Abstract
Background and Objectives:
Abilities and activities that are often simultaneously valued may not be simultaneously achievable for older adults with multicomplexity. Because of this, the Geriatrics 5Ms framework prioritizes care on “what matters most.” This study aimed to evaluate and refine the What Matters Most—Structured Tool (WMM-ST).
Research Design and Methods:
About 105 older adults with an average of 4 chronic conditions completed the WMM-ST along with open-ended questions from the Serious Illness Conversation Guide. Participants also provided demographic and social information, completed cognitive screening with the Telephone-Montreal Cognitive Assessment-Short and frailty screening with the Frail scale. Quantitative and qualitative analyses aimed to (a) describe values; (b) evaluate the association of patient characteristics with values; and (c) assess validity via the tool’s acceptability, educational bias, and content accuracy.
Results:
Older adults varied in what matters most. Ratings demonstrated modest associations with social support, religiosity, cognition, and frailty, but not with age or education. The WMM-ST was rated as understandable (86%) and applicable to their current situation (61%) independent of education. Qualitative analyses supported the content validity of WMM-ST, while revealing additional content.
Discussion and Implications:
It is possible to assess what matters most to older adults with multicomplexity using a structured tool. Such tools may be useful in making an abstract process clearer but require further validation in diverse samples.
Keywords: Aging, Goals, Multimorbidity, Values
Background and Objectives
Older adults face multiple chronic conditions along with acute episodes of life-threatening illnesses. Providing disease-specific care for each condition is not feasible when treatments for one condition adversely affect another. Various frameworks, most recently the Geriatrics 5Ms (Tinetti et al., 2017) and Age-Friendly Health Systems (Institute for Healthcare Improvement, 2020), thus center care for older adults with multicomplexity on patients’ values and goals, referred to as “what matters most” (Molnar et al., 2017). The Geriatric 5Ms is a framework for optimizing geriatric care including mind, mobility, medications, multicomplexity (considering multimorbidity and complex biopsychosocial situations), and what matters most (Molnar et al., 2017).
Values reflect relatively stable beliefs about one’s self and life, whereas preferences are an expression of the attractiveness of an option and goals are desired outcomes (Naik et al., 2016; Van Haitsma et al., 2020). Thus, some distinguish two processes necessary in geriatric care. First, there needs to be a process to discern health care values, then there needs to be a conversation between the patient and clinician to align care preferences and goals with these values, such as specified in guidelines of the American Geriatrics Society (Boyd et al., 2019) and care planning protocols such as CHAT and PLAN (Corbett et al., 2020) and Patient Priorities Care (Tinetti et al., 2016). These guidelines and protocols are consistent with the principles of person-centered care in which “an individual’s values and preferences are elicited and, once expressed, guide all aspects of their health care” (American Geriatrics Society Expert Panel on Person-Centered Care, 2016) in a collaborative shared decision-making process (Kivelitz et al., 2021). Values-aligned person-centered care orients health outcomes toward quality of life rather than a specific health metric, such as a laboratory value (American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity, 2012).
There are various methods for eliciting health care values: (a) open-ended interviews, (b) rating scales, (c) narratives (i.e., stories and scenarios), and (d) decision analysis (i.e., often applied to a specific treatment decision; Fagerlin et al., 2013). Many health care values tools focus on eliciting values for persons with a serious life-limiting illness who may have a life expectancy of fewer than 6 months (Butler et al., 2014) which inform end-of-life care preferences (Bernacki & Block, 2014), for example, completion of a Physicians Order for Life-Sustaining Treatment (Bomba et al., 2012). However, such end-of-life care tools may not be entirely relevant for patients living with multicomplexity (Figure 1). Thus, tools specific to discerning values relevant to goal setting for managing multicomplexity are needed.
Figure 1.
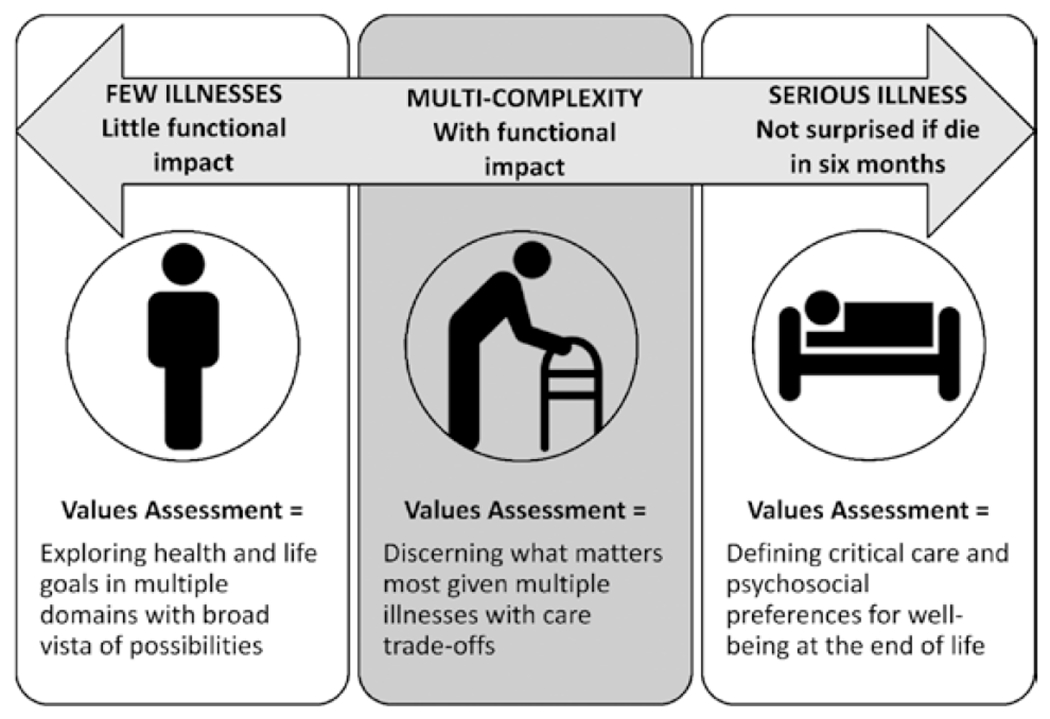
Values approaches at different levels of illness complexity and severity.
One of the challenges in eliciting values for older adults with multicomplexity is in the context of health trade-offs. That is, abilities and activities that are often simultaneously valued—such as mental clarity, avoidance of pain, privacy, caring for oneself—may not be simultaneously achievable in the setting of multicomplexity (Karel et al., 2016). Thus, the Geriatrics 5Ms framework emphasizes helping the older adults prioritize what matters most given the likelihood that not all states are simultaneously achievable (Tinetti et al., 2017). Several strategies may be used to achieve such prioritization such as Likert rating scales, forced-choice pairs, and visual analog scales (Fried et al., 2011; Karel et al., 2007, 2016; Witteman et al., 2016).
Another challenge is to ensure that values tools are understandable (Feder et al., 2019) to older adults at all levels of education, health literacy, and cognitive function (Fleary & Ettienne, 2019; McGilton et al., 2018) as individuals with multimorbidity may have some degree of associated cognitive impairment that may make abstract thinking and planning more difficult. Such patients might benefit from lists and structured questions to make an abstract process more concrete. In addition, tool characteristics such as comprehensiveness must be balanced with time efficiency in the setting of clinical practice demands, particularly as patients may need time to reflect upon and be ready to share personal values (Naik et al., 2018).
The present work is grounded in the conceptual framework of the Geriatrics 5Ms and in the domain framework of Patient Priorities Care. Patient Priorities Care categorizes values relevant to multicomplexity in four domains: functioning, enjoying life, connecting, and managing health (Tinetti et al., 2018). The goal of the project was to evaluate a new tool, the What Matters Most—Structured Tool (WMM-ST), which is structured for those with lower education or for those whose thinking may be more concrete, in older adults with multicomplexity. Our specific aims are to (a) describe values reported; (b) evaluate the association of patient characteristics with values; and (c) assess validity via the tool’s acceptability, educational bias, and content accuracy.
Research Design and Methods
Study Design
Observational cohort.
Setting
Outpatient clinics at VA Medical Center in Boston, Massachusetts between February 2019 and March 2020. This study was approved by the Institutional Review Board at VA Boston Healthcare System.
Participants
Participants were 105 older adults recruited from outpatient renal (n = 65), heart failure (n = 20), or pulmonary clinics (n = 20). Inclusion criteria were determined through electronic record review to identify those with multicomplexity defined as at least one diagnosis of metastatic/nonsurgically resectable cancer, congestive heart failure, chronic obstructive pulmonary disease, advanced renal disease, history of stroke, or failure to thrive; at least one hospitalization in the past year or Care Assessment Need (1-year event) score (Wang et al., 2013) greater than 85. Additional inclusion criteria were the ability to participate in the interview in English; no active psychotic disorder or moderate to severe dementia that would preclude the ability to provide informed consent and participate in the interview. Following the screening, participants were approached in person or by phone after a clinic appointment. Of 243 patients who met eligibility criteria, 142 agreed to participate; interviews were scheduled with 123, and 105 completed face-to-face interviews with a trained interviewer for a response rate of 43.2%.
Data Sources/Measurement
Demographic variables
Participants reported their gender (male, female, other), age, education level, marital status, and race/ethnicity (open-ended, e.g., “what is your racial and ethnic identity”). Participants also reported their religious affiliation (if any) and rated “do you consider yourself a religious person” on a 3-point scale (“not at all,” “somewhat,” and “mostly”).
Social support
Participants rated one item from the Medical Outcomes Social Support Survey (Sherbourne & Stewart, 1991), how often do you have someone “you can count on to listen to you when you need to talk” on a 5-point scale (“none of the time” to “all of the time”). This item was selected from eight items from the Emotional Support subscale (α = 0.96), with an item–subscale correlation of r = 0.82, to reduce participant burden.
Cognitive screening
Cognitive function was assessed with the Telephone-Montreal Cognitive Assessment (T-MoCA)-Short (Pendlebury et al., 2013) which assesses verbal fluency, recall, and orientation (12-point scale: 12 = intact, 9–11 = mild impairment, <9 = impairment). The T-MoCA-Short demonstrates good validity in detecting mild cognitive impairment (area under the curve for predicting multidomain mild cognitive impairment = 0.85; Pendlebury et al., 2013). We selected this instrument in the event that cognitive screening could not be completed in person, it could be completed over the telephone. However, all screening was completed in person.
Frailty screening
Frailty was assessed with the FRAIL scale (Morley et al., 2012) which assesses fatigue, resistance, ambulation, illness, and weight loss (5-point scale: 0 = robust, 1–2 = prefrail, 3–5 = frail). The FRAIL scale demonstrates good validity in association with measures of activities of daily living and physical performance in both cross-sectional and longitudinal regression analyses (Morley et al., 2012).
What Matters Most—Structured Tool
A structured values interview was constructed based on a series of prior studies (Karel et al., 1996, 2007, 2016; Moye et al., 2007). In these studies, a set of items to represent values important for health care decisions was developed through literature review and open-ended interviews with older adults (Karel et al., 1996). The test–retest reliability and validity of these items were then evaluated in three studies with older adults: persons diagnosed with mild dementia and healthy controls (Karel et al., 2007); persons diagnosed with mild dementia or schizophrenia, and healthy controls (Moye et al., 2007); and cancer survivors Karel et al., 2016). Item refinements were made based on factor analyses that identified four domains: functioning, enjoying life, connecting, and managing health (Karel et al., 2016). The present study extends this work to older adults with multiple chronic health conditions, dividing items into two sections. Section one focuses on activity and ability ratings in three domains: functioning, enjoying life, and connecting. Section two probes preferences for Managing Health. The WMM-ST research interview used in this study is given in the Supplementary Appendix.
Prior studies used one of the two approaches for values prioritization: (a) selecting the top three most important values items (Moye et al., 2007)—a potentially efficient approach in clinical application but one that does not achieve ratings of all items necessary for data analysis in research studies; (b) rating all items with a Likert scale (Karel et al., 2016)—which provides data on all items but can result in many participants rating most items at the top of the scale. As this was a research study, we used Likert ratings but included anchoring instructions to encourage the use of the full rating scale. After reading all items, participants selected one item as “of utmost importance” and one item as “not important.” Then, they were asked to rank the remaining items relative to these anchors on a 5-point scale (0 = not important, 1 = somewhat important, 2 = very important, 3 = extremely important, and 4 = of utmost importance). If a participant rated a second item “of utmost importance,” they were prompted to compare it to the other and adjust the rating if possible. Section one consisted of 12 items, culled from 16 items (Karel et al., 2016) on the basis of factor loadings as initial feasibility testing proved it was challenging to use anchoring across 16 items. Section two probed preferences for managing health as avoiding discomfort (two items), the influence of religious/spiritual beliefs on decisions (one item), desired input from others in health care decision making (two items), and perspectives on quality versus length of life (two items).
Serious Illness Conversation Guide open-ended questions
Participants rated six open-ended questions from the “explore” portion of the Serious Illness Conversation Guide (Ariadne Labs, 2015) assessing (a) Goals: What are your most important goals if your health situation worsens?; (b) Fears/Worries: What are your biggest fears and worries about the future with your health?; (c) Strengths: What gives you strength as you think about the future with your illness?; (d) Function: What abilities are so critical to your life that you can’t imagine living without them?; (e) Trade-offs: If you become sicker, how much are you willing to go through for the possibility of gaining more time?; (f) Family: How much does your family know about your priorities and wishes? The Serious Illness Conversation Guide was developed for patients with serious life-limiting illnesses in oncology (Paladino et al., 2020). Responses were audio-recorded and transcribed.
Acceptability
Participants rated the acceptability of the WMM-ST and the Serious Illness Conversation Guide on a 5-point Likert scale (“not at all” to “completely”): questions are easy for me to understand, apply to what I am going through now, and make me sad to think about.
Statistical Methods
Quantitative
WMM-ST values responses were characterized through frequency and mean endorsement for values items and subscales. Values response categories were reduced to 3-point scales across items to permit comparison across items (see Table 2 note) and creation of seven subscales, from Section one (functioning, enjoying life, and connecting) and Section two (avoiding discomfort, influence of religion, input from others, and quality vs. length of life). The association of patient characteristics with values was evaluated through a series of seven multivariate linear regression analyses of demographic and clinical variables (age, education, social support, religiosity, cognition, and frailty) on the seven subscales. Because of the small number of individuals who identified their race or ethnicity as Black, Latinx, or other (n = 12), we did not include this variable in the regression analyses but rather examined potential relationships between race/ethnicity and values using t-tests. Acceptability was examined by determining frequency ratings on three acceptability items and comparing the WMM-ST and Serious Illness Conversation Guide using chi-square tests. Educational bias was examined through a bivariate correlation between education and patient ratings of understandability. We also examined the relationship of education and total response length on the Serious Illness Conversation Guide.
Table 2.
Percent and Mean Endorsement on What Matters Most–Structured Tool
| Percent endorsement |
|||||
|---|---|---|---|---|---|
| Domain and item | 1 | 2 | 3 | M | SD |
| 1. Functioning | 2.59 | 0.39 | |||
| Taking care of self | 12.4 | 15.2 | 72.4 | 2.60 | 0.70 |
| Thinking clearly about things | 9.5 | 22.9 | 67.6 | 2.58 | 0.66 |
| Walking/moving around by self | 7.6 | 23.8 | 68.6 | 2.61 | 0.63 |
| Living at home | 8.6 | 26.7 | 64.8 | 2.56 | 0.65 |
| 2. Enjoying life | 1.74 | 0.44 | |||
| Participating in hobbies | 17.1 | 41.0 | 41.9 | 2.25 | 0.73 |
| Participating in religious/spiritual life | 58.1 | 23.8 | 18.1 | 1.60 | 0.78 |
| Having physical/sexual intimacy | 76.2 | 10.5 | 13.3 | 1.37 | 0.71 |
| 3. Connecting | 2.44 | 0.47 | |||
| Having relationships with family and friends | 9.5 | 22.9 | 67.6 | 2.58 | 0.66 |
| Avoiding being a burden to others | 23.8 | 17.1 | 59.0 | 2.35 | 0.84 |
| Considering the needs/interests of family | 15.2 | 31.4 | 53.3 | 2.38 | 0.74 |
| 4. Managing health | |||||
| 4.1. Avoiding discomfort | 2.14 | 0.61 | |||
| Living without serious pain/discomfort | 21.0 | 26.7 | 52.4 | 2.31 | 0.80 |
| Having privacy | 36.2 | 31.4 | 32.4 | 1.96 | 0.83 |
| 4.2. Influence of religion/spirituality | 53.3 | 19.3 | 27.6 | 0.74 | 0.87 |
| 4.3. Quality vs. Length of life | 1.28 | 0.52 | |||
| Quality of life more important than how long I live | 3.8 | 28.6 | 67.6 | 1.64 | 0.56 |
| If very sick, do everything possible to prolong lifea | 32.4 | 26.7 | 41.0 | 1.09 | 0.86 |
| 4.4. Desired Input from Others When Making a Decision | 1.59 | 0.47 | |||
| From family | 12.4 | 30.5 | 57.1 | 1.45 | 0.71 |
| From the physician | 6.7 | 13.3 | 80.0 | 1.73 | 0.58 |
Note: Importance ratings are 1 = not at all/somewhat, 2 = very, 3 = extremely/of utmost except for Items 4.2 and 4.3 where 1 = not at all/a little, 2 = somewhat, 3 = mostly/completely and Item 4.4 where 1 = make decision myself, 2 = mostly myself, 3 = together.
Item reverse-scored before creating the mean score for this subdomain.
Qualitative
The approach to qualitative analysis was informed by the goal of the analysis, which was to determine the content validity of WMM-ST, specifically if open-ended responses on the Serious Illness Conversation Guide supported content on the WMM-ST. As a first step, interviews were administered and transcribed. Then, two members of the research team, the interviewer and a research investigator, met in weekly meetings to discuss procedural or clinical concerns and to review content for data saturation. The entire research team further reviewed content for data saturation at regular intervals during 2019 (April [N = 8], August [N = 22], October [N = 37], and December [N = 57]). At this point, the team agreed adequate data saturation for qualitative interviews was met, as new interviews were finding similar responses to what was previously expressed (Saunders et al., 2018). Thus, the interview was modified to reduce participant burden by eliminating open-ended questions. However, we retained the first open-ended question as a helpful introduction to the interview.
As the next step, we applied thematic analysis (Braun & Clarke, 2006) to responses to three questions determined by the research team to be most relevant to values in chronic illness: what are your most important goals if your health situation worsens (n = 94), what gives you strength as you think about the future with your illness (n = 42), and what abilities are so critical to your life that you cannot imagine living without them (n = 42)? Responses not coded included three not recorded due to instrument failure and others with no content (e.g., response was “none”).
Consistent with the concept of reflexivity in qualitative research (Finlay, 2002), we acknowledge the influence of the research team members on the qualitative process. The primary coding team consisted of an individual with a background in psychology and another individual with a background in chronic illness. A third team member with a background in geropsychology and health care values measurement joined for review of coding and discussion of themes.
We used a mixed deductive and inductive approach to create codes. First, we developed an initial codebook with code names, definitions, and examples using four domains from the WMM-ST (functioning, enjoying life, connecting, and managing health). Next, we coded participant responses using an inductive approach to assign emergent codes to phrases categorized within these domains.
Two team members (E. J. Auguste and J. C. Whitley) coded the same responses, meeting regularly to review codes and discuss discrepancies. We revised the codebook using an iterative process to reflect refinements in code names and definitions, adding newly generated codes as needed. The process continued throughout the complete data set, and data saturation was obtained with an initial 73% agreement adjusted to 100% intercoder agreement upon discussion. A third team member (J. Moye) reviewed the final coding considering ease of understanding and fit with the WMM-ST and Patient Priorities Care. Final code names and groupings were determined by group consensus.
Results
Participants
Participants were mostly male, White older adults as presented in Table 1. Almost half (40%) had a high school education or less. About 31% scored in the impaired range and 64% in the mildly impaired range for cognition on the T-MoCA-Short while 44% scored in the prefrail range and 44% in the frail range on the Frail Scale. On average participants reported having four illnesses on the Frail Scale (Supplementary Table A).
Table 1.
Patient Characteristics (N = 105)
| Variable | M | SD | N | % |
|---|---|---|---|---|
| Age (range: 65–93) | 75.46 | 6.30 | ||
| Religiosity (range: 0–2) | 1.01 | 0.74 | ||
| Social support (range: 0–4) | 3.05 | 1.01 | ||
| Cognition (range: 4–12) | 9.11 | 1.65 | ||
| Frailty (range: 0–5) | 2.32 | 1.42 | ||
| Gender | ||||
| Male | 101 | 96.2 | ||
| Female | 4 | 3.8 | ||
| Education | ||||
| Some high school or less | 21 | 20.0 | ||
| High or vocational school graduate | 21 | 20.0 | ||
| Some college | 28 | 26.7 | ||
| Graduated college | 22 | 21.0 | ||
| Some or completed graduate school | 13 | 12.4 | ||
| Race/ethnicity | ||||
| African American | 10 | 9.5 | ||
| Latinx | 1 | 1.0 | ||
| Asian | 0 | 0.0 | ||
| White | 93 | 88.6 | ||
| Other | 1 | 1.0 | ||
| Religious affiliation | ||||
| Jewish | 5 | 4.8 | ||
| Catholic | 58 | 55.2 | ||
| Protestant | 26 | 24.8 | ||
| Other | 3 | 2.9 | ||
| None | 13 | 12.4 |
Values Responses
Percent and mean endorsement for WMM-ST values items and subscales are given in Table 2. As a group, items related to independence in functioning were most highly rated in this sample. However, there was individual variability in what items were rated as of “utmost importance.” For example, most participants rated physical and sexual intimacy of the least importance based on the mean response, but 13% of the sample rated this extremely important or of utmost importance. Additionally, participants varied considerably as to whether religious or spiritual beliefs influence health care decisions with 53% stating not at all or a little, whereas 28% stated mostly or completely.
Association of Patient Characteristics With Values
Results of multivariate linear regressions examining the relationship of demographic and clinical characteristics with values on the WMM-ST are given in Table 3. Age and education were not associated with any specific values domain. Those with more social support prioritized values items in the Connecting domain as well as a desire for input from others; those with lower social support prioritized avoiding discomfort. Participants who described themselves as more religious or spiritual rated more highly that religious beliefs influence medical decisions and valuing a preference for length over the quality of life. These participants also had higher ratings in the Enjoying Life domain—likely related to the inclusion of an item about the importance of participating in religious/spiritual life in this domain. Those who were less frail were more likely to prioritize Functioning. Those who had higher cognition were more likely to prioritize Enjoying Life. Individuals who identified as Black, Latinx, or from other (non-White) racial/ethnic backgrounds were more likely than those who identified as White to say that religious beliefs influenced medical decisions (t = 2.16, p = .049).
Table 3.
Association of Demographic and Clinical Factors With What Matters Most–Structured Tool Values Domains in Multiple Regression
| Values domains and subscales |
|||||||
|---|---|---|---|---|---|---|---|
| Managing health |
|||||||
| Functioning | Enjoying life | Connecting | Avoiding discomfort | Influence of religion | Input from others | Quality vs. Length of life | |
|
|
|
||||||
| Variable | β | β | β | β | β | β | β |
| Age | 0.02 | 0.02 | 0.06 | −0.14 | 0.06 | −0.06 | −0.08 |
| Education | −0.13 | 0.03 | −0.02 | −0.15 | −0.17 | −0.19 | 0.08 |
| Social support | −0.08 | −0.06 | 0.30** | −0.22* | −0.17 | 0.26** | 0.09 |
| Religiosity | 0.03 | 0.21* | 0.32* | −0.03 | 0.45** | −0.08 | −0.22** |
| Cognition | 0.06 | 0.27** | 0.19 | −0.09 | 0.10 | 0.09 | 0.15 |
| Frailty | −0.30** | −0.03 | −0.03 | 0.01 | −0.05 | −0.13 | −0.12 |
| R 2 | 0.10 | 0.13 | 0.22 | 0.08 | 0.26 | 0.14 | 0.11 |
| F | 1.87 | 2.39* | 4.51** | 1.22 | 5.62** | 2.63* | 2.01 |
p < .05,
p < .01.
Validity
Acceptability
Participants rated the WMM-ST as somewhat more “easy to understand” than the Serious Illness Conversation Guide (“mostly” easy = 86.0% vs. 80.7%, χ2 = 26.66, p < .001) and as somewhat less likely to “apply to what I am going through now” (“mostly” applicable = 61.4% vs. 71.9%, χ2 = 29.18, p < .001). Participants also rated the WMM-ST questions as somewhat less likely to make them sad (“somewhat or mostly” = 36.9% vs. 42.1%, χ2 = 19.56, p = .001; see Supplementary Table B for all response frequencies). Completion of the WMM-ST portion of the interview averaged 9 min.
Educational bias
Those with more education provided longer responses on the Serious Illness Conversation Guide (r = 0.38, p = .007) and reported greater ease of understanding questions on it (r = 0.28, p = .034) than those with lower education. Level of education was not associated with ease of understanding the WMM-ST.
Content
Qualitative coding supported the validity of much of the WMM-ST content. See Supplementary Table C for codes and exemplar responses. Many open-ended responses were similar to the WMM-ST except in the Functioning domain, where participants also identified the importance of vision/senses and driving/travel. In the Enjoying Life domain, general content related to recreation (e.g., exercise, camping) was mentioned, but not content specific to having physical/sexual intimacy, which was an item on the WMM-ST. Responses relevant to spirituality and connecting to a higher power or faith emerged, but the coding team felt responses reflected a sense of connecting to a higher power rather than Enjoying Life where it appears on the WMM-ST. In response to the question “what gives you strength as you think about the future,” most participants (n = 13) mentioned content consistent with having input in treatment choices. A small number of individuals (n = 8) mentioned a positive personal attribute, for example, “I’m kinda a half-way intelligent individual and you know, I can participate in various protocols and things, so I think that will help me some. And I, you know, I’ve been a guy who can usually take care of himself.” While there was agreement on the code, the team debated which theme this code aligned with—functioning or connecting (in this case to oneself). We tentatively placed it under connecting. The placement of this code is further considered in the Discussion section.
In the Managing Health domain, participants reported content that aligned with the WMM-ST in the areas of quality versus length of life and a desire for control or input into treatment. In discussing control or input into treatment, participants not only mentioned how decisions were made but also having options for the type and location of treatment. Additional content included the value of a healthy lifestyle and the role of access and financial resources in making health decisions.
Discussion and Implications
Aligning health care with patient values is critical to the person-centered care of older adults with multiple chronic conditions (Institute for Healthcare Improvement, 2020; Molnar et al., 2017; Tinetti et al., 2017). In this study, we used a structured tool to assess what matters most in 105 older adults selected for multicomplexity with the goal of describing values, evaluating the association of patient characteristics with values, and examining the acceptability, educational bias, and content validity of the tool. We found that the WMM-ST was an acceptable tool which older adults were able to complete relatively quickly, including those with lower levels of education who were not as verbal in responding to open-ended questions. We also found that values ratings demonstrated interesting, albeit modest, associations with demographic and clinical factors in this relatively homogeneous sample. Qualitative analysis supported content validity and suggested additional items to extend content. In the next paragraphs, we discuss these findings considering challenges in values elicitation and measurement, along with limitations to this work, including important next steps in expanding this work to more diverse samples.
We aligned this tool with Patient Priorities Care, although the best ways to define core domains or constructs in assessing what matters most are not entirely clear. In our previous work, we found consistent evidence for the domains of Functioning, Enjoying Life, and Connecting—but the concept of Managing Health was less clear. These domains are similar to related efforts focusing on patients with chronic illness which identify four domains (functioning, reducing pain, reducing symptoms, and length of life; Fried et al., 2011) and six domains (relationships, abilities, activities, principles, emotions, and possessions; Lim et al., 2017). In the present study, personal attributes (similar to “principles” in the six-domain model) and resources (similar to “possessions” in the six-domain model) emerged as potential values items in qualitative coding. These chronic illness values domains share some features and are also different from values related to end-of-life care which may focus more on values underpinning important care preferences (e.g., resuscitation, hospital transfer).
The relatively homogeneous group of older adults interviewed in this study had both similarities and differences in prioritizing what matters most. Individuals varied in their level of social support, and not surprisingly those with high social support rated more highly values reflecting the importance of relationships and input from others. In contrast, some in our sample had low levels of social support and were more likely to endorse the importance of avoiding pain and having privacy—perhaps revealing a preference for stoicism and self-reliance when socially isolated. The degree to which individuals rated themselves as religious or spiritual varied widely, but when present, was a strong driver of health-related values such as considering religious views in making decisions, valuing length of life over quality of life, and valuing the ability to continue religious practices. Those who were less frail were more likely to prioritize the importance of Functioning—perhaps reflecting a desire to retain their level of function. Similarly, those who had higher cognition were more likely to prioritize Enjoying Life—perhaps reflecting their greater capacity to engage in a wider range of life activities and hobbies. Of interest, neither age nor education was associated with values ratings. In summary, associations with demographic and clinical factors were modest and intriguing and require more examination in diverse samples. At the same time, the differences in which items were rated as of “utmost importance” and the lack of specific associations with age or education underscores the importance of inquiring directly about values rather than assuming values based on demographic or clinical characteristics.
Qualitative findings supported the content validity of the WMM-ST and suggested additional items within domains, particularly for the Managing Health domain in which we identified the potential preferences related to a healthy lifestyle and the critical role of access to resources and financial considerations in health decision making. This domain in Patient Priorities Care is somewhat different than others—including considerations that may enter into health decisions like finances, preferences related to shared decision making, and overall preferences related to quality in contrast to the length of life. The Managing Health domain may have a role as a values concept but also as an instrumental bridge between values and goal setting. The content of this domain and its function in goal setting needs additional work.
Two codes under the domain of Connecting deserve ongoing consideration. The code “Spirituality” is one we placed here under Connecting (to a higher power) based on coder consensus. Its alignment under Connecting is consistent with prior work (Karel et al., 2016) that found the values item “to practice my religion or spiritual life (faith, prayer)” to load with other items related to “connecting” (e.g., to have relationships with family and friends) in factor analyses. However, it seems possible that religious practice may be an activity that creates a spiritual connection with a higher power for some and may also be a meaningful social activity for others. The code “Self/Personal Attributes” is one for which we debated its placement. For some in our coding group, responses seemed to align with a sense of connection to positive aspects of oneself (e.g., statements about the positive frame of mind); for others, the responses potentially aligned with Functioning (e.g., statements about intelligence and adaptation). These responses emerged from the question “what gives you strength as you think about the future” from the Serious Illness Conversation Guide, which while potentially important in helping persons navigate end-of-life illness may not be the best prompt for eliciting values related to current care planning. The nature and inclusion of this item need further study. In practice, it may be useful to ask older adults follow-up questions about what a prioritized value means within their own lives in their own words. A revised version of the WMM-ST formatted for potential use in future clinical trials is shown in Figure 2 including new content identified in this study. Tips for completing the tool are provided in Supplementary Table D.
Figure 2.
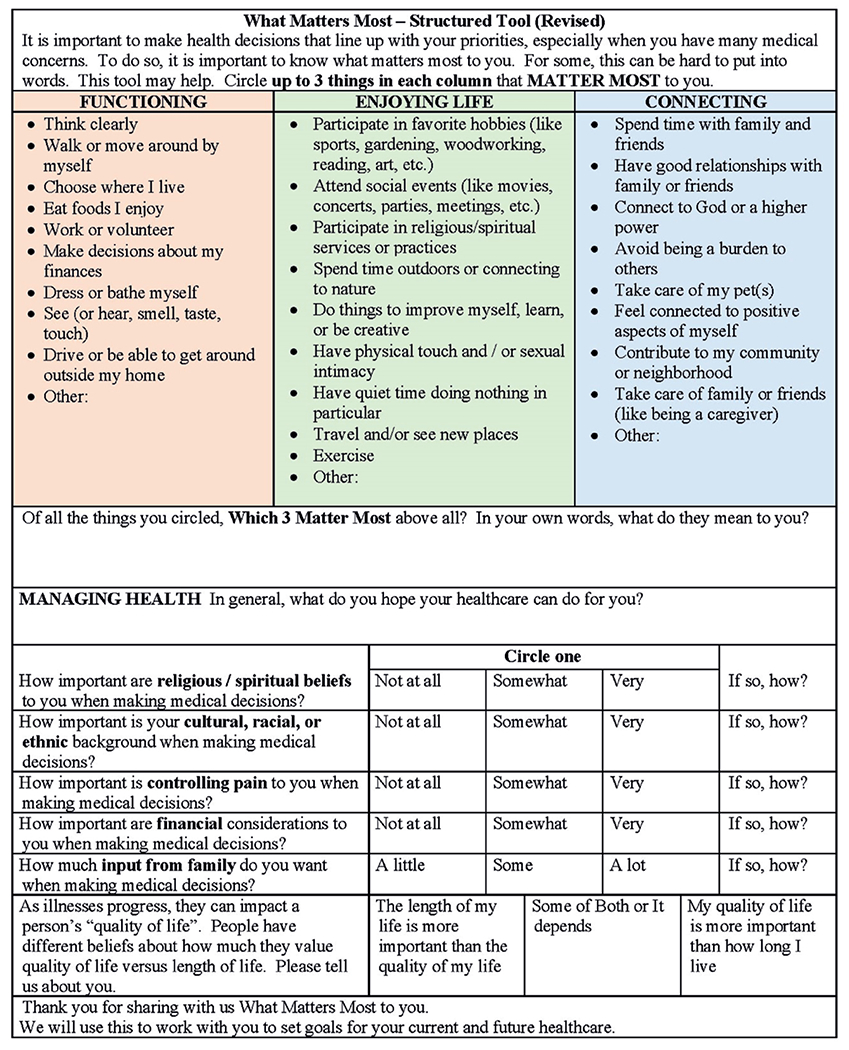
What Matters Most–Structured Tool (revised version).
Open-ended conversations can be helpful in eliciting values—and in this study, our participants rated open-ended questions as relevant and the conversations did reveal important content. However, open-ended questions were also seen as less understandable—and the overall length of response to the open-ended questions was associated with higher education. One impetus for our continued work in this area is to provide a useful tool for discerning what matters most—especially for patients who may have lower education, are more concrete, or have mild cognitive problems. A structured tool and response options may help. However, one of the challenges of having structure and response options is having enough options to be relevant to diverse values, but not so many options as to be overwhelming. Grouping response options as shown in Figure 2 may help—although some values may cross domains. Also challenging is determining the best route to encourage relative prioritization of values. In this study, we used Likert ratings with anchoring instructions for items across the three domains of Functioning, Enjoying Life, and Connecting. This approach was feasible. In Figure 2, we show the alternative approach of selecting three items within domains. Determining the best process to elicit prioritization still needs further exploration.
Limitations
There are many limitations to this study. This study was conducted within a U.S. Veterans Health Administration health care system, where older participants were mostly White and male, limiting generalizability. Examination of race and ethnicity suggested some important considerations, but the study was underpowered to fully consider the potential role of race and ethnicity as well as gender. Clearly, additional work is needed to determine the utility and validity of the tool in diverse samples—where qualitative interviews may be particularly valuable in eliciting how values manifest in diverse populations. Future studies should also determine the tool’s utility when used with individuals with diverse levels of cognitive function as measured by more comprehensive assessment measures than the cognitive screener employed in this study. Such studies could also incorporate assistance or comments from caregivers. We completed 105 face-to-face interviews prior to the onset of the coronavirus disease 2019 pandemic when the research was halted in our organization. While our analyses are adequately powered, we had initially anticipated completing more face-to-face interviews, which may have provided somewhat more diversity in our sample.
In addition, this interview tool appears acceptable and meaningful to the older adults we spoke with, although it was rated as somewhat less likely to apply to what they were currently going through than the Serious Illness Conversation Guide. We did not evaluate whether the tool could be employed in clinical care, which would be an important future direction of research. Furthermore, we evaluated validity by comparing two tools—one structured and one open-ended—a novel solution to employing the data structure at hand. Future studies might compare two structured tools to each other. Future qualitative studies should carefully assess content validity from the perspective of patients and content experts (Brod et al., 2009). Finally, we completed the tool via face-to-face interviews, which would require the availability of this resource in practice. It would be important to explore ways this interview tool might be deployed more efficiently (e.g., online format) or if it could be completed reliably by the patient alone as a precursor to a conversation with a clinician. Given the explosion of interest in the assessment of “what matters most” as Age-Friendly Health Care Systems proliferate, we hope that providing this tool in its present form may be useful to researchers interested in further evaluation and refinement of values elicitation tools.
Implications
Understanding what matters most to older patients with multicomplexity may facilitate person-centered care and goal setting. We describe a structured tool for eliciting such values which may be useful for older adults with lower levels of education and may help to make the abstract process of values discernment more concrete and achievable.
Supplementary Material
Acknowledgments
The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. The authors wish to acknowledge Drs. Michele Karel and Aanand Naik for their collaborative work with J. Moye to develop values assessment protocols which formed the basis for this work. We thank the veterans who completed the values interviews and allowed us to participate in their care.
Funding
This work was funded by the Rx Foundation. This material is the result of work supported with resources and the use of facilities at the VA Boston Healthcare System and Bedford VA Medical Center.
Footnotes
Supplementary Material
Supplementary data are available at The Gerontologist online.
Conflict of Interest
The authors have no financial or personal relationships to disclose.
References
- American Geriatrics Society Expert Panel on Person-Centered Care. (2016). Person-centered care: A definition and essential elements. Journal of the American Geriatrics Society, 64(1), 15–18. doi: 10.1111/jgs.13866 [DOI] [PubMed] [Google Scholar]
- American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. (2012). Guiding principles for the care of older adults with multimorbidity: An approach for clinicians: American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. Journal of the American Geriatrics Society, 60(10), e1–e25. doi: 10.1m/j.1532-5415.2012.04188.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labs Ariadne. (2015). Serious illness conversation guide. https://www.ariadnelabs.org/wp-content/uploads/sites/2/2017/05/SI-CG-2017-04-21_FINAL.pdf [Google Scholar]
- Bernacki RE, & Block SD; American College of Physicians High Value Care Task Force. (2014). Communication about serious illness care goals: A review and synthesis of best practices. JAMA Internal Medicine, 174(12), 1994–2003. doi: 10.1001/jamainternmed.2014.5271 [DOI] [PubMed] [Google Scholar]
- Bomba PA, Kemp M, & Black JS (2012). POLST: An improvement over traditional advance directives. Cleveland Clinic Journal of Medicine, 79(7), 457–464. doi: 10.3949/ccjm.79a.11098 [DOI] [PubMed] [Google Scholar]
- Boyd C, Smith CD, Masoudi FA, Blaum CS, Dodson JA, Green AR, Kelley A, Matlock D, Ouellet J, Rich MW, Schoenborn NL, & Tinetti ME (2019). Decision making for older adults with multiple chronic conditions: Executive summary for the American Geriatrics Society Guiding Principles on the Care of Older Adults With Multimorbidity. Journal of the American Geriatrics Society, 67(4), 665–673. doi: 10.1111/jgs.15809 [DOI] [PubMed] [Google Scholar]
- Braun V, & Clarke V (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Brod M, Tesler LE, & Christensen TL (2009). Qualitative research and content validity: Developing best practices based on science and experience. Quality of Life Research, 18(9), 1263–1278. doi: 10.1007/s11136-009-9540-9 [DOI] [PubMed] [Google Scholar]
- Butler M, Ratner E, McCreedy E, Shippee N, & Kane RL (2014). Decision aids for advance care planning: An overview of the state of the science. Annals of Internal Medicine, 161(6), 408–418. doi: 10.7326/M14-0644 [DOI] [PubMed] [Google Scholar]
- Corbett TK, Cummings A, Lee K, Calman L, Fenerty V, Farrington N, Lewis L, Young A, Boddington H, Wiseman T, Richardson A, Foster C, & Bridges J (2020). Planning and optimising CHAT&PLAN: A conversation-based intervention to promote person-centred care for older people living with multimorbidity. PLoS One, 15(10), e0240516. doi: 10.1371/journal.pone.0240516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagerlin A, Pignone M, Abhyankar P, Col N, Feldman-Stewart D, Gavaruzzi T, Kryworuchko J, Levin CA, Pieterse AH, Reyna V, Stiggelbout A, Scherer LD, Wills C, & Witteman HO (2013). Clarifying values: An updated review. BMC Medical Informatics and Decision Making, 13(Suppl. 2), S8. doi: 10.1186/1472-6947-13-s2-s8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feder SL, Kiwak E, Costello D, Dindo L, Hernandez-Bigos K, Vo L, Geda M, Blaum C, Tinetti ME, & Naik AD (2019). Perspectives of patients in identifying their values-based health priorities. Journal of the American Geriatrics Society, 67(7), 1379–1385. doi: 10.1111/jgs.15850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay L (2002). “Outing” the researcher: The provenance, process, and practice of reflexivity. Qualitative Health Research, 12(4), 531–545. doi: 10.1177/104973202129120052 [DOI] [PubMed] [Google Scholar]
- Fleary SA, & Ettienne R (2019). Social disparities in health literacy in the United States. Health Literacy Research and Practice, 3(1), e47–e52. doi: 10.3928/24748307-20190131-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried TR, Tinetti ME, Iannone L, O’Leary JR, Towle V, & Van Ness PH (2011). Health outcome prioritization as a tool for decision making among older persons with multiple chronic conditions. Archives of Internal Medicine, 171(20), 1854–1856. doi: 10.1001/archinternmed.2011.424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute for Healthcare Improvement. (2020). Age-friendly health systems: Guide to using the 4Ms in the care of older adults. http://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Documents/IHIAgeFriendlyHealthSystems_GuidetoUsing4MsCare.pdf [Google Scholar]
- Karel MJ, Moye J, Bank A, & Azar AR (2007). Three methods of assessing values for advance care planning. Journal of Aging & Health, 19(1), 123–151. doi: 10.1177/0898264306296394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karel MJ, Moye J, & Oville A (1996, November). The assessment of values in medical decision making. Gerontological Society of America Annual Meeting, Washington, DC. [Google Scholar]
- Karel MJ, Mulligan EA, Walder A, Martin LA, Moye J, & Naik AD (2016). Valued life abilities among veteran cancer survivors. Health Expectations, 19(3), 679–690. doi: 10.1111/hex.12343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivelitz L, Schäfer J, Kanat M, Mohr J, Glattacker M, Voigt-Radloff S, & Dirmaier J (2021). Patient-centeredness in older adults with multimorbidity: Results of an online expert Delphi study. Gerontologist. Advance online publication. doi: 10.1093/geront/gnaa223 [DOI] [PubMed] [Google Scholar]
- Lim CY, Berry ABL, Hirsch T, Hartzler AL, Wagner EH, Ludman EJ, & Ralston JD (2017). Understanding what is most important to individuals with multiple chronic conditions: A qualitative study of patients’ perspectives. Journal of General Internal Medicine, 32(12), 1278–1284. doi: 10.1007/s11606-017-4154-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGilton KS, Vellani S, Yeung L, Chishtie J, Commisso E, Ploeg J, Andrew MK, Ayala AP, Gray M, Morgan D, Chow AF, Parrott E, Stephens D, Hale L, Keatings M, Walker J, Wodchis WP, Dubé V, McElhaney J, … Puts M (2018). Identifying and understanding the health and social care needs of older adults with multiple chronic conditions and their caregivers: A scoping review. BMC Geriatrics, 18(1), 231. doi: 10.1186/s12877-018-0925-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molnar F, Huang A, & Tinetti M (2017). Update: The public launch of the geriatric 5Ms. http://canadiangeriatrics.ca/wp-content/uploads/2017/04/update-the-public-launch-of-the-geriatric-5ms.pdf [Google Scholar]
- Morley JE, Malmstrom TK, & Miller DK (2012). A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. The Journal of Nutrition, Health & Aging, 16(7), 601–608. doi: 10.1007/s12603-012-0084-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moye J, Karel MJ, Edelstein B, Hicken B, Armesto JC, & Gurrera RJ (2007). Assessment of capacity to consent to treatment: Challenges, the “ACCT” approach, future directions. Clinical Gerontologist, 31(3), 37–66.doi: 10.1080/07317110802072140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naik AD, Dindo LN, Van Liew JR, Hundt NE, Vo L, Hernandez-Bigos K, Esterson J, Geda M, Rosen J, Blaum CS, & Tinetti ME (2018). Development of a clinically feasible process for identifying individual health priorities. Journal of the American Geriatrics Society, 66(10), 1872–1879. doi: 10.1111/jgs.15437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naik AD, Martin LA, Moye J, & Karel MJ (2016). Health values and treatment goals of older, multimorbid adults facing life-threatening illness. Journal of the American Geriatrics Society, 64(3), 625–631. doi: 10.1111/jgs.14027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paladino J, Koritsanszky L, Nisotel L, Neville BA, Miller K, Sanders J, Benjamin E, Fromme E, Block S, & Bernacki R (2020). Patient and clinician experience of a serious illness conversation guide in oncology: A descriptive analysis. Cancer Medicine, 9(13), 4550–4560. doi: 10.1002/cam4.3102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pendlebury ST, Welch SJ, Cuthbertson FC, Mariz J, Mehta Z, & Rothwell PM (2013). Telephone assessment of cognition after transient ischemic attack and stroke: Modified telephone interview of cognitive status and telephone Montreal Cognitive Assessment versus face-to-face Montreal Cognitive Assessment and neuropsychological battery. Stroke, 44(1), 227–229. doi: 10.1161/STROKEAHA.112.673384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, Burroughs H, & Jinks C (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & Quantity, 52(4), 1893–1907. doi: 10.1007/s11135-017-0574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne CD, & Stewart AL (1991). The MOS social support survey. Social Science & Medicine (1982), 32(6), 705–714. doi: 10.1016/0277-9536(91)90150-b [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Esterson J, Ferris R, Posner P, & Blaum CS (2016). Patient priority-directed decision making and care for older adults with multiple chronic conditions. Clinics in Geriatric Medicine, 32(2), 261–275. doi: 10.1016/j.cger.2016.01.012 [DOI] [PubMed] [Google Scholar]
- Tinetti M, Huang A, & Molnar F (2017). The geriatrics 5M’s: A new way of communicating what we do. Journal of the American Geriatrics Society, 65(9), 2115. doi: 10.1111/jgs.14979 [DOI] [PubMed] [Google Scholar]
- Tinetti M, Naik A, & Dindo L (2018). Conversation guide for patients and caregivers for identifying their health priorities. https://patientprioritiescare.org/wp-content/uploads/2018/11/Conversation-Guide-for-Patients-and-Caregivers-for-Identifying-their-Health-Priorities.pdf [Google Scholar]
- Van Haitsma K, Abbott KM, Arbogast A, Bangerter LR, Heid AR, Behrens LL, & Madrigal C (2020). A preference-based model of care: An integrative theoretical model of the role of preferences in person-centered care. The Gerontologist, 60(3), 376–384. doi: 10.1093/geront/gnz075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Porter B, Maynard C, Evans G, Bryson C, Sun H, Gupta I, Lowy E, McDonell M, Frisbee K, Nielson C, Kirkland F, & Fihn SD (2013). Predicting risk of hospitalization or death among patients receiving primary care in the Veterans Health Administration. Medical Care, 51(4), 368–373.doi: 10.1097/MLR.0b013e31827da95a [DOI] [PubMed] [Google Scholar]
- Witteman HO, Scherer LD, Gavaruzzi T, Pieterse AH, Fuhrel-Forbis A, Chipenda Dansokho S, Exe N, Kahn VC, Feldman-Stewart D, Col NF, Turgeon AF, & Fagerlin A (2016). Design features of explicit values clarification methods:A systematic review. Medical Decision Making, 36(4), 453–471. doi: 10.1177/0272989X15626397 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


