Abstract
Eleven clonally related Klebsiella pneumoniae isolates were examined. These had been isolated at an intensive care unit in Amsterdam in 1994. Their resistance was associated with a conjugative 170-kb plasmid which encoded a novel SHV β-lactamase designated SHV-13. The SHV-13 enzyme had two substitutions compared with SHV-1: Leu35Gln and Gly238Ala. It hydrolyzed cefotaxime much more rapidly than ceftazidime or aztreonam.
Klebsiella pneumoniae is a successful opportunistic pathogen and is often multiresistant to antibiotics. Extended-spectrum β-lactamases (ESBLs) are more prevalent in K. pneumoniae than in any other enterobacterial species, and outbreaks of infections caused by ESBL-producing strains have been reported widely (3, 7, 10, 14, 15). Most ESBLs are mutant TEM and SHV enzymes (2, 5; G. A. Jacoby and K. Bush [http://www.lahey.org/studies/webt.htm]), and over 60 ESBL variants have been described within these β-lactamase families (Jacoby and Bush website). Hydrolysis kinetics vary among different TEM and SHV mutants, but the general pattern is for activity to be gained against oxyimino-aminothiazolyl cephalosporins but not cephamycins or carbapenems. The plasmids determining ESBLs are mostly large (≥80 kb) and encode multiple resistances (5).
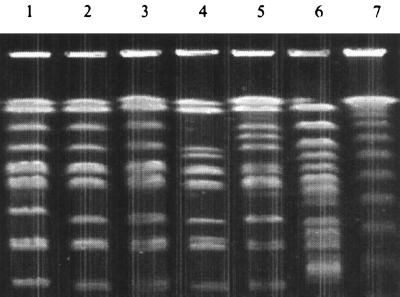
New ESBLs continue to be described. In a recent survey of isolates from intensive care units in Europe, we found a cluster of 11 ESBL-positive klebsiellae at a hospital in Amsterdam (17). These appeared to be clonally related, giving similar DNA fingerprints following pulsed-field gel electrophoresis (PFGE) of XbaI genomic digests (Fig. 1). They had a pI 7.6 β-lactamase, which was inferred to be of the SHV type. Single-strand conformational polymorphism analysis of the PCR product of blaSHV was undertaken for four representatives, and a pattern was observed that was different from that of any control (17). This result implied that the SHV β-lactamase might be a novel type. We now report the properties of this enzyme and the sequence of its encoding gene.
FIG. 1.
DNA profiles of representatives of the K2/PN16 strain determined by PFGE. Tracks: 1 to 5, representatives of the K2/PN16 strain with isolate 803 (used for sequencing of blaSHV and as a source of enzyme for purification in track 2); 6, an unrelated ESBL-positive K. pneumoniae strain collected at the same hospital in Amsterdam; 7, molecular weight marker.
The 11 isolates were from the medical intensive care unit serving the pediatric and neonatal wards of the hospital. Eight were from the respiratory tracts of patients, one was from blood, and two were from unrecorded sites. Nine of the source patients were under 1 year old; the others were 1 and 3 years old. Collection was done from January to October 1994, and over half of the isolates were obtained in January. The isolates were identified to the genus level with the API 20E system (bioMerieux, La Balme les Grottes, France) and confirmed as K. pneumoniae by their ability to grow at 42°C but not at 4 and 10°C (17). Eight of the isolates were of capsular serotype K2, and three were acapsular (17).
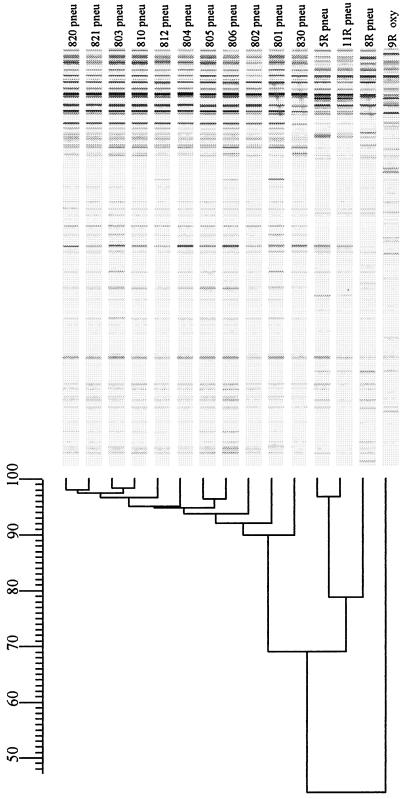
Amplified fragment length polymorphism (AFLP) fingerprinting of genomic DNA was performed by the method of Koeleman et al. (8). Briefly, purified chromosomal DNA was digested with EcoRI and MseI and ligated into double-stranded oligonucleotide adapters. The ligated restriction fragments were amplified by the method of Vos et al. (16), with a fluorescently labeled Eco primer (8), and the amplified fragments were separated by polyacrylamide gel electrophoresis on an automated DNA sequencer (Vistra; Amersham, Buckinghamshire, United Kingdom). A dendrogram to illustrate the relatedness of the isolates was constructed with Gelcompar software (Applied Maths, Kortrijk, Belgium).
MICs were determined on IsoSensitest agar (Oxoid, Basingstoke, Hampshire, United Kingdom) with inocula of 104 CFU/spot (10). Antimicrobials were supplied as follows: aztreonam, Bristol-Myers Squibb, Hounslow, Middlesex, United Kingdom; cefotaxime, Hoechst-Marion-Roussel, Uxbridge, Middlesex, United Kingdom; ceftazidime and cefuroxime, Glaxo Wellcome, Stevenage, Hertfordshire, United Kingdom; piperacillin and tazobactam, Wyeth, Taplow, Berkshire, United Kingdom; cefoxitin and imipenem, Merck Sharp & Dohme, Hoddesdon, Hertfordshire, United Kingdom; ceftriaxone, Roche, Welwyn Garden City, Hertfordshire, United Kingdom; amikacin, gentamicin, and ciprofloxacin, Sigma, St. Louis, Mo.; clavulanate, SmithKline Beecham, Harlow, Essex, United Kingdom.
Plasmids were extracted by the method of Kado and Liu (6) and electrophoresed at 100 V for 1 to 2 h on 0.8% agarose gels in Tris-borate-EDTA buffer. Estimation of plasmid sizes was done by comparison to Escherichia coli NCTC 50192, with plasmids of 154, 66, 38, and 7 kb, and E. coli NCTC 50193, with plasmids of 11.5, 8.0, 5.9, 3.0, 2.7, and 2.1 kb. Conjugation was done by plate mating of logarithmic-phase cultures with E. coli K-12 J62-1 (lac Nalr) (9). Transconjugants were selected on Diagnostic Sensitivity Test agar (Oxoid) containing ceftazidime at 2 or 5 μg/ml plus nalidixic acid at 250 μg/ml.
Isoelectric focusing was performed on polyacrylamide gels (9, 17) with TEM-1 (pI 5.4), TEM-2 (pI 5.6), TEM-3 (pI 6.3), SHV-1 (pI 7.6), SHV-3 (pI 7.0), SHV-4 (pI 7.8), and SHV-5 (pI 8.2) as controls. PCR was used to amplify blaSHV with the primers SHV A (5′-TCAGCGAAAAACACCTTG-3′, corresponding to positions 435 to 452 in blaSHV (11), SHV C (5′-ATGCGTTATATTCGCCTGTG-3′, corresponding to positions 125 to 144 in blaSHV, SHV D (5′-GTTAGCGTTGCCAGTGCTCG-3′; complementary strand, corresponding to positions 970 to 989 in blaSHV), and SHV E (5′-CCGTTTCCCAGCGGTCAAGG-3′; complementary strand, corresponding to positions 595 to 614 in blaSHV). The PCR products were sequenced on an automatic sequencer (ABI 377; Perkin-Elmer, Warrington, Cheshire, United Kingdom) with AmpliTaq DNA polymerase FS (Perkin-Elmer), both used in accordance with the manufacturer's directions. Results were collected with Data Collection Software (Perkin-Elmer) and analyzed with the Sequence Navigator software (Perkin-Elmer) run on a Power Macintosh. GCG software (Human Genome Mapping Project, Cambridge, United Kingdom) was used to compare the sequences with those in the GenBank database.
K. pneumoniae 803 was used as a source of enzyme for purification on the ground that it was the most resistant representative of the strain, implying that it makes the most β-lactamase; this isolate was also among the four representatives previously shown to give the novel single-strand conformational polymorphism-PCR fingerprint for blaSHV (17). Cultures were grown overnight at 37°C in Iso-Sensitest broth with shaking and then diluted 10-fold into fresh warm broth. After incubation for a further 4 h, the cells were harvested by centrifugation at 5,000 × g and 37°C for 15 min, washed once in 0.05 M phosphate buffer (pH 7.0), and disrupted by three cycles of freezing and thawing. Debris was removed by ultracentrifugation at 100,000 × g and 4°C for 45 min, and the supernatant was applied to a carboxymethyl–Sephadex C-50 column (40 by 2.6 cm [diameter]; Pharmacia, Milton Keynes, Buckinghamshire, United Kingdom) equilibrated with 50 mM phosphate buffer (pH 7.0). After overnight washing at 4°C with the same buffer, this column was eluted with 500 ml of 50 mM phosphate buffer (pH 7.0) containing a linear gradient of 0 to 0.5 M NaCl, also at 4°C. The β-lactamase-containing fractions were dialyzed at 4°C against 5 liters of 25 mM malonate buffer (pH 6.0) and then loaded onto a 16/10 S-Sepharose High Performance column (Pharmacia) equilibrated with this same buffer at 4°C. This column was washed with 60 ml of 25 mM malonate buffer (pH 6.0) and then eluted at 4°C with a 0 to 0.5 M NaCl gradient. The fractions with the greatest β-lactamase activity were retained, dialyzed extensively against 0.1 M phosphate buffer (pH 7.0), and stored at −20°C. Hydrolysis of β-lactams was examined by UV spectrophotometric assay in 0.1 M phosphate buffer (pH 7.0) at 37°C using the wavelengths listed previously (9). Km and Vmax values were calculated by linear regression analysis of Hanes plots of initial-velocity data. Inhibition studies were undertaken at 37°C in 0.1 M phosphate buffer (pH 7.0) with benzylpenicillin as the substrate and with clavulanate and tazobactam as inhibitors.
All 11 isolates gave similar PFGE profiles after digestion of genomic DNA with XbaI (Fig. 1). Based on criteria described previously—i.e., not more than three band differences from the most similar isolate of the strain—the isolates were judged to belong to the same strain, designated K2/PN16 (17). Their relatedness was confirmed by AFLP, which gave similar patterns for all 11 isolates, whereas grossly different patterns were given by epidemiologically unrelated isolates from the same hospital (Fig. 2).
FIG. 2.
DNA fingerprints of members of the K2/PN16 strain determined by AFLP. Tracks: 1 to 11, members of the K2/PN16 strain, as labeled; 12 to 15, unrelated strains used as controls.
All 11 isolates were highly resistant to piperacillin (MICs, 512 to 1,024 μg/ml). MICs of cefotaxime, ceftazidime, ceftriaxone, cefuroxime, and aztreonam ranged widely but were 4- to 32-fold above the modal MICs for ESBL-negative K. pneumoniae (Table 1). All of the isolates were susceptible to imipenem at ≤0.5 μg/ml). They also remained susceptible to gentamicin at ≤2 μg/ml and to amikacin at ≤16 μg/ml; nevertheless, the MICs of these aminoglycosides were slightly above modal values for ESBL-negative K. pneumoniae from the 1994 survey (Table 1). All 11 isolates were susceptible to ciprofloxacin at ≤0.25 μg/ml.
TABLE 1.
MICs of antibiotics for K. pneumoniae isolates and comparators and for E. coli J62-1 and its transconjugant with the SHV-13 β-lactamasea
| Isolate | Gm | Ak | Cip | Azt | Caz | Caz-Clav | Ctx | Ctr | Cxm | Fox | Pip | Pip-Taz | Imp | Profile of plasmid sizes (kb) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 801 | 0.5 | 2 | 0.06 | 1 | 8 | 0.25 | 4 | 8 | 16 | 4 | 512 | 4 | 0.25 | 170/50/3.1 |
| 802 | 0.5 | 2 | 0.25 | 2 | 16 | 0.5 | 4 | 16 | 16 | 8 | 1,024 | 16 | 0.25 | 170/100/50/3.5 |
| 803 | 1 | 2 | 0.03 | 256 | 256 | 0.5 | 8 | 16 | 16 | 4 | 512 | 8 | 0.25 | 170/50/3.1 |
| 804 | 0.25 | 1 | 0.03 | 0.5 | 16 | 0.25 | 4 | 16 | 16 | 2 | 1,024 | 4 | 0.25 | 170/50/3.1 |
| 805 | 0.5 | 2 | 0.03 | 1 | 8 | 0.25 | 4 | 32 | 8 | 4 | 512 | 8 | 0.25 | 170/50/3.1 |
| 806 | 1 | 4 | 0.06 | 8 | 32 | 0.5 | 4 | 32 | 16 | 4 | 1,024 | 8 | 0.5 | 170/50/3.1 |
| 810 | 0.25 | 4 | 0.03 | 1 | 4 | 0.25 | 2 | 16 | 16 | 4 | 512 | 4 | 0.12 | 170/50/3.1 |
| 812 | 0.25 | 2 | 0.03 | 1 | 4 | 0.25 | 4 | 8 | 8 | 4 | 512 | 2 | 0.25 | 170/50/3.1 |
| 820 | 0.25 | 2 | 0.03 | 2 | 8 | 0.5 | 8 | 8 | 16 | 4 | 1,024 | 8 | 0.25 | 170/38/3.1 |
| 821 | 2 | 16 | 0.06 | 2 | 8 | 0.25 | 16 | 16 | 16 | 4 | 512 | 4 | 0.5 | 170/66/50/3.1 |
| 830 | 1 | 2 | 0.06 | 1 | 8 | 0.25 | 4 | 8 | 32 | 4 | 512 | 16 | 0.25 | 170/50/3.1 |
| Mode MICs for ESBL-negative: | ||||||||||||||
| K. pneumoniaeb | 0.5 | 1 | 0.03 | 0.03 | 0.25 | 0.12 | NDe | 0.06 | 2 | 4 | 4 | 2 | ND | |
| E. coli K-12 J62-1 R− c | 0.5 | 2 | 0.12 | ≤0.25 | ≤0.25 | ≤0.25 | ≤0.25 | ≤0.25 | 4 | 4 | 2 | 2 | 0.25 | |
| E. coli K-12 J62-1/803d | 2 | 8 | 0.12 | 8 | 64 | 0.12 | 4 | 4 | 16 | 4 | 256 | 4 | 0.25 | 170 |
MICs are given in micrograms per milliliter. Abbreviations: Gm, gentamicin; Ak, amikacin; Cip, ciprofloxacin; Caz, ceftazidime; Caz-Clav, ceftazidime-clavulanate; Ctr, ceftriaxone; Ctx, cefotaxime; Cxm, cefuroxime; Fox, cefoxitin; Pip, piperacillin; Pip-Taz, piperacillin-tazobactam; Imp, imipenem.
From reference 10.
Recipient.
Transconjugant of strain 803.
ND, not determined.
A pI 7.6 β-lactamase activity was detected by isoelectric focusing in all 11 isolates, and no other β-lactamase activities were found. All 11 isolates had a 170-kb plasmid and various smaller plasmids (Table 1); 50- and 3.1-kb plasmids also were present in most isolates. Ceftazidime resistance was conjugatively transferred to E. coli K-12 J62-1 from isolate 803, which was taken as a representative. The transconjugants were confirmed to be ceftazidime resistant and lactose negative and were found to have acquired only the 170-kb plasmid; they also acquired the pI 7.6 enzyme and became resistant to all aminothiazolyl cephalosporins and piperacillin but not to cephamycins, carbapenems, or gentamicin (Table 1). Although isolate 803 was unusually resistant to aztreonam, this behavior was not seen in its transconjugant and may have reflected some other factor, possibly a permeability lesion.
The nucleotide sequence of the SHV β-lactamase gene from isolate 803 was determined twice, with identical results in both experiments. The deduced amino acid sequence had two substitutions compared with SHV-1: Gly238Ala (GGC replaced by GCC) and Leu35Glu (CTA replaced by CAA). Leu35Glu is shared by SHV-2a, -11, and -12 (Table 2), but alanine at position 238 is unique to the present enzyme, which therefore differed from all of the SHV variants reported previously and was named SHV-13. No further silent mutations were observed. Gly238Ser alone allows hydrolysis of cefotaxime, whereas both Ser238 and Lys240 are needed for rapid hydrolysis of ceftazidime (4). It now appears that Ala238 can give cefotaximase activity, as can Ser238. Alanine and serine both have a small α-carbon side chain (-CH3 and -CH2OH, respectively), whereas glycine has no side chain. Although position 35 is remote from the active site, it may influence resistance to cephaloridine and cefotaxime (7, 12, 13). Like other ESBLs, the SHV-13 enzyme hydrolyzed all of the penicillins and cephalosporins tested except cephamycins. It had similarly strong activity against benzylpenicillin, ampicillin, piperacillin, and cephaloridine, but the Km for cephaloridine exceeded that for penicillins (Table 3), reducing the kinetic efficiency (Vmax/Km). The Vmax for cefotaxime was 27% of that for benzylpenicillin, confirming that SHV-13 is an ESBL; nevertheless, its relative rates of ceftazidime and aztreonam hydrolysis were slow compared with those of many other ESBLs, and the Vmax/Km ratios for cefotaxime, ceftriaxone, and cefuroxime were only 2 to 11% of those for benzylpenicillin. The preferential activity of SHV-13 against cefotaxime resembled the behavior of SHV-2a, an enzyme with similar substitutions (Table 2). Hydrolysis of ceftazidime was slow, despite the considerable ceftazidime resistance of the isolates (Tables 1 and 3). Like other ESBLs, SHV-13 lacked activity against cefoxitin and imipenem. Slow hydrolysis of oxacillin was detected, and it obeyed nonlinear kinetics, with the hydrolysis rate declining more swiftly than was explicable by substrate depletion. Clavulanate and tazobactam were potent inhibitors. When the SHV-13 enzyme was preincubated with inhibitor for 10 min at 37°C before addition of 1 mM benzylpenicillin, the 50% inhibitory concentration (I50) of clavulanate for inhibition of the hydrolysis of 1 mM benzylpenicillin was 0.003 μM, whereas the I50 of tazobactam was 0.5 μM. The reported I50s of clavulanate and tazobactam for the classical SHV-1 enzyme are 0.03 and 0.14 μM, respectively (2).
TABLE 2.
Comparative amino acid sequences of SHV-13 and closely related SHV β-lactamases
| β-Lactamase | pI | Amino acid at position:a
|
|||
|---|---|---|---|---|---|
| 8 | 35 | 238 | 240 | ||
| SHV-1 | 7.6 | Ile | Leu | Gly | Glu |
| SHV-2 | 7.6 | Ser | |||
| SHV-2a | 7.6 | Gln | Ser | ||
| SHV-11 | 7.6 | Gln | |||
| SHV-12 | 8.2 | Gln | Ser | Lys | |
| SHV-13b | 7.6 | Gln | Ala | ||
Details are from the Jacoby and Bush website (http://www.lahey.org/studies/webt.htm); amino acid numbering follows Ambler et al. (1).
This study.
TABLE 3.
Kinetic properties of the SHV-13 enzyme from K. pneumoniae 803
| Substrate | Km (μM) | Relative Vmaxa of SHV-13 (%) | Vmax/Kma ratio | Relative Vmaxa of SHV-1 (%)d |
|---|---|---|---|---|
| Benzylpenicillin | 10 | 100 | 100 | 100 |
| Ampicillin | 28 | 178 | 64 | 150 |
| Piperacillin | 18 | 136 | 76 | |
| Oxacillin | NDb | NLKc | ND | <0.5 |
| Cephaloridine | 97 | 176 | 18 | 48 |
| Cefuroxime | 61 | 11 | 1.8 | ND |
| Ceftriaxone | 11 | 12 | 11 | ND |
| Cefotaxime | 52 | 27 | 5.2 | 0.18 |
| Ceftazidime | 91 | 0.38 | 0.42 | 0.02 |
| Cefoxitin | ND | <0.1 | ND | 0 |
| Aztreonam | 77 | 0.66 | 0.86 | <0.38 |
| Imipenem | ND | <0.1 | ND | ND |
Relative to that for benzylpenicillin, which was set at 100%.
ND, not determined.
NLK, nonlinear kinetics.
From reference 2.
We cannot discount the possibility that isolate 803 also had SHV-1 β-lactamases, as do the majority of K. pneumoniae isolates, and that this copurified with SHV-13. Nevertheless, sequencing gave single signals for the bases corresponding to amino acids 35 and 238, suggesting a much higher gene dosage of SHV-13. Moreover, the kinetics of SHV-13 were linear (except with oxacillin), suggesting that contamination was, at worst, minimal.
In summary, SHV-13 adds to the growing catalogue of ESBLs. It had substitutions at amino acids 35 and 238, which are critical residues in defining the substrate specificity of SHV enzymes. Replacement of glycine 238 with alanine seems to be unique to SHV-13, but replacement with serine at position 238 is well known to be associated with ESBL activity.
Nucleotide sequence accession number.
GenBank accession no. AF 164577 was allocated to the sequence for blaSHV-13.
Acknowledgments
We are grateful to Wyeth Laboratories UK (Taplow, Berkshire, United Kingdom) and Wyeth International Division (St. Davids, Philadelphia, Pa.) for financial support.
REFERENCES
- 1.Ambler R P, Coulson A F, Frère J M, Ghuysen J M, Joris B, Forsman M, Levesque R C, Tiraby G, Waley S G. A standard numbering scheme for the class A β-lactamases. Biochem J. 1991;276:269–270. doi: 10.1042/bj2760269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bush K, Jacoby G A, Medeiros A A. A functional classification scheme for β-lactamases and its correlation with molecular structure. Antimicrob Agents Chemother. 1995;39:1211–1233. doi: 10.1128/aac.39.6.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hobson R P, MacKenzie F M, Gould I M. An outbreak of multiply-resistant Klebsiella pneumoniae in the Grampian region of Scotland. J Hosp Infect. 1996;33:249–262. doi: 10.1016/s0195-6701(96)90011-0. [DOI] [PubMed] [Google Scholar]
- 4.Huletsky A, Knox J R, Levesque R C. Role of Ser-238 and Lys-240 in the hydrolysis of third-generation cephalosporins by SHV-type β-lactamases probed by site-directed mutagenesis and three-dimensional modeling. J Biol Chem. 1993;268:3690–3697. [PubMed] [Google Scholar]
- 5.Jacoby G A, Medeiros A A. More extended-spectrum β-lactamases. Antimicrob Agents Chemother. 1991;35:1697–1704. doi: 10.1128/aac.35.9.1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kado C I, Liu S T. Rapid procedure for detection and isolation of large and small plasmids. J Bacteriol. 1981;145:1365–1373. doi: 10.1128/jb.145.3.1365-1373.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim J, Kwon Y, Pai H, Kim J-W, Cho D-T. Survey of Klebsiella pneumoniae strains producing extended-spectrum β-lactamases: prevalence of SHV-12 and SHV-2a in Korea. J Clin Microbiol. 1998;36:1446–1449. doi: 10.1128/jcm.36.5.1446-1449.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koeleman J G M, Stoof J, Biesmans D J, Savelkoul P H M, Vandenbroucke-Grauls C M J E. Comparison of amplified ribosomal DNA restriction analysis, random amplified polymorphic DNA analysis, and amplified fragment length polymorphism fingerprinting for identification of Acinetobacter genomic species and typing of Acinetobacter baumannii. J Clin Microbiol. 1998;36:2522–2529. doi: 10.1128/jcm.36.9.2522-2529.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Livermore D M, Williams J D. β-Lactams: mode of action and mechanisms of bacterial resistance. In: Lorian V, editor. Antibiotics in laboratory medicine. 4th ed. Baltimore, Md: The Williams & Wilkins Co.; 1996. pp. 502–578. [Google Scholar]
- 10.Livermore D M, Yuan M. Antibiotic resistance and extended-spectrum β-lactamases amongst Klebsiella spp. from intensive care units in Europe. J Antimicrob Chemother. 1996;38:409–424. doi: 10.1093/jac/38.3.409. [DOI] [PubMed] [Google Scholar]
- 11.Mercier J, Levesque R C. Cloning of SHV-2, OHIO-1, and OXA-6 β-lactamases and cloning and sequencing of SHV-1 β-lactamase. Antimicrob Agents Chemother. 1990;34:1577–1583. doi: 10.1128/aac.34.8.1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nüesch-Inderbinen M T, Hächler H, Kayser F H. New system based on site-directed mutagenesis for highly accurate comparison of resistance levels conferred by SHV β-lactamases. Antimicrob Agents Chemother. 1995;39:1726–1730. doi: 10.1128/aac.39.8.1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nüesch-Inderbinen M T, Kayser F H, Hächler H. Survey and molecular genetics of SHV β-lactamases in Enterobacteriaceae in Switzerland: two novel enzymes, SHV-11 and SHV-12. Antimicrob Agents Chemother. 1997;41:943–949. doi: 10.1128/aac.41.5.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Podschun R, Ullmann U. Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin Microbiol Rev. 1998;11:589–603. doi: 10.1128/cmr.11.4.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shannon K, Stapleton P, Xiang X, Johnson A, Beattie H, Bakri F E, Cookson B, French G. Extended-spectrum β-lactamase-producing Klebsiella pneumoniae strains causing nosocomial outbreaks of infection in the United Kingdom. J Clin Microbiol. 1998;36:3105–3110. doi: 10.1128/jcm.36.10.3105-3110.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vos P, Hogers R, Bleeker M, Reijans M, van de Lee T, Hornes M, Frijters A, Pot J, Peleman J, Kuiper M. AFLP: a new technique for DNA fingerprinting. Nucleic Acids Res. 1995;23:4407–4414. doi: 10.1093/nar/23.21.4407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yuan M, Aucken H, Hall L M C, Pitt T L, Livermore D M. Epidemiological typing of klebsiellae with extended-spectrum β-lactamases from European intensive care units. J Antimicrob Chemother. 1998;41:527–539. doi: 10.1093/jac/41.5.527. [DOI] [PubMed] [Google Scholar]