Abstract
Children exhibit a broad range of clinical outcomes from SARS-CoV-2 infection, with the majority having minimal to mild symptoms. However, some succumb to a hyperinflammatory post-infectious complication, Multisystem Inflammatory Syndrome in Children, which predominantly affects previously healthy children. Studies characterizing the immunologic differences associated with these clinical outcomes have identified key pathways important for host immunity against SARS-CoV-2 and innate modulators of disease severity. Herein, we delineate the immunologic mechanisms underlying the spectrum of pediatric immune response to SARS-CoV-2 infection, with comparisons to that of adults.
Introduction
At the start of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, most children were initially spared, with very few developing moderate to severe coronavirus 2019 disease (COVID-19).1–7 As the virus spread globally, the great majority of children <18 years of age had asymptomatic infection or mild COVID-19 and hospitalization was rare.8–12 Those children that did develop severe COVID-19 generally had risk factors including underlying respiratory, neurologic and immune disorders.13 This contrasts with the susceptibility of young children to other respiratory viruses, including respiratory syncytial virus (RSV), influenza, and parainfluenza where infants and young children are highly susceptible to severe disease.14,15 In April 2020, a post-infectious syndrome known as Multisystem Inflammatory Syndrome in Children (MIS-C) emerged in patients under 21 years of age, with the majority of patients requiring intensive care for life-threatening complications. Investigating age-associated determinants of the spectrum of clinical outcomes in children and adults related to SARS-CoV-2 infection is paramount for understanding host susceptibility and outcome and could help optimize disease prevention and treatment.
This review synthesizes key principles of developmental immunology with published evidence linking immunobiology and clinical outcomes of SARS-CoV-2 infections in children and adults. We do not address neonatal SARS-CoV-2 infection, given that the many differences between host immunity during the neonatal period and subsequent developmental stages merit a separate review. Because severe COVID-19 and MIS-C are uncommon in children, sample sizes for published studies are limited. To address this, we highlight findings that are common as well as disparate across published studies, with the goal of identifying fundamental distinctions between the pediatric and adult response to SARS-CoV-2 infections. Due to the spectrum of disease associated with SARS-CoV-2 infections, We compare the immunologic response of children and adults within distinct clinical phenotypes. These include asymptomatic SARS-CoV-2 infections, mild COVID-19, characterized by the presence of upper respiratory symptoms not requiring supportive care, and symptomatic COVID-19 prompting medical attention. Within each section, we discuss the hypotheses that have been investigated to explain why children are protected from moderate to severe COVID-19 compared to older adults.
Asymptomatic SARS-CoV-2 Infection to Mild COVID-19
Overall, studies have shown that responses to asymptomatic or mild COVID-19 are largely similar between adults and children. Three studies found that the viral loads of children with asymptomatic SARS-CoV-2 or mild disease have been found to be comparable16 to, or slightly lower than that of those of adults with similarly mild infections.17,18 Jia et al. showed that the cytokine profiles of children with mild COVID-19 resembles that of healthy children, reflecting a low level of inflammation.19 Similarly, Cohen et al. found no differences in the percentages of IFN-γ CD4+ or CD8+ T cells against structural, accessory, and non-structural proteins in nine asymptomatic children compared to nine adults, with comparable capacities for generating multiple cytokines.20 This occurred despite reduced levels of cross-reactive antibodies to β-coronaviruses other than SARS-CoV-2 in children compared to adults with similarly mild infections, suggesting that differences in antecedent infections do not significantly affect the T cell response in individuals with mild SARS-CoV-2 infections.20
In parallel with a robust cellular response to SARS-CoV-2, children are capable of mounting a robust serologic response to mild SARS-CoV-2 infections. A study comparing 25 children and adolescents to 34 adults with mild COVID-19 showed that both cohorts had similar levels of anti-spike IgG with comparable functionality, including the capacity for activating complement and phagocytic cells.21 Two studies showed even higher neutralizing activity in anti-SARS-CoV-2 antibodies from children under 10 years of age, compared to adolescents and young adults.22,23 The impact of disease severity on the antibody response is indicated by lower levels of convalescent antibodies to the spike and nucleocapsid proteins in children with asymptomatic or mild infections compared to those with moderate COVID-19 requiring hospitalization.24,25 Collectively, these studies do not show major differences in the viral load or measured immune response to mild COVID-19 between children and adults, although relative few studies have investigated the immune response in individuals with asymptomatic or mild SARS-CoV-2 infections.
Moderate to severe COVID-19
In contrast to the comparable pediatric and adult immune responses during mild COVID-19, notable differences emerge in cases of patients hospitalized with COVID-19. Even though the numbers of pediatric inpatients with COVID-19 increased after spread of the Delta variant,26 most children and adolescents hospitalized for COVID-19 required shorter hospitalizations, less respiratory support, and had less mortality compared to hospitalized adults.27,28 In the United States, individuals older than 50 years of age account for at least 90% of all deaths.29 When reviewing these studies, it is important to consider that differences in immune responses could be either predictive or reflective of COVID-19 disease severity. Additionally, comorbid conditions differ between adults and children, as does alcohol and tobacco use and obesity, which all influence immune outcomes. In this section, we discuss the differences in the immune systems of children and adults that have been investigated as potential drivers of age-associated clinical outcomes from COVID-19 (Fig. 1).
Figure 1.
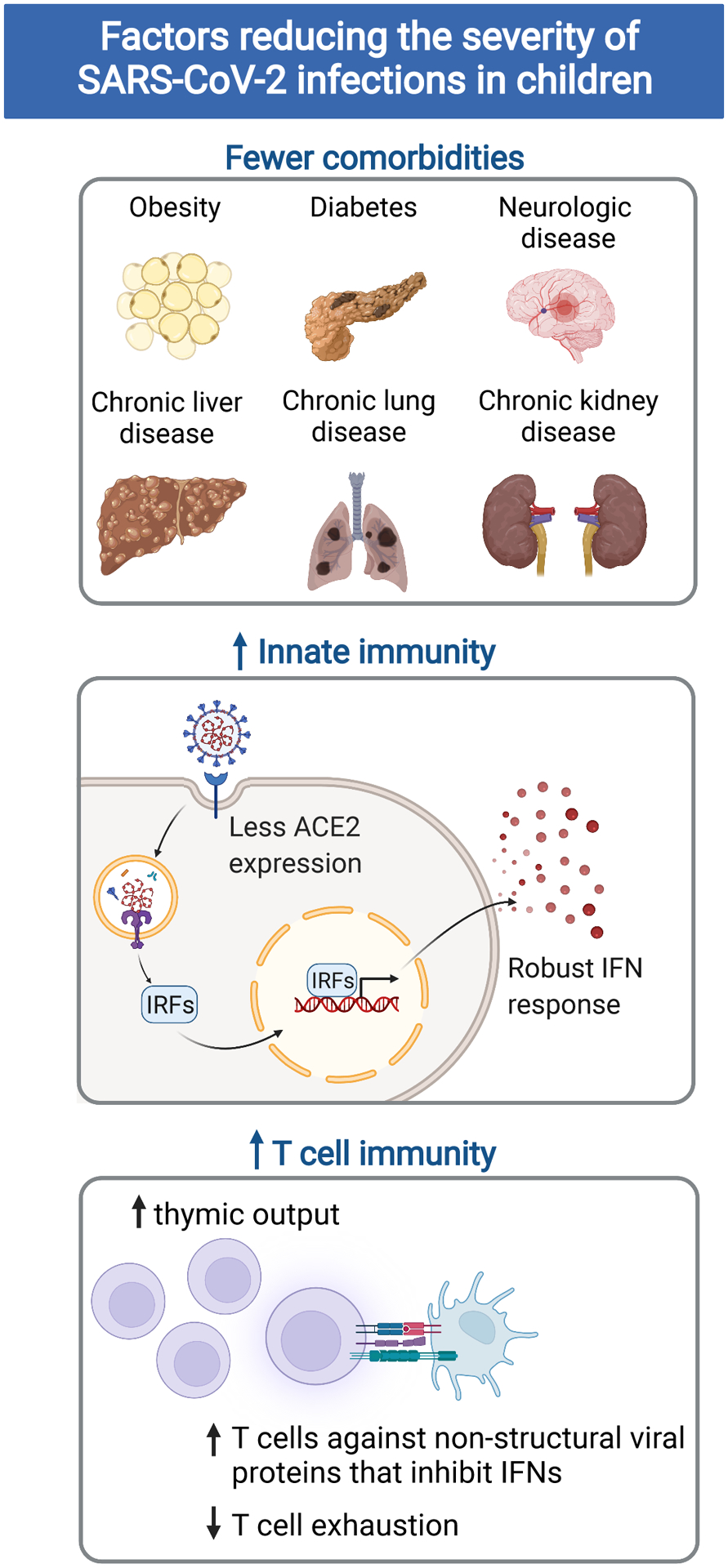
Summary of factors reducing the severity of SARS-CoV-2 infections in children
SARS-CoV-2 entry factors
Upon encountering respiratory mucosa, the receptor binding domain (RBD) of the SARS-CoV-2 spike protein binds to the widely expressed angiotensin-converting enzyme 2 (ACE2) receptor.30–32 The subsequent fusion of viral and cellular membranes is facilitated by cleavage of the viral spike protein by host proteases, such as transmembrane serine protease 2 (TMPRSS2) and cathepsin L, thereby enabling cellular entry.33,34 The expression of TMPRSS2 increases with age, and is significantly higher in the airway epithelium of healthy adults compared to that of infants.35–38 Similarly, a meta-analysis of 31 lung single-cell RNA-sequencing studies from 228 individuals without a history of lung disease showed a positive correlation between age and the expression of ACE2 in alveolar cells.39 However, distinctions in the expression of viral entry factors between children and adults are less clear: some, but not all, studies have evidence supporting the hypothesis that fewer ACE2 receptors in children may account for reduced viral entry into the lung.35,40,41
In adults with COVID-19, higher viral loads measured through naso- or oro-pharyngeal swabs have been associated with more severe disease in some, but not all studies, particularly since asymptomatic individuals may have viral loads comparable to those found in hospitalized individuals.16,42–45 While studies have found higher viral loads in symptomatic children than asymptomatic children, viral loads have not been found to be predictive of disease severity in children either.46,47 Furthermore, children and adults with similar disease severity have comparable viral loads.16,17 The variability in these studies may arise from differences in collection techniques and the inability to sample the lower respiratory tract in non-intubated patients. Nonetheless, studies have not conclusively shown that differences in viral loads account for the improved clinical outcomes seen in the majority of children with COVID-19.
Interferon signaling
While the ACE2 receptor is critical for SARS-CoV-2 entry in cells, other viral components activate widely expressed pattern recognition receptors, such as Toll-like receptors (TLR) and retinoic acid inducible gene I (RIG-I)-like receptors, to initiate the innate immune response.48 Structural proteins, such as the SARS-CoV-2 envelope protein and spike protein, are sensed by TLR2 and TLR4, respectively. Single-stranded viral genomic RNA activates TLR7/8, while the virus’s double-stranded RNA intermediates bind TLR3; cytosolic RNA is sensed by the RIG-I-like receptors.49 Activation of TLRs and RIG-I induce a robust interferon response. As a counter-regulatory mechanism, SARS-CoV2 proteins, such as ORF9b, non-structural proteins 1 and 13, and the nucleocapsid protein inhibit the host interferon response.49,50 Differences in interferon signaling has been investigated in children and adults with COVID-19. Adults with severe COVID-19 have lower circulating levels of Type I IFNs, which has been attributed to neutralizing antibodies to type I IFNs51–53 as well as reduced Type I IFN secretion from plasmacytoid dendritic cells (DCs).54,55 Pierce et al. compared the immune response in nasal secretions from 12 children and 27 adults hospitalized for moderate to severe COVID-19; the children had much milder disease than the adults, requiring no respiratory support and resulting in no mortality.40 The children exhibited increased expression of genes downstream of Type I and II IFNs and the NLR Family Pyrin Domain Containing 3 (NLRP3) inflammasome compared to the adults, but both groups had similar viral loads and levels of anti-SARS-CoV-2 IgG and IgA in nasal fluid.40 In correlating the increased IFN and inflammasome signaling in the nasal mucosa with better clinical outcomes, this study further supports the hypothesis that children are protected from severe disease due to more robust innate immunity allowing them to overcome SARS-CoV-2. One caveat is that upper respiratory samples may not reflect the cellular composition and gene expression of cells and fluid from lower airways or peripheral blood.56,57
The heightened interferon response in children does not arise exclusively from intrinsic age-associated differences in this pathway. IFN responses are reduced from the time of birth until approximately two years of age; between two to five years of life, cytokine profiles shift toward that of an adult, with increased expression of Type I IFNs, reduced IL-6 and IL-23, and increased IL-12 and IL-10.58,59 A reduction in the IFN response is seen again in adults over the age of 65 years, in part due to age-associated reductions in Interferon Regulatory Factor 8 (IRF), a transcription factor downstream of RIG-I signaling, and proteolysis of tumor receptor-associated factor 3 (TRAF3), a signaling protein utilized by multiple TLRs.60 Additionally, as individuals age, Type I IFN receptors in CD4+ T cells are more frequently complexed with Src homology region 2 domain-containing phosphatase 1 (SHP-1), an inhibitory protein tyrosine phosphatase that restrains Type I IFN signaling.61,62 Exogenous factors that reduce the IFN response also accumulate with age. These include chronic viral infections, such as human cytomegalovirus, known to cause exhaustion of plasmacytoid DCs and reduced IFN secretion, as well as anti-interferon autoantibodies.51,63–65 Although the effects of reduced IFN signaling are most pronounced in individuals over the age of 65 years, these factors progressively impair the IFN response and may contribute to the increased frequency of severe COVID-19 in middle-aged and older adults.
T cell homeostasis and activation
T cell lymphopenia in the blood and airway fluid is a marker of COVID-19 severity in both children and adults.40,57,66 In a study comparing the immune response of 65 children and young adults under the age of 24 years to 60 adults, all of whom were hospitalized for COVID-19, pediatric patients had significantly higher absolute lymphocyte counts.27 However, adults generated increased percentages of spike-specific CD4+IFN-γ+ T cells compared to children and infants.27 In another study analyzing T cell responses from 34 children and 36 adults, the overall magnitude of SARS-CoV-2-specific-CD4+ and CD8+ T cell responses were lower in the blood of children than adults.20 The targets of CD4+ T cells varied widely between children and adults, with those of adults targeting primarily structural proteins; in contrast, pediatric CD4+ T cells had a significant proportion of targets in Open Reading Frame (ORF) 1ab, which encodes 16 non-structural proteins.20 As some of these non-structural proteins are known to block the host interferon response,50 these studies raise the possibility that differences in T cell targets may contribute to the age-associated decline in the IFN response to SARS-CoV-2 infection.
Given the dynamic changes affecting T cell development throughout life, multiple age-related differences in T cell number and function likely contribute to the increased frequency of severe COVID-19 in adults compared to children. Thymic output is maximal at one year of age, and declines gradually thereafter, with negligible output occurring by approximately 85 years of age.67 The TCR repertoire is another factor that evolves throughout an individual’s lifetime. Pathogen-specific memory responses expand as infants and young children encounter new infections, including the formation of tissue resident memory T cells.68 Although studies have identified cross-reactivity between T cell recognizing the epitopes of SARS-CoV-2 and those of other human coronaviruses, no definitive correlation between clinical outcomes and T cell epitope cross-reactivity has yet emerged.69 Aging is also associated with shifts in the transcriptional profiles of T cells. Studies of aging mice kept in specific pathogen-free environments accumulate cytotoxic and effector CD4+ T cells, with increased expression of genes associated with chronic inflammation (such as S100 protein family members), the cytotoxic T cell response to viral infections (such as granzymes and the transcription factor eomesodermin), and T cell exhaustion.70 The similarities between T cell dysfunction in aging adults and in those with severe COVID-19 suggest that the gradual onset of T cell dysfunction in adulthood may set the stage for the dysfunction T cell response associated with severe COVID-19. Although studies have delved deeply into mechanisms of T cell dysfunction in the elderly,71,72 additional investigations are needed to delineate the threshold of T cell dysfunction associated with susceptibility to severe COVID-19.
Serologic responses during COVID-19
SARS-CoV-2 drives the expansion of plasmablasts and plasma cells during both mild and severe COVID-19, even beyond what is usually associated with influenza vaccination and infection.73–76 Children and adults hospitalized with COVID-19 had comparable levels of plasmablasts, regardless of need for ventilatory support.77 Increased plasmablast frequencies correlated with percentages of proliferating CD4+ T cells, rather than levels of anti-spike antibodies.77,78 Adults with acute severe COVID-19 had increased levels of neutralizing antibodies compared to titers from convalescent adults or pediatric patients with MIS-C, the latter two of which were comparable in one study.57
The differences in the serologic response to COVID-19 in children and adults are concordant with known age-associated differences in B cell development (Fig. 1). The response to T-independent antigens takes approximately two years to mature, as infants produce more IgG1 than IgG2, the latter of which preferentially recognizes polysaccharide antigens.79,80 Environmental factors also shape B cell development. Clonal expansion and somatic hypermutation begin during infancy and increase with environmental and infectious exposures.80–82 The rate of SHM can be increased, even during infancy, through exposures to infectious pathogens.81 However, it is also important to note that the severity of COVID-19 in adults also impacts the serologic response.8–12 In support of this, Bartsch et al. showed that adults with severe COVID-19 have increased titers of anti-SARS-CoV-2 IgG and IgA with more functionality in activating complement and phagocytic cells compared to either adults or children with mild SARS-CoV-2 infections.21
Antibody repertoires also evolve with age and infectious exposures. With respect to other common coronaviruses, including 229E, NL63, OC43, and KHU1, a study of 231 children and 1168 adults found that children had increased levels of antibodies against the spike, nucleocapsid, and matrix structural proteins, while a nonstructural protein of unknown function was the most common target of antibodies in adults.83 Age-associated differences in epitope reactivity have been identified in antibodies against other respiratory viruses as well, including RSV and influenza, suggesting that serologic immunity is achieved through targeting of different viral epitopes in children compared to adults.84–87 These differences have been attributed, at least in part, to original antigenic sin or immunologic imprinting, in which exposures to specific pathogen epitopes skew subsequent antibody repertoires due to the reliance of adaptive immunity on existing memory cells.87 Antigenic sin has been shown to contribute to differences in age-associated mortality with influenza virus subtypes.88–90 With response to COVID-19, no definitive associations between prior coronavirus infections and the serologic response to SARS-CoV-2. A study of 37 adults with COVID-19 found that serologic responses to the spike protein of other betacoronaviruses were inversely proportional to IgM and IgG antibodies against the spike and nucleocapsid proteins of SARS-CoV-2.91 Similarly, another study of 232 patients with COVID-19 identified a negative correlation between antibody responses to SARS-CoV-2 and other human coronaviruses.92 In contrast, another study of young and older adults hospitalized for COVID-19 (10 young adults, aged 27 to 39 years old; 20 older adults spanning 69 to 82 years of age, of whom nine required ventilation) found positive correlations between antibodies to the spike protein of other human betacoronaviruses and SARS-CoV-2; serologic memory to earlier coronaviruses did not correlate with clinical outcomes.93 Another study of 65 children and 60 adults did not find significant correlations between serologic memory to other human coronaviruses and either age or outcome.27 The heterogeneous outcomes from these studies indicates the complexity of investigating immunologic imprinting in diverse human populations with a broad range of environmental and infectious exposures; future studies with animal models of serial viral infections may provide more definitive conclusions.
Summary of mechanisms increasing the prevalence of severe COVID-19 in adults
Collectively, these studies show that developmental differences in innate and adaptive immunity, particularly those relating to IFN signaling and T cell function, likely contribute to the increased susceptibility to severe COVID-19 in adults. In support of this, the prevalence of severe COVID-19 was higher in immunodeficient cohorts enriched in disorders of T cell development and/or function,94–96 compared to that of the general pediatric population or cohorts of patients with a broader diversity of primary or secondary immunodeficiencies, such as antibody deficiencies, autoimmune disorders, and use of immunosuppressive medications.6,97,98 This parallels increased mortality from COVID-19 in the elderly, another population with reduced T cell number and function.99,100 Notably, co-morbidities associated with severe COVID-19,101 including cardiovascular disease, diabetes, malignancies, renal failure, and neurodegenerative disease, occur more frequently in adults than children. Certain chronic diseases, such as cerebrovascular disease, obesity, and diabetes, result in a dysfunctional immune response to infections through epigenetic and metabolic reprogramming of immune activation.102–104 Other comorbidities, such as chronic lung disease, may result in anatomic susceptibility to more severe COVID-19. When present in children and young adults, these comorbidities also increase the risk of severe COVID-19.6,9,10,13,105
Multisystem Inflammatory Syndrome in Children (MIS-C)
In April 2020, during the wake of viral surges occurring in Italy and the United Kingdom,106–109 children presented with mucocutaneous features resembling Kawasaki disease (KD) and/or toxic shock syndrome. Soon after, descriptive reports by Feldstein et al. and Dufort et al., totaling almost 300 U.S. cases, confirmed that the timing was approximately 4 weeks after the peak of SARS-CoV-2 activity in a region.110,111 This disease entity is now referred to as pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS)108 or Multisystem Inflammatory Syndrome in Children (MIS-C).112 The diagnostic criteria from the Centers for Disease Control and Prevention for MIS-C include at least 24 hours of fever and inflammation severe enough to affect at least two organ systems and require hospitalization. These symptoms must occur within four weeks of SARS-CoV-2 infection or exposure to COVID-19 in an individual younger than 21 years of age who has no alternative diagnosis for these symptoms.112 At least 75% of children in published cohorts have positive SARS-CoV-2 antibody testing, but fewer (up to 52%) have positive respiratory testing, suggesting the post-infectious timing of MIS-C.109–111,113 Milder symptoms of MIS-C include fevers, rashes, and gastrointestinal symptoms, but can progress to life-threatening cytopenias, coagulopathy, myocardial dysfunction, coronary aneurysms, and/or shock.1–5 The majority of children diagnosed with MIS-C were previously healthy, but critically ill mostly due to shock and/or left ventricular dysfunction, with less severe or no respiratory involvement.110,111 Approximately 40% of the patients met criteria for KD, a vasculitic syndrome associated with coronary artery aneurysms. In a study of over 1,000 children with MIS-C or severe COVID-19, those with MIS-C were more likely to have cardiovascular and/or mucocutaneous involvement, with higher CRP levels and a neutrophil to lymphocyte ratios.113 Compared to children and adolescents with acute COVID-19, MIS-C is more likely to affect those between six and 12 years of age, rather than younger or older patients.113,114 MIS-C has been reported in Europe, North and South America, the Middle East, South Africa, and South Asia.115 Relatively fewer cases have been reported from East Asia which has a high frequency of Kawasaki disease, and it is unclear if this is due to differences in the genetic background of local populations or environmental conditions.115,116 In the U.S., non-Hispanic Black children may be at higher risk of developing MIS-C than acute COVID-19, compared to non-Hispanic White patients.113,114
Analogously, multisystem inflammation in adults (MIS-A) has been reported in individuals 21 years or older.117–123 The diagnosis of MIS-A differs from that of MIS-C in that patients with MIS-A cannot have severe respiratory disease, thereby differentiating this disease from severe COVID-19 in adults.124 Additionally, the diagnosis of MIS-A requires hospitalization for at least one extra-pulmonary complication occurring within 12 weeks of SARS-CoV-2 infection. In a study of 839 adults hospitalized with SARS-CoV-2 infection, 11.7% were diagnosed with MIS-A.117 Patients with MIS-A were younger than those with COVID-19, with a median age of 45.1 years for the MIS-A cohort compared to 56.5 years for COVID-19 patients.117 No other differences in demographics or other comorbidities were found between adults with MIS-A and those with COVID-19.117 As the immunologic features of MIS-A are largely not understood, and there is believed to be overlap with acute COVID-19 with cardiovascular involvement,117,121 the remainder of this section will focus on the immunobiology underlying MIS-C with comparisons to COVID-19 in children and adults.
Cellular activation affecting multiple hematopoietic lineages is a consistent feature of MIS-C. High levels of inflammatory cytokines, including IFN-α, IFN-γ, IL-1β, IL-6, IL-8, IL-10, IL-17, have been identified in all studies of MIS-C,125–131 but no single archetypal cytokine signature of MIS-C has emerged. Evidence of myeloid cell activation in patients with MIS-C include increased expression of CD64 on monocytes and neutrophils as well as the alarmin-related S100A genes, both of which are also elevated in adults with severe COVID-19.125,132 NK cells from patients with MIS-C also exhibit evidence of increased activation, with higher expression of perforin and granzymes compared to controls.132 Single cell RNA-seq of peripheral blood mononuclear cells from eight children with MIS-C, compared to four children with COVID-19 pneumonia and nine controls, showed that those with MIS-C and COVID-19 had similarly increased expression of genes downstream of inflammatory cytokines (Type I/II IFNs, IL-1, IL-6, and IL-17) and NF-κB activation, even though all patients with MIS-C had been treated with immunomodulatory therapies prior to study enrollment.131 The inflammatory signature in the MIS-C cohort was restricted to monocytes and dendritic cells, highlighting the contributions of these cells to the systemic inflammation characteristic of MIS-C.131
Commensurate with multi-lineage immune activation, patients with MIS-C have evidence of tissue inflammation, including increased gastrointestinal permeability, schistocytes and elevated circulating levels of complement C5b9 indicative of microangiopathy, and release of troponin and natriuretic peptides indicative of cardiac inflammation.109–111,113,126,129,130,133 Patients with MIS-C may have mucocutaneous inflammation and coronary artery aneurysms, features characteristic of Kawasaki disease. However, studies have identified distinctions between the immunologic abnormalities associated with these diseases. Compared to patients with KD, those with MIS-C have more severe lymphopenia, neutropenia, and thrombocytopenia as well as increased expression of T cell activation markers, including HLA-DR and CD57, a marker of CD4+ T cell senescence.126,127 Circulating levels of Discoidin as well as CUB And LCCL Domain Containing 2 (DCBLD2), a protein associated with endothelial damage, are higher in patients with KD than MIS-C,127 reflecting the more frequent coronary artery involvement in KD.126 These differences may explain why the great majority of coronary artery aneurysms in MIS-C resolve within 30 days, which contrasts with the persistent aneurysms associated with KD.
T cells have been investigated for their role in MIS-C pathogenesis. In patients with MIS-C, lymphopenia appeared to be a general feature in the acute phase of disease.134 One study found a strong enrichment for patrolling CX3CR1+CD8+ T cells, potentially contributing to the vascular manifestations of MIS-C.77 PD1+CD39+CD8+ T cells were also elevated, nominally higher than levels in adults with severe disease, indicative of prolonged activation and TCR signaling. Three separate studies, each with unique cohorts of children with MIS-C, identified pronounced skewing of the T cell receptor (TCR) Vβ repertoire,132,135,136 with up to 24% of the sequenced clones expressing the TRBV11-2 V-region (Vβ21.3) in one study.136 The polyclonal nature of this expansion, highlighted in two studies,135,136 is suggestive of superantigen-driven activation. Concordant with these findings, a superantigen-like motif has been identified in the SARS-CoV-2 spike protein sequence.137 TCR skewing has been similarly identified in adults with severe COVID-19, although the Vβ signatures identified in adults with severe COVID-19 appears to differ, thus far, from those found in patients with MIS-C.137,138 In contrast, TRBV11-2 enrichment was not observed in subjects with mild SARS-CoV-2, KD, toxic shock syndrome, or age-matched febrile controls.132,135,136 After resolution of the disease, the repertoire of T cells from children with MIS-C re-normalized in distribution.132 In light of the skewed TCR repertoires evident in some patients with MIS-C, studies have investigated post-infectious sources of antigens.130,139 Given the frequency of gastrointestinal symptoms in patients with MIS-C,6,108–110,113 it has been hypothesized that the gastrointestinal tract may serve as a reservoir for SARS-CoV-2,130,139,140 as the virus is known to infect gut enterocytes.141 Compared to controls and children with COVID-19, a single-center cohort of 19 patients with MIS-C investigated by Yonker et al. had evidence of significantly increased gastrointestinal permeability and increased circulating levels of SARS-CoV-2 spike protein and the S1 subunit, the latter of which correlated with TRBV11-2 expression.130 Additional studies with larger, multi-center MIS-C cohorts are needed to determine the generalizability of these findings.
The serologic features of MIS-C reflect the post-infectious timing of this disease. Patients with MIS-C have IgG antibodies to SARS-CoV-2 with levels and neutralizing capacity similar to those of convalescent adults, irrespective of concomitant RT-PCR positivity.21,128 Additionally, higher levels of total and neutralizing antibodies against the spike and RBC proteins have been found in children with MIS-C compared to those with acute COVID-19.142 These findings suggest that the nasopharyngeal load of virus reflects an antecedent, rather than acute, infection.128,133 In addition to robust antibody responses to SARS-CoV-2, children with MIS-C have a concomitant expansion of antibodies against other common viruses, including common coronaviruses, influenza, respiratory syncytial viruses, Epstein-Barr virus.21 This is similar to the antibody profiles of non-hospitalized adult patients with mild to moderate COVID-19; in contrast, adults with severe COVID-19 requiring hospitalization have more limited expansion of antibodies to pathogens other than SARS-CoV-2.21,92 The cause of differences in the breadth of the serologic response are not known, but studies have hypothesized that the attenuated immunity with aging leads to a narrower humoral response during SARS-CoV-2 infection.92 In concordance with this, patients with MIS-C exhibit increased frequencies of proliferating CD27+CD38+ plasmablasts, which correlated with increased percentages of proliferating CD4+ T cells – a feature that diminishes with age.77,78
Differences in age-associated morbidity and mortality to subtypes of respiratory viruses has prompted investigations of how exposure to other coronavirus infections affects susceptibility to MIS-C. A small study of three children with MIS-C identified a lack of antibodies against common human coronaviruses HKU1 and betacoronavirus 1.127 However, subsequent studies have identified comparable or increased levels antibodies against HKU1 and other seasonal coronaviruses in children hospitalized with either MIS-C, compared to those with acute COVID-19 and healthy children, with no consistent correlation across studies in the relationship between antibodies against seasonal coronaviruses and neutralizing antibodies to SARS-CoV-2.143,144
The end organ inflammation characteristic of MIS-C has prompted studies to investigate the contributions of autoantibodies to the pathogenesis of MIS-C. Increased levels of circulating autoantibodies have been identified in patients with MIS-C,127,128,132 including in samples taken prior to administration of IVIG. The spectrum of autoantibodies targets antigens enriched in endothelial cells and the gastrointestinal tract, those associated with rheumatologic disorders (systemic lupus erythematosus, Sjogren’s disease, and idiopathic inflammatory myopathies), and those against widely expressed tissue antigens (MAP2K2 and members of the casein kinase family).127,128,132 Additionally, two studies have found evidence of B cell clonal expansion in patients with MIS-C,132,145 with the study by Porritt et al. showing that a higher frequency of immunoglobulin heavy chain genes associated with autoimmune disorders in patients with TRBV11-2 expression.145 Notably, studies of children with MIS-C have not identified autoantibodies against IFN or interferon stimulated genes,131,146 thus differentiating autoantibodies in children with MIS-C from those found in adults with severe COVID-19.51,65
Genetic risk factors associated with susceptibility to MIS-C are also distinct from those associated with severe COVID-19 in adults. Multiple studies of adults with severe COVID-19 have identified an association between severe COVID-19 and loss of function variants in TLR7, a sensor for SARS-CoV-2 single stranded RNA.147–150 TLR7 signaling promotes IFN signaling, the secretion of IL-6, IL-1β, and IL-23, and the generation of Th17 T cells in response to viral infections.151,152 Thus, reduced function of TLR7, which is located on the X chromosome, is one mechanism contributing to the increased prevalence of severe COVID-19 in men compared to women.153–155 In contrast to these risk variants for COVID-19, variants impairing negative regulators of inflammation have been found in patients with MIS-C.156,157 These include SOCS1 (encoding Suppressor of Cytokine Signaling 1), XIAP (encoding X-linked Inhibitor of Apoptosis), and CYBB (encoding cytochrome b-245, beta subunit).157 Even seven months after recovery, patients with these genetic risk variants exhibited transcriptional evidence of increased interferon and inflammatory signaling, thus constituting a counterpoint to the reduced IFN signature associated with severe COVID-19 in adults. Extending beyond monogenic risk factors, studies have identified HLA class I alleles as factors potentially increasing a child’s risk of MIS-C. In the study by Porritt et al., which had a predominance of Hispanic patients from the U.S., four of seven patients with MIS-C had TRBV11-2 expansion and all four also shared the HLA class I alleles A02, B35, and C04,135 In contrast, this was not found in the sub-cohort of HLA genotyped patients presented by Moreews et al., which was comprised predominantly of children from Afro-Caribbean backgrounds.136 Thus, larger cohort studies will be necessary to quantify the association between HLA genotype on the susceptibility to MIS-C.
In summary, studies have shown that the post-infectious timing and broad hyperactivity of both innate and adaptive immunity distinguish MIS-C from severe COVID-19 in children and adults,77,133 as well as KD and macrophage activation syndrome.126,128 Many questions remain regarding genetic and environmental risk factors, since MIS-C most often occurs in previously healthy school-aged children who have been exposed to a diversity of infectious pathogens in group care and school settings. Triggers for MIS-C onset remain unknown, and it is challenging to distinguish driver pathways in MIS-C from those activated as a result of disease progression. Overall, immunity in older children and adolescents is an understudied area and MIS-C may provide the impetus for future studies of the immune response in these pediatric age groups.
Limitations of research generated during a pandemic
Many limitations of the studies presented here arise from challenges inherent in a pandemic. Worldwide, clinicians faced unpredictable barriers in providing medical care due to supply chain shortages and viral surges,158 rendering it even more difficult for investigators to obtain biospecimens. This was further compounded by the fact that many parents of children hospitalized with COVID-19 are ill themselves, and unable to provide consent for their child to participate in research, and critically ill COVID-19 adults are unable to consent. There was no precedent for use of deferred consent in a pandemic, which could have helped with obtaining early samples in adults and children.159
The enrollment of children in research studies has additional complexities, including limitations on blood volume, and smaller sample sizes due to the lower prevalence of SARS-CoV-2-associated complications in pediatric populations compared to adult cohorts.160 The relative rarity of intubation required for children with COVID-19 limited the amount of pediatric bronchial lavage samples available, prompting the use of nasopharyngeal samples as surrogates. The viral load, immune cell composition, and gene expression profiles of nasal and airway samples are distinct and not interchangeable.56 Differences in the inflammatory response observed in cells obtained from bronchial samples compared to peripheral blood suggest that high-resolution immune studies of circulating and tissue-resident cells would enable a more complete understanding of COVID-19 or MIS-C pathogenesis.161
Studies showing the real-world effectiveness of intravenous immunoglobulin and glucocorticoids for the treatment of MIS-C prompted rapid initiation of treatment in children with MIS-C,113,162,163 and thus, most studies utilized samples from pre-treated children. The immunomodulatory treatments given to patients with MIS-C affects the transcriptional signature of immune cells, as seen in longitudinal studies of MIS-C.77,125,127 Finally, differences in processing methodologies among research studies, including types of anti-coagulants used, timing of sample processing and freezing, affect measurements of circulating cytokines, a parameter investigated in most studies of SARS-CoV-2.164 Historically, these types of limitations have been overcome by utilizing animal models of disease to confirm the findings from patient studies. However, due to interspecies differences in the susceptibility and response to SARS-CoV-2 infection, there are no animal models that recapitulate the two most severe manifestations of SARS-CoV-2 infection in humans, acute respiratory distress syndrome or MIS-C.165
Concluding remarks
Collectively, these studies show that the immune response of children and adults to mild SARS-CoV-2 infection are similar, but diverge upon development of severe disease (Fig. 2). Adults with severe COVID-19 may have loss of immune synchrony: T cell lymphopenia, reduced circulating T follicular helper cells, and impaired IFN-mediated signaling juxtaposed with high frequencies of activated SARS-CoV-2-specific T cells, robust humoral responses, and myeloid cell activation. In contrast, patients with MIS-C exhibit multilineage immune cell activation beyond that of pediatric or adult COVID-19, as evidenced by greater IFN and inflammasome signaling, widespread T cell activation, and activation of a broad humoral response reactive to common viruses as well as SARS-CoV-2. These differences in the immunologic profiles point to many unanswered questions.
Figure 2.
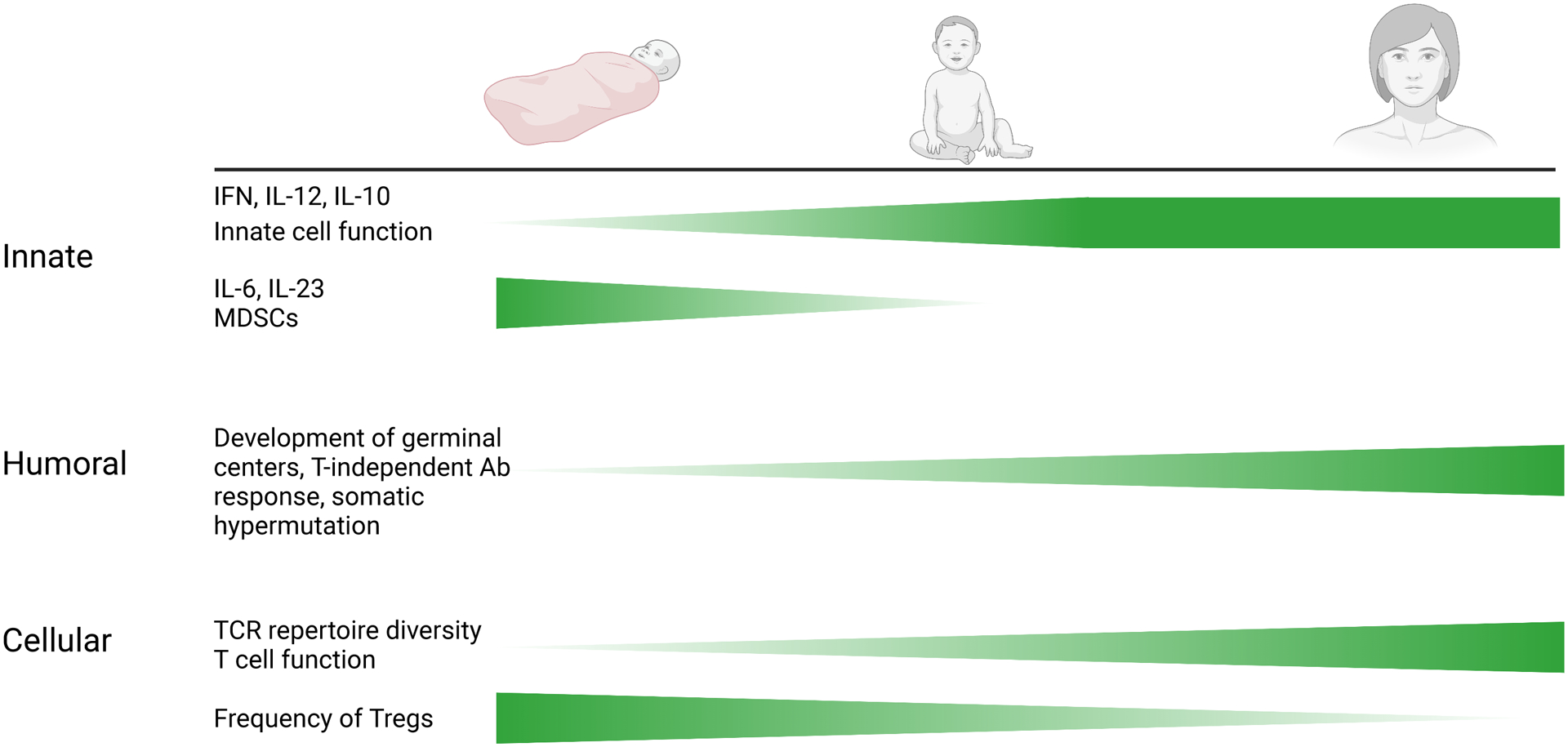
Key developmental differences in pediatric and adult immune mechanisms against viral infections.
The association of severe COVID-19 in children and adults with pre-existing medical conditions underscores the contributions of these comorbidities to disease severity. However, the impact of these comorbidities on immune synchrony are incompletely understood. Studies of pediatric populations in multiple countries have shown that SARS-CoV-2 infections across the developmental spectrum encompassing the neonatal period through adolescence are mostly asymptomatic or mild, despite developmental differences in immunity, variations in genetic background, and diversity of living environments. This suggests that developmental immaturity in host immunity is not, in and of itself, a risk factor for severe COVID-19 or MIS-C. Although studies have started to identify demographic and genetic risk factors for MIS-C, the constellation of factors that lead to MIS-C remains largely undefined. Diagnosis of MIS-C will become more challenging as more of the pediatric population becomes SARS-CoV-2 antibody positive through prior infection or vaccination. The spread of viral variants among unvaccinated pediatric populations may also change the spectrum of disease in children. The solutions to these questions will emerge as scientists and clinicians continue to develop multi-center studies with larger cohorts alongside new tools for investigating SARS-CoV-2 pathogenesis.
Figure 3.
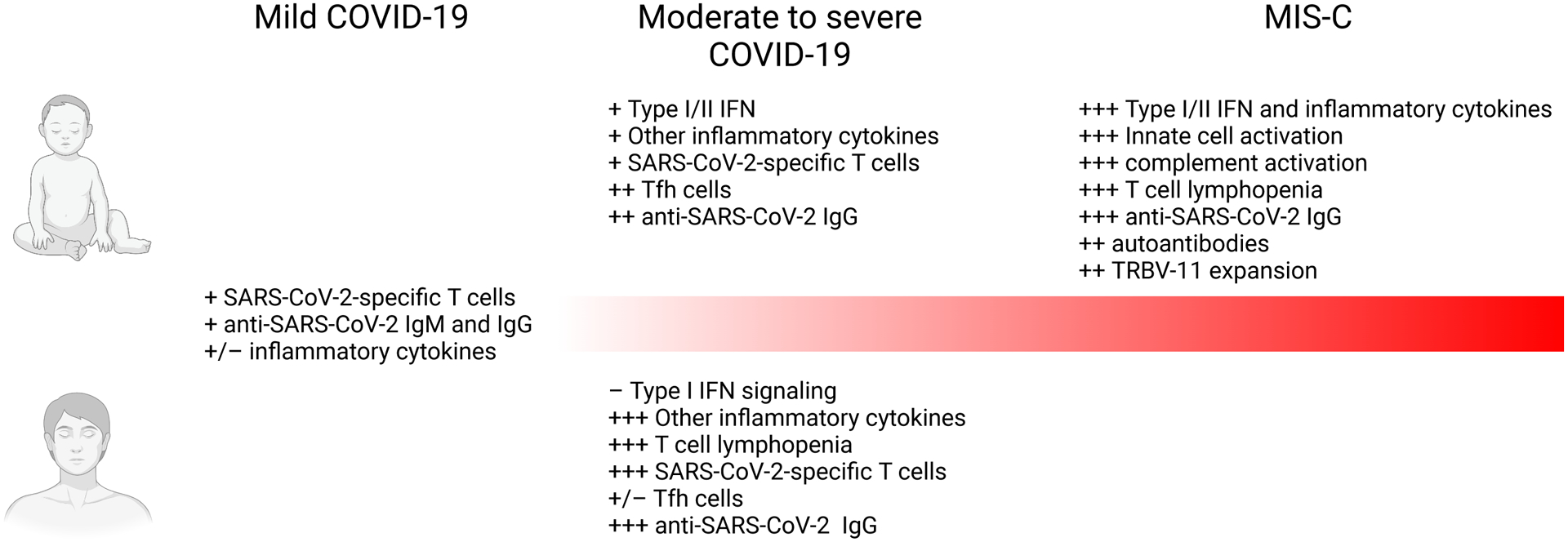
Comparison of differences in the immune response to SARS-CoV-2 in children and adults, across the spectrum of disease severity.
Acknowledgements
This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK130465 to JC), National Institute of Allergy and Infectious Diseases (R01AI139633-04S1 to JC, R01AI154470 to PT, AR), by ALSAC at St. Jude (PT), the Center for Influenza Vaccine Research for High-Risk Populations (CIVR-HRP) contract number 75N93019C00052 (PT), the St. Jude Center of Excellence for Influenza Research and Surveillance (PT), HHSN272201400006C, and 3U01AI144616-02S1 (PT), and the Perkin Foundation (JC).
Footnotes
Competing interests statement
P.G.T. serves on the Scientific Advisory Board of Immunoscape and Cytoagents. The other authors declare no competing interests.
References
- 1.Gudbjartsson DF et al. Spread of SARS-CoV-2 in the Icelandic Population. New England Journal of Medicine 382, 2302–2315 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pan X et al. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. The Lancet Infectious Diseases 20, 410–411 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jiehao C et al. A Case Series of Children With 2019 Novel Coronavirus Infection: Clinical and Epidemiological Features. Clin Infect Dis 71, 1547–1551 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu X et al. SARS-CoV-2 Infection in Children. N Engl J Med 382, 1663–1665 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grasselli G et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 323, 1574–1581 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Götzinger F et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. The Lancet Child & Adolescent Health 4, 653–661 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saatci D et al. Association Between Race and COVID-19 Outcomes Among 2.6 Million Children in England. JAMA Pediatrics 175, 928–938 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Viner RM et al. Susceptibility to SARS-CoV-2 Infection Among Children and Adolescents Compared With Adults: A Systematic Review and Meta-analysis. JAMA Pediatrics 175, 143–156 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsankov BK et al. Severe COVID-19 Infection and Pediatric Comorbidities: A Systematic Review and Meta-Analysis. International Journal of Infectious Diseases 103, 246–256 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Preston LE et al. Characteristics and Disease Severity of US Children and Adolescents Diagnosed With COVID-19. JAMA Network Open 4, e215298–e215298 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dewi R et al. Mortality in children with positive SARS-CoV-2 polymerase chain reaction test: Lessons learned from a tertiary referral hospital in Indonesia. International Journal of Infectious Diseases 107, 78–85 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Velásquez SR et al. The toll of COVID-19 on African children: A descriptive analysis on COVID-19-related morbidity and mortality among the pediatric population in Sub-Saharan Africa. International Journal of Infectious Diseases 110, 457–465 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shekerdemian LS et al. Characteristics and Outcomes of Children With Coronavirus Disease 2019 (COVID-19) Infection Admitted to US and Canadian Pediatric Intensive Care Units. JAMA Pediatr (2020) doi: 10.1001/jamapediatrics.2020.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kenmoe S et al. Systematic review and meta-analysis of the prevalence of common respiratory viruses in children < 2 years with bronchiolitis in the pre-COVID-19 pandemic era. PLOS ONE 15, e0242302 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang X et al. Global burden of respiratory infections associated with seasonal influenza in children under 5 years in 2018: a systematic review and modelling study. The Lancet Global Health 8, e497–e510 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones TC et al. Estimating infectiousness throughout SARS-CoV-2 infection course. Science 373, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chung E et al. Comparison of Symptoms and RNA Levels in Children and Adults With SARS-CoV-2 Infection in the Community Setting. JAMA Pediatrics (2021) doi: 10.1001/jamapediatrics.2021.2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madera S et al. Nasopharyngeal SARS-CoV-2 viral loads in young children do not differ significantly from those in older children and adults. Sci Rep 11, 3044 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jia R et al. Mild Cytokine Elevation, Moderate CD4+ T Cell Response and Abundant Antibody Production in Children with COVID-19. Virol Sin 35, 734–743 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen CA et al. SARS-CoV-2 specific T cell responses are lower in children and increase with age and time after infection. Nat Commun 12, 4678 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bartsch YC et al. Humoral signatures of protective and pathological SARS-CoV-2 infection in children. Nat Med 27, 454–462 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garrido C et al. Asymptomatic or mild symptomatic SARS-CoV-2 infection elicits durable neutralizing antibody responses in children and adolescents. JCI Insight (2021) doi: 10.1172/jci.insight.150909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang HS et al. Association of Age With SARS-CoV-2 Antibody Response. JAMA Network Open 4, e214302–e214302 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Méndez-Echevarría A et al. Long-Term Persistence of Anti-SARS-CoV-2 Antibodies in a Pediatric Population. Pathogens 10, 700 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oygar PD et al. Longitudinal Follow-up of Antibody Responses in Pediatric Patients With COVID-19 up to 9 Months After Infection. Pediatr Infect Dis J 40, e294–e299 (2021). [DOI] [PubMed] [Google Scholar]
- 26.Delahoy MJ Hospitalizations Associated with COVID-19 Among Children and Adolescents — COVID-NET, 14 States, March 1, 2020–August 14, 2021. MMWR Morb Mortal Wkly Rep 70, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pierce CA et al. Immune responses to SARS-CoV-2 infection in hospitalized pediatric and adult patients. Science Translational Medicine 12, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Laxminarayan R et al. Epidemiology and transmission dynamics of COVID-19 in two Indian states. Science 370, 691–697 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.COVID-19 Provisional Counts - Weekly Updates by Select Demographic and Geographic Characteristics. https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm (2021). [Google Scholar]
- 30.Wan Y, Shang J, Graham R, Baric RS & Li F Receptor Recognition by the Novel Coronavirus from Wuhan: an Analysis Based on Decade-Long Structural Studies of SARS Coronavirus. Journal of Virology 94, e00127–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou P et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579, 270–273 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shang J et al. Structural basis of receptor recognition by SARS-CoV-2. Nature 581, 221–224 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Walls AC et al. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell 181, 281–292.e6 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ou X et al. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat Commun 11, 1620 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schuler BA et al. Age-determined expression of priming protease TMPRSS2 and localization of SARS-CoV-2 in lung epithelium. Journal of Clinical Investigation 131, e140766 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang A et al. Single-cell multiomic profiling of human lungs reveals cell-type-specific and age-dynamic control of SARS-CoV2 host genes. eLife 9, e62522 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Letko M, Marzi A & Munster V Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol 5, 562–569 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hoffmann M et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 181, 271–280.e8 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Muus C et al. Single-cell meta-analysis of SARS-CoV-2 entry genes across tissues and demographics. Nat Med 27, 546–559 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pierce CA et al. Natural mucosal barriers and COVID-19 in children. JCI Insight 6, e148694 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bunyavanich S, Do A & Vicencio A Nasal Gene Expression of Angiotensin-Converting Enzyme 2 in Children and Adults. JAMA 323, 2427–2429 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heald-Sargent T et al. Age-Related Differences in Nasopharyngeal Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Levels in Patients With Mild to Moderate Coronavirus Disease 2019 (COVID-19). JAMA Pediatr 174, 902 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fajnzylber J et al. SARS-CoV-2 viral load is associated with increased disease severity and mortality. Nature Communications 11, 5493 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Argyropoulos KV et al. Association of Initial Viral Load in Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Patients with Outcome and Symptoms. Am J Pathol 190, 1881–1887 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yang Q et al. Just 2% of SARS-CoV-2−positive individuals carry 90% of the virus circulating in communities. PNAS 118, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aykac K et al. The association of viral load and disease severity in children with COVID-19. Journal of Medical Virology 93, 3077–3083 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim C et al. COVID-19 infection with asymptomatic or mild disease severity in young patients: Clinical course and association between prevalence of pneumonia and viral load. PLOS ONE 16, e0250358 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zheng M et al. TLR2 senses the SARS-CoV-2 envelope protein to produce inflammatory cytokines. Nat Immunol 22, 829–838 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Anaeigoudari A, Mollaei HR, Arababadi MK & Nosratabadi R Severe Acute Respiratory Syndrome Coronavirus 2: The Role of the Main Components of the Innate Immune System. Inflammation (2021) doi: 10.1007/s10753-021-01519-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xia H & Shi P-Y Antagonism of Type I Interferon by Severe Acute Respiratory Syndrome Coronavirus 2. Journal of Interferon & Cytokine Research 40, 543–548 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bastard P et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science 370, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lemarquis A et al. Severe COVID-19 in an APS1 patient with interferon autoantibodies treated with plasmapheresis. Journal of Allergy and Clinical Immunology 148, 96–98 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bastard P et al. Preexisting autoantibodies to type I IFNs underlie critical COVID-19 pneumonia in patients with APS-1. Journal of Experimental Medicine 218, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hadjadj J et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science 369, 718–724 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Arunachalam PS et al. Systems biological assessment of immunity to mild versus severe COVID-19 infection in humans. Science 369, 1210–1220 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Broggi A et al. Type III interferons disrupt the lung epithelial barrier upon viral recognition. Science 369, 706–712 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Weisberg SP et al. Distinct antibody responses to SARS-CoV-2 in children and adults across the COVID-19 clinical spectrum. Nat Immunol 22, 25–31 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nguyen M et al. Acquisition of Adult-Like TLR4 and TLR9 Responses during the First Year of Life. PLoS One 5, e10407 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Holt PG et al. Developmental regulation of type 1 and type 3 interferon production and risk for infant infections and asthma development. Journal of Allergy and Clinical Immunology 143, 1176–1182.e5 (2019). [DOI] [PubMed] [Google Scholar]
- 60.Molony RD et al. Aging impairs both primary and secondary RIG-I signaling for interferon induction in human monocytes. Science Signaling 10, eaan2392 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li G, Ju J, Weyand CM & Goronzy JJ Age-Associated Failure To Adjust Type I IFN Receptor Signaling Thresholds after T Cell Activation. J.I. 195, 865–874 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Le Page A et al. Downregulation of inhibitory SRC Homology 2 Domain-containing Phosphatase-1 (SHP-1) leads to recovery of T cell responses in elderly. Cell Communication and Signaling 12, 2 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Macal M et al. Self-Renewal and Toll-like Receptor Signaling Sustain Exhausted Plasmacytoid Dendritic Cells during Chronic Viral Infection. Immunity 48, 730–744.e5 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zuniga EI, Liou L-Y, Mack L, Mendoza M & Oldstone MBA Persistent Virus Infection Inhibits Type I Interferon Production by Plasmacytoid Dendritic Cells to Facilitate Opportunistic Infections. Cell Host & Microbe 4, 374–386 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.van der Wijst, M. G. P. et al. Type I interferon autoantibodies are associated with systemic immune alterations in patients with COVID-19. Science Translational Medicine (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen Z & John Wherry E T cell responses in patients with COVID-19. Nat Rev Immunol 20, 529–536 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bains I, Thiébaut R, Yates AJ & Callard R Quantifying Thymic Export: Combining Models of Naive T Cell Proliferation and TCR Excision Circle Dynamics Gives an Explicit Measure of Thymic Output. The Journal of Immunology 183, 4329–4336 (2009). [DOI] [PubMed] [Google Scholar]
- 68.Kumar BV, Connors TJ & Farber DL Human T Cell Development, Localization, and Function throughout Life. Immunity 48, 202–213 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mateus J et al. Selective and cross-reactive SARS-CoV-2 T cell epitopes in unexposed humans. Science 370, 89–94 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Elyahu Y et al. Aging promotes reorganization of the CD4 T cell landscape toward extreme regulatory and effector phenotypes. Science Advances 5, eaaw8330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tu W & Rao S Mechanisms Underlying T Cell Immunosenescence: Aging and Cytomegalovirus Infection. Frontiers in Microbiology 7, 2111 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nikolich-Žugich J Ageing and life-long maintenance of T-cell subsets in the face of latent persistent infections. Nat Rev Immunol 8, 512–522 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Turner JS et al. SARS-CoV-2 infection induces long-lived bone marrow plasma cells in humans. Nature 595, 421–425 (2021). [DOI] [PubMed] [Google Scholar]
- 74.Mathew D et al. Deep immune profiling of COVID-19 patients reveals distinct immunotypes with therapeutic implications. Science 369, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mudd PA et al. Distinct inflammatory profiles distinguish COVID-19 from influenza with limited contributions from cytokine storm. Sci Adv 6, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kuri-Cervantes L et al. Comprehensive mapping of immune perturbations associated with severe COVID-19. Sci. Immunol 5, eabd7114 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Vella LA et al. Deep immune profiling of MIS-C demonstrates marked but transient immune activation compared to adult and pediatric COVID-19. Science Immunology 6, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ramaswamy A et al. Immune dysregulation and autoreactivity correlate with disease severity in SARS-CoV-2-associated multisystem inflammatory syndrome in children. Immunity 54, 1083–1095.e7 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pollard AJ, Perrett KP & Beverley PC Maintaining protection against invasive bacteria with protein–polysaccharide conjugate vaccines. Nat Rev Immunol 9, 213–220 (2009). [DOI] [PubMed] [Google Scholar]
- 80.Nielsen SCA et al. Shaping of infant B cell receptor repertoires by environmental factors and infectious disease. Sci Transl Med 11, eaat2004 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wendel BS et al. Accurate immune repertoire sequencing reveals malaria infection driven antibody lineage diversification in young children. Nat Commun 8, 531 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Olin A et al. Stereotypic Immune System Development in Newborn Children. Cell 174, 1277–1292.e14 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Khan T et al. Distinct antibody repertoires against endemic human coronaviruses in children and adults. JCI Insight 6, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Goodwin E et al. Infants Infected with Respiratory Syncytial Virus Generate Potent Neutralizing Antibodies that Lack Somatic Hypermutation. Immunity 48, 339–349.e5 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gilman MSA et al. Rapid profiling of RSV antibody repertoires from the memory B cells of naturally infected adult donors. Science Immunology 1, eaaj1879–eaaj1879 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Meade P et al. Influenza Virus Infection Induces a Narrow Antibody Response in Children but a Broad Recall Response in Adults. mBio 11, e03243–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ranjeva S et al. Age-specific differences in the dynamics of protective immunity to influenza. Nat Commun 10, 1660 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gostic KM, Ambrose M, Worobey M & Lloyd-Smith JO Potent protection against H5N1 and H7N9 influenza via childhood hemagglutinin imprinting. 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gostic KM et al. Childhood immune imprinting to influenza A shapes birth year-specific risk during seasonal H1N1 and H3N2 epidemics. PLOS Pathogens 15, e1008109 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Arevalo CP et al. Original antigenic sin priming of influenza virus hemagglutinin stalk antibodies. PNAS 117, 17221–17227 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Aydillo T et al. Immunological imprinting of the antibody response in COVID-19 patients. Nat Commun 12, 3781 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Shrock E et al. Viral epitope profiling of COVID-19 patients reveals cross-reactivity and correlates of severity. Science 370, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sasson JM et al. Diverse Humoral Immune Responses in Younger and Older Adult COVID-19 Patients. mBio 12, e01229–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Karakoc Aydiner E et al. Adverse COVID-19 outcomes in immune deficiencies: Inequality exists between subclasses. Allergy n/a,. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Delavari S et al. Impact of SARS-CoV-2 Pandemic on Patients with Primary Immunodeficiency. J Clin Immunol 41, 345–355 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Esenboga S et al. COVID-19 in Patients with Primary Immunodeficiency. J Clin Immunol 1–8 (2021) doi: 10.1007/s10875-021-01065-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Meyts I et al. Coronavirus disease 2019 in patients with inborn errors of immunity: An international study. Journal of Allergy and Clinical Immunology 0, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Shaunak M et al. COVID-19 symptom surveillance in immunocompromised children and young people in the UK: a prospective observational cohort study. BMJ Open 11, e044899 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet 395, 1054–1062 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Li X et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. Journal of Allergy and Clinical Immunology 146, 110–118 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Williamson EJ et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 584, 430–436 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Noz MP et al. Trained Immunity Characteristics Are Associated With Progressive Cerebral Small Vessel Disease. Stroke 49, 2910–2917 (2018). [DOI] [PubMed] [Google Scholar]
- 103.Netea MG et al. Defining trained immunity and its role in health and disease. Nat Rev Immunol 20, 375–388 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Berbudi A, Rahmadika N, Tjahjadi AI & Ruslami R Type 2 Diabetes and its Impact on the Immune System. Curr Diabetes Rev 16, 442–449 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sandoval M, Nguyen DT, Vahidy FS & Graviss EA Risk factors for severity of COVID-19 in hospital patients age 18–29 years. PLOS ONE 16, e0255544 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Verdoni L et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. The Lancet 395, 1771–1778 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N & Theocharis P Hyperinflammatory shock in children during COVID-19 pandemic. The Lancet 395, 1607–1608 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Viner RM & Whittaker E Kawasaki-like disease: emerging complication during the COVID-19 pandemic. Lancet 395, 1741–1743 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Whittaker E et al. Clinical Characteristics of 58 Children With a Pediatric Inflammatory Multisystem Syndrome Temporally Associated With SARS-CoV-2. JAMA (2020) doi: 10.1001/jama.2020.10369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Feldstein LR et al. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. New England Journal of Medicine 383, 334–346 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Dufort EM et al. Multisystem Inflammatory Syndrome in Children in New York State. New England Journal of Medicine 383, 347–358 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Centers for Disease Control and Prevention. Emergency preparedness and response: multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease 2019 (COVID-19). HAN Archive - 00432 | Health Alert Network (HAN) https://emergency.cdc.gov/han/2020/han00432.asp (2021). [Google Scholar]
- 113.Feldstein LR et al. Characteristics and Outcomes of US Children and Adolescents With Multisystem Inflammatory Syndrome in Children (MIS-C) Compared With Severe Acute COVID-19. JAMA 325, 1074 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Abrams JY et al. Factors linked to severe outcomes in multisystem inflammatory syndrome in children (MIS-C) in the USA: a retrospective surveillance study. The Lancet Child & Adolescent Health 5, 323–331 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sancho-Shimizu V et al. SARS-CoV-2–related MIS-C: A key to the viral and genetic causes of Kawasaki disease? Journal of Experimental Medicine 218, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kwak JH, Lee S-Y & Choi J-W Clinical features, diagnosis, and outcomes of multisystem inflammatory syndrome in children associated with coronavirus disease 2019. Clin Exp Pediatr 64, 68–75 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Davogustto GE et al. Characteristics Associated With Multisystem Inflammatory Syndrome Among Adults With SARS-CoV-2 Infection. JAMA Netw Open 4, e2110323 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chau VQ et al. Cardiogenic Shock and Hyperinflammatory Syndrome in Young Males With COVID-19. Circulation: Heart Failure 13, e007485 (2020). [DOI] [PubMed] [Google Scholar]
- 119.Fox SE, Lameira FS, Rinker EB & Vander Heide RS Cardiac Endotheliitis and Multisystem Inflammatory Syndrome After COVID-19. Ann Intern Med 173, 1025–1027 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Newton-Cheh C et al. Case 24–2020: A 44-Year-Old Woman with Chest Pain, Dyspnea, and Shock. N Engl J Med 383, 475–484 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hékimian G et al. Coronavirus Disease 2019 Acute Myocarditis and Multisystem Inflammatory Syndrome in Adult Intensive and Cardiac Care Units. Chest 159, 657–662 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Shaigany S et al. An adult with Kawasaki-like multisystem inflammatory syndrome associated with COVID-19. Lancet 396, e8–e10 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Morris SB et al. Case Series of Multisystem Inflammatory Syndrome in Adults Associated with SARS-CoV-2 Infection — United Kingdom and United States, March–August 2020. MMWR Morb Mortal Wkly Rep 69, 1450–1456 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Morris SB Case Series of Multisystem Inflammatory Syndrome in Adults Associated with SARS-CoV-2 Infection — United Kingdom and United States, March–August 2020. MMWR Morb Mortal Wkly Rep 69, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Carter MJ et al. Peripheral immunophenotypes in children with multisystem inflammatory syndrome associated with SARS-CoV-2 infection. Nat Med (2020) doi: 10.1038/s41591-020-1054-6. [DOI] [PubMed] [Google Scholar]
- 126.Lee PY et al. Distinct clinical and immunological features of SARS–CoV-2–induced multisystem inflammatory syndrome in children. Journal of Clinical Investigation 130, 5942–5950 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Consiglio CR et al. The Immunology of Multisystem Inflammatory Syndrome in Children with COVID-19. Cell S0092867420311570 (2020) doi: 10.1016/j.cell.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gruber CN et al. Mapping Systemic Inflammation and Antibody Responses in Multisystem Inflammatory Syndrome in Children (MIS-C). Cell 183, 982–995.e14 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chang JC et al. Skewed Cytokine Responses Rather Than the Magnitude of the Cytokine Storm May Drive Cardiac Dysfunction in Multisystem Inflammatory Syndrome in Children. J Am Heart Assoc 10, e021428 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Yonker LM et al. Multisystem inflammatory syndrome in children is driven by zonulin-dependent loss of gut mucosal barrier. J Clin Invest 131, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.de Cevins C et al. A monocyte/dendritic cell molecular signature of SARS-CoV-2-related multisystem inflammatory syndrome in children with severe myocarditis. Med (N Y) (2021) doi: 10.1016/j.medj.2021.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Ramaswamy A et al. Immune dysregulation and autoreactivity correlate with disease severity in SARS-CoV-2-associated multisystem inflammatory syndrome in children. Immunity 54, 1083–1095.e7 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Diorio C et al. Multisystem inflammatory syndrome in children and COVID-19 are distinct presentations of SARS–CoV-2. J Clin Invest 130, 5967–5975 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Okarska-Napierała M et al. Recurrent assessment of lymphocyte subsets in 32 patients with multisystem inflammatory syndrome in children (MIS-C). Pediatr Allergy Immunol (2021) doi: 10.1111/pai.13611. [DOI] [PubMed] [Google Scholar]
- 135.Porritt RA et al. HLA class I–associated expansion of TRBV11-2 T cells in multisystem inflammatory syndrome in children. Journal of Clinical Investigation 131, e146614 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Moreews M et al. Polyclonal expansion of TCR Vb 21.3+ CD4+ and CD8+ T cells is a hallmark of multisystem inflammatory syndrome in children. Sci. Immunol 6, eabh1516 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Cheng MH et al. Superantigenic character of an insert unique to SARS-CoV-2 spike supported by skewed TCR repertoire in patients with hyperinflammation. Proc Natl Acad Sci USA 117, 25254–25262 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Notarbartolo S et al. Integrated longitudinal immunophenotypic, transcriptional, and repertoire analyses delineate immune responses in patients with COVID-19. Science Immunology 6, eabg5021 (2021). [DOI] [PubMed] [Google Scholar]
- 139.Josyabhatla R et al. Recognizing a MIS-Chievous Cause of Acute Viral Gastroenteritis. Frontiers in Pediatrics 9, 1123 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Noval Rivas M, Porritt RA, Cheng MH, Bahar I & Arditi M COVID-19–associated multisystem inflammatory syndrome in children (MIS-C): A novel disease that mimics toxic shock syndrome—the superantigen hypothesis. Journal of Allergy and Clinical Immunology 147, 57–59 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lamers MM et al. SARS-CoV-2 productively infects human gut enterocytes. Science (2020) doi: 10.1126/science.abc1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Anderson EM et al. Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2) Antibody Responses in Children With Multisystem Inflammatory Syndrome in Children (MIS-C) and Mild and Severe Coronavirus Disease 2019 (COVID-19). Journal of the Pediatric Infectious Diseases Society 10, 669–673 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lapp SA et al. Original antigenic sin responses to Betacoronavirus spike proteins are observed in a mouse model, but are not apparent in children following SARS-CoV-2 infection. PLOS ONE 16, e0256482 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Sermet-Gaudelus I et al. Prior infection by seasonal coronaviruses, as assessed by serology, does not prevent SARS-CoV-2 infection and disease in children, France, April to June 2020. Euro Surveill 26, (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Porritt RA et al. The autoimmune signature of hyperinflammatory multisystem inflammatory syndrome in children. Journal of Clinical Investigation 131, e151520 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Combes AJ et al. Global absence and targeting of protective immune states in severe COVID-19. Nature 591, 124–130 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.van der Made CI et al. Presence of Genetic Variants Among Young Men With Severe COVID-19. JAMA 324, 663 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Asano T et al. X-linked recessive TLR7 deficiency in ~1% of men under 60 years old with life-threatening COVID-19. Science Immunology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Fallerini C et al. Association of Toll-like receptor 7 variants with life-threatening COVID-19 disease in males: findings from a nested case-control study. eLife 10, e67569 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Solanich X et al. Genetic Screening for TLR7 Variants in Young and Previously Healthy Men With Severe COVID-19. Frontiers in Immunology 12, 2965 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Swiecki M & Colonna M The multifaceted biology of plasmacytoid dendritic cells. Nat Rev Immunol 15, 471–485 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.de Marcken M, Dhaliwal K, Danielsen AC, Gautron AS & Dominguez-Villar M TLR7 and TLR8 activate distinct pathways in monocytes during RNA virus infection. Sci. Signal 12, eaaw1347 (2019). [DOI] [PubMed] [Google Scholar]
- 153.Ioannou GN et al. Risk Factors for Hospitalization, Mechanical Ventilation, or Death Among 10 131 US Veterans With SARS-CoV-2 Infection. JAMA Network Open 3, e2022310–e2022310 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Peckham H et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun 11, 6317 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Nguyen NT et al. Male gender is a predictor of higher mortality in hospitalized adults with COVID-19. PLOS ONE 16, e0254066 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Lee PY et al. Immune dysregulation and multisystem inflammatory syndrome in children (MIS-C) in individuals with haploinsufficiency of SOCS1. Journal of Allergy and Clinical Immunology 146, 1194–1200.e1 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Chou J et al. Mechanisms underlying genetic susceptibility to multisystem inflammatory syndrome in children (MIS-C). J Allergy Clin Immunol S0091–6749(21)01052–6 (2021) doi: 10.1016/j.jaci.2021.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Ranney ML, Griffeth V & Jha AK Critical Supply Shortages — The Need for Ventilators and Personal Protective Equipment during the Covid-19 Pandemic. New England Journal of Medicine 382, e41 (2020). [DOI] [PubMed] [Google Scholar]
- 159.van der Graaf R, Hoogerwerf M-A & de Vries MC The ethics of deferred consent in times of pandemics. Nat Med 26, 1328–1330 (2020). [DOI] [PubMed] [Google Scholar]
- 160.Bourgeois FT, Avillach P & Turner MA The urgent need for research coordination to advance knowledge on COVID-19 in children. Pediatr Res (2020) doi: 10.1038/s41390-020-01259-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Xu G et al. The differential immune responses to COVID-19 in peripheral and lung revealed by single-cell RNA sequencing. Cell Discovery 6, 1–14 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Son MBF et al. Multisystem Inflammatory Syndrome in Children — Initial Therapy and Outcomes. N Engl J Med 385, 23–34 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.McArdle AJ et al. Treatment of Multisystem Inflammatory Syndrome in Children. N Engl J Med 385, 11–22 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Simpson S, Kaislasuo J, Guller S & Pal L Thermal stability of cytokines: A review. Cytokine 125, 154829 (2020). [DOI] [PubMed] [Google Scholar]
- 165.Muñoz-Fontela C et al. Animal models for COVID-19. Nature 586, 509–515 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]


