Abstract
Objective
The aim was to evaluate the impact of the coronavirus disease 2019 (COVID-19) pandemic on the clinical experiences, research opportunities and well-being of rheumatology trainees.
Methods
A voluntary, anonymous, Web-based survey was administered in English, Spanish or French from 19 August 2020 to 5 October 2020. Adult and paediatric rheumatology trainees were invited to participate via social media and email. Using multiple-choice questions and Likert scales, the perceptions of trainees regarding the impact of the COVID-19 pandemic on patient care and redeployment, learning and supervision, research and well-being were assessed.
Results
There were 302 respondents from 33 countries, with 83% in adult rheumatology training. An increase in non-rheumatology clinical work was reported by 45%, with 68% of these having been redeployed to COVID-19. Overall, trainees reported a negative impact on their learning opportunities during rheumatology training, including outpatient clinics (79%), inpatient consultations (59%), didactic teaching (55%), procedures (53%), teaching opportunities (52%) and ultrasonography (36%). Impacts on research experiences were reported by 46% of respondents, with 39% of these reporting that COVID-19 negatively affected their ability to continue their pre-pandemic research. Burnout and increases in stress were reported by 50% and 68%, respectively. Physical health was negatively impacted by training programme changes in 25% of respondents.
Conclusion
The COVID-19 pandemic has had a substantial impact on rheumatology training and trainee well-being. Our study highlights the extent of this impact on research opportunities and clinical care, which are highly relevant to future curriculum planning and the clinical learning environment.
Keywords: Medical Education, COVID-19, Rheumatology Fellowship
Key messages
The impact of the COVID-19 pandemic on rheumatology trainees is poorly understood.
The COVID-19 pandemic has negatively impacted rheumatology training, including clinical care, research, procedural skills/ultrasonography and didactic teaching.
Rheumatology trainees reported an increase in burnout and work-related stress owing to the pandemic.
Introduction
The global coronavirus disease 2019 (COVID-19) pandemic profoundly altered health-care delivery, medical education and physician training [1]. These shifts place a unique strain on health-care trainees, because changes in patient care, disruptions in research, and the redeployment of trainees outside of their typical setting can impact training experience and the development of necessary clinical skills [2]. Surveys of trainees in other medical specialties have described the impact of the COVID-19 pandemic on hands-on training and didactic sessions, in addition to increases in trainee burnout and stress [3–5]. The impact of the COVID-19 pandemic on rheumatology trainees has not yet been described. The COVID-19 Global Rheumatology Alliance (GRA), an international collaborative that includes rheumatology trainees, providers in academic and community-based practice, in addition to patients, was formed to understand the impact of the COVID-19 pandemic on patients and providers [6, 7]. We leveraged this international collaborative network to conduct a cross-sectional survey of the experiences of rheumatology trainees during the COVID-19 pandemic, with the aims of evaluating and describing the impact on rheumatology trainees’ clinical experiences, research opportunities and well-being.
Methods
Survey design and dissemination
A 77-question survey was developed by members of the GRA to evaluate the above-listed goals, which included multiple-choice and Likert scale questions. Fifteen questions that specifically addressed telemedicine are reported separately. Key domains evaluated were general demographics, impact on rheumatology training and research, patient care and trainee wellness. Questions were designed collaboratively with listed authors and pre-tested on five rheumatology trainees before global distribution. The survey instrument is available is Supplementary Appendix 1 (Rheumatology Advances in Practice online).
A Web-based survey was available in English, Spanish and French via the REDCap platform. Members of the GRA, the ACR Fellows-in-Training list and the Emerging EULAR Network (EMEUNET) Trainee list were contacted by email and invited to participate. An invitation was sent to the ILAR Executive Committee requesting them to share the survey with their constituents. Regional/country representatives from the GRA were also asked to disseminate invitations to participate to rheumatology trainees in their countries. US Program directors were requested to send invitations to their Fellows. Additionally, respondents were recruited on Twitter via invitations from official accounts of the GRA, ACR and EMEUNET. All surveys were completed between 19 August and 5 October 2020.
Eligibility was established by self-report of being an adult and paediatric rheumatology trainee. Trainees were included if they reported rheumatology as part of their job description, had not completed their rheumatology training before 2020, were aged ≥18 years and consented to participate in the survey. The survey was voluntary and did not include personal identifiers, protected health information or incentives for participation.
Ethics statement
Ethical approval was granted by the Institutional Review Board at Temple University Hospital (protocol 27279), by the National Research Ethics Committee for COVID-19, Ireland (application number 20-NREC-COV-073) and by University College London Research Ethics Committee (UCL ethics approval ID 18859/001). Data from the UK/European Economic Area (EEA) were hosted on a REDCap database at University College London, UK. Non-UK/EEA data were hosted at Temple University Hospital, USA. The institutional review board waived documentation of written consent by avoiding collection of identifying information. Respondents were required to verify that they consented to participate before the beginning the survey.
Reporting and statistical analysis
All respondents were included in the analysis. Data are presented as the number followed by the percentage. Data from five-point Likert scales (with anchors strongly disagree to strongly agree, very negatively impacted to very positively impacted, or not helpful to very helpful) are also reported as the number followed by the percentage. Neutral (or no impact) components of the Likert scales are not reported, and only the positive and negative components of the Likert scales are reported, where the extent of each component is specified (i.e. agree and strongly agree). Data are presented using descriptive statistics and processed using R Studio v.1.4.1103.
Results
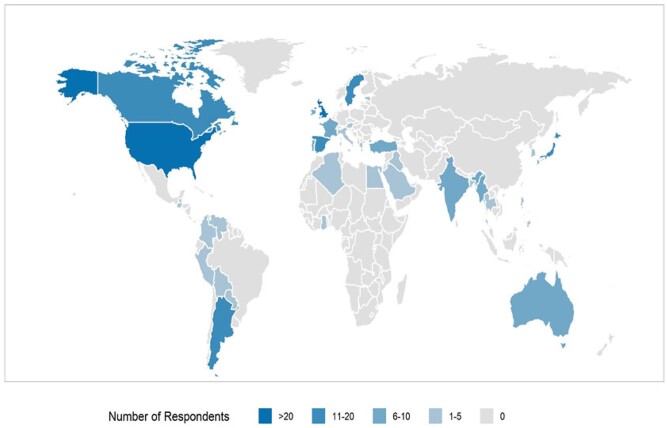
In total, 302 rheumatology trainees from 33 countries responded to the survey: 116 (38%) were from the USA, 89 (29%) from Europe and 97 (32%) from other countries (Table 1; Fig. 1). Most of the respondents (n = 252, 83%) were in adult rheumatology training, with 29 (10%) in paediatric rheumatology training and 21 (7%) in dual adult/paediatric training. Before December 2019, most (n = 279, 92%) were in full-time training, with 208 (69%) in rheumatology clinical training and 39 (13%) undertaking research in a designated research track. The majority of respondents were in the early training years, with 204 (68%) in the first 3 years of training programmes, 60 (20%) in later training years and 38 (13%) having completed training in 2020. The majority of respondents reported career intent after rheumatology training of entering an academic or teaching hospital-affiliated clinical practice (n = 213, 71%).
Table 1.
Respondent characteristics
| Training characteristics | Combined n = 302 |
|---|---|
| Location | |
| USA | 116 |
| Europe | 89 |
| Rest of world | 97 |
| Acquired COVID19 | |
| PCR-confirmed | 14 (4.6) |
| Serology-confirmed | 4 (1.3) |
| PCR and serology | 9 (3.0) |
| Symptoms only | 14 (4.6) |
| Training track or concentration | |
| Clinical | 63 (51.2) |
| Research | 40 (32.5) |
| Education | 11 (8.9) |
| No track designated | 7 (5.7) |
| Other | 2 (1.6) |
| Weekly work, h | |
| <20 | 55 (18.4) |
| 20–29 | 20 (6.7) |
| 30–39 | 43 (14.4) |
| 40–49 | 96 (32.1) |
| 50–59 | 50 (16.7) |
| 60–69 | 26 (8.7) |
| 70–79 | 10 (3.3) |
| COVID-19 risk and behaviours | |
| Disability | 10 (3.3) |
| High risk | 30 (9.9) |
| Pregnant | 19 (6.4) |
| Shielding/quarantining | 82 (32.5) |
| Current career plans | |
| Basic science research | 45 (14.9) |
| Clinical research (including clinical trials and epidemiology) | 117 (38.7) |
| Clinical practice, academic setting | 213 (70.5) |
| Clinical practice, non-academic/ private/community setting | 124 (41.1) |
| Industry | 9 (3.0) |
| Regulatory agencies | 1 (0.3) |
| Other | 2 (0.7) |
| Prefer not to answer | 2 (0.7) |
| For those who completed training in 2020, impact on career plans | 38/302 (12.6%) |
| Rheumatology training was extended beyond the usual duration | 6 (15.8) |
| Post-training job offer was rescinded | 13 (34.2) |
| Negative impact on ability to find job | 14 (36.8) |
COVID-19: corona virus disease 2019.
Fig. 1.
Global distribution of respondents
Impact of COVID-19 on rheumatology training
Patient care experiences
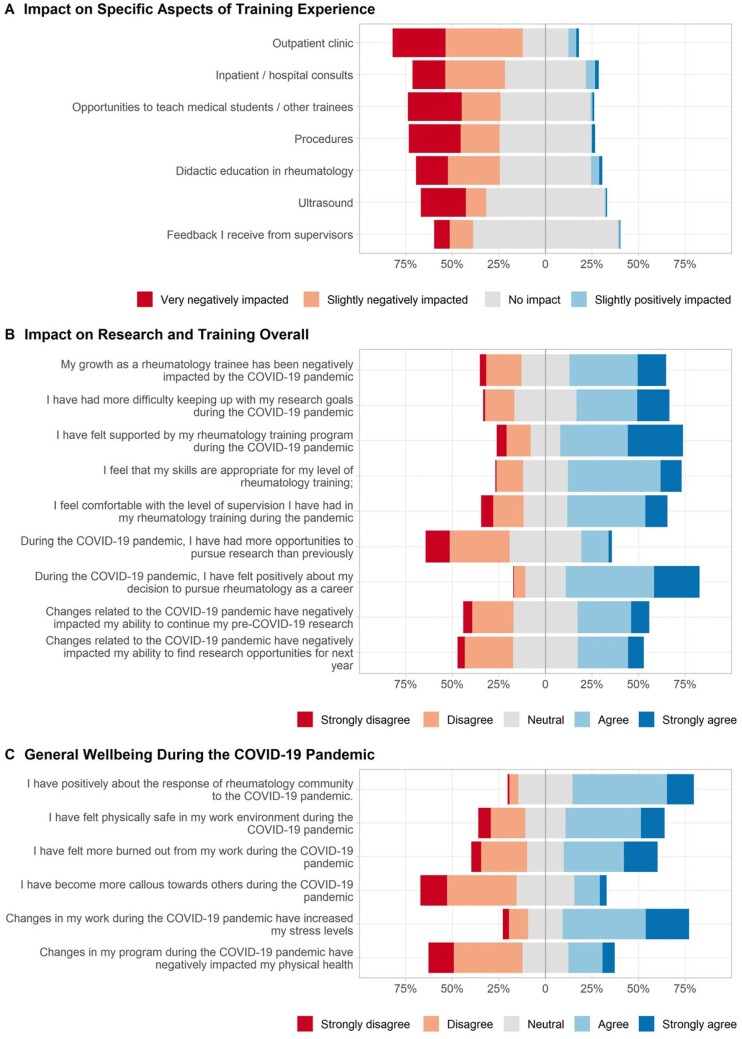
Trainees reported a substantial impact of the COVID-19 pandemic on clinical training experiences (Fig. 2C). Most trainees (n = 238, 79%) reported an impact on outpatient clinical work, with a negative impact reported by the majority of those who responded (n = 211, 90%). Many trainees continued to see some patients in person in outpatient settings, with 97 (32%) continuing routine follow-up in person, 170 (56%) seeing urgent follow-up in person, 107 (35%) seeing new patient visits in person and 59 (30%) seeing hospital discharge follow-up patients in person (Table 2). About a quarter (n = 73, 24%) did not continue to see outpatients in person.
Fig. 2.
Impact on training, clinical experiences, research and well-being
Table 2.
Impact of COVID-19 on research and clinical activities
| Research experience | Combined n = 217 (%) |
|---|---|
| Research before December 2019 | |
| Basic science | 48 (22) |
| Clinical research | 158 (73) |
| Other | 11 (5) |
| Research part of a postgraduate degree (e.g. PhD, Master’s) | 62 (31) |
| Changes in research experience during COVID-19 | 128 (46) |
| Research laboratory was closed | 37 (12) |
| Research laboratory was used for COVID-19 research/clinical care | 13 (4) |
| Research resources were redirected to COVID-19 projects | 29 (10) |
| Unable to participate in research owing to clinical responsibilities | 40 (13) |
| Unable to apply for research grants owing to clinical responsibilities | 15 (5) |
| Limited opportunities to recruit patients | 69 (23) |
| Research projects halted/postponed | 52 (17) |
| Research projects cancelled | 15 (5) |
| Cancellation of research grant awards | 8 (3) |
| Limited support-staff resources (owing to redirection of workforce or furlough) | 31 (10) |
| Redirection of own research project to COVID-19-related research | |
| Other | 16 (5 |
| 9 (3) | |
|
| |
| Clinical training | Combined |
| n = 302 (%) | |
|
| |
| Received training on care of COVID-19 patients | 175 (58) |
| Increased non-rheumatology clinical duties (i.e. Internal Medicine wards, intensive care unit) | 135 (44) |
| Clinical department | |
| Emergency department | 40 (13) |
| Internal medicine (non-COVID-19 wards) | 60 (20) |
| Outpatient COVID-19 screening facility | 17 (6) |
| Inpatient COVID-19 ward or facility | 93 (31) |
| High-dependency unit/intensive care unit | 16 (5) |
| Non-clinical work (e.g. COVID-related laboratory) | 4 (1) |
| Weekly hours in this new role | |
| <20 | 30 (22) |
| 20–29 | 16 (12) |
| 30–39 | 16 (12) |
| 40–49 | 35 (26) |
| 50–59 | 19 (14) |
| 60–69 | 11 (8) |
| 70–79 | 6 (4) |
| 80+ | 2 (2) |
| Number of weeks worked in this role | |
| ≤1 | 11 (4) |
| 2–3 | 0 |
| 4–6 | 0 |
| 7–9 | 0 |
| ≥10 | 46 (15) |
| Voluntary | 67 (59) |
| Assigned | 68 (50) |
| Compensated | 44 (33) |
| Pay reduced or delayed | 6 (7) |
| Outpatient rheumatology patients were evaluated in-person for: | 302 (%) |
| Routine follow-up visits | 97 (32) |
| Urgent visits | 170 (56) |
| New patient visits | 107 (35) |
| Hospital discharge follow-up | 59 (20) |
| I did not evaluate outpatient rheumatology patients in person | 73 (24.2) |
| Inpatient rheumatology patients were evaluated | 302 (%) |
| In-person by myself | 129 (43) |
| In-person by myself with a supervising physician | 132 (44) |
| In-person by the supervising physician only | 22 (7) |
| Virtually (remotely) | 61 (20) |
| Other | 6 (2) |
COVID-19: corona virus disease 2019.
More than half the respondents (n = 177, 59%) reported an impact of the pandemic on inpatient consultation services; the majority of those trainees (n = 150, 85%) perceived this impact as being negative. Most trainees continued to see inpatient consultations in person, either alone (n = 129, 43%) and/or with a supervising physician (n = 132, 44%). Some trainees reported virtual inpatient consultations (n = 66, 22%), and a small number (n = 22, 7%) reported that inpatient consultations were seen in person by the supervising physician only.
An impact on clinical procedures was reported by 159 (53%), with most respondents noting a negative change (n = 147, 92%). US training was impacted for 110 (36%), with 106 (96%) reporting a negative impact.
Education and supervision
Trainee perceptions of their training programmes are summarized in Fig. 2B. In terms of education, 167 (55%) reported an impact on didactic education in rheumatology, with 136 of these (81%) reporting a negative impact. Half the respondents (n = 157, 52%) reported an impact on opportunities to teach medical students, with 150 (96%) of these reporting a negative impact.
Overall, clinical supervision was impacted for only one-quarter of trainees (n = 78, 26%), but most of them reported a negative impact (n = 63, 81%). More than half reported that they felt comfortable with the level of supervision of their training during the pandemic (n = 158, 54%) and that their rheumatology skills were appropriate to their level of training (n = 180, 61%). However, about half (n = 153, 52%) reported that their growth as a rheumatology trainee had been negatively impacted by the COVID-19 pandemic. Two-thirds of trainees (n = 198, 66%) felt they were supported by their training programme during the pandemic.
Redeployment
Many trainees (n = 135, 45%) reported being redeployed to other clinical settings during the pandemic (Table 2); time spent in the new role counted towards rheumatology training requirements for 70 (52%). Seventy trainees (52%) continued rheumatology clinical work during redeployment. A large proportion (n = 98, 73%) undertook evening or overnight duties as part of redeployment. A small number of the 29 paediatric trainees surveyed were redeployed (n = 5, 17%); of these, 4 (80%) were asked to practise adult medicine. Redeployment was reported to be compulsory for about two-thirds (n = 91, 68%); however, one-third (n = 44, 33%) were compensated for this additional clinical work. Over half of all trainees (n = 175, 58%) reported having instruction in the care of COVID patients; 168 (96%) found this helpful.
Research
The majority of trainees (n = 217, 72%) reported participating in research before the onset of the COVID-19 pandemic (Table 2); one-third (n = 62, 31%) were undertaking their research as part of a postgraduate degree (such as master’s degree or PhD) concurrently, separate from their rheumatology training. A change in research experience owing to COVID-19 was reported by 128 (46%), owing to closure of the research laboratory, postponement of their projects and redirection of resources, staff or their own efforts to COVID-19 research. Half of these (n = 69, 54%) reported limited opportunities for patient recruitment for research. In addition, clinical responsibilities during the pandemic affected the participation of trainees in research and their ability to apply for research grants.
One-third of trainees (n = 101, 33%) felt that the COVID-19 pandemic had negatively impacted their ability to find research opportunities for the forthcoming training year (Fig. 2B), and 110 (36%) reported that the pandemic had negatively impacted their ability to continue their pre-COVID-19 research projects. Nearly half (n = 142, 47%) reported difficulty in keeping up with their research goals. Interestingly, some trainees (n = 47, 16%) reported more research opportunities available during the pandemic.
Impact of COVID-19 on rheumatology careers
Of the 38 trainees who completed training in 2020, 6 (16%) reported that their training had to be extended owing to the COVID-19 pandemic. One-third (n = 13, 34%) of graduates reported that they had a post-training job offer rescinded, and 14 (37%) reported a negative impact on their ability to find a job.
Overall, the majority of trainees (n = 212, 70%) remained positive about their decision to pursue a career in rheumatology, with only 19 (6%) expressing negative feelings about their career choice.
Impact of COVID-19 on health and well-being
Thirty (10%) respondents had health conditions that put them at high risk for poor outcomes of COVID-19. Additionally, 19 (6%) were pregnant during the pandemic, 10 (3%) reported having a disability, and 82 (33%) reported being advised to shield or quarantine at some point during the pandemic. Forty-one (14%) respondents reported a COVID-19 infection (Table 1).
Using a validated two-question modified Maslach burnout inventory, assessing depersonalization and emotional exhaustion [8], many trainees reported personal impacts of the pandemic (Fig. 2A), including an increase in work-related stress (n = 204, 68%) and burnout (n = 151, 50%) and a negative impact on physical health (n = 75, 25%). Some (62, 17%) expressed being more callous towards others. Physical safety was also a concern; 160 (53%) reported feeling physically safe in the workplace, whereas 76 (25%) reported not feeling physically safe. Trainees expressed concerns about lack of training concerning care for COVID-19 patients (n = 61, 20%), lack of comfort in the clinical setting (n = 81, 27%), insufficient personal protective equipment (n = 100, 33%), an immunocompromised state (n = 16, 5%) and pregnancy (n = 12, 4%).
Discussion
The data from this survey of 302 rheumatology trainees show that the COVID-19 pandemic has had a substantial impact on rheumatology trainees globally. These findings have important implications for training programmes, their faculty and leadership.
Impact on rheumatology training
Clinical training and patient care
The COVID-19 pandemic was perceived by a majority of rheumatology trainees to have a substantial, usually negative impact on almost all aspects of clinical training. Requirements for completion of rheumatology training vary [9–11], but do require an adequate number of patient interactions to reach competency achievements. Any decrease in outpatient or inpatient volume and procedures (e.g. arthrocentesis, US), as reported by trainees in this and other surveys [12–15], could threaten completion of training.
Supervision and education
Despite the substantial impact on inpatient and outpatient care experiences, it is reassuring that trainees felt comfortable with their level of clinical supervision and supported by their programmes during the pandemic. However, a large number of trainees felt that their learning was affected. Looking ahead, increased adoption of online and virtual instruction could mitigate the impact of future disruptions to in-person training. Surveys of trainees in other fields highlight changes in the mode of education: in-person conferences [13] and simulation procedure training [12, 16, 17] shifted to online delivery, with generally positive appraisal [18]. The ACR and others have created online lectures to maintain knowledge acquisition through the pandemic. Rheumatology programmes might benefit from creating opportunities to address learning loss to augment trainee education through virtual standardized patient encounters and other forms of clinical reasoning simulation. Ultimately, modernization of the rheumatology curriculum to suit digital (‘millennial’) learners is perhaps a long-term benefit of the rapid transition to online education.
Redeployment
As with trainees in other disciplines [14, 19], many rheumatology trainees reported being reassigned to new clinical roles. Although about half continued their work in rheumatology, some were redirected to clinical areas of need. Our survey did not assess trainees’ feelings about how reassignment affected their rheumatology clinical skills, and in future trainee surveys it might be necessary to assess how redeployment affected knowledge acquisition and clinical training. Importantly, a survey of allergy/immunology trainees in the USA found that confidence in clinical skills among those reassigned to patients with COVID-19 was associated with feeling safe in the practice setting [20], suggesting that if there is a need to redeploy trainees in the future, continued support and training might help them to navigate changes without detriment to their education.
Impact on research
Impact on trainee research opportunities has been widely observed during the pandemic. Although not assessed in this survey, it is well documented that the COVID-19 pandemic has disproportionately affected the ability of some physicians and scientists to continue research, owing to obligations outside of training, such as parenthood, location in a COVID-19 hotspot and lack of research support in smaller institutions, for example [21–23]. Many respondents also expressed difficulty in submitting research grants because of competing clinical demands, which might impact on the pipeline of rheumatology researchers. Although the pandemic negatively impacted many areas of research, some trainees found opportunities researching COVID-19 and the impact on rheumatic disease patients [7].
Impact on rheumatology careers
Nearly two-thirds of trainees who completed training in 2020 reported having had at least one post-training job offer rescinded, perhaps owing to decreased revenue and hiring freezes [15, 24, 25]. Although the impacts are not yet clear, a minority of trainees reported a negative impact of the pandemic on their ability to find a job.
Impact on trainee health and well-being
Our survey revealed negative impacts on trainee health and well-being. Rheumatology trainees expressed increased stress from work, burnout and feelings of callousness. Other surveys have also identified patterns of stress and burnout during the pandemic: an early global trainee survey noted that a strong predictor of burnout symptoms was related to taking care of a higher volume of COVID-19 patients. Trainees in Saudi Arabia reported frequently feeling anxiety and low mood [28, 29], and a survey of hospital physicians in England showed that nearly half reported that their mental health had deteriorated during the pandemic [30]. The long-term effects of these negative psychological impacts are as yet unknown, though prior studies have shown that burnout among health-care professionals is associated with personal and professional adverse effects including depression, suicidal ideation, substance abuse, relationship difficulties, decreased productivity, work dissatisfaction, self-reported medical errors and suboptimal patient care [31]. Supporting trainees’ feeling of safety in the practice setting might also have broader impacts on their confidence in clinical skills [20]. Rheumatology programmes should remain vigilant about potential stressors that trainees have experienced through the pandemic.
Limitations and strengths
Our study has limitations. Respondents might be more likely to complete a survey if they perceive a greater impact on their training, contributing to selection bias. In addition, many of the respondents had research experience; trainees who participate in research might have been more likely to be aware of the survey owing to advertisements by the GRA and major rheumatology societies. Selection and response bias were difficult to minimize, but a wide recruitment strategy was used. Survey respondents were mostly trainees in the USA and Europe, limiting generalizability. We were unable to obtain information about factors that might have contributed to variable training and trainee experiences, such as regional infrastructure of telemedicine, local severity of the COVID-19 pandemic and local policy. Finally, our study was one of several surveys being distributed to trainees, which might have contributed to survey fatigue and decreased participation.
Strengths of our study include the international distribution in three languages, with the respondents being from 33 countries. To our knowledge, this is the only international survey focused on rheumatology during the COVID-19 pandemic. Our survey was designed by a multi-regional team and trialled by trainees and programme directors, addressing relevant aspects of training.
Conclusions
Sudden and unexpected changes to health services and educational institutions during the COVID-19 pandemic have significantly impacted the clinical training, research opportunities and health and well-being of rheumatology trainees. These findings highlight the importance of curriculum and workforce assessments, along with reforms to ensure that rheumatology trainees have the support and training required to adapt to the changes brought about by the pandemic.
Funding: Su-Ann Yeoh has received research grants from Royal College of Physicians, Rosetrees Trust, NIHR University College London Hospitals Biomedical Research Centre and UCLH Charities, all unrelated to this work. Richard Conway has received consulting fees, speaking fees, honoraria from Janssen, Roche, Sanofi, Abbvie (all less than $10 000), all unrelated to this work. Maximilian Konig has received consulting fees, speaking fees, honoraria from Celltrion (less than $10 000), all unrelated to this work. Jeff Sparks has received consulting fees from Bristol-Myers Squibb, Gilead, Inova Diagnostics, Optum, Pfizer (less than $10 000), all unrelated to this work. Manuel Ugarte-Gil has received research grants from Pfizer and Janssen, unrelated to this work. Suleman Bhana reports non-branded consulting work for AbbVie, Horizon, Novartis and Pfizer (all less than US$10 000), all unrelated to this work. Jonathan Hausmann has received consulting fees, speaking fees, honoraria from Novartis, Biogen, Pfizer (less than $10 000), all unrelated to this work. Pedro Machado has received consulting fees, speaking fees, honoraria from Abbvie, BMS, Celgene, Eli Lilly, Galapagos, Janssen, MSD, Novartis, Orphazyme, Pfizer, Roche and UCB (all less than $10 000), all unrelated to this work. Philip Robinson has received consulting fees, speaking fees, honoraria from Abbvie, Atom Biosciences, Janssen, Lilly, Novartis, Pfizer, Roche, UCB (less than $10 000), all unrelated to this work. Philip Robinson has also received other research grants from Janssen, Novartis, Pfizer and UCB, all unrelated to this work. Emily Sirotich has received non-financial support from Canadian Arthritis Patient Alliance, outside the submitted work. Emily Sirotich is a board member of the COVID-19 Global Rheumatology Alliance and has received honoraria from the COVID-19 Global Rheumatology Alliance (all less than $10 000). Jinoos Yazdany has received consulting fees, speaking fees, honoraria from Pfizer, Astra Zeneca, Eli Lilly and Aurinia (less than $10 000), all unrelated to this work. Jean Liew has received research grant funding from Pfizer (more than $10 000), unrelated to this work. Rebecca Grainger has received honoraria for speaking from Pfizer Australia, Cornerstones, Jannsen New Zealand, Jannsen Australia and consultancy fees from Novartis (all less than $10 000), all unrelated to this work. Kristen Young, Michael Putman, Sebastian Sattui, Elizabeth Graef, Adam Kilian, Laura Upton, Francis Berenbaum, Wendy Costello, Paul Sufka, Zachary Wallace and Arundathi Jayatilleke report no disclosures.
Disclosure statement: The views expressed here are those of the authors and participating members of the COVID-19 Global Rheumatology Alliance and do not necessarily represent the views of the American College of Rheumatology, the European League Against Rheumatism (EULAR), or any other organization.
Data availability statement
Data are available upon reasonable request. The data underlying this article are available in the article and in its online supplementary material.
Supplementary data
Supplementary data are available at Rheumatology Advances in Practice online.
Supplementary Material
References
- 1. Gallagher TH, Schleyer AM.. “We signed up for this!” — student and trainee responses to the Covid-19 pandemic. N Engl J Med 2020;382:e96. [DOI] [PubMed] [Google Scholar]
- 2. Potts JR. Residency and fellowship program accreditation: effects of the novel coronavirus (COVID-19) pandemic. J Am Coll Surg 2020;230:1094–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nair A, Mishra D, Gandhi R. et al. The impact of COVID-19 related lockdown on ophthalmology training programs in India – outcomes of a survey. Indian J Ophthalmol 2020;68:999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Osama M, Zaheer F, Saeed H. et al. Impact of COVID-19 on surgical residency programs in Pakistan; a residents’ perspective. Do programs need formal restructuring to adjust with the “new normal”? A cross-sectional survey study. Int J Surg 2020;79:252–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pelargos PE, Chakraborty A, Zhao YD. et al. An evaluation of neurosurgical resident education and sentiment during the Coronavirus Disease 2019 pandemic: a North American survey. World Neurosurg 2020;140:e381–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wallace ZS, Bhana S, Hausmann JS. et al. The Rheumatology Community responds to the COVID-19 pandemic: the establishment of the COVID-19 global rheumatology alliance. Rheumatology 2020;59:1204–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liew JW, Bhana S, Costello W. et al. ; for the COVID-19 Global Rheumatology Alliance. The COVID-19 Global Rheumatology Alliance: evaluating the rapid design and implementation of an international registry against best practice. Rheumatology 2021;60:353–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. West CP, Dyrbye LN, Sloan JA, Shanafelt TD.. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med 2009;24:1318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Subspecialty Training Requirements in Adult Rheumatology. Royal College of Physicians and Surgeons of Canada. https://www.royalcollege.ca/rcsite/documents/ibd/rheumatology_adult_str_e.pdf (4 April 2021, date last accessed).
- 10. European Training Requirements in Rheumatology. European Union of Medical Specialists. https://www.eular.org/myUploadData/files/European-Training-Requirements-in-Rheumatology%20endorsed%20UEMS%20April%2012%202014.pdf (4 April 2021, date last accessed).
- 11. Core Curriculum Outline for Rheumatology Programs. American College of Rheumatology. https://www.rheumatology.org/Portals/0/Files/Core-Curriculum-Outline.pdf (4 April 2021, date last accessed).
- 12. Hope C, Reilly JJ, Griffiths G. et al. The impact of COVID-19 on surgical training: a systematic review. Tech Coloproctol 2021;25:505–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. An TW, Henry JK, Igboechi O. et al. How are orthopaedic surgery residencies responding to the COVID-19 pandemic? An assessment of resident experiences in cities of major virus outbreak. J Am Acad Orthop Surg 2020;28:e679–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Caruana EJ, Patel A, Kendall S. et al. Impact of coronavirus 2019 (COVID-19) on training and well-being in subspecialty surgery: a national survey of cardiothoracic trainees in the United Kingdom. J Thorac Cardiovasc Surg 2020;160:980–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Irastorza LE, Hopson P, Ta A. et al. The impact of COVID-19 on job prospects and educational training for pediatric gastroenterology fellows. J Pediatr Gastroenterol Nutr 2021;72:514–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chong JH, Chahal A, Ricci F. et al. The transformation of cardiology training in response to the COVID-19 pandemic: enhancing current and future standards to deliver optimal patient care. Can J Cardiol 2021;37:519–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ferrara M, Romano V, Steel DH. et al. ; OphthaTraining Group. Reshaping ophthalmology training after COVID-19 pandemic. Eye 2020;34:2089–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. White CA, Guido P, Young L. et al. Redesigning fellowship curriculum amidst the Covid-19 pandemic: our shared experiences. Endocr Pract 2020;26:926–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Johnson J, Chung MT, Stathakios J. et al. The impact of the COVID-19 pandemic on fellowship training: a national survey of pediatric otolaryngology fellowship directors. Int J Pediatr Otorhinolaryngol 2020;136:110217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kahwash BM, Deshpande DR, Guo C. et al. Allergy/immunology trainee experiences during the COVID-19 pandemic: AAAAI work group report of the fellows-in-training committee. J Allergy Clin Immunol Pract 2021;9:1–6.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Breuning M, Fattore C, Ramos J. et al. Gender, parenting, and scholarly productivity during the global pandemic. APSA Preprints. 2020. https://preprints.apsanet.org/engage/apsa/article-details/5f16fc5660b4ad001212f977 (24 March 2022, date last accessed).
- 22. Squazzoni F, Bravo G, Grimaldo F. et al. Only second-class tickets for women in the COVID-19 race. A study on manuscript submissions and reviews in 2329 Elsevier Journals. 2020. https://papers.ssrn.com/abstract=3712813 (7 April 2021, date last accessed).
- 23.The impact of the COVID-19 pandemic on the extramural scientific workforce – outcomes from an NIH-led survey – NIH extramural nexus. https://nexus.od.nih.gov/all/2021/03/25/the-impact-of-the-covid-19-pandemic-on-the-extramural-scientific-workforce-outcomes-from-an-nih-led-survey/ (8 April 2021, date last accessed).
- 24. Givi B, Moore MG, Bewley AF. et al. Advanced head and neck surgery training during the COVID-19 pandemic. Head Neck 2020;42:1411–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. COVID-19 financial impact on physician practices. https://www.ama-assn.org/practice-management/sustainability/covid-19-financial-impact-physician-practices (4 April 2021, date last accessed).
- 26. Battafarano DF, Ditmyer M, Bolster MB. et al. 2015 American College of Rheumatology workforce study: supply and demand projections of adult rheumatology workforce, 2015–2030. Arthritis Care Res 2018;70:617–26. [DOI] [PubMed] [Google Scholar]
- 27. Correll CK, Ditmyer MM, Mehta J. et al. 2015 American College of Rheumatology workforce study and demand projections of pediatric rheumatology workforce, 2015–2030. Arthritis Care Res 2020;74:340–48. [DOI] [PubMed] [Google Scholar]
- 28. Cravero AL, Kim NJ, Feld LD. et al. Impact of exposure to patients with COVID-19 on residents and fellows: an international survey of 1420 trainees. Postgraduate Med J 2020;97:706–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Balhareth A, AlDuhileb MA, Aldulaijan FA. et al. Impact of COVID-19 pandemic on residency and fellowship training programs in Saudi Arabia: a nationwide cross-sectional study. Ann West Med Surg 2020;57:127–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cubitt LJ, Im YR, Scott CJ. et al. Beyond PPE: a mixed qualitative–quantitative study capturing the wider issues affecting doctors’ well-being during the COVID-19 pandemic. BMJ Open 2021;11:e050223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shanafelt TD, Dyrbye LN, West CP. et al. Potential impact of burnout on the US physician workforce. Mayo Clin Proc 2016;91:1667–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. The data underlying this article are available in the article and in its online supplementary material.