Abstract
Aims:
Better documentation of vulvar pain is needed. We examined pain locations marked on general body and genital specific outlines among women with vulvodynia.
Methods:
62 women (mean age 32.1 ± 9.5 years) with vulvodynia marked their pain on a digital genital specific outline (22 segments) and 59 of those women also marked their pain on a digital general body outline (48 segments). We used ImageJ software to determine body surface area (BSA) for each outline.
Results:
On the general body outline, 24/48 segments were marked; 22/22 segments were marked on the genital specific outline. There was a moderate correlation (r = 0.43; p = 0.001) between the BSA marked on the general body outline and the BSA marked on the genital area outline.
Conclusions:
Findings support concurrent validity of the BSA as a measure of pain location using either outline.
Keywords: : pain tool, PAINReportIt, tool development, vulvar pain, vulvodynia
Lay abstract
Women with genital pain need to be able to show their healthcare provider where they have pain, and providers need to document where women have pain. In total, 62 women with vulvodynia used a computer tablet to mark their pain on a general body outline and a genital specific outline. We used computer software to document the location of women’s pain looking at percent body surface area. Women marked half of the segments on the general body outline and all the segments on the genital specific outline. Because women marked almost the same percent of body surface area on the general body outline as they did on the genital specific outline, percent body surface may be used to measure pain location.
Background
Vulvodynia is “vulvar pain of at least 3 months duration without clear identifiable cause, which may have potential associated factors” [1]. Burning, itching, hot, stabbing, aching, tight, stinging, tingling and pricking are frequent descriptors of vulvodynia [2]. There are two types of vulvodynia: provoked vestibulodynia and generalized vulvodynia. Provoked vestibulodynia is pain confined to the vulvar vestibule and vaginal introitus that is provoked by vaginal insertion or touching the vulva. Generalized vulvodynia is diffuse, spontaneous pain of the vulva that may radiate to the perineum and inner thighs [3]. Pain from vulvodynia severely impacts up to 7 million American women's lives ranging from the inability to wear clothing that contacts the vulva to the inability to have sexual intercourse, devastating women’s lives and intimate relations [3,4]. When women discuss their vulvar pain with their healthcare providers, they are not provided with a tool to effectively report their pain location and often do not clearly articulate where they feel their pain, referring to the pain ‘down there’ [5]. To address this gap, the purpose of our study was to examine pain locations marked on general body and genital specific outlines among women with vulvodynia.
Unfortunately, vulvodynia is underdiagnosed for several reasons including the taboo nature of discussing issues related to the genitalia and sex; and a lack of awareness about vulvodynia among women and healthcare providers [3,6]. In a study of 2542 women, only 49% sought care for their pain [3], and in another study, only 26% of women with vulvar pain were comfortable telling a female friend about it [7].
For more than four decades, the location of pain, anywhere on the body, has been identified by patients by drawing on paper general body outlines [8]. However, this method is not effective for identifying the location of vulvodynia due to the lack of specific external genitalia. Paper general body outlines, without a genitalia outline, inhibit women from accurately describing the location of their pain, prevent the tool from being integrated into the woman’s electronic medical record and limit advanced data aggregation and analysis [9–12]. A digital body outline with a genitalia specific outline could solve many of the problems associated with a general body outline paper tool to improve patient care and further vulvodynia research.
Digital general body outlines have been found to be acceptable and reliable for reporting pain location [12–16]. A specific genitalia outline provides women with a digital picture of a vulva and thighs to draw where they feel pain. Women could use this digital tool to report the location of their pain or a clinician could use it when examining a patient. Having a patient first identify where the pain is on the digital image prior to meeting with the healthcare provider can allow the patient to communicate where the pain is without having to verbally describe or point to the location, which may be embarrassing or uncomfortable [6,7]. Using an electronic pain location tool instead of a paper tool allows the data to be incorporated into the patient’s electronic record with easily assessed pain location across patient visits for all vulvodynia types.
Currently vulvodynia research is plagued by small sample sizes and a lack of standardized methods for identification of pain location, preventing cross study comparison [17–19]. The digital tool could standardize documentation of vulvodynia pain location across research studies. Using a standardized measure integrated into the electronic record would facilitate data aggregation and allow for large vulvodynia studies via data extraction. More detailed information about pain location from a larger sample could lead to improved characterization of provoked and generalized vulvodynia. Digital drawings of pain location offer the opportunity to apply image analysis that has been used for other purposes to efficiently summarize the pain location data as body surface area (BSA) in the areas drawn as painful [20,21]. BSA is the total surface area of the human body and is measured as a percentage. BSA is used routinely to calculate drug dosages and intravenous fluids administration. We recognized the opportunity to advance this area of science by using the free ImageJ software available from the National Institutes of Health to calculate the BSA of pain location drawings on a general body outline (Figure 1A) and on a genital specific outline (Figure 1B). The specific aim of our study was to describe pain locations of women with vulvodynia who marked their pain on digital images of general body outlines and genital specific outlines. We also examined relationships between the resulting BSA values.
Figure 1. . General body and genital specific outlines.
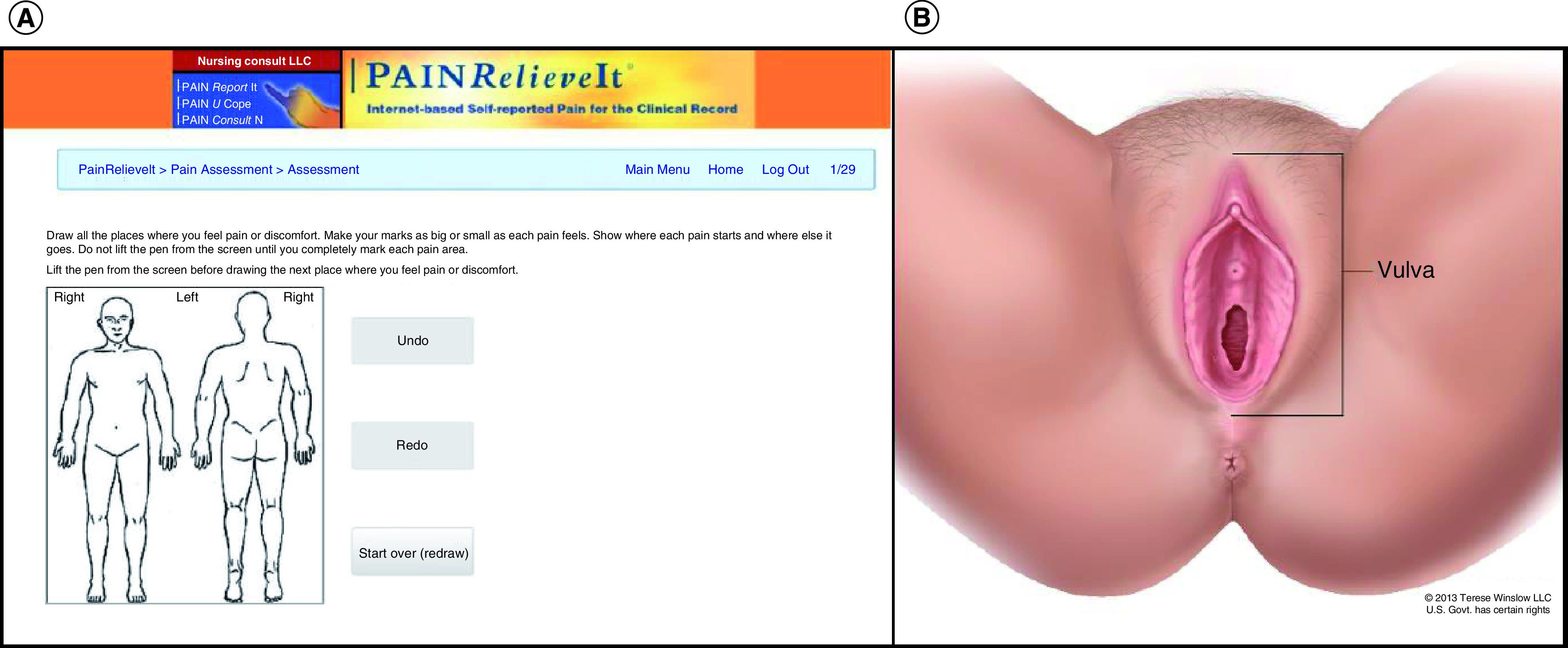
(A) 2D body images displaying a front and back of the general body outline as included in PAINReportIt®, which is the pain assessment component of PAINRelieveIt® © 2020 DJ Wilkie. (B) Genital specific outline. Reprinted with permission from Vulvar Anatomy © 2013 Terese Winslow LLC US Government has certain rights.
Methods
Design
For this study, we used baseline data from an ongoing double-blind randomized controlled trial (RCT) of acupuncture as a treatment for vulvodynia [22]. The Institutional Review Board (IRB) at the University of Illinois Chicago (UIC, IRB2017-0885) approved the RCT and the IRB at the University of Florida (UF) approved the study of de-identified data as exempt (IRB201800566). Informed written consent was obtained from all enrolled women.
Setting/sample
The ongoing study is being conducted in research space at the UIC College of Nursing. Women were recruited from clinics and the community in metropolitan Chicago. Enrolled women were those who met the eligibility criteria: over 18 years of age, clinically diagnosed with vulvodynia, and acupuncture naive. Exclusion criteria included pregnancy, pelvic pain, other pathologic causes of vulvar pain and concomitant use of other therapeutic pain relief techniques including physical therapy and biofeedback.
The enrolled sample included 62 women who completed study measures. Their ages ranged from 20 to 62 years (mean = 32.1 ± 9.5), and of those reporting their race, 11% were Asian, 5% were Black, 2% were Mixed, 7% were other and 75% were White. Of those reporting their ethnicity, 23% were Hispanic and 77% were non-Hispanic. Of those reporting their education level, nearly all (93%) reported education beyond high school (Table 1).
Table 1. . Sample demographic characteristics (N = 62).
| Variable | Frequency (%) |
|---|---|
| Age (n = 62) | |
| Mean (SD) min–max | 32.1 (9.5), 20–62 |
| Education (n = 57) | |
| High school or less | 4 (7%) |
| Some college | 5 (9%) |
| Bachelor | 25 (45%) |
| Advanced | 22 (39%) |
| Race (n = 56) | |
| Asian | 6 (11%) |
| Black | 3 (5%) |
| Mixed | 1 (2%) |
| Other | 4 (7%) |
| White | 41 (75%) |
| Ethnicity (n = 57) | |
| Hispanic | 13 (23%) |
| Non-Hispanic | 43 (77%) |
Note: n < 62 due to missing data.
Procedures
After informed consent, the study research specialist asked women to complete the PAINReportIt software using a touchscreen, internet-enabled tablet. The software resided on a secure server at the UF, and the encrypted data were automatically written to a secure UF database server. Other details of the ongoing RCT are published elsewhere [22].
Instruments
A component of the PAINRelieveIt suite of mobile health programs (apps) to support pain care and research, PAINReportIt [16,23,24] is an electronic version of the McGill Pain Questionnaire [8]. PAINReportIt allows individuals to report the location, intensity on a 0–10 scale (none to pain as bad as it could be), quality and pattern of their pain. To report pain location, the participant is asked to draw, using a computer mouse or pen, all the places where pain is felt on a general body outline (Figure 1A). For this study, a genital specific outline, designed by Terese Winslow LLC (VA, USA) Medical and Scientific Illustration, was also available (Figure 1B). The validity and reliability of PAINReportIt as a measure of pain have been evaluated [2,16].
The ImageJ software [20] was used to process the women’s digital drawings. For this study, BSA was calculated from where women drew their pain on a digital image of the vulva and/or body. This information is used to identify the areas of the vulva and/or body where women with vulvodynia may have pain. We developed an algorithm to handle the analysis steps that included eliminating any markings drawn outside the outlines and calculating the BSA by counting the area of red pixels drawn within the lines of each segment on the outlines (general or genital specific) and reporting as a BSA percentage of the segment. To indicate the anatomical locations of the pain markings, the general body outline was divided into 48 segments (Figure 2A), and the genital specific image was divided into 22 segments (Figure 2B). The algorithm also calculated a total BSA percentage (total BSA%) across the segments of each outline.
Figure 2. . Frequency of markings on the general body and the genital specific outlines.
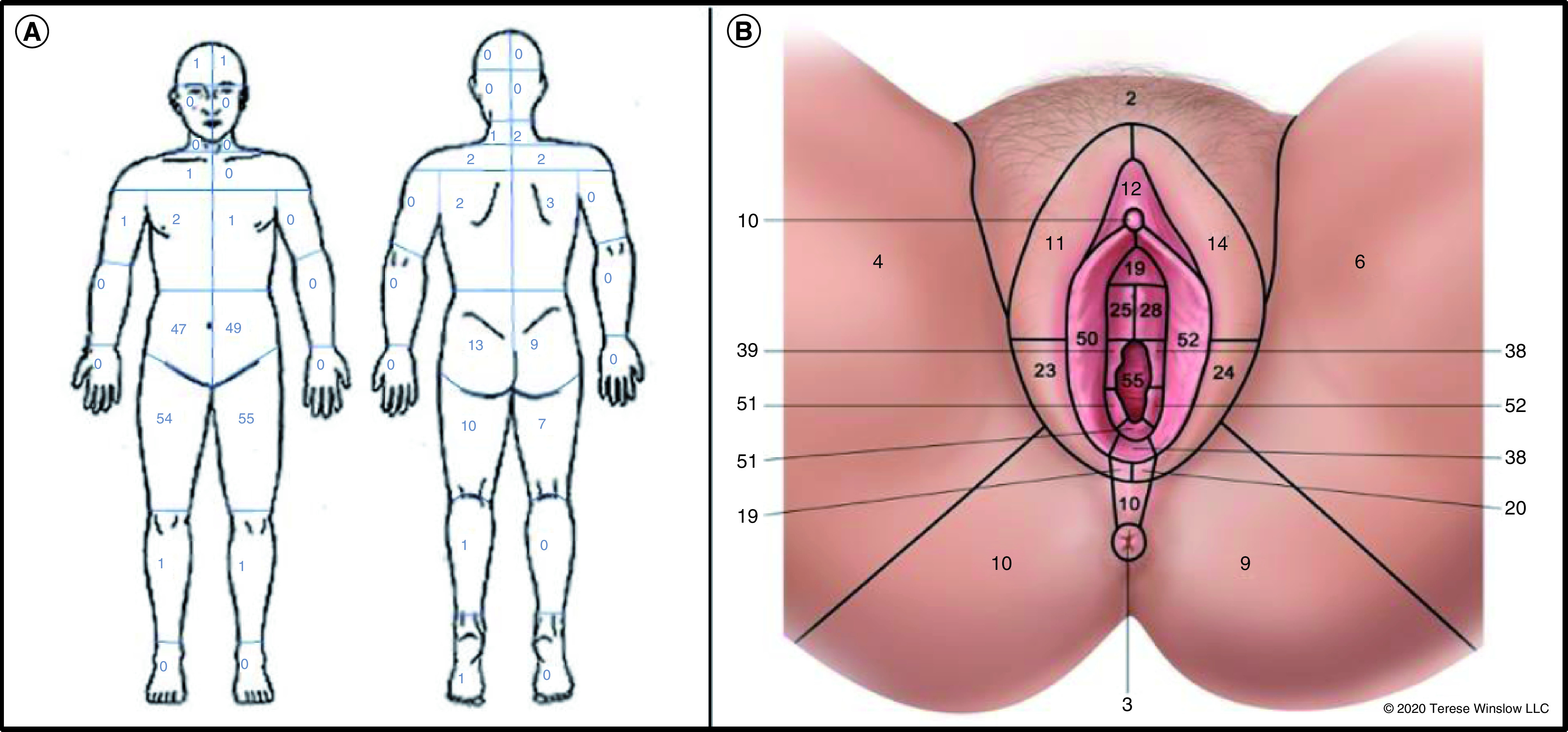
(A) Frequency of markings on the general body outline for each of its 48 segments (n = 59). (B) Frequency of markings on the genital specific outline for each of its 22 segments (N = 62).
(A) Reprinted with permission from © 1990 DJ Wilkie.
Analysis
Descriptive statistics were used to analyze the frequency of markings per segment on each outline and the total BSA% on each outline. Pearson’s correlation and independent t-tests were used to examine relationships between the BSA values from both outlines. Statistical significance was set a priori at p < 0.05.
Results
As a context for women’s pain experience, the mean of the current, least and worst pain intensity in the previous 24 h was used to create the average pain intensity (API). The mean average pain intensity was 3.9 ± 2.6, representing moderate pain intensity. From pre-enrollment gynecological examination findings, 41 women had generalized vulvodynia and 18 women had provoked vestibulodynia; there were missing data on 3 women.
General body outline
On the general body outline, 59 women marked the area of their pain on the genital area with 41 women marking only on the genital area of the general body outline and 18 marking in both the genital region and elsewhere. Of the 48 segments on the general body outline, 24 were marked. As indicated in Figure 2A, the most frequently marked were segments near the vulvar region; left anterior thigh (n = 59), right anterior thigh (n = 54), left lumbar/iliac region (n = 49) and right lumbar/iliac region (n = 47). The areas marked elsewhere than the genital region included: left gluteal region (n = 13), left hamstrings (n = 10), right gluteal region (n = 9) and right hamstrings (n = 7). Across all 48 segments, the average total BSA% was 1.1% ± 1.7%, ranging from 0% to 11.4%.
Genital specific outline
On the genital specific outline, all 62 women marked the area of their pain on the vulvar area, with 34 marking areas not within the vulvar area. Of the 22 segments included on the genital specific outline, all 22 segments were marked by at least one woman. Figure 2B includes the frequency distribution for each segment. The following segments, however, were the most frequent: fourchette (n = 38), 3 o’clock vulvar vestibule (n = 38), 9 o’clock vulvar vestibule (n = 39), right labia minora (n = 50), vestibular fossa (n = 51), 8 o’clock vulvar vestibule (n = 51), 4 o’clock vulvar vestibule (n = 52), left labia minora (n = 52) and vagina (n = 55). Across all 22 segments, the average total BSA% was 1.3% ± 1.2%, ranging from 0% to 5.5%.
BSA: relationships between outlines
The correlation coefficient between the total BSA% values for the general body outline and the genital specific outline indicated a statistically significant moderate positive correlation (r = 0.43; p = 0.001). Since some women marked pain only in the genital area and others marked both pain in the genital area and elsewhere in other areas, we compared the total BSA% between these groups of women. On the general body outline, the BSA of the women who marked on the genital area only region was 0.7% ± 1.1% and women who marked on both the genital area and elsewhere were 1.8% ± 2.6%. The difference in total BSA% between both groups of women was not statistically significant (p = 0.11). On the genital specific outline, the BSA of women who marked the genital only regions were 1.2% ± 1.1%, and the women marking both genital region and elsewhere were 1.5% ± 1.2%. The difference in BSA between the two groups of women was not statistically significant (p = 0.49).
Discussion
This study is based on baseline data from an ongoing double-blind RCT. We examined two ways of measuring pain location among women with vulvodynia: internet-based digital pain assessment tools and an open-source image analysis tool. Our key findings showed that women with vulvodynia used both general body and genital specific outlines to document pain location in the genital area as well as elsewhere in other body areas. A genital specific outline risks missing pain in the other body areas but provides genital specific information that allows women to better communicate the specific location of their pain. This genital specific information is lacking on the general body outline. The average total BSA% shows promise as an aggregate measure of pain location. Overall, study findings support the value of using the general body outline to detect pain in the genital area and the potential added value of the detailed vulvar information that is obtained with the genital specific outline among women with vulvar pain.
PAINReportIt is a potential tool that could help to overcome vulvar pain monitoring difficulties, such as women’s use of nonspecific language to report their pain ‘down there’ [5]. Having the ability to identify vulvar pain on a computer screen may be less confrontational for women as they can have an opportunity to show the clinician where their pain is without removing their clothing. Also, women with vulvar pain may be less inclined to delay their care due to embarrassment about scheduling a physical examination of the genitals. Investigators of two previous studies [2,25] noted benefits and limitations of the general body outline for women to report the details of their vulvar pain. Our study corrected these weaknesses with the addition of the genital specific outline and our findings indicate that both general and genital specific outlines are needed to fully document pain experienced by women with vulvodynia and allow them to feel comfortable addressing their symptoms. The significance of better documentation of vulvodynia may signify improved patient–clinician communication that can help break the taboo surrounding women’s reporting of gynecological problems.
We examined BSA as a measure of pain location. Future studies of vulvodynia should focus on relationships between BSA and other pain parameters such as pain intensity, pain quality and pain pattern, as those measures are included in the PAINReportIt software. In clinical practice, this method of data collection can allow women to express aspects of their pain in the comfort of their homes or in the waiting room prior to seeing their clinician. This approach allows the short time during an appointment with a clinician to be focused on interpreting and validating the data with physical exam findings. The use of such software also allows for monitoring of pain to detect any changes. Findings from a previous study indicated that some women were unfamiliar with the anatomical words associated with the female genitalia and were unable to draw the external female genitalia [26]. However, we found that women were able to locate their pain location when given both general body and genital specific outlines. In a future analysis, we will compare physical exam findings and self-reported pain location to examine construct validity of women’s report of vulvodynia.
Some limitations in our study warrant consideration. The women in our sample were relatively young, predominately White, and 84% had college or graduate degrees. Additional research is needed to determine whether our findings apply to Black women, older adult White women and women with less than college education. It is unknown why three women did not complete the general body outline but did complete the genital specific outline. Furthermore, our study focused on a pain condition experienced only by women. Additional research is needed to address the validity and reliability of the BSA% as a measure of pain location for women and males with pain conditions.
Conclusion
The study’s findings from women with vulvodynia support concurrent validity of the BSA% as a measure of pain location using either outline. The general body outline alerts to the need for more specific genital information and that pain also is present in other areas. The genital area outline provides more specific information about the precise location of pain in the vulvar region, and implications for its use have potential to improve the detection and monitoring of vulvodynia.
Future perspective
Future management of women with vulvodynia will be enhanced by their self-report of vulvodynia pain locations drawn on a genital outline on a computerized tablet that will automatically calculate the BSA% of the painful areas. Monitoring of BSA% will enable the clinician to evaluate the pain status of women with vulvodynia. This health information will be automatically uploaded to the electronic health record for detection and monitoring of women with vulvodynia.
Summary points.
Vulvodynia is difficult to diagnose, treat and monitor.
Providing a tool to women with vulvodynia to report their pain location may lead to improved communication about pain during healthcare visits and help overcome barriers to discussion of gynecological issues.
A specific genitalia outline provides women with a digital picture of a vulva and thighs to draw where they feel their vulvodynia.
Implications for a digital genital outline have potential to improve the reporting, detection and monitoring of vulvodynia.
Findings support beginning validity of body surface area as a measure of pain location using either outline.
Footnotes
Author contributions
DJ Wilkie and JM Schlaeger conceptualized this study. DJ Wilkie and Y Yao contributed to the design and plan for analysis. Acquisition of the data was completed by JM Schlaeger, G Telisnor and JE Glayzer. DJ Wilkie, Y Yao and R Garg developed the computer program. Analysis and interpretation of the data was performed by Y Yao and DJ Wilkie. The manuscript was drafted by G Telisnor, JE Glayzer, G-E Kiros, WH Kobak, DJ Wilkie and JM Schlaeger. All authors edited and revised the manuscript for content and also read and approved the final version of the manuscript accepted for publication.
Financial & competing interests disclosure
This research was made possible by grant numbers U54CA233396, U54CA233444, U54CA233465, R25CA214225, R01HD091210 and F31NR019529 from the National Institutes of Health (NIH), National Cancer Institute (NCI), Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the National Institute for Nursing Research (NINR). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCI or NICHD. The final peer-reviewed manuscript is subject to the National Institutes of Health Public Access Policy. This publication is co-sponsored by the Rockefeller University Heilbrunn Family Center for Research Nursing through the generosity of the Heilbrunn Family and the National Center for Advancing Translational Sciences, National Institutes of Health, through Rockefeller University, Grant Number UL1TR001866. DJ Wilkie is the founder and chairman of eNURSING LLC, a company without current ownership of the PAINReportIt software. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Ethical conduct of research
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
Data sharing statement
The authors certify that this manuscript reports original clinical trial data (NCT03364127). The datasets used and/or analyzed during the current study are available from the corresponding author after deidentification on reasonable request. Other documents available are the study protocol, statistical analysis plan and the analytical code. The data will be available beginning 9 months and up to 36 months following article publication. Data will be shared with researchers who provide a methodologically sound proposal to achieve aims in the approved proposal. Proposals should be directed to jschlaeg@uic.edu. Data requesters will need to sign a data use agreement.
References
- 1.Bornstein J, Goldstein AT, Stockdale CK et al. 2015 ISSVD, ISSWSH and IPPS consensus terminology and classification of persistent vulvar pain and vulvodynia. Obstet. Gynecol. 127(4), 745–751 (2016). [DOI] [PubMed] [Google Scholar]
- 2.Schlaeger JM, Patil CL, Steffen AD et al. Sensory pain characteristics of vulvodynia and their association with nociceptive and neuropathic pain: an online survey pilot study. Pain Rep. 4(2), e713 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reed BD, Harlow SD, Sen A et al. Prevalence and demographic characteristics of vulvodynia in a population-based sample. Am. J. Obstet. Gynecol. 206(2), 170 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schlaeger JM, Pauls HA, Powell-Roach KL et al. Vulvodynia, “a really great torturer”: a mixed methods pilot study examining pain experiences and drug/non-drug pain relief strategies. J. Sex. Med. 16(8), 1255–1263 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodriguez SB, Schonfeld TL. The organ-that-must-not-be-named: female genitals and generalized references. Hastings Cent. Rep. 42(3), 19–21 (2012). [DOI] [PubMed] [Google Scholar]
- 6.Shallcross R, Dickson JM, Nunns D, Mackenzie C, Kiemle G. Women’s subjective experiences of living with vulvodynia: a systematic review and meta-ethnography. Arch. Sex. Behav. 47(3), 577–595 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen R, MacLehose RF, Veasley C, Turner RM, Harlow BL, Horvath KJ. Comfort in discussing vulvar pain in social relationships among women with vulvodynia. J. Reprod. Med. 57(3-4), 109–114 (2012). [PubMed] [Google Scholar]
- 8.Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain 1(3), 277–299 (1975). [DOI] [PubMed] [Google Scholar]
- 9.Margolis RB, Tait RC, Krause SJ. A rating system for use with patient pain drawings. Pain 24(1), 57–65 (1986). [DOI] [PubMed] [Google Scholar]
- 10.Savedra MC, Holzemer WL, Tesler MD, Wilkie DJ. Assessment of postoperation pain in children and adolescents using the adolescent pediatric pain tool. Nurs. Res. 42(1), 5–9 (1993). [PubMed] [Google Scholar]
- 11.Toomey TC, Gover VF, Jones BN. Site of pain: relationship to measures of pain description, behavior and personality. Pain 19(4), 389–397 (1984). [DOI] [PubMed] [Google Scholar]
- 12.Türp J, Kowalski C, O’Leary N, Stohler C. Pain maps from facial pain patients indicate a broad pain geography. J. Dent. Res. 77(6), 1465–1472 (1998). [DOI] [PubMed] [Google Scholar]
- 13.Lai HH, Jemielita T, Sutcliffe S et al. Characterization of whole body pain in urological chronic pelvic pain syndrome at baseline: a MAPP research network study. J. Urol. 198(3), 622–631 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lluch Girbés E, Dueñas L, Barbero M et al. Expanded distribution of pain as a sign of central sensitization in individuals with symptomatic knee osteoarthritis. Phys. Ther. 96(8), 1196–1207 (2016). [DOI] [PubMed] [Google Scholar]
- 15.Saltychev M, Laimi K. Predicting self-reported disability level by a number of pain sites marked on pain drawing. Int. J. Rehabil. Res. 41(3), 276–279 (2018). [DOI] [PubMed] [Google Scholar]
- 16.Wilkie DJ, Judge MK, Berry DL, Dell J, Zong S, Gilespie R. Usability of a computerized PAINReportIt in the general public with pain and people with cancer pain. J. Pain Symptom Manage. 25(3), 213–224 (2003). [DOI] [PubMed] [Google Scholar]
- 17.Pukall CF, Bergeron S, Brown C, Bachmann G, Wesselmann U. Vulvodynia collaborative research group recommendations for self-report outcome measures in vulvodynia clinical trials. Clin. J. Pain 33(8), 756–765 (2017). [DOI] [PubMed] [Google Scholar]
- 18.Rosen NO, Bergeron S, Pukall CF. Recommendations for the study of vulvar pain in women, part 2: methodological challenges. J. Sex. Med. 17(4), 595–602 (2020). [DOI] [PubMed] [Google Scholar]
- 19.Rosen NO, Bergeron S, Pukall CF. Recommendations for the study of vulvar pain in women, part 1: review of assessment tools. J. Sex. Med. 17(2), 180–194 (2020). [DOI] [PubMed] [Google Scholar]
- 20.Schneider CA, Rasband WS, Eliceiri KW. NIH image to ImageJ: 25 years of image analysis. Nat. Methods 9(7), 671–675 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miksch RC, Hao J, Schoenberg MB et al. Development of a reliable and accurate algorithm to quantify the tumor immune stroma (QTiS) across tumor types. Oncotarget 8(70), 114935 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steffen AD, Burke LA, Pauls HA et al. Double-blinding of an acupuncture randomized controlled trial optimized with clinical translational science award resources. Clin. Trials 17(5), 545–551 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jha A, Suarez ML, Ferrans CE, Molokie R, Kim YO, Wilkie DJ. Cognitive testing of PAINReportIt® in adult African Americans with sickle cell disease. Comput. Inform. Nurs. 28(3), 141 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilkie DJ, Yao Y, Ezenwa MO et al. A stepped-wedge randomized controlled trial: effects of ehealth interventions for pain control among adults with cancer in hospice. J. Pain Symptom Manage. 59(3), 626–636 (2020). [DOI] [PubMed] [Google Scholar]
- 25.Schlaeger JM, Takakura N, Yajima H et al. Double-blind acupuncture needles: a multi-needle, multi-session randomized feasibility study. Pilot Feasibility Stud. 4(1), 1–8 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Preti M, Selk A, Stockdale C et al. Knowledge of vulvar anatomy and self-examination in a sample of Italian women. J. Low. Genit. Tract Dis. 25(2), 166–171 (2021). [DOI] [PubMed] [Google Scholar]


