Abstract
This quality improvement study assesses COVID-19 vaccination in dialysis clinics, vaccination coverage, and disparities from December 1, 2020, to June 13, 2021.
For patients who undergo maintenance dialysis, COVID-19 is associated with increased risk for severe illness and death.1,2,3 However, this population was not specifically recommended to be prioritized for COVID-19 vaccination.4 On March 25, 2021, a federal effort was announced to offer COVID-19 vaccinations in dialysis clinics as part of the COVID-19 Health Equity Plan.5 Two national dialysis care organizations—DaVita Inc and Fresenius Medical Care—partnered with the Centers for Disease Control and Prevention (CDC) to provide COVID-19 vaccination in their clinics and coordinate vaccine distribution to other dialysis organizations. We evaluated COVID-19 vaccination in dialysis clinics, vaccination coverage, and disparities from December 1, 2020, to June 13, 2021.
Methods
In this public health program evaluation, eligible patients had an active DaVita or Fresenius clinic admission and 1 or more in-center or home dialysis treatments between December 1, 2020, and June 13, 2021. Beginning December 2020, patients undergoing dialysis could receive COVID-19 vaccination at dialysis clinics or other locations subject to availability and local eligibility. Beginning March 29, 2021, dialysis clinics could receive federally supplied COVID-19 vaccines for in-clinic administration. Participating DaVita and Fresenius clinics (N = 5192) tracked patients’ race and ethnicity, vaccination status, and location of vaccination.
We calculated vaccination status based on 1 or more vaccine doses and examined coverage on the date preceding initiation of federal allocation (March 28, 2021) and on June 13, 2021. Proportions were compared using χ2 tests. This activity was reviewed by the CDC and conducted per applicable federal law and CDC policy.
Results
In all, 483 602 patients were included: 17.3% Hispanic, 4.1% non-Hispanic Asian, 32.1% non-Hispanic Black, 40.6% non-Hispanic White, 2.9% other, and 3.1% unknown. By June 13, 2021, 64.5% of patients had received at least 1 COVID-19 vaccine dose (Table). Before federal vaccine allocation, vaccination coverage among non-Hispanic White patients was 52.0%, exceeding that among non-Hispanic Black patients (45.2%) and similar to Hispanic patients (51.3%); non-Hispanic Asian patients had higher coverage (60.0%). By June 13, 2021, vaccination coverage among non-Hispanic Black patients approached that for non-Hispanic White patients (63.0% vs 65.5%) and was higher among non-Hispanic Asian (74.1%) and Hispanic (69.5%) patients than non-Hispanic White patients.
Table. Patients Undergoing Dialysis Who Received at Least 1 Dose of COVID-19 Vaccine by Race and Ethnicity and Datea.
| Race and ethnicity | Total patients, No. | By March 28, 2021b | By June 13, 2021c | ||
|---|---|---|---|---|---|
| Partially or fully vaccinated patients, No. (%) | P value | Partially or fully vaccinated patients, No. (%) | P value | ||
| All | 483 602 | 236 315 (48.9) | NA | 312 046 (64.5) | NA |
| Hispanic | 83 530 | 42 867 (51.3) | .001 | 58 080 (69.5) | <.001 |
| Non-Hispanicd | |||||
| Asian | 19 947 | 11 967 (60.0) | <.001 | 14 790 (74.1) | <.001 |
| Black | 155 215 | 70 150 (45.2) | <.001 | 97 739 (63.0) | <.001 |
| White | 196 235 | 102 042 (52.0) | [Reference] | 128 557 (65.5) | [Reference] |
| Othere | 13 876 | 7253 (52.3) | .54 | 9289 (66.9) | <.001 |
| Unknown | 14 799 | 2036 (13.8) | <.001 | 3591 (24.3) | <.001 |
Abbreviation: NA, not applicable.
Race and ethnicity were from patient self-report via data submitted from DaVita Inc and Fresenius Medical Care to the Centers for Disease Control and Prevention.
Date preceding the initiation of federal vaccine allocation.
End of the evaluation period.
Non-Hispanic White is the reference group for all other patient race and ethnicity categories.
Other included American Indian/Alaska Native, Native Hawaiian, Pacific Islander, and multirace.
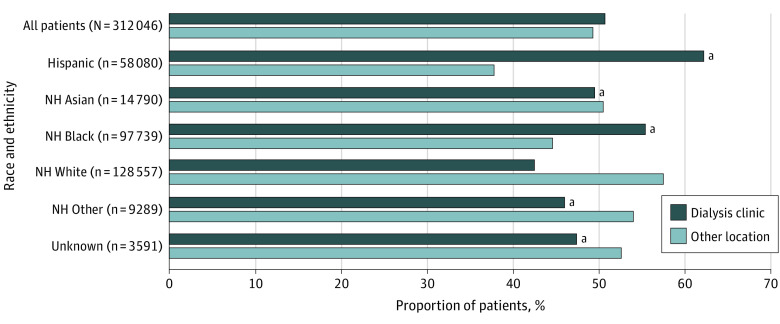
Overall, 50.7% of patients were vaccinated in a dialysis clinic (Figure). Among non-Hispanic White vaccinees, 42.5% received vaccination in a dialysis clinic; in comparison, Hispanic (62.2%), non-Hispanic Black (55.4%), and non-Hispanic Asian (49.5%) patients were more likely to receive vaccination in a dialysis clinic (P < .001 for each comparison).
Figure. Proportion of Vaccinated Patients Who Received a COVID-19 Vaccination in a Dialysis Clinic vs Other Location by Race and Ethnicity.
Race and ethnicity were from patient self-report via data submitted from DaVita Inc and Fresenius Medical Care to the Centers for Disease Control and Prevention. Non-Hispanic White is the reference group for all other patient race and ethnicity categories. Other includes American Indian/Alaska Native, Native Hawaiian, Pacific Islander, and multirace. NH indicates non-Hispanic.
aP < .001.
Discussion
Of all vaccinated patients, 50.7% were vaccinated in a dialysis clinic, and Hispanic patients had greater vaccination coverage than non-Hispanic White patients after the federal vaccine allocation increased clinic access to vaccine. Offering vaccination at the regular point of care may facilitate vaccinations in minority groups disproportionately affected by COVID-19 and may have improved vaccine access for Hispanic and Black patients.
Higher proportions of racial and ethnic minority patients than non-Hispanic White patients received vaccination in a dialysis clinic, suggesting that offering vaccines in a convenient location by a trusted source was particularly beneficial to these groups. Few other strategies have demonstrated reductions in vaccination disparities.6
This evaluation had limitations. Although we focused on partial vaccination, 90.0% of patients who received at least 1 dose were fully vaccinated by July 11, 2021. Incomplete tracking of vaccinations administered outside of dialysis clinics may have occurred. In addition, some patients had limited duration of care and opportunity for in-clinic vaccination.
The findings suggest that offering COVID-19 vaccines within dialysis clinics could reduce vaccination disparities. The federal vaccine allocation improved the ability to vaccinate high-risk patients when many states still had a limited vaccine supply. For ongoing and future vaccination efforts, public health agencies and policy makers should consider ensuring vaccine is available to dialysis clinics for onsite administration.
References
- 1.Khan MMA, Khan MN, Mustagir MG, Rana J, Islam MS, Kabir MI. Effects of underlying morbidities on the occurrence of deaths in COVID-19 patients. J Glob Health. 2020;10(2):020503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hsu CM, Weiner DE, Aweh G, et al. COVID-19 among US dialysis patients. Am J Kidney Dis. 2021;77(5):748-756.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ziemba R, Campbell KN, Yang TH, et al. Excess death estimates in patients with end-stage renal disease—United States, February-August 2020. MMWR Morb Mortal Wkly Rep. 2021;70(22):825-829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dooling K, Marin M, Wallace M, et al. The Advisory Committee on Immunization Practices’ updated interim recommendation for allocation of COVID-19 vaccine—United States, December 2020. MMWR Morb Mortal Wkly Rep. 2021;69(5152):1657-1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The White House. Fact sheet: Biden administration announces historic $10 billion investment to expand access to COVID-19 vaccines and build vaccine confidence in hardest-hit and highest-risk communities. March 25, 2021. Accessed July 28, 2021. Available at https://www.whitehouse.gov/briefing-room/statements-releases/2021/03/25/fact-sheet-biden-administration-announces-historic-10-billion-investment-to-expand-access-to-covid-19-vaccines-and-build-vaccine-confidence-in-hardest-hit-and-highest-risk-communities/
- 6.Wong CA, Pilkington W, Doherty IA, et al. Guaranteed financial incentives for COVID-19 vaccination. JAMA Intern Med. 2022;182(1):78-80. [DOI] [PMC free article] [PubMed] [Google Scholar]