Abstract
Complications after open arch repair much decreased over time thanks to better methods of organ and cerebral protection. The crossroads was the introduction of antegrade cerebral perfusion as a method of cerebral protection. Other intraoperative techniques also contributed to facilitate arch reconstruction, such as performing circulatory arrest at higher core temperature, using hybrid grafts or endografts, and monitoring cerebral functions during the procedure. As part of this exciting process, we go back in Bologna in the early 1970s to relive some of these fundamental steps on aortic arch surgery. Today a large number of issues on cerebral protection remain for which we have incomplete responses. Probably, a super specialized approach and endovascular techniques will continue to improve the quality of care of patients with different arch pathologies.
Keywords: Aortic, Cerebral protection, Arch, Endovascular
Introduction
Open aortic arch surgery can be considered one of the fields of cardiac surgery that developed the most during the last decades. If we think at the early beginning in the ‘50, pioneers like Cooley and De Bakey, to replace the arch, needed to perform complex repair without extracorporeal circulation with extremely high hospital mortality often secondary to neurologic complications [1]. Afterward, deep hypothermia was introduced, initially in congenital cardiac surgery and then in arch surgery with still unsatisfactory results. Barnard in 1963 published a series of 8 cases of thoracic aortic repair, and 4 of them underwent arch surgery using deep hypothermic circulatory arrest with about 50% mortality [2].
Thanks to Dr. Griepp at Stanford University in the early 1970s, arch surgery made substantial progress. He standardized the technique of Deep Hypothermic Circulatory Arrest (DHCA) obtaining a significant reduction in perioperative mortality and morbidity [3].
Nowadays many things have changed. A great contribution was given by a better understanding of aortic pathologies including acute aortic syndrome and chronic aortic aneurysms, including the opportunity to evaluate carefully the entire aorta, and its relationship with the other thoracic and abdominal structures, using excellent imaging techniques as computed tomography (CT) scan or magnetic resonance imaging (MRI). Now, different treatment options are available to treat the aorta, including hybrid open and endovascular procedures, and much safer techniques for cerebral and visceral organ protection.
In this article we will go through the history of aortic surgery in Bologna, current options for aortic arch reconstruction and future perspectives in this field.
The evolution of aortic surgery in Bologna
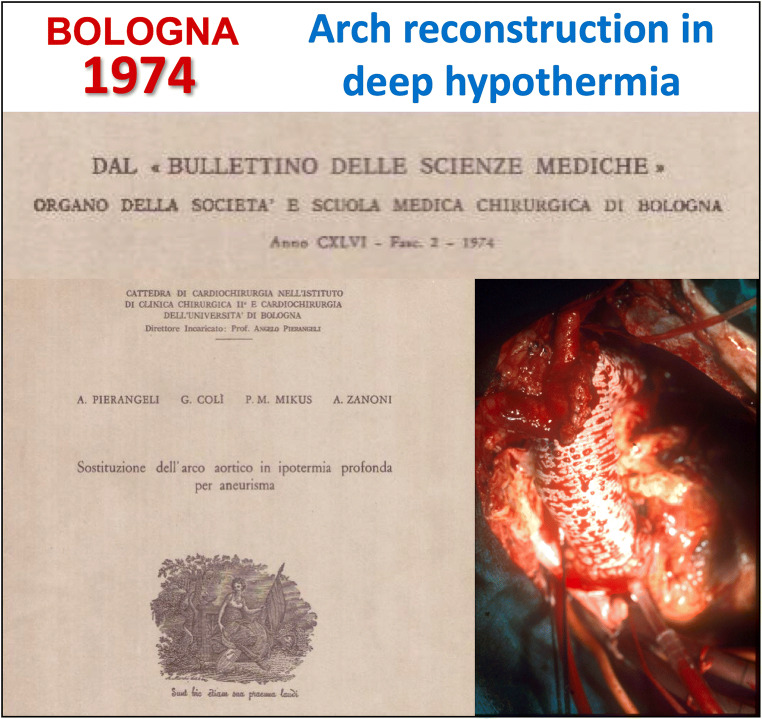
Our experience in aortic arch surgery started in 1974 when Prof Pierangeli was the first to utilize DHCA to repair an atherosclerotic aneurysm (Fig.1) [4]. The technique consisted in cooling down the body temperature to 18 °C to reduce metabolic demand and preserve organ function. To reduce the circulatory arrest time, we used the Pearce technique (island technique). This case was published in 1974 within the “Bullettino delle scienze mediche” - a review of the “Bologna medical-surgical society”- and not in any international journal, reason for which was not given any prominence nor highlighted worldwide. Since then, we have utilized this technique with acceptable results in terms of mortality and neurological morbidity.
Fig. 1.
First case in Bologna of arch reconstruction performed under Deep Hypothermic Circulatory Arrest
The main advantages of the DHCA as a method of brain protection consist in a bloodless operative field, no supra-aortic vessels manipulation and cannulation, and it can be used in almost any circumstance with a regular cardio-pulmonary bypass (CPB) circuit. However, as it is well documented by various authors, DHCA has important limitations: first the limited safe time of circulatory arrest. A safe time of circulatory arrest should be 25 min at 18 °C [5]. Second, the long time required to cool down and to re-warm the patient results in a prolonged CPB time with consequent increase of pulmonary, renal, cardiac and endothelial dysfunction. Moreover, it has been held responsible also for generating important coagulation and inflammatory disorders.
In 1978 we treated a ruptured aortic arch aneurysm in a young (44 years old) patient using for the first time, as method of cerebral protection, the innominate artery perfusion and deep hypothermia (Fig.2). Extracorporeal circulation was instituted from the femoral artery and using a Y graft on the arterial line, a selective unilateral cerebral perfusion was performed during hypothermic arrest.
Fig. 2.
First case in Bologna of arch reconstruction using as method of cerebral protection a unilateral innominate artery perfusion and deep hypothermia
In 1986, Dr. Ueda introduced the Retrograde Cerebral Perfusion with DHCA as method of cerebral protection. This technique prolonged the “safe period” of circulatory arrest, providing metabolic support, removing potentially toxic metabolites and preventing rewarming of the brain during the period without antegrade flow [6, 7]. Moreover, it is considered also a possible method of flushing out cerebral emboli. We started using this technique for few years and then it was abandoned in 1996, because cerebral protection remains unclear and it does not avoid the problems associated with DHCA.
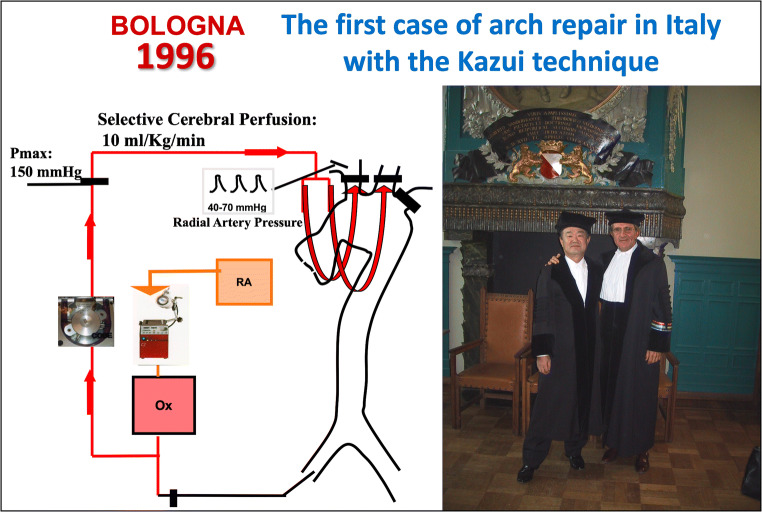
The revolution arrived in 1992 when Kazui et al. introduced the use of a separate arterial pump for the cerebral and systemic circulations with single heat exchanger in a new technique called “antegrade cerebral perfusion” [8]. Cerebral perfusion was obtained by cannulating the innominate and left common carotid arteries. The body temperature was cooled down to 21 °C and cerebral perfusion began with a flow rate of 10 ml/Kg/min, maintaining a right radial artery pressure between 40 to 70 mmHg. This was the Kazui’s first report of 32 patients in which he reported good results [8]. This technique has had a large diffusion all over the world.
Antegrade perfusion to the brain, during the ischemic period necessary to perform aortic arch repair, is beneficial and has its advantages: namely, providing uniform cerebral cooling, maintaining cerebral autoregulation and prolongation of “safe” cerebral protection time. Furthermore, the use of moderate hypothermia allows the reduction of the prolonged cooling and rewarming times and reduces the coagulative complications related to profound hypothermia.
However, a careful deairing of the entire cerebral perfusion system is required, and care must be taken during introduction and positioning of the cannulas to prevent distal dissection of the supra-aortic vessels or debridement of atherosclerotic plaques.
In November 1996 we started to routinely use the Kazui technique with some modifications: the use of a bio-pump for the systemic perfusion and the use of the retrograde cardioplegia cannula for the perfusion of the epiaortic vessels (Fig.3). Other monitoring systems utilized are venous jugular bulb saturation, transcranial spectroscopy (shows changes in cerebral oxygen saturation) and transcranial doppler ultrasound. At that time the hypothermic arrest was performed at 21–22 °C, but after 1 year we started to perform a warmer 25–26 °C arrest [9, 10].
Fig. 3.
The introduction of Bilateral Antegrade Selective Cerebral protection in Bologna, thanks to Prof Kazui
Since 2004 we started using, as arterial line inflow, the axillary artery, in order to achieve antegrade systemic perfusion. During systemic arrest, we perfuse the brain with two separate cannulae, the axillary one guarantees right hemisphere perfusion after clamping the proximal innominate artery. The left side is perfused through a cannula inserted in the left common carotid artery, after opening the arch.
In 2006, a new cannula for brain perfusion was created and began to be used in Bologna. This was the first specific device for epiaortic vessels’ cannulation to obtain a CE mark approval. Named “true flow RDB cannula” (European Medical Supplies S.r.l, Bologna, Italy), it is entirely made of silicon and presents a simplified lock system and a malleable steel wire that reduces the risk of kinking. Moreover, it presents an inflatable balloon and additional side perfusion holes on the tip of the cannula. There are three sizes available (14,17 and 20F). Its unique features allow a safe positioning, low risk of displacement and optimal blood flow to the brain.
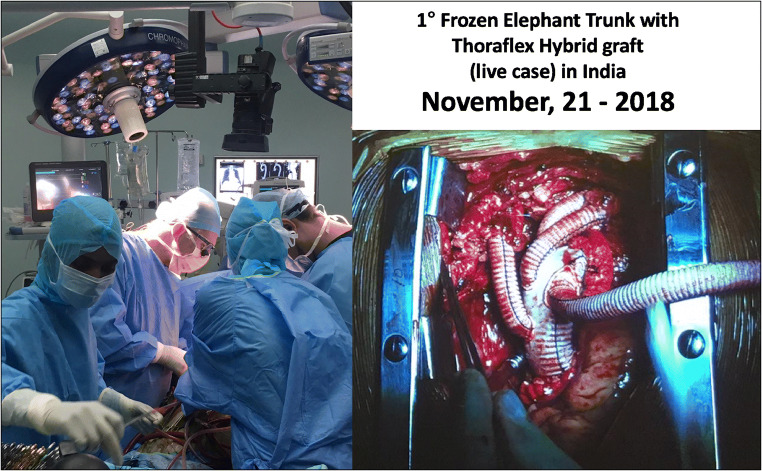
The possibility to better protect the brain and introduction of endovascular techniques allowed to make more complex aortic arch procedures using hybrid grafts. In 2007 we implanted the first E-vita prosthesis in Italy using the frozen elephant trunk technique (FET). Since then, more than 300 FET have been performed using different prostheses and attracting adjuncts to facilitate the procedure [11–13]. We also share our experience in difficult cases with many other experts around the globe (Fig.4).
Fig. 4.
The first Frozen Elephant Trunk procedure with Thoraflex hybrid prosthesis performed in India during a live congress
At the end of ‘90, the possibility to actively contribute in this challenging field gave us the privilege to organize for the first time a specific aortic course with live surgery named “The thoracic aortic surgery”. The congress progressively gained popularity and during the 10th meeting edition more than 600 attendees participated from many countries all around the world.
Current cerebral protection strategies in aortic arch surgery
In recent decades, the outcome of patients after aortic arch surgery has improved considerably [14–17]. However, surgery of the thoracic aorta and, in particular, of the aortic arch, is still associated with significantly high mortality and morbidity caused by neurological complications resulting from temporary suspension of cerebral circulation.
Based on the assumption that all the three brain protection techniques (Antegrade Selective Cerebral Perfusion, Retrograde Cerebral Perfusion, Deep Hypothermic Circulatory Arrest) provide good results in terms of protection of the brain from ischemic damage, the open question remains which technique has to be used in case of short circulatory arrest times in arch reconstructive surgery, taking into account that the antegrade selective cerebral perfusion has proven to be the technique that guarantees the best results in terms of neurological complications, when long period of circulatory arrest is required. Hypothermia is the essential component of all neuroprotective strategies due to its capacity to reduce the metabolic rate of the central nervous system.
There is still controversy about optimal management of DHCA focusing on optimal temperature at arrest, cooling and warming rates, pH strategies, hemodilution and the duration of circulatory arrest.
According to the worldwide experience coming from Europe, North America and Japan, it is possible to draw current trends on cerebral and visceral organs protection towards an increasing use of antegrade brain perfusion performed at higher core temperatures. Another important finding is the less effective cerebral protection achieved using a DHCA without an interval of retrograde or antegrade cerebral perfusion.
In the last survey across European cardiac centres to evaluate the methods used for cerebral protection during aortic surgery involving the aortic arch, bilateral antegrade cerebral perfusion was the most frequent method for brain protection in both acute and chronic clinical presentation.
Unilateral perfusion was utilized in 1/3 of the cases, while deep hypothermic arrest and retrograde perfusion were used very rarely, and almost exclusively in acute presentation [18].
In North America, according to the data coming from the Society of Thoracic Surgeons Database until 2014, out of 12,521 aortic arch repairs, DHCA was the preferred method of cerebral protection over RCP and ASCP, but overall rates of the primary end-point, operative mortality and stroke were 23%, 12% and 8%, respectively [19]. Moreover, only 17% of the procedures were performed under moderate hypothermia and the median circulatory arrest time was 27 min.
However, within North America, higher volume centres appear to have moved towards moderate degrees of hypothermia, potentially indicating a preference for this strategy.
In Bologna we always prefer to achieve a bilateral cerebral perfusion under moderate hypothermia using a central cannulation for both the CPB and brain perfusion. The axillary, innominate or carotid arteries should be selected for cannulation according to a meticulous preoperative angio-CT evaluation. During circulatory arrest the contralateral cerebral hemisphere is directly perfused to establish bilateral cerebral perfusion.
Early outcome and mid-term survival after open arch repair using selective antegrade cerebral perfusion: Bologna experience
Recently, we published our overall experience on aortic arch surgery with ASCP as method of cerebral protection [20]. In summary, we retrospectively reviewed our experience between 1997 and 2017, including in our study all patients who underwent surgical replacement of the aortic arch using selective Antegrade Cerebral Perfusion (n = 938). In order to confirm the effectiveness of this cerebral protection method, early outcome and results were evaluated.
The mean age of the patients was 62.7 ± 11.9 years, and regarding the surgical indications, most of the patients underwent surgery for degenerative aneurysm (331 patients - 35.3%), for acute type A aortic dissection (311–33.1%) and for a post-dissection chronic aneurysm (187–20%). Four hundred and six patients (43.3%) underwent hemiarch replacement, 255 (27.2%) total arch replacement, 58 (6.2%) Elephant Trunk and 219 (23.3%) Frozen Elephant Trunk technique.
In the postoperative period, 175 patients (18.7%) developed a neurological dysfunction; of them, 60 (6.4%) experienced a Permanent Neurological Dysfunction and 115 (12.3%) a Temporary Neurological Dysfunction.
Overall hospital mortality was 11.9% (n = 112). On multivariable analysis, age > 75 years, female gender, EuroSCORE at increment of 1 point, chronic renal failure, extension of thoracic aorta replacement and CPB time emerged as independent risk factors for hospital mortality. The mid-term survival at 1,5,10 and 15 years was 92%,78%,60% and 49% respectively. The cumulative incidence of Permanent Neurological Dysfunction and aortic reoperations was 2% at 3 years, 3% at 5 years and 6% at 10 years and 12% at 3 years,15% at 5 years and 19% at 10 years respectively.
Limitations and new challenges in open arch surgery
The bright innovative course of aortic surgery allowed us to treat many patients with excellent results which we could not have imagined before. However conventional aortic arch surgery still has limitations in terms of invasiveness. Many fields of cardiac surgery are becoming less invasive and trans-catheter based. In the same way, there are new solutions to keep improving results on arch reconstruction. Two big goals need to be achieved:
The first is to embrace endovascular skill in the routine practice. Open and endovascular solutions alone have limitations; it is the reason why both approaches should be a part of the skills of the new generation of surgeons. This possibility will fasten recovery and guarantee a broader possibility of treatment in those patients who are more fragile.
Second important point, what we have learnt from structural heart valve disease, is the concept of centralization of care, where a multidisciplinary aortic team can decide and perform, in specialized centres, open and endovascular solutions. The “aortic team” should involve multi-speciality competences like anesthesiology, radiology, pathology and surgical. According to all the currently available treatment options, it is possible to tailor personalized treatment solutions taking into account expertise, current aortic recommendations and, of course, common sense.
Recently, the European Association for Cardio-thoracic surgery developed an expert consensus document covering all aspects of aortic arch disease to provide the community a pragmatic guide to indication of treatment, and to provide support in choosing the right treatment modality, in the right patient, at the right point in time [21]. The first 5 recommendations, with a class I of evidence, advocate that an aortic team should be closely involved from diagnosis to treatment. Moreover, centralization of care of aortic arch pathologies in large centres is recommended, because it is the only way to effectively understand the natural course of the disease, provide the entire range of treatment options and treat potential complications of each individual therapy.
So, according to the title of the manuscript “Aortic Arch Surgery: What I would have done different?”, much has been done, but we should embrace our energy to reduce neurological complications and offer less invasive solutions to our patients. Aortic arch surgery continues to represent a formidable challenge for cardiac surgeons.
Conclusion
The evolution of open aortic arch surgery made possible to treat safely many different pathologies. The results are excellent if appropriate methods of neurologic and organ protection are adopted.
Antegrade cerebral perfusion as a method of cerebral protection is probably the major adjunct provided to this field. However, neurological issues still remain a concern of this procedure. The possibility to minimize invasiveness using endovascular techniques will probably contribute to ameliorate the outcomes and offer a better quality of life.
Declarations
Conflict of interest
None declared.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cooley DA, Mahaffey DE, Debakey ME. Total excision of the aortic arch for aneurysm. Surg Gynecol Obstet. 1955;101:667–672. [PubMed] [Google Scholar]
- 2.Barnard CN, Schrire V. The surgical treatment of acquired aneurysm of the thoracic aorta. Thorax. 1963;18:101–115. doi: 10.1136/thx.18.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griepp RB, Stinson EB, Hollingsworth JF, Buehler D. Prosthetic replacement of the aortic arch. J Thorac Cardiovasc Surg. 1975;70:1051–1063. doi: 10.1016/S0022-5223(19)39653-9. [DOI] [PubMed] [Google Scholar]
- 4.Pierangeli A, Colì G, Mikus PM. Sostituzione dell’arco aortico in ipotermia profonda per aneurisma aterosclerotico. Bull Scienze Med. 1974;2:1–16. [Google Scholar]
- 5.McCullough JN, Zhang N, Reich DL, et al. Cerebral metabolic suppression during hypothermic circulatory arrest in humans. Ann Thorac Surg. 1999;67:1895–1899. doi: 10.1016/S0003-4975(99)00441-5. [DOI] [PubMed] [Google Scholar]
- 6.Ueda Y, Miki S, Kusuhara K, Okita Y, Tahata T, Yamanaka K. Deep hypothermic systemic circulatory arrest and continuous retrograde cerebral perfusion for surgery of aortic arch aneurysm. Eur J Cardiothorac Surg. 1992;6:36–41. doi: 10.1016/1010-7940(92)90096-G. [DOI] [PubMed] [Google Scholar]
- 7.Estrera AL, Miller CC, 3rd, Lee T-Y, Shah P, Safi HJ. Ascending and transverse aortic arch repair: the impact of retrograde cerebral perfusion. Circulation. 2008;118:S160–S166. doi: 10.1161/CIRCULATIONAHA.107.757419. [DOI] [PubMed] [Google Scholar]
- 8.Kazui T, Inoue N, Yamada O, Komatsu S. Selective cerebral perfusion during operation for aneurysms of the aortic arch: a reassessment. Ann Thorac Surg. 1992;53:109–114. doi: 10.1016/0003-4975(92)90767-X. [DOI] [PubMed] [Google Scholar]
- 9.Di Bartolomeo R, Pacini D, Di Eusanio M, Pierangeli A. Antegrade selective cerebral perfusion during operations on the thoracic aorta: our experience. Ann Thorac Surg. 2000;70:10–15. doi: 10.1016/S0003-4975(00)01400-4. [DOI] [PubMed] [Google Scholar]
- 10.Pacini D, Pantaleo A, Di Marco L, et al. Visceral organ protection in aortic arch surgery: safety of moderate hypothermia. Eur J Cardiothorac Surg. 2014;46:438–443. doi: 10.1093/ejcts/ezt665. [DOI] [PubMed] [Google Scholar]
- 11.Pacini D, Murana G, Di Marco L. Frozen elephant trunk technique: ready to get back to the future? J Thorac Cardiovasc Surg. 2018;156:e79–e80. doi: 10.1016/j.jtcvs.2018.04.071. [DOI] [PubMed] [Google Scholar]
- 12.Murana G, Di Marco L, Amodio C, et al. Use of the frozen elephant trunk technique for type B aortic dissection and aberrant right subclavian artery: an anatomic repair of the "arteria lusoria". Ann Cardiothorac Surg. 2020;9:254–256. doi: 10.21037/acs.2020.03.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Marco L, Murana G, Fiorentino M, et al. The frozen elephant trunk surgery: a systematic review analysis. Indian J Thorac Cardiovasc Surg. 2019;35:118–126. doi: 10.1007/s12055-019-00815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shrestha M, Martens A, Kruger H, et al. Total aortic arch replacement with the elephant trunk technique: single-Centre 30-year results. Eur J Cardiothorac Surg. 2014;45:181–186. doi: 10.1093/ejcts/ezt357. [DOI] [PubMed] [Google Scholar]
- 15.Cefarelli M, Murana G, Surace GG, et al. Elective aortic arch repair: factors influencing neurologic outcome in 791 patients. Ann Thorac Surg. 2017;104:2016–2023. doi: 10.1016/j.athoracsur.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Fiorentino M, de Beaufort HWL, Sonker U, Heijmen RH. Thoraflex hybrid as frozen elephant trunk in chronic, residual type A and chronic type B aortic dissection. Interact Cardiovasc Thorac Surg. 2021;32:566–572. doi: 10.1093/icvts/ivaa305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roselli EE, Idrees JJ, Bakaeen FG, et al. Evolution of simplified frozen elephant trunk repair for acute debakey type I dissection: midterm outcomes. Ann Thorac Surg. 2018;105:749–755. doi: 10.1016/j.athoracsur.2017.08.037. [DOI] [PubMed] [Google Scholar]
- 18.De Paulis R, Czerny M, Weltert L, et al. Current trends in cannulation and neuroprotection during surgery of the aortic arch in Europe. Eur J Cardiothorac Surg. 2015;47:917–923. doi: 10.1093/ejcts/ezu284. [DOI] [PubMed] [Google Scholar]
- 19.Englum BR, He X, Gulack BC, et al. Hypothermia and cerebral protection strategies in aortic arch surgery: a comparative effectiveness analysis from the STS adult cardiac surgery database. Eur J Cardiothorac Surg. 2017;52:492–498. doi: 10.1093/ejcts/ezx133. [DOI] [PubMed] [Google Scholar]
- 20.Di Marco L, Berardi M, Murana G, et al. Early outcome and mid-term survival after open arch repair using selective antegrade cerebral perfusion. Asian Cardiovasc Thorac Ann. 2021. 10.1177/02184923211028782. [DOI] [PubMed]
- 21.Czerny M, Schmidli J, Adler S, et al. Current options and recommendations for the treatment of thoracic aortic pathologies involving the aortic arch: an expert consensus document of the European Association for Cardio-Thoracic surgery (EACTS) and the European Society for Vascular Surgery (ESVS) Eur J Cardiothorac Surg. 2019;55:133–162. doi: 10.1093/ejcts/ezy313. [DOI] [PubMed] [Google Scholar]