Abstract
Background
Chronic cough is a debilitating medical condition that is often complicated by psychomorbidities such as depressive symptoms. Nevertheless, little is known about the impact of chronic cough on the risk of developing depression. Therefore, we investigated the association between chronic cough and prevalent, incident and recurrent depression in a population-based sample of middle-aged and older persons.
Methods
Within the Rotterdam Study, a population-based cohort, we defined chronic cough as reporting daily coughing for ⩾3 months. Depression was assessed using the Center for Epidemiologic Studies Depression scale, clinical interviews and medical records. Associations between chronic cough and depression were determined with linear, logistic and Cox regression analyses.
Results
The study included 5877 participants (mean±sd age 72±8 years, 59% female) who contributed 37 287 person-years of follow-up. At baseline, participants with chronic cough reported more depressive symptoms (adjusted standardised mean difference 0.15, 95% CI 0.07–0.22) compared to those without chronic cough. Over time, chronic cough was associated with an increased risk of depression in participants with a history of depression (hazard ratio (HR) 1.45, 95% CI 1.13–1.84), but not in those without a history of depression (HR 0.91, 95% CI 0.68–1.22).
Conclusions
Adults with chronic cough have a disproportionate burden of depressive symptoms and an increased risk of recurrent depression. This highlights the importance of screening for depression in patients with chronic cough.
Short abstract
Adults with chronic cough have a disproportionate burden of depressive symptoms and are more likely to suffer recurrent depression, highlighting the need for screening for depression in individuals with chronic cough https://bit.ly/3sPvYTd
Introduction
Chronic cough, defined as a cough lasting ⩾8 weeks, is a common medical condition affecting ∼1–12% of the general adult population [1, 2]. It is debilitating, often complicating associated clinical disorders such as asthma and COPD, and necessitating visits to primary care and referral to specialist clinics [3–7].
Individuals with chronic cough frequently experience physical and psychosocial conditions including social isolation, physical exhaustion, sleep complaints, stress incontinence, cough syncope and a lower quality of life [8–13]. In addition, mental health complaints including depressive symptoms and major depressive disorder are common in people with chronic cough [5, 9, 13–15]. Depression contributes to the overall clinical burden of the diseases commonly underlying chronic cough [13, 16]. Potentially, chronic cough may even have a negative impact on the risk of developing depression [17, 18]. The complex nature of risk factors for depression is such that the vulnerability for onset and recurrent depressive events differs with regard to triggers [18]. Some of these factors, such as low socioeconomic status and reduced work ability, are also more prevalent in patients with chronic cough [19, 20].
Previous studies have highlighted the link between chronic cough and depression [17]. Clinical studies have shown that treatment of chronic cough decreases depressive symptoms in patients with chronic cough [9, 13], which may suggest that chronic cough could be a causal factor for developing depressive symptoms. For example, French et al. [9] studied the impact of cough treatment on depressive symptoms in 55 women with a 7-year mean cough duration and reported a significant reduction in depressive symptoms after 3 and 6 months of treating chronic cough. Similarly, Dicpinigaitis et al. [13] followed 81 chronic cough patients for 3 months and found that cough treatment significantly reduced both cough severity and depressive symptom scores.
So far, most studies on chronic cough and depression have involved patients referred to specialist cough clinics, whose clinical profiles may differ from that of the general population [9, 13, 16]. Furthermore, the evidence on the burden of depression in chronic cough in population-based samples has come mainly from cross-sectional studies and has provided little insight into the temporal association between chronic cough and depression [5, 15].
We conducted a population-based observational cohort study in middle-aged and older adults to investigate the association between chronic cough and prospectively assessed depressive symptoms and disorders over time.
Methods
Study design and study population
The Rotterdam Study is a prospective population-based cohort study on the epidemiology of chronic diseases among 14 926 middle-aged and older adults (aged ≥45 years) living in the well-defined Ommoord district, a suburb of the city of Rotterdam, the Netherlands [21]. The Rotterdam Study data are acquired through home interviews and clinical examinations at the research centre every 3–6 years, and from medical records of general practitioners (GPs), hospitals, pharmacies and nursing homes.
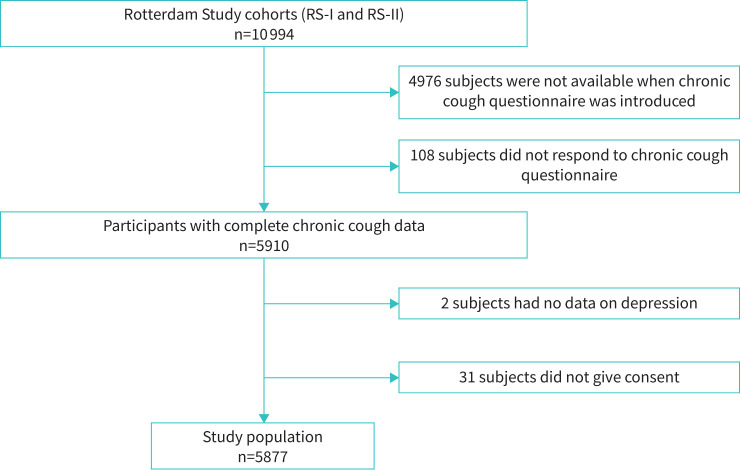
Within this study, we included participants who had chronic cough data collected during the home interview between January 2002 and December 2005, and had cross-sectional data on depressive symptoms from the home interview and/or data on incident depressive events via the follow-up of medical records up until February 2012 (figure 1).
FIGURE 1.
Strengthening the Reporting of Observational studies in Epidemiology study flow chart (Rotterdam Study (RS)-I and RS-II).
The medical ethics committee of the Erasmus Medical Centre (registration number MEC 02.1015) and the Dutch Ministry of Health, Welfare and Sport (Population Screening Act WBO, licence number 1071272–159521-PG) approved the Rotterdam Study. The Rotterdam Study has been registered with the Netherlands National Trial Register (www.trialregister.nl) and the WHO International Clinical Trials Registry Platform (ICTRP; https://trialsearch.who.int/) under the joint catalogue number NTR6831. All participants provided written informed consent to participate in the study and to have their information obtained from treating physicians [21].
Chronic cough
Chronic cough was assessed using the question “In the last 2 years, did you cough almost every day for three consecutive months or more?” [22]. Chronic cough was defined as daily coughing lasting for ⩾3 months, in line with most epidemiological studies [1].
Depression
Depression was assessed in three ways. First, during the home interviews, depressive symptoms were assessed with the Dutch version of the Center for Epidemiologic Studies Depression (CES-D) scale. The CES-D scale ranges from 0 through 60 and assesses the burden of self-reported depressive symptoms with higher scores denoting more severe symptoms [23, 24]. A score of ≥16 was defined as clinically relevant depressive symptoms. This measure of depression was used in our cross-sectional analyses. Second, if participants had a score of ≥16, they were invited for a semi-structured interview by a trained professional using the Dutch version of the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) [25] to identify depressive disorders. Based on these interviews, participants were diagnosed as having no depression, depressive symptoms, a depressive syndrome (i.e. mild depressive disorder or dysthymia) or major depressive disorder according to the Statistical Manual of Mental Disorders, 4th revised edition (DSM-IV-TR) criteria [26]. Third, we used medical records, including data from GPs' notes, specialist reports and hospital discharge letters, to assess depression in between examination rounds, coding both depressive symptoms and diagnoses of depressive disorders. Participants were categorised as having a history of depression if they experienced a depressive event over 5 years prior to or at baseline.
For our longitudinal analyses, we combined data of the CES-D and SCAN across multiple research rounds and medical records to indicate any incident event of depression, including depressive symptoms, depressive syndrome and major depressive disorder. Within this project we focused on the first occurring event. Participants were continuously followed from baseline (2002–2005) until the occurrence of the first event of depressive condition, death or the end of study (February 2012), whichever came first.
Other variables
Other variables relevant to the association of chronic cough with depression were assessed at baseline including participants’ age and sex. Body mass index (BMI) was calculated as the ratio of weight in kilograms to height in squared metres, as measured with calibrated scales. Smoking was assessed in the interview and divided into three categories: never-, past and current smoking. Asthma was physician-diagnosed, and COPD cases were validated using spirometry data and medical records. The diagnoses of asthma and/or COPD at baseline were grouped as obstructive airway disease. Cases of lung cancer were ascertained with the Dutch Cancer Registry and diabetes cases validated using laboratory and medical records. Heart failure was defined using the European Society of Cardiology criteria [27]. Pharmacy data were used to determine the use of angiotensin converting enzyme (ACE) inhibitors (Anatomical Therapeutic Chemical (ATC) code C09A, C09B). Gastro-oesophageal reflux disease (GORD) and chronic rhinosinusitis were defined with pharmacy data as a proxy. In particular, participants who received more than two prescriptions of medications for acid-related disorders such as peptic ulcer or reflux disease (ATC A02B) were considered to have GORD. Chronic rhinosinusitis was also defined as having received at least three prescriptions of nasal steroids (ATC R01AD) within 1 year before baseline.
Statistical analysis
Baseline characteristics were presented with descriptive statistics, and compared between participants according to prevalent chronic cough status. Normally distributed variables were presented as means with standard deviations and compared using independent t-tests. Mann–Whitney tests were performed for skewed continuous variables and their median and interquartile range were reported. Categorical data were compared using Chi-squared tests.
We performed active imputation of 874 (14.9%) missing BMI data using fully conditional specification (10 imputed datasets). Prior to performing linear regression analyses, the CES-D scores were square-root normalised and standardised to unit variance using the z-transformation. To assess the cross-sectional association of chronic cough with depressive symptoms (CES-D) at baseline, we performed a linear regression which was adjusted for age and sex (model 1), and additionally for BMI, smoking, chronic rhinosinusitis, GORD, obstructive airway disease, lung cancer, diabetes and heart failure (model 2). Analyses were repeated after stratification for prevalent respiratory conditions (chronic rhinosinusitis, obstructive airway disease and lung cancer). Next, we studied the association between chronic cough and clinically relevant depressive symptoms at baseline using logistic regression in the sex-age adjusted model (model 1) and the confounder adjusted model (model 2).
The longitudinal association between chronic cough and incident depression (including depressive symptoms, depressive syndrome and major depressive disorder to maximise power) was estimated using Cox regression and adjusted for age and sex (model 1), and additionally for model 2 plus history of depressive events (model 2a) in all eligible participants. The analyses were repeated and stratified for history of depression in the past 5 years based on the incident data (yes/no), since history of depression might confound the risk of recurrent depression. We additionally adjusted for baseline CES-D scores (model 3) in the stratified analysis.
All statistical analyses were performed using SPSS statistical software version 24 (IBM SPSS Statistics for Windows; IBM, Armonk, NY, USA). Statistical significance was set at a p-value of <0.05.
Results
Baseline characteristics
5877 participants were included in this study (table 1). Participants were mainly female (n=3460, 58.9%) and predominantly elderly (mean±sd age 72.3±7.9 years); 13.9% (n=818) were current smokers, and 23.5% (n=1381) used ACE inhibitors. At baseline, 32.1% (n=1884) of the participants had at least one comorbidity. Within the sample, the prevalences of comorbidities were as follows 14.4% (n=848) for asthma and/or COPD, 14.5% (n=850) for GORD, 0.3% (n=20) for lung cancer, 2.6% (n=152) for chronic rhinosinusitis, 2.6% (n=153) for diabetes and 5.7% (n=336) for heart failure. Nearly 13% (n=755) of the participants reported clinically relevant depressive symptoms, whereas 21.9% (n=1285) had previously suffered from depression.
TABLE 1.
Baseline characteristics of the study population
| Total | No chronic cough | Chronic cough | p-value | |
| Participants | 5877 | 5148 | 729 | |
| Age, years | 72.3±7.9 | 72.2±7.9 | 72.7±7.7 | 0.081 |
| Female | 3460 (58.9) | 3031 (58.9) | 429 (58.8) | 0.988 |
| BMI, kg·m−2 | 27.6±4.1 | 27.6±4.0 | 27.6±4.4 | 0.645 |
| Smoking | ||||
| Never | 1876 (31.9) | 1693 (32.9) | 183 (25.1) | <0.001 |
| Past | 3180 (54.1) | 2818 (54.8) | 362 (49.7) | |
| Current | 818 (13.9) | 634 (12.3) | 184 (25.2) | |
| ACE inhibitor use | 1381 (23.5) | 1153 (22.4) | 228 (31.3) | <0.001 |
| CES-D scores | 4 (1–10) | 4 (1–9) | 6 (2–12) | <0.001 |
| CES-D score ≥16 | 755 (12.9) | 636 (12.4) | 119 (16.4) | 0.002 |
| History of depressive events | 1285 (21.9) | 1095 (21.3) | 190 (26.1) | 0.003 |
| Baseline comorbidities | 1884 (32.1) | 1506 (29.3) | 378 (51.9) | <0.001 |
| Chronic rhinosinusitis | 152 (2.6) | 120 (2.3) | 32 (4.4) | 0.001 |
| GORD | 850 (14.5) | 716 (13.9) | 134 (18.4) | 0.001 |
| Obstructive airway disease# | 848 (14.4) | 595 (11.6) | 253 (34.7) | <0.001 |
| Lung cancer | 20 (0.3) | 11 (0.2) | 9 (1.2) | <0.001 |
| Diabetes | 153 (2.6) | 133 (2.6) | 20 (2.7) | 0.800 |
| Heart failure | 336 (5.7) | 273 (5.3) | 63 (8.6) | <0.001 |
Data are presented as n, mean±sd, n (%) or median (interquartile range), unless otherwise stated. BMI: body mass index; ACE: angiotensin-converting enzyme; CES-D: Center for Epidemiological Studies Depression scale; GORD: gastro-oesophageal reflux disease. #: COPD and/or asthma.
Approximately 12% of the participants had chronic cough at baseline (n=729). Compared to participants without chronic cough (n=5148), those with chronic cough were more often current smokers (25.2% versus 12.3%, p<0.001), and had more comorbidities (51.9% versus 29.3%, p<0.001) such as chronic rhinosinusitis (4.4% versus 2.3%, p=0.001), GORD (18.4% versus 13.9%, p=0.001), obstructive airway disease (34.7% versus 11.6%, p<0.001), lung cancer (1.2% versus 0.2%, p<0.001) and heart failure (8.6% versus 5.3%, p<0.001).
Chronic cough and baseline depressive symptoms
Participants with chronic cough reported a 0.25-sd higher depressive symptoms score than those without chronic cough after adjusting for age and sex (adjusted standardised mean difference 0.25, 95% CI 0.18–0.33). The association remained significant after further adjustment for BMI, smoking, chronic rhinosinusitis, GORD, obstructive airway disease, lung cancer, diabetes and heart failure (adjusted standardised mean difference 0.15, 95% CI 0.08–0.22) (table 2). This suggests that persons with CES-D scores of 4, 17 and 40 would have 1, 2 and 3 points higher CES-D scores, respectively, if they had chronic cough, independent of any related medical conditions. Stratified analyses demonstrated that chronic cough was associated with more depressive symptoms in participants without respiratory disease (adjusted standardised mean difference 0.19, 95% CI 0.10–0.28), but not in those with respiratory disease (adjusted standardised mean difference 0.06, 95% CI −0.08–0.19) (supplementary table S1). Persons with CES-D scores of 3, 11 and 24 would have 1, 2 and 3 points higher CES-D scores, respectively, if they had chronic cough not explained by a respiratory disease.
TABLE 2.
The cross-sectional association between chronic cough and depressive symptoms at baseline (n=5852)#
| Participants n | CES-D scores¶ median (IQR) | Model 1 standardised mean adjusted difference (95% CI) in depressive symptoms at baseline + | Model 2 standardised mean adjusted difference (95% CI) in depressive symptoms at baseline § |
CES-D score ≥16
(n=755, 12.9%) |
Model 1
OR (95% CI) |
Model 2
OR (95% CI) |
|
| No chronic cough | 5128 | 4 (1–9) | Ref. | Ref. | 636 (12.4%) | Ref. | Ref. |
| Chronic cough | 724 | 6 (2–12) | 0.25 (0.18–0.33) | 0.15 (0.08–0.22) | 119 (16.4%) | 1.39 (1.12–1.73) | 1.12 (0.89–1.41) |
CES-D: Center for Epidemiological Studies Depression scale; IQR: interquartile range. #: 25 participants did not have CES-D score data; ¶: scores were square root-transformed and z-standardised; +: adjusted for age and sex; §: adjusted for age, sex, body mass index, smoking, chronic rhinosinusitis, gastro-oesophageal reflux disease, obstructive airway disease, lung cancer, diabetes and heart failure.
Chronic cough was significantly associated with more clinically relevant depressive symptoms after adjusting for age and sex (OR 1.39, 95% CI 1.12–1.73), but the effect size decreased after further adjustment for BMI, smoking, chronic rhinosinusitis, GORD, obstructive airway disease, lung cancer, diabetes and heart failure (OR 1.12, 95% CI 0.89–1.41) (table 2). Stratified analyses showed that chronic cough was associated with more clinically relevant depressive symptoms in participants who did not have respiratory disease (OR 1.35, 95% CI 1.02–1.77), but not in those with respiratory disease (OR 0.78, 95% CI 0.52–1.17) (supplementary table S2).
Chronic cough and risk of developing depression
Over a total observation period of 37 287 person-years, 900 out of 5799 participants (with complete follow-up data) developed depressive symptoms (n=670), a depressive syndrome (n=112) or a major depressive disorder (n=118). Chronic cough was significantly associated with an increased risk of any event of depression after adjustment for confounders (hazard ratio (HR) 1.22, 95% CI 1.01–1.46) (table 3).
TABLE 3.
The longitudinal association between chronic cough and incident/recurrent depression#
| Participants¶ | Incident depression¶ | Recurrent depression¶ | Model 1+ | Model 2§ | Model 2aƒ | Model 3## | |
| All eligible participants regardless of history of depression | 5799 | 900 | |||||
| No chronic cough | 5080 | 758 | Ref. | Ref. | Ref. | ||
| Chronic cough | 719 | 142 | 1.40 (1.17–1.68) | 1.22 (1.01–1.46) | 1.22 (1.01–1.46) | ||
| Participants without a history of depression | 4516 | 466 | |||||
| No chronic cough | 3987 | 408 | Ref. | Ref. | Ref. | ||
| Chronic cough | 529 | 58 | 1.11 (0.84–1.46) | 0.96 (0.73–1.28) | 0.91 (0.68–1.22) | ||
| Participants with a history of depression | 1283 | 434 | |||||
| No chronic cough | 1093 | 350 | Ref. | Ref. | Ref. | ||
| Chronic cough | 109 | 84 | 1.53 (1.21–1.95) | 1.46 (1.14–1.86) | 1.45 (1.13–1.84) |
Data are presented as n or hazard ratio (95% CI). #: includes any event of depressive symptoms, depressive syndromes and major depressive disorder; ¶: 78 participants had no follow-up data on incident/recurrent depression; +: adjusted for age and sex; §: adjusted for age, sex, body mass index (BMI), smoking, chronic rhinosinusitis, gastro-oesophageal reflux disease (GORD), obstructive airway disease, diabetes and heart failure; ƒ: adjusted for age, sex, BMI, smoking, chronic rhinosinusitis, GORD, obstructive airway disease, diabetes, heart failure and history of depressive event; ##: adjusted for age, sex, BMI, smoking, chronic rhinosinusitis, GORD, obstructive airway disease, diabetes, heart failure and baseline depressive symptoms (Center for Epidemiological Studies Depression scores).
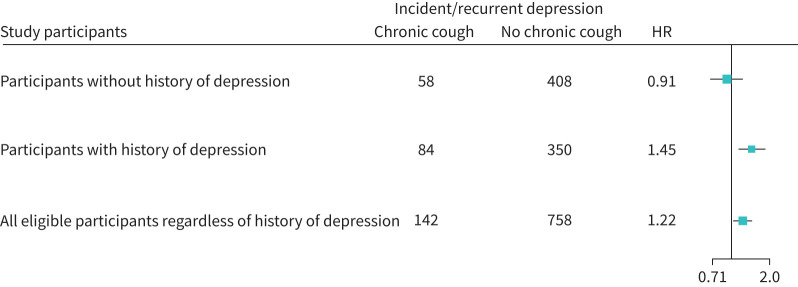
However, stratification for a history of depression demonstrated that chronic cough was only associated with an increased risk of recurrent depression in participants with a history of depression (HR 1.45, 95% CI 1.13–1.84) (table 3). In contrast, chronic cough was not associated with an increased risk of depression in participants without history of depression at baseline (adjusted HR 0.91, 95% CI 0.68–1.22) (table 3, figure 2).
FIGURE 2.
Summary of risk of incident/recurrent depression among study participants. HR: hazard ratio.
Discussion
In this prospective population-based study of middle-aged and older persons, we observed that chronic cough was cross-sectionally associated with more depressive symptoms. Moreover, chronic cough increased the risk of depressive events in persons with a history of depression, but not in persons without a history of depression.
Our findings corroborate previous studies indicating that persons with chronic cough have a substantially higher burden of depressive symptoms [9, 13], independent of commonly associated risk factors and comorbidities such as smoking and asthma [5, 15, 16]. In our study, chronic cough was also associated with higher burden of depressive symptoms after adjusting for pre-existing respiratory diseases including chronic rhinosinusitis, asthma, COPD and lung cancer, albeit with smaller effect sizes. This is line with previous research; for example, Heo et al. [15] found that, compared to persons without chronic cough, patients with chronic cough had more severe depressed mood regardless of their smoking and lung function status.
Our stratified analyses showed that chronic cough is associated with depressive symptoms, particularly in persons whose chronic cough is not explained by a known respiratory disease. Although this might be explained in part by more power in the analyses including those with chronic cough not explained by respiratory disease, we also see substantially larger effect sizes for the association of chronic cough not explained by a known respiratory disease and depression. This is consistent with the findings of Hulme et al. [16], who examined the psychological profiles of patients presenting with chronic cough and observed that individuals without a pulmonary disease had significantly more depressive symptoms than those with explainable causes of chronic cough as well as those without cough. Chronic cough is refractory in ∼50% of patients with treatable traits for cough [28] and remains unexplained in ∼40% of affected persons [29]. We might speculate that some patients may suffer psychological distress due to suboptimal response to cough treatment and lack of definitive diagnosis despite several health visits for cough.
Chronic cough also increased the risk of depression in our study participants, but only in those with a history of depression. Studies have shown that recurrent episodes of depressive disorders have a predilection for clinico-demographic factors relevant in chronic cough [18], and the overall disease burden of chronic cough negatively impacts the risk of depression [8, 10, 12, 14, 30]. Although we were unable to assess any bidirectional effects in this study, we hypothesise that, while depression is more common in chronic cough, it is usually mild rather than severe, and that chronic cough might only lead to depression in those who are already more vulnerable to depression or exacerbate existing depressive symptoms.
A plausible explanation for chronic cough as a risk factor for depression could be neurobiological; for example, patients with cough hypersensitivity show increased neural activity in the periaqueductal gray [31, 32], a region involved in emotional processing of stress and pain, and also implicated in chronic depression [32, 33]. Furthermore, the psychological determinants of chronic cough [17] and its associated negative social effects [34] highlight the potential concerted role of psychosocial factors on depressive events in chronic cough patients. In particular, cough-related psychosocial problems, such as altered social identity, social embarrassment and isolation, preoccupation and attentional focus and obsessive and unsuccessful attempts to suppress cough [34, 35] have a negative impact on depression [16]. Indeed, these psychosocial factors may play a role in mediating the pathological link between chronic cough and depression. Another potential connection between chronic cough and depression is impaired modulation of excitatory and inhibitory neurotransmission in the brain [31, 36]. Indeed, centrally acting neuromodulators such as gabapentin and opioids are effective therapeutic options in both conditions [2, 37, 38]. Notably, during cough therapy, there is a concurrent reduction in cough intensity and depressive symptoms [9, 13]. Therefore, recognising and treating both conditions may improve the overall clinical management outcomes and patient satisfaction.
Our study has several strengths. The results were based on a large sample from the general population, and the prospective longitudinal assessment of depressive events was based on a combination of questionnaires, clinical interviews and medical records. However, some limitations need to be considered. First, we lacked the power to further explore the impact of chronic cough on specific incident depressive events. Second, although we have information on history of depression up to 5 years before the baseline assessment, these participants might have suffered from depression before this period. Third, recurrent bouts of depression are not unusual in people with a history of depression, and they may be more easily recognised by a general practitioner who is often seen for a complaint of chronic cough. Fourth, our population-based study included older adults and elderly participants, whose clinical profiles may differ from those of patients presenting to healthcare facilities. Consequently, our findings may not be generalisable to hospital-based cohorts. Fifth, chronic pain might be a major confounding factor in the chronic cough–depression link [39]. However, because we did not have chronic pain data during this study period in the Rotterdam Study, we could not adjust for it in our analyses. Sixth, the overlapping symptoms of chronic cough and depression may have artificially inflated the CES-D score. Furthermore, we acknowledge the potential confounding effect of female sex on the association of chronic cough and depressive symptoms and have adjusted for it in our analyses. Lastly, we were unable to assess potential bidirectionality of the association, that is including the potential effects of depression on chronic cough.
In conclusion, middle-aged and older persons with chronic cough have a disproportionate burden of depressive symptoms, particularly those with chronic cough not explained by a respiratory disease (chronic rhinosinusitis, obstructive airway disease and lung cancer). Moreover, in individuals who have a history of depression, chronic cough increases the risk of recurrent depressive events. This emphasises the importance of screening for depression in patients with chronic cough.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material 00069-2022.SUPPLEMENT (215.8KB, pdf)
Footnotes
Provenance: Submitted article, peer reviewed.
Conflict of interest: J.T. Arinze reports support for the present manuscript received from Merck Sharp and Dohme (MSD), support for attending meetings and/or travel received from Lung Foundation Netherlands (Long Fonds), outside the submitted work. G.G. Brusselle reports support for the present manuscript received from MSD, and payment or honoraria for lectures, presentations, speaker bureaus, manuscript writing or educational events received from AstraZeneca, GlaxoSmithKline, Boehringer Ingelheim, Novartis, Chiesi, Sanofi and Teva, outside the submitted work. The remaining authors have nothing to disclose.
Support statement: This study was supported by a Merck Sharp & Dohme research grant for investigator-initiated study. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Song WJ, Chang YS, Faruqi S, et al. The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J 2015; 45: 1479–1481. doi: 10.1183/09031936.00218714 [DOI] [PubMed] [Google Scholar]
- 2.Morice AH, Millqvist E, Bieksiene K, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J 2020; 55: 1901136. doi: 10.1183/13993003.01136-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schappert SM. National Ambulatory Medical Care Survey: 1991 summary. Adv Data 1993; 230: 1–16. [PubMed] [Google Scholar]
- 4.Chung KF, Pavord ID. Prevalence, pathogenesis, and causes of chronic cough. Lancet 2008; 371: 1364–1374. doi: 10.1016/S0140-6736(08)60595-4 [DOI] [PubMed] [Google Scholar]
- 5.Sohn KH, Song WJ, Kim SH, et al. Chronic cough, not asthma, is associated with depression in the elderly: a community-based population analysis in South Korea. Korean J Intern Med 2019; 34: 1363–1371. doi: 10.3904/kjim.2018.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koo H-K, Park S-W, Park J-W, et al. Chronic cough as a novel phenotype of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2018; 13: 1793–1801. doi: 10.2147/COPD.S153821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Çolak Y, Afzal S, Lange P, et al. Role and impact of chronic cough in individuals with asthma from the general population. J Allergy Clin Immunol Pract 2019; 7: 1783–1792. doi: 10.1016/j.jaip.2019.02.021 [DOI] [PubMed] [Google Scholar]
- 8.Irwin RS, Dudiki N, French CL, et al. Life-threatening and non-life-threatening complications associated with coughing: a scoping review. Chest 2020; 158: 2058–2073. doi: 10.1016/j.chest.2020.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.French CL, Crawford SL, Bova C, et al. Change in psychological, physiological, and situational factors in adults after treatment of chronic cough. Chest 2017; 152: 547–562. doi: 10.1016/j.chest.2017.06.024 [DOI] [PubMed] [Google Scholar]
- 10.French CL, Irwin RS, Curley FJ, et al. Impact of chronic cough on quality of life. Arch Intern Med 1998; 158: 1657–1661. doi: 10.1001/archinte.158.15.1657 [DOI] [PubMed] [Google Scholar]
- 11.Chamberlain SA, Garrod R, Douiri A, et al. The impact of chronic cough: a cross-sectional European survey. Lung 2015; 193: 401–408. doi: 10.1007/s00408-015-9701-2 [DOI] [PubMed] [Google Scholar]
- 12.Dicpinigaitis P. Prevalence of urinary incontinence in women seeking evaluation for chronic cough. Eur Respir J 2020; 56: Suppl. 64, 1286. [Google Scholar]
- 13.Dicpinigaitis PV, Tso R, Banauch G. Prevalence of depressive symptoms among patients with chronic cough. Chest 2006; 130: 1839–1843. doi: 10.1378/chest.130.6.1839 [DOI] [PubMed] [Google Scholar]
- 14.Adams RJ, Appleton SL, Wilson DH, et al. Associations of physical and mental health problems with chronic cough in a representative population cohort. Cough 2009; 5: 10. doi: 10.1186/1745-9974-5-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heo IR, Kim J-Y, Go S-I, et al. Chronic cough is associated with depressive mood in women regardless of smoking status and lung function. Clin Respir J 2021; 15: 753–760. doi: 10.1111/crj.13357 [DOI] [PubMed] [Google Scholar]
- 16.Hulme K, Deary V, Dogan S, et al. Psychological profile of individuals presenting with chronic cough. ERJ Open Res 2017; 3: 00099-02016. doi: 10.1183/23120541.00099-2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vertigan AE. Somatic cough syndrome or psychogenic cough – what is the difference? J Thorac Dis 2017; 9: 831–838. doi: 10.21037/jtd.2017.03.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burcusa SL, Iacono WG. Risk for recurrence in depression. Clin Psychol Rev 2007; 27: 959–985. doi: 10.1016/j.cpr.2007.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Won HK, Lee JH, An J, et al. Impact of chronic cough on health-related quality of life in the Korean adult general population: the Korean National Health and Nutrition Examination Survey 2010–2016. Allergy Asthma Immunol Res 2020; 12: 964–979. doi: 10.4168/aair.2020.12.6.964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johansson H, Johannessen A, Holm M, et al. Prevalence, progression and impact of chronic cough on employment in Northern Europe. Eur Respir J 2021; 57: 2003344. doi: 10.1183/13993003.03344-2020 [DOI] [PubMed] [Google Scholar]
- 21.Ikram MA, Brusselle G, Ghanbari M, et al. Objectives, design and main findings until 2020 from the Rotterdam Study. Eur J Epidemiol 2020; 35: 483–517. doi: 10.1007/s10654-020-00640-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arinze JT, de Roos EW, Karimi L, et al. Prevalence and incidence of, and risk factors for chronic cough in the adult population: the Rotterdam Study. ERJ Open Res 2020; 6: 00300-2019. doi: 10.1183/23120541.00300-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beekman AT, van Limbeek J, Deeg DJ, et al. [A screening tool for depression in the elderly in the general population: the usefulness of Center for Epidemiological Studies Depression Scale (CES-D)]. Een screeningsinstrument voor depressie bij ouderen in de algemene bevolking: de bruikbaarheid van de Center for Epidemiologic Studies Depression Scale (CES-D). Tijdschr Gerontol Geriatr 1994; 25: 95–103. [PubMed] [Google Scholar]
- 24.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- 25.Wing JK, Babor T, Brugha T, et al. SCAN. Schedules for Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatry 1990; 47: 589–593. doi: 10.1001/archpsyc.1990.01810180089012 [DOI] [PubMed] [Google Scholar]
- 26.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). 4th Edn. Washington, DC, American Psychiatric Association, 2010; pp. 345–428. [Google Scholar]
- 27.Bleumink GS, Knetsch AM, Sturkenboom MC, et al. Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure. The Rotterdam Study. Eur Heart J 2004; 25: 1614–1619. doi: 10.1016/j.ehj.2004.06.038 [DOI] [PubMed] [Google Scholar]
- 28.Ryan NM, Vertigan AE, Birring SS. An update and systematic review on drug therapies for the treatment of refractory chronic cough. Expert Opin Pharmacother 2018; 19: 687–711. doi: 10.1080/14656566.2018.1462795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haque RA, Usmani OS, Barnes PJ. Chronic idiopathic cough: a discrete clinical entity? Chest 2005; 127: 1710–1713. doi: 10.1378/chest.127.5.1710 [DOI] [PubMed] [Google Scholar]
- 30.Johansson H, Johannessen A, Holm M, et al. Prevalence, progression and impact of chronic cough on employment in Northern Europe. Eur Respir J 2021; 57: 2003344. doi: 10.1183/13993003.03344-2020 [DOI] [PubMed] [Google Scholar]
- 31.Ando A, Smallwood D, McMahon M, et al. Neural correlates of cough hypersensitivity in humans: evidence for central sensitisation and dysfunctional inhibitory control. Thorax 2016; 71: 323. doi: 10.1136/thoraxjnl-2015-207425 [DOI] [PubMed] [Google Scholar]
- 32.Buhle JT, Kober H, Ochsner KN, et al. Common representation of pain and negative emotion in the midbrain periaqueductal gray. Soc Cogn Affect Neurosci 2013; 8: 609–616. doi: 10.1093/scan/nss038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ho YC, Lin TB, Hsieh MC, et al. Periaqueductal gray glutamatergic transmission governs chronic stress-induced depression. Neuropsychopharmacology 2018; 43: 302–312. doi: 10.1038/npp.2017.199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hulme K, Dogan S, Parker SM, et al. ‘Chronic cough, cause unknown’: a qualitative study of patient perspectives of chronic refractory cough. J Health Psychol 2019; 24: 707–716. doi: 10.1177/1359105316684204 [DOI] [PubMed] [Google Scholar]
- 35.Van den Bergh O, Van Diest I, Dupont L, et al. On the psychology of cough. Lung 2012; 190: 55–61. doi: 10.1007/s00408-011-9347-7 [DOI] [PubMed] [Google Scholar]
- 36.Sanacora G, Gueorguieva R, Epperson CN, et al. Subtype-specific alterations of γ-aminobutyric acid and glutamate in patients with major depression. Arch Gen Psychiatry 2004; 61: 705–713. doi: 10.1001/archpsyc.61.7.705 [DOI] [PubMed] [Google Scholar]
- 37.Yovell Y, Bar G, Mashiah M, et al. Ultra-low-dose buprenorphine as a time-limited treatment for severe suicidal ideation: a randomized controlled trial. Am J Psychiatry 2016; 173: 491–498. doi: 10.1176/appi.ajp.2015.15040535 [DOI] [PubMed] [Google Scholar]
- 38.Yasmin S, Carpenter LL, Leon Z, et al. Adjunctive gabapentin in treatment-resistant depression: a retrospective chart review. J Affect Disord 2001; 63: 243–247. doi: 10.1016/S0165-0327(00)00187-7 [DOI] [PubMed] [Google Scholar]
- 39.Arinze JT, Verhamme KMC, Luik AI, et al. The interrelatedness of chronic cough and chronic pain. Eur Respir J 2021; 57: 2002651. doi: 10.1183/13993003.02651-2020 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material 00069-2022.SUPPLEMENT (215.8KB, pdf)