Abstract
Objectives
Literature has assessed skilled birth attendants (SBAs) utilisation, but little is known about what contributes to the changes in SBA use. Multivariate decomposition analysis was thus applied in this study to examine; levels, trends, inequalities and drivers of changes in SBA utilisation.
Design and setting
A cross-sectional analysis of five-waves of NDHS-data (1990, 2003, 2008, 2013, and 2018), collected through similar multistage sampling across the 36 states and the federal-capital-territory of Nigeria.
Participants
Women of reproductive age (15–49 years), and with at least one birth in the last 5 years preceding each of the surveys.
Main outcome measure
SBA use is the response variable while explanatory variables were classified into; Demographics, Health, Economic and Corporal factors.
Methods
Chi-square test for trends of proportions across the ordered survey years assessed trends in SBA use. MDA that quantifies and partition predictors effect into endowment and coefficient components evaluated contributors to changes in SBA use. Statistical analysis was carried out at a 95% confidence interval in Stata 16.
Results
SBA use increased with significant (p<0.05) linear trends by 12% between 2003 and 2018. The decomposition analysis showed that differences in characteristics (endowment) accounted for 11.5% of the changes while the remaining 88.5% were due to differences in effects (coefficient). SBA utilisation rises by 61% when respondents decided on her health compared to when such decisions were made by the spouse. Utilisation of SBA, however, fell by 88% among women who reside in the states with high rural populations percentage.
Conclusions
SBA use remained low in Nigeria, and slowly increase at the rate of <1% yearly. Women health decision-making power contributed most to positive changes. Residing in states with high rural populations has a negative impact on SBA use. Maternal health programmes that strengthen women’s health autonomy and capacity building in rural communities should be encouraged.
Keywords: health services administration & management, epidemiology, public health, reproductive medicine, statistics & research methods
Strengths and limitations of this study.
The study might have suffered from recall bias, which is associated with cross-sectional studies.
Our findings are limited to association and do not infer causality. Therefore, caution must be exercised while interpreting the results.
The study strength can, however, be drawn from the largeness of the study sample size based on five-waves of the survey that allow us to achieve fair and reliable estimates.
The use of sampling weights and year-women weight to accommodate differentials in women population across the survey years enhanced the accuracy of our estimates and their generalisation thereof.
The application of multivariate decomposition analysis that quantifies the contribution of individual predictors in this study is also a strength. Though non-linear multivariate decomposition estimate is generally biased by identification problem but the normalisation option in the multivariate decomposition analysis reduced such bias.
Introduction
Consistent and effective utilisation of skilled birth attendants (SBAs) before, during and after delivery remained a viable approach to timely management of pregnancy complications, reduced pregnancy, and childbirth-related deaths, and optimal pregnancy outcomes.1–4 However, many pregnant women in sub-Saharan African (SSA) countries including Nigeria do not use this preventive intervention technique to curb the high burden of maternal and newborn mortality and morbidity.3 4 The contributions of unskilled births attendants to maternal deaths in Africa has been reported.3–7
While developed countries; such as Sweden, Norway, Netherlands and Denmark have rapidly reduced their maternal mortality by increasing the use of SBA, developing nations including South-Sudan, Chad, Sierra-Leone and Nigeria, are struggling to ensure that all pregnant women use SBA.8 Whereas, the use of SBA is one of the formidable strategies to achieve the United Nations Sustainable Development Goal (SDG)-3.9 South Sudan, Chad, Sierra Leone and Nigeria are the topmost four low/middle-income countries most affected by maternal mortality in 2017 with an estimated high maternal mortality ratio (MMR) of 1150, 1140, 1140 and 917 deaths per 100 000 live births, respectively.8 Nonetheless, the most recent national survey in Nigeria reported a lower MMR of 512 (95% CI 447 to 578) per 100 000 live births.10
In Nigeria, SBA coverage has remained below the global average and fluctuates periodically across the geopolitical zones and states despite the recent increase in turn-up at antenatal care (ANC) services.10 According to the reports from Nigerian Demographic and Health Survey (NDHS), 67% of women aged 15–49 years received ANC in 2018 (6% increase from 2013) while SBAs utilisation increased only slightly from 39% in 2013 to 43% in 2018 while that of traditional birth attendants decreased by only 2% during the same period.10 11 For instance, health facility delivery was 32%, 33%, 35%, 36% and 39% of all births in 1990, 2003, 2008, 2013 and 2018 respectively, and pregnancy-related mortality ratio (PRMR) was 545/100,000 for 2001–2008, 576/100,000 for 2006–2013 and 556/100 000 for 2011–2018 while MMR was 512/100 000 live births in 2018.10 11
However, as shown in these statistics, an increase in ANC uptake alone is insufficient to improve the use of SBA owing to drop out from the maternal continuum of care before delivery. This has been reported to be high in Nigeria and driven by low or lack of formal education, poverty and socioeconomic status.12 Also, as high as one-third of ANC clients in 28 African countries including Nigeria usually drop out from the skilled maternal care continuum and in turn fail to reduce pregnancy and child-related mortality.13 Recent statistics however showed an insignificant difference in the reported PRMR in 2013 and 2018 while child (including neonatal) mortality has increased by 2% from 37/1000 live births in 2013 to 39/1000 live births in 2018, thus explaining why 80% of currently married women have the potential for a high-risk birth in Nigeria.10 11
There has been a haphazard rise and fall in the use of SBA in Nigeria with the reported 6% insignificant difference between 1990 and 2013.4 While it remains unclear whether the 12% difference in SBA use between 1990 and 2018 is statistically significant, it took nearly three decades to achieve such little increase. This, therefore, implies that at this rate, SBA utilisation will only increase by about 4% by 2030 which will undermine the attainment of the UN SDG-3 target of reducing world MMR to less than 70 per 100 000 live births.9 14 This signals the need to expand efforts/strategies geared towards increasing SBA use in Nigeria by doubling skilled health personnel to childbirth ratio and strengthening healthcare delivery services. If adopted and adequately implemented, this approach could reduce MMR by half as experienced in Egypt between 1983 and 2000.15
Literature on the determinants of SBA utilisation has identified several factors classified into sociocultural—maternal age, education, marital status, ethnicity; perceived benefit—ANC adequacy, SBA history; economic and physical accessibility-related factors—employment, household social economy, healthcare mobility.16–18 Fagbamigbe et al identified sociocultural, maternal education and urban residence as strong determinants of SBA use in Nigeria.4 Olakunde et al also reported maternal age alongside household wealth quintile, geopolitical zone, parity and ANC as influential factors of SBA utilisation among adolescent girls in Nigeria.7 Maternal/partner education, household wealth/socioeconomic status, parity and ANC attendance were also major determinants of SBA use in southern and northern Ghana.19 20 Whereas, education, urban residence, wealth status, ANC visits, age at first birth and previous pregnancy complications were significantly associated with the use of skilled birth delivery in Ethiopia.21 22 These factors have also been linked to the determinants of ANC utilisation and predictors of infant and child survival.23–26
Although studies abound on SBA use and its associated factors in Nigeria4 7 14 19 21 22 27 only a few have assessed trends, inequalities, and the predictors of the changes. We are not aware of any study on the changes in SBA use and the drivers of these changes at both the national and subnational levels in Nigeria. Fagbamigbe et al had ascertained the dearth of studies on the comparison of SBA use across states and regions of Nigeria4. Thus, the current study was designed to assess the trends in SBA use in Nigeria between 1990 and 2018 and also evaluate the factors that contributed to the changes across the periods using the multivariate decomposition analysis (MDA) technique. We sought to provide answers to the questions; were there any significant changes in the level of SBA use in Nigeria between 1990 and 2018? How significant are the changes in the level of SBA use over this period? What are the factors contributing to the changes in SBA use over this period? This study provided evidence-based information that could aid strategic maternal health programming in Nigeria.
Methodology
Study design, data and area
The study is a secondary analysis of data extracted from the five successive NDHS conducted in 1990, 2003, 2008, 2013, and 2018. The NDHS is a cross-sectional population-based nationally representative survey, routinely collected across all states and the Federal Capital Territory (FCT) of Nigeria. The sampling design is similar across the surveys. The survey usually uses stratified and multistage sampling techniques that accommodate household clusters (primary sampling unit) of respondents providing information on their demographic status and reproductive health behaviours of women aged 15–49 years. Nigeria is divided into six geopolitical zones called regions and each region is subdivided into states and FCT. As of 1990, Nigeria has 21 states. These were then divided and grouped into 30 states and the FCT in 1991. Additional 6 states were created in 1996, which resulted in the present number of 36 states as shown in figure 1.
Figure 1.
Map of Nigeria showing the 36 states and the federal capital territory, by the geopolitical zones.
Sampling procedures
Similar two-stage cluster sampling was used in each of the five-waves of the survey. The 36 states and FCT were subdivided into local government areas (LGAs) whereby rural and urban LGAs were separated. Enumeration areas were selected from the LGAs at the first stage and households were then selected at the second stage where all women aged 15–49 years in the selected households were interviewed. In-depth information on the NDHS sampling methodology where 8781, 7620, 33385, 38 984 and 41 821 women participated in 1990, 2003, 2008, 2013 and 2018 surveys respectively have been documented.10 11 28
Patient and public involvement
No patient was involved. We applied the strobe reporting guidelines.29
Outcome and explanatory variables
Utilisation of SBA during the last childbirth within 5 years preceding each survey was the outcome variable and was measured as whether birth was assisted by skilled provider or not.4 14 30 Skilled delivery services are rendered by doctors, nurses, midwives and auxiliary nurses/midwives. Independent/explanatory variables that includes; maternal age, education, ANC visit, parity, socioeconomic status and place of residence that are consistently associated with SBA use in Nigeria and SSA were studied.4 7 19–22 31–33 Other set of independent factors associated with the use of SBA and captured in each survey year of the DHS were included.10 11 28 To ensure uniformity in all the survey data used, independent variables were classified in this study as; demographic/societal, women health, economic and corporal factors based on extensive literature search and review.5 16 17 31 34 We further adopted the extended behavioural-ecological framework for healthcare access and navigation in selecting and classifying independents variables.35 The independent variables and the respective classification are as follows.
Demographic, cultural and societal factors: maternal age (15–24, 25–34, 35–49 years), highest educational level (no education, primary, secondary+) Husband/partner’s educational level (no education, primary, secondary+), sex of household head (male, female), marital status (never married, currently married or living with a sexual partner, formerly married), tribe/ethnic group (Hausa/Fulani, Yoruba, Igbo, others), religion (Islam, Christianity, others), region (northcentral, northeast, northwest, south-east, south-south, southwest), place of residence (urban, rural).
Women health benefit/SBA purpose: wanted last child (wanted then, wanted later, wanted no more), number of ANC visits during pregnancy (none, less than the recommended 4, 4+visits), covered by health insurance (no, yes), birth order (1, 2, 3, 4 and 5+), birth interval (first birth, ≤36 months, 36+ months).
Economic class: employment status (employed, unemployed), paternal employment status (employed, unemployed), wealth index (poorest, poorer, middle, richer, richest), media access (no, yes), community poverty level (low, high) community unemployment (low, high), community media access (low, high), community social economy disadvantage (least disadvantage, less disadvantage, disadvantage, more disadvantage, most disadvantage).
Corporal convenience: distance to health facility (no problem, big problem), person who usually decides on respondent’s healthcare (respondent alone, both, spouse alone), getting permission to go for medical help for self (no problem, big problem), years lived at place of residence/mobility (5+years, ≤5 years), state rural population percentage (low, high), community illiteracy level (low, high).
Statistical analysis
Simple descriptive statistics reporting frequency and percentages of women utilising SBA viz-a-viz independent characteristics were presented in tables 1 and 2. Bivariate association was examined for each category of nominal/ordinal independent variables and SBA use was examined across the periods between 1990 and 2018 ‘(1990–2003, 2003–2008, 2008–2013 and 2013–2018) and longer periods of 2003–2018 and 1990–2018’ using the χ2 test for trends of proportions, with the survey years being an ordinal exposure variable.36 The χ2 analysis of trend and Rao-Scot χ2,37 38 were used to determine if there are any significant changes or not at alpha (α)=0.05. We found no difference between the conclusions from the χ2 for trend and the Rao-Scot χ2. MDA was employed to decompose changes in SBA use between 2003 and 2018. The MDA presents an opportunity to decompose what contributes to changes over two time points or among two mutually exclusive groups. We excluded 1990 from the MDA and considered 2003–2018, to allow full comparison across the current 36 states in Nigeria. In the MDA, respondents’ SBA use is the response variable with outcomes in 2003 as one ‘group’ and 2018 as another ‘group’ while predictor effects were partitioned into differences in characteristics or endowment and differences in the effects or coefficients in the regression decomposition.39 This is to identify the root of the changes in the utilisation of SBA in the last one and half decades (2003–2018) and evaluate how SBA use responds to changes in women characteristics. Data management and analysis were conducted using Stata V.16.0. Survey design was considered in the analysis due to sample disproportionality and was managed by probability weights. Hence, we applied the sample weight (SW) using the weighting factors included in the NDHS data and adjusted for the complex survey design (that incorporate the sample weighting, clustering, and stratification) through the ‘svy’ analysis on Stata to account for unequal population sizes. Test of statistical significance was carried out at 5% level of significance (95% confidence level) in all the statistical analysis. We computed and applied the year-women weight (YWW) to the analysis to reflect the differences in population sizes of the women in each survey year. The YWW is the product of SW (provided in the NDHS data) and year-specific weight (YSW). We computed the YSW as the number of sampled women aged 15–49 years divided by the population of women aged 15–49 years for each year as earlier reported.40 We controlled for multicollinearity using the ‘colin’ command in Stata and the variance inflation factor (VIF) was evaluated. The mean VIF was 1.97.
Table 1.
Distribution of mothers’ background characteristics
| Characteristics | 1990 (%) | 2003 (%) | 2008 (%) | 2013 (%) | 2018 (%) | Total (%) | Sample (n) |
| Respondent’s current age | |||||||
| 15–24 | 28.7 | 28.8 | 26.3 | 25.8 | 24.9 | 25.9 | 17 809 |
| 25–34 | 48.0 | 46.7 | 46.5 | 46.7 | 47.0 | 46.8 | 32 249 |
| 35–49 | 23.3 | 24.6 | 27.2 | 27.5 | 28.1 | 27.3 | 18 621 |
| Highest educational level | |||||||
| No education | 63.9 | 49.9 | 49.1 | 46.9 | 44.3 | 47.7 | 32 297 |
| Primary | 23.3 | 24.2 | 22.5 | 20.0 | 15.5 | 19.2 | 13 772 |
| Secondary+ | 12.8 | 25.9 | 28.4 | 33.0 | 40.1 | 33.2 | 22 610 |
| Husband/partner’s educational level | |||||||
| No education | 55.2 | 39.9 | 41.3 | 38.9 | 36.1 | 39.6 | 25 387 |
| Primary | 24.7 | 24.3 | 20.8 | 18.8 | 14.3 | 18.1 | 12 400 |
| Secondary+ | 20.1 | 35.8 | 37.8 | 42.3 | 49.6 | 42.3 | 27 543 |
| Place of residence | |||||||
| Urban | 31.6 | 34.7 | 26.6 | 33.0 | 34.7 | 31.9 | 22 416 |
| Rural | 68.4 | 65.3 | 73.4 | 67.0 | 65.3 | 68.1 | 46 263 |
| Employment status | |||||||
| Employed | 64.5 | 63.6 | 64.7 | 69.2 | 68.2 | 66.9 | 45 967 |
| Unemployed | 35.5 | 36.4 | 35.3 | 30.8 | 31.8 | 33.1 | 22 494 |
| Paternal employment status | |||||||
| Employed | 98.8 | 99.6 | 98.8 | 98.5 | 96.8 | 97.9 | 64 853 |
| Unemployed | 1.2 | 0.4 | 1.2 | 1.5 | 3.2 | 2.1 | 1287 |
| Sex of household head | |||||||
| Male | 93.3 | 90.6 | 89.8 | 88.9 | 89.5 | 89.8 | 61 489 |
| Female | 6.7 | 9.4 | 10.2 | 11.1 | 10.5 | 10.2 | 7190 |
| Marital status | |||||||
| Never married | 0.8 | 2.6 | 2.5 | 2.6 | 2.8 | 2.5 | 1750 |
| Living with sexual partner | 95.9 | 93.4 | 94.5 | 94.3 | 93.7 | 94.2 | 64 626 |
| Formerly married | 3.3 | 4.1 | 3.0 | 3.1 | 3.5 | 3.3 | 2302 |
| Media access | |||||||
| No | na | 39.3 | 46.4 | 54.0 | 59.7 | 53.8 | 33 234 |
| Yes | na | 60.7 | 53.6 | 46.0 | 40.3 | 46.2 | 30 270 |
| Wealth index | |||||||
| Poorest | 22.6 | 22.7 | 26.4 | 22.7 | 23.6 | 24.1 | 16 030 |
| Poorer | 22.6 | 21.5 | 23.4 | 23.0 | 22.7 | 22.9 | 15 548 |
| Middle | 13.9 | 20.3 | 19.6 | 19.9 | 21.0 | 19.9 | 13 581 |
| Richer | 18.0 | 18.8 | 17.0 | 18.6 | 18.1 | 17.9 | 12 517 |
| Richest | 22.8 | 16.7 | 13.8 | 15.8 | 14.5 | 15.2 | 11 003 |
| No of ANC visits during pregnancy | |||||||
| None (0) | 39.4 | 33.9 | 39.1 | 34.5 | 25.0 | 31.9 | 21 957 |
| Inadequate (less than 4) | 10.9 | 14.4 | 10.9 | 12.6 | 17.5 | 14.2 | 9280 |
| Adequate (four or more) | 49.7 | 51.6 | 49.9 | 53.0 | 57.6 | 53.9 | 37 075 |
| Religion | |||||||
| Islam | 58.8 | 60.4 | 55.2 | 58.9 | 58.4 | 57.7 | 38 983 |
| Christianity | 37.3 | 37.9 | 42.3 | 39.6 | 40.8 | 40.7 | 28 456 |
| Others | 3.9 | 1.7 | 2.5 | 1.4 | 0.8 | 1.6 | 1237 |
| Tribe/ethnic group | |||||||
| Hausa/Fulani | na | 40.0 | 36.6 | 40.5 | 40.5 | 39.3 | 24 525 |
| Yoruba | na | 10.9 | 11.9 | 11.6 | 10.6 | 11.2 | 7373 |
| Igbo | na | 11.6 | 10.1 | 9.8 | 12.9 | 11.4 | 7206 |
| Others | na | 37.6 | 41.4 | 38.1 | 36.0 | 38.1 | 24 683 |
| A person who usually decides on respondent’s healthcare | |||||||
| Respondent | na | 13.8 | 7.6 | 5.2 | 8.9 | 8.1 | 4704 |
| Both | na | 10.6 | 33.5 | 31.1 | 31.7 | 31.2 | 18 494 |
| Spouse alone | na | 75.6 | 58.9 | 63.7 | 59.3 | 60.7 | 36 542 |
| Getting medical help for self: distance to a health facility | |||||||
| No problem | na | 73.9 | 59.4 | 67.5 | 69.7 | 66.4 | 42 557 |
| Big problem | na | 26.1 | 40.6 | 32.5 | 30.3 | 33.6 | 21 063 |
| Getting medical help for self: getting permission to go | |||||||
| No problem | na | 89.5 | 84.4 | 88.3 | 87.7 | 86.9 | 55 313 |
| Big problem | na | 10.5 | 15.6 | 11.7 | 12.3 | 13.1 | 8283 |
| Wanted the last-child | |||||||
| Wanted then | 87.4 | 84.8 | 89.6 | 90.3 | 87.8 | 88.6 | 60 331 |
| Wanted later | 9.7 | 9.6 | 5.6 | 7.6 | 8.8 | 7.8 | 5554 |
| Wanted no more | 2.9 | 5.6 | 4.8 | 2.1 | 3.5 | 3.7 | 2534 |
| Years lived in a place of residence/mobility | |||||||
| More than 5 years | 88.9 | 79.5 | 74.2 | 83.8 | 80.7 | na | 38 854 |
| 0–4 years | 11.1 | 20.5 | 25.8 | 16.2 | 19.3 | na | 9626 |
| Covered by health insurance | |||||||
| No | na | Na | 98.7 | 98.3 | 97.8 | 98.2 | 58 746 |
| Yes | na | Na | 1.3 | 1.7 | 2.2 | 1.8 | 1103 |
| Birth order | |||||||
| 1 | 16.4 | 19.2 | 17.0 | 17.7 | 17.0 | 17.2 | 11 940 |
| 2 | 15.9 | 15.2 | 16.3 | 16.1 | 17.3 | 16.6 | 11 347 |
| 3 | 14.3 | 13.8 | 15.0 | 14.7 | 15.2 | 14.9 | 10 225 |
| 4 | 12.9 | 12.6 | 13.2 | 13.1 | 13.4 | 13.2 | 9040 |
| 5 | 40.4 | 39.2 | 38.6 | 38.4 | 37.1 | 38.1 | 26 127 |
| Birth interval | |||||||
| First birth | 16.5 | 19.3 | 17.0 | 17.8 | 17.0 | 17.2 | 11 940 |
| <36 months | 49.7 | 46.8 | 47.6 | 46.8 | 47.9 | 47.7 | 32 630 |
| 36+ months | 33.8 | 33.9 | 35.4 | 35.4 | 35.1 | 35.1 | 23 986 |
| States rural population percentage | |||||||
| Low | 34.1 | 27.0 | 27.3 | 26.7 | 28.3 | 28.1 | 19 856 |
| High | 65.9 | 73.0 | 72.7 | 73.3 | 71.7 | 71.9 | 48 823 |
| Community poverty level | |||||||
| Low | 58.4 | 44.9 | 43.5 | 38.8 | 62.0 | 52.0 | 33 830 |
| High | 41.6 | 55.1 | 56.5 | 61.2 | 38.0 | 48.0 | 34 849 |
| Community illiteracy level | |||||||
| Low | 30.8 | 46.2 | 45.2 | 38.9 | 67.2 | 53.0 | 33 901 |
| High | 69.2 | 53.8 | 54.8 | 61.1 | 32.8 | 47.0 | 34 778 |
| Community unemployment | |||||||
| Low | 34.6 | 20.3 | 40.6 | 42.2 | 72.1 | 53.6 | 33 914 |
| High | 65.4 | 79.7 | 59.4 | 57.8 | 27.9 | 46.4 | 34 765 |
| Community media access | |||||||
| Low | 91.2 | 45.9 | 42.6 | 34.9 | 57.7 | 51.4 | 33 750 |
| High | 8.8 | 54.1 | 57.4 | 65.1 | 42.3 | 48.6 | 34 929 |
| Community socialeconomic status disadvantage | |||||||
| Least disadvantage | 29.0 | 2.0 | 13.6 | 15.3 | 28.9 | 21.2 | 13 752 |
| Less disadvantage | 27.2 | 15.5 | 19.5 | 19.0 | 21.1 | 20.5 | 13 733 |
| Disadvantage | 16.0 | 33.8 | 22.5 | 17.6 | 18.5 | 20.0 | 13 758 |
| More disadvantage | 15.7 | 29.7 | 22.5 | 20.3 | 16.3 | 19.2 | 13 716 |
| Most disadvantage | 12.1 | 18.9 | 21.9 | 28.0 | 15.2 | 19.2 | 13 720 |
| Region | |||||||
| North Central | 15.6 | 16.5 | 18.5 | 14.8 | 17.4 | 17.2 | 11 658 |
| North East | 11.5 | 23.2 | 22.0 | 20.3 | 20.8 | 20.5 | 13 832 |
| North West | 35.5 | 30.9 | 26.8 | 32.4 | 29.4 | 29.6 | 19 979 |
| South East | 10.1 | 8.1 | 8.2 | 8.1 | 10.9 | 9.5 | 6481 |
| South-South | 8.1 | 10.1 | 11.8 | 11.9 | 9.9 | 10.6 | 7637 |
| South West | 19.2 | 11.4 | 12.7 | 12.6 | 11.6 | 12.6 | 9092 |
| Total | 3106 | 3761 | 17 920 | 20 100 | 21 792 | 666,79 | 66 679 |
na, not available.
Table 2.
Trends and prevalence of SBA use by background characteristics of mothers
| Characteristics | 1990 | 2003 | 2008 | 2013 | 2018 | All | 1990–2003 | 2003–2008 | 2008–2013 | 2013–2018 | 1990–2018 | 2003–2018 | Trend test (X2, p value)* |
| Respondent’s current age | |||||||||||||
| 15–24 | 28.7 | 31.8 | 27.3 | 29.9 | 34.8 | 30.7 | 10.8 | −14.2 | 9.5 | 16.4 | 21.3 | 9.4 | 4.2; 0.040 |
| 25–34 | 33.9 | 40.5 | 38.0 | 39.4 | 45.4 | 40.6 | 19.5 | −6.2 | 3.7 | 15.2 | 33.9 | 12.1 | 62.4; 0.000 |
| 35–49 | 32.2 | 40.1 | 33.5 | 38.3 | 44.1 | 38.7 | 24.5 | −16.5 | 14.3 | 15.1 | 37.0 | 10.0 | 39.1; 0.000 |
| Highest educational level | |||||||||||||
| No education | 15.9 | 14.6 | 11.1 | 11.5 | 14.5 | 12.8 | −8.2 | −24.0 | 3.6 | 26.1 | −8.8 | −0.7 | 22.4; 0.000 |
| Primary | 50.4 | 45.7 | 39.3 | 39.7 | 45.4 | 42.4 | −9.3 | −14.0 | 1.0 | 14.4 | −9.9 | −0.7 | 55.1; 0.000 |
| Secondary+ | 79.4 | 75.5 | 69.1 | 70.5 | 72.0 | 71.3 | −4.9 | −8.5 | 2.0 | 2.1 | −9.3 | −4.6 | 3.6; 0.056 |
| Husband/partner’s education level | |||||||||||||
| No education | 12.4 | 14.4 | 10.4 | 10.0 | 12.0 | 11.1 | 16.1 | −27.8 | −3.8 | 20.0 | −3.2 | −16.7 | 20.1; 0.000 |
| Primary | 48.9 | 38.5 | 37.4 | 37.9 | 43.5 | 40.3 | −21.3 | −2.9 | 1.3 | 14.8 | −11.0 | 13.0 | 32.5; 0.000 |
| Secondary+ | 63.1 | 61.2 | 57.7 | 60.1 | 63.3 | 60.9 | −3.0 | −5.7 | 4.2 | 5.3 | 0.3 | 3.4 | 8.6; 0.003 |
| Rural/place of residence | |||||||||||||
| Urban | 59.8 | 58.4 | 60.7 | 65.2 | 65.3 | 63.4 | −2.3 | 3.9 | 7.4 | 0.2 | 9.2 | 11.8 | 53.2; 0.000 |
| Rural | 19.2 | 26.9 | 24.2 | 22.6 | 30.2 | 25.4 | 40.1 | −10.0 | −6.6 | 33.6 | 57.3 | 12.3 | 39.9; 0.000 |
| Employment status | |||||||||||||
| Employed | 38.7 | 42.7 | 39.1 | 40.6 | 47.7 | 42.5 | 10.3 | −8.4 | 3.8 | 17.5 | 23.3 | 11.7 | 53.6; 0.000 |
| Unemployed | 20.0 | 29.3 | 24.6 | 27.8 | 31.1 | 27.5 | 46.5 | −16.0 | 13.0 | 11.9 | 55.5 | 6.1 | 27.0; 0.000 |
| Paternal employment status | |||||||||||||
| Employed | 31.5 | 37.0 | 33.9 | 36.1 | 42.2 | 37.1 | 17.5 | −8.4 | 6.5 | 16.9 | 34.0 | 14.1 | 78.1; 0.000 |
| Unemployed | 53.7 | 42.9 | 26.1 | 54.5 | 29.3 | 36.3 | −16.3 | −42.3 | 108.8 | −46.2 | −45.7 | −35.2 | 78.2; 0.000 |
| Sex of household head | |||||||||||||
| Male | 30.6 | 35.7 | 32.6 | 34.4 | 40.6 | 35.7 | 16.7 | −8.7 | 5.5 | 18.0 | 32.7 | 13.7 | 90.7; 0.000 |
| Female | 52.6 | 58.8 | 45.8 | 54.5 | 58.1 | 53.6 | 11.8 | −22.1 | 19.0 | 6.6 | 10.5 | −1.2 | 2.0; 0.157 |
| Marital status | |||||||||||||
| Never married | 63.4 | 68.9 | 40.4 | 46.6 | 54.1 | 49.4 | 9.3 | −41.7 | 15.3 | 16.1 | −14.7 | −21.9 | 5.4; 0.020 |
| Currently married | 31.4 | 36.8 | 33.6 | 36.2 | 41.8 | 37.0 | 17.2 | −8.7 | 7.7 | 15.5 | 33.1 | 13.6 | 103.9; 0.000 |
| Formerly | 41.4 | 43.5 | 38.0 | 43.1 | 49.8 | 44.0 | 5.1 | −12.6 | 13.4 | 15.5 | 20.3 | 14.5 | 6.1; 0.013 |
| Media access | |||||||||||||
| No | na | 23.2 | 16.9 | 20.2 | 28.5 | 22.7 | Na | −27.2 | 19.5 | 41.1 | na | 22.8 | 183.7; 0.000 |
| Yes | na | 47.6 | 48.6 | 56.1 | 63.1 | 55.1 | Na | 2.1 | 15.4 | 12.5 | na | 32.6 | 23.6; 0.000 |
| Wealth index | |||||||||||||
| Poorest | 11.1 | 13.4 | 7.8 | 5.5 | 11.4 | 8.8 | 20.7 | −41.8 | −29.5 | 107.3 | 2.7 | −14.9 | 11.6; 0.001 |
| Poorer | 14.8 | 23.1 | 17.2 | 16.5 | 24.2 | 19.3 | 56.1 | −25.5 | −4.1 | 46.7 | 63.5 | 4.8 | 7.2; 0.007 |
| Middle | 22.5 | 32.5 | 34.2 | 38.1 | 47.1 | 39.1 | 45.1 | 5.2 | 11.4 | 23.6 | 110.3 | 44.9 | 169.1; 0.000 |
| Richer | 39.3 | 51.2 | 58.5 | 59.0 | 66.1 | 59.3 | 30.3 | 14.3 | 0.9 | 12.0 | 68.2 | 29.1 | 191.9; 0.000 |
| Richest | 70.0 | 81.5 | 81.9 | 82.6 | 84.9 | 81.6 | 16.4 | 0.5 | 0.9 | 2.8 | 21.3 | 4.2 | 72.7; 0.000 |
| No of antenatal visits during pregnancy | |||||||||||||
| None | 2.1 | 4.0 | 4.0 | 4.1 | 7.4 | 4.7 | 90.5 | 0.0 | 2.5 | 80.5 | 252.4 | 85.0 | 1.07; 0.300 |
| Inadequate | 27.8 | 28.9 | 29.2 | 26.0 | 28.6 | 28.0 | 4.0 | 1.0 | −11.0 | 10.0 | 2.9 | −1.0 | 0.1; 0.833 |
| Adequate | 57.6 | 62.6 | 58.6 | 60.3 | 61.8 | 60.3 | 8.7 | −6.4 | 2.9 | 2.5 | 7.3 | −1.3 | 7.6; 0.006 |
| Religion | |||||||||||||
| Islam | 17.5 | 22.5 | 19.7 | 21.4 | 26.0 | 22.3 | 28.6 | −12.4 | 8.6 | 21.5 | 48.6 | 15.6 | 60.2; 0.000 |
| Christian | 56.5 | 63.4 | 53.4 | 59.8 | 66.2 | 60.0 | 12.2 | −15.8 | 12.0 | 10.7 | 17.2 | 4.4 | 19.5; 0.000 |
| Others | 18.5 | 19.2 | 18.1 | 24.3 | 25.2 | 20.8 | 3.8 | −5.7 | 34.3 | 3.7 | 36.2 | 31.3 | 1.5; 0.225 |
| Tribe | |||||||||||||
| Hausa/Fulani | na | 13.1 | 9.7 | 12.5 | 17.9 | 13.7 | Na | −26.0 | 28.9 | 43.2 | na | 36.6 | 61.1; 0.000 |
| Yoruba | na | 77.5 | 74.7 | 81.4 | 82.0 | 79.4 | Na | −3.6 | 9.0 | 0.7 | na | 5.8 | 7.3; 0.007 |
| Igbo | na | 75.8 | 71.3 | 79.3 | 82.3 | 78.3 | Na | −5.9 | 11.2 | 3.8 | na | 8.6 | 41.5; 0.000 |
| Others | na | 41.3 | 34.6 | 37.8 | 43.9 | 39.0 | Na | −16.2 | 9.2 | 16.1 | na | 6.3 | 0.8; 0.372 |
| A person who usually decides on respondent’s healthcare | |||||||||||||
| Respondent | na | 57.4 | 53.2 | 62.9 | 57.0 | 57.3 | Na | −7.3 | 18.2 | −9.4 | na | −0.7 | 1.5; 0.218 |
| Both | na | 61.1 | 46.6 | 55.3 | 59.3 | 54.2 | Na | −23.7 | 18.7 | 7.2 | na | −2.9 | 10.4; 0.001 |
| Spouse alone | na | 30.1 | 23.7 | 24.6 | 30.2 | 26.6 | Na | −21.3 | 3.8 | 22.8 | na | 0.3 | 1.2; 0.268 |
| Getting medical help for self: distance to a health facility | |||||||||||||
| No problem | na | 44.7 | 41.1 | 44.9 | 47.9 | 45.0 | Na | −8.1 | 9.2 | 6.7 | na | 7.2 | 40.0; 0.000 |
| Big problem | na | 18.7 | 23.6 | 19.6 | 29.8 | 24.1 | Na | 26.2 | −16.9 | 52.0 | na | 59.4 | 11.9; 0.001 |
| Getting medical help for self: getting permission to go | |||||||||||||
| No_problem | na | 41.2 | 36.8 | 39.5 | 44.5 | 40.6 | Na | −10.7 | 7.3 | 12.7 | na | 8.0 | 27.7; 0.000 |
| Big_problem | na | 9.8 | 18.8 | 15.6 | 27.4 | 20.2 | Na | 91.8 | −17.0 | 75.6 | na | 179.6 | 38.9; 0.000 |
| Wanted the last-child | |||||||||||||
| Wanted then | 30.8 | 35.3 | 32.9 | 35.1 | 40.5 | 35.9 | 14.6 | −6.8 | 6.7 | 15.4 | 31.5 | 14.7 | 87.0; 0.000 |
| Wanted later | 37.8 | 48.4 | 42.5 | 50.6 | 56.5 | 49.9 | 28.0 | −12.2 | 19.1 | 11.7 | 49.5 | 16.7 | 65.9; 0.000 |
| Wanted no more | 49.8 | 59.2 | 47.0 | 58.2 | 55.9 | 53.1 | 18.9 | −20.6 | 23.8 | −4.0 | 12.2 | −5.6 | 9.0; 0.003 |
| Family mobility | |||||||||||||
| No | 29.0 | 34.6 | 28.3 | na | 38.4 | 33.6 | 19.3 | −18.2 | −100.0 | na | 32.4 | 11.0 | 134.3; 0.000 |
| Yes | 56.2 | 50.6 | 50.2 | na | 63.0 | 55.4 | −10.0 | −0.8 | −100.0 | na | 12.1 | 24.5 | 7.01; 0.008 |
| Has health insurance | |||||||||||||
| No | na | na | 33.2 | 35.8 | 41.6 | 37.1 | Na | na | 7.8 | 16.2 | na | na | 287.6; 0.000 |
| Yes | na | na | 87.6 | 85.5 | 76.7 | 82.0 | Na | na | −2.4 | −10.3 | na | na | 15.6; 0.000 |
| Birth order | |||||||||||||
| 1 | 37.9 | 48.7 | 41.9 | 46.2 | 52.4 | 46.6 | 28.5 | −14.0 | 10.3 | 13.4 | 38.3 | 7.6 | 24.6; 0.000 |
| 2 | 32.3 | 41.2 | 40.3 | 42.8 | 48.6 | 43.3 | 27.6 | −2.2 | 6.2 | 13.6 | 50.5 | 18.0 | 59.6; 0.000 |
| 3 | 28.6 | 38.7 | 38.3 | 40.3 | 48.8 | 41.7 | 35.3 | −1.0 | 5.2 | 21.1 | 70.6 | 26.1 | 74.2; 0.000 |
| 4 | 31.7 | 39.1 | 35.8 | 39.0 | 44.1 | 39.3 | 23.3 | −8.4 | 8.9 | 13.1 | 39.1 | 12.8 | 22.6; 0.000 |
| 5 | 30.8 | 30.6 | 25.4 | 27.4 | 31.7 | 28.6 | −0.6 | −17.0 | 7.9 | 15.7 | 2.9 | 3.6 | 1.17; 0.279 |
| Preceding birth interval | |||||||||||||
| First birth | 37.9 | 48.7 | 41.9 | 46.2 | 52.4 | 46.6 | 28.5 | −14.0 | 10.3 | 13.4 | 38.3 | 7.6 | 24.6; 0.000 |
| <36 months | 32.2 | 32.8 | 32.1 | 33.1 | 38.8 | 34.6 | 1.9 | −2.1 | 3.1 | 17.2 | 20.5 | 18.3 | 33.2; 0.000 |
| 36+ months | 28.6 | 38.8 | 32.4 | 36.3 | 42.2 | 36.7 | 35.7 | −16.5 | 12.0 | 16.3 | 47.6 | 8.8 | 48.1; 0.000 |
| % rural proportion | |||||||||||||
| Low rural prop | na | 71.5 | 69.5 | 74.5 | 75.6 | 73.3 | Na | −2.8 | 7.2 | 1.5 | na | 5.7 | 19.6; 0.000 |
| High rural prop | na | 25.5 | 20.6 | 22.9 | 29.3 | 24.6 | Na | −19.2 | 11.2 | 27.9 | na | 14.9 | 18.8; 0.000 |
| Community poverty rate | |||||||||||||
| Low | 40.3 | 28.3 | 34.6 | 48.6 | 47.6 | 43.3 | −29.8 | 22.3 | 40.5 | −2.1 | 18.1 | 68.2 | 241.4; 0.000 |
| High | 20.5 | 45.7 | 33.4 | 29.1 | 34.0 | 32.0 | 122.9 | −26.9 | −12.9 | 16.8 | 65.9 | −25.6 | 28.9; 0.000 |
| Community illiteracy rate | |||||||||||||
| Low | 44.0 | 28.3 | 32.6 | 52.0 | 45.8 | 43.1 | −35.7 | 15.2 | 59.5 | −11.9 | 4.1 | 61.8 | 103.8; 0.000 |
| High | 26.7 | 46.1 | 35.1 | 26.9 | 35.6 | 32.2 | 72.7 | −23.9 | −23.4 | 32.3 | 33.3 | −22.8 | 132.8; 0.000 |
| Community unemployment rate | |||||||||||||
| Low | 39.6 | 34.5 | 36.6 | 35.7 | 40.3 | 38.2 | −12.9 | 6.1 | −2.5 | 12.9 | 1.8 | 16.8 | 39.0; 0.000 |
| High | 28.0 | 38.8 | 32.1 | 37.3 | 47.9 | 36.9 | 38.6 | −17.3 | 16.2 | 28.4 | 71.1 | 23.5 | 20.5; 0.000 |
| Community media access | |||||||||||||
| High | na | 29.0 | 32.5 | 51.5 | 46.7 | 43.1 | Na | 12.1 | 58.5 | −9.3 | na | 61.0 | 169.2; 0.000 |
| Low | na | 45.5 | 35.0 | 28.7 | 36.5 | 33.6 | Na | −23.1 | −18.0 | 27.2 | na | −19.8 | 293.5; 0.000 |
| Community Disadvantage | |||||||||||||
| Least | 65.7 | 55.7 | 67.9 | 79.9 | 72.2 | 72.4 | −14.5 | 20.8 | 17.7 | −9.6 | 9.9 | 28.5 | 6.2; 0.013 |
| 2 | 27.5 | 52.5 | 54.2 | 58.3 | 39.7 | 48.0 | 90.9 | 3.2 | 7.6 | −31.9 | 44.4 | −24.4 | 9.1; 0.003 |
| 3 | 10.4 | 36.8 | 30.8 | 40.0 | 28.8 | 32.2 | 253.8 | −16.3 | 29.9 | −28.0 | 176.9 | −21.7 | 22.4; 0.000 |
| 4 | 17.9 | 37.5 | 20.4 | 20.9 | 30.5 | 24.5 | 109.5 | −45.6 | 2.5 | 45.9 | 70.4 | −18.7 | 55.3; 0.000 |
| Most | 8.7 | 26.4 | 12.0 | 7.7 | 19.1 | 12.6 | 203.4 | −54.5 | −35.8 | 148.1 | 119.5 | −27.7 | 201.9; 0.000 |
| Region | |||||||||||||
| North Central | 36.9 | 47.1 | 40.0 | 51.1 | 53.2 | 47.5 | 27.6 | −15.1 | 27.8 | 4.1 | 44.2 | 13.0 | 32.6; 0.000 |
| North East | 14.8 | 19.6 | 15.6 | 18.2 | 22.6 | 18.9 | 32.4 | −20.4 | 16.7 | 24.2 | 52.7 | 15.3 | 8.2; 0.004 |
| North West | 5.7 | 15.6 | 9.2 | 12.1 | 16.7 | 12.6 | 173.7 | −41.0 | 31.5 | 38.0 | 193.0 | 7.1 | 50.5; 0.000 |
| South East | 54.5 | 75.4 | 68.1 | 78.5 | 80.7 | 74.6 | 38.3 | −9.7 | 15.3 | 2.8 | 48.1 | 7.0 | 134.3; 0.000 |
| South-South | 41.7 | 59.6 | 48.6 | 46.1 | 54.2 | 49.5 | 42.9 | −18.5 | −5.1 | 17.6 | 30.0 | −9.1 | 1.4; 0.242 |
| South West | 71.6 | 76.6 | 73.8 | 76.5 | 81.1 | 76.5 | 7.0 | −3.7 | 3.7 | 6.0 | 13.3 | 5.9 | 14.9; 0.000 |
| Total | 32.0 | 37.9 | 33.9 | 36.6 | 42.4 | 37.5 | 18.4 | −10.6 | 8.0 | 15.8 | 32.5 | 11.9 | 39.43;0.000 |
All percentages calculated as [(b-a)/a * 100].
*Trend test of proportions across the survey year.
na, not available; SBA, skilled birth attendants.
The MDA
MDA technique is useful in decomposing changes or group differences in statistics such as; mean, proportion, and count in linear, logit and count multivariate models into characteristic and coefficient functions, respectively.41 The approach is an improvement of the Oaxaca-Blinder decomposition.42 43 It has been extended to non-linear models including logit and probit models.44 45 The main purpose of MDA is to determine explanatory variables attributed to changing composition or effects, especially in trends spanning overtime to explain the root cause of those changes.46–48 In this study, the options offered in multivariate decomposition were applied to construct a normalised decomposition towards limiting the bias associated with the choice of reference categories (the identification problem). MDA automatically determine the high-outcome group (SBA used) and reference the low-outcome group (SBA not used) in the analysis of group variables (dummy) which was set for ANOVA normalisation, such that the coefficients of the multivariate (logistic) regression for all the level of the categories approximately sum to zero.39 The decomposition or standardisation of the difference in the first moment (1. e proportion using SBA) was based on logit model and is thus a function of a linear combination of the predictors and the regression (logistic) coefficients and can be in general, additively decomposed into:
| (1) |
| (2) |
| (3) |
Where Y is the n x 1 vector of the dependent variable 0≤p≤1, X is the n x k matrices of the independent variables and β is the k x 1 vector of the regression coefficients in (1). The difference in the proportion of respondents using and not using SBA was decomposed in (2). In (3) the component {F () – F ()} refers to the differential attributable to differences in characteristics or endowment (explained component) while {F () – F ()} refers to the differential attributable to differences in coefficients or effects (unexplained component). denotes the proportion of mothers who used SBA (comparison group) while subscript denotes the proportion of mothers who did not utilise SBA (reference group).
Results
Characteristics of the studied women population
Table 1 shows the distribution of the sampled women. Nearly half (46.8%) of the respondents were aged 25–34 years. Around two-thirds of women have no education in the 1990 survey and it reduced to 44.3% in the 2018 survey. The proportion of partners without formal education decreased from 55.2% to 36.1% from the 1990 to 2018 surveys respectively. In all, about two-thirds (68.1%) of respondents reside in rural areas. Similarly, two-thirds (66.9%) of respondents were employed at the time of all the surveys. Most (94.2%) of respondents lives with a sexual partner over the five-survey period and the highest decline was between 1990 (95.9%) and 2003 (93.4%). Two-fifths (60.7%) of women have access to media in the 2003 survey but it declined to 40.3% in 2018. Also, most (47.7%) of respondents have less than 36 months’ birth interval. Low or high community poverty, illiteracy level, unemployment and media assessment were different among women.
Trends and bivariate analysis of SBA utilisation in Nigeria
Table 2 shows the prevalence, percentage change, and significance in the trend in SBA use by maternal characteristics over the study periods. The overall weighted prevalence of SBA use in 1990, 2003, 2008, 2013 and 2018 were 32.0%, 37.9%, 33.9%, 36.6% and 42.4%, respectively. The use of SBA increased by 18.4% between 1990 and 2003, decreased by 10.6% between 2003 and 2008, increased again by 8.0% between 2008 and 2013, and further by 15.8% between 2013 and 2018. In all, SBA use increased by 33% between 1990 and 2018 compared with only 12% between 2003 and 2018. These changes were significant over the studied period. Trends in SBA use were significant with all women characteristics considered.
Major significant changes were observed across maternal characteristics such as; respondent age, partner’s educational level, place of residence, mobility and birth interval, marital and socioeconomic status among other factors presented in table 2. There is a significant trend in SBA use over the intervals in all the geopolitical zone except in the south-south. Similarly, there was a significant trend in SBA use when both respondent and spouse decide on respondent healthcare and insignificant when either respondent or spouse decides alone. Also, there are significant trends in SBA use when mother’s ANC visits are adequate.
Subnational analysis of SBA use across states
Table 3 shows the prevalence and trend of SBA use in the states of Nigeria. Overall, the highest SBA use was in Osun (90.2%), Imo (87.3%) and Abia (84.1%) while the lowest use of SBA was in Kebbi (6.0%), Zamfara (6.5%) and Sokoto (6.6%). Between 2003 and 2018, SBA use reduced by 39.8% in Yobe, 34.4% in Niger, and 33.7% in Borno but increased by 2188.9% in Jigawa, 627.3% in Zamfara, and 3148% in Sokoto. There was no appreciable change in Lagos, Kebbi, Abia and Imo over the period.
Table 3.
Prevalence of SBA use by the states of residence of the participants
| State of residence | 1990 | 2003 | 2008 | 2013 | 2018 | All | 1990–2003 | 2003–2008 | 2008–2013 | 2013–2018 | 1990–2018 | 2003–2018 | Trend test (X2, p value) |
| Abia | na | 94.0 | 73.5 | 78.8 | 94.4 | 84.1 | na | −21.8 | 7.2 | 19.8 | na | 0.4 | 19.51, p<0.001 |
| Adamawa | 22.9 | 31.6 | 14.7 | 33.2 | 38.3 | 28.7 | 38.0 | −53.5 | 125.9 | 15.4 | 67.2 | 21.2 | 1.11,0.302 |
| Akwa Ibom | 45.6 | 48.5 | 39.4 | 42.6 | 37.3 | 40.8 | 6.4 | −18.8 | 8.1 | −12.4 | −18.2 | −23.1 | 1.71,0.196 |
| Anambra | 41.0 | 96.1 | 92.8 | 91.1 | 89.8 | 80.9 | 134.4 | −3.4 | −1.8 | −1.4 | 119.0 | −6.6 | 1.05,0.305 |
| Bauchi | 5.7 | 11.3 | 12.9 | 15.9 | 23.2 | 16.4 | 98.2 | 14.2 | 23.3 | 45.9 | 307.0 | 105.3 | 22.31, p<0.001 |
| Bayelsa | na | 23.3 | 17.3 | 21.5 | 24.3 | 21.1 | na | −25.8 | 24.3 | 13.0 | na | 4.3 | 0.88,0.347 |
| Benue | 45.7 | 55.3 | 48.5 | 58.6 | 65.5 | 56.0 | 21.0 | −12.3 | 20.8 | 11.8 | 43.3 | 18.4 | 3.02,0.083 |
| Borno | 15.1 | 33.2 | 15.0 | 21.4 | 22.0 | 19.9 | 119.9 | −54.8 | 42.7 | 2.8 | 45.7 | −33.7 | 29.76, p<0.001 |
| Cross River | 19.7 | 45.5 | 39.7 | 36.6 | 51.3 | 40.8 | 131.0 | −12.7 | −7.8 | 40.2 | 160.4 | 12.7 | 2.54,0.110 |
| Delta | na | 72.2 | 58.1 | 58.0 | 61.0 | 59.8 | na | −19.5 | −0.2 | 5.2 | na | −15.5 | 4.99,0.025 |
| Ebonyi | na | 36.5 | 42.4 | 55.9 | 46.6 | 47.7 | na | 16.2 | 31.8 | −16.6 | na | 27.7 | 1.01,0.314 |
| Edo | 62.9 | 69.3 | 77.8 | 76.9 | 88.5 | 78.1 | 10.2 | 12.3 | −1.2 | 15.1 | 40.7 | 27.7 | 0.66, 0.414 |
| Ekiti | na | 67.2 | 79.3 | 80.8 | 80.6 | 79.8 | na | 18.0 | 1.9 | −0.2 | na | 19.9 | 5.34,0.021 |
| Enugu | na | 81.0 | 55.5 | 84.5 | 92.0 | 79.8 | na | −31.5 | 52.3 | 8.9 | na | 13.6 | 38.18,0.000 |
| FCT-Abuja | 83.3 | 27.6 | 64.2 | 64.3 | 69.7 | 65.8 | −66.9 | 132.6 | 0.2 | 8.4 | −16.3 | 152.5 | 21.75,0.000 |
| Gombe | na | 22.7 | 15.5 | 16.0 | 17.3 | 16.6 | na | −31.7 | 3.2 | 8.1 | na | −23.8 | 1.24,0.264 |
| Imo | 66.9 | 93.2 | 92.3 | 93.3 | 93.6 | 87.3 | 39.3 | −1.0 | 1.1 | 0.3 | 39.9 | 0.4 | 0.31,0.576 |
| Jigawa | na | 0.9 | 5.0 | 9.5 | 20.6 | 11.7 | na | 455.6 | 90.0 | 116.8 | na | 2188.9 | 48.56,0.000 |
| Kaduna | 15.4 | 24.4 | 21.7 | 31.5 | 26.5 | 25.1 | 58.4 | −11.1 | 45.2 | −15.9 | 72.1 | 8.6 | 0.31,0.572 |
| Kano | 5.2 | 26.6 | 14.5 | 16.3 | 21.1 | 16.6 | 411.5 | −45.5 | 12.4 | 29.4 | 305.8 | −20.7 | 2.33,0.126 |
| Katsina | 3.5 | 19.2 | 5.1 | 7.6 | 19.6 | 10.9 | 448.6 | −73.4 | 49.0 | 157.9 | 460.0 | 2.1 | 0.59,0.439 |
| Kebbi | na | 3.8 | 6.3 | 8.5 | 3.8 | 6.0 | Na | 65.8 | 34.9 | −55.3 | na | 0.0 | 0.02,0.881 |
| Kogi | na | 77.1 | 64.2 | 71.0 | 70.0 | 69.0 | Na | −16.7 | 10.6 | −1.4 | na | −9.2 | 0.99,0.318 |
| Kwara | 53.1 | 72.1 | 48.1 | 73.7 | 58.8 | 60.6 | 35.8 | −33.3 | 53.2 | −20.2 | 10.7 | −18.4 | 0.63,0.426 |
| Lagos | 73.9 | 81.1 | 80.2 | 82.6 | 79.9 | 79.2 | 9.7 | −1.1 | 3.0 | −3.3 | 8.1 | −1.5 | 0.04,0.484 |
| Nasarawa | na | 27.7 | 31.4 | 45.0 | 57.1 | 44.5 | na | 13.4 | 43.3 | 26.9 | na | 106.1 | 25.68,0.000 |
| Niger | 27.7 | 36.0 | 17.0 | 25.0 | 23.6 | 22.9 | 30.0 | −52.8 | 47.1 | −5.6 | −14.8 | −34.4 | 7.74,0.005 |
| Ogun | 72.0 | 61.4 | 65.5 | 86.2 | 77.3 | 75.4 | −14.7 | 6.7 | 31.6 | −10.3 | 7.4 | 25.9 | 17.52,0.000 |
| Ondo | 57.2 | 68.0 | 50.5 | 55.7 | 82.2 | 62.7 | 18.9 | −25.7 | 10.3 | 47.6 | 43.7 | 20.9 | 1.03,0.309 |
| Osun | na | 86.5 | 88.9 | 88.9 | 93.2 | 90.2 | na | 2.8 | 0.0 | 4.8 | na | 7.7 | 0.74,0.388 |
| Oyo | 72.0 | 77.7 | 73.9 | 67.8 | 75.5 | 72.5 | 7.9 | −4.9 | −8.3 | 11.4 | 4.9 | −2.8 | 0.86,0.352 |
| Plateau | 19.2 | 42.9 | 27.9 | 40.0 | 44.2 | 35.3 | 123.4 | −35.0 | 43.4 | 10.5 | 130.2 | 3.0 | 6.11,0.013 |
| Rivers | 28.7 | 63.4 | 61.5 | 51.7 | 67.4 | 58.0 | 120.9 | −3.0 | −15.9 | 30.4 | 134.8 | 6.3 | 0.53,0.463 |
| Sokoto | 0.7 | 2.7 | 5.7 | 6.2 | 11.2 | 6.6 | 285.7 | 111.1 | 8.8 | 80.6 | 1500.0 | 314.8 | 1.47,0.225 |
| Taraba | na | 19.8 | 25.4 | 15.0 | 25.0 | 21.4 | na | 28.3 | −40.9 | 66.7 | na | 26.3 | 0.75,0.386 |
| Yobe | na | 22.6 | 10.2 | 12.2 | 13.6 | 12.6 | na | −54.9 | 19.6 | 11.5 | na | −39.8 | 4.01,0.045 |
| Zamfara | na | 1.1 | 5.7 | 6.4 | 8.0 | 6.5 | na | 418.2 | 12.3 | 25.0 | na | 627.3 | 4.07,0.043 |
| Total | 32.0 | 37.9 | 33.9 | 36.6 | 42.4 | 37.5 | 18.4 | −10.6 | 8.0 | 15.8 | 32.5 | 11.9 | 39.43,0.000 |
FCT, Federal Capital Territory; na, not available; SBA, skilled birth attendants.
Multivariate decomposition of SBA used from 2003 to 2018
The decomposition of the change in SBA utilisation between 2003 and 2018 revealed that 11.5% of the overall percentage change can be attributed to differences in characteristics effects (explained/endowment component) while the remaining 88.5% is due to differences in coefficient effects (unexplained/coefficient component). In general, increase in SBA use from 2003 to 2018 is more attributed to the difference in characteristics effect (behavioural changes) than the changes in compositional factors among women respondents. However, the most significant contributions to change in SBA utilisation based on the compositional factors, was observed in who decides on women healthcare utilisation. Compared with the utilisation when spouses alone made the decisions, there was a 61.3% increment in SBA utilisation between 2003 and 2018 when such decisions were made by the respondents alone. Also, residing in the states with a high rural population percentage contributed 88% to changes in the utilisation of SBA as shown in table 4. Women and partners’ educational levels however contributed significant change to SBA use through primary and secondary/tertiary attainment respectively. While the SBA use was reduced by the educational attainment of the respondents, it nonetheless increased with higher educational attainment among the spouses. Though at a low proportion, maternal age and religion also contributed significantly to the positive change in SBA use.
Table 4.
Decomposition of change in utilisation of SBA in Nigeria from 2003 to 2018
| Characteristics | Difference due to characteristics (E) | Difference due to coefficients (C) | ||||
| Coefficient | P value | Per cent | coefficient | P value | Per cent | |
| Respondent’s age | ||||||
| 15–24 | Ref | |||||
| 25–34 | 0.0000 | 0.037 | 0.1 | −0.0003 | 0.969 | −0.6 |
| 35–49 | 0.0006 | 0.008 | 1.3 | −0.0031 | 0.495 | −7.0 |
| Highest educational level | ||||||
| No education | Ref | |||||
| Primary | −0.0027 | 0.000 | −6.2 | −0.0015 | 0.641 | −3.4 |
| Secondary+ | 0.0097 | 0.000 | 21.9 | −0.0057 | 0.156 | −13.1 |
| Husband/partner’s education level | ||||||
| No education | Ref | |||||
| Primary | −0.0027 | 0.004 | −6.0 | 0.0089 | 0.024 | 20.2 |
| Secondary+ | 0.0059 | 0.000 | 13.3 | 0.0083 | 0.134 | 18.8 |
| Employment status | ||||||
| Employed | −0.0001 | 0.655 | −0.1 | 0.0080 | 0.624 | 18.2 |
| Sex of household head | ||||||
| Male | 0.0000 | 0.525 | 0.0125 | 0.518 | 28.3 | |
| Media access | ||||||
| No | −0.0058 | 0.000 | −13.1 | −0.0082 | 0.087 | −18.6 |
| Wealth index | ||||||
| Poorest | −0.0014 | 0.000 | −3.2 | −0.0028 | 0.610 | −6.3 |
| Poorer | −0.0026 | 0.000 | −5.9 | −0.0064 | 0.153 | −14.6 |
| Middle | −0.0003 | 0.000 | −0.7 | −0.0002 | 0.958 | −0.5 |
| Richer | 0.0005 | 0.000 | 1.1 | −0.0010 | 0.765 | −2.2 |
| Richest | Ref | |||||
| No of ANC visits during pregnancy | ||||||
| None (0) | Ref | |||||
| Inadequate (less than 4) | 0.0050 | 0.000 | 11.5 | −0.0038 | 0.138 | −8.7 |
| Adequate (four or more) | 0.0127 | 0.000 | 28.9 | −0.0127 | 0.126 | −28.8 |
| Religion | ||||||
| Islam | Ref | |||||
| Christianity | 0.0004 | 0.000 | 0.9 | −0.0131 | 0.027 | −29.7 |
| Others | 0.0006 | 0.042 | 1.4 | 0.0004 | 0.656 | 0.8 |
| Tribe/Ethnic group | ||||||
| Hausa/Fulani | Ref | |||||
| Yoruba | −0.0002 | 0.000 | −0.4 | −0.0010 | 0.691 | −2.3 |
| Igbo | 0.0010 | 0.000 | 2.2 | −0.0075 | 0.020 | −17.2 |
| Others | −0.0013 | 0.000 | −2.9 | −0.0053 | 0.347 | −12.1 |
| A person who usually decides on respondent’s healthcare | ||||||
| Spouse alone | Ref | |||||
| Both | −0.0023 | 0.166 | −5.1 | 0.0007 | 0.756 | 1.5 |
| Respondent alone | 0.0008 | 0.538 | 1.8 | 0.0270 | 0.029 | 61.3 |
| Distance to HC is a big problem | ||||||
| Yes | −0.0006 | 0.023 | −1.3 | 0.0112 | 0.004 | 25.4 |
| Getting permission to go to HC is a big problem | ||||||
| Yes | −0.0002 | 0.139 | −0.4 | −0.0003 | 0.910 | −0.7 |
| Wanted the last-child | ||||||
| Wanted then | Ref | |||||
| Wanted later | 0.0002 | 0.298 | 0.4 | −0.0016 | 0.336 | −3.6 |
| Wanted no more | −0.0001 | 0.468 | −0.2 | −0.0007 | 0.528 | −1.5 |
| Family mobility | ||||||
| Mobile (<5 years) | −0.0017 | 0.000 | −3.9 | 0.0042 | 0.149 | 9.5 |
| Birth Interval | ||||||
| First birth | Ref | |||||
| <36 months | −0.0006 | 0.000 | −1.3 | 0.0109 | 0.185 | 24.7 |
| 36+ months | 0.0001 | 0.001 | 0.2 | 0.0048 | 0.466 | 10.9 |
| Place of residence | ||||||
| Rural | −0.0001 | 0.002 | −0.3 | 0.0004 | 0.962 | 0.9 |
| States rural population percentage | ||||||
| Low | Ref | |||||
| High | 0.0009 | 0.000 | 2.0 | −0.0388 | 0.002 | −88.1 |
| Community socioeconomic status disadvantage | ||||||
| Least disadvantage | −0.0105 | 0.000 | −23.9 | 0.0007 | 0.425 | 1.5 |
| Less disadvantage | 0.0002 | 0.481 | 0.4 | −0.0019 | 0.637 | −4.4 |
| Disadvantage | 0.0005 | 0.639 | 1.2 | −0.0026 | 0.619 | −5.9 |
| More disadvantage | −0.0008 | 0.080 | −1.9 | 0.0063 | 0.111 | 14.3 |
| Most disadvantage | Ref | |||||
| Constant | 0.0534 | 0.244 | 121.3 | |||
| E | 0.0051 | 0.138 | 11.5 | 0.0390 | 0.000 | 88.5 |
| R | −0.0529 | 0.000 | ||||
ANC, antenatal care; HC, healthcare; SBA, skilled birth attendants.
Based on the coefficient effect, a significant impact on the observed positive change in SBA use was also observed when household heads are males. Factors including partner’s education and distance to healthcare providers also showed a significant effect on the positive change in SBA use (table 4).
State-level decomposition analysis
In all, there were significant increments in SBA use between 2003 and 2018 in FCT, Jigawa, Sokoto, Zamfara, Ekiti, Edo, Ogun, Benue, Ondo, Enugu, Nasarawa and Bauchi states. There was a significant decrease in SBA use between 2003 and 2018 in Yobe, Borno and Niger states. Other states had insignificant changes over the period. Due to insufficient sample sizes, FCT, Jigawa, Sokoto and Zamfara states with a significant increase in SBA utilisation were excluded from the state-level decomposition analysis.
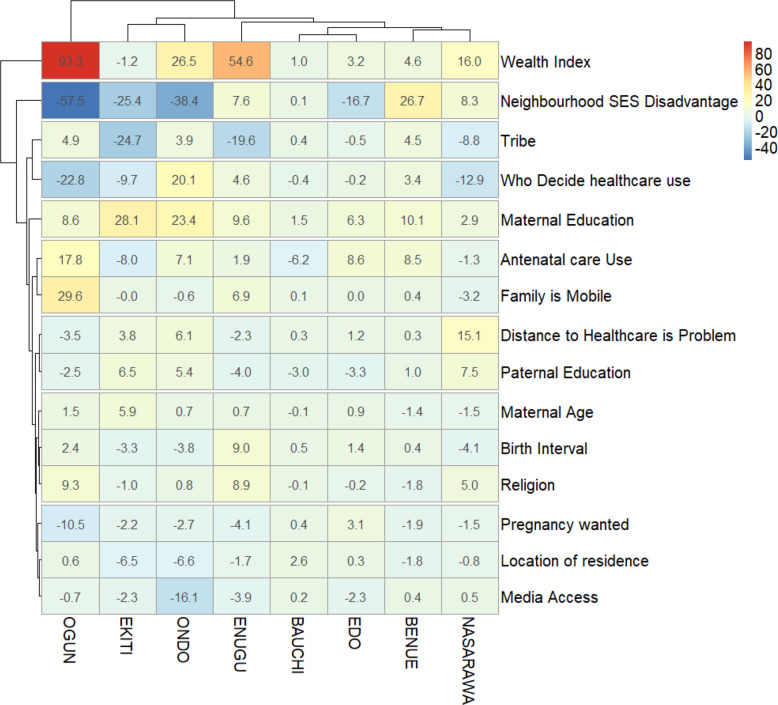
Decomposition analysis of factors associated with increase in SBA use among states
As shown in figure 2, the contributors to the increased changes in SBA use are mostly household wealth index, neighbourhood SES disadvantage, tribe, decision-takers on women healthcare utilisation and women educational attainment. The household wealth index contributed mostly to the increment recorded between 2003 and 2018 in SBA use with 93% in Ogun and 55% in Enugu, 27% in Ondo and 16% in Nasarawa. This was followed by neighbourhood SES disadvantage which contributed 58% to the increments in Ogun, 38% in Ondo, 27% in Benue and 25% in Ekiti.
Figure 2.
A decomposition analysis of factors associated with increase in SBA utilisation from 2003 to 2018 by states in Nigeria. SBA, skilled birth attendants; SES, socioeconomic status.
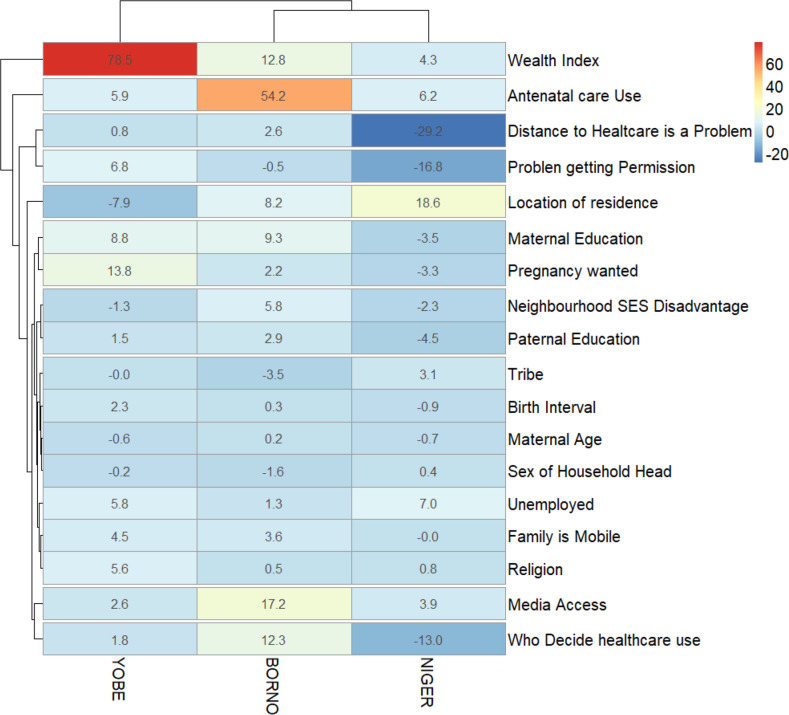
Decomposition analysis of factors associated with decreased in SBA use among states
The decomposition analysis of the factors contributing to the reduction in SBA use between 2003 and 2018 is shown in figure 3. In Yobe, differences in household wealth index contributed mostly (79%) to the changes in SBA use followed by whether or not the pregnancy was wanted as of the time of its conception (14%). Having problem with distance to healthcare centres was the greatest contributor to the reduction in SBA use during the period (29.2%), followed by the place of residence (19%), having a problem getting permission to go to healthcare (17%) in Niger and the person who decide healthcare utilisation (13%) while ANC use (54%) and media access (17%) were the greatest contributors to the differences in SBA use in Borno.
Figure 3.
A decomposition analysis of factors associated with decrease in SBA utilisation from 2003 to 2018 by states in Nigeria. SBA, skilled birth attendants; SES, socioeconomic status.
Discussion
The integral focus of this study is to evaluate levels, trends and identify factors that drive the changes in SBA use over the years. We applied MDA to assess the contributions of the key factors to the changes in SBAs utilisation over time.
Two-fifths of women used SBA in the last three decades in Nigeria. We found that SBA use has increased generally by 33% between 1990 and 2018, but the increase was not steady during the earlier part of the interval. However, a percentage increase of 12% in SBA use was observed between 2003 and 2018. It is worth noting that a 16% increase in SBA use was recorded in the last 5 years of the interval studied compared with only 6% upward trends between 2003 and 2013 reported in a previous study in Nigeria.4 The increase can be credited to various capacity-building programmes and government involvement in healthcare funding as well as the support of non-governmental organisation that have hitherto strengthened the community healthcare system and enhanced women empowerment schemes.9 49 Nonetheless, the overall 12% increase in SBA use between 2003 and 2018 translated to less than 1% increment every year. At this rate, efforts modelled towards the realisation of SDG will be weakened and Nigeria may not achieve the SDG goal on health for all.
The factors contributing to SBA use over the studied period include demographic/cultural/societal factors, perceived health benefits, corporal convenience, and economic factors. Nonetheless, trends in SBA use were insignificant among women from female-headed households but significant in male-headed households. This was in agreement with the findings of a study in northern Nigeria27 but in consonance with another study in southern Nigeria.14
Similarly, trends in SBA use were insignificant at higher birth orders but significant for lower birth orders. Trends in SBA use was also significant among women with adequate ANC visit and when both respondent and spouse decide on the woman’s healthcare. The relationship between women’s ANC and SBA utilisation has been documented.7 Whereas, an insignificant trend was found when women’s ANC visit is inadequate and when a spouse decides on healthcare alone. All regions other than south-south, other tribes apart from Hausa/Fulani, Igbo and Yoruba and other religions apart from Islam and Christianity did not have significant linear trends in SBA changes.
We employed the MDA to determine the contribution of individual women characteristics marked in the bivariate analysis of changes in the SBA use. Over 1/10th, (11.5%) of the changes in SBA use was due to characteristics component while nearly 9/10th (88.5%) of those changes in SBA use were attributed to coefficient effect component, which implies that policies that strengthens SBA use in addition to quality childbirth services could ultimately increase SBA use by nearly nine times more than relying on the basic existing healthcare system function. The major compositional contributor to changes in SBA utilisation was among the women who make decisions about respondents’ healthcare utilisation as it contributed a substantial 61% to increment in SBA use between 2003 and 2018. This is a signal that pregnant women are in the best position to decide on their healthcare utilisation. Whether distance to healthcare was a big problem for the respondents or not also contributed to the explained changes in SBA use. Women’s use of SBAs was not motivated by long-distance healthcare facilities. On the contrary, the closeness of health facilities, especially, the facilities with SBA have increased SBA use over the studied periods. This finding corroborates the outcomes of earlier studies which reported that long distances prevent the use of SBA in Ogun state Nigeria and healthcare distance is a determinant of SBA use in northern Ghana.14 20 This positive development could be attributed to an upsurge in the number of health facilities in Nigeria over the years. The increase in the number of health facilities could have reduced distances travelled to access skill delivery services. Unsurprisingly, residing in states with high rural population proportion however contributed a huge decrease to SBA use. This is due to poor household social-economic class, low patronage/lack of healthcare centres, low educational level and preference for use of traditional births attendants among other factors associated with barriers to use of SBA among rural community dwellers.19 27 43
Spouses with at least primary education contributed to change in SBA use, respondents, and spouses’ educational level however both contributed significantly to changes in SBA use. Adequacy of ANC visits contributed to a positive significant change in SBA use. This is a pointer to the fact that, for SBA use, pregnant women must be enrolled and kept in the continuum of care. Even though at low proportion, religion and family mobility contributed to change in SBA use respectively. Tribe and birth order contributed both positively and negatively to the significant change in SBA use. Impact of education, ANC visit, ethnicity, and religion has also been reported as an important set of contributors to SBA use.4 19–22
We further decomposed the characteristics that contribute to SBA use at the state level. The highest SBA use was found among the Southern states with at least 4 of every 5 women using an SBA during the most recent childbirth in Osun, Imo, and Abia compared with barely one SBA user in every 5 women in Kebbi, Zamfara and Sokoto. We found significant increments in SBA use in FCT, Jigawa, Sokoto, Zamfara, Ekiti, Edo, Ogun, Benue, Ondo, Enugu, Nasarawa and Bauchi states. On trends, SBA use reduced by 40% in Yobe, 34% in both Niger and Borno between 2003 and 2018. However, the greatest increment during the same period was in the north, with Jigawa recording over 2000%, Zamfara over 600% and over 300% increase in Sokoto. There was a significant decrease in SBA use between 2003 and 2018 in Yobe, Borno and Niger states. There are needs for the states with negative changes to benchmark what is been done right in the state with high prevalence, and high increase in SBA use.
Household wealth index contributed most to the rise in SBA use in Ogun, Enugu, Ondo, and Nasarawa states. Differences in community socioeconomic status disadvantage also contributed to an increase in SBA use in Ogun, Ondo, Benue and Ekiti. Fall in SBA use was however stimulated by long-distance to healthcare in Niger, tribe/ethnicity in Borno, and place of residence in Yobe states. The effect of household wealth status differences observed in our study is in agreement with the outcome of the study on the practice of SBAs in Bangladesh.50
Conclusions
With only a 12% increment over 15 years, progress made in SBA use in Nigeria is both low and slow. Overall, nine in a tenth of the changes in SBA was due to the coefficient’s component. Women’s sociodemographic, health, economic and corporal factors are significantly associated with an increase and decrease in SBA use over the studied period. Women’s ability to decide on their healthcare utilisation alone contributed mostly to an increase in SBA use while residing in states with a high rural population decreased SBA use most. Women/partners’ education and ANC adequacy contributed to a rise in SBA use while tribe, place of residence and distance to healthcare contributed to a fall in SBA use in northern states. Household wealth however contributed to an increase in SBA use in some states.
Recommendations
Based on our findings, we recommend the implementation of interventions that could increase the use of SBAs. Our findings suggested that a multisectoral approach will yield the desired change as there are urgent needs to accelerate SBA progress towards 100% utilisation. Moreover, the northern sub nationals where poor SBA persists, need to emulate southern states on what works and what doesn’t work. Maternal health programmers should rekindle their commitment towards eliminating barriers to SBA use and adopt interventions focusing on strengthening the capacity of women in healthcare autonomy and education. There is also a need for healthcare capacity development to increase access to trained and qualified SBAs and other professional health workers especially in rural communities. Further study on contextual analysis of respondents and spouse decision making regarding the use of SBA is essential to the development of interventional strategies.
Supplementary Material
Acknowledgments
The authors thank the ICF for granting access to the dataset. [Dataset] 44. 1990-2018 data from; National Population Commission (NPC) [Nigeria] and ICF International, DHS Data Reprository dhsprogram.com “Nigeria Demographic and Health Survey 2018,” Abuja, Nigeria, And Rockville, Maryland, USA, 2019.
Footnotes
Contributors: AFF conceptualised the study, designed the study, AFF and OKO analysed the data, provided the visualisations and wrote the results. OKO searched for the literatures. All authors contributed to the literature review, data interpretation, writing of the manuscript and abstract. All authors read, scrutinised and approved the final version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available in a public, open access repository. Data are available on reasonable request. The anonymised data are available in the public domain. The data supporting this article is available on request at www.dhsprogram.com. Extra data are available by emailing Bridgette Wellington (thedhsprogram@gmail.com) the Data Archivist.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by ICF Institutional Review Board with ref Number FWA000008450 and ID number 144644. Participants gave informed consent to participate in the study before taking part.
References
- 1.Tey N-P, Lai S-li. Correlates of and barriers to the utilization of health services for delivery in South Asia and sub-Saharan Africa. ScientificWorldJournal 2013;2013:1–11. 10.1155/2013/423403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO . Who recommendation on antenatal care for a positive pregnancy experience 2016. [PubMed]
- 3.Afulani PA, Moyer C. Explaining disparities in use of skilled birth attendants in developing countries: a new conceptual framework. Ann Glob Health 2016;82:375. 10.1016/j.aogh.2016.04.602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fagbamigbe AF, Hurricane-Ike EO, Yusuf OB, et al. Trends and drivers of skilled birth attendant use in Nigeria (1990-2013): policy implications for child and maternal health. Int J Womens Health 2017;9:843–53. 10.2147/IJWH.S137848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fapohunda B, Orobaton N. Factors influencing the selection of delivery with no one present in northern Nigeria: implications for policy and programs. Int J Womens Health 2014;6:171–83. 10.2147/IJWH.S54628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Austin A, Fapohunda B, Langer A, et al. Trends in delivery with no one present in Nigeria between 2003 and 2013. Int J Womens Health 2015;7:345–56. 10.2147/IJWH.S79573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olakunde BO, Adeyinka DA, Mavegam BO, et al. Factors associated with skilled attendants at birth among married adolescent girls in Nigeria: evidence from the multiple indicator cluster survey, 2016/2017. Int Health 2019;11:545–50. 10.1093/inthealth/ihz017 [DOI] [PubMed] [Google Scholar]
- 8.WHO . Trends in maternal mortality 2000 to 2017: estimates by who, UNICEF, UNFPA, world bank group and the United nations population division: Executive summary, 2019. Available: https://apps.who.int/iris/handle/10665/327596
- 9.United Nations . Sustainable development goals (SDG. Washington, DC, 2015. [Google Scholar]
- 10.National Population Commission(NPC)[Nigeria] and ICF International. Nigeria Demographic and Health Survey 2018 2019. [Google Scholar]
- 11.National Population Commission(NPC)[Nigeria] and ICF International. Nigeria Demograhic Health Survey, 2013 Abuja, 2014. [Google Scholar]
- 12.Akinyemi JO, Afolabi RF, Awolude OA. Patterns and determinants of dropout from maternity care continuum in Nigeria. BMC Pregnancy Childbirth 2016;16:282. 10.1186/s12884-016-1083-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chukwuma A, Wosu AC, Mbachu C, et al. Quality of antenatal care predicts retention in skilled birth attendance: a multilevel analysis of 28 African countries. BMC Pregnancy Childbirth 2017;17:152. 10.1186/s12884-017-1337-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olowokere AE, Oyedele AT, Komolafe AO, et al. Birth preparedness, utilization of skilled birth attendants and delivery outcomes among pregnant women in Ogun state, Nigeria. Eur J Midwifery 2020;4:22. 10.18332/ejm/120116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Graham WJ, Hussein J. Universal reporting of maternal mortality: an achievable goal? International Journal of Gynecology & Obstetrics 2006;94:234–42. 10.1016/j.ijgo.2006.04.004 [DOI] [PubMed] [Google Scholar]
- 16.Gabrysch S, Campbell OMR. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth 2009;9:34. 10.1186/1471-2393-9-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kyei NNA, Campbell OMR, Gabrysch S. The influence of distance and level of service provision on antenatal care use in rural Zambia. PLoS One 2012;7:e46475. 10.1371/journal.pone.0046475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fapohunda BM, Orobaton NG. When women deliver with no one present in Nigeria: who, what, where and so what? PLoS One 2013;8:e69569. 10.1371/journal.pone.0069569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manyeh AK, Akpakli DE, Kukula V, et al. Socio-Demographic determinants of skilled birth attendant at delivery in rural southern Ghana. BMC Res Notes 2017;10:268. 10.1186/s13104-017-2591-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dickson KS, Amu H. Determinants of skilled birth attendance in the Northern parts of Ghana. Adv Public Health 2017;2017:1–8. 10.1155/2017/9102808 [DOI] [Google Scholar]
- 21.Yaya S, Bishwajit G, Ekholuenetale M, et al. Factors associated with maternal utilization of health facilities for delivery in Ethiopia. Int Health 2018;10:310–7. 10.1093/inthealth/ihx073 [DOI] [PubMed] [Google Scholar]
- 22.Negero MG, Mitike YB, Worku AG, et al. Skilled delivery service utilization and its association with the establishment of women's health development Army in Yeky district, South West Ethiopia: a multilevel analysis. BMC Res Notes 2018;11:83. 10.1186/s13104-018-3140-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fagbamigbe AF, Idemudia ES. Barriers to antenatal care use in Nigeria: evidences from non-users and implications for maternal health programming. BMC Pregnancy Childbirth 2015;15:1–10. 10.1186/s12884-015-0527-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fagbamigbe AF, Idemudia ES. Wealth and antenatal care utilization in Nigeria: policy implications. Health Care Women Int 2017;38:17–37. 10.1080/07399332.2016.1225743 [DOI] [PubMed] [Google Scholar]
- 25.Fagbamigbe AF, Olaseinde O, Setlhare V. Sub-national analysis and determinants of numbers of antenatal care contacts in Nigeria: assessing the compliance with the who recommended standard guidelines. BMC Pregnancy Childbirth 2021;21:1–20. 10.1186/s12884-021-03837-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oyedele OK, Fagbamigbe AF, Ayeni O. Modelling time-to-discontinuation of exclusive breastfeeding: analysis of infants and under-2 survival in Nigeria. Etude la Popul. Africaine 2020;34. [Google Scholar]
- 27.Adewemimo AW, Msuya SE, Olaniyan CT, et al. Utilisation of skilled birth attendance in northern Nigeria: a cross-sectional survey. Midwifery 2014;30:e7–13. 10.1016/j.midw.2013.09.005 [DOI] [PubMed] [Google Scholar]
- 28.National Population Commission(NPC)[Nigeria] & ICF International . Nigeria Demographic and Health Survey. In: DHS measure macro, New York and Nigeria population Commission. Abuja, Nigeria, 2008. [Google Scholar]
- 29.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 2007;4:e296–7. 10.1371/journal.pmed.0040296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Idowu A, Olowookere SA, Abiola OO, et al. Determinants of skilled care utilization among pregnant women residents in an urban community in Kwara state, northcentral Nigeria. Ethiop J Health Sci 2017;27:291–8. 10.4314/ejhs.v27i3.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Adedokun ST, Uthman OA. Women who have not utilized health service for delivery in Nigeria: who are they and where do they live? BMC Pregnancy Childbirth 2019;19:1–14. 10.1186/s12884-019-2242-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shivalli S, Kaup S. Comment on "The Prevalence of Skilled Birth Attendant Utilization and Its Correlates in North West Ethiopia". Biomed Res Int 2015;2015:1–2. 10.1155/2015/379836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ameyaw EK, Dickson KS. Skilled birth attendance in Sierra Leone, niger, and Mali: analysis of demographic and health surveys. BMC Public Health 2020;20:1–10. 10.1186/s12889-020-8258-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fagbamigbe AF, Bello S, Salawu MM, et al. Trend and decomposition analysis of risk factors of childbirths with no one present in Nigeria, 1990–2018. BMJ Open 2021;11:e054328–2018. 10.1136/bmjopen-2021-054328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ryvicker M. A conceptual framework for examining healthcare access and navigation: a behavioral-ecological perspective. Soc Theory Health 2018;16:224–40. 10.1057/s41285-017-0053-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koletsi D, Pandis N. The chi-square test for trend. Am J Orthod Dentofacial Orthop 2016;150:1066–7. 10.1016/j.ajodo.2016.10.001 [DOI] [PubMed] [Google Scholar]
- 37.Rao JNK, Thomas DR. Analysis of categorical response data from complex surveys: an appraisal and update. Anal. Surv. Data 2003;1989:85–108. [Google Scholar]
- 38.Skinner CJ, Skinner C. Analysis of categorical data for complex surveys article (accepted version) (Refereed) analysis of categorical data for complex surveys 2018.
- 39.Powers DA, Yoshioka H, Yun M-S. mvdcmp: multivariate decomposition for nonlinear response models. Stata J 2011;11:556–76. 10.1177/1536867X1201100404 [DOI] [Google Scholar]
- 40.UN Department of Economics and Social Affairs . World Population Prospects - Population Division - United Nations. The International Journal of Logistics Management 2015;9:1–13 https://esa.un.org/unpd/wpp/ [Google Scholar]
- 41.Powers DA, Yoshioka H, Yun M-S. Mvdcmp: multivariate decomposition for nonlinear response models. Stata J 2011;11:556–76. 10.1177/1536867X1201100404 [DOI] [Google Scholar]
- 42.Blinder AS. Wage discrimination: reduced form and structural estimates. J Hum Resour 1973;8:436–55. 10.2307/144855 [DOI] [Google Scholar]
- 43.Oaxaca R. Male-Female wage differentials in urban labor markets. Int Econ Rev 1973;14:14:693–709. 10.2307/2525981 [DOI] [Google Scholar]
- 44.Pritchett J, Yun M-S. The in-hospital mortality rates of slaves and freemen: evidence from Touro Infirmary, new Orleans, Louisiana, 1855–1860. Explor Econ Hist 2009;46:241–52. 10.1016/j.eeh.2008.09.001 [DOI] [Google Scholar]
- 45.Bowblis JR, Yun M-S. Racial and ethnic disparities in the use of drug therapy. Soc Sci Res 2010;39:674–84. 10.1016/j.ssresearch.2010.03.010 [DOI] [Google Scholar]
- 46.Pillai V, Teboh C. A decade of contraceptive use in Cameroon: influences of structural changes. Open Access J. Contracept 2010;2:5–11. 10.2147/OAJC.S12621 [DOI] [Google Scholar]
- 47.Worku AG, Tessema GA, Zeleke AA. Trends of modern contraceptive use among young married women based on the 2000, 2005, and 2011 Ethiopian demographic and health surveys: a multivariate decomposition analysis. PLoS One 2015;10:e0116525–14. 10.1371/journal.pone.0116525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Muhoza DN, Rutayisire PC, Umubyeyi A. Measuring the success of family planning initiatives in Rwanda: a multivariate decomposition analysis. J Popul Res 2016;33:361–77. 10.1007/s12546-016-9177-9 [DOI] [Google Scholar]
- 49.NPHCDA . Minimum standards for primary health care in Nigeria. Production of department of planning, research and statistics, Port-Harcourt Crescent, Garki II, Abuja, 2012. [Google Scholar]
- 50.Kibria GMA, Burrowes V, Choudhury A, et al. A comparison of practices, distributions and determinants of birth attendance in two divisions with highest and lowest skilled delivery attendance in Bangladesh. BMC Pregnancy Childbirth 2018;18:122. 10.1186/s12884-018-1770-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available in a public, open access repository. Data are available on reasonable request. The anonymised data are available in the public domain. The data supporting this article is available on request at www.dhsprogram.com. Extra data are available by emailing Bridgette Wellington (thedhsprogram@gmail.com) the Data Archivist.