients <40 years old, the progression rate to THA was 3.0%, which is comparable with our findings of a 3.78% progression rate in patients with a mean age of 33.9 years. The rate of THA progression decreased steadily over time from 14.3% in 2005 to 10.3% in 2010. 110
Age seems to be a risk factor for THA progression: patients aged >50 years exhibited a progression rate of about 20%.71,110 This contrasted with the findings of the present systematic review, where age was not significantly associated with a higher rate of THA progression. Differences between our results and the findings of others might be explained by the fact that we included all types of surgical treatment for FAI, instead of focusing on arthroscopic procedures; other potential reasons include the type of data used, the type of analysis conducted (registry vs systematic), and the younger age of the patients in our study.
BMI at baseline was significantly associated with an increase in the rate of THA progression at a mean follow-up of 38 months. These findings confirm previous results, which found that obesity is an independent risk factor for THA progression after hip arthroscopy at a mean follow-up of 2 years. 110 In addition, Gupta et al 43 and Collins et al 24 confirmed, in small case series studies, that obesity is associated with higher rates of THA progression after arthroscopic procedures. Our results showed that BMI was a risk factor for THA progression, regardless of the surgical technique.
We were also able to show that the preoperative acetabular index was significantly associated with an increased rate of progression to THA. So far, no studies showed an association between the preoperative acetabular index and the progression rate to THA. However, high lateral center-edge angles and low acetabular indices, which require more complex surgical techniques for adequate treatment, are associated with higher rates of revision surgery. 59
Furthermore, we found that labral debridement was associated with an increase in the rate of THA revision for the 3 major surgical techniques analyzed in the present investigation. Schilders et al 111 demonstrated superior outcomes after labral repair as compared with labral debridement in 96 patients with a mean follow-up of 2 years. This was confirmed by Larson et al 65 in a case-control study, with better Harris Hip Score, SF-12, and visual analog scale outcomes in the labral repair group. Menge et al 75 compared 79 patients who underwent labral repair and 75 patients who underwent labral debridement at a mean follow-up of 10 years: no difference in clinical outcomes between the techniques was evident. However, when controlling for acetabular microfracture, Menge et al reported that labral debridement was associated with a significantly higher risk of progression to THA, confirming our findings.
This study presents several limitations. Although we have carefully followed recommended guidelines for the preparation of systematic reviews, the overall quality of the studies was low. Most of the studies were retrospective, and eligibility criteria and rehabilitation protocols were not frequently reported. The overall CMS of 64 shows acceptable quality. The mean follow-up of the studies was 30 months, which is longer than most previous studies, but revision and progression rates are likely to increase with long-term follow-up. Given these premises, the risk of biased results is moderate to high; thus, data from the present study must be interpreted with caution. The purpose of the present study was to investigate whether the aforementioned endpoints are associated with the rate of revision and subsequent progression to THA. Thus, every endpoint was investigated independently, and its risk of recurrence in revision and progression to THA was assessed. We did not perform any comparison between endpoints and their overall effect on the surgical outcomes. This may represent a limitation of the present study. However, in the current literature, there is a multitude of studies focusing on several aspects of FAI correction, evaluating and comparing all the endpoints and their effect on the surgical outcomes. Future studies should overcome these limitations, and high-quality investigations with longer follow-up should be performed.
Conclusion
Surgical treatment for FAI leads to satisfactory outcomes. In this systematic review of 99 studies and 9357 procedures, we found an overall revision rate of 5.29% after surgical treatment. After a median follow-up of 30 months, the progression rate to THA was 3.78%. Patients were at higher risk for a subsequent progression to THA if they had a high BMI, a pathologic acetabular index, or labral debridement during correction of FAI. Therefore, we do advocate additional education of this patient population in terms of its expected outcomes and surgical labral repair instead of simple debridement if needed and technically feasible.
Supplemental Material
Supplemental material, sj-pdf-1-ajs-10.1177_03635465211011744 for Revision Surgery and Progression to Total Hip Arthroplasty After Surgical Correction of Femoroacetabular Impingement: A Systematic Review by Filippo Migliorini, Nicola Maffulli, Alice Baroncini, Jörg Eschweiler, Markus Tingart and Marcel Betsch in The American Journal of Sports Medicine
Acknowledgments
The authors thank Michael Berner for his support and motivation during the study conceptualization. They also thank Paolo Aretini, PhD, for his consistent support and motivation during the statistical analyses.
Footnotes
Submitted September 8, 2020; accepted December 22, 2020.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
An online CME course associated with this article is available for 1 AMA PRA Category 1 Credit™ at http://www.sportsmed.org/aossmimis/Members/Education/AJSM_Current_Concepts_Store.aspx. In accordance with the standards of the Accreditation Council for Continuing Medical Education (ACCME), it is the policy of The American Orthopaedic Society for Sports Medicine that authors, editors, and planners disclose to the learners all financial relationships during the past 12 months with any commercial interest (A ‘commercial interest’ is any entity producing, marketing, re-selling, or distributing health care goods or services consumed by, or used on, patients). Any and all disclosures are provided in the online journal CME area which is provided to all participants before they actually take the CME activity. In accordance with AOSSM policy, authors, editors, and planners’ participation in this educational activity will be predicated upon timely submission and review of AOSSM disclosure. Noncompliance will result in an author/editor or planner to be stricken from participating in this CME activity.
ORCID iDs: Filippo Migliorini  https://orcid.org/0000-0001-7220-1221
https://orcid.org/0000-0001-7220-1221
Nicola Maffulli  https://orcid.org/0000-0002-5327-3702
https://orcid.org/0000-0002-5327-3702
References
- 1. Anwander H, Siebenrock KA, Tannast M, Steppacher SD. Labral reattachment in femoroacetabular impingement surgery results in increased 10-year survivorship compared with resection. Clin Orthop Relat Res. 2017;475(4):1178-1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bardakos NV, Vasconcelos JC, Villar RN. Early outcome of hip arthroscopy for femoroacetabular impingement: the role of femoral osteoplasty in symptomatic improvement. J Bone Joint Surg Br. 2008;90(12):1570-1575. [DOI] [PubMed] [Google Scholar]
- 3. Beaulé PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89(4):773-779. [DOI] [PubMed] [Google Scholar]
- 4. Beck M, Buchler L. Prevalence and impact of pain at the greater trochanter after open surgery for the treatment of femoro-acetabular impingement. J Bone Joint Surg Am. 2011;93(suppl 2):66-69. [DOI] [PubMed] [Google Scholar]
- 5. Beck M, Leunig M, Parvizi J, et al. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67-73. [PubMed] [Google Scholar]
- 6. Bedi A, Dolan M, Hetsroni I, et al. Surgical treatment of femoroacetabular impingement improves hip kinematics: a computer-assisted model. Am J Sports Med. 2011;39:43S-49S. [DOI] [PubMed] [Google Scholar]
- 7. Bellotti V, Cardenas C, Astarita E, et al. Mini-open approach for femoroacetabular impingement: 10 years experience and evolved indications. Hip Int. 2016;26(suppl 1):38-42. [DOI] [PubMed] [Google Scholar]
- 8. Boone GR, Pagnotto MR, Walker JA, Trousdale RT, Sierra RJ. Caution should be taken in performing surgical hip dislocation for the treatment of femoroacetabular impingement in patients over the age of 40. HSS J. 2012;8(3):230-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Botser IB, Jackson TJ, Smith TW, et al. Open surgical dislocation versus arthroscopic treatment of femoroacetabular impingement. Am J Orthop (Belle Mead NJ). 2014;43(5):209-214. [PubMed] [Google Scholar]
- 10. Bryan AJ, Krych AJ, Pareek A, et al. Are short-term outcomes of hip arthroscopy in patients 55 years and older inferior to those in younger patients? Am J Sports Med. 2016;44(10):2526-2530. [DOI] [PubMed] [Google Scholar]
- 11. Büchler L, Neumann M, Schwab JM, et al. Arthroscopic versus open cam resection in the treatment of femoroacetabular impingement. Arthroscopy. 2013;29(4):653-660. [DOI] [PubMed] [Google Scholar]
- 12. Byrd JW, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467(3):739-746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement in athletes. Am J Sports Med. 2011;39:7S-13S. [DOI] [PubMed] [Google Scholar]
- 14. Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy. 2011;27(10):1379-1388. [DOI] [PubMed] [Google Scholar]
- 15. Byrd JW, Jones KS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up. Arthroscopy. 2009;25(4):365-368. [DOI] [PubMed] [Google Scholar]
- 16. Byrd JW, Jones KS, Gwathmey FW. Arthroscopic management of femoroacetabular impingement in adolescents. Arthroscopy. 2016;32(9):1800-1806. [DOI] [PubMed] [Google Scholar]
- 17. Camenzind RS, Steurer-Dober I, Beck M. Clinical and radiographical results of labral reconstruction. J Hip Preserv Surg. 2015;2(4):401-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chaudhary MM, Chaudhary IM, Vikas KN, et al. Surgical hip dislocation for treatment of cam femoroacetabular impingement. Indian J Orthop. 2015;49(5):496-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cho SH. Open surgical treatment for femoroacetabular impingement in patients over thirty years: two years follow-up results. Hip Pelvis. 2015;27(4):241-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Clohisy JC, McClure JT. Treatment of anterior femoroacetabular impingement with combined hip arthroscopy and limited anterior decompression. Iowa Orthop J. 2005;25:164-171. [PMC free article] [PubMed] [Google Scholar]
- 21. Clohisy JC, St John LC, Schutz AL. Surgical treatment of femoroacetabular impingement: a systematic review of the literature. Clin Orthop Relat Res. 2010;468(2):555-564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cohen SB, Huang R, Ciccotti MG, Dodson CC, Parvizi J. Treatment of femoroacetabular impingement in athletes using a mini-direct anterior approach. Am J Sports Med. 2012;40(7):1620-1627. [DOI] [PubMed] [Google Scholar]
- 23. Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD; Victorian Institute of Sport Tendon Study Group. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Scand J Med Sci Sports. 2000;10(1):2-11. [DOI] [PubMed] [Google Scholar]
- 24. Collins JA, Beutel BG, Garofolo G, Youm T. Correlation of obesity with patient-reported outcomes and complications after hip arthroscopy. Arthroscopy. 2015;31(1):57-62. [DOI] [PubMed] [Google Scholar]
- 25. Comba F, Yacuzzi C, Ali PJ, et al. Joint preservation after hip arthroscopy in patients with FAI: prospective analysis with a minimum follow-up of seven years. Muscles Ligaments Tendons J. 2016;6(3):317-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Degen RM, Mayer SW, Fields KG, et al. Functional outcomes and cam recurrence after arthroscopic treatment of femoroacetabular impingement in adolescents. Arthroscopy. 2017;33(7):1361-1369. [DOI] [PubMed] [Google Scholar]
- 27. Domb BG, Chaharbakhshi EO, Rybalko D, et al. Outcomes of hip arthroscopic surgery in patients with Tönnis grade 1 osteoarthritis at a minimum 5-year follow-up: a matched-pair comparison with a Tönnis grade 0 control group. Am J Sports Med. 2017;45(10):2294-2302. [DOI] [PubMed] [Google Scholar]
- 28. Domb BG, El Bitar YF, Stake CE, et al. Arthroscopic labral reconstruction is superior to segmental resection for irreparable labral tears in the hip: a matched-pair controlled study with minimum 2-year follow-up. Am J Sports Med. 2014;42(1):122-130. [DOI] [PubMed] [Google Scholar]
- 29. Domb BG, Linder D, Finley Z, et al. Outcomes of hip arthroscopy in patients aged 50 years or older compared with a matched-pair control of patients aged 30 years or younger. Arthroscopy. 2015;31(2):231-238. [DOI] [PubMed] [Google Scholar]
- 30. Domb BG, Stake CE, Botser IB, Jackson TJ. Surgical dislocation of the hip versus arthroscopic treatment of femoroacetabular impingement: a prospective matched-pair study with average 2-year follow-up. Arthroscopy. 2013;29(9):1506-1513. [DOI] [PubMed] [Google Scholar]
- 31. Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88(5):925-935. [DOI] [PubMed] [Google Scholar]
- 32. Ezechielia M, De Meob F, Bellottic V, et al. Arthroscopic assisted mini-open approach of the hip: early multicentric experience. Technol Health Care. 2016;24:359-365.33. [DOI] [PubMed] [Google Scholar]
- 33. Fabricant PD, Fields KG, Taylor SA, et al. The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. J Bone Joint Surg Am. 2015;97(7):537-543. [DOI] [PubMed] [Google Scholar]
- 34. Flores SE, Borak KR, Zhang AL. Hip arthroscopic surgery for femoroacetabular impingement: a prospective analysis of the relationship between surgeon experience and patient outcomes. Orthop J Sports Med. 2018;6(2):2325967118755048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Frank RM, Lee S, Bush-Joseph CA, et al. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42(11):2634-2642. [DOI] [PubMed] [Google Scholar]
- 36. Fukui K, Briggs KK, Trindade CA, Philippon MJ. Outcomes after labral repair in patients with femoroacetabular impingement and borderline dysplasia. Arthroscopy. 2015;31(12):2371-2379. [DOI] [PubMed] [Google Scholar]
- 37. Fukui K, Trindade CA, Briggs KK, Philippon MJ. Arthroscopy of the hip for patients with mild to moderate developmental dysplasia of the hip and femoroacetabular impingement: outcomes following hip arthroscopy for treatment of chondrolabral damage. Bone Joint J. 2015;97(10):1316-1321. [DOI] [PubMed] [Google Scholar]
- 38. Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-120. [DOI] [PubMed] [Google Scholar]
- 40. Gedouin JE, May O, Bonin N, et al. Assessment of arthroscopic management of femoroacetabular impingement: a prospective multicenter study. Orthop Traumatol Surg Res. 2010;96(8):S59-S67. [DOI] [PubMed] [Google Scholar]
- 41. Gicquel T, Gedouin JE, Krantz N, et al. Function and osteoarthritis progression after arthroscopic treatment of femoro-acetabular impingement: a prospective study after a mean follow-up of 4.6 (4.2-5.5) years. Orthop Traumatol Surg Res. 2014;100(6):651-656. [DOI] [PubMed] [Google Scholar]
- 42. Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010;92(5):1162-1169. [DOI] [PubMed] [Google Scholar]
- 43. Gupta A, Redmond JM, Hammarstedt JE, et al. Does obesity affect outcomes after hip arthroscopy? A cohort analysis. J Bone Joint Surg Am. 2015;97(1):16-23. [DOI] [PubMed] [Google Scholar]
- 44. Gupta A, Redmond JM, Stake CE, Dunne KF, Domb BG. Does primary hip arthroscopy result in improved clinical outcomes? 2-year clinical follow-up on a mixed group of 738 consecutive primary hip arthroscopies performed at a high-volume referral center. Am J Sports Med. 2016;44(1):74-82. [DOI] [PubMed] [Google Scholar]
- 45. Gupta A, Redmond JM, Stake CE, et al. Does the femoral cam lesion regrow after osteoplasty for femoroacetabular impingement? Two-year follow-up. Am J Sports Med. 2014;42(9):2149-2155. [DOI] [PubMed] [Google Scholar]
- 46. Haefeli PC, Albers CE, Steppacher SD, Tannast M, Buchler L. What are the risk factors for revision surgery after hip arthroscopy for femoroacetabular impingement at 7-year followup? Clin Orthop Relat Res. 2017;475(4):1169-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Harris JD, McCormick FM, Abrams GD, et al. Complications and reoperations during and after hip arthroscopy: a systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29(3):589-595. [DOI] [PubMed] [Google Scholar]
- 48. Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20-33. [PubMed] [Google Scholar]
- 49. Hartigan DE, Perets I, Yuen LC, Domb BG. Results of hip arthroscopy in patients with MRI diagnosis of subchondral cysts—a case series. J Hip Preserv Surg. 2017;4(4):324-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hartmann A, Gunther KP. Arthroscopically assisted anterior decompression for femoroacetabular impingement: technique and early clinical results. Arch Orthop Trauma Surg. 2009;129(8):1001-1009. [DOI] [PubMed] [Google Scholar]
- 51. Hatakeyama A, Utsunomiya H, Nishikino S, et al. Predictors of poor clinical outcome after arthroscopic labral preservation, capsular plication, and cam osteoplasty in the setting of borderline hip dysplasia. Am J Sports Med. 2018;46(1):135-143. [DOI] [PubMed] [Google Scholar]
- 52. Honda E, Utsunomiya H, Hatakeyama A, et al. Patients aged in their 70s do not have a high risk of progressive osteoarthritis following arthroscopic femoroacetabular impingement correction and labral preservation surgery. Knee Surg Sports Traumatol Arthrosc. 2020;28(5):1648-1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoral acetabular impingement in patients with preoperative generalized degenerative changes. Arthroscopy. 2010;26(5):623-629. [DOI] [PubMed] [Google Scholar]
- 54. Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoroacetabular impingement of the hip: a new technique to access the joint. Clin Orthop Relat Res. 2010;468(1):182-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Howick J, Chalmers I, Glasziou P, et al. The 2011 Oxford levels of evidence. Oxford Centre for Evidence-Based Medicine. Published 2011. https://wwwcebmnet/indexaspx?o=5653
- 56. Hufeland M, Kruger D, Haas NP, Perka C, Schroder JH. Arthroscopic treatment of femoroacetabular impingement shows persistent clinical improvement in the mid-term. Arch Orthop Trauma Surg. 2016;136(5):687-691. [DOI] [PubMed] [Google Scholar]
- 57. Ilizaliturri VM, Jr, Nossa-Barrera JM, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of femoroacetabular impingement secondary to paediatric hip disorders. J Bone Joint Surg Br. 2007;89(8):1025-1030. [DOI] [PubMed] [Google Scholar]
- 58. Ilizaliturri VM, Jr, Orozco-Rodriguez L, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of cam-type femoroacetabular impingement: preliminary report at 2 years minimum follow-up. J Arthroplasty. 2008;23(2):226-234. [DOI] [PubMed] [Google Scholar]
- 59. Kaplan FS, Dalinka M, Karp JS, et al. Quantitative computed tomography reflects vertebral fracture morbidity in osteopenic patients. Orthopedics. 1989;12(7):949-955. [DOI] [PubMed] [Google Scholar]
- 60. Khanduja V, Villar RN. The arthroscopic management of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):1035-1040. [DOI] [PubMed] [Google Scholar]
- 61. Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29(1):46-53. [DOI] [PubMed] [Google Scholar]
- 62. Kunze KN, Beck EC, Nwachukwu BU, Ahn J, Nho SJ. Early hip arthroscopy for femoroacetabular impingement syndrome provides superior outcomes when compared with delaying surgical treatment beyond 6 months. Am J Sports Med. 2019;47(9):2038-2044. [DOI] [PubMed] [Google Scholar]
- 63. LaFrance R, Kenney R, Giordano B, et al. The effect of platelet enriched plasma on clinical outcomes in patients with femoroacetabular impingement following arthroscopic labral repair and femoral neck osteoplasty. J Hip Preserv Surg. 2015;2(2):158-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25(4):369-376. [DOI] [PubMed] [Google Scholar]
- 65. Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40(5):1015-1021. [DOI] [PubMed] [Google Scholar]
- 66. Lavigne M, Parvizi J, Beck M, et al. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61-66. [PubMed] [Google Scholar]
- 67. Levy DM, Cvetanovich GL, Kuhns BD, et al. Hip arthroscopy for atypical posterior hip pain: a comparative matched-pair analysis. Am J Sports Med. 2017;45(7):1627-1632. [DOI] [PubMed] [Google Scholar]
- 68. Levy DM, Kuhns BD, Frank RM, et al. High rate of return to running for athletes after hip arthroscopy for the treatment of femoroacetabular impingement and capsular plication. Am J Sports Med. 2017;45(1):127-134. [DOI] [PubMed] [Google Scholar]
- 69. Maldonado DR, Krych AJ, Levy BA, et al. Does iliopsoas lengthening adversely affect clinical outcomes after hip arthroscopy? A multicenter comparative study. Am J Sports Med. 2018;46(11):2624-2631. [DOI] [PubMed] [Google Scholar]
- 70. Maldonado DR, Laseter JR, Perets I, et al. The effect of complete tearing of the ligamentum teres in patients undergoing primary hip arthroscopy for femoroacetabular impingement and labral tears: a match-controlled study. Arthroscopy. 2019;35(1):80-88. [DOI] [PubMed] [Google Scholar]
- 71. Malviya A, Raza A, Jameson S, et al. Complications and survival analyses of hip arthroscopies performed in the national health service in England: a review of 6,395 cases. Arthroscopy. 2015;31(5):836-842. [DOI] [PubMed] [Google Scholar]
- 72. Mardones R, Via AG, Tomic A, et al. Arthroscopic release of iliopsoas tendon in patients with femoro-acetabular impingement: clinical results at mid-term follow-up. Muscles Ligaments Tendons J. 2016;6(3):378-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Matsuda DK, Gupta N, Burchette RJ, Sehgal B. Arthroscopic surgery for global versus focal pincer femoroacetabular impingement: are the outcomes different? J Hip Preserv Surg. 2015;2(1):42-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. McConkey MO, Chadayammuri V, Garabekyan T, et al. Simultaneous bilateral hip arthroscopy in adolescent athletes with symptomatic femoroacetabular impingement. J Pediatr Orthop. 2019;39(4):193-197. [DOI] [PubMed] [Google Scholar]
- 75. Menge TJ, Briggs KK, Dornan GJ, McNamara SC, Philippon MJ. Survivorship and outcomes 10 years following hip arthroscopy for femoroacetabular impingement: labral debridement compared with labral repair. J Bone Joint Surg Am. 2017;99(12):997-1004. [DOI] [PubMed] [Google Scholar]
- 76. Mohan R, Johnson NR, Hevesi M, et al. Return to sport and clinical outcomes after hip arthroscopic labral repair in young amateur athletes: minimum 2-year follow-up. Arthroscopy. 2017;33(9):1679-1684. [DOI] [PubMed] [Google Scholar]
- 77. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. BMJ. 2009;339:B2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Moriya M, Fukushima K, Uchiyama K, et al. Clinical results of arthroscopic surgery in patients over 50 years of age—what viability does it have as a joint preservative surgery? J Orthop Surg Res. 2017;12(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:178-181. [DOI] [PubMed] [Google Scholar]
- 80. Naal FD, Miozzari HH, Schar M, Hesper T, Nötzli HP. Midterm results of surgical hip dislocation for the treatment of femoroacetabular impingement. Am J Sports Med. 2012;40(7):1501-1510. [DOI] [PubMed] [Google Scholar]
- 81. Naal FD, Miozzari HH, Wyss TF, Nötzli HP. Surgical hip dislocation for the treatment of femoroacetabular impingement in high-level athletes. Am J Sports Med. 2011;39(3):544-550. [DOI] [PubMed] [Google Scholar]
- 82. Nawabi DH, Degen RM, Fields KG, et al. Outcomes after arthroscopic treatment of femoroacetabular impingement for patients with borderline hip dysplasia. Am J Sports Med. 2016;44(4):1017-1023. [DOI] [PubMed] [Google Scholar]
- 83. Nho SJ, Magennis EM, Singh CK, Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39:14S-19S. [DOI] [PubMed] [Google Scholar]
- 84. Nielsen TG, Miller LL, Lund B, Christiansen SE, Lind M. Outcome of arthroscopic treatment for symptomatic femoroacetabular impingement. BMC Musculoskelet Disord. 2014;15:394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Novais EN, Heyworth BE, Stamoulis C, et al. Open surgical treatment of femoroacetabular impingement in adolescent athletes: preliminary report on improvement of physical activity level. J Pediatr Orthop. 2014;34(3):287-294. [DOI] [PubMed] [Google Scholar]
- 86. Nwachukwu BU, Rebolledo BJ, McCormick F, et al. Arthroscopic versus open treatment of femoroacetabular impingement: a systematic review of medium- to long-term outcomes. Am J Sports Med. 2016;44(4):1062-1068. [DOI] [PubMed] [Google Scholar]
- 87. Palmer DH, Ganesh V, Comfort T, Tatman P. Midterm outcomes in patients with cam femoroacetabular impingement treated arthroscopically. Arthroscopy. 2012;28(11):1671-1681. [DOI] [PubMed] [Google Scholar]
- 88. Perets I, Gupta A, Chaharbakhshi EO, et al. Does bony regrowth occur after arthroscopic femoroplasty in a group of young adolescents? Arthroscopy. 2017;33(5):988-995. [DOI] [PubMed] [Google Scholar]
- 89. Perets I, Hartigan DE, Chaharbakhshi EO, et al. Clinical outcomes and return to sport in competitive athletes undergoing arthroscopic iliopsoas fractional lengthening compared with a matched control group without iliopsoas fractional lengthening. Arthroscopy. 2018;34(2):456-463. [DOI] [PubMed] [Google Scholar]
- 90. Perets I, Rybalko D, Chaharbakhshi EO, et al. Minimum five-year outcomes of hip arthroscopy for the treatment of femoroacetabular impingement and labral tears in patients with obesity: a match-controlled study. J Bone Joint Surg Am. 2018;100(11):965-973. [DOI] [PubMed] [Google Scholar]
- 91. Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and debridement in young adults. J Bone Joint Surg Am. 2006;88(8):1735-1741. [DOI] [PubMed] [Google Scholar]
- 92. Peters CL, Schabel K, Anderson L, Erickson J. Open treatment of femoroacetabular impingement is associated with clinical improvement and low complication rate at short-term followup. Clin Orthop Relat Res. 2010;468(2):504-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91(1):16-23. [DOI] [PubMed] [Google Scholar]
- 94. Philippon MJ, Ejnisman L, Ellis HB, Briggs KK. Outcomes 2 to 5 years following hip arthroscopy for femoroacetabular impingement in the patient aged 11 to 16 years. Arthroscopy. 2012;28(9):1255-1261. [DOI] [PubMed] [Google Scholar]
- 95. Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):1041-1047. [DOI] [PubMed] [Google Scholar]
- 96. Philippon MJ, Schroder ESBG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy. 2012;28(1):59-65. [DOI] [PubMed] [Google Scholar]
- 97. Philippon MJ, Stubbs AJ, Schenker ML, et al. Arthroscopic management of femoroacetabular impingement: osteoplasty technique and literature review. Am J Sports Med. 2007;35(9):1571-1580. [DOI] [PubMed] [Google Scholar]
- 98. Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38(1):99-104. [DOI] [PubMed] [Google Scholar]
- 99. Polesello GC, Lima FR, Guimaraes RP, Ricioli W, Queiroz MC. Arthroscopic treatment of femoroacetabular impingement: minimum five-year follow-up. Hip Int. 2014;24(4):381-386. [DOI] [PubMed] [Google Scholar]
- 100. Polesello GC, Queiroz MC, Ono NK, et al. Arthroscopic treatment of femoroacetabular impingement. Rev Bras Ortop. 2009;44(3):230-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Rafols C, Monckeberg JE, Numair J, Botello J, Rosales J. Platelet-rich plasma augmentation of arthroscopic hip surgery for femoroacetabular impingement: a prospective study with 24-month follow-up. Arthroscopy. 2015;31(10):1886-1892. [DOI] [PubMed] [Google Scholar]
- 102. Rego PA, Mascarenhas V, Oliveira FS, et al. Arthroscopic versus open treatment of cam-type femoro-acetabular impingement: retrospective cohort clinical study. Int Orthop. 2018;42(4):791-797. [DOI] [PubMed] [Google Scholar]
- 103. Rhee SM, Kang SY, Jang EC, Kim JY, Ha YC. Clinical outcomes after arthroscopic acetabular labral repair using knot-tying or knotless suture technique. Arch Orthop Trauma Surg. 2016;136(10):1411-1416. [DOI] [PubMed] [Google Scholar]
- 104. Roos BD, Roos MV, Camisa Junior A, Lima EMU, Betto MD. Open versus arthroscopic approach in the treatment of femoroacetabular impingement: a case-control study with two-years follow up. Rev Bras Ortop. 2017;52(suppl 1):21-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Sanders TL, Reardon P, Levy BA, Krych AJ. Arthroscopic treatment of global pincer-type femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):31-35. [DOI] [PubMed] [Google Scholar]
- 106. Sankar WN, Nevitt M, Parvizi J, et al. Femoroacetabular impingement: defining the condition and its role in the pathophysiology of osteoarthritis. J Am Acad Orthop Surg. 2013;21(suppl 1):S7-S15. [DOI] [PubMed] [Google Scholar]
- 107. Sansone M, Ahldén M, Jonasson P, et al. Good results after hip arthroscopy for femoroacetabular impingement in top-level athletes. Orthop J Sports Med. 2015;3(2):2325967115569691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Sansone M, Ahldén M, Jonasson P, et al. Outcome after hip arthroscopy for femoroacetabular impingement in 289 patients with minimum 2-year follow-up. Scand J Med Sci Sports. 2017;27(2):230-235. [DOI] [PubMed] [Google Scholar]
- 109. Sansone M, Ahldén M, Jonasson P, et al. Outcome of hip arthroscopy in patients with mild to moderate osteoarthritis—a prospective study. J Hip Preserv Surg. 2016;3(1):61-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Schairer WW, Nwachukwu BU, McCormick F, Lyman S, Mayman D. Use of hip arthroscopy and risk of conversion to total hip arthroplasty: a population-based analysis. Arthroscopy. 2016;32(4):587-593. [DOI] [PubMed] [Google Scholar]
- 111. Schilders E, Dimitrakopoulou A, Bismil Q, Marchant P, Cooke C. Arthroscopic treatment of labral tears in femoroacetabular impingement: a comparative study of refixation and resection with a minimum two-year follow-up. J Bone Joint Surg Br. 2011;93(8):1027-1032. [DOI] [PubMed] [Google Scholar]
- 112. Singh PJ, O’Donnell JM. The outcome of hip arthroscopy in Australian football league players: a review of 27 hips. Arthroscopy. 2010;26(6):743-749. [DOI] [PubMed] [Google Scholar]
- 113. Sink EL, Fabricant PD, Pan Z, Dayton MR, Novais E. Results of treatment of femoroacetabular impingement in adolescents with a surgical hip dislocation approach. Clin Orthop Relat Res. 2013;471(8):2563-2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Skendzel JG, Philippon MJ, Briggs KK, Goljan P. The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med. 2014;42(5):1127-1133. [DOI] [PubMed] [Google Scholar]
- 115. Skowronek P, Synder M, Polguj M, Marczak D, Sibinski M. Treatment of femoroacetabular impingement with a mini-open direct anterior approach. Indian J Orthop. 2017;51(6):677-680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Stake CE, Jackson TJ, Stone JC, Domb BG. Hip arthroscopy for labral tears in workers’ compensation: a matched-pair controlled study. Am J Sports Med. 2013;41(10):2302-2307. [DOI] [PubMed] [Google Scholar]
- 117. Steppacher SD, Huemmer C, Schwab JM, Tannast M, Siebenrock KA. Surgical hip dislocation for treatment of femoroacetabular impingement: factors predicting 5-year survivorship. Clin Orthop Relat Res. 2014;472(1):337-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Tjong VK, Cogan CJ, Riederman BD, Terry MA. A qualitative assessment of return to sport after hip arthroscopy for femoroacetabular impingement. Orthop J Sports Med. 2016;4(11):2325967116671940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Tjong VK, Gombera MM, Kahlenberg CA, et al. Isolated acetabuloplasty and labral repair for combined-type femoroacetabular impingement: are we doing too much? Arthroscopy. 2017;33(4):773-779. [DOI] [PubMed] [Google Scholar]
- 120. Tran P, Pritchard M, O’Donnell J. Outcome of arthroscopic treatment for cam type femoroacetabular impingement in adolescents. ANZ J Surg. 2013;83(5):382-386. [DOI] [PubMed] [Google Scholar]
- 121. Wang WG, Yue DB, Zhang NF, Hong W, Li ZR. Clinical diagnosis and arthroscopic treatment of acetabular labral tears. Orthop Surg. 2011;3(1):28-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Wu CT, Mahameed M, Lin PC, et al. Treatment of cam-type femoroacetabular impingement using anterolateral mini-open and arthroscopic osteochondroplasty. J Orthop Surg Res. 2019;14(1):222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Zingg PO, Ulbrich EJ, Buehler TC, et al. Surgical hip dislocation versus hip arthroscopy for femoroacetabular impingement: clinical and morphological short-term results. Arch Orthop Trauma Surg. 2013;133(1):69-79. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-ajs-10.1177_03635465211011744 for Revision Surgery and Progression to Total Hip Arthroplasty After Surgical Correction of Femoroacetabular Impingement: A Systematic Review by Filippo Migliorini, Nicola Maffulli, Alice Baroncini, Jörg Eschweiler, Markus Tingart and Marcel Betsch in The American Journal of Sports Medicine