Abstract
Background
Patient safety competencies in nursing are essential for the quality of healthcare. To develop practices and collaboration in nursing care, valid instruments that measure competencies in patient safety are needed.
Objective
To identify instruments that measure the patient safety competencies of nurses.
Design
A scoping review.
Data sources
The Cochran Library, Epistemonikos, Eric, Ovid Medline, CINAHL, Embase and Web of Science databases were searched for articles reporting on instruments measuring patient safety competence in nursing. The search was limited to English peer-reviewed scientific papers published from January 2010 to April 2021.
Review method
A blinded selection of articles fulfilling the inclusion criteria was performed by two researchers based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews. Data were then extracted, synthesised and presented in tables and text.
Results
Our search identified 1,426 papers, of which 32 met the inclusion criteria. The selected papers described nine instruments, of which the ‘Health Professional Education in Patient Safety Survey’ was the most used instrument. The identified instruments comprised domains for patient safety skills, attitudes, knowledge, communication, teamwork and errors. The instruments had been tested for content (face) and construct validity as well as for reliability. However, sensitivity and responsiveness were rarely assessed.
Conclusions
Over the last decade, there has been a growing body of instruments aimed at measuring patient safety competencies among nurses. The future development of new instruments should consider including the important dimension of ethics in patient safety as well as evaluating the instrument’s responsiveness to be able to track changes over time.
Keywords: Professional Competence, Patient safety, Quality improvement
Key messages.
What is already known on the topic?
Due to an increased focus on patient safety, several instruments that measure patient safety competencies have arisen over the last few years. The instruments vary on aspects of patient safety and the intended group of healthcare professionals they assess.
What this study adds?
Our review identified instruments for measuring patient safety competencies in nursing; however, we found that ethics are a missing part of the instruments, even though this is a central aspect of patient safety. Moreover, responsiveness, which is important for evaluating quality improvement projects and education, was seldom reported.
How this study might affect research, practice or policy?
Our study has identified instruments that are possible to use in a clinical setting. Easy access to this new information might inspire healthcare providers to apply these instruments in their hospital wards and education programmes to improve patient safety.
Background
Patient safety competencies (PSC) in nursing are essential for healthcare quality and for nurses to address patient safety through their full scope of nursing practice.1 The core values for healthcare are quality and safety in accordance with the ethical principles to do no harm and always include preventive safety measures in patient care.1 Nurses spend most of their time at the bedside of patients and have a critical role and responsibility to identify patient safety risks.2 3 Furthermore, they assure that patients receive safe and high-quality care through all disease trajectories.2
Patient safety in nursing is achieved through advocating for patient safety, safeguarding patient care and reporting adverse events.4 5 However, the healthcare system is continually haunted by quality and safety issues.4 Healthcare errors occur at a high rate and 1 in 10 patients is affected by adverse events due to patient safety failures.6 The economic impact of medical errors is substantial, and the annual cost of adverse events, just in UK hospitals, is 728 million pounds sterling per year and, in total, over the developed countries, the costs are 606 billion US dollars.6 7 The personal costs are even higher, when pain, loss in quality of life, and even death have been caused by an unwanted event.8 PSC are, therefore, crucial for all personnel caring for patients to ensure that errors and adverse events are systematically prevented.
Nurse PSC consist of having a professional attitude combined with values, knowledge, self-efficacy and skills.9 PSC in nursing range from specific knowledge and tasks to safety in teamwork and systems thinking. In terms of frameworks, nursing knowledge and skills have been defined in domains such as patient safety culture, teamwork, communication, human and system factor optimisation, recognition, response to and disclosure of patient safety incidents.10 Other frameworks have included domains such as person-centred care, therapeutic communication, clinical reasoning and evidence-based infection control and prevention.11 Furthermore, PSC represent an integral part of other nursing competencies, although a consensus has never been reached.9
Several PSC instruments have been developed over the last two decades.12 Using instruments to measure PSC is considered an effective strategy with low economic costs in relation to both time and money.12 An overview that identifies instruments that measure PSC was last published in 2011.13 Since then, several instruments have emerged and a new review is warranted. Furthermore, a summary of available instruments may facilitate the process of selecting the most suitable outcome measure for education and quality improvement projects on PSC development in nursing as well as identifying instruments that have been tested for reliability and validity.
Objective(s)
This scoping review aims to identify instruments that measure PSC in nursing, including their content, validity and reliability.
Method(s)
A scoping review based on Arksey and O'Malley’s framework was chosen to explore the literature for instruments that measure PSC in nursing.14The framework consists of five stages: identifying the research question, identifying relevant studies, selecting the studies, charting the data and collating, summarising and reporting the results.14 Furthermore, the review was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews.15
Identifying the research question and relevant studies
In the first stage, we developed the research questions, search terms and a search strategy. The PICOS (Population, Intervention, Comparison, Outcome, Study) framework was used to support searches in which the population referred to nurses, intervention to patient safety, outcomes to questionnaires/instruments that measure skills, knowledge, attitude and self-efficacy in patient safety and study to a quantitative study design.16 A combination of search terms with free words and medical subject headings (MeSH) terms was used and the terms were combined with Boolean operators as follows: (nurse OR RN OR nursing student OR nursing staff OR licensed practical nurse) AND (questionnaire OR instrument OR measure OR survey OR tool) AND (learning OR clinical competence OR curriculum OR learning OR in-service training OR competenc*) AND (patient safety OR safety). The searches were limited to the last 10 years, from January 2010 to April 2021. In addition, the searches were limited to original, peer-reviewed scientific studies published in the English language. Electronic searches were then carried out in the Cochran Library, Epistemonikos, ERIC, Ovid MEDLINE, CINAHL, Embase and the Web of Science databases, and a grey literature search was performed in Google Scholar. The planning of databases and search terms was conducted in collaboration with a health science librarian.
Selecting the studies
In the second stage, articles were selected based on the inclusion criteria. An article was included if all criteria were fulfilled: (1) the full text was in English, (2) the study included a questionnaire or instruments measuring nurses’ PSC, (3) the article was original and peer-reviewed and (4) the target group included nurses/nursing students.
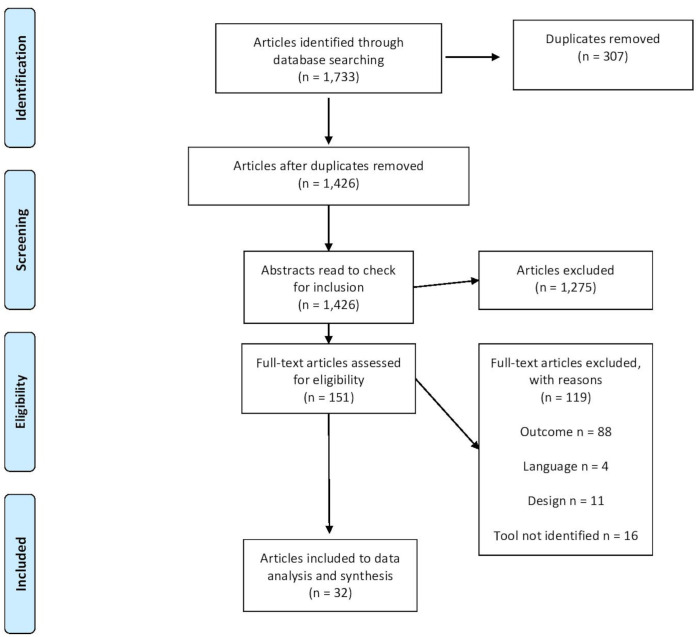
In order to ensure a blinded and unbiased selection of articles, we used the software Rayyan.17 The initial searches in electronic databases identified 1,733 articles. Following the removal of 307 duplicates, a total of 1,426 articles were transferred to Rayyan. To test the inclusion criteria, three of the authors (MM, KIN and ALM) performed a blinded pilot screening of titles and abstracts on 10% (n=120) before a blinded screening was performed on the remaining abstracts. In the following and final screening phase, a total of 10.6% (n=151) of the articles were included, while 89.4% (n=1,275) were excluded.
Charting the data and summarising the results
The articles included in the synthesis (table 1) were charted into two tables to categorise the different instruments, including patient safety dimensions (table 2) and documented psychometric properties (table 3). We did not perform a quality appraisal of the articles, as a scoping review method was used.14 15 The quality of the instruments was evaluated according to the taxonomy and terminology given by Streiner et al and the COnsensus-based Standards for the selection of health Measurement INstruments guidelines (COSMIN).18 19 The criteria evaluation contains the assessment of reliability and validity (content validity, construct validity and criterion validity), sensitivity and responsiveness. An analysis was performed as a summary on a descriptive level.20 The instrument’s original reference was used as the primary source of information on the instrument content and psychometric properties.
Results
Sample and settings
Of the 1,426 results from the selected databases, the full texts of the 151 selected articles were independently screened by two researchers (MM and KIN) (blinded for review) based on the inclusion and a total of 32 studies were included in the final full-text review (figure 1; table 1). Six studies were conducted in the USA, four in Canada, five in South Korea, four in China, three in Australia, two in Palestine, two in Saudi Arabia, two in Italy and one in each of the countries of Lithuania, Iran, Turkey and the UK (table 1).
Figure 1.
PRISMA flow diagram of the study selection process. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 1.
Articles included to data analysis and synthesis
| Author | Year | Country | Instrument identified in study |
| Abu-El-Noor et al53 | 2019 | Palestine | Attitudes to Patient Safety Questionnaire III (APSQ III) |
| Alquwez et al54 | 2019 | Saudi Arabia | The Health Professional Education in Patient Safety Survey (H-PEPSS) |
| Armstrong et al34 | 2017 | USA | Nurses’ Attitudes and Skills around Updated Safety Concepts Scale (NASUS) |
| Bottcher et al55 | 2019 | Palenstine | APSQ III |
| Brasaite et al56 | 2016 | Lituania | Patient Safety Attitudes, Skills and Knowledge (PS-ASK) |
| Bressan et al57 | 2015 | Italy | H-PEPSS |
| Chen et al58 | 2019 | China | H-PEPSS |
| Cho and Choi59 | 2018 | South Korea | Patient Safety Compentency Self-Evaluation Tool (PSCSE) |
| Colet et al60 | 2015 | Saudia Arabia | H-PEPSS |
| Duhn et al50 | 2012 | Canada | H-PEPSS |
| Ginsburg et al29 | 2013 | Canada | H-PEPSS |
| Huang et al61 | 2020 | China | H-PEPSS |
| Hwang62 | 2015 | South Korea | H-PEPSS |
| Lee et al21 | 2014 | South Korea | PSCSE |
| Lee et al63 | 2020 | South Korea | PSCSE |
| Lee et al64 | 2016 | South Korea | PSCSE |
| Lewis et al65 | 2016 | USA | Healthcare Professionals Patient Safety Assessment Curriculum Survey (HPPSACS) |
| Li et al39 | 2020 | China | Medical Student Safety Attitudes and Professionalism Survey (MSSAPS) |
| Mansour66 | 2015 | UK | HPPSACS |
| Marchi and Gropelli67 | 2017 | USA | HPPSACS |
| Murray et al36 | 2020 | Australia | Medical Students' Questionnaire of Knowledge, Skills, and Attitudes Regarding Patient Safety (MSQ-KSA) |
| Oates et al68 | 2019 | Australia | Attitudes to Patients Safety Questionnaire (APSQ3) |
| Raymond et al69 | 2016 | Canada | H-PEPSS |
| Rebeschi70 | 2020 | USA | H-PEPSS |
| Shanty and Gropelli71 | 2018 | USA | H-PEPSS |
| Stevanin et al72 | 2015 | Italy | H-PEPSS Italian version |
| Taskiran et al73 | 2020 | Turkey | H-PEPSS |
| Torkaman et al74 | 2020 | Iran | H-PEPSS |
| Usher et al75 | 2017 | Australia | H-PEPSS |
| VandenKerkhof et al76 | 2017 | Canada | H-PEPSS |
| Weatherford and Viveiros77 | 2015 | USA | H-PEPSS |
| Yan et al44 | 2021 | China | Patient Safety Competency Self Scale (PSCNES) |
The total number of study participants was 16,961 and comprised nursing students (n=8,795) nurses (n=5,345), medical doctors (n=2,075), pharmacists (n=521) and nursing assistants (n=180) (table 2). The included studies were conducted both in educational (n=25) and hospital settings (n=7).
Table 2.
Instruments assessing patient safety competencies in nursing
| Instruments, authors and country | Target group | Number of items and subdomains | |
|
Patient Safety Attitudes, Skills and Knowledge (PS-ASK) Schnall et al, USA22 |
Nurses and physicians | 26 | Attitude (9 items) Skills (13 items) Knowledge (4 items) |
|
Attitudes to Patient Safety Questionnaire III (APSQ III) Carruthers et al, UK25 |
Health professionals and students | 30 | Patient safety training received (3 items) Error reporting confidence (4 items) Working hours as error cause (3 items) Error Inevitability (4 items) Professional incompetence as error cause (4 items) Disclosure responsibility (4 items) Team functioning (2 items) Patient involvement in reducing error (2 items) Importance of patient safety in the curriculum (4 items) |
|
Healthcare Professionals Patient Safety Assessment Curriculum Survey (HPPSACS) Chenot and Daniel, USA10 |
Nursing students | 22 | Comfort (5 items) Error reporting (8 items) Denial (4 items) Culture (5 items) |
|
The Health Professional Education in Patient Safety Survey (H-PEPSS) Ginsburg et al, Canada29 |
Health professionals and students | 23 | Working in teams with other health professionals (6 items) Communicating effectively (3 items) Managing safety risks (3 items) Understanding human and environmental factors (3 items) Recognise, respond to, disclose adverse events and close calls (4 items) Culture of safety (4 items) |
|
Patient Safety Competency Self Evaluation (PSCSE) Lee et al, Korea21 |
Nursing students and nurses | 41 | Attitude (14 items) Skills (21 items) Knowledge (6 items) |
|
Nurses’ Attitudes and Skills around Updated Safety Concepts Scale (NASUS) Armstrong et al, USA34 |
Nursing students | 24 | Attitude (17 items) Perceived skills (7 items) |
|
The Medical Student Safety Attitudes and Professionalism Survey (MSSAPS) Liao et al, USA38 |
Medical students/nursing students | 28 | Safety culture (8 items) Teamwork (6 items) Error disclosure culture (4 items) Experiences with professionalism (7 items) Comfort expressing professional concerns (3 items) |
|
Medical Students’ Questionnaire of Knowledge, Skills and Attitude Regarding Patient Safety (MSQ-KSA) Flin et al, UK35 |
Medical students/nursing students | 34 | Knowledge of error and patient safety (7 items) Knowledge of workplace safety (6 items) Feelings about making errors (4 items) Speaking up about errors (4 items) Attitudes to patient safety (6 items) Safety at the workplace (7 items) |
|
The Patient Safety Competency Nurse Evaluation Scale (PSCNES) Wang, China37 |
Nurses | 35 | Patient-centred care (4 items) Safety risk management (10 items) Evidence-based nursing practice (5 items) Patient safety culture (4 items) Clinical practice (5 items) Continuous quality improvement (7 items) |
Description of identified instruments
Nine instruments were used to measure PSC (table 2). All of the instruments were designed to be self-administered Likert-type scales and had an average of 30 items, of which the shortest instrument was the Health Care Professionals Patient Safety Assessment Curriculum Survey (HPPSACS),10 containing 22 items (table 2). In contrast, the longest was the Patient Safety Competency Self-Evaluation (PSCSE),21 containing 41 items (table 2). The majority (n=9) of the instruments was originally published in English, but later translated and validated into nine other languages.
Included instruments
The Patient Safety Attitudes, Skills and Knowledge (PS-ASK) tool originated in the USA and was first published in 2008.22 The items were based partly on Madigosky et al. 28‐item questionnaire targeting medical students23 and items from Reason’s model of human error.24 The final tool consists of three subscales that measure error analysis, patient safety threats and decision support technology (table 2). The target groups for this instrument are nurses and other clinicians during educational preparation and in practice.
The Attitudes to Patient Safety Questionnaire (APSQ III) was developed by Carruthers et al in the UK in 2009.25 The questionnaire was based on the Operating Room Management Attitude Questionnaire,26 the Medical Student Survey27 and the Safety Attitudes Questionnaire.28 The APSQ III questions are divided into nine categories and the target groups for this instrument were initially medical students and tutors but later adapted to a nursing context (table 2).
The Healthcare Professional Patient Safety Assessment Curriculum Survey (HPPSACS) was developed in 2010 by Chenot et al10 based on Madigosky et al’s 28‐item questionnaire.23 The purpose of this instrument is to establish undergrad students’ perceived awareness, skills and attitudes towards patient safety in education.10 The HPPSACS is a 22-items survey in which respondents answer questions about attitudes and comfort with patient safety skills (table 2).
The Health Professional Education in Patient Safety Survey (H-PEPSS) was originated in Canada and was developed by Ginsburg et al.29 The H-PEPSS consists of 23 items and concentrates mainly on the sociocultural aspects of patient safety, including culture, teamwork, communication, risk management and the understanding of human factors (table 2). The H-PEPPS was created for healthcare workers in general.
The Patient Safety Competency Self-Evaluation (PSCSE)30 originated in Korea and is based on several earlier instruments, including those developed by Frank and Brien,31 Madigosky et al,23 Schnall et al,22 Sullivan et al32 and Wolf et al.33 Items relevant to healthcare in Korea were chosen from these instruments. The PSCSE focuses on the subdomains’ attitude, skills, knowledge and specific nursing areas of the subdomain skills, such as ulcer prevention and medication safety (table 2).
The Nurses’ Attitudes and Skills around Updated Safety Concepts Scale (NASUS) was developed by Armstrong et al34 in 2017 and is based on two previous instruments, the PS-ASK22 and the HPPSACS,10 and assesses the perceived skills and attitudes of nurses toward updated safety concepts (table 2).
The Medical Students’ Questionnaire of Knowledge, Skills and Attitudes Regarding Patient Safety (MSQ-KSA, author’s own abbreviation) is a 34-item instrument developed in the UK in 2009 by Flin et al35 that assesses student levels of knowledge and skills as well as attitudes and feelings, relating to patient safety and medical errors (table 2). The instrument was initially aimed at undergraduate medical students, but the questions were later adapted to a nursing setting by Murray et al.36
The instrument Patient Safety Competency Nurse Evaluation Scale (PSCNES) was constructed by Wang in 201837 and consists of 35 items that measure patient-centred care, safety risk management, evidence-based nursing practice, patient safety culture, clinical practice and continuous quality improvement (table 2).
The Medical Student Safety Attitudes and Professionalism Survey (MSSAPS) is a 28-item instrument that measures safety culture, team culture, error disclosure culture, experiences with professionalism, professional problem statements and the implementation of safety behaviour intention (table 2). The MSSAPS was initially developed by Liao et al38 for medical students and validated in a nursing setting by Li et al.39
Types of competencies in the identified instruments
As regards the identified competencies, some instruments map attitudes, skills and knowledge related to patient safety on an individual level (PS-ASK, NASUS, PSCSE, MSQ-KSA).21 22 34 35 These instruments identify student or nurse levels of competence in these domains and their patient safety attitudes and self-evaluation of competencies. Other instruments focus on participant perceptions of patient safety issues on a more system level, for example, teamwork, safety culture, communication and error management. Teamwork is a recurrent element and consists of questions about whether better multidisciplinary teamwork could reduce errors and if learning about teamwork would reduce errors in clinical practice. Other issues, such as how to communicate effectively, how to manage safety risks and how human factors such as fatigue affect patient safety, are also found in the instruments.
Attitudes towards patient safety were identified by the responses to such questions as what the respondent would have done if an unwanted event had been detected in a patient setting and whether they would have reported it. Content on disclosing an error to a peer or supervisor was also considered an attitude. In the MSQ-KSA instrument, the respondents were also asked to choose between several emotions to patient safety: ‘afraid’, ‘ashamed’, ‘guilty’ or ‘upset’.36
Skills were concentrated around hygiene, safe medication distribution, how to report an incident report accurately and how to examine a case to determine the cause of an unwanted event. In the specific instruments for nurses, issues concerning safe nursing practices included fall prevention, pressure ulcers and patient identification verification.21
Knowledge about patient safety focused on the health professionals’ level of competence in identifying errors, adverse events, near misses and hazards as well as the human factors that are important in creating a safe patient environment.
Psychometric properties of the instruments
Face validity was reported in six instruments (table 3) and content validity index reported in one of the included instruments.34 Furthermore, construct validity was measured in eight of nine instruments. Moreover, criterion validity (n=2), sensitivity (n=1) and responsiveness (n=1) were seldom reported. Reliability was most often (n=9) described as internal consistency using Cronbach’s alpha values. The included instruments were reported to be acceptable, ranging from 0.64 to 0.91. The most often (n=8) used reply scale was the 5-point Likert-type scale (table 3).
Table 3.
The psychometric properties of patient safety competence instruments in nursing
| Instruments | Sample | Face validity | Construct validity | Criterion validity | Reliability | Sensitivity | Responsiveness | Translations |
| Patient Safety Attitudes, Skills and Knowledge (PS-ASK) | Nursing students | X | X | X | X | English, Lithuanian | ||
| Attitudes to Patient Safety Questionnaire III (APSQ III) | Medical students | X | X | X | X | English, Arabic | ||
| Health Care Professionals Patient Safety Assessment Curriculum Survey (HPPSACS) | Nursing students | X | X | X | X | English | ||
| The Health Professional Education in Patient safety Survey (H-PEPSS) | Health professionals | X | X | X | English, Italian, Arabic, Chinese, Turkish, French |
|||
| Patient Safety Competency Self Evaluation (PSCSE) | Nursing students | X | X | X | Korean | |||
| Nurses’ Attitudes and Skills around Updated Safety Concepts (NASUS) Scale | Nurses | X | English | |||||
| The Medical Student Safety Attitudes and Professionalism Survey (MSSAPS) | Medical students/ nursing students | X | X | X | X | English, Chinese |
||
| Medical Students’ Questionnaire of Knowledge, Skills, and Attitude regarding patient safety (MSQ-KSA) | Medical students/nursing students | X | X | English | ||||
| The Patient Safety Competency Nurse Evaluation Scale (PSCNES) | Nurses | X | X | Chinese |
Discussion
This scoping review adds to the literature the content, validity and reliability of nine instruments used in nursing education and management to measure PSC in nursing. Nurse competence in patient safety is a precondition for good healthcare quality and adequate training is warranted.40 Patient safety has been raised as a global health priority by the WHO and can be categorised under the United Nations’ Sustainable Development Goal three, stating that everyone should have access to quality essential healthcare services.5 In order to provide nursing professionals with an ample competency level to ensure safe patient care, courses and modules in patient safety to improve student knowledge, skills and attitudes are offered at universities.41
Across the included instruments, identical measurement areas such as teamwork and communication can be reidentified in the existing frameworks for patient safety.5 11 31 However, one of the frameworks includes evidence-based practices in nursing and medication safety.11 The area of medication is of utmost importance and is a specific Global Patient Safety Challenge issued by the WHO that aims to reduce medication-related harm by 50% over the next five years.4 42 Moreover, patient safety in securing treatment and care based on current best evidence depends on nurses bringing the best evidence to the patient.43 In this respect, nursing education warrants efficient and non-hierarchical collaboration. The framework originating from Canada can, therefore, be interpreted as assessing patient safety on a more complex system level, which is reidentified in the APSQ-3, H-PEPSS, HPPSACS, MSSAPS, PSCNES instruments.10 11 25 29 38 44
The identified instruments that assess several of the general nursing competencies on patient safety presented by Takase and Teraoka9 include the healthcare provider’s perceived attitudes, skills and knowledge of patient safety. The instruments that measure dimensions close to these nurse competencies can be reidentified in the NASUS Scale,34 PS-ASK,22 PSCSE30 and the HPPSACS.10 With the exception of the NASUS scale, all include the three above-mentioned dimensions. It can be observed that many of the elements are recurrent, such as error disclosure and reporting and how the healthcare professional communicates an unwanted event to peers or supervisors.
Nursing ethical values seem to be lacking as a dimension in the included instruments. Even though patient safety has been an area of increased focus in recent years, ethical aspects are not well described; nonetheless, these issues form the basis of patient safety.45 Nurses should act as ‘whistle-blowers’ and be held responsible for identifying situations that may compromise patient safety.45 The ethical and patient safety values of nurses are critical factors that can potentially influence the safe practices of nurses and patient safety.46 Elements concerning ethical values that should be included when measuring competencies in patient safety are nurse knowledge of how to protect and promote human dignity as well as how nurses can respect patient autonomy and care for the entire patient, including his or her ethical values.45
Safety problems relating to non-technical skills (NTS) are significant, but appear to be underrepresented in medical and nursing education and training curricula.47 Typical NTS training topics are described in the literature as performance-shaping factors, planning, preparation and prioritisation, situation awareness and perception of risk, decision-making, communication, teamwork and leadership.47 NTS elements can be found in the APSQ-3, H-PEPSS, HPPSACS, MSSAPS, PSCNES instruments. When these NTS are compared with the frameworks and definition of nurse competence, it can be observed that communication and teamwork are typically recurrent elements in the instruments: both dimensions are undeniably crucial to patient safety.
An instrument that measures PSC must be useful on several levels, such as for clinical practice, educational or managerial purposes.5 First, at an individual level, the respondent could be made aware of and increase his or her knowledge and PSC. Second, an instrument can be used on an educational level to investigate the discordance between what is taught and what clinical competence reflects. A possible difference between theory and practice may warrant the possibility of universities to make curriculum changes in theoretical and practical studies. Finally, hospital administrators could use instruments to establish employee knowledge of PSC. Knowing more about employee levels of knowledge could potentially lead to the need for more training, leading to a higher level of patient safety and quality in the nursing given.4 However, in our review, two of the instruments were not developed with nurses as the target group in the original version: the MSSAPS and MSQ-KSA were made for medical students, but later adapted and used for nurses.35 38 Awareness of the use of instruments created for a different profession or domain should be taken into account, as there are potential pitfalls and the measured outcome could be erroneous.48
Patient safety frameworks contain important dimensions and competencies for nurses and future nurses. For future nurses, Bianchi et al49 comment that more research is needed to identify more explicit education strategies to develop nursing student competencies in patient safety. Although several frameworks describe different PSC, it has been made clear that it is essential to introduce safety principles in student curricula as soon as they have started their degree programme and the topic must be continued throughout their studies.50 Nevertheless, more knowledge and research must identify what they need to learn and what competencies are required. The identified instruments may facilitate improved patient safety curricula and courses through the quality of outcome assessments.
Reliability and validity of identified instruments
Validity was assessed in all but one of the instruments, either as content or construct validity. Validity assures that the instrument measures what it is intended to assess.51 However, reliability is a prerequisite to obtaining validity and internal consistency in terms of Cronbach’s alpha was assessed in all instruments, but the test–retest stability was only tested in one instrument, the PS-ASK.22 Criterion validity was reported in only one study, perhaps because of no established ‘gold standards’. Furthermore, sensitivity and responsiveness seem to be very rarely reported, raising uncertainty about the instrument’s ability to distinguish between groups or identify change over time. Both features are essential to reveal the effects of an intervention study like an educational patient safety programme.
Strengths and limitations
This scoping review has limitations and by adopting this methodology, it is intended to investigate breadth rather than depth.14 First, a comparison of findings across studies must be carried out with caution, given the variations in how data were reported. Second, the search for studies was systematic and comprehensive, but English manuscripts might limit the applicability of the findings to English‐speaking parts of the world. In addition, our search was up to date as of April 2021 and the findings only reflect that they have been indexed and assigned MeSH. According to the guidelines for scoping reviews, performing a quality check is not considered obligatory.14 Furthermore, whereas a systematic review intends to provide a complete and exhaustive summary of the existing literature, we were limited to a general overview of the instruments that exist.52
Conclusion
Our scoping review identified nine instruments that can be used to measure patient safety competencies in nursing. The identified instruments measure and contain a wide variety of domains, such as attitudes, skills and knowledge, communication skills, patient safety culture and talking openly about patient safety issues. These dimensions are identified in the instruments from existing frameworks in patient safety, but a measurement of the ethical and patient safety values of nurses is lacking in all of the instruments. Future research and development of instruments should include ethical issues in patient safety. Furthermore, the measurement of instruments responsiveness is seldom measured. In order to assure that instruments distinguish between groups or identify change over time, this psychometric aspect should be taken into account in future studies in which new instruments are created or validated into new languages.
Footnotes
Contributors: Planning: all authors. Data collection: MM, KIN. Data analysis: all authors. Manuscript preparation: MM, KIN. Manuscript review: all authors. Guarantor: MM.
Funding: This review is a part of the project ‘Hybrid curriculum in patient safety: integration of academic master’s education and continuous professional education in Estonia and Norway 2019-2022’ funded by the EEA/Norway Cooperation Programme in Higher Education.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Egan EA. Clinical ethics and patient safety. In: Agrawal A, ed. Patient safety: a case-based comprehensive guide. New York: Springer, 2014: 87–100. [Google Scholar]
- 2.Butterworth T, Jones K, Jordan S. Building capacity and capability in patient safety, innovation and service improvement: an English case study. J Res Nurs 2011;16:243–51. 10.1177/1744987111406008 [DOI] [Google Scholar]
- 3.Vaismoradi M. Nursing education curriculum for improving patient safety. J Nurs Educ Pract 2012;2:101–4. 10.5430/jnep.v2n1p101 [DOI] [Google Scholar]
- 4.Hughes RG. ‘Nurses at the “Sharp End” of patient care. In: Hughes RG, ed. Patient safety and quality: an evidence-based Handbook for nurses. Rockville, MD: Agency for Healthcare Research and Quality (US), 2008. http://www.ncbi.nlm.nih.gov/books/NBK2672/ [PubMed] [Google Scholar]
- 5.World Health Organization and WHO Patient Safety . Patient safety curriculum guide: multi-professional edition, 2011. Available: https://apps.who.int/iris/handle/10665/44641
- 6.Slawomirski L, Klazinga N. The economics of patient safety, from analysis to action. OECD, 2020. [Google Scholar]
- 7.Elliott RA, Camacho E, Jankovic D, et al. Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Qual Saf 2021;30:96–105. 10.1136/bmjqs-2019-010206 [DOI] [PubMed] [Google Scholar]
- 8.Kuriakose R, Aggarwal A, Sohi RK, et al. Patient safety in primary and outpatient health care. J Family Med Prim Care 2020;9:7–11. 10.4103/jfmpc.jfmpc_837_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Takase M, Teraoka S. Development of the holistic nursing competence scale. Nurs Health Sci 2011;13:396–403. 10.1111/j.1442-2018.2011.00631.x [DOI] [PubMed] [Google Scholar]
- 10.Chenot TM, Daniel LG. Frameworks for patient safety in the nursing curriculum. J Nurs Educ 2010;49:559–68. 10.3928/01484834-20100730-02 [DOI] [PubMed] [Google Scholar]
- 11.Levett-Jones T. Patient safety competency framework (PSCF) for nursing students, 2017. Available: https://research.usc.edu.au/discovery/fulldisplay/alma99451213402621/61USC_INST:ResearchRepository [Accessed 19 Jan 2021].
- 12.Flin R. Measuring safety culture in healthcare: a case for accurate diagnosis. Saf Sci 2007;45:653–67. 10.1016/j.ssci.2007.04.003 [DOI] [Google Scholar]
- 13.Okuyama A, Martowirono K, Bijnen B. Assessing the patient safety competencies of healthcare professionals: a systematic review. BMJ Qual Saf 2011;20:991–1000. 10.1136/bmjqs-2011-000148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 15.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 16.Methley AM, Campbell S, Chew-Graham C, et al. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 2014;14:579. 10.1186/s12913-014-0579-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016;5:210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. USA: Oxford University Press, 2015. [Google Scholar]
- 19.Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol 2010;63:737–45. 10.1016/j.jclinepi.2010.02.006 [DOI] [PubMed] [Google Scholar]
- 20.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee N-J, An J-Y, Song T-M, et al. Psychometric evaluation of a patient safety competency self-evaluation tool for nursing students. J Nurs Educ 2014;53:550–62. 10.3928/01484834-20140922-01 [DOI] [PubMed] [Google Scholar]
- 22.Schnall R, Stone P, Currie L, et al. Development of a self-report instrument to measure patient safety attitudes, skills, and knowledge. J Nurs Scholarsh 2008;40:391–4. 10.1111/j.1547-5069.2008.00256.x [DOI] [PubMed] [Google Scholar]
- 23.Madigosky WS, Headrick LA, Nelson K, et al. Changing and sustaining medical students' knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med 2006;81:94–101. 10.1097/00001888-200601000-00022 [DOI] [PubMed] [Google Scholar]
- 24.Reason J. Human error: models and management. BMJ 2000;320:768–70. 10.1136/bmj.320.7237.768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carruthers S, Lawton R, Sandars J, et al. Attitudes to patient safety amongst medical students and tutors: developing a reliable and valid measure. Med Teach 2009;31:e370–6. 10.1080/01421590802650142 [DOI] [PubMed] [Google Scholar]
- 26.Helmreich R, Sexton B, Merritt A. ‘The Operating Room Management Attitudes Questionnaire (ORMAQ). Univ Tex Aerosp Crew Res Proj Tech Rep 1997:97–6. [Google Scholar]
- 27.Sorokin R, Riggio JM, Hwang C. Attitudes about patient safety: a survey of physicians-in-training. Am J Med Qual 2005;20:70–7. 10.1177/1062860604274383 [DOI] [PubMed] [Google Scholar]
- 28.Sexton JB, Helmreich RL, Neilands TB, et al. The safety attitudes questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res 2006;6:44. 10.1186/1472-6963-6-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ginsburg L, Castel E, Tregunno D, et al. The H-PEPSS: an instrument to measure health professionals’ perceptions of patient safety competence at entry into practice. BMJ Qual Saf 2012;21:676–84. 10.1136/bmjqs-2011-000601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee N-J, Jang H. Development of Questionnaires to Measure Baccalaureate Nursing Students’ Patient Safety Competencies. Nurs Inform 2012:1. [Google Scholar]
- 31.Frank JR, Brien S. The safety competencies: enhancing patient safety across the health professions. Canadian Patient Safety Institute 2008. [Google Scholar]
- 32.Sullivan DT, Hirst D, Cronenwett L. Assessing quality and safety competencies of graduating prelicensure nursing students. Nurs Outlook 2009;57:323–31. 10.1016/j.outlook.2009.08.004 [DOI] [PubMed] [Google Scholar]
- 33.Wolf ZR, Altmiller G, Bicknell P. Development and testing of the patient safety test: current concepts. Nurse Educ 2011;36:187–91. 10.1097/NNE.0b013e3182297ca9 [DOI] [PubMed] [Google Scholar]
- 34.Armstrong GE, Dietrich M, Norman L, et al. Development and psychometric analysis of a nurses' attitudes and skills safety scale: initial results. J Nurs Care Qual 2017;32:E3–10. 10.1097/NCQ.0000000000000216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flin R, Patey R, Jackson J, et al. ‘Year 1 medical undergraduates’ knowledge of and attitudes to medical error’, Med. Educ 2009;43:1147–55. [DOI] [PubMed] [Google Scholar]
- 36.Murray M, Sundin D, Cope V. A mixed-methods study on patient safety insights of new graduate registered nurses. J Nurs Care Qual 2020;35:258–64. 10.1097/NCQ.0000000000000443 [DOI] [PubMed] [Google Scholar]
- 37.Wang Q. Development of the patient safety competency nurse evaluation scale. Peking Union Medical College, 2018. [Google Scholar]
- 38.Liao JM, Etchegaray JM, Williams ST, et al. Assessing Medical Students’ Perceptions of Patient Safety. Acad Med 2014;89:343–51. 10.1097/ACM.0000000000000124 [DOI] [PubMed] [Google Scholar]
- 39.Li H, Kong X, Sun L, et al. Major educational factors associated with nursing adverse events by nursing students undergoing clinical practice: a descriptive study. Nurse Educ Today 2021;98:104738. 10.1016/j.nedt.2020.104738 [DOI] [PubMed] [Google Scholar]
- 40.Jang H, Lee N-J. Patient safety competency and educational needs of nursing educators in South Korea. PLoS One 2017;12:e0183536. 10.1371/journal.pone.0183536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fukada M. Nursing competency: definition, structure and development. Yonago Acta Med 2018;61:1–7. 10.33160/yam.2018.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.World Health Organization . Medication without harm WHO global patient safety challenge, 2017. Available: https://apps.who.int/iris/bitstream/handle/10665/255263/WHO-HIS-SDS-2017.6-eng.pdf;jsessionid=137E2C6ACE784A9238A497EA2FEB1417?sequence=1
- 43.Vaismoradi M, Tella S, A. Logan P, et al. Nurses’ adherence to patient safety principles: a systematic review. Int J Environ Res Public Health 2020;17:2028. 10.3390/ijerph17062028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yan L, Yao L, Li Y, et al. Assessment and analysis of patient safety competency of Chinese nurses with associate degrees: a cross-sectional study. Nurs Open 2021;8:395–403. 10.1002/nop2.640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kangasniemi M, Vaismoradi M, Jasper M, et al. Ethical issues in patient safety: implications for nursing management. Nurs Ethics 2013;20:904–16. 10.1177/0969733013484488 [DOI] [PubMed] [Google Scholar]
- 46.Feng X, Bobay K, Krejci JW, et al. Factors associated with nurses’ perceptions of patient safety culture in China: a cross-sectional survey study. J Evid Based Med 2012;5:50–6. 10.1111/j.1756-5391.2012.01177.x [DOI] [PubMed] [Google Scholar]
- 47.Ricciardi W, Cascini F. Guidelines and safety practices for improving patient safety. In: Textbook of patient safety and clinical risk management. Cham: Springer, 2021: 3–18. [PubMed] [Google Scholar]
- 48.Hyman L, Bulmer M, Lamb J. ‘The use of pre-existing survey questions: implications for data quality’, presented at the The Conference on Quality in Survey Statistics, 2006. Available: https://researchportal.port.ac.uk/en/publications/the-use-of-pre-existing-survey-questions-implications-for-data-qu [Accessed 01 Sep 2021].
- 49.Bianchi M, Bressan V, Cadorin L, et al. Patient safety competencies in undergraduate nursing students: a rapid evidence assessment. J Adv Nurs 2016;72:2966–79. 10.1111/jan.13033 [DOI] [PubMed] [Google Scholar]
- 50.Duhn L, Karp S, Oni O, et al. Perspectives on patient safety among undergraduate nursing students. J Nurs Educ 2012;51:526–31. 10.3928/01484834-20120706-04 [DOI] [PubMed] [Google Scholar]
- 51.Streiner DL, Kottner J. Recommendations for reporting the results of studies of instrument and scale development and testing. J Adv Nurs 2014;70:1970–9. 10.1111/jan.12402 [DOI] [PubMed] [Google Scholar]
- 52.Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018;18:143. 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Abu-El-Noor NI, Abu-El-Noor MK, Abuowda YZ, et al. Patient safety culture among nurses working in Palestinian governmental Hospital: a pathway to a new policy. BMC Health Serv Res 2019;19. 10.1186/s12913-019-4374-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alquwez N, Cruz JP, Almoghairi AM, et al. Nurses' perceptions of patient safety culture in three hospitals in Saudi Arabia. J Nurs Scholarsh 2018;50:422–31. 10.1111/jnu.12394 [DOI] [PubMed] [Google Scholar]
- 55.Bottcher B, Abu-El-Noor N, Abuowda Y, et al. Attitudes of doctors and nurses to patient safety and errors in medical practice in the Gaza-Strip: a cross-sectional study. BMJ Open 2019;9:e026788. 10.1136/bmjopen-2018-026788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brasaitė I, Kaunonen M, Martinkėnas A, et al. Health care professionals’ skills regarding patient safety. Medicina 2016;52:250–6. 10.1016/j.medici.2016.05.004 [DOI] [PubMed] [Google Scholar]
- 57.Bressan V, Stevanin S, Bulfone G, et al. Measuring patient safety knowledge and competences as perceived by nursing students: an Italian validation study. Nurse Educ Pract 2016;16:209–16. 10.1016/j.nepr.2015.08.006 [DOI] [PubMed] [Google Scholar]
- 58.Chen L, Huang F, Yuan X, et al. An assessment of the reliability and factorial validity of the Chinese version of the health professional education in patient safety survey (H-PEPSS). Front Psychol 2019;10. 10.3389/fpsyg.2019.02183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cho SM, Choi J. Patient safety culture associated with patient safety competencies among registered nurses. J Nurs Scholarsh 2018;50:549–57. 10.1111/jnu.12413 [DOI] [PubMed] [Google Scholar]
- 60.Colet PC, Cruz JP, Cruz CP, et al. Patient safety competence of nursing students in Saudi Arabia: a self-reported survey. Int J Health Sci 2015;9:411–9. 10.12816/0031231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Huang FF, Shen XY, Chen XL, et al. Self-reported confidence in patient safety competencies among Chinese nursing students: a multi-site cross-sectional survey. BMC Med Educ 2020;20:32. 10.1186/s12909-020-1945-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hwang J-I. What are hospital nurses' strengths and weaknesses in patient safety competence? findings from three Korean hospitals. Int J Qual Health Care 2015;27:232–8. 10.1093/intqhc/mzv027 [DOI] [PubMed] [Google Scholar]
- 63.Lee SE, Lee MH, Peters AB, et al. Assessment of patient safety and cultural competencies among senior Baccalaureate nursing students. Int J Environ Res Public Health 2020;17. 10.3390/ijerph17124225. [Epub ahead of print: 13 06 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee N-J, Jang H, Park S-Y. Patient safety education and baccalaureate nursing students’ patient safety competency: A cross-sectional study. Nurs Health Sci 2016;18:163–71. 10.1111/nhs.12237 [DOI] [PubMed] [Google Scholar]
- 65.Lewis DY, Stephens KP, Ciak AD. QSEN: curriculum integration and bridging the gap to practice. Nurs Educ Perspect 2016;37:97–100. [PubMed] [Google Scholar]
- 66.Mansour M. Factor analysis of nursing students’ perception of patient safety education. Nurse Educ Today 2015;35:32–7. 10.1016/j.nedt.2014.04.020 [DOI] [PubMed] [Google Scholar]
- 67.Marchi NM, Dolansky M. Using active learning to foster patient safety knowledge, perceived skills, and attitudes in Baccalaureate nursing students. Nurs Educ Perspect 2017;38:146–8. 10.1097/01.NEP.0000000000000127 [DOI] [PubMed] [Google Scholar]
- 68.Oates K, Burgess A, Dalton S, et al. The Academy for emerging leaders in patient safety: developing a community of practice. Clin Teach 2020;17:508–14. 10.1111/tct.13127 [DOI] [PubMed] [Google Scholar]
- 69.Raymond J, Medves J, Godfrey C. Perspectives on patient safety among practical nursing students. Can J Nurs Res 2016;48:41–7. 10.1177/0844562116664260 [DOI] [PubMed] [Google Scholar]
- 70.Rebeschi LM. Perceived patient safety competence of Baccalaureate nursing students: a descriptive comparative study. SAGE Open Nurs 2020;6:237796082093013. 10.1177/2377960820930134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shanty JA, Gropelli T. Self-Reported patient safety competence among nursing, respiratory care, and nuclear medicine technology students. J Allied Health 2018;47:141–6. [PubMed] [Google Scholar]
- 72.Stevanin S, Bressan V, Bulfone G, et al. Knowledge and competence with patient safety as perceived by nursing students: the findings of a cross-sectional study. Nurse Educ Today 2015;35:926–34. 10.1016/j.nedt.2015.04.002 [DOI] [PubMed] [Google Scholar]
- 73.Taskiran G, Eskin Bacaksiz F, Harmanci Seren AK. Psychometric testing of the Turkish version of the Health Professional Education in Patient Safety Survey: H-PEPSSTR. Nurse Educ Pract 2020;42:102640. 10.1016/j.nepr.2019.102640 [DOI] [PubMed] [Google Scholar]
- 74.Torkaman M, Sabzi A, Farokhzadian J. The Effect of Patient Safety Education on Undergraduate Nursing Students’ Patient Safety Competencies. Community Health Equity Research & Policy 2022;42:219–24. 10.1177/0272684X20974214 [DOI] [PubMed] [Google Scholar]
- 75.Usher K, Woods C, Parmenter G, et al. Self-reported confidence in patient safety knowledge among Australian undergraduate nursing students: a multi-site cross-sectional survey study. Int J Nurs Stud 2017;71:89–96. 10.1016/j.ijnurstu.2017.03.006 [DOI] [PubMed] [Google Scholar]
- 76.VanDenKerkhof E, Sears N, Edge DS, et al. Patient safety in practical nurses’ education: A cross-sectional survey of newly registered practical nurses in Canada. Nurse Educ Today 2017;51:48–56. 10.1016/j.nedt.2017.01.003 [DOI] [PubMed] [Google Scholar]
- 77.Weatherford BH, Viveiros JA. Senior nursing students’ perspectives on safety competencies: an end-of-program outcome evaluation. Nurs Educ Perspect 2015;36:182–4. 10.5480/13-1182 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon request.