Highlights
-
•
SGRT introduction in clinical practice is team effort by RTTS, physicists and clinicians.
-
•
It improves set up precision and is an important tool to reduce late effects by better sparing of normal tissues.
-
•
SGRT enhances patient comfort by eliminating skin markers in a majority of cases.
Keywords: SGRT, Clinical practice, Treatment delivery
Abbreviations: SGRT, surface guided radiotherapy
Abstract
To describe the rationale and process how SGRT was implemented in our department from the original decision to daily clinical practice.
Introduction
Our main reason to start with SGRT was the challenge of further optimising radiotherapy treatment after the proliferation of modulated treatments by IMRT or V-MAT in order to reduce late tissue damage. Since one of our most important case load groups are breast cancer patients, the idea to spare the lungs and heart was discussed. We decided to concentrate at first with techniques to reduce the dose to the heart, as our patients were younger, and many had an excellent prognosis and a long survival. In addition, many systemic therapies like anthracyclines or anti HER 2 substances are cardiotoxic and often used in this patient group.
According to the literature, sparing of the heart can lead to the reduction of excess morbidity and mortality in these patients. To minimise late toxicity and morbidities related to radiotherapy was, therefore, paramount. One way to achieve the sparing of normal tissue in this setting is the implementation of Deep Inspiration Breathhold (DIBH) treatment with Surface Guided Radiotherapy (SGRT). In Fig. 1, you can see the effect of gating to the heart dose in left sided breast cancer patients, taken from Heart toxicity from breast cancer radiotherapy: Current findings, assessment, and prevention Marc D. Piroth, René Baumann, Wilfried Budach, et al, Strahlenther Onkol. 2019; 195(1): 1–12.
Fig. 1.
Influence of gating on irradiated heart volumes. Marc D. Piroth, René Baumann, Wilfried Budach, et al, Strahlenther Onkol. 2019; 195(1): 1–12.
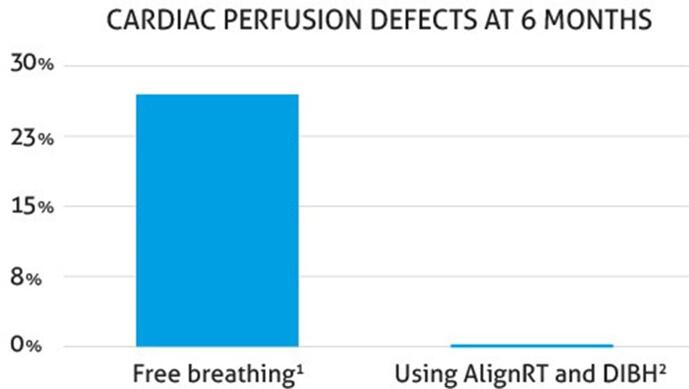
As studies showed, you can maintain cardiac perfusion by using DIBH, Fig. 2, and therefore reducing late cardiac toxicity. Therefore, we evaluated SGRT for our centre.
-
1.
Darby et al. Risk of Ischemic Heart Disease in Women after Radiotherapy for Breast Cancer. N Engl J Med 2013; 368:987–998
-
2.
Gierga et al. A Voluntary Breath-Hold Treatment Technique for the Left Breast With Unfavorable Cardiac Anatomy Using Surface Imaging. Int J Radiat Oncol Biol Phys. 2012 Dec 1;84(5):e663–8
Fig. 2.
Reduction of Cardiac Perfusion Defects By DIBH. Gierga et al. A Voluntary Breath-Hold Treatment Technique for the Left Breast With Unfavorable Cardiac Anatomy Using Surface Imaging. Int J Radiat Oncol Biol Phys. 2012 Dec 1;84(5):e663–8
Methodology
Evaluation
The evaluation team comprised a physicist, a RTT and a physician. We consider it very important that all specialty groups are included since the introduction of SGRT has major consequences for setup, treatment planning, and clinical aspects. Therefore, an interdisciplinary group should be tasked with the evaluation process.
Issues to be considered
If you start to think about implementing SGRT, there are some important points to consider as it will change your daily routine in many ways:
-
•
Compatibility: Your SGRT system has to be compatible with your treatment machines. Be aware of local modifications that might be important.
-
•
Versatility: Since most treatment centres have more than just one type of machine, make sure the SGRT system is versatile enough for all treatment units.
-
•
Ease of handling: If possible, integrate SGRT early on to avoid having multiple care paths and adapt your clinical pathways to ensure efficiency.
-
•
Reduction of kV-MV imaging: Think how to reduce imaging by ionising radiation and substitute it with SGRT.
-
•
Establish accuracy: To enhance confidence in SGRT, measure set up data before going marker and tattoo free.
Implementation
First steps: When we started treatment with SGRT, we decided to include only left sided breast cancer patients in a supine treatment position. As we saw that accuracy was enhanced and the setup time was not much longer than for traditionally treated patients, we opted to include all breast cancer patients in the SGRT set up in order to streamline the care path.
Second steps: We then went on to apply SGRT to right sided breast patients in supine position with DIBH to achieve a standard workflow for all breast cancer cases in supine setting. The next step was patients in prone position. This posed a challenge since the ROI placement is not necessarily aligned with treatment fields. As the results with the breast cancer patients was very encouraging, we went on to SGRT treatment for all planning CT based cases.
Third steps: The final step for us was going marker free. This markedly improved set up accuracy precision and patient comfort. By introducing SGRT we could omit skin markers for the majority of our patients. One note of caution: 3 of 120 pts still needed skin marks due to half beam techniques at that stage.
Results
Setup of ROIs
To get the maximum benefit from SGRT, you have to keep in mind the position of the machine gantry, of the SGRT cameras and of the patient anatomy. The setup ROIs are usually defined during the planning CT procedure.Fig. 3
Fig. 3.
Various Set Up Photos of Patients Treated With SGRT.Presented at SASRO Annual Meeting 2018
Comparison of setup accuracy before going marker free
To make sure that set up precision was maintained, we prospectively evaluated the differences before eliminating markers altogether. As shown in Fig. 4, the setup precision was even higher with SGRT.
Fig. 4.
Set Up Precision Is Higher With SGRT.Presented at SASRO Annual Meeting 2018
Sparing of normal tissues
We evaluated 44 consecutive patients with left sided breast cancer in regard to heart and lung doses and pattern of respiration (DIBH vs free breathing). One patient was excluded (male, gynecomastia, total dose 20 Gy). The mean age for DIBH was 61 years, for free breathing 68 years. Mean dose was 48 Gy + 10 Gy boost in both groups. Patient characteristics, radiotherapy techniques, and type of surgery are shown in Table 1.
Table 1.
Patient Characteristics and Treatment Modalities.
| Free breathing | DIBH | |
|---|---|---|
| Patient Characteristics, n = 43 | ||
| Number of patients | 9 | 34 |
| Radiotherapy breast only | 15 | 16 |
| Radiotherapy locoregional | 6 | 6 |
| Radiotherapy Modality | ||
| Modulated | 6 | 28 |
| 3 D conformal | 3 | 6 |
| Surgery | ||
| Breast conserving surgery | 21 | 20 |
| Mastectomy | 1 | 1 |
Mean heart and lung doses are listed in Table 2. As shown, DIBH could significantly reduce the heart in this patient group, validating our initial idea.
Table 2.
Mean heart and lung doses.
| DIBH | Free breathe | Modulated | 3 D conformal | |||
|---|---|---|---|---|---|---|
| lung | 6.51 Gy | 7.43 Gy, | n.s. | 7.56 Gy | 6.02 Gy | n.s. |
| heart | 1.11 Gy | 1.66 Gy | p < 0.005 | 1.24 Gy | 1.21 Gy | n.s. |
Next steps
After a learning phase of 4 weeks, the time for patient positioning was not prolonged by using SGRT. The machine time was given by the RT technique (modulated or 3 D conformal) and the breathing technique (DIBH vs free breathing), with of course longer time for modulated and DIBH techniques. Due to the easy implementation in our clinical routine, we could develop standardized care path for all 3 D planned patients. SGRT was highly accepted by the patients as skin markers were no longer necessary.
Conclusion
The introduction of SGRT in our department was an evolutionary process from the beginning. A team of RTTs, phycisists, and clinicians evaluated the SGRT systems and a shared decision was made. The implementation phase was accompanied by checking the various steps in clinical routine and measuring the effects prospectively.
SGRT was easily and rapidly integrating into our clinical routine and helps to optimise the clinical treatment by enhancing setup precision, sparing of normal tissues, and patient comfort.
Take home messages
-
•
Optimal sparing of normal tissue (heart and lung) with SGRT in DIBH
-
•
Compatible with modulated techniques (IMRT or VMAT)
-
•
Enhanced patient convenience (no skin markings or tattoos)
-
•
Daily routine: plan patient positioning and planning CT with SGRT:
-
•
mind camera position in regard to anatomy and ROI setting
-
•
Setup time is not increased
-
•
Very high acceptance by RTT team
-
•
Standardised workflow for all CT planned patients
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.